Abstract
Over the last 10 years, accumulated experimental and clinical evidence has supported the idea that AT1 receptor subtype is involved in epilepsy. Recently, we have shown that the selective AT1 receptor antagonist losartan attenuates epileptogenesis and exerts neuroprotection in the CA1 area of the hippocampus in epileptic Wistar rats. This study aimed to verify the efficacy of long-term treatment with losartan (10 mg/kg) after kainate-induced status epilepticus (SE) on seizure activity, behavioral and biochemical changes, and neuronal damage in a model of co-morbid hypertension and epilepsy. Spontaneous seizures were video- and EEG-monitored in spontaneously hypertensive rats (SHRs) for a 16-week period after SE. The behavior was analyzed by open field, elevated plus maze, sugar preference test, and forced swim test. The levels of serotonin in the hippocampus and neuronal loss were estimated by HPLC and hematoxylin and eosin staining, respectively. The AT1 receptor antagonism delayed the onset of seizures and alleviated their frequency and duration during and after discontinuation of treatment. Losartan showed neuroprotection mostly in the CA3 area of the hippocampus and the septo-temporal hilus of the dentate gyrus in SHRs. However, the AT1 receptor antagonist did not exert a substantial influence on concomitant with epilepsy behavioral changes and decreased 5-HT levels in the hippocampus. Our results suggest that the antihypertensive therapy with an AT1 receptor blocker might be effective against seizure activity and neuronal damage in a co-morbid hypertension and epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical data suggest a bidirectional link between hypertension and epilepsy and that the risk factors for cardiovascular disease and epilepsy are common. Cerebrovascular damage resulting from chronic hypertension might decrease seizure threshold and predispose to epilepsy (Goel et al. 2012; Scorza et al. 2006), suggesting a vascular contribution to the pathogenic state. Furthermore, seizures onset can activate sympathetic system that in turn causes hypertension and bradyarrhythmia (Beig et al. 2009). A few experimental and clinical reports have demonstrated beneficial activity of antihypertensive and anti-seizure drug combination. Thus, simultaneous treatment with carvedilol and gabapentin has shown good result in hypertensive patients predisposed to epilepsy (Goel et al. 2012), while administration of nifedipine alone or in combination with valproic acid has exerted cardioprotection during ictal state in rats (Beig et al. 2009).
The spontaneously hypertensive rats (SHRs) have been extensively explored as a model of essential hypertension (Okamoto and Aoki 1963; Linthorst et al. 1994), while behavioral patterns have suggested a face validity and the use of this strain as a model of attention-deficit hyperactivity disorder (ADHD) (Sagvolden et al. 2006). Several reports, including ours, have shown that SHRs, compared to normotensive rats, exhibit a low anxiety level, increased locomotion, exploration, and impulsivity leading to deficit in attention and impaired hippocampus-dependent spatial learning in the water maze and radial arm maze tests (De Bruin et al. 2003; Gattu et al. 1997; Gentsch et al. 1987; Kulikov et al. 1997; Petkova et al. 2014; Ramos et al. 2002; Tchekalarova et al. 2010; Wyss et al. 2000). In addition, strain- and area-dependent difference has been demonstrated in the 5-HTergic activity in basal and pathological conditions (Nakamura et al. 2001; Tchekalarova et al. 2015).
The SHRs are characterized by a hyperactive central renin–angiotensin system (RAS), a higher number of AT1 receptors and expression of AT1A mRNA in the hypothalamus compared to their progenitor Wistar-Kyoto (WKY) rats (Raizada et al. 1993). Since the RAS system is known to participate in the control of many physiological and behavioral functions, including regulation of blood pressure, hormonal pituitary gland release, water and salt homeostasis via hypothalamus and brain stem (reviewed in: Wright and Harding 2011), it is reasonable to assume that this system and the activation of angiotensin (Ang) II type 1 (AT1) receptor, in particular, are responsible for the elevated blood pressure in the SHRs (Allen et al. 1998, de Gasparo et al. 1995; Thomas and Mendelsohn 2003). Although AT1 receptors are mostly localized in the anterior pituitary, area postrema, hypothalamus, and CVOs, they are also found in areas involved in the control of brain excitability, including the hippocampus, piriform cortex, lateral geniculate, caudate putamen, amygdala, and septum (Wright et al. 2008). The predominant role of the AT1 receptor in mediating the pathophysiological actions of Ang II underlies the efficacy and broad use of AT1 receptor antagonists in clinical practice for the treatment of hypertension, congestive heart failure, and diabetic nephropathy (Ribeiro-Oliveira et al. 2008). Sartans, including losartan, have been shown to overcome easily brain barrier (Nishimura et al. 2000) and to contribute to a decreased blood pressure and neuronal injury through a blockade of central AT1 receptors (Kawano et al. 1994; Nishimura et al. 2000).
Over the last 10 years, accumulated clinical and experimental evidences have supported the hypothesis that brain AT1 receptor subtype is involved in the regulation of seizure susceptibility (Argañaraz et al. 2008; Łukawski et al. 2010; Pereira et al. 2010; Tchekalarova and Georgiev 2005; Tchekalarova et al. 2014a, b). The elevated levels of RAS components, including increased expression of AT1 receptors in the hippocampus, are verified both in patients with temporal lobe epilepsy (TLE) (Argañaraz et al. 2008) and in two experimental models of epilepsy (Gouveia et al. 2012; Pereira et al. 2010). Although the functional meaning of these plastic changes has not been fully elucidated, the experimental results suggest that up-regulated AT1 receptors under epileptic conditions might be involved in the mechanism of enhanced seizure susceptibility.
The importance of increased hippocampal monoamine neurotransmission for limiting seizure development has been established earlier (Linthorst et al. 1994; Łukawski et al. 2010, 2014), and therefore, it is interesting to have also knowledge about possible changes in seizure-evoked hippocampal neurotransmitter dialysate levels in SHRs.
Losartan potentiated the anticonvulsant effect of antiepileptic drugs (AEDs), valproate and lamotrigine, in the mouse test of maximal electroshock (Łukawski et al. 2010, 2014). Furthermore, long-term administration of this AT1 receptor antagonist was able to prevent the development of spontaneous recurrent seizures (SRS) after vascular injury and brain exposure to albumin (Bar-Klein et al. 2014) and to alleviate seizure intensity in Wistar audiogenic rat (WAR) (Pereira et al. 2010). Recently, our group has reported that long-term blockade of AT1 receptors after kainate (KA)-induced status epilepticus (SE) can exert disease-modifying activity on epileptogenesis in normotensive Wistar rats (Tchekalarova et al. 2014a, b). In view of the accumulated evidence that broadly used antihypertensive AT1 receptor drugs might also be considered as a relevant therapeutic target in epilepsy, in the present study, we further demonstrate that the continuous AT1 receptor blockade after SE is efficient against SRS and neuronal damage in the hippocampus using a model of co-morbid hypertension and epilepsy.
Materials and Methods
The study was conducted according to the European Communities Council Directive 2010/63/EU for the protection of animals used for scientific purposes. The experimental design was approved by the Institutional Ethics Committee at the Institute of Neurobiology and the Ethics Committees for research at the Sofia Medical University, contract No. 30/2011 for the application grant DTK 02/56 2009–2012.
Subjects
Adult (two-month aged) male SHRs were obtained from the local breeding house of the Medical University of Sofia. Each animal was single caged upon arrival on a controlled 12 h light/dark cycle (lights on at 08:00 h) at standard temperature (20 ± 3 °C) and humidity (40–50 %). The rats were habituated for 10 days and handled daily during this period. Throughout the study, food and water were given ad libitum except during the testing. All tests were carried out in the autumn–winter season.
Experimental Design and Drug Treatment
The study design is described in Fig. 1. The rats were allocated at random to the following four experimental groups: (I) vehicle control group, referred to as C-veh (n = 10); (II) losartan control group, (C-los) (n = 10); (III) kainate vehicle group, (KA-veh) (n = 15); and (IV) kainate losartan group, (KA-los) (n = 15). The observers who conducted the experiments were blinded to the treated groups. Two additional groups with implanted electrodes used preferably for video- and EEG analysis were added as follows: EEG-KA-veh (n = 7) and EEG-KA-los (n = 7). Treatment with losartan (gifted by MERCK&CO., INC, New Jersey, USA) started 2 h after the beginning of SE at a dose of 10 mg/kg, previously shown to alleviate seizure activity and to have antioxidant activities (Pechlivanova et al. 2010; Tchekalarova et al. 2014a, b). During the first 6 days after SE, losartan was injected subcutaneously (s.c.) (10 mg/kg at a volume of 20 ml) in lactated Ringer’s as the animals were unable to drink via bottles. Matched control groups were injected with losartan or vehicle, respectively. A week after SE, losartan, diluted in drinking water, was administered via drinking water as described previously (Tchekalarova et al. 2014a, b). The amount of the drinking water containing losartan was adjusted daily based on the individual volume of liquid consumed the previous day.
Induction of Status Epilepticus with Kainic Acid
Kainic acid was diluted in sterile saline (0.9 % NaCl) at a dose of 2.5 mg/ml. The protocol of KA-induced SE was performed as previously described (Tchekalarova et al. 2014a, b), according to Hellier et al. (1998) with a minor modification in order to decrease the mortality of rats experiencing SE. The seizure intensity was evaluated using the modified Racine’s scale (1972) as follows: class III, forelimb clonus with lordotic posture; class IV, rearing and continued forelimb clonus; and class V, forelimb clonus and loss of the posture. Only rats which developed SE (i.e., recurrent seizures of class IV or V for at least 3 h) and survived thereafter were included in the subsequent analyses.
Surgery and EEG Recording
Experimental groups for EEG analysis were anesthetized with ketamine (40 mg/kg, i.p.) and xylazine (20 mg/kg, i.m.). Following local anesthesia with procaine 0.5 % and fixation in a stereotaxic device (Narishige Sci. Inst. Labs, Japan), silver ball wire (200 µm) (Biomed Instr., Germany) was inserted into pre-made small holes in the calvaria bilaterally of both hemispheres above the frontal (A = +1, L = ±2) and parietal cortical areas (A = −4.2, L = ±3.0). The reference and the ground electrodes were placed into the occipital bone. All electrodes were connected to a six-plug female connector, and the whole assembly was attached to the skull by means of fast curing dental acrylic. After the surgery, the rats were allowed to recover for 1 week before the first control EEG recordings. Simultaneous EEG and video recording was performed in two separate monitoring periods during losartan treatment (15–30 days after SE) and more than a month after discontinuation of treatment (70–90 days after SE), respectively, for a period of 1 h three times a week. Visual detection of ictal events was performed through inspections of the EEG files recorded by means of the AcqKnowledge software ACK100 W (BIOPAC Inc., USA). The criteria for epileptic seizures were abrupt onset of epileptiform activity that lasted at least 5 s and amplitude that was two times higher compared with the baseline EEG.
Video Monitoring of Spontaneous Recurrent Seizures
Spontaneous motor seizures (24 h/day for 12 weeks) of class IV or V (secondarily generalized seizures) were detected by two independent observers through video-software in a computer connected with an infrared-sensitive colored camera (S-2016, AVTECH, Taiwan, no. AVC307R). No partial seizures of classes I and II without simultaneous EEG recording were taken into consideration because they could easily be missed. All additional spontaneous seizures detected during the experimental manipulations were taken into account as well. Latency for onset of the first motor seizure and seizure frequency per day were evaluated.
Behavioral Tests
All tests were performed during losartan treatment (20–30 days after SE) (Ist trial) and a month after discontinuation of treatment (70–80 days after SE) (IInd trial), respectively. Time interval between the behavioral tests was at least 2 days. They were performed in two time points: 6 h after lights on (15:00 p.m.) under artificial diffused light during and after lights off (03:00 a.m.) under red dim light. The behavioral experiments were conducted in a soundproof room, where the animals were moved at least 30 min before each test. In case a rat had seizure within 1 h before starting the test, it was excluded from the experimental procedure. The behavior was recorded using an infrared-sensitive CCD camera and a video tracking system (SMART PanLab software, Harvard Apparatus, USA).
Open Field Test
The apparatus consisted of a gray polystyrene box (100 × 100 × 60 cm3) divided into two zones: outer square (periphery) and inner square (center). The rat was placed in the center of the box and was allowed to explore it for 5 min. The calculated standard measures were as follows: (1) total distance traveled (cm); (2) time spent in the central zone (s) versus total time in %; and (3) an anxiety index calculated using the following equation: After each test, the OF apparatus was thoroughly cleaned with 0.1 % acetic acid solution to prevent any odor traces.
Elevated Plus Maze Test
The apparatus consisted of two open arms (50 × 10 cm2), two enclosed arms (50 × 10 × 50 cm3), and a central platform (10 × 10 cm2) elevated 50 cm above the floor level. At the beginning of the test, the rat was placed on the central platform facing an open arm. The test lasted 5 min. The calculated standard measures were as follows: 1) total distance traveled (cm); 2) time (s) spent in the open arms versus total time in %. After each test elevated plus maze (EPM) was cleaned with 0.1 % acetic acid solution.
Sucrose Preference Test
The test for evaluating hedonic state was performed as described previously (Tchekalarova et al. 2011). Sucrose preference was expressed as a percentage of the volume of sucrose solution of the total amount of liquid (sucrose plus regular water) consumed during 12 h (light phase—8:00–20:00 h and dark phase—20:00–8:00 h).
Forced Swim Test
The despair-like behavior was evaluated by a classic forced swim test (Porsolt et al. 1979) as previously described (Tchekalarova et al. 2011). Two swim sessions were conducted: 15 min of training followed by a 5-min test session 24 h later. After each test, the rat was dried and kept warm by a heating device for 10 min. The immobility (s), which occurred when the rat remained motionless, or made only movements necessary to keep its head above the water, was recorded.
Histology
After a deep anesthesia with urethane (1500 mg/kg, i.p., Sigma-Aldrich) (n = 5 per group), rats were transcardially perfused initially with 0.05 M phosphate buffered saline, at pH 7.3 followed by 4 % paraformaldehyde in 0.1 M phosphate buffer (PB), at pH 7.3. The brains were dissected out and postfixed overnight at 4o C in the same fixative solution. After postfixation, the brains were sliced in the coronal plane; the tissue blocks were washed in PB, embedded in paraffin, and cut into 5-μm-thick sections. The samples were then deparaffinized with xylene and ethanol, and routinely stained with hematoxylin and eosin to better identify pyknotic nuclei of damaged neurons. The sections were investigated on a Nikon Eclipse 80i light microscope (Japan), and photographed with a digital camera (Nikon DMX 1200). Sections were analyzed for major cell loss with special attention to the dorsal and ventral hippocampi as previously described (Tchekalarova et al. 2014a, b). The staining intensity and density of nerve cell bodies were estimated using Nikon’s NIS Elements Digital Imaging software. The relative neuronal densities of the selected brain areas were quantified by determining the percentage of the measurement grid occupied by stained cells. The resulting values provide a relative index of the number of stained neurons in the selected brain areas.
High-Performance Liquid Chromatography
Eight rats from each group were used for HPLC analysis. After light anesthesia with CO2, the rats were decapitated, brains were quickly dissected on ice, and hippocampi and frontal cortex were removed bilaterally. The tissue samples were frozen in liquid nitrogen, lyophilized, and stored at −70 °C before HPLC analysis as previously described (Tchekalarova et al. 2011).
Statistical Analysis
Parametric (for normally distributed data) or nonparametric tests (for data not normally distributed) were used for the statistical analysis (SigmaStat® 11.0). Experimental data were evaluated by ANOVA analysis of variance with Condition (Control vs KA), Drug (Vehicle vs losartan), Phase (Light vs Dark) as between-group factors. Group differences after significant ANOVAs were measured by post hoc Bonferroni or Holm Sidak test. If data were not normally distributed, ANOVA for nonparametric data (Kruskal–Wallis on ranks) followed by the Mann–Whitney U test was used. A p < 0.05 value was accepted for statistical significance.
Results
Seizure Activity
The EEG recordings in the KA-veh and KA-los groups before, during SE, latent and chronic phases are demonstrated in Fig. 2a, b.
EEG activity from the left and right frontal (FrL and FrR) and parietal cortices (PL and PR) in a SHR from the kainate vehicle (KA-veh) group (a) and a rat from the KA-losartan (KAlos) group (b). The control records before KA-induced status epilepticus (Aa, Ba), during the latent (Ab, Bb), and the chronic phase (Ac, Bc) are presented. Calibration: 10 s, 100 µV
Repetitive injection of KA at a low subconvulsive dose led to SE in rats after approximately 3 h, and the average dose required to induce SE was median ± S.D: 18.79 ± 5.5 mg/kg; range: 20–30 mg/kg. Five out of 44 rats (11 %) died during SE. The final number of survived rats per group treated with KA was as follows: 14 (KA-veh), 14 (KA-los), 5 (EEG- KA-veh), and 6 (EEG- KA-los), respectively. The losartan treatment during epileptogenesis significantly delayed the onset of the first spontaneous seizure in SHRs (median ± SD: 23 ± 2.2 days; range 9–99 days KA-los group versus KA-veh group: median ± SD: 12 ± 6 days; range 5–26 days) (Mann–Whitney Rank Sum Test: T = 177; p = 0.022). The EEG recording did not show obvious difference during the latent phase compared to the baseline EEG activity but only sporadic spike activity. The losartan treatment did not prevent development of epilepsy and onset of spontaneous seizures. However, the number of paroxysmal events and their duration was significantly decreased during the two monitoring periods in the losartan-treated group (Tables 1, 2). The video-monitored behavioral motor seizures were also with significantly lower frequency during losartan treatment (Ist month) and after discontinuation of treatment (IInd–IVth month after SE) (Fig. 3) (*p < 0.05). Compared to the KA-veh group, no progression of seizure activity was demonstrated in the KA-los group (o p < 0.05).
A daily seizure frequency monitored by a 24-h video recording in KA-veh (n = 14) and KAlos (n = 14) groups from the Ist to the IVth month after SE. Data are mean ± SEM. Repeated ANOVA indicated a main effect of Condition [F1, 110 = 13.158, p < 0.001]. *p < 0.05 between groups (vs KA-veh group); o p < 0.05 within a group (Kruskal–Wallis test)
Behavioral Tests
Open Field Test
Diurnal fluctuations of total activity were detected only in control rats (Ist and IInd trials) (# p < 0.05) (Fig. 4a, b). Losartan treatment caused hypolocomotion in control rats, mainly during the light phase, which effect was preserved a month after drug washout (*p < 0.05). However, the blockade of AT1 receptors did not affect the KA-induced hyperlocomotion during both the light and dark phases (Ist and IInd trials) (p > 0.05). During the period of treatment, losartan did not influence the KA-induced decrease in anxiety level, measured by time spent in the aversive central zone, but a month after its discontinuation, a phase-dependent alleviating effect to control level was demonstrated during the light phase (*o p < 0.05) (Fig. 5a, b). The same tendency was observed during the dark phase.
Diurnal variations of locomotor activity in open field test measured by total distance traveled (cm) during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—a main condition effect [F 1.90 = 46.890, p < 0.001] and Phase effect [F 1.90 = 17.945, p < 0.001]; b For the IInd trial—a main condition effect [F 1.89 = 59.759, p < 0.001] and phase effect [F 1.89 = 11.838, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Diurnal variations of anxiety level measured by time spent in center versus total time (%) in the open field test during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—a main phase effect [F 1.88 = 10.533, p < 0.02] as well as condition × phase interaction [F 1.88 = 5.624, p < 0.019]; b For the IInd trial—a main condition effect [F 1.90 = 8.138, p < 0.005], drug effect [F 1.90 = 6.806, p < 0.010], and phase effect [F 1.90 = 12.101, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Elevated Plus Maze Test
Like in the OF test, total activity of control rats was characterized by diurnal fluctuations in the EPM test (Ist and IInd trials) (# p < 0.05). Losartan treatment caused hypolocomotion during both the light and dark phases in control rats (*p < 0.05) (Fig. 6a, b). Furthermore, the AT1 receptor antagonism was unable to alleviate the increased motor activity of rats after SE (Ist and IInd trials) (* p < 0.05). Losartan produced an anxiogenic effect in the control group measured by the ratio of time spent in the open arms versus total time during both the light and the dark phases, respectively (Ist and IInd trials) (*p < 0.05) (Fig. 7a, b).
Diurnal variations of locomotor activity in elevated plus maze test measured by total distance traveled (cm) during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—a main condition effect [F 1.90 = 30.528, p < 0.001] and phase effect [F 1.90 = 9.104, p < 0.003]; b For the IInd trial—a main condition effect [F 1.90 = 64.689, p < 0.001] and phase effect [F 1.90 = 12.880, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Diurnal variations of anxiety level measured by time spent in open arms versus total time (%) in the elevated plus maze test during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—a main condition effect [F 1.90 = 10.922, p < 0.001], drug effect [F 1.90 = 13.092, p < 0.001] as well as condition × drug interaction [F 1.90 = 6.813, p < 0.010]; b For the IInd trial—a main condition effect [F 1.90 = 22.860, p < 0.001], drug effect [F 1.90 = 15.439, p < 0.001], phase effect [F 1.90 = 13.101, p < 0.001], as well as condition × drug interaction [F 1.90 = 12.221, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Sucrose Preference Test
Controls and epileptic rats exhibited diurnal fluctuations in the sugar preference test (SPT) with higher preference to sweet solutions during the dark phase (Ist and IInd trail) (# p < 0.05) (Fig. 8a, b). Losartan treatment tended to increase the preference to sweet solutions in control conditions during the light phase of the Ist trial with significant effect after discontinuation of drug exposure (* p < 0.05). However, losartan exposure was unable to prevent a co-morbid anhedonia in the KA-treated rats (o p < 0.05).
Diurnal variations in sucrose consumption test during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—a main effect of condition [F 1.90 = 8.647, p < 0.004], phase effect [F 1.90 = 15.948, p < 0.001] as well as condition × drug × phase interaction [F 1.90 = 11.899, p < 0.001]; b For the IInd trial—a main condition effect [F 1.90 = 12.872, p < 0.001], phase effect [F 1.90 = 26.925, p < 0.001], as well as condition × drug × phase interaction [F 1.90 = 14.802, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Forced Swim Test
Losartan treatment did not prevent the depressive-like behavior as a consequence of SE during the treatment period and after its discontinuation (Fig. 9a, b) (* p < 0.05).
Diurnal variations of immobility time (s) in the forced swim test during the Ist trial and the IInd trial. Data are mean ± SEM (n = 10–15). Three-way ANOVA indicated: a For the Ist trial—condition × phase interaction [F 1.89 = 15.865, p < 0.001], as well as condition × drug × phase interaction [F 1.89 = 3.935, p < 0.05]. b For the IInd trial—a main phase effect [F 1.90 = 9.193, p < 0,003] and condition × phase interaction [F 1.90 = 17.726, p < 0.001]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats, # p < 0.05 within a group (15:00 h vs 03:00 h)
Histology
The KA-induced neurotoxicity caused a severe neuronal loss in the CA1 and CA3 areas of the hippocampus as well as in the dentate gyrus hilus area, preform cortex, and basolateral amygdala in the KA-veh group, (*p < 0.05 vs C-veh) (Figs. 10a, b, c, d, 11a, b, 12a, b). The long-term losartan treatment during epileptogenesis prevented the neuronal damage selectively in the CA3 area of the hippocampus and in the septo-temporal dentate gyrus hilus area of epileptic rats (o p < 0.05) (Figs. 10a, b, c, d, 11a, b). Partial neuroprotection in the KA-los group was detected in the basolateral amygdala (Fig. 12a, b).
Representative hematoxylin and eosin-stained coronal sections of the hippocampal formation of a control rat (a), an epileptic rat treated with a vehicle after SE (b) and an epileptic rat treated with losartan after SE (c). The representative images on the right panels are higher magnifications of the boxed areas in the left images from the CA1 and CA3c areas of the hippocampus, respectively. The KA-veh rats (b) showed severe neuronal loss in CA1 and CA3 pyramidal cell layers, and the hilus of the dentate gyrus (DG) when compared to the control rats (a). The KA-los rats did not obviously differ from controls. Scale bars = 200 µm (a–f); 50 µm in higher-magnification insets (b)
Histology scores (Nissl staining) during epileptic chronic phase in a the hippocampus—CA1, CA3a CA3c; in b the hilus of the dentate gyrus. *p < 0.05 versus C-veh group; o p < 0.05 versus KA-veh group. Two-way ANOVA for the hippocampus indicated a CA1 for the septal: condition effect [F 1.9 = 4,365, p < 0.050]; septo-temporal: condition effect [F 1.9 = 15.234, p < 0.005]; temporal: condition effect [F 1.9 = 26.422, p < 0.001]; CA3a for the septal: condition effect [F 1.9 = 8.189, p < 0.024]; septo-temporal: condition effect [F 1.9 = 20.393, p < 0.002] and drug effect [F 1.9 = 10.203, p < 0.013]; temporal: condition effect [F 1.9 = 27.089, p < 0.001]; CA3c for the septal: condition effect [F 1.9 = 17.260, p < 0.004] and drug effect [F 1.9 = 10.618, p < 0.014]; septo-temporal: condition effect [F 1.9 = 16.125, p < 0.004] and drug effect [F 1.9 = 7.350, p < 0.027]; temporal: condition effect [F 1.9 = 28.693, p < 0.001] and drug effect [F 1.9 = 16.441, p < 0.004]. Two-way ANOVA for the hilus of DG indicated b for the septal: condition effect [F 1.9 = 16.578, p < 0.005]; septo-temporal: condition effect [F 1.9 = 131.349, p < 0.001] and drug effect [F 1.9 = 46.643, p < 0.001]; temporal: condition effect [F 1.9 = 6.157, p < 0.042]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats
Histology scores during epileptic chronic phase in a the piriform cortex and in b the basolateral amygdala. Two-way ANOVA for the piriform cortex indicated a condition effect [F 1.14 = 15.411, p < 0.002]. Two-way ANOVA for the basolateral amygdala indicated b for the septal: condition effect [F 1.9 = 30.093, p < 0.001]; septo-temporal: condition effect [F 1.9 = 8.187, p < 0.024] and drug effect [F 1.9 = 46.643, p < 0.001]; temporal: condition effect [F 1.9 = 14.050, p < 0.010]. *p < 0.05 versus controls, o p < 0.05 versus KA-treated rats
High-Performance Liquid Chromatography
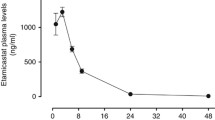
The level of 5-HT in the frontal cortex and the hippocampus was evaluated using the HPLC system. No difference for the 5-HT levels in the frontal cortex was detected among groups (Fig. 13a). Long-term losartan treatment significantly decreased the 5-HT levels in the hippocampus of both the C-los and the KA-los groups, respectively (Fig. 13b) (*o p < 0.05).
Discussion
In the present study, we demonstrated that long-term treatment with losartan, a selective AT1 receptor antagonist, after KA-induced SE exerted a disease-modifying effect on the spontaneous seizure activity and the neuronal damage in a co-morbid model of hypertension and epilepsy. Identically with these results, recently we have reported that losartan is able to attenuate seizure frequency, neuronal damage, and behavioral changes caused by KA-induced SE in normotensive Wistar rats (Tchekalarova et al. 2014a, b). The seizure-attenuating efficacy was still evident 3 months after discontinuation of the treatment suggesting a potential antiepileptogenic activity of losartan in the SHRs. However, the AT1 receptor blockade was unable to prevent the development of epileptogenesis and onset of spontaneous seizures. Our results agree with a report of Pereira et al. (2010) showing that orally given losartan at a higher dose of 50 mg/kg for 21 days to WARs decreased limbic seizures from day 8 of the acoustic stimulation and from day 15 of the drug treatment, respectively, while tonic–clonic seizures were influenced from the first day of the stimuli and 7 days from losartan exposure. Moreover, the activity of losartan on limbic seizures was comparable to that of the ACE inhibitor enalapril but higher regarding mesencephalic seizures, which effect was accompanied by lowering of the systolic blood pressure. Recently, Bar-Klein et al. (2014) revealed that systemic administration of losartan via drinking water (2 g/l) for 21 days suppressed epileptogenesis in a model of vascular injury and cortical exposure to albumin in Wistar rats. The underlying mechanism of losartan activity was suggested to involve either suppression of TGF-β signaling or AT1 receptor blockade or both.
Unlike the above-mentioned models of epilepsy, losartan did not show any activity in acute seizure tests in naive animals (Łukawski et al. 2010; Tchekalarova and Georgiev 1999). It is worth mentioning that in the three doses used, losartan was inactive in maximal electroshock seizure (MES) test just like telmisartan (Łukawski et al. 2010). However, co-injection of a single higher dose of losartan (50 mg/kg) potentiated the anticonvulsant effect of valproate and lamotrigine without affecting plasma or brain drug levels suggesting pharmacodynamic interactions (Łukawski et al. 2010, 2014). Our previous data have demonstrated that the biologically active neuropeptides Ang II, Ang III, and Ang IV exerted anticonvulsant activity in acute pentylenetetrazol (PTZ) seizure test and in PTZ kindling model of epilepsy in mice (Tchekalarova and Georgiev 2005). The anticonvulsant activity of Ang IV was also detected in pilocarpine seizure test in rats (Stragier et al. 2006). However, the combination of intracerebroventricular injection of ineffective doses of Ang II and losartan produced an anticonvulsant effect in PTZ-kindled mice (Georgiev et al. 1996).
A number of studies revealing that one of the mechanisms underlying barrier leakage is the increased blood pressure (Johansson 1981; Ndode-Ekane et al. 2010; Cornford and Oldendorf, 1986) suggest vulnerability of hypertension to blood–brain barrier (BBB) damage. On the other hand, both experimental and clinical results revealed that a breakdown of BBB before, during, and after seizures can cause extravasation of plasma constituents and vasogenic brain edema (Gorter et al. 2015; Ndode-Ekane et al. 2010; Van Vliet et al. 2007). Previous reports demonstrated that a repeated losartan treatment is effective in prevention of BBB permeability in hypertensive rats (Kaya et al. 2003; Kucuk et al. 2002) suggesting that this drug might be also protective against barrier leakage in epileptic conditions, as well as epilepsy accompanied with hypertension. However, further studies are required to explore this hypothesis. Losartan has been earlier demonstrated to decrease the central sympathetic nerve activity in hypertensive rats (Ye et al. 2002). Although in this study blood pressure was not measured in epileptic condition, we can assume that long-term exposure to 10 mg/kg losartan decreased the blood pressure based on the results reported earlier in naive SHRs (Pechlivanova et al. 2010).
Behavioral data related to losartan treatment have often been encountered controversial findings because of the divergence in the experimental protocols among laboratories and can be also attributed to differences in treatment routes (central vs systemic or single vs repeated) and strains used. Srinivasan et al. (2003) showed that acute injection of 10 mg/kg losartan increased locomotion of normotensive Wistar rats while alleviated hyperactivity in naive SHRs. In the present study, the long-term losartan treatment decreased the motor activity of SHRs specifically during the light phase, which results agree with decreased locomotion after AT1 receptor blockade in normotensive rats (Tchekalarova et al. 2014a, b). However, unlike in epileptic Wistar rats (Tchekalarova et al. 2014a, b), the AT1 receptor antagonist losartan did not prevent KA-induced hyperactivity of SHRs, suggesting a strain-specific response as a result of the AT1 receptor blockade under pathological state. Our present findings correspond to previous reports of other researchers that in addition to hypertensive conditions, epileptogenesis is also crucial for the activity of the AT1 receptors causing their up-regulation in the hippocampus both in animal models of epilepsy and in patients with epilepsy (Gouveia et al. 2012; Pereira et al. 2010).
Patients with co-morbid hypertension and depression have shown significant emotional and mood improvement when were exposed on ACE inhibitor therapy—captopril and enalapril instead of other antihypertensive drugs (Braszko et al. 2003; Germain and Chouinard 1988, 1989). Antidepressant activity of AT1 receptor blockers, including losartan, has been demonstrated only in screening tests for antidepressant activity in naive rats but not in models of depression (Gard et al. 1999; Nayak and Patil 2008; Vijayapandi and Nagappa 2005). Recently, Pedreañez et al. (2011) reported that long-term losartan pretreatment alleviated depressive-like responses of renal oxidative stress in rats induced by repeated FSTs. In the present study, we addressed the role of the hippocampal 5-HT to the effects of losartan on anxiety and depression in KA-treated SHRs. While our previous work in Wistar rats has demonstrated potent antidepressant activity of AT1 receptor antagonism, which is in agreement with literature data, the present results showed that in hypertensive rats, the long-term losartan treatment after SE was unable to alleviate associated with epileptogenesis depressive-like behavior during the light phase. In addition, losartan treatment caused 5-HT deficit in the hippocampus in both intact and KA-treated SHRs. Recently, we have found that long-term AT1 receptor blockade alleviated depressive-like behavior in epileptic normotensive Wistar rats, which beneficial effect was associated with decreased hippocampal levels of 5-HT. Therefore, the present findings, together with our previous report on Wistar rats, indicated strain-specific outcome on depression developed during epileptogenesis and a lack of direct link between emotional disturbance and serotoninergic neurotransmission.
In agreement with our previous results and a report of Sun et al. (2015), the KA-induced neuronal damage was detected mainly in the hippocampus, the piriform cortex, and the basolateral amygdala in SHRs (Petkova et al. 2014, Tchekalarova et al. 2014a, b). In the present study, the long-term losartan treatment alleviated SE-induced neuronal damage specifically in the CA3c area of the hippocampus and the septo-temporal hilus of the dentate gyrus. Recently, we have reported that a repeated losartan or Ang II treatment during epileptogenesis exerted a neuroprotection mainly in the CA1 area of the hippocampus in Wistar rats (Tchekalarova et al. 2014a, b, Ivanova et al. 2015), suggesting a strain-dependent difference in the brain structures involved in the neuroprotective activity of losartan and a possible role of the AT2 receptors, which were reported to be up-regulated under pathological conditions both in humans with epilepsy (Argañaraz et al. 2008) and in a rat model of epilepsy (Pereira et al. 2010). The stronger potency of the selective AT1 receptor antagonist against the KA-induced neurotoxicity in SHRs than in Wistar rats is in accordance with our recent finding that the efficacy of a sub-chronic losartan infusion on the KA-induced SE, and oxidative stress is more pronounced in a model of essential hypertension.
In conclusion, the present results confirmed our previous ones and those of other authors that the AT1 receptor blockade might be used as an effective adjuvant therapy in a co-morbid hypertension and epilepsy. Like in normotensive rats, losartan diminished seizure activity in both the period of exposure and after discontinuation of the treatment and exerted neuroprotection in specific brain regions, suggesting common long-term plastic changes against development of epileptogenesis in SHRs. Despite the AT1 receptor blockade had beneficial effect on SE-induced behavioral changes in Wistar rats, it was unable to affect hyperactivity and depression in hypertensive rats. In addition, while losartan exerted neuroprotection in the CA1 area of the hippocampus in Wistar rats, the AT1 receptor antagonism had beneficial effect in the CA3 area and the hilus of dentate gyrus in SHRs. Further experiments are needed to explain the mechanism underlying strain-specific responses of losartan treatment in KA model of TLE.
References
Allen AM, Mbeller I, Jenkins TA, Zhuo J, Aldred GP, Chai SY, Mendelsohn FAO (1998) Angiotensin receptors in the nervous system. Brain Res Bull 47:17–28
Argañaraz GA, Konno AC, Perosa SR, Santiago JF, Boim MA, Vidotti DB, Varella PP, Costa LG, Canzian M, Porcionatto MA, Yacubian EM, Sakamoto AC, Carrete H Jr, Centeno RS, Amado D, Cavalheiro EA, Jnaj JA, Mazzacoratti MG (2008) The renin-angiotensin system is upregulated in the cortex and hippocampus of patients with temporal lobe epilepsy related to mesial temporal sclerosis. Epilepsia 49:1348–1357
Bar-Klein G, Cacheaux LP, Kamintsky L, Prager O, Weissberg I, Schoknecht K, Cheng P, Kim SY, Wood L, Heinemann U, Kaufer D, Friedman A (2014) Losartan prevents acquired epilepsy via TGF-β signaling suppression. Ann Neurol 75:864–875
Beig MI, Chandra R, Talwar A, Fahim M, Katyal A (2009) Epileptic seizure-induced hypertension and its prevention by calcium channel blockers: a real-time study in conscious telemetered rats. Can J Physiol Pharmacol 87:572–580
Braszko JJ, Karwowska-Polecka W, Halicka D, Gard PR (2003) Captopril and enalapril improve cognition and depressed mood in hypertensive patients. J Basic Clin Physiol Pharmacol 14:323–343
Cornford EM, Oldendorf WH (1986) Epilepsy and the blood-brain barrier. Adv Neurol 44:787–812
De Bruin NM, Kiliaan AJ, De Wilde MC, Broersen LM (2003) Combined uridine and choline administration improves cognitive deficits in spontaneously hypertensive rats. Neurobiol Learn Mem 80:63–79
De Gasparo M, Husain A, Alexander W, Catt KJ, Chiu AT, Drew M, Goodfriend T, Harding JW, Inagami T, Timmermans PB (1995) Proposed uptade of angiotensin receptor nomenclature. Hypertension 25:924–939
Gard PR, Mandy A, Sutcliffe MA (1999) Evidence of a possible role of altered angiotensin function in the treatment, but not etiology, of depression. Biol Psychiatry 45:1030–1034
Gattu M, Terry AV Jr, Pauly JR, Buccafusco JJ (1997) Cognitive impairment in spontaneously hypertensive rats: role of central nicotinic receptors. Part II. Brain Res 771:104–114
Gentsch C, Lichtsteiner M, Feer H (1987) Open field and elevated plus-maze: a behavioural comparison between spontaneously hypertensive (SHR) and Wistar-Kyoto (WKY) rats and the effects of chlordiazepoxide. Behav Brain Res 25:101–107
Georgiev VP, Lazarova MB, Kambourova TS (1996) Effects of non-peptide angiotensin II-receptor antagonists on pentylenetetrazol kindling in mice. Neuropeptides 30:401–404
Germain L, Chouinard G (1988) Treatment of recurrent unipolar major depression with captopril. Biol Psychiatry 23:637–641
Germain L, Chouinard G (1989) Captopril treatment of major depression with serial measurements of blood cortisol concentrations. Biol Psychiatry 25:489–493
Goel R, Goel A, Kumar Y (2012) Hypertension: a major factor for epilepsy. Carvedilol potentiates gabapentin effect. LAP Lambert Acad Publ Germany, Saarbrùcken, p 84
Gorter JA, van Vliet EA, Aronica E (2015) Status epilepticus, blood-brain barrier disruption, inflammation, and epileptogenesis. Epilepsy Behav 49:13–16
Gouveia TL, Frangiotti MI, de Brito JM, de Castro Neto EF, Sakata MM, Febba AC, Casarini DE, Amado D, Cavalheiro EA, Almeida SS, Manchini MT, Araújo RC, Silva JA Jr, Naffah-Mazzacoratti Mda G (2012) The levels of renin-angiotensin related components are modified in the hippocampus of rats submitted to pilocarpine model of epilepsy. Neurochem Int 61:54–62
Hellier JL, Partylo PR, Buckmaster PS, Dudek FE (1998) Recurrent spontaneous motor seizures after repeated low-dose systemic treatment with kainate: assessment of a rat model of temporal lobe epilepsy. Epilepsy Res 31:73–84
Ivanova N, Pechlivanova D, Atanasova D, Mitreva R, Lazarov N, Stoynev Al, Tchekalarova J (2015) Long-term intracerebroventricular infusion of angiotensin II after kainate-induced status epilepticus: Effects on epileptogenesis, brain damage and diurnal behavioral changes. Epilepsy Behav 51:1–12
Johansson BB (1981) Indomethacin and cerebrovascular permeability to albumin in acute hypertension and cerebral embolism in the rat. Exp Brain Res 42:331–336
Kawano Y, Yoshida K, Matsuoka H, Omae T (1994) Chronic effects of central and systemic administration of losartan on blood pressure and baroreceptor reflex in spontaneously hypertensive rats. Am J Hypertens 7:536–542
Kaya M, Kalayci R, Küçük M, Arican N, Elmas I, Kudat H, Korkut F (2003) Effect of losartan on the blood-brain barrier permeability in diabetic hypertensive rats. Life Sci 73:3235–3244
Kucuk M, Kaya M, Kalayci R, Cimen V, Kudat H, Arican N, Elmas I, Korkut F (2002) Effects of losartan on the blood-brain barrier permeability in long-term nitric oxide blockade-induced hypertensive rats. Life Sci 71:937–946
Kulikov A, Aguerre S, Berton O, Ramos A, Mormede P, Chaouloff F (1997) Central serotonergic systems in the spontaneously hypertensive and Lewis rat strains that differ in the elevated plus-maze test of anxiety. J Pharmacol Exp Ther 281:775–784
Linthorst AC, van Giersbergen PL, Gras M, Versteeg DH, de Jong W (1994) The nigrostriatal dopamine system: role in the development of hypertension in spontaneously hypertensive rats. Brain Res 639:261–268
Łukawski K, Janowska A, Jakubus T, Tochman-Gawda A, St Czuczwar (2010) Angiotensin AT1 receptor antagonists enhance the anticonvulsant action of valproate in the mouse model of maximal electroshock. Eur J Pharmacol 640:172–177
Łukawski K, Janowska A, Jakubus T, Czuczwar SJ (2014) Interactions between angiotensin AT1 receptor antagonists and second-generation antiepileptic drugs in the test of maximal electroshock. Fundam Clin Pharmacol 28:277–283
Nakamura K, Shirane M, Koshikawa N (2001) Site-specific activation of dopamine and serotonin transmission by aniracetam in the mesolcorticolimbic pathway of rats. Brain Res 897:82–92
Nayak V, Patil PA (2008) Antidepressant activity of fosinopril, ramipril and losartan, but not of lisinopril in depressive paradigms of albino rats and mice. Indian J Exp Biol 46:180–184
Ndode-Ekane XE, Hayward N, Gröhn O, Pitkänen A (2010) Vascular changes in epilepsy: functional consequences and association with network plasticity in pilocarpine-induced experimental epilepsy. Neuroscience 166:312–332
Nishimura Y, Ito T, Saavedra JM (2000a) Angiotensin II AT(1) blockade normalizes cerebrovascular autoregulation and reduces cerebral ischemia in spontaneously hypertensive rats. Stroke 31:2478–2486
Nishimura Y, Ito T, Hoe K, Saavedra JM (2000b) Chronic peripheral administration of the angiotensin II AT(1) receptor antagonist candesartan blocks brain AT(1) receptors. Brain Res 871:29–38
Okamoto K, Aoki K (1963) Development of a strain of spontaneously hypertensive rats. Jpn Circ J 27:282–293
Pechlivanova D, Markova P, Stoynev A (2010) Effect of the AT1 receptor antagonist losartan on diurnal variation in pain threshold in spontaneously hypertensive rats. Methods Find Exp Clin Pharmacol 32:663–668
Pedreañez A, Arcaya JL, Carrizo E, Rincón J, Viera N, Peña C, Vargas R, Mosquera J (2011) Experimental depression induces renal oxidative stress in rats. Physiol Behav 104:1002–1009
Pereira M, Becari C, Oliviera J, Salgadoc O, Garcia-Cairasco N, Costa-Net C (2010) Inhibition of the renin–angiotensin system prevents seizures in a rat model of epilepsy. Clin Sci 119:477–482
Petkova Z, Tchekalarova J, Pechlivanova D, Moyanova S, Kortenska L, Mitreva R, Popov D, Markova P, Lozanov V, Atanasova D, Lazarov N, Stoynev A (2014) Treatment with melatonin after status epilepticus attenuates seizure activity and neuronal damage but does not prevent the disturbance in diurnal rhythms and behavioral alterations in spontaneously hypertensive rats in kainate model of temporal lobe epilepsy. Epilepsy Behav 31:198–208
Porsolt RD, Bertin A, Blavet N, Deniel M, Jalfre M (1979) Immobility induced by forced swimming in rats: effects of agents which modify central catecholamine and serotonin activity. Eur J Pharmacol 57:201–210
Racine RJ (1972) Modification of seizure activity by electrical stimulation: II. Motor seizure. Electroencephalogr. Clin Neurophysiol 32:281–294
Raizada MK, Sumners C, Lu d (1993) Angiotensin II type 1 receptor mRNA levels in the brains of normotensive and spontaneously hypertensive rats. J Neurochem 60:1949–1952
Ramos A, Kangerski AL, Basso PF, Da Silva Santos JE, Assreuy J, Vendruscolo LF, Takahashi RN (2002) Evaluation of Lewis and SHR rat strains as a genetic model for the study of anxiety and pain. Behav Brain Res 129:113–123
Ribeiro-Oliveira A Jr, Nogueira AI, Pereira RM, Boas WW, Dos Santos RA, Simões e Silva AC (2008) The renin-angiotensin system and diabetes: an update. Vasc Health Risk Manag 4(4):787–803
Sagvolden T, Johansen EB, Aase H, Russell VA, Okamoto K, Aoki K (2006) Development of a strain pilocarpine-induced limbic seizures in rats. J Neurochem 98:1100–1113
Scorza FA, Arida RM, De Albuquerque M, Cavalheiro EA (2006) Epilepsy and hypertension. J Epilepsy Clin Neurophysiol 12:219–224
Srinivasan J, Suresh B, Ramanathan M (2003) Differential anxiolytic effect of enalapril and losartan in normotensive and renal hypertensive rats. Physiol Behav 78:585–591
Stragier B, Clinckers R, Meurs A, De Bundel D, Sarre S, Ebinger G, Michotte Y, Smolders I (2006) Involvement of the somatostatin-2 receptor in the anticonvulsant effect of angiotensin IV against pilocarpine-induced limbic seizures in rats. J Neurochem 98:1100–1113
Sun H, Wu H, Yu X, Zhang G, Zhang R, Zhan S, Wang H, Bu N, Ma X, Li Y (2015) Angiotensin II and its receptor in activated microglia enhanced neuronal loss and cognitive impairment following pilocarpine-induced status epilepticus. Mol Cell Neurosci 65:58–67. doi:10.1016/j.mcn.2015.02.014
Tchekalarova J, Georgiev V (1999) Adenosine-angiotensin II interactions in pentylenetetrazol seizure threshold in mice. J Physiol (Paris) 93:191–197
Tchekalarova J, Georgiev V (2005) Angiotensin peptides modulatory system: how is it implicated in the control of seizure susceptibility? Rev Life Sci 76:955–970
Tchekalarova J, Pechlivanova D, Itzev D, Lazarov N, Markova P, Stoynev A (2010) Diurnal rhythms of spontaneous recurrent seizures and behavioural alterations of Wistar and spontaneously hypertensive rats in kainate model of epilepsy. Epilepsy Behav 17:23–32
Tchekalarova J, Pechlivanova D, Ts Atanasova, Markova P, Lozanov V, Stoynev A (2011) Diurnal variations of depressive-like behavior of Wistar and spontaneously hypertensive rats in kainate model of temporal lobe epilepsy. Epilepsy Behav 20:277–285
Tchekalarova J, Ivanova N, Pechlivanova D, Atanasova D, Lazarov N, Kortenska L, Mitreva R, Lozanov V, Stoynev A (2014a) Antiepileptogenic and neuroprotective effect of losartan in kainate model of temporal lobe epilepsy. Pharmacol Biochem Behav 127:27–36
Tchekalarova J, Ivanova N, Pechlivanova D, Illieva K, Atanasova M (2014b) Strain-dependent effects of chronically infused losartan against kainic acid induced seizures, oxidative stress and heat shock protein 72 expression. Cell Mol Neurobol 34:133–142
Tchekalarova J, Shishmanova M, Atanasova D, Stefanova M, Alova L, Lazarov N, Georgieva K (2015) Effect of endurance training on seizure susceptibility and behavioral changes after kainate-induced status epilepticus in spontaneously hypertensive rats. Brain Res 1625:39–53
Thomas WG, Mendelsohn FA (2003) Angiotensin receptors: form and function and distribution. Int J Biochem Cell Biol 35:774–779
van Vliet EA, da Costa Araújo S, Redeker S, van Schaik R, Aronica E, Gorter JA (2007) Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain. 130:521–534
Vijayapandi P, Nagappa AN (2005) Biphasic effects of losartan potassium on immobility in mice. Yakugaku Zasshi. (The Pharm Soc Japan) 125:653–657
Wright JW, Harding JW (2011) Brain renin-angiotensin system- a new look at an old system. Prog Neurobiol 95:49–67
Wright JW, Yamamoto BJ, Harding JW (2008) Angiotensin receptor subtype mediated physiologies and behaviors: new discoveries and clinical targets. Prog Neurobiol 84:157–181
Wyss JM, Chambless BD, Kadish I, van Groen T (2000) Age-related decline in water maze learning and memory in rats: strain differences. Neurobiol Aging 21:671–681
Ye S, Zhong H, Duong VN, Campese VM (2002) Losartan reduces central and peripheral sympathetic nerve activity in a rat model of neurogenic hypertension. Hypertension 39:1101–1106
Acknowledgments
This work was supported by contract No. 30/2011 and National Science Fund (Research Grant # DTK 02/56 2009-2012). The authors thank Sabina Mitova, Medical Department, Medical University, Sofia for her expert technical assistance with the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors has any conflict of interest concerning this manuscript.
Rights and permissions
About this article
Cite this article
Tchekalarova, J.D., Ivanova, N., Atanasova, D. et al. Long-Term Treatment with Losartan Attenuates Seizure Activity and Neuronal Damage Without Affecting Behavioral Changes in a Model of Co-morbid Hypertension and Epilepsy. Cell Mol Neurobiol 36, 927–941 (2016). https://doi.org/10.1007/s10571-015-0278-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-015-0278-3