Abstract
Despite the central role culture plays in racial and ethnic disparities in mental health among ethnic minority and immigrant children and families, existing measures of engagement in mental health services have failed to integrate culturally specific factors that shape these families’ engagement with mental health services. To illustrate this gap, the authors systematically review 119 existing instruments that measure the multi-dimensional and developmental process of engagement for ethnic minority and immigrant children and families. The review is anchored in a new integrated conceptualization of engagement, the culturally infused engagement model. The review assesses culturally relevant cognitive, attitudinal, and behavioral mechanisms of engagement from the stages of problem recognition and help seeking to treatment participation that can help illuminate the gaps. Existing measures examined four central domains pertinent to the process of engagement for ethnic minority and immigrant children and families: (a) expressions of mental distress and illness, (b) causal explanations of mental distress and illness, (c) beliefs about mental distress and illness, and (d) beliefs and experiences of seeking help. The findings highlight the variety of tools that are used to measure behavioral and attitudinal dimensions of engagement, showing the limitations of their application for ethnic minority and immigrant children and families. The review proposes directions for promising research methodologies to help intervention scientists and clinicians improve engagement and service delivery and reduce disparities among ethnic minority and immigrant children and families at large, and recommends practical applications for training, program planning, and policymaking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1977, Stanley Sue raised a serious concern about racial and ethnic disparities in mental health service use and treatment outcomes. More than three decades later, the Surgeon General (2001) echoed the same concern, exposing racial and ethnic disparities as an unrelenting and unresolved challenge. Despite decades of attention to the issue, ethnic and racial minority children and families continue to be less likely to access mental health services than their mainstream counterparts (Wang et al. 2005) and are more likely to delay seeking treatment and to drop out of treatment (Addis et al. 1999; Chorpita et al. 2002; Hoagwood et al. 2010; McKay et al. 2004). Contemporary thinkers have posited that racial and ethnic disparities in mental health services may result not only from logistical barriers, but also from the ubiquitous pressures of poverty and racism (Johnson et al. 2000), stigma associated with receiving mental health care (McCabe 2002), and lack of knowledge about mental health (McKay et al. 2004). The effects are particularly concerning: While there is variation among ethnic and cultural groups, ethnic minority children and families in general face additional sociocultural stressors, such as discrimination, acculturation, cultural isolation, and poverty, that may increase their risk for developing psychopathology and reduce service use despite need (Chorpita et al. 2002; Stormshak et al. 2005). The combination of increased risk for psychopathology and less use of services produces a double burden for these families, as well as increased healthcare costs for communities and the country as a whole.
Improving engagement in mental health treatment may be the key to solve these enduring problems. Examining key mechanisms of engagement that affect ethnic minority and immigrant children and families’ perceived need and utilization of mental health care may help to improve engagement. Better understanding of cultural and contextual factors specific to mental health service use may be critical in identifying some of those mechanisms and enhancing care for ethnic minority and immigrant children and families.
Emerging scholarship points to the centrality of culture in the contextualization of mental health problems among ethnic minorities (Bernal and Domenech-Rodríguez 2012). Although the definition of culture has been constantly debated among social scientists, it is largely agreed upon that culture has both the stability to define the boundary of a group and the flexibility to be transformed along with people’s everyday actions and interactions. In line with this, in this paper, we define culture as an intergenerationally transmitted system of meanings that encompasses values, beliefs, and expectations, including traditions, customs, and practices shared by a group or groups of people (Betancourt and López 1993). Culture shapes the very meaning of health and approaches to healing at multiple levels—from the individual’s beliefs, attitudes, and practices to the broader expectations, beliefs, and practices of families, communities, and cultures. For ethnic minority and immigrant children and families, the process of engaging in mental health treatment involves the complex challenge of navigating individual, familial, and culturally derived sets of beliefs, attitudes, and practices. Lau (2006) and Barrera and Castro (2006) underscore the need to empirically examine this indwelling effect of culture on the engagement process. However, limited empirical work has addressed ethnic and cultural factors that influence the treatment engagement process (Alegría et al. 2011; Cauce et al. 2002). Thus, better understandings of cultural and contextual factors specific to mental health service use may be critical in identifying key mechanisms of treatment engagement that can enhance care for ethnic minority children and families.
Our paper addresses this existing gap by proposing a conceptual framework of engagement for ethnic minority and immigrant children and families that is derived from a review of existing measures assessing culturally specific approaches to problem recognition, help seeking, and treatment participation. It builds on, and extends, the conceptualization of culture as endogenous to the socialization and development of ethnic minority and immigrant children and families and proposes the need to incorporate culturally anchored methods in assessments and interventions involving ethnic minority and immigrant children and families (Yasui and Dishion 2007). We review the significant contributions and limitations of existing conceptual models of engagement, which have informed the development of the culturally infused engagement (CIE) model (Fig. 1). Further, the systematic review of existing measures will demonstrate the relevance of our conceptual dimensions of culturally informed engagement and measurement, as well as for training, program planning, and policymaking.
Current Conceptualization and Assessment of Engagement
Conceptual frameworks of engagement in mental health treatment describe engagement as process, occurring over stages. According to McKay and Bannon (2004), treatment engagement includes: (a) the recognition of the child/family member’s mental health issues, (b) bridging the child and his/her family to appropriate services, and (c) involvement with a mental health provider (e.g., mental health center or school-based mental health care). Interian et al. (2013) also describe engagement as a process that involves a progression of linked steps: from the encouragement of seeking treatment and client continuation in care, to treatment retention and medication adherence.
This process-based conceptualization of engagement is shared by scholars across professional fields, but the increasing awareness of racial and ethnic disparities in mental health among children has directed empirical investigations to focus particularly on engagement in mental health treatment/care participation, specifically in two domains: (a) behavioral, which encompasses the client’s “performance of tasks necessary to implement treatment and achieve outcomes” and (b) attitudinal, described as the “emotional investment in and commitment to treatment” (Staudt 2007, p. 185). Within these domains, empirical literature has assessed, for example, session attendance (Nock and Ferriter 2005), adherence (Garvey et al. 2006; Nock and Ferriter 2005), therapeutic alliance (Bordin 1994), and cognitive preparation (Becker et al. 2015).
Current measures have predominantly assessed behavioral indicators, and to a lesser degree, attitudinal aspects of engagement. For example, in their systematic review, Tetley et al. (2011) identified 40 measures assessing clients’ behavioral engagement in treatment including session attendance, completion of treatment (within identified timeframe), completion of homework, client contribution such as self-disclosure or completing session activities, working alliance with the therapist, and helpful behavior in group therapies. Similarly, Becker et al. (2015) conducted a systematic review of existing engagement interventions and found of the 40 studies examined, 25 used measures of behavioral engagement, and 13 included measures of cognitive preparation, which targeted clients’ attitudes and expectations as well as knowledge regarding treatment.
Overall, these reviews highlight the importance of assessing the behavioral and attitudinal indicators of engagement, but also point to limitations of the existing literature in the near-exclusive focus on engagement behaviors or attitudes at entry into or during receipt of treatment services, and the lack of attention to preceding engagement processes (i.e., recognition of clinical need and help seeking) that is the prerequisite for treatment utilization.
The Need for a Paradigm Shift: Bridging the Gap in Existing Conceptualization and Measurement of Engagement for Ethnic Minority and Immigrant Children and Families
While existing operationalizations of engagement provide a comprehensive understanding of individual clients’ behavioral and attitudinal participation in treatment, limitations may arise in their application in addressing poor engagement among ethnic minority and immigrant children and families. Scholars note that cultural incompatibility can significantly influence ethnic minority and immigrant children and families’ seeking of, and involvement in, mental health services, because mainstream notions of mental health and appropriate treatments may counter specific cultural values, beliefs, attitudes, and behaviors endorsed by these families (Comas-Díaz 2006; Yeh and Kwong 2009). For example, among some immigrant and refugee communities, discussion of mental health problems or mental illnesses is taboo due to cultural perspectives that mental illnesses signify being “crazy” or “mad,” thereby preventing families from seeking help despite need because of their fear of bringing shame on the family (Green et al. 2006; Hsiao et al. 2006; Scuglik et al. 2007). McCabe (2002) found that Mexican-American families tended to endorse negative attitudes toward modern medical and psychological approaches to treating mental health, which in turn impacted their retention in treatment. Sanders Thompson et al. (2004) noted that for African Americans, cultural beliefs that stressed family strength and emphasized resolving family concerns within the family clashed with views on seeking psychotherapy, influencing attitudes toward use of professional help. Further, the historical legacies of institutional racism have resulted in cultural mistrust at the system level, thereby increasing African Americans’ negative expectations of mental health services (Richardson 2001). These studies suggest that failure to understand engagement behaviors and attitudes from within the families’ cultural contexts can impede awareness of central mechanisms of engagement in mental health treatment.
Ethnic minority and immigrant children and families’ culture is likely also to influence the trajectory of engagement. Existing operationalizations that primarily focus on engagement behaviors and attitudes in treatment presume clients: (a) understand and accept the concept of “mental health” in the mainstream culture, (b) recognize their problem as a mental health problem, and (c) perceive mental health services as appropriate solutions for treatment. However, evidence suggests that even at the initial stage of problem recognition, ethnic minorities and immigrants vary in their perceptions and experiences of mental health problems, resulting in complex expressions of symptoms that conventional measures may not adequately capture. Studies report that ethnic minority and immigrant populations are likely to exhibit somatic rather than psychological symptoms (Mak 2005; Ryder et al. 2008; Tseng et al. 1990), as well as engage in culturally specific expressions of distress (Kirmayer 2001). Conceivably, these culturally derived frames for identifying symptoms and experiences of distress also shape ethnic minority and immigrant families’ expectations and preferences for treatment—i.e., families may be more likely to seek cultural remedies or healing approaches that align with their cultural interpretations of mental health distress.
Taken together, the aforementioned studies highlight the shortcomings of current conceptualizations of engagement in empirically addressing poor engagement among ethnic minority families. For ethnic minority and immigrant children and families, culture is infused in their individual and social understandings of health and well-being, thereby shaping what they might consider “problems” as well as what healing approaches they might think as acceptable, available, and preferable. These complex cultural influences intertwined at multiple levels of the immigrant, ethnic minority client’s life (i.e., from individual beliefs, attitudes, and practices to familial expectations, beliefs, and practices, and further, community norms, worldviews, and practices) dictate the process of engaging in the sequence of treatment from the initial stage of help seeking (e.g., recognizing the presence of a “problem” and finding appropriate sources) to the latter stages of treatment participation (e.g., attending consecutive treatment sessions) (Cauce et al. 2002; Gopalan et al. 2010; McKay and Bannon 2004).
These shortcomings signal the need for a paradigm shift from a more mechanistic view of engagement to a culturally infused process, by which culture shapes the ethnic minority and immigrant children and families’ trajectory of engagement via multiple levels and domains. The new paradigm can provide a wide lens that will help clinicians, program planners, and policymakers with information to improve the delivery of mental health services and treatment through innovations in community education and outreach, as well as in clinical work. We propose a model for a culturally infused process of engagement that draws from four theoretical models of health and mental health. Further, we apply this framework to systematically review and critique existing measures pertinent to ethnic minority and immigrant children and families. It is important to note that our review uses racial and ethnic categories as they are reported in existing studies. We recognize that these categories may be controversial in certain contexts, and we acknowledge that they may be culturally, contextually, and geographically defined. We refer to them solely in reporting the descriptions of previous articles.
Theoretical Models Informing Mechanisms of Engagement Among Ethnically Diverse Populations
The CIE model (Fig. 1) draws from four theoretical models from several disciplines (e.g., health study, medical anthropology, and mental health study) that address the salience of culture in the pathways to treatment engagement among ethnic minority and immigrant children and families. These include: (a) the sociocultural framework for the study of Health Service Disparities (SCF-HSD; Alegría et al. 2011) that highlights the multi-level factors of culture within the ecology of ethnic minority and immigrant children that influence engagement, (b) the mental help-seeking framework (Cauce et al. 2002) which illustrates the influence of culture on the progression of the engagement process (i.e., from problem recognition to treatment participation), and (c) the explanatory models of illness framework (Kleinman 1980) that describes the centrality of culture in the individual’s conceptualization of mental illness or mental distress, thereby shaping approaches to problem recognition and help seeking. Finally, we apply the theory of planned behavior model (TPB; Ajzen 1991) as a foundation for our framework to identify the influence of culture on the internal mechanisms of help-seeking intentions and actions that guide the engagement process of ethnic minority and immigrant children and families.
An Ecological Model of Influences on Engagement
The sociocultural framework for the study of Health Service Disparities (SCF-HSD; Alegría et al. 2011) is a theoretical framework of health disparities that conceptualizes the influences of multiple systems and their interactions in which cultural and societal factors shape the treatment process for ethnic minority clients. The SCF-HSD delineates influences across micro-, meso-, and macro-level contexts in two central domains: (a) the healthcare system and (b) the client’s community. Further, it identifies how these systems interact. Specifically, within the healthcare system, ethnic minority and immigrant clients’ pathways to appropriate clinical care are impacted from macro-level policies (e.g., federal, state, and economic), to meso-level influences of healthcare systems and provider organizations (e.g., diversity in workforce, organizational culture, climate), and finally, to micro-level clinician influences (e.g., gender, race, ethnicity, and provider training). Similarly, ethnic minority and immigrant clients themselves are impacted by influences from the macro-level environmental context (e.g., poverty, available health programs, residential segregation), meso-level community systems (e.g., social cohesion/support, community perceptions of health care), and micro-level individual influences (e.g., client beliefs, language, health literacy, acculturation). In this way, the SCF-HSD highlights that cultural and contextual influences saturate and further transform pathways to engagement for the ethnic minority and immigrant child.
Extending the Conceptual Understanding of “Engagement” as a Process
While the SCF-HSD illuminates the influences of culture at multiple system levels, Cauce et al. (2002) highlight the centrality of culture in the individual’s internal processes that develop through progressive stages of the engagement process. Cauce et al. (2002)’s mental help-seeking framework builds on the existing conceptual models that identify engagement as a process (e.g., Interian et al. 2013; McKay and Bannon 2004) by identifying the central cultural and contextual influences within a client’s ecology that guides the pathways to seeking help for mental health. Within each phase, culture and context have distinctive roles in shaping client’s motivation, commitment, and activation to engage in stages of seeking mental health treatment—from how problems are conceptualized, to whether help is sought, to what sources of help were targeted. For example, the authors describe that even at the first phase of problem recognition clients undergo a process of balancing an individual’s view of a “problem” with familial and larger cultural definitions of what constitutes a mental health problem. Thus, by addressing engagement processes prior to service utilization, Cauce’s model highlights the trajectory of engagement through illustrating the individual’s internal processes that are shaped by culture.
Models of Illness as a Framework for Internal Engagement Processes
Whereas the above models identify the external influence of culture on individual engagement, culturally anchored explanatory models of illness illustrate the cardinal effect of culture within the individual via beliefs and experiences of mental health. Defined as “the notions about an episode of sickness and its treatment that are employed by all those engaged in the clinical process” (Kleinman 1980, p. 12), explanatory models are central frameworks that provide an understanding of both perceived causes of illnesses and appropriate healing methods. Since cultures vary in their explanatory models of illness, the clinical reality of clients is culturally constructed, suggesting that cultural context plays a fundamental role in shaping internal mechanisms of how individuals explain their distress, make meaning of experiences, and cope with or seek treatment for their illness.
Evidence suggests that there are cultural variations in the expression and conceptualization of mental health symptoms and problems. Ethnic minorities and immigrants are more likely to interpret and express distress in ways that are consonant with their culture (e.g., somatic symptoms, idioms of distress) (Fung and Wong 2007; Yeh et al. 2004). Moreover, these expressions of mental health distress are linked to culturally specific explanations that give meaning to the illness experience and guide approaches to healing. In this way, cultural explanatory models of illness shape the process of engagement through individuals’ (a) beliefs about their mental health distress, (b) beliefs about healing and treatment, and (c) cultural norms regarding mental health distress and appropriate treatments.
Understanding the explanatory models of mental health for ethnic minority and immigrant children and families may be critical in the context of mental health care in the USA. The explanatory model’s culturally driven approach to conceptualizing mental distress or illness distinctly contrasts with the biomedical framework that postulates a disease-oriented approach to the identification (i.e., diagnosis) and treatment of mental disorders. The increasing biomedical emphasis on precise identification of mental health dysfunction and the specialization of treatments designed to target specific dysfunctions directly have resulted in important contributions to clinical practice. But for ethnic minority and immigrant children, cultural considerations are paramount to enhance engagement, tailoring treatment and service delivery approaches to be congruent with their lived illness experiences and those of their families.
Theory of Planned Behavior—Internal Processes of Engagement
The theory of planned behavior model (TPB) (Ajzen 1991) has been applied widely to predict engagement in health behaviors (Armitage and Conner 2001) and services (Dumas et al. 2007), suggesting its relevance as a model for examining individuals’ engagement in mental health services. According to the TPB, behaviors are largely determined by the individual’s intention to perform a behavior, where intentions are a function of three domains: (a) the individual’s attitude toward the behavior, (b) the subjective norms associated with the performance of the behavior, and (c) the individual’s perception of efficacy in performing the behavior (Ajzen 1991). Thus, the TPB’s focus on the interplay of cognitive and behavioral processes in individuals’ decisions regarding their behaviors can be instrumental in identifying culturally informed individual-level attitudes, beliefs, and practices about engagement shaped by network-driven explanatory models of illness.
Proposed Model of Engagement—Cultural/Contextual Process of Engagement
Integrating and synthesizing the above models, we propose the culturally infused engagement (CIE) model (Fig. 1) that can facilitate the identification of gaps in the understanding of the engagement processes for ethnic minority and immigrant children and families. As a more comprehensive model of the help-seeking process, it is the foundation of our literature review, as its application can also provide insight into unexplored areas of the help-seeking process for ethnic minorities and immigrants that contribute to disparities in treatment and service delivery.
Figure 1 shows how the ecological context of the ethnic minority and/or immigrant child is saturated with cultural and contextual influences from multiple systemic levels. It underscores that children are primarily dependent on their parents or adult family members to seek, obtain, and participate in mental health services. Thus, family members’ explanatory models of mental health and illness are likely to be critical determinants in shaping the trajectory of treatment engagement for the ethnic minority and immigrant child. At the meso-level, the values, beliefs, and practices of the ethnic community, church, school, and neighborhood may serve as the foundation for the specific explanatory models adopted by ethnic minority and immigrant children and their families. Lastly, macro-level influences such as discrimination or the US mainstream culture (e.g., media exposure on mental health) directly or indirectly influence ethnic minority and immigrant children’s understanding of mental distress and illness, and hence, treatment engagement. These complex multi-level influences are manifested at the individual level, as the explanatory model of illness.
The explanatory model serves as a map of interwoven beliefs, intentions, and behavioral and emotional responses that uncovers how an individual understands his or her lived experience of illness. This involves examining (a) the individual’s conceptualization of the distress, which involves understanding the illness cause, course, identity, and illness experience, and (b) his or her response to the mental illness/distress (i.e., healing approaches). The conceptualization of mental distress, which points to the stage of problem recognition, could be manifested either through causal beliefs (e.g., psychological, biological, supernatural) derived from the expressions or the identity of the illness (e.g., idioms of distress), or through the way in which the client conceives the personal meaning of the illness experience. That conception can be shaped (a) by behavioral beliefs about mental distress (i.e., its expected outcomes) and (b) by agency beliefs (i.e., perceived control over the illness or distress) that encompass the effect of external barriers (e.g., lack of insurance, transportation issues, lack of childcare) on the lived illness experience. At the same time, perceived norms (the perceived meanings of the illness or distress for others) can also play a role in determining the meaning of the individual’s lived experience of illness within broader sociocultural contexts. Together, beliefs and perceived norms form the conceptualization that influences the seeking of relevant methods of healing, and, subsequently, an individual’s response to the illness experience in both help seeking and treatment participation.
Using the framework of the culturally infused process of engagement, we empirically examined the multi-dimensional and progressive process of engagement by conducting a systematic review of existing assessments that inform culturally specific approaches to problem recognition, help seeking, and treatment participation among ethnic minority and immigrant children and families. While the primary focus of our framework is ethnic minority and immigrant children and families in the US context, we also draw from cross-cultural literature to inform our understanding based on the following reasons: (a) In certain domains, evidence with culturally diverse populations is limited and (b) the studies are conducted in cultures of origin of immigrant populations in the USA.
Methods
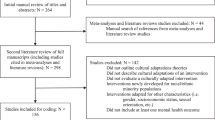
We conducted a computerized literature search of the PsycINFO, ERIC, IngentaConnect, Google Scholar, and JSTOR databases using a keyword approach to identify relevant empirical measures in domains of problem recognition, help seeking, and engagement in services between 1960 and 2015. The following keywords were used individually and in combination to guide the literature search by each domain: for problem recognition, “idioms of distress,” “culturally bound syndromes,” “child psychological problems,” “mental health symptoms,” “explanatory models of illness,” “mental health beliefs,” and “causal beliefs about mental illness/mental health problems”; for help seeking, “help seeking,” “mental health,” “explanatory models of illness,” “stigma,” “mental health beliefs,” “healing approaches,” and “treatment”; and for engagement in services, “mental health,” “explanatory models of illness,” “treatment,” “psychotherapy,” “treatment engagement,” “treatment participation,” and “mental health service use.” Across all of these, the keywords “culture,” “ethnic minority,” “immigrant,” “measures,” “scale,” and “inventory” were combined to identify existing measures within these domains. In addition to the electronic searches, we conducted manual searches for existing measures that included examining the reference lists for each paper. Measures were included in the review if they met the following criteria: (a) The instrument was designed to measure the domains according to the CIE, (b) the paper was published in a peer-reviewed journal or was a published or unpublished assessment manual, (c) the paper reported psychometric properties of the measure, (d) the paper reported measures that provided the original items or authors shared the unpublished measure, and (e) children, youth, and families, and (f) ethnic minorities, immigrants, or the measures were used with cross-cultural samples. Four semi-structured interview assessments that captured open-ended responses were also included based on the culturally anchored probes utilized to elicit client-defined beliefs about mental distress and healing approaches. Measures were excluded if they assessed beliefs and behaviors regarding one specific treatment modality or approach or if they assessed provider-centered beliefs. In addition, because an item-level analysis of existing measures was performed, instruments for which we were unable to locate the original measure were excluded.
Two systematic reviews of measures on help seeking and treatment (Gulliver et al. 2010) and treatment participation (Tetley et al. 2011) are in the extant literature. Those reviews examine engagement as a universal construct, rather than as a culturally defined process. While some overlap in the identification of measures between our review and theirs is inevitable, we focus on a different aim: whether the measures assess culturally specific mechanisms of engagement.
Based on the above criteria, 119 measures published between 1963 and 2015 were included in this review.
Coding of the Measures
All existing measures were coded independently by a team of 6 coders that categorized the measures at the item level according to the domains defined by the culturally infused engagement (CIE) model. Coders were trained (a) on the theoretical frameworks of the SCF-HSD (Alegría et al. 2011), the help-seeking model (Cauce et al. 2002), explanatory models of illness (Kleinman 1987), and the theory of planned behavior model (Ajzen 1991), (b) on differentiating items according to the domains of the TPB (Ajzen 1991), and (c) on categorizing items based on the domains identified that corresponded to the CIE. All coders were trained by the first author.
Domains were operationalized using the definitions from the aforementioned theoretical frameworks. Coders categorized items from measures according to whether they assessed the following dimensions of the CIE: (a) causal beliefs, (b) symptom presentation or expression, (c) beliefs about the mental distress (conceptualization and illness experience of the distress), (d) beliefs about seeking help, and (e) behaviors of help seeking. Within the category of beliefs about the mental distress, items were further categorized into: (i) beliefs about the illness identity, (ii) beliefs about characteristics/internal traits of individuals with the illness, (iii) the individual’s beliefs about the illness experience (i.e., attitudes and expected responses, and agency/control beliefs), and (iv) perceived norms regarding the internal and external illness experience. Beliefs about seeking help included: (v) expectations and efficacy beliefs about seeking help (professional and alternate), (vi) perceived norms associated with seeking help, (vii) agency/control beliefs and the willingness/intent to seek help (professional vs. other), and (viii) relational beliefs regarding seeking help.
Each item was examined for its relevance in assessing the CIE domains. For domains that reflected the TPB model (e.g., behavioral beliefs, agency/control beliefs, social norms, intentions), we followed the descriptions of TPB items by Fishbein and Ajzen (2010). For other domains that were uniquely identified in the CIE (e.g., causal beliefs, expressions, illness identity, beliefs about internal traits/characteristics), definitions for each domain were derived using the existing literature. For example, illness identity beliefs were defined as beliefs about the illness or distress itself and not the individual with the illness (e.g., “depression is not a real medical illness,” “I do not believe that psychological disorder is ever completely cured”), whereas beliefs about the characteristics/internal traits of the individual with the illness included items that described perceived qualities of the individual that shaped the self-illness experience (e.g., “A problem like X’s is a sign of personal weakness,” “mentally ill people tend to be violent”). Causal beliefs were defined as applying to the mental health problem itself and a range of attributed causes (e.g., “the illness is caused by a brain disease”). The expressions of illness encompassed symptoms (physical, psychological, emotional, behavioral, relational), as well as cultural idioms of distress (e.g., “Did your ears suddenly become blocked and as a result you experienced buzzing sounds in your ears?”, “I experience brain burning, crawling heat or cold or other unpleasant sensations in my head, while studying”).
Coders received training until they reached reliability in categorizing items. Discrepancy among coders on item categorization was reviewed by all coders and discussed in weekly consensus meetings. Generally, disagreements among coders were resolved by refamiliarizing them with the definitions of each domain and discussing the correspondence of specific items to their respective domains. Inter-rater reliability was assessed using Cohen’s (1960) kappa because it adjusted for raters’ agreement that can occur due to chance. The kappa coefficient obtained for this study was 0.92 which suggests an excellent level of agreement on the codes across raters (Landis and Koch 1977).
Findings
Table 1 contains 119 existing measures categorized based on the proposed domains in our conceptual model: (a) expressions of distress (idioms of distress and symptom expression across culture), (b) causal beliefs (explanations of mental distress and illness), (c) beliefs about mental distress and illness (illness identity and meaning of the illness), (d) beliefs and experiences of seeking help (beliefs about healing approaches and help-seeking behaviors). Twenty-six percent (31 measures) were identified as reflective of symptoms and expressions of mental distress, 30% (36 measures) identified causal beliefs, 50% (60 measures) assessed self and others’/public beliefs about mental health problems, and 51% (61 measures) assessed beliefs about mental health services. Further, 78% of the measures (93 of the 119) have been utilized with ethnic minority, immigrant, or cross-cultural samples; 55% of the measures (66) have been assessed with children, youth, or families; and 35% (42) have been used with ethnic minority, immigrant, or cross-cultural samples and with children, youth, or families (Table 1). These findings highlight the relative under-exploration of symptoms and expressions of distress and causal beliefs that precede problem recognition and help seeking. This phase in the help-seeking process may have the most importance for ethnic minority and immigrant children and families because it defines how the client understands the problem, setting the course for culturally responsive service use. An item-level analysis of these measures that we describe in our review reveals multiple and important contributions to measurement that is culturally sensitive. The analysis also shows significant gaps in measurement to understand the help-seeking processes for ethnic minority and immigrant populations. The review of the four domains and the item-level analysis supports the wisdom of a culturally infused perspective on the help-seeking process prior to the clinical encounter. Effective community outreach and treatment interventions are predicated on this culturally infused understanding. Below, we discuss our review of existing measures according to each of these domains, respectively.
Expressions of Distress: Idioms of Distress and Symptom Expression Across Cultures
The biomedical/biopsychosocial framework is the underlying basis for the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) which classifies mental distress as psychological, behavioral, and biophysical dysfunctions or abnormalities (American Psychiatric Association 2013). The central notion of dysfunction is foundational to the DSM’s approach to the identification of psychopathology by which symptoms are perceived as objective, measurable indicators of abnormalities (i.e., a disease) in an individual’s biological and psychological makeup and function that determine diagnoses (Thakker and Ward 1998). Further, this approach to problem identification has guided the development of mental health treatments that centralize on the reduction of symptoms, leading to the advancement of evidence-based treatments (Yasui and Dishion 2007).
Despite the significant utility of the biopsychosocial/biomedical model’s scientific, objective approach to addressing mental health problems by the identification of areas of dysfunction, studies have found that cultures differ in their notions of distress (Kirmayer 2001; Ryder et al. 2008). Rather than perceiving symptoms as indicators of dysfunction, some cultures apply a holistic interpretation that encapsulates not only the specific expressions of dysfunction but also the multifaceted reactions of the individual and their relationships and culture to the distress. This constellation of changes in state and function along with the subjective and experiential aspects of the distress is described in medical anthropology as the illness experience (Kleinman 1980). Culture shapes the illness experience through the various beliefs, values, practices, and norms, giving rise to significant variations in how illness is characterized, how individuals make meaning of the illness such as its cause and course, and appropriate ways of healing or treating the illness (Harwood 1981). In this way, culture determines the conceptualization and recognition of symptoms, as well as the idioms and expressions used to communicate the experience of the distress or illness.
Table 1 shows our review of existing measures and indicates that 99 of the 119 measures (83%) did not include items that targeted problem recognition, but rather, defined the “illness” either by the use of mental health terminology or vignettes that portrayed specific symptoms or DSM disorders. Of these, the majority used mental health terminology that included general mental health terms (e.g., mental illness, mental disorder, mental health problem, psychological problem, emotional/behavioral problem), or descriptions of receiving mental health care (e.g., psychiatric patient, mental patient, seeing therapist, psychosocial treatment) as definitions of mental distress in their questionnaires/interviews. This wide application of a generalized mental health terminology and the defining of illness expressions by DSM diagnostic criteria among existing measures reflect the implicit assumptions of the current mental health field that conceptualizations of mental health disorders/problems hold equivalent meanings and are commonly shared by the public.
Of the total 119 measures, 31 (26%) assess the culturally infused engagement (CIE) model’s dimension of illness expressions (Fig. 1). Overall, measures assessing symptoms or expressions of mental distress captured expressions across a variety of domains including somatic symptoms, psychological (emotional, cognitive, behavioral) symptoms, culturally specific somatic symptoms, culturally specific emotional and psychological distresses, and spiritual/supernaturally related symptom expressions. Among the 31 measures (Table 2), 19% (6) of measures included items that inquired about general mental health symptoms (i.e., without specification of disorder type), 39% (12) assessed symptoms specified to DSM disorders and symptoms (e.g., depression, schizophrenia, suicide, etc.) of which 26% (8) were culturally adapted. Additionally, based on our scope to identify culturally specific symptoms, 61% of the measures (19) were identified that assessed culturally specific symptom expressions of distress or culturally bound syndromes. The diverse constellations of culturally specific symptoms across somatic, behavioral, psychological, and spiritual domains of these measures highlight their distinctiveness from the conventional symptom structures of the DSM.
Review of the measures revealed that 58% (18) of the 31 measures endorsed somatic symptoms, suggesting the salience of physical or bodily symptoms as indicators of distress. This propensity for physical and physiological symptoms as major indicators for recognizing mental distress has been documented across ethnic groups—studies among Asian, Latino, and African Americans indicate that somatic expression of psychological symptoms is much more prevalent compared to European-Americans (Choi 2002; Mak 2005; Myers et al. 2002; Ryder et al. 2008; Tseng et al. 1990). Moreover, 45% of the measures (14) included somatic symptoms that were culturally specific [e.g., sputum moving upward and causing sensations of a heart arrest or inability to breathe (e.g., the Cambodian Somatic Symptom and Syndrome Inventory), noises in ears (i.e., symptoms of Ode-Ori)], suggesting the important role of culture in the shaping the recognition/identification of distress and meanings attached to these bodily sensations. In particular, among cultures that view health holistically, interpretations of distress are viewed as stemming from the body, spirit, mind, and human relationships, resulting in expressions that link emotional and behavioral states to physical sensations (e.g., anger in the liver). Furthermore, historical influences may also shape the identification of culturally specific somatic symptoms; for example, Hinton et al. (2013) describe that somatic symptoms such as neck soreness among Cambodians are associated with the traumatic experiences of the genocide by which individuals engaged in slave labor were forced to carry heavy loads of dirt on a pole that was balanced at the neck. Thus, although there are some universal somatic representations of distress, the identification of these symptoms appears to be primarily culturally derived.
In addition to somatic symptoms, 84% (26) of measures also included psychosocial (emotional, behavioral, cognitive, and interpersonal/relational) symptoms. Thus, while ethnic minorities and immigrants may primarily endorse somatic symptoms, examining co-occurring psychological symptoms is also important. Symptoms described indicated a range of culturally specific symptoms to symptoms identified in conventional DSM disorders (e.g., little interest in doing things, trouble concentrating). Culturally specific psychological symptoms ranged from cultural phenomena such as haan, which is described as “the collapsed pain of the heart due to psychosomatic, interpersonal, social, political, economic, and cultural oppression and repression” (Park 1993, p. 16), to context-specific symptoms (e.g., “When I read I feel that the words don’t make sense”, an item of the Brain Fag Scale; Prince 1962).
Lastly, 13% of the measures (4) assessed spiritual/supernatural indicators of distress. For example, the Cambodian Somatic Symptoms and Syndrome Inventory (CSSI; Hinton et al. 2013) includes items that symbolize spiritual associations to the body (e.g., “ghost pushing you down” for sleep paralysis, lightness in the body as if your soul was not in your body). This link between spiritual or supernatural factors and symptoms/idioms of distress demonstrates the intricate connection between culturally anchored causal beliefs and the sociocultural meanings of distress and their expressions (Kleinman 1978).
In sum, our review of measures on culturally unique symptom expressions and idioms covers a wide range of indicators of distress—from somatic symptoms, to emotional or psychological problems, to spiritual or supernatural expressions—that are represented by several different ethnic minority and immigrant groups, showing the significant diversity among those groups in their conceptualization and recognition of mental illness. According to the CIE (Fig. 1), this diversity in illness expressions might fundamentally shape ethnic minority and immigrant children and families’ beliefs about, attitudes toward, and reactions to the mainstream mental health diagnoses and services which are largely based on the DSM framework, thereby affecting their engagement in treatment. However, our review also highlights a critical gap in the literature, reflected in the paucity of existing measures that capture these cultural variations. Limitations of this kind can have significant implications in clinical practice—including the misdiagnosis or underdiagnosis of mental health symptoms and disorders among ethnic minority and immigrant children and families. In fact, evidence suggests that the lack of attention to culturally specific indicators of distress has resulted in repeated underdiagnosis and misdiagnosis of psychological disorders among some minority youth and adults (Choi 2002). Thus, while conventional measures of psychological distress and dysfunction continue to be important, our review points to the need for measures that simultaneously address culturally determined presentations of psychological distress. The consideration of these cultural nuances at the symptom expression stage would position the role of culture at the foreground for understanding how ethnic minority children and families formulate their conceptions of “problems” as well as identifying their thresholds of need for help seeking, which might be an effective means to address ethnic and racial disparities in mental health service engagement.
Causal Beliefs: Explanations of Mental Distress and Illness
The culturally infused engagement (CIE) model identifies causal explanations of mental illness or distress as the crux of the conceptualization of mental health distress and response to healing (Fig. 1). Differences in causal beliefs between mental healthcare professionals and ethnic minority and immigrant children and families therefore may have significant implications in the clinical context. As we have described, mental health care in the USA has predominately operated from a biomedical framework that prioritizes the identification of the cause of the “disease” (i.e., mental disorder) in the biological, psychological, and behavioral domains. While the integration of the biopsychosocial model has broadened the scope in locating causal factors of mental distress and illness across domains, the primary focus on identifying specific causal mechanisms to target intervention may often be at odds with ethnic minority and immigrant clients’ understanding of their illness experience. For ethnic minority and immigrant children and families, causal beliefs stem from their cultures’ conceptualizations of mental health that are often holistic, without definitive boundaries between cultural, spiritual, physical, and psychosocial domains (Betancourt 2004; Bolton et al. 2004; Carrillo et al. 1999). Our review of individuals’ causal beliefs about mental health distress/mental illness across the existing measures highlighted the dichotomy between the biomedical framework (i.e., biology/genetics, psychological, or social/environmental causes) and cultural explanatory models of illness (i.e., supernatural/spiritual and culturally specific causes). We organize relevant measures in Table 3 and describe each of the causal domains identified in our review below.
Biological/Genetic/Physical Causes
Of the 36 measures assessing causal beliefs, 24 (67%) identified biological, genetic, or physical causes, highlighting the dominant view that mental health problems/illnesses are biological, medical illnesses in nature (Table 3). Biomedical causes assessed included genetic/heredity, to brain mechanisms (e.g., disorder of brain, neurochemical imbalance), prenatal influences, physical illness or injuries, and physical reactions (e.g., allergies, sensitivity to foods/drugs/alcohol). The attribution of biological/genetic/physical causes of mental health problems was evident across measures assessing: (a) clinically diagnostic as well as cultural conceptualizations of mental health distress/mental illness, and (b) diverse ethnic and racial populations, which suggests a prevalent view of biomedical explanations of mental health problems. Such may reflect the increasing spread of biomedical knowledge of causes of mental health problems/mental illness not only in mental health disciplines but further, to the general public (Insel 2009).
Seventeen percent (6) of the 36 measures also captured physical causes embedded in culturally based explanatory models of illness. These measures included culturally based physiological causes that were generally identified as an imbalance or disruption of harmony in the body (e.g., energy imbalance, humoral imbalance, yin/yang, cold/hot, energy, or vitality flow). Traditional Chinese medicine (TCM) and Indian Ayurveda medicine are two examples of still commonly believed and practiced medical systems holding such holistic views of life and health. In TCM’s epistemology, for example, mind and body are considered inseparable, and balance of energies needs to be maintained to achieve a “healthy” state of life (Kuriyama 2002). Studies suggest that among Asian Americans, TCM is frequently used either as an alternative to or in combination with Western medical treatment approaches (Feng et al. 2006), which may reflect their strong reference to traditional causal beliefs when contemplating biological or organic causes of mental health problems (Matthews 2012).
Psychological Causes
Psychological causes of mental health problems included dimensions of cognitive, behavioral, emotional, personality/character, and trauma history/past experiences. Reflective of the centrality of the biomedical/BPS framework, 86% (31 of 36) of the measures assessed one or more dimensions of psychological causes (Table 3).
Cognitive, Emotional, Behavioral, and Personality Causes
Eighty-one percent (29) of the 36 measures assessed cognitive, emotional, behavioral, and personality causes—consisting of the following types: (a) lay perceptions of symptoms/descriptors associated with specific clinical disorders (e.g., for schizophrenia: thinking too much, for ADHD: not trying hard enough), (b) therapeutic descriptions of psychological processes related to mental distress (e.g., not having a realistic view of the good and the bad things that have happened), (c) engagement in dysfunctional behaviors or habits (e.g., substance or alcohol use or misuse), and (d) traits or qualities related to a person’s nature (e.g., bad character). Further, the psychological causes reflect two prevailing perspectives related to mental health problems/mental illness—the ascription of responsibility to the individual for his or her mental illness (e.g., not trying hard enough to control behavior) and the perceived changeability of the mental illness. Across types, the ascription of responsibility for one’s mental health problem/illness is evident, although variation exists in the degree to which the responsibility is inferred, and further, intersects with perceptions of changeability. For example, while internal causal mechanisms are implied in both the cause “having learned the wrong reactions to certain situations” and “bad character,” the latter suggests a broader internal cause that has more permanency or rootedness, and thus is more difficult to change. Thus, perceptions of the controllability, intentionality, and stability of an individual’s negative behaviors are likely to play a central role in whether others respond negatively or positively (Weiner et al. 1988). Studies examining parental attributions of child behaviors suggest that parental beliefs about causes of mental health problems influence attributions of child responsibility for negative behaviors (Gerdes and Hoza 2006; Johnston and Freeman 1997; Johnston et al. 2005; Pottick and Davis 2001). Further, culture may influence the ways in which parental causes are attributed to mental health problems among children (Mah and Johnston 2007).
Psychological Trauma Causes
Among 36% (13 of 36) of the measures included in our review, psychological trauma was identified as the cause of mental health problems/mental illness. Measures assessed causes of interpersonal trauma (e.g., physical abuse, sexual abuse, witnessing violence), as well as traumatic events or situations experienced by the family or the community (e.g., poverty, hardships, natural disaster, war, genocide).
The inclusion of psychological trauma in measures is indicative of the BPS model of mental health, which conceptualizes the interaction of traumatic events with the psychological and physical functioning of the individual. Within the field of mental health, recognition for the significance of trauma in shaping mental health problems/mental illness became widespread with the identification of post-traumatic stress disorder (PTSD) as a formal diagnosis (Schnurr and Green 2004) and resulted in a large body of literature supporting the link between trauma and poor psychological functioning (Hutchinson and Dorsett 2012; Mollica et al. 1993; Steel et al. 2002). This increased awareness of the causal effects of trauma has resulted in numerous benefits such as the development of evidence-based programs addressing trauma (Westoby and Ingamells 2010).
Despite these advances, the notion of trauma is not always shared across various cultures. Some scholars have noted that the labeling of certain past experiences or events as “trauma” inadvertently promotes the biomedical conceptualization of a deficit or pathology framework of mental health (Marlowe 2009; Raymond 2005), thereby overlooking cultural explanations and ways of healing from the event(s). For example, in his study on Sudanese refugees, Marlowe (2009) highlights participants’ discomfort with others’ assumptions that trauma is a central characteristic of their identity and group identity, and argues for the understanding of the event within the lens of the ordinary lives of the individuals that are anchored within their cultural context. Such underscores the importance of assessments that capture the individual’s culturally determined experiences, expressions, and meanings of the distress that conventional measures are limited in assessing (Eisenbruch 1991).
Social/Interrelational Causes
Fifty percent (18) of the 36 measures captured social/interrelational causes highlighting a dominant belief in interpersonal contextual causes of the development of mental health problems/mental illness (Table 3).
Social/relational causes included familial (15 measures) (e.g., parental, marital, extended family relations), and non-familial (general) relational causes (10 measures) (e.g., peer relations and relations with others). Among familial causes, parental causes of mental health problems/mental illness were the majority and included negative parenting (e.g., negative discipline, poor parental involvement, and poor parent–child relationships), familial relationship problems (e.g., marital discord, conflict with relatives), and parental distress (e.g., parental mental health). Negative parenting was the most frequently assessed relational cause across measures, which likely reflects a commonly held belief that attributes responsibility to parents for a child’s mental health outcome. Particularly in the case of child mental health, evidence indicates that across ethnic groups perceptions of parental responsibility are frequent (Malacrida 2001; Singh 2004), both among parents themselves and also by others. Studies suggest that parents often blame themselves and attribute the causes of their child’s mental health problems to themselves, despite acknowledging other causes such as biological, genetic, or environmental causes (Moses 2010). The attribution of parental responsibility for child mental health problems appears to be shared widely—not only by the general public (Corrigan and Miller 2004; Struening et al. 2001; Weiner et al. 1988) but by teachers (Edwardraj et al. 2010) and mental health professionals (Johnson et al. 2000, 2003). Moreover, recent studies have reported ethnic differences in attributions of parental responsibility to child mental health problems (Young and Rabiner 2015), highlighting the importance of examining variations in these beliefs across cultures.
Three measures assessed familial relationship causes that ranged from illness or death of a family member to family conflict, reflecting the belief that the family context significantly affects the healthy functioning of individual family members. Studies indicate that family members (i.e., parents, spouses, siblings) often report concerns of being blamed or held responsible for causing family members’ mental health problems as well as the management of the illness (Greenberg et al. 1997; Phelan et al. 1998). Moses’ (2010) study on parental beliefs regarding their youth’s mental illness describes the parents’ sense of responsibility for their child’s exposure to a negative family contexts such as instability or violence. For ethnic minority and immigrant children and families from collectivistic cultures, the attribution to familial causes may be even more acute as individuals’ identities are viewed as embedded within central relationships (i.e., familial) rather than independent, autonomous entities (Markus and Kitayama 1991).
Non-familial social/relational causes included general relationship with others, peer relations, and relationships at work. Twenty-eight percent (10 of 36) of the measures assessed non-familial causes which may reflect the lower significance of such relationships compared to parental and familial relationships in their impact on the mental health of individuals.
Contextual (Environmental/Societal/Cultural) Causes
Several measures cited environmental causes of mental health problems/mental illness. Forty-seven percent (17) of the 36 measures assessed specific contextual causes such as exposure to environmental substances (e.g., contamination, atomic rays, lead), cultural factors (e.g., assimilation to American culture), societal influences (e.g., media), and socioeconomic factors (e.g., financial difficulties, family poverty) as well as a broader category of stress which was most frequently cited (Table 3).
Six measures assessed socioeconomic causes that consisted of: (a) income-related specific causes (e.g., financial difficulties, family financial crises), (b) work-related causes (e.g., unemployment), and (c) social position-related causes (e.g., single parent, lives in inner city). The causal belief in the negative impact of socioeconomic stressors on mental health is reflective of evidence establishing the causal link (Conger et al. 2002; McLoyd 1998) as well as a widespread public perception that associates mental health problems with the poor (Lind 2004; Orloff 2002) and ethnic minorities (Gilens 1999; Neubeck and Cazenave 2001).
Only a handful of measures assessed other societal causes, including such things as the influence of media, and the hectic pace of modern life. Moreover, it is alarming that only one measure (Yeh and Hough 1997) specifically assessed cultural factors as causes of mental distress. The paucity in the range of contextual causes for mental health problems signifies a need for assessments also to consider factors that may be particularly salient for ethnic minority and immigrant children and families. For example, significant literature has demonstrated the negative effects of racism or discrimination on mental health outcomes among African American, Latino, Asian American, and Native American youth and adults (Rosenbloom and Way 2004; Whitbeck et al. 2002; Wong et al. 2003). Studies indicate that the negative effects of discrimination on youth developmental outcomes include increased delinquency and problem behaviors such as shoplifting, skipping class, lying to parents, cheating, stealing cars, and bringing drugs or alcohol to school (Okamoto et al. 2009; Prelow et al. 2004; Wong et al. 2003) as well as internalizing problems such as depressive symptoms (Seaton et al. 2008) and anxiety (Gaylord-Harden and Cunningham 2009; Hwang and Goto 2008). Similarly, studies on Latino and Asian American immigrant youth suggest that acculturative stress is a significant predictor of poor mental health—including internalizing problems (e.g., withdrawal, anxiety, somatic and depressive symptoms), and externalizing behavior problems (i.e., delinquency, aggressive behaviors) (Dinh et al. 2008; Gil et al. 2000; Hovey and Magaña 2002; Vega and Gil 1998). Considering the supporting evidence, including salient contextual factors that are predictive of poor outcomes among ethnic minority and immigrant children and families will be a critical direction for future measures.
Spiritual/Supernatural Causes
The explanatory models of health among ethnic minority and immigrant children and families often include holistic conceptualizations, of which supernatural/spiritual factors are an integral component (Betancourt 2004; Carrillo et al. 1999). Of the 36 measures examined, 44% (16) identified supernatural/spiritual causal beliefs about mental illness/mental health problems, suggesting the importance of this dimension (Table 3). The supernatural causes assessed clustered under spiritual or religious (e.g., work of the devil, will of God), magical (e.g., curses, witchcraft), karmic (e.g., previous deeds of ancestors or in former life), and cosmic (e.g., born on specific days) dimensions.
The centrality of the supernatural in health and mental health is highlighted in the proposed frameworks of medical anthropologists that encompass supernatural causes of illness (e.g., Eisenbruch 1990; Murdock et al. 1980; Young 1976). Evidence supports the saliency of supernatural causal beliefs among ethnic minority and immigrant populations (Cohen et al. 2009; Tarakeshwar et al. 2003). Studies suggest that individuals and cultures where spirituality and religion play a significant role are more likely to attribute symptoms or expressions of distress to supernatural, religious, or spiritual causes, and further, seek help from religious, spiritual, and alternate sources (Abe-Kim et al. 2004; Hartog and Gow 2005; Mathews 2008; Wilcox et al. 2007). The causal attribution to supernatural factors has also been found to explain child mental illness cross-culturally. For example, autism in children has been attributed to wicked ghosts (Hwang and Charnley 2010), child psychiatric disorders have been linked to the evil eye or a curse (Guzder et al. 2013), and ADHD is seen as coming by God’s hand or the influence of stars and planets (Wilcox et al. 2007). These findings highlight the importance of addressing supernatural beliefs in mental healthcare practice, as misconstruing culturally unique conceptualizations of mental distress and illness will likely overlook ethnic minority and immigrant children and families’ existing help-seeking beliefs, resources, and behaviors, as well as deter their engagement in professional mental health services. While the ways in which supernatural causal beliefs can be addressed in clinical practice are multifaceted and dependent on the unique explanatory model of the client, gaining an understanding and knowledge of them and how they shape clients’ own understanding and meaning of their illness is essential in identifying appropriate avenues for intervention. For example, a clinician who learns that a client attributes an imbalance in the energy within her body as the cause of her mental distress may approach the discussion of psychiatric medication with an individualized caution and sensitivity, examining alternate treatment options that match the client’s culturally anchored explanatory model of illness.
Overall, our review of existing measures illustrates the diverse range of causal beliefs associated with mental distress and illness. As expected, the majority of measures assessed causal factors that represented a biomedical or biopsychosocial perspective of mental illness or distress, which suggests the predominance of these frameworks in contemporary mental health care. There are also several measures capturing causal beliefs that illustrated culturally anchored explanatory models of illness such as supernatural forces, the cultural context, and natural factors (e.g., yin yang). These measures are examples of the increased number of studies recognizing the relevance of cultural alternatives in causal beliefs for ethnic minority and immigrant populations, which is also reflected in the recent changes to the DSM through the inclusion of the cultural formulation interview (CFI). The integration of the CFI, which incorporates the explanatory model of illness framework, highlights a promising potential in broadening the current paradigms of mental health assessment and diagnosis, by taking cultural diversity and alternative epistemologies of health into serious consideration when evaluating immigrants’ and ethnic minorities’ causal beliefs about their illness experiences. However, these changes have still positioned culturally specific factors as supplements/alternatives to the mainstream biopsychosocial model.
It is worth noticing, based on the culturally infused process of engagement model, that culture should be understood as cross-system influences which shape individuals’ explanatory model of illness through the dynamics between different systemic mechanisms—from macro-level acculturation experiences, meso-level community norms and beliefs, to familial-level expectations and practices (see Fig. 1). Therefore, the mainstream biomedical/biopsychosocial perspective in mental health could also be integrated into this overarching framework as one aspect affecting ethnic minority and immigrant families’ causal beliefs about mental illness in their current living contexts. For example, immigrant parents might shift their causal beliefs about mental illness after being exposed to this mainstream perspective through media or their children’s education for a period of time. In this way, we might approach these different sources of causal beliefs not as oppositional, but as interactive in ethnic minority and immigrant families’ lived experiences. This integrative framework calls for the development of measures that allow more comprehensive and dynamic assessments of ethnic minority and immigrant populations’ causal beliefs about mental illness.
Beliefs About Mental Distress and Illness: Illness Identity and Meaning of the Illness Experience
The culturally infused engagement (CIE) model proposes that the conceptualization of mental illness and mental health problems significantly shapes the ways in which an individual may ascribe meaning to the experiences of distress or illness and hence their motivation to engage in treatment. Beliefs play a central role in how individuals interpret the illness experience, which is expressed in the attitudes, affect, and behaviors toward the illness or persons with the illness (Petrie et al. 2007). Beliefs and attitudes toward mental distress and mental illness have largely been examined within two overlapping literatures—the literature on explanatory models of illness and on mental health stigma.
As illustrated in the CIE, explanatory models of illness are central to conceptualizations of mental health. Kleinman (1978) purports that explanatory models encompass several dimensions of an individual’s beliefs about mental illness/distress—from beliefs about the illness, about personal and social meanings associated with the illness, and about healing approaches and expected outcomes. Since culture is the essential context that shapes explanatory models of illness, it provides the foundation for variations in the interpretations and definitions of distress/illness that are represented in individuals’ beliefs, norms, and practices regarding the illness experience.
Cross-cultural evidence suggests that cultural health beliefs often determine individuals’ endorsement of positive or negative beliefs about mental illness. For example, among German adults, Schomerus et al. (2014) found links between biogenetic beliefs and lower social acceptance for schizophrenia and depression but higher acceptance for alcohol dependence, whereas psychosocial beliefs for schizophrenia resulted in higher acceptance. Wong et al. (2004) found that Chinese caregivers of individuals with mental illness felt less of a family burden that those from other cultures, positing that traditional Chinese medical beliefs de-emphasized family members themselves as a cause of the mental illness. Among Latino parents, Lawton et al. (2014) found that parents who reported higher levels of familism and strongly endorsed traditional gender roles were more likely to attribute sociological or spiritual causes for their child’s ADHD. Fan (1999) noted that compared to Caucasians, Asians and others (participants of other ethnicities) were more likely to endorse authoritarian attitudes that perceived individuals with mental illness as different and inferior to normal persons. Overall, research demonstrates the important role of culture as a key determinant in the variations across individuals’ endorsement of positive/supportive or negative/stigmatizing beliefs about mental health.
Related to explanatory models of illness, the literature on mental health stigma has provided a rich empirical basis of negative beliefs, attributions, and attitudes associated with mental illness. Stigma, which is defined as either an actual or inferred attribute marked by social deviance or social disapproval (Goffman 1963), manifests itself via negative sociocultural stereotypes and prejudices that are ascribed to the mental illness itself or the person with mental illness. Research suggests that the stigma of mental illness is pervasive cross-culturally, as are its adverse effects on individuals’ life experiences and opportunities (Koro-Ljungberg and Bussing 2009; Mak and Cheung 2012; Mukolo and Heflinger 2011). Evidence also indicates, however, that the concept of stigma and its influence on individuals is culturally determined, resulting in varied understandings of what constitutes “abnormal” or “undesirable” (Mak et al. 2007; Kleinman 2004). Through shaping explanatory models of illness, culture influences the formation of specific stigmatizing beliefs and attributions regarding mental health problems.
Beliefs about mental illness that are manifested as stigma are present in three forms: public stigma, self-stigma, and courtesy or associate stigma. Public stigma, which is the most examined, is described as the shared negative beliefs and attitudes that prompt others to reject, avoid, and discriminate against individuals with mental illness (Corrigan and Miller 2004; Corrigan and Penn 1999). When stigma about mental illness is manifested within an individual, it leads to a loss of self-esteem and self-efficacy (Watson et al. 2007). Self-stigma involves a process: The individual becomes aware of the social stereotypes associated with mental illness, agrees with them, and then applies stigma to the self (Corrigan et al. 2009). Finally, courtesy or associate stigma affects those who are close to the stigmatized individual. They are devalued or socially downgraded based solely on their relationship with the individual with mental illness. These distinct forms of stigma reflect critical dimensions of beliefs about mental illness that we follow in our review of existing measures below.
Our review found of the 119 measures, 50% (60) assessed CIE domains regarding attributions and beliefs toward mental distress including: (a) illness identity beliefs regarding mental distress, (b) beliefs about characteristics or internal traits of individuals with mental distress, (c) attitudes and expected responses of individuals with mental distress, (d) agency and control beliefs of the individual with mental distress, (e) perceived norms of external responses to individuals with mental distress, and (f) beliefs about close family members or associates of individuals with mental illness (Fig. 1; Table 4).
Illness Identity Beliefs About Mental Illness/Mental Health Problems
Illness identity beliefs about mental illness were assessed by 33% (20 of the 60) measures that broadly identified two views of mental illness: (a) beliefs and attitudes regarding the legitimacy or authenticity of mental illness/mental health problems, and (b) and beliefs and attitudes about the severity, treatability, and curability of mental illness/mental health problems (Table 4). Both views encompass beliefs that directly relate to the perceived origin or cause of mental illness or mental health problems.
Of the 60 measures, 12% (7) of the measures assessed beliefs related to the legitimacy/authenticity of mental illness (Table 4). These included beliefs about mental illness as: “not a real illness or disease,” involving “fake symptoms,” invented by drug companies,” “behaviors that people engage into gain medications,” and “habitual behaviors.” These beliefs were predominantly identified in measures of stigma for specific DSM diagnoses (e.g., ADHD, generalized anxiety disorder) and not commonly found across measures. In general, these beliefs pointed to an inclination of others to minimize the authenticity of mental illness/mental health problems—a view that sharply contrasts with pervasive notions of mental illness that are characterized by visible deviations from the norm (e.g., crazy, dangerous). This is likely to demonstrate the proclivity of the lay public to perceive symptoms of schizophrenia as indicators of mental illness, and hence, ambiguity in identifying symptoms of other mental disorders such as depression, anxiety, and ADHD (Angermeyer and Dietrich 2006; Bussing et al. 2003).
Twenty-three percent (14) of the measures assessed beliefs regarding the permanency, severity, and controllability of mental illness. Measures identified the following beliefs about mental illness/mental health problems as: “a serious or severe illness,” “controllable,” “incurable,” “unable to recover from,” “will not improve if treated” and “will never get better.” These responses highlight the dichotomy in the public perception of mental illness as either: (a) a condition that is unchangeable, or (b) a condition that is changeable and under the control of the suffering individual. Beliefs regarding the controllability versus permanency of mental illness link directly to the attributed causes of mental illness, for example, biological or genetic explanations are likely to be associated with perceptions that mental illness is permanent and outside of the control or responsibility of the individual (Angermeyer et al. 2003). In contrast, a belief that mental illness can be controlled suggests that the causal factors are malleable, and further, that the responsibility of mental illness lies within the individual (Feldman and Crandall 2007). It has been noted that attributions that place responsibility outside the individual are associated with less stigmatizing beliefs and attitudes (Barrowclough and Hooley 2003) and decreases in harsh treatment (Wilcox et al. 2007); however, cultural variations appear to exist (Milstein et al. 1995).
Overall, these measures illustrate that despite the predominance of the biomedical framework in health services, lay conceptualizations of mental health tend to follow explanatory models of illness. This discrepancy in the conceptualization of mental health highlights the critical need to bridge the gap between health services and the lay individual in approaching the diagnosis and treatment of mental illness or mental health problems.
Beliefs About the Meaning of the Illness Experience to the Self
Explanatory models of illness highlight the notion that illness extends beyond biological mechanisms of pain and/or dysfunction to encompass meaning and personal impact, which are influenced by the beliefs and attitudes of the individual (Kirmayer 2001; Kleinman 1980, 1987). Individuals make meaning of their lived illness experience through the dynamic process of developing an understanding of it, then responding to this understanding through cognitive, attitudinal, emotional, and behavioral avenues. The meaning of the illness experience that is derived serves a critical foundation from which emerges the beliefs, attitudes, and actions of help seeking, as illustrated in the pathway of engagement from problem recognition, help seeking, and finally to actual engagement (Fig. 1).
Reflective of this, 78% (47) of the 60 existing measures on beliefs about mental distress assessed individuals’ interpretations of the lived illness experience of mental illness/mental health problems. The measures assessed the following dimensions of the individual’s lived illness experience: (a) beliefs about the characteristics/internal traits of the individual with mental distress, (b) attitudes and expected outcomes toward the illness experience, (c) agency or control beliefs/attitudes of the illness experience, (d) perceived norms of the (i) internal experience (beliefs about how others think of the illness experience) and (ii) external responses (beliefs about how others respond to the individual), and (e) beliefs about close family members or associates of individuals with mental illness (see Table 4).
Beliefs About Characteristics/Internal Traits of Individuals with Mental Illness or Mental Health Problems
Fifty-eight percent (35) of the 60 measures assessed beliefs that described characteristics or internal traits of individuals with mental illness or distress (Table 4). Characteristics were described according to their internal traits and behaviors. Internal traits included being bad (e.g., flawed, damaged), dangerous, unstable, lazy, egoistic, untrustworthy, weak, lacking competency, and having a deficit (e.g., lower IQ, lower social status). Behavioral characteristics clustered into behaviors related to: (a) harming others, (b) level of trustworthiness, (c) level of competency or functioning, (d) self-centeredness, and (e) personal responsibility for the mental illness/mental health problem. The majority of responses on behavioral characteristics recorded beliefs doubting the competence of individuals with mental illness/mental health problems: that they are unable to keep a job, follow social rules, function in society, or take on roles of responsibility (in parenting, for example). Overall, the items assessing characteristics of individuals with mental illness portrayed beliefs reflective of a deficit approach to mental illness—a perspective that continues to dominate across research and practice and among the general public (Kleinman 2004).
These shared beliefs about the internal traits or characteristics of individuals with mental illness or mental distress are also manifested at the individual level, in the form of self-stigma. Eight measures assessed self-concept beliefs reflective of public stigma (e.g., feeling damaged, belief that he/she is not good/is bad), signifying an internalization or self-concurrence of the negative social stereotypes associated with individuals with mental illness (Watson et al. 2007). The internalization of such stereotypes associated with mental health problems or mental illness elicits negative emotional, attitudinal, and behavioral responses and thereby significantly shapes the internal illness experience of the individual.
While the negative estimation of individuals with mental illness is shared across social contexts, evidence also points to significant cultural differences. For example, Whaley (1997) found that Asian Americans and Latinos attributed more dangerous perceptions to individuals with mental illness, regardless of the level of contact, than Caucasians. Differences also were observed between African Americans and Caucasians: Greater contact with individuals with mental illness decreased perceptions of dangerousness among Caucasians, and conversely increased those perceptions among African American participants. Rao et al. (2007) also noted ethnic differences in perceptions of individuals with mental illness. African Americans indicated the highest level of perceived dangerousness, followed by Caucasians and Asian Americans (similar levels) and Latinos endorsing the least. These cultural variations in beliefs about individuals with mental illness suggest the significance of culture in the conceptualization of mental health, the meaning individuals make of the illness experience, and, consequently, attitudes and behaviors toward engaging in healing and treatment.
Attitudes and Expected Outcomes of the Internal Illness Experience
Existing measures that assessed attitudes toward the individual’s illness experience consisted of: (a) the experiential attitude/emotions elicited in response to the lived illness experience, and (b) expected outcomes of the individual’s response to the lived illness experience. Thirty-one of the 60 measures (52%) included items that assessed these dimensions from the perspective of the individual with the mental illness (i.e., attitudes and expected outcomes in Fig. 1), as well as others’ inferred beliefs about the individual’s lived experience (i.e., perceived norms of the internal lived illness experience, see Fig. 1).
Seventeen measures (28%) assessed the emotional responses by the individual to the illness experience. Measures primarily described negative feelings of shame and embarrassment, guilt or disappointment, feeling different or alone (e.g., isolated, lonely, trapped), and sadness or hopelessness (e.g., depressed, miserable). These affective experiences were assessed from the perspective of the individual with the mental distress or illness (e.g., “the term ‘psychological disorder’ makes me feel embarrassed”) or inferred by others (e.g., “people who have ADHD feel guilty about it”).
Seventeen measures (28%) assessed expected responses and outcomes toward the lived illness experience that included the following beliefs: (a) beliefs about the individual’s behavioral reaction to stigma or social distancing (e.g., hiding or keeping it a secret, staying away from social situations, avoiding getting close to others), (b) beliefs about proactive responses of the individual to his or her distress or dysfunction (e.g., pulling oneself together, work out one’s own problems), and (c) beliefs about the individual’s hindering or inhibiting responses (e.g., should not apply for work/education). Eighteen percent (11) of the measures captured beliefs associated with stigma that correspond with emotional responses of feelings of shame and embarrassment. Relatedly, negative feelings of loneliness or isolation corresponded to inhibitory responses of individuals to their illness experience. These attitudes and beliefs about expected responses are reflective of the prejudices that arise from the negative beliefs or stereotypes of individuals with mental illness. This is described in the sequential process of stigma effects by Corrigan and Watson (2002) that begins with stereotypes, and moves to prejudice and consequently to discrimination. Moreover, the predominance of stigma items among the reviewed measures illustrates that it remains a primary aspect of the lived illness experience of individuals with mental distress/mental illness.
Agency and Control Beliefs
The second dimension that emerged from the measures assessed beliefs about the level of agency or efficacy of the individual with mental distress/mental illness (Fig. 1; Table 4). Forty-seven percent of the measures (28 of 60) captured beliefs that ranged from low agency or self-efficacy beliefs (e.g., cannot pull myself together, little can be done to improve me, I cannot contribute to society) to positive efficacy beliefs (e.g., able to live life I want, I have goals to reach, I can control my mood/behavior). These agency or efficacy beliefs correspond with the negative attitudes and expected responses assessed among our measures, highlighting that together, they shape meanings the individual makes of his/her lived illness experience. For example, a belief that “I cannot contribute to society because of my mental distress” (efficacy belief) may elicit feelings of guilt or shame along with the belief that “I should stop pursuing a job” (attitudes and expected responses or outcomes), and hence, determine the actual behavioral outcome shaped by these internal processes (i.e., stop applying for a job).
According to Corrigan and Watson (2002), the internalization of negative social/public stereotypes of individuals with mental illness yields the undesired effects of diminished self-esteem and self-efficacy, which are manifested as negative feelings and attitudes associated with having a mental illness/mental health problem. The measures reflect this process of self-stigma through the dimensions of (a) negative attitudes and expected responses, (b) agency or efficacy beliefs, and (c) perceived norms or negative feelings and attributions associated with inferred social judgments or social responses toward the self (which we discuss below). These internal mechanisms may result in behavioral responses of self-discrimination such as isolating the self, hiding or keeping one’s mental illness/mental health problem a secret, and avoiding others. In this way, understanding the internal processes of attitudes, expected outcomes, and agency beliefs is particularly pertinent to examining the lived illness experiences that then determine help-seeking behaviors.
The internal experience of mental illness across cultural groups is less understood. A study by Wong et al. (2016) compared the stigma of mental illness across a multiethnic sample of adults and found that Asian Americans felt the highest levels of self-stigma, followed by Latinos interviewed in English. Authors noted that Asian Americans culturally tend to endorse higher levels of stigma beliefs about mental illness than others, which are likely to be transposed onto self-beliefs, resulting in high self-stigma. Brown et al. (2010) found that internalized stigma mediated the effects of public stigma on attitudes toward mental health treatment among Caucasian adults, but, conversely, for African American adults, internalized stigma was directly associated with negative attitudes toward mental health treatment, which suggests ethnic differences in how public stigma and self-stigma influence help-seeking attitudes. Although limited, the variation across ethnic groups noted in these studies suggests the need for the examination of culturally specific beliefs about the self in relation to mental illness/mental health.
Perceived Norms of External Responses to Individuals with Mental Illness
This last dimension of the lived illness experience of individuals captured perceived social norms about others’ responses to individuals with mental illness/mental health problems. Specifically, the measures identified beliefs about others’ responses toward individuals with mental illness (descriptive norms) from a societal or public perspective (e.g., public stigma), or inferred by the individual with the mental illness. These beliefs, which were partitioned into either discriminatory or supportive behavioral beliefs, represent the construct of social distance, defined as the proximity of relationships one willingly engages in with individuals with mental illness (Bulanda et al. 2014). Social distance that is low is characterized by a shared set of experiences that facilitates a sense of belonging to a group and a common identity, thus inferring involvement and identification with individuals with mental illness. In contrast, high social distance is described as aloofness and disengagement often due to fear, by which individuals with mental illness are considered as an outsider or even as adversaries (Steinbach 2004). Conceptualizations of mental illness underlie the behavioral beliefs related to social distance—evidence indicates that social distance is significantly tied to perceptions of dangerousness (Angermeyer et al. 2004), perceived control or responsibility the individual has over his or her mental illness (Dietrich et al. 2004), and perceived course of the mental illness (e.g., curability) (Angermeyer et al. 2003).
Review of existing measures shows that 57% of measures (34 of the 60) assessed the endorsement of discriminatory behaviors such as limiting or restricting responsibilities of individuals with mental illness (e.g., not hiring), unfair treatment (e.g., discrimination, talking down, patronizing), social exclusion and avoidance (e.g., treating individuals like outcasts, ignoring them, being unwilling to associate with them) (Table 4). The predominance of high social distance beliefs across measures points to the pervasiveness of stigmatizing attitudes and behaviors among the public. This is of critical concern particularly for ethnic minority and immigrant children and families, since evidence identifies public stigma as a significant barrier to engagement in mental health services and a predictor of poorer psychological outcomes (Parcesepe and Cabassa 2013; Pescosolido 2013).
However, understanding public stigma among ethnic minority and immigrant children and families has its complexities. Culture has a powerful effect in shaping beliefs about mental illness through specific cultural beliefs, practices and explanatory models of illness, resulting in differences across cultural groups in the norms and attitudes toward individuals with mental illness. Moreover, the extent to which a culture exerts its influence in shaping norms related to mental illness (and hence public stigma) may vary depending how individualistic or collectivistic it is. In collectivistic cultures, where the individual is viewed as an extension of systems or relationships rather than an autonomous entity, cultural and social norms of mental illness and help seeking are likely to heavily influence individuals’ attitudes and behaviors toward people with mental illness. For example, it is common among Asian cultures that displays of emotionality are considered counter to the cultural values of emotional restraint and social conformity, which may result in stigmatizing attitudes and associated behaviors toward individuals who display emotional distress or mental health symptoms (Park et al. 2010; Yong and McCallion 2004). On the contrary, individualistic cultures place emphasis on the needs, desires, and autonomy of the individual over those of the group; thus, individuals’ own attitudes and beliefs toward the mentally ill might be less affected by the pressures from the broadly shared cultural values and norms. This link between stigma and culture has been noted in a few studies of collectivistic cultures that positively associated stigma toward mental health treatment (e.g., counseling, use of medications) and the endorsed cultural values (Interian et al. 2007; Miville and Constantine 2007).
Of the 60 measures, 20% (12) assessed low social distance behavioral beliefs. These included: caring for mentally ill individuals (e.g., supporting them financially), showing sympathy to them, engaging with them (e.g., working closely, socializing, being willing to be a friend, family, neighbor, being comfortable talking with), and giving responsibility to them (e.g., having same rights to a job). In general, these beliefs reflected benevolent and inclusive attitudes and behaviors toward individuals with mental illness. The literature describes benevolent attitudes toward individuals with mental illness as a moral, paternal, sympathetic, and embedded in humanistic principles (Cohen and Struening 1962). Higher benevolent attitudes toward persons with mental illness have been associated with higher education (Barke et al. 2011), increased contact (Corrigan et al. 2001), lower adherence to traditional gender roles (Hinkelman and Granello 2003), and familiarity with mental illness (Arvaniti et al. 2009).
Studies have also found cultural or ethnic differences in supportive or benevolent beliefs that are linked to cultural health beliefs and values. Shokoohi-Yekta and Retish (1991) examined Chinese and American adult males’ attitudes toward individuals with mental illness and found that, compared to Chinese men, American men were more likely to be benevolent, less authoritarian (i.e., stigmatizing), and less socially restrictive, believing that individuals with mental illness should be more integrated into society. Among a sample of college students, African Americans endorsed lower benevolence and higher authoritarianism and social restrictiveness compared to Caucasians, while Hispanic students had similar ratings to Caucasians of benevolence and social restrictiveness (de Crane and Spielberger 1981). Corrigan and Watson (2007) also found that compared to Caucasians, ethnic minority participants endorsed higher levels of stigma toward individuals with mental illness and their families. Despite the fact that these studies highlight the interwoven nature of culture in mental health beliefs and attitudes, existing measures largely assess stigma as an etic construct and are not sensitive to capturing culturally nuanced stigma beliefs. That points to the need for methodological advances in this area.
Beliefs About Close Family Members or Associates of Individuals with Mental Illness (Courtesy Stigma)
Courtesy stigma bridges the internal experience and external responses, extending the consequences of the identity of a person in a network (e.g., a family member) to the affected individual. This final domain identified 17% (10) of the 60 measures that assessed beliefs and attitudes associated with family or close associates of individuals with mental illness/mental health problems (Table 4). While fewer measures assessed courtesy stigma, the examination of beliefs and attitudes toward family members/close associates of individuals with mental illness may be pertinent for immigrant and ethnic minority children and families. Family members of individuals with mental illness often experience significant hardships that include objective burdens (practical, financial, and logistic aspects of caring for the individual with the mental illness) and subjective burdens (psychological, social, emotional, and relational difficulties) (Hinshaw 2005). Families report that subjective burdens, which include the challenges of mental health stigma, are greater than the objective ones (Thompson and Doll 1982). Family members of individuals with mental illness are likely to encounter courtesy stigma, which is the extension of stigmatizing beliefs and attitudes to close others based on mere association (Corrigan and Miller 2004; Mehta and Farina 1988). Research indicates courtesy stigma affects parents and family members in several ways including self-stigma/internalization of stigma, relational stigma, and further, institutional stigma (Muhlbauer 2002; Singh 2004). Our review found that 9 of the 10 measures captured the internalization of stigma of a child or close family member with mental health problems. Examples of internalized beliefs due to a child/family member’s mental health problems include: embarrassment, feeling helpless or sad, feeling inferior, feeling incompetent, and thinking one’s reputation is damaged. The self-identification with stigma may be particularly relevant for caregivers or parents of children with mental illness/mental health problems. Studies suggest that parental internalization of courtesy stigma is closely linked with parental causal beliefs that identify parental discipline or care as causes of mental illness. These beliefs lead to perceptions of the self as a “bad parent” (Lee et al. 2014) and also lower parental efficacy (Singh 2004). In contrast, when causes of the child’s mental illness are located externally, family members are likely to experience less subjective burden (Wong et al. 2004).
In addition, for immigrant and ethnic minority families from collectivistic cultures, courtesy stigma may be particularly salient due to the interdependent construal of self which is defined by close relationships (Markus and Kitayama 1991). In interdependent relationships, the negative attributions associated with a family member suffering from mental illness are extrapolated to a negative sense of self among others in the relationship. For example, Mak and Cheung (2012) found that Chinese caregivers who endorsed strong concerns about maintaining mianzi, or face (social image and worth constructed through interpersonal relationships), tended to internalize stigmatizing beliefs associated with their family member’s mental illness, and, as a result, experience greater subjective burden and distress.
Measures assessing courtesy stigma also captured the relational effects of the stigma on family members who believed it caused problems for family, affected the marriage of family members, caused others to think less of the family, and made family members unwilling to include those suffering from mental illness as a part of the family. Studies indicate that parents and family members struggle with the burden of courtesy stigma on interrelationships. For example, beliefs associated with the fear of avoidance by others, social rejection, and discrimination are reported among parents of children with mental health diagnoses (Corrigan and Miller 2004; Dempster et al. 2015; Shibre et al. 2001). Moreover, evidence suggests that family members engage in behavioral responses to the stigma by concealing the family members’ mental illness from others (Stengler-Wenzke et al. 2004), avoiding seeking treatment (Moses 2010), staying silent about their child (Koro-Ljungberg and Bussing 2009), and hiding or limiting the social contact of the family member with the illness (Lin et al. 1981).
Overall review of existing measures indicates that an individual’s conceptualizations of mental health significantly influence and are influenced by his or her own understandings of the illness experiences (the meaning of the distress) and further, the interpersonal illness experiences of the individual and his/her associated networks (reactions to the distress). These influences may function on different ecosystemic levels, as well as through interactions between these systemic mechanisms (see Fig. 1). For ethnic minority and immigrant children and families, the interwoven nature of networks within their ecosystem (e.g., immediate family, relatives and friends, church, ethnic community, broader social institutions) is especially strong and integral to their lived experience and sense of self, which underlines the importance of using a more culturally/contextually infused and dynamic perspective in understanding ethnic minority and immigrant families’ beliefs about mental illness.
Our review also highlights some gaps in empirical measures. Of the 60 measures, only 2% (1) were designed to assess beliefs associated with culturally specific interpretations of mental distress. The remaining measures either assessed beliefs about mental disorders described by the DSM classification, which posits the biomedical/biopsychosocial view of mental distress, or assessed beliefs associated with general mental health terminology (e.g., mental illness, mental health problems) that presume universality in the understanding these terms across culturally diverse individuals (i.e., construct equivalence). An over-reliance on existing measures may result in mismeasurement and misrepresentation of ethnic minority and immigrant families’ beliefs, attitudes, and reactions to their own illness experiences. To more effectively recognize ethnic minority and immigrant children and families’ multi-leveled needs, encourage their motivations for change, and identify proper resources and approaches to improve their engagement in services, more culturally/contextually infused empirical measures need to be developed to better understand these groups’ unique beliefs in the first place about mental distresses and their effects on the individual and his/her interpersonal relationships.
Beliefs and Experiences of Seeking Help: Beliefs About Healing Approaches and Help-Seeking Behaviors
Epidemiological studies indicate that 40% or less of individuals in the general public with diagnosable mental health problems seek any type of professional help (e.g., Howard et al. 1996; Kessler et al. 2001; Norquist and Regier 1996; Wang et al. 2005), and even fewer seek help among ethnic minority children and families (Kim et al. 2011; Matsuoka et al. 1997; Nguyen and Anderson 2005; Derr 2016; Sue et al. 2012; Sue and Sue 1974; Vega et al. 1999). Although research has tried to explore and identify a variety of factors that may affect the aspects, levels, and processes of mental health service utilization for people in need, most scholarship on service utilization is founded on modern medical and psychological philosophies and practical frameworks of mental health treatment, which has overlooked the notion that help seeking could be a culturally determined behavior (Messent 1992; Nadler 1986a; Seiffge-Krenke and Shulman 1990).
Current empirical literature on service utilization examines either individuals’ beliefs and/or attitudes toward professional services for mental health, or individuals’ past or present experiences of treatment encounters. Thematically, across this belief–attitude–experience spectrum, these literatures largely fall into four overlapping areas—mental health knowledge and literacy, stigma of using professional service, control factors and willingness of help seeking, and provider–client relationship.
The culturally infused engagement (CIE) model depicts help-seeking intentions as the entanglements of three major belief dimensions—beliefs about the potential outcomes and/or attributions of the help-seeking behavior (behavioral belief), beliefs related to social and subjective norms of the behavior (perceived norms), and beliefs about individuals’ capacity in dealing with factors that might hinder or facilitate the behavior (agency/control belief) (Fig. 1). The literature on mental healthcare knowledge and expectations, one major aspect of which focuses on beliefs about the efficacy/outcomes of mental health treatment, offers us one direction in investigating individuals’ behavioral beliefs about help seeking. An article by Jorm et al. (1997) first introduced the comprehensive concept “mental health literacy,” developed from earlier literature on general health literacy, evaluating not only individuals’ ability to recognize specific types of mental health problems and their causes, but also individuals’ knowledge and beliefs about available professional help and attitudes facilitating proper help seeking (Jorm 2000). In line with this, many have argued that low levels of knowledge about and negative attitudes toward mental health treatments discourage treatment enrollment and adherence (Bayer and Peay 1997; Downs and Eisenberg 2012; Kelly and Achter 1995; Moskos et al. 2007; Strong and Claiborn 1982). In particular, certain negative beliefs about the efficacy of professional services might be caused by the inadequate knowledge and false information about the mental disorder and its attributions, resulting in delayed help seeking (Johnston and Freeman 2002). Thus, researchers with this perspective have called for expanding educational interventions to improve the public’s mental health literacy (Hom et al. 2015; Jorm et al. 1997).
Positive beliefs and attitudes about a behavior’s consequences alone cannot lead to individuals’ intentions of enacting this behavior; perceived norms also play a major role in directing individuals away from engaging in behaviors that would potentially cause social deviance and disapproval. The impacts of norms in the field of mental health have largely been captured within the framework of stigma. In accordance with the importance of stigma in understanding negative beliefs and attitudes associated with mental illness, a number of studies have examined the forms and degree of stigma toward mental health treatment as well as how it may affect treatment engagement. Similar to the conceptual structure of stigmatizing beliefs about mental illness, two major forms of stigma, i.e., public stigma and self-stigma, have been identified and operationalized in discussing normative beliefs about mental health treatment, while very limited numbers of studies have included survey items assessing courtesy stigma toward treatment (e.g., Hirai and Clum 2000; Taylor and Dear 1981). Building upon the discussions about societal stigma toward mental illness, public stigma toward mental health treatment has been understood as “label avoidance” (Corrigan 2004, p. 616): that individuals may avoid seeking professional services due to the fear of being labeled as the stigma-attached “mentally ill” (Clement et al. 2015). Self-stigma on the other hand addresses the beliefs that seeking professional help would lead to the acknowledgement of one’s weakness, inferiority, or failure, and thus threaten one’s self-esteem (Corrigan 2004; Fisher et al. 1982; Vogel et al. 2006). Courtesy stigma signifies the beliefs that individuals or communities would be downgraded by geographically or socially closely associating with those seeking mental health treatment or mental health facilities.
In addition to beliefs about efficacy and stigma, real-life barriers and individuals’ beliefs about their ability to overcome the barriers to engagement are another important aspect frequently discussed in mental health service utilization literatures. Our review of existing measures revealed that measures assessed perceived control factors that might hinder or facilitate help seeking as well as individuals’ beliefs about their own agency and inclination toward seeking professional help (see Table 5). Objective barriers and resources have long been discussed in the literature of mental health service utilization (e.g., Staudt 1999; Stefl and Prosperi 1985). Several recent studies have adopted a more comprehensive perspective, building upon the TPB model, taking into account the dynamics between perceived barriers and the subjective beliefs about one’s willingness and self-efficacy regarding help seeking (King et al. 2007; Mackenzie et al. 2004). Besides, many studies on service utilization also include survey items measuring sources of help other than professional services that one might be inclined to reach out to (e.g., Cohen 1999; Rostain et al. 1993; Scior and Furnham 2011). From a service utilization perspective, rather than a social network one, these alternative sources of help have been considered “barriers” to professional help seeking (Kuhl et al. 1997). Scholarship of this aspect has offered us a more complex framework to explore why levels of stress or recognition of the need for psychological assistance alone cannot consistently predict behaviors of service engagement.
A significant amount of literature also points to the centrality of individuals’ beliefs and experiences of the therapeutic relationship in their intentions of engaging in mental health treatment. In particular, the therapeutic alliance, which is defined as the quality of involvement between the therapist and client, the task teamwork and personal rapport, and the therapist’s alliance-building skills (Orlinsky et al. 2004), is a central element in the therapeutic relationship that is established as a core predictor of treatment outcome, retention, client satisfaction, and treatment progress in adults and youth (Horvath and Symonds 1991; Shapiro and Shapiro 1987).
Among our reviewed 119 existing measures, 51% (61) contain items on the beliefs and experiences of mental health treatment that were organized into the following domains (see Table 5): (a) beliefs and expectations about the efficacy of professional services (behavioral beliefs about help seeking), (b) public, self, and courtesy stigma toward seeking professional help (perceived norms of help seeking), (c) beliefs about control factors and willingness of help seeking (agency/control beliefs and intentions of seeking professional help, beliefs about seeking other help), (d) beliefs about provider–client relationship, and (e) engagement behaviors (past or current experiences or behaviors).
Beliefs and Expectations About the Efficacy of Professional Services
Evidence on both mental health literacy and, to a lesser extent, clinical self-disclosure has identified that individuals’ beliefs about the helpfulness or benefits of treatment are effective predictors of help-seeking behavior (Strong and Claiborn 1982; Seiffge-Krenke and Shulman 1990; Kelly and Achter 1995; Bayer and Peay 1997). Sixty-one percent of the measures reviewed (37) contain survey items assessing this domain (Fig. 1; Table 5). In particular, these items measure either beliefs about the general effectiveness of mental health treatment or focus on specific attributes or consequences of certain treatments. Both kinds are worded in both positive and negative ways.
Among these 37 measures, 92% (34) contain items evaluating the general positive beliefs about treatment efficacy, while 53% (21) have items on general negative beliefs. On the positive side, items are framed in fairly broad terms, assessing if the respondent generally considers a certain type of treatment (e.g., social skills training for ADHD or family-centered services) or professional service to be “effective,” “helpful,” “useful,” “sufficient,” “beneficial,” or “not a waste of money.” General negative beliefs are worded as to whether professional service is “a poor way,” “not needed,” “limited,” “doesn’t work,” or “is a waste of time.” These beliefs are likely to provide a broad yet somewhat vague picture of whether or not the individual holds a favorable attitude toward professional mental health services.
With regard to positive beliefs about the specific attributes or consequences of services, measures identified: (a) What specific type or aspect of treatment (e.g., services provided through community-based facilities) is efficacious, (b) under what specific conditions the treatment (e.g., more helpful to adults than to teenagers) is efficacious, and most importantly, (c) whether the treatment is efficacious in obtaining a specific outcome (e.g., solving my emotional problem, curing my illness, preventing negative effects of my illness, controlling my illness, accomplishing the changes that I want, restoring me to my normal level of functioning).
Negative beliefs about specific attributes or consequences of services mostly follow two themes: (a) concerns about potential harmful consequences of certain treatments (e.g., medication is not safe, therapy can be harmful, my child would be taken away, people die every day because of mistakes by the health care system) or unwanted experiences (e.g., mental hospitals seem like prison, treatment would make me feel like an experimental guinea pig, I would learn things about myself that I don’t really want to know, or be pressured to make changes in my lifestyle); and (b) more detailed concerns about the ineffectiveness of certain treatments based on specific standards of judgment, which vary from a cost–benefit calculation (e.g., psychotherapy is of doubtful value considering time and expense, therapy is not universally effective due to the mismatch between self-identified needs and treatment activities) to the belief that certain service models, for instance mental hospitals, are outdated.
Studies have shown that beliefs about the efficacy of professional services are dependent upon an individual’s level of mental health knowledge (Jorm et al. 1997; Johnston and Freeman 2002; Fox et al. 2013). Furthermore, researchers have identified ethnic minority and immigrant populations as having less knowledge and awareness of existing services than Caucasian Americans, which was shown to be a significant barrier to ethnic minorities’ service utilization (Takeuchi et al. 1988; Loo et al. 1989). Researchers have emphasized that intended sources of help and problem-solving strategies correlate with indigenous beliefs about the nature and attributed causes of the problems (Kleinman 1980; Cheung et al. 1983; Leong and Lau 2001). When discussing “services” and “knowledge,” however, researchers have largely focused on a contemporary mainstream Western conceptualization of “mental health,” predominantly influenced by biomedical and biopsychosocial paradigms. Pushing back on this trend, there are studies showing that ethnic minority and immigrant populations might have different epistemological systems (e.g., mind–body holism, common among Asian Americans) in perceiving symptoms of “mental disorders,” which could impact their beliefs about what healing approaches are reasonable or legitimate, as well as the effectiveness of different help-seeking options (Kung 2004; Yang et al. 2008; Kim and Zane 2016). Although this framework of explanatory models of illness has been widely utilized in mental health research conceptually, there are hardly any empirical measures integrating a culturally informed perspective in investigating efficacy beliefs toward treatments for mental health.
Perceived Norms of Seeking Professional Help: Public, Self-, and Courtesy Stigma
Given that “people with mental illness” could be considered an institutional category co-constituted with the invention and development of modern psychology and psychiatry since the nineteenth century (Hacking 2007), the identity “mentally ill” has always been associated with certain institutional practices such as diagnosis and treatment. Someone “receiving mental health treatment” can be socially assigned into this institutional category of identity and, consequently, stigmatized as having a mental disorder.
Public Stigma
Corrigan (2004) has defined public stigma toward mental health treatment as a “label avoidance” mechanism in which people avoid seeking professional services due to a fear of being labeled as “mentally ill.” Elsewhere, Corrigan (2005) also framed public stigma as the societal prejudice (attitude) and discrimination (behavior) toward those stigmatized, which leads to reduced opportunities and unfair treatment in everyday life. Along these lines, our review of existing measures shows that 18% (11) of measures contain items assessing one or more of the following three attitudinal aspects of public stigma toward seeking professional help: (a) public beliefs about the characteristics of people receiving professional help (e.g., friends or family would think one was crazy or weak or inadequate), (b) public affective responses to people receiving professional help (e.g., parents would be upset, neighbors of mental health facilities would fear people coming to obtain services), and (c) endorsement of discriminatory behaviors against people receiving treatment or treatment facilities themselves (e.g., persons should hide from others that they have been treated, facilities should be kept out of residential neighborhoods). Measures also assessed beliefs about discriminatory behaviors that would lead to unfair treatment or limited opportunities against people receiving professional help, for example, “treatment would make me an outsider,” “I would lose friends due to treatment,” “treatment would harm my reputation/career,” or “peers might treat me differently.”
Self-stigma
Building on Scheff (1966)’s discussion of individuals’ internalization of cultural stereotypes of mental illness, Link (1987) summarized two negative consequences that might arise through individuals’ association with mental health institutions, premised upon the largely negative images of mental illness and mental services in Western culture and beyond: First, individuals may devalue themselves since they are now officially falling into an institutional category that is negatively viewed by the public, and second, individuals may develop defensive or other negative social actions and interactions due to internalized concerns of how others may think of them. As for the former, studies have shown that in fear of losing self-esteem, self-efficacy, or self-autonomy, individuals might choose not to seek professional assistance despite the fact that they are suffering mental distress (Miller 1985; Nadler 1986a, b; Vogel et al. 2006). As for the latter, individuals might avoid services or even rearrange their lives because of feelings of shame, embarrassment, or guilt that could be invoked by fear that others would find out that they are receiving services (Shapiro 1983).
Our review of the existing measures also identifies 16% (10 measures) reflecting these two aspects of self-stigma toward seeking professional help. The first aspect included beliefs about the potential reduction or loss of self-esteem due to professional service utilization, for example, treatment makes me “makes me feel like I’m crazy,” “show weakness,” “feel inadequate,” or “feel less satisfied with myself.” The second assessed the feelings or reactions individuals might have in response to subjective concerns about how others would think of them, for example, being uncomfortable seeking help because people in social or business circles might find out, being embarrassed that a neighbor might see them walking into the office of a professional, and, proactively, attempting to appear strong by dealing with problems by themselves, or arranging their lives so no one would notice.
Courtesy Stigma
The topic of courtesy stigma has not been much discussed in the literature of mental health service utilization. Only 2 different items from 3 measures fall into this category: “I would be embarrassed if people knew that I dated a person who once received psychological treatment” and “Locating mental health facilities in a residential area downgrades the neighborhood.” One possible explanation of the limited presence of courtesy stigma items in service utilization literature might be that courtesy stigma often uniquely impacts people from collectivistic cultures in which self is interdependently constructed through interactions with others in sociocultural contexts (Mak and Cheung 2012; Shibre et al. 2001). However, as we mentioned earlier, existing measures of mental health service utilization are largely rooted in mainstream philosophies and practical frameworks of mental health treatment, with very limited attention paid to minority cultures and non-traditional frameworks. The two courtesy stigma items reviewed here are from studies focused on an Asian American population and community-based care, respectively, which are relatively exceptional topics among literature of this domain.
As we discussed above, there are complexities in understanding stigma among ethnic minority and immigrant populations due to the influences of culture, which could fundamentally shape the way in which people conceptualize self, health and illness, normality and deviance, social inclusion and exclusion, and of course, “mental illness” and legitimate healing approaches. It is reasonable to argue that the ways and degrees in which culture impacts the stigma toward mental illness may offer us some insights into understanding the role culture plays in the stigma toward service utilization. However, the mechanisms of service utilization could be even more complex with regard to factors such as the subjective level of distress, the global expansion of the legitimacy of the biopsychosocial model in mental health conceptualization, and the disparities in the quality and quantity of mental health education and service infrastructures. Even the conceptualizations and enactments of culture itself have become more complicated in reflection of the vibrant global mobility of people, knowledge, and practices. An interesting finding revealed by our review of this area might speak to this complexity: The correlation between stigma toward mental illness and mental health service utilization is inconsistent across several different studies. While some argue that stigma dissuades help seeking (Hirai and Clum 2000; Vogel et al. 2006; Fox et al. 2013), others find an insignificant relationship between indifference to stigma and help-seeking propensity (Farina 2000; Mackenzie et al. 2004; Golberstein et al. 2008). Future empirical studies are needed to incorporate cultural aspects as well as the experiences of ethnic minority and immigrant children and families, to better explore the complex mechanisms of how stigma toward mental health treatment impacts service utilization.
Agency and Control Beliefs and Willingness of Help Seeking
In their proposed “elements of treatment” model, Aday et al. (1984) have identified the need for help, predispositions toward help seeking, and enabling factors (the accessibility and cost of services), as the three major elements that contribute to individuals’ professional help-seeking behaviors in medical care. In other words, individuals’ decisions and actions regarding seeking professional help are affected not only by their internal recognition of problems/needs and normative attitudes toward mental illness and treatment, but also by their beliefs about external factors that might hinder or facilitate the access to services. Similarly to the “elements of treatment” model, Stefl and Prosperi (1985) have categorized four dimensions of barriers that contribute to the underutilization of mental health services: availability (knowledge about service resources), accessibility (transportation and company), acceptability (concerns about what others might think), and affordability (cost of money and time). Among these dimensions, their empirical study further concluded that for those in need of services, affordability, availability, and accessibility are greater barriers than individuals’ concerns about being stigmatized by others. In line with these arguments, Mackenzie et al. (2004) also pointed out the weak relationship between indifference to stigma and help-seeking propensity which is complicated by factors such as “how busy individuals see themselves at any given time” (Mackenzie et al. 2004, p. 2428). These studies highlight the importance of understanding how individuals’ beliefs about external control factors might affect help-seeking intentions and behaviors.
Control Factors in Seeking Professional Help
Among our reviewed measures, 8% (5) assessed individuals’ beliefs about barriers that lessen help-seeking intentions (see Table 5). Items are framed as “[I] don’t have time,” “[I] could not afford [treatment],” “[treatment would] cost too much money,” “[I] do not have adequate transportation,” “[I] have no accompany me,” or “[I have] difficulty getting time off work/school.” From the TPB perspective, a lack of sense of control over these external barriers, due to lack of knowledge and resources, may prevent individuals from getting treatment, even when they obtain a positive attitude toward seeking treatment after weighing treatment benefits over perceived stigma (Britt et al. 2008). On this note, there are also measures directly assessing beliefs about one’s agency (or lack of agency) in getting services in regard to the barriers. Twenty-one percent (13) of measures have items examining if an individual “feels responsible for this choice of treatment,” “knows where to find a therapist if needed,” “has the skills or abilities needed to participate in the treatment,” “can easily find the time to see a professional for psychological problems,” or “knows the advantages of individual treatment options.”
Facilitating Factors in Seeking Professional Help
Five percent of measures (3) capture individuals’ beliefs about facilitating factors for treatment engagement from a personal help-seeking perspective, i.e., what might make me more willing and able to get services, most of which emphasized the influences of intimate relationships in one’s help-seeking intentions and behaviors (see Table 5). Items are framed as “my child’s behavior cannot change without my involvement in treatment,” “others encourage me to seek help,” or “I’m sure my family will not let me live at home if I did not come to treatment.” This aligns with the finding of Gulliver et al. (2010) in their literature review that facilitators were under-researched compared to barriers. However, some measures promoting specific treatment models (e.g., family-centered care, community-based care) assess beliefs about what elements on the treatment paradigm or welfare system level might contribute to better engagement and/or outcomes of professional care. For example, items include beliefs about the importance of “having health insurance coverage,” “attending to needs of all family members,” or “spending more tax money on treatment of the mentally ill.” Two measures adopted a client-centered narrative-based approach that also assesses clients’ beliefs about “what made that treatment work well,” according to their own narratives of illness and treatment experiences. These measures, though having very particular focus in each case, signify the need for and potential of acting upon professional mental health care on the conceptual paradigm, and structural levels limit current gaps and disparities in service utilization on a larger scale.
Intentions to Seek Professional Help
Lastly, 33% (20) of reviewed measures contain items directly assessing intentions to seek professional care (see Fig. 1; Table 5). Some items are framed as willingness under certain conditions, without suggesting factors that might contribute to this intention. Items like this are often framed in the following structure: if I had a problem of XXX (e.g., if I was worried or upset for a long period of time, significantly anxious or depressed, having a mental breakdown, or experiencing a serious emotional crisis), I would want to see a professional (e.g., therapist, psychologist, counselor). There also some items assessing individuals’ intentions without identifying conditions, such as “getting counseling seems like a good idea to me,” “I am getting counseling because I want to,” or “I accept that I will come to every appointment.” Fischer and Turner (1970) conceptualized items like this as indicators of “recognition of need for psychotherapeutic help,” which, together with stigma tolerance, interpersonal openness, and confidence in mental health practitioners, forms comprehensive attitudes toward seeking professional help. Mackenzie et al. (2004), building upon Fischer and Turner (1970)’s framework, and using “help-seeking propensity” to capture both willingness toward and agency of seeking professional help, argue that help-seeking propensity much more strongly correlates with mental health service use than either psychological openness or indifference to stigma. Though items of this kind have offered us empirical evidence supporting the relationship between the intention and action of service use as proposed by TPB, they are limited, compared to other domains of items we have reviewed, in further identifying how and why the intention to seek help or engage in services might have been developed and transformed.
Items of our reviewed measures have covered a wide range of dimensions regarding individuals’ perceived control factors and willingness to seek professional help, offering rich empirical data and analytical possibilities to form more comprehensive conceptual models in understanding the complex relationship between beliefs, attitudes, and actual actions of service utilization. However, there are different kinds of barriers to treatment faced by ethnic minority and immigrant populations that are not yet captured by these measures. These barriers not only reveal the systematic gaps within the current service infrastructure in serving those populations, but also reflect the role of culture in shaping their perceived availability of supports. For example, empirical studies by Uba (1982) and Spencer and Chen (2004) have shown that language barriers and a shortage of bilingual and culturally sensitive service providers are significant barriers to service utilizations for Asian Americans, in addition to other factors such as differentiated mental health conceptualizations and limited mental health literacy that we reviewed earlier. Shin (2002) focused on prolonged informal care practices and lack of interface between medical and mental health services as factors that contribute to delayed help seeking among Korean immigrants in the USA. Studies like these call for integrating ethnic minority and immigrant populations’ unique cultural preferences and life experiences into understanding their help-seeking barriers as well as systematically intervening on their underutilization of services.
Seeking Other Help
Interestingly, research on service utilization for mental illness has inconsistent findings on whether alternative coping strategies and the availability of other sources of help are barriers or facilitators for professional treatment engagement. Review of measures indicated that 36% (22) assessed alternative approaches to coping with or healing mental distress (Table 7). Twenty-one percent (12) of the measures contain items assessing self-reliance as a coping strategy that prevents one from reaching out to services. Items range from generalized beliefs about “solving [issues] by oneself” or “working out one’s own problems” to specific self-coping strategies such as “getting out more,” “going on holiday,” and “keeping one’s mind on a job.” Nineteen percent (11) of the 61 measures have items evaluating informal sources people might turn to for help, including family, relatives, friends, teachers, and community networks. Though it has been argued that prior tendency to use informal supports may positively associate with help-seeking tendency in general (Saunders 1993), studies have also found that reliance on family, friends, self, indigenous practices, or other informal social support networks could be an important factor that delays individuals’ entering of the professional service delivery system or keeps them out entirely (Horwitz 1978; Kuhl et al. 1997; Saunders 1993).
Twenty-three percent (14) of the measures assessed alternative or folk remedies as coping strategies for mental illness. From a mental health literacy framework, folk remedies are considered barriers that could lead to delayed treatment seeking due to individuals’ lacking understanding of the nature and causes of certain illnesses (Johnston and Freeman 2002; Mackenzie et al. 2004; Rostain et al. 1993). Measures captured individuals’ beliefs about the effectiveness of “special diet,” “reducing sugar intake,” “vitamin therapy,” or “massage therapy” for treating ADHD. From an explanatory model of illness perspective, alternative healing approaches are valued neutrally, if not positively, as culturally bound coping strategies that align with individuals’ own epistemologies of their illness experiences. In addition, measures also assessed beliefs about using alternative healers and healing approaches in dealing with mental illness, such as “using natural remedies,” “using herbal remedies,” “chanting,” or “attending a place of worship more often.” However, our current review project doesn’t fully incorporate the rich literature on social networks and support for mental health care, which limits our ability to evaluate more thoroughly if and how informal sources of help may affect professional service utilization for mental illness.
Relational Beliefs: The Provider–Client Relationship
In addition to help-seeking beliefs, beliefs about the therapeutic relationship was prominent in our review of existing measures that indicated 30% (18) of the 61 measures assessed its dimensions (Table 5). Across measures, items clustered in the following aspects: (a) client disclosure, (b) trust, (c) provider attitudes and behaviors, and (d) provider–client collaboration.
Self-disclosure
Self-disclosure is described as the communication of information about the self to another (Cozby 1973). Self-disclosure is considered a hallmark of therapy that is vital to the development and maintenance of the provider–client relationship (Collins and Miller 1994; Farber and Hall 2002) and central to clients’ therapeutic progress and change in outcome (Ridley 1984).
Client self-disclosure was assessed by 11% (7) of the 61 measures that captured client beliefs and attitudes regarding the disclosure of personal or private details and emotions. The majority of items assessed client beliefs about such topics as the risks of disclosure, therapists’ view of clients after disclosure, and fear of confidentiality. In contrast, only one measure also included positive expectations of therapy from self-disclosure. This predominant emphasis on the risks of self-disclosure appears to be a common experience—evidence suggests that clients report feeling anxious and vulnerable before self-disclosure (Farber et al. 2004). Moreover, for ethnic minority and immigrant clients, beliefs regarding self-disclosure may be even more convoluted due to factors such as unfamiliarity with mainstream psychotherapy’s emphasis on client self-disclosure, cultural mistrust toward providers, and stigmatizing beliefs related to seeking help for emotional distress (Nickerson et al. 1994). Studies suggest that ethnic minority and immigrant clients are less likely to self-disclose with a Caucasian provider due to fears of discrimination and unfair treatment (Chang and Berk 2009) and more likely to disclose willingly to racially similar providers (Helms and Carter 1991; Thompson et al. 2004). This indicates that an important strength of the provider–client therapeutic relationship, without the understanding of culturally nuanced dimensions, may be diminished in effectiveness with ethnic minority and immigrant clients.
Provider Trust and Confidentiality
Client trust of the provider emerged as a second dimension assessed in existing measures. Client trust is a central component of the therapeutic relationship that is associated with greater client self-exploration, disclosure, and treatment progress (Dunkle and Friedlander 1996; Patterson and Forgatch 1985). Among the 61 measures, 21% (12) identified dimensions of trust that included beliefs associated with the confidentiality and privacy of personal information, as well as beliefs regarding the credibility of the provider.
The literature indicates that provider credibility plays a markedly important role in the development of trust among culturally different clients. Unlike Caucasian clients, ethnic minority and immigrant clients have been found to suspend trust of providers who are ethnically dissimilar from them until they are proven credible and trustworthy (LaFromboise and Dixon 1980). In fact, lack of trust in the provider has been identified as an indicator of poor engagement among ethnic minority clients (Snowden 2003; Terrell and Terrell 1984). Particularly for ethnic minority and immigrant clients who are less accustomed to mainstream psychological concepts and approaches to mental health treatment, entering a therapeutic relationship with an ethnically similar clinician and/or one who fits culturally consonant expectations (e.g., older, male, having professional titles) may inadvertently enhance the client’s level of trust in the clinician’s expertise and skills (Sue 2006). In contrast, when culture is overlooked in the therapeutic process, misunderstandings are likely to arise, stemming from conflicting worldviews, values, and goals, resulting in client discomfort and poor treatment engagement and outcome (Pan et al. 2011). In fact, clients’ level of trust and perceptions of clinician credibility were linked to clinicians’ ability to tailor treatment to clients’ specific contexts and history, and to address minority-specific experiences such as discrimination and acculturation (Chang and Berk 2009).
Client trust regarding confidentiality was identified by 5% (3) of measures. The literature suggests that client–provider confidentiality is a barrier that impedes ethnic minority and immigrant families’ engagement in physical as well as mental health services. For example, Yeh et al. (2003) found that parental concerns about the confidentiality of mental health services were one of the factors that discouraged Latino families from seeking services for their children. Barkley (2000) also notes that among African American youth, confidentiality is a significant concern in relation to a Caucasian therapist. Among the Chinese, concerns surrounding confidentially are especially strong, due to the cultural stigma attached to mental illness (Nash et al. 2006).
Provider Attitudes and Behaviors
Client perceptions of providers have important implications for whether individuals engage in treatment (Furnham and Wardley 1990; Wong 1994). Clients bring to treatment anticipatory beliefs about the provider, treatment, therapeutic process, and outcome that can influence how they experience engagement in mental health treatments (Nock and Kazdin 2005). The literature indicates that clients hold preconceived expectations for the therapeutic relationship, including provider approval, advice, audience, and relationship (Berzins 1977) and that these shape the strength of the alliance.
Anticipatory beliefs related to the therapeutic relationship were identified in 14% (8) of measures and encompassed beliefs about being respected, understood, and not judged by the provider. Studies support the salience of client beliefs about provider–client relationships. For example, Bachelor (1995) found in her qualitative study that roughly half of patients indicated therapist respect as a central element of a positive therapeutic alliance. Bachelor (2013) also found that client ratings of the bond in the therapeutic alliance were derived from perceptions including therapists’ liking of and respect for the client, empathy, and perceived trustworthiness. Studies among youth indicate that perceptions of therapists’ warmth, respect, trust, openness, and guidance are important factors that facilitate developing a strong therapeutic relationship (Martin et al. 2006; Shirk and Karver 2003).
While these dimensions are central across all client–provider relationships, the provider’s ability to be responsive to the client’s culture may be particularly important for establishing alliance cross-culturally. For ethnic minority and immigrant clients, cultural mistrust, which is described as the mistrust of White systems (e.g., educational, political, legal), social contexts (e.g., education, work), and interpersonal relationships with Whites (Terrell and Terrell 1981), may inadvertently affect the therapeutic relationship. In fact, evidence suggests that ethnic minority and immigrant clients’ perceptions of therapist cultural insensitivity adversely impact their level of engagement in treatment and expectations for treatment outcome (Austin et al. 1990; Helms and Cook 1999). Some studies have found that in ethnically dissimilar provider–client dyads, cultural mistrust may be displayed in ethnic minority and immigrant clients’ testing of the provider’s understanding of, and skills in dealing with, racial, ethnic, or cultural issues (Sue and Sue 2003). These findings highlight that the perceptions of clients of color of comfort with and trust of a provider due to a shared culture are likely to play a crucial role in the initial stages of engaging and forming a strong therapeutic alliance.
Collaborative Nature of the Alliance
The final domain, provider–client collaboration, was assessed by 19% (11) of existing measures. Items captured aspects of collaboration such as sharing in decision making, open communication, and joint client involvement in treatment. Provider–client collaboration, described as the ability of the dyad to agree on and engage in therapeutic tasks within the context of a positive relationship, is considered a central element of the therapeutic alliance (Constantino et al. 2002; Horvath and Bedi 2002). In fact, a client’s sense of collaboration and agreement with his/her provider regarding the tasks in treatment is found to be instrumental for successful outcomes (Horvath and Greenberg 1989; Orlinsky et al. 2004).
Evidence suggests that several factors contribute to the establishment of a collaborative alliance. For example, therapeutic alliance has been positively associated with coherent and open communication between the client and therapist (Price and Jones 1998). Similarly, Allen et al. (1996) found that clients found their therapeutic relationship to be more collaborative when the therapist engaged in clarification or interpretation. In a study by Ackerman et al. (2000), clients reported the assessment experience more positively when therapists interacted collaboratively with them to develop treatment goals and engaged in exploring assessment results.
Although the centrality of collaboration in building alliance applies across client classes (Horvath 2001), establishing a collaborative therapeutic relationship can be complex in cross-cultural relationships. Cultural differences in the understanding of mental health and treatment approaches may influence client expectations of the provider–client relationship. For ethnic minority and immigrant clients, in fact, the very notion of receiving therapy may be foreign and dissonant with their culture. For example, Leong and Lau (2001) note that for Asian Americans, the values endorsed in mainstream mental health systems such as open communication and disclosure of personal and emotional information contrast with cultural values of keeping personal problems within the family to avoid family shame (Ho 1984). Ridley (1984) explains that for African Americans, cultural mistrust may stem from perceptions of prior experiences of racism or discrimination, thereby affecting the level of client collaboration. For culturally dissimilar provider–client dyads, the provider’s integration of culturally responsive approaches to establishing a collaborative alliance becomes essential. Evidence supports the salience of cultural responsiveness in engagement: Studies indicate that ethnic minority clients who receive ethnicity-specific or culturally sensitive services are more likely to remain in treatment and achieve higher functioning, compared to those who receive mainstream services (Yeh et al. 1994).
Scholars note that it is critical for providers to develop a shared understanding of the client’s worldview and perspectives regarding his/her presenting problems, which requires learning cultural values, norms, and expectations, to appropriately tailor the relationship to the client’s specific needs (Comas-Díaz 2006; Yasui et al. 2015). Despite this noted need for actively modifying the therapeutic relationship to the client’s culture, limited measures of engagement have attempted to address culturally specific elements of a collaborative therapeutic alliance.
Engagement Behaviors: Past or Present Experiences of Service Encounters
Individuals’ beliefs and attitudes toward mental health treatment develop not only from learned knowledge or socialization of normative beliefs, but also from their treatment engagement behaviors and experiences (Jourard 1964; Seiffge-Krenke and Shulman 1990). Gulliver and colleagues’ literature review summarized that past engagement behaviors and experiences could facilitate or hinder current intentions of help seeking in two ways: (a) by providing direct experiential references for individuals to form and transform their feelings and attitudes toward treatment, and (b) by changing (in most cases, improving) their level of mental health knowledge or literacy about utilizing professional services for mental illness (Gulliver et al. 2010). Evaluations of past engagement thus introduce a temporal-behavioral dimension in explaining individuals’ intentions of help seeking by integrating present beliefs and attitudes into the flow of individuals’ life experiences.
Twenty-three percent (14) of reviewed measures contain items capturing individuals’ engagement in treatment (see Fig. 1; Table 5). Among these, 16% (10) of the measures have items focusing on the clinical interactions between provider and client regarding specific aspects such as information sharing, decision making, feeling of inclusion and respect, and level of mutual trust and respect. As we reviewed, therapeutic relationship is considered a core predictor of treatment outcome, retention, and client satisfaction, and positive experiences of this relationship may serve as a direct affective and cognitive reference for individuals to form and/or change their attitudes toward professional services. Also 20% (12) of reviewed measures contained items that capture individuals’ experiences of what they have been doing or feeling during treatment. Items are often framed as “I am frustrated by the things I am doing in therapy,” “I am finally doing some work on my problem,” or “I established a good understanding of the kind of changes that would be good for me.” Among the measures are a few assessing experiences of seeking other sources of help.
Studies have shown that a favorable therapeutic experience may change not only an individual’s initial negative attitudes toward professional treatment (Jourard 1964), but also his/her beliefs about the nature and causes of illness (Johnston and Freeman 2002). For example, in their study of parents’ beliefs about ADHD, Johnston and Freeman (2002) demonstrated that parents whose children have been involved in professional treatment would be likely to see their children’s symptomatic behaviors as caused by more controllable and less enduring factors. These studies have informed us about the importance of incorporating the temporal-behavioral aspect in measuring individuals’ present attitudes and beliefs about mental health treatment, which in turn calls for more dynamic collaborations between literatures on help-seeking beliefs and those on detailed treatment engagement behaviors. This experiential aspect may be of particular importance when it comes to ethnic minority and immigrant populations regarding their significantly lower knowledge of and exposure to the mainstream mental health paradigm, compared to the Caucasian population. For them, the direct encounter with treatment might cause greater departures from their original explanatory models of illness/healing and thus initiate greater affective, cognitive, and attitudinal reactions.
Our review of the 61 measures on beliefs and experiences of mental health treatment has shown that factors shaping individuals’ intention and action of seeking professional services are manifold and entwined. These different dimensions are also shaped by broader structural and cultural circumstances, such as the mainstream mental health paradigm’s expectations of clients’ engagement, the present distribution of mental health services and other helping resources, the width and depth of mental health knowledge expansion within certain communities, and the indigenous conceptualizations of health and healing among certain groups (see Fig. 1). These complexities indicate that a more structurally and culturally informed perspective, beyond the currently predominant individual-based and mainstream-centered perspective, is needed to remediate the underutilization of mental health services, particularly among ethnic minority and immigrant children and families.
Yet, among the 61 original studies with measures of mental health treatment we reviewed in this section, only 13 were developed using majority ethnic minority, immigrant, or cross-cultural samples. Ethnic minorities’ and immigrants’ unique beliefs and experiences of mental health services are underrepresented and under-discussed. Moreover, the participants’ ethnic and immigrant backgrounds are largely considered as merely demographic variables in most of those studies, rather than fundamental aspects that have shaped their living experiences. Similarly, under the predominant influences of the biopsychosocial paradigm in professional services, other culturally bound beliefs and healing approaches of mental health have been considered at best as supplements, and at worst as barriers to the mainstream treatment models. Although there are rich scholarly discussions (e.g., the explanatory models of illness) reflecting upon the historical formation and philosophical presumptions of the biopsychosocial paradigm and its conceptual and practical limitations, these insights haven’t been well extended to the literature of service utilization, illustrating the necessity of developing more culturally informed and diverse paradigms for the field of mental health.
Discussion and Conclusion
Despite movement toward addressing client culture through widespread calls for cultural responsiveness in mental health (Bernal et al. 1995; U.S. Department of Health and Human Services 2001; Sue 1998), those in the mental health services field continue to grapple with the amorphous concept of culture that they encounter that unconsciously affects client engagement and treatment response. The current paper is an initial attempt to address this “black box” phenomenon of culture by identifying multiple processes involved in recognizing the need for seeking and receiving help among people from different sociocultural backgrounds. Specifically, it reviews existing measures that evaluate the extent to which culture is infused in the process of engagement. The culturally infused engagement model (CIE) emerged from this review and highlights salient multifaceted processes of engagement that intersect with the lived illness experiences of ethnic minority and immigrant children and families. It reflects one advance toward unraveling the complex phenomenon of culturally infused engagement that is a fluid and heterogeneous process shaped by the multi-dimensional cultural influences of ethnic minority and immigrant children and families. While we wholeheartedly recognize that the CIE cannot fully address the cultural plurality of ethnic minority and immigrant children and families, the comprehensive illustration of multi-dimensional engagement processes provides a promising framework that can guide the flexible application of the model to identify client-specific cultural domains pertinent to engagement. It is our hope that the CIE can be used as a framework to facilitate further uncovering of more elaborate cultural dimensions of engagement that will allow clinicians, researchers, and program planners to address cultural specificity in engagement among an increasingly diverse population.
Our review highlights several advancements of empirical assessments of engagement in mental health treatments, as well as areas for future development. Through bridging the literature in problem recognition, help seeking, and treatment engagement, the review reveals the substantial contributions made across the disciplines of medical anthropology, mental health services, social psychology, and clinical psychology. Evident from the large number of measures identified, significant empirical measurements that capture culturally specific processes of engagement are available, to be readily integrated into clinical practice. Further, by illuminating the measures that capture the multi-level, multistage process of engagement, practicing clinicians can identify instruments that may be pertinent to the presenting issues of a particular ethnic minority and immigrant children and families, thereby allowing for the tailoring of assessment and treatment to their specific needs. In this way, the CIE presents a model that can have significant practical applications to be used by clinicians and program planners to develop culturally responsive services and treatments for ethnic minority and immigrant children and families, as well as to guide recommendations for research.
The practical application of the CIE in clinical practice and training is multifold. First, on a broad level, the CIE can be used as a guiding framework to prompt practicing clinicians to consider the complex influences of culture that affect client engagement. Similar to the ADDRESSING framework by Hays (1996) that directs clinicians to attend to salient background factors of clients (e.g., acculturation, ethnicity, sexual orientation, gender), the dimensions identified in the CIE can serve as a reminder for clinicians to address multiple domains of engagement within the context of assessment and intervention. For example, the CIE may cue a clinician to consider the possibility that typical mainstream notions of depression or anxiety may not be congruent with the ethnic minority and immigrant child’s understanding of his or her distress, thereby propelling the clinician to focus on client-defined conceptualizations of distress. Moreover, considerations of multi-level influences may further prompt the clinician to examine not only the child’s but also family members’ and the ethnic community’s understanding or conceptualization of the ethnic minority and immigrant child’s distress. In this way, the CIE can guide areas of inquiry from which directions for assessment and intervention follow. Second, the use of the CIE as an overarching framework can direct clinicians to use our review of 119 existing measures as a practical resource for identifying empirical measures that assess dimensions of engagement relevant to their client. For example, a clinician may learn from her inquiry of the client’s conceptualization of the distress that cultural stigma was a prominent barrier to his or her accepting mental health treatment, and move to further assess the effects of stigma by administering a self-report questionnaire. Third, the CIE can also serve as an instrumental frame for clinician training in cultural competence (a) by illuminating dimensions of engagement that may be less familiar to the clinician, thus prompting further education; (b) by enhancing clinician awareness of personal conceptualizations of distress, mental health problems and disorders, and approaches to healing through self-exploration of CIE dimensions, and (c) by reflecting upon clinician–client differences in conceptualizations of distress and preferred healing approaches to determine particular culturally responsive skills or strategies that will help facilitate a shared understanding of the “problem” or “distress” and plans for treatment/healing.
There also are also practical applications of the CIE model for administrators and program planners to tailor outreach efforts to ethnic minority and immigrant children and families to improve help-seeking efforts and treatment and service utilization. The model underscores the importance of the conceptualization of distress and the meaning of illness. For example, it can provide groundwork for educational public health messages that inform ethnic minority and immigrant children and families about the variety of ways that mental distress may by expressed and experienced, as well as providing culturally specific information to activate caring family networks to facilitate help seeking for family members. Culturally infused messaging in local communities and neighborhoods using the CIE domains and its findings could help to recognize distress, reduce stigma, and identify barriers to increase the likelihood that help may be sought when it might otherwise be avoided. Pediatricians and other primary care providers, who are generally the first (and most often only) medical professionals to see ethnic minority and immigrant children, can also be included in education and outreach programs that focus on culturally infused engagement models, improving engagement of their patients in mental health care. These types of community engagement efforts could potentially improve the overall mental health literacy of large communities of underserved ethnic minority and immigrant children and families.
The CIE model also has implications at the policy level for staffing mental health services and developing a competent workforce. Many, indeed probably most, but certainly not all, ethnic minority and immigrant children are in lower-income families, and there is a lack of mental health providers in many low-income neighborhoods. Developing incentives for mental health providers to operate in low-income neighborhoods through loan forgiveness programs could increase the availability of mental health services. Additionally, investing in community-based and clinical research that theoretically tests culturally infused engagement interventions could develop an instrumental knowledge base for improvements in working with ethnic minority and immigrant children and families.
In addition to these practical advancements, we also propose some recommendations for measurement enhancement. First, as illustrated in the culturally infused engagement model, measures should be developed that specifically assess dimensions of behavioral beliefs, social norms, and control/agency, which may be instrumental in identifying the underlying beliefs of ethnic minority and immigrant children and families that are particularly influential in determining their engagement behaviors. These areas have been underdeveloped and understudied in engagement in helping processes. Research has indicated that among collectivistic cultures, subjective norms are more predictive than behavioral beliefs in regard to individuals’ intentions and behavioral outcomes [e.g., use of contraception in Ethiopia (Fekadu and Kraft 2001); environmentally friendly purchasing behavior in China (Chan and Lau 2001)]. In the same manner, it is likely that for ethnic minority and immigrant families who espouse more collectivistic cultural views, the norms of their cultural group, community, or family will have significant effects on determining the behavioral engagement in mental health services. In fact, growing evidence appears to demonstrate the importance of assessing the beliefs and norms of ethnic minority and immigrant family members and their community. For example, Young and Rabiner (2015) found that Hispanic parents endorsed a higher level of beliefs associated with negative social responses (being worried that the child would be teased or that the child’s mental health problem would reflect poorly on the parents) than did Caucasian or African American parents. Lee et al. (2005) found that 59.6% of the sample indicated that their family members wanted to conceal the individual with mental illness from others, and 41.1% reported family members being treated unfairly due to associations with the mentally ill person. The authors note that for the Chinese, loss of face can significantly affect the family’s linkage to social networks of resource and life chances, highlighting the increased burdens of courtesy stigma that trouble Chinese families having an individual with mental illness.
Additionally, assessing behavioral beliefs, perceived norms, and agency/control beliefs separately may be particularly important for ethnic minority and immigrant children and their parents. The literature indicates that youths adjust to American culture faster than their parents (Portes 1997), creating a difference in orientation toward individualistic (e.g., American) or collectivistic (e.g., Asian) cultures that may facilitate divergent behavioral beliefs or subjective norms and control/agency beliefs regarding mental health and help seeking. For example, an acculturated youth may hold the behavioral belief, “I believe mental health services will help me better cope with my distress,” which contrasts with his parents’ belief that “My family believes it is shameful to go to mental health services,” adversely impacting the youth’s control/agency beliefs: “It will be difficult for me to go to mental health services because it will be shameful for my family.” It will be critical to develop approaches that assess the specific behavioral beliefs, subjective norms, control beliefs, and intentions of not only the ethnic minority and immigrant child but also those of his or her family, as well as those of relevant subsystems such as the ethnic community and church.
Second, more attention should be paid to the significant role of beliefs associated with the conceptualization of the illness or distress. Existing research on the TPB model’s application to engagement behaviors has paid insufficient attention to this area. The culturally infused engagement model addresses this gap by expanding the TPB framework to include belief mechanisms prior to help seeking (i.e., beliefs related to the cause, identity of the illness, and the meaning of the illness to the self). Developing measures that assess specific belief domains within the conceptualization of mental distress will help further clarify the mechanisms linking causal beliefs or illness identification and mental health service use. Further, the development of measurement items across these domains will allow measures to capture the independent as well as combined effects of beliefs in predicting the ethnic minority and immigrant family’s intention and eventual engagement in mental health treatment.
Third, more attention should be paid to culturally specific processes of engagement. Of the 119 measures, only 24 (20%) were designed to assess them. This lack of attention illustrates the inclination within current mental health care to place culture on the periphery of mental disorder or illness rather than infused within the multifaceted processes of engagement, resulting in the widespread utilization of etic measures that assume cross-cultural equivalence in mental health constructs. To systematically examine the underlying factors contributing to racial and ethnic disparities in mental health, assessment approaches that lay hold of the cultural nuances of ethnic minority and immigrant children and families’ pathways of engagement will be crucial. Development of measures that capture culturally specific constructs, experiences, and meanings of mental health and distress will help establish an empirical knowledge base of culturally general (shared across individuals of varying cultural groups) as well as culturally specific (unique to a particular culture) engagement processes. Advancement in this area will help identify culturally driven symptom structures of mental distress and culturally constructed “thresholds” of clinical need and help seeking. For ethnic minority and immigrant children and families who approach mental health services with skepticism and apprehension, every clinical encounter is a critical juncture for engagement; the future development of assessments that accurately speak to their illness experiences and cultural viewpoints is likely to have far-reaching effects in engaging families in mental health treatment.
Fourth, it will be critical for future studies to approach mental health treatment engagement using a multi-agent approach that will allow service providers to identify within the family concordant as well as incongruous beliefs that impact engagement. Only 8% (10) of the measures reviewed are surveys that assess the beliefs and behaviors of those other than the reporting individual (i.e., view of family members, relatives, kin). For many ethnic minority and immigrant families, the decisions regarding a child’s engagement in mental health treatment often involve the input of multiple family members or kin.
Finally, the predominance of survey methods signifies the need for alternative methodological approaches to assessing the engagement process. One measurement strategy that may help to close some of the gaps of traditional survey methods described in our review is the use of analogue, vignette-based techniques which present realistic case situations on which respondents report their beliefs, feelings, attitudes, or judgments. The use of vignettes in the field of mental health has grown in recent years to include both national samples (e.g., Kirk et al. 1999; Pescosolido et al. 2008; Pottick et al. 2003, 2007; Wakefield et al. 1999) and regional and local ones (Chavez et al. 2010; Mukolo and Heflinger 2011).
In contrast to survey methods alone, vignette methodologies have the advantage of experimental control. Compared to other social scientific methods, controlled experimentation has a better chance of uncovering specific mechanisms that lead to disparities in mental health detection and service use, and thus, it can speed up scientific discovery. This is especially critical in relation to problems of ethnic minority youth and their families because children’s development is rapid; mental health problems must be presented quickly to avoid permanent consequences (Pottick and Warner 2002; New Freedom Commission on Mental Health 2003; Breslau et al. 2008).
For the study of processes in the stages of engagement as described in our culturally infused engagement model, a second advantage of vignette methodology is that multiple domains can be investigated simultaneously. Respondents may be asked to react to vignettes from batteries of existing measures, such as the Depression Stigma Scale or the Social Distance Scale, as recently examined in a vignette study by Yap et al. (2014). In that way, the measurement literatures may be valuably integrated. Vignette methodology can also use single-item measures that have face validity, an aspect reflected by some studies of clinicians’ judgments about mental health problems (Hsieh and Kirk 2003; Marsh et al. 2016; Pottick et al. 2007) or about parents’ or laypersons’ recognition of mental health problems and their decisions to seek help (Thurston et al. 2015). Underlying behavioral beliefs, social norms and perceived control or agency of ethnic minority and immigrant families can be investigated systematically in reaction to vignettes that use controlled variations of characteristics that can be hypothesized to influence likely engagement behaviors. In addition, these studies can systematically explore beliefs of respondents of different races or ethnicities to better understand the role of culture in the engagement process. For example, a number of researchers have examined racial differences in beliefs about mental health (e.g., seriousness of illness), help seeking (what help would be appropriate), and treatment effectiveness with vignettes depicting different forms of mental health illnesses, such as major depressive disorder or schizophrenia (Anglin et al. 2008) or conduct disorder (Pottick et al. 2007) or social anxiety disorder (Coles et al. 2016). With comparisons of vignettes representing other mental health illnesses, physical illnesses (Patel and Bakken 2010), marital and family problems (Uomoto and Gorsuch 1984), or no clinically significant diagnosis (Thurston et al. 2015), vignette studies can uncover how individuals of different races or ethnicities view mental health and helping processes. Yap and Jorm (2012) have found that responses to vignettes predicted later mental health service use in congruent ways, suggesting that vignettes may be a useful tool to identify important aspects of service utilization and barriers to it. Similarly, vignettes may be used productively to test aspects of the culturally infused engagement model that posit connections between different beliefs that precede help seeking, such as ideas about the cause of illness or distress, about the illness identity, and about the meaning of the illness to the self. The single existing study that tested the TPB with a vignette approach examined multiple factors associated with welfare workers’ decisions about whether to place a child in residential care or to keep the child with the family (Rodrigues et al. 2015). The results of that study were able to unmask factors that may bias decisions about parental neglect. Using traditional quantitative methods of structural equation modeling, the study demonstrated that multiple domains of the TPB could be tested empirically with a vignette stimulus. A test of the multiple domains of the TPB-based culturally infused engagement model would enrich scientific understanding of engagement processes for minority families.
Another shortcoming of current research that we identified in our review can be mitigated by vignette methods, which can help to detect how different members of families perceive treatment engagement processes. A number of studies have compared the perspectives of clinicians and laypersons to the same vignette (Marsh et al. 2016), but to our knowledge, there are none that investigate the views of multiple members of the family. Identifying the varying perspectives on recognizing the problem, seeking help, and participating and engaging in treatment itself will be especially important in understanding ethnic minority families’ beliefs about whether or how they will engage in help. Our review has demonstrated that insufficient attention to the infusion of culture in processes of engagement has limited our understanding of disparities. There are opportunities to accelerate knowledge development for minority and immigrant families and their children.
Finally, in addition to the perspectives of different family members, vignette studies can systematically investigate the beliefs, attitudes, and judgments of key gatekeepers, such as teachers, police, doctors, nurses, social workers, psychologists, or psychiatrists, in the engagement process. Several vignette studies have begun such investigations. For example, Pottick et al. (2007) found differences among psychologists, psychiatrists, and social workers in their judgment of the existence of mental disorder in a vignette youth with symptoms of conduct disorder. In another report from the same data set, Kirk and Hsieh (2004) showed that social workers, in relation to psychologists and psychiatrists, were less likely to make a diagnosis of conduct disorder, were more likely to use other DSM-IV diagnoses (especially adjustment disorders), and were more likely to report no diagnosis. Exploring the role of differential socialization processes among gatekeepers in the domains identified in our review may shed light on implicit biases that could negatively affect engagement at any stage of problem recognition, help seeking or treatment participation—especially for ethnic minorities. Moreover, we have argued that parents are gatekeepers for their children, but they also can be gatekeepers for other children in their neighborhoods. Basic processes of race relations may be uncovered by examining parents’ conceptualization of illness or attitudes about healing among children of races or ethnicities different from their own. The culturally infused engagement model can provide guidance for scientific investigations at the macro-community level that may affect disparities in engagement because it can investigate multiple domains across different community members.
Such analogue methods as the vignette model, as potentially valuable as they can be, are only proxies for what actually occurs in clinical practice situations, though they do provide powerful ways of discovering relationships that may not otherwise be readily detectable. Brief case vignettes obviously cannot reproduce the complex reality of a clinical case, with personal interviews that add greatly to the information available in clinical files. Moreover, complicating interpretation of results, the methods are subject to many correlated factors that may be incorporated unwittingly into the vignettes. It is difficult for a case vignette to capture the ambiguities, contradictory evidence, and multiplicities of causal pathways that often are present in a real case record. However, for practice research, experimentally controlled vignette methods are promising, as they can discern mechanisms of clinical decision making relatively efficiently to improve practice in a timely way (Converse et al. 2015). Moreover, future studies can capitalize on the measures reviewed here and potentially integrate the measurement literatures, to produce practical and theoretically relevant responses to disparities in engagement.
Although the CIE’s central focus is on engagement, the model may be instrumental in informing intervention development. The conceptual frameworks of culturally adapted interventions by Castro et al. (2010) and Lau (2006) highlight the imperative role of engagement in intervention effectiveness and call for a dual approach for adaptations that target both barriers to engagement and client outcomes. Yet, empirical literature that specifically addresses cultural considerations targeting engagement is still limited. In light of this, the comprehensive identification of central processes of engagement in the CIE may serve as a guide for future interventions by (a) helping to target work on specific domains to develop strategies or brief interventions to enhance engagement among particular cultural groups and (b) facilitating cultural adaptations of existing engagement practices or interventions. For example, although psychoeducation about services is recognized as one of the most frequent and successful practices utilized by clinicians to enhance engagement (Becker et al. 2015), an initial discussion about psychotherapeutic services may be antithetical to the ethnic minority and immigrant family’s conceptualization of their child’s distress as not mental health related, but rather physical. Conceptualizations stemming from particular causal beliefs about such issues as imbalance in the body and poor energy flow might shape ethnic minority and immigrant families’ preferred healing approach toward, for instance, traditional Chinese medicine, while attempts to engage in a conversation about “mental health” would likely invalidate families’ concerns and result in treatment dropout.
In addition, the CIE provides a frame for developing interventions that integrate real-world complexities of multifaceted cultural and contextual influences on the engagement process. Because the saliency of a particular domain or domains of the CIE on client engagement is determined by the unique ecological context and clinical needs of each specific child and family (Yasui and Dishion 2007; Yasui and Henry 2014), engagement approaches for one family may significantly vary from another. The comprehensiveness of the CIE allows for such variability: Engagement interventions can be selected and tailored depending on the identified CIE domains. Thus, the CIE lends itself to the development of flexible engagement approaches by which clinicians can draw from a menu of options, thereby dovetailing the engagement process in treatment to the individualized needs of the ethnic minority and immigrant child and family. Such an approach to intervention, in which a menu of intervention options is provided to clients, is found to be particularly effective in child and family interventions (e.g., Webster-Stratton 1984; Dishion and Stormshak 2007), which suggests promising directions in utilizing the CIE to develop a menu of engagement interventions that are domain specific.
Finally, although enhancing the engagement of ethnic minority and immigrant children and families in mental health services continues to be a critical public health endeavor, in the case of many, given their cultural beliefs, norms, and practices, professional mental health services may not even be a plausible option for healing. This points to the need to pursue alternate avenues in addressing ethnic and racial disparities in mental health, in particular, avenues that allow for the integration of mental health interventions into the everyday life of ethnic minority and immigrant children and families. For example, one promising approach employs community-based participatory methods in which the communities themselves are active, equal partners in designing interventions that are culturally congruent and acceptable (Stacciarini et al. 2011). As researchers and practitioners partner with local ethnic and immigrant communities, the CIE can serve as a guiding framework for developing culturally and community-driven approaches to bringing mental health interventions to the doorsteps of ethnic minority and immigrant families. By considering the multifaceted cultural and contextual influences depicted in the CIE, ethnic and immigrant communities and partnering researchers, clinicians, and policymakers may identify central mechanisms of engagement to target and begin to address mental health disparities from the bottom-up.
In conclusion, our paper reflects the substantial contributions of existing empirical measures that capture dimensions of culturally infused engagement in mental health as well as the need for future methodological advances that can propel theoretical and empirical approaches to addressing culturally specific engagement processes that impact racial and ethnic disparities in mental health. The significant breadth of the empirical measures that capture the specific dimensions of culturally infused engagement is a promising foundation for the future development of culturally responsive assessments and interventions. However, the review also highlights the urgency for a paradigm shift in the conceptualization of engagement in mental health treatment—from current operationalizations that limit engagement to the process of treatment involvement/participation, to a broader conceptualization of engagement as a culturally infused process that begins from problem recognition and runs through participation in treatment services. It is our hope that this review of existing empirical measures that is anchored in the culturally infused engagement model will serve as a roadmap to galvanize researchers, clinicians, and program developers at the forefront of addressing racial and ethnic disparities in mental health to move beyond the biomedical framework of diagnosis and treatment to assessments and treatments that embrace the infused nature of culture in the engagement and treatment of ethnic minority and immigrant children and families.
References
Abe-Kim, J., Gong, F., & Takeuchi, D. (2004). Religiosity, spirituality, and help-seeking among Filipino Americans: Religious clergy or mental health professionals? Journal of Community Psychology, 32(6), 675–689.
Abera, M., Robbins, J. M., & Tesfaye, M. (2015). Parents’ perceptions of child and adolescent mental health problems and their choice of treatment option in southwest Ethiopia. Child and Adolescent Psychiatry and Mental Health, 9, 40. doi:10.1186/s13034-015-0072-5.
Ackerman, S. J., Hilsenroth, M. J., Baity, M. R., & Blagys, M. D. (2000). Interaction of therapeutic process and alliance during psychological assessment. Journal of Personality Assessment, 75(1), 82–109.
Aday, L. A., Fleming, G. V., & Andersen, R. (1984). Access to medical care in the US: Who has it, who doesn’t. Chicago, IL: Pluribus Press, Inc. and Center for Health Administration Studies.
Addis, M. E., Wade, W. A., & Hatgis, C. (1999). Barriers to dissemination of evidence-based practices: Addressing practitioners’ concerns about manual-based psychotherapies. Clinical Psychology: Science and Practice, 6, 430–441.
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211.
Alcázar-Olán, R. J., Deffenbacher, J. L., & Escamilla-Tecalco, H. (2016). Developing a valid version of an inventory to measure anger in Mexican adolescents of middle school level: The ML-STAXI-MS. Youth & Society, 48(1), 126–143.
Alegría, M., Pescosolido, B. A., Williams, S., & Canino, G. (2011). Culture, race/ethnicity and disparities: Fleshing out the socio-cultural framework for health services disparities. In Handbook of the sociology of health, illness, and healing (pp. 363–382). New York: Springer.
Allen, J. G., Coyne, L., Colson, D. B., Horowitz, L., Gabbard, G. O., Frieswick, S. H., et al. (1996). Pattern of therapist interventions associated with patient collaboration. Psychotherapy, 33(2), 254–261.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5 ® ). Arlington: American Psychiatric Publishing.
Angermeyer, M. C., Beck, M., & Matschinger, H. (2003). Determinants of the public’s preference for social distance from people with schizophrenia. Canadian Journal of Psychiatry, 48, 663–668.
Angermeyer, M. C., & Dietrich, S. (2006). Public beliefs about and attitudes towards people with mental illness: A review of population studies. Acta Psychiatrica Scandinavica, 113(3), 163–179.
Angermeyer, A. A., & Klusmann, D. (1988). The causes of functional psychoses as seen by patients and their relatives. European Archives of Psychiatry and Neurological Sciences, 238, 47–54.
Angermeyer, M. C., & Matschinger, H. (1996). Relatives’ beliefs about the causes of schizophrenia. Acta Psychiatrica Scandinavica, 93, 199–204.
Angermeyer, M. C., Matschinger, H., & Corrigan, P. W. (2004). Familiarity with mental illness and social distance from people with schizophrenia and major depression: Testing a model using data from a representative population survey. Schizophrenia Research, 69(2), 175–182.
Anglin, D., Alberti, P., Link, B., & Phelan, J. (2008). Racial differences in beliefs about the effectiveness and necessity of mental health treatment. American Journal of Community Psychology, 42(1–2), 17–24.
Angold, A., Messer, S., Stangl, D., Farmer, E., Costello, E., & Burns, B. (1998). Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health, 88(1), 75–80.
Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology, 40(4), 471–499.
Arvaniti, A., Samakouri, M., Kalamara, E., Bochtsou, V., Bikos, C., & Livaditis, M. (2009). Health service staff’s attitudes towards patients with mental illness. Social Psychiatry and Psychiatric Epidemiology, 44(8), 658–665.
Austin, N. L., Carter, R. T., & Vaux, A. (1990). The role of racial identity in Black students’ attitudes toward counseling and counseling centers. Journal of College Student Development, 31, 237–244.
Austin, J. K., & Huberty, T. J. (1993). Development of the child attitude toward illness scale. Journal of Pediatric Psychology, 18(4), 467–480.
Bachelor, A. (1995). Clients’ perception of the therapeutic alliance: A qualitative analysis. Journal of Counseling Psychology, 42(3), 323–337.
Bachelor, A. (2013). Clients’ and therapists’ views of the therapeutic alliance: Similarities, differences and relationship to therapy outcome. Clinical Psychology & Psychotherapy, 20(2), 118–135.
Barke, A., Nyarko, S., & Klecha, D. (2011). The stigma of mental illness in Southern Ghana: Attitudes of the urban population and patients’ views. Social Psychiatry and Psychiatric Epidemiology, 46(11), 1191–1202.
Barker, C., Pistrang, N., & Shapiro, D. A. (1983). Opinions about psychological problems. Unpublished manuscript, Bloomsbury and Islington District Psychology Department.
Barkley, L. C. (2000). Make an impact before that teen leaves your office. Minority Health Today, 1(4), 25–30.
Barrera, M., Jr., & Castro, F. G. (2006). A heuristic framework for the cultural adaptation of interventions. Clinical Psychology: Science and Practice, 13(4), 311–316.
Barrowclough, C., & Hooley, J. M. (2003). Attributions and expressed emotion: A review. Clinical Psychology Review, 23(6), 849–880.
Batterham, P. J., Calear, A. L., & Christensen, H. (2013). The Stigma of Suicide Scale: Psychometric properties and correlates of the stigma of suicide. Crisis, 34(1), 13–21.
Bayer, J. K., & Peay, M. Y. (1997). Predicting intentions to seek help from professional mental health services. Australian and New Zealand Journal of Psychiatry, 31, 504–513.
Becker, K. D., Lee, B. R., Daleiden, E. L., Lindsey, M., Brandt, N. E., & Chorpita, B. F. (2015). The common elements of engagement in children’s mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology, 44(1), 30–43.
Bernal, G., Bonilla, J., & Bellido, C. (1995). Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology, 23(1), 67–82.
Bernal, G. E., & Domenech-Rodríguez, M. M. (2012). Cultural adaptations: Tools for evidence-based practice with diverse populations. Arlington: American Psychological Association.
Berzins, J. I. (1977). Therapist-patient matching. In A. S. Gurman & A. M. Razin (Eds.), Effective psychotherapy: A handbook of research (pp. 222–251). New York: Pergamon Press.
Betancourt, J. R. (2004). Cultural competence—marginal or mainstream movement? New England Journal of Medicine, 351(10), 953–955.
Betancourt, H., & López, S. R. (1993). The study of culture, ethnicity, and race in American psychology. American Psychologist, 48(6), 629.
Bird, H., Shaffer, D., Fisher, P., Gould, M., Staghezza, B., Chen, J., et al. (1993). The Columbia Impairment Scale (CIS): Pilot findings on a measure of global impairment for children and adolescents. International Journal of Methods in Psychiatric Research, 3(3), 167–176.
Bolton, P., Wilks, C., & Ndogoni, L. (2004). Assessment of depression prevalence in rural Uganda using symptom and function criteria. Social Psychiatry and Psychiatric Epidemiology, 39(6), 442–447.
Bonner, B. L. (1984). Influence of Client Preparation and Problem Severity on Attitudes and Expectations in Child Psychotherapy (unpublished doctoral dissertation). Stillwater, Oklahoma: Oklahoma State University.
Bordin, E. S. (1994). Theory and research on the therapeutic working alliance: New directions. The working alliance: Theory, research, and practice, pp. 13–37.
Boyd Ritsher, J. E. (2003). Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research, 121(1), 31–49.
Breda, C. S., & Riemer, M. (2012). Motivation for Youth’s Treatment Scale (MYTS): A new tool for measuring motivation among youths and their caregivers. Administration and Policy in Mental Health and Mental Health Services Research, 39(1–2), 118–132.
Breslau, J., Lane, M., Sampson, N., & Kessler, R. (2008). Mental disorders and subsequent educational attainment in a US national sample. Journal of Psychiatric Research, 42(9), 708–716.
Britt, T. W., Greene-Shortridge, T. M., Brink, S., Nguyen, Q. B., & Rath, J. (2008). Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. Journal of Social and Clinical Psychology, 27(4), 317–335.
Brohan, E., Clement, S., Rose, D., Sartorius, N., Slade, M., & Thornicroft, G. (2013). Development and psychometric evaluation of the Discrimination and Stigma Scale (DISC). Psychiatry Research, 208(1), 33–40.
Brown, C., Conner, K. O., Copeland, V. C., Grote, N., Beach, S., Battista, D., et al. (2010). Depression stigma, race, and treatment seeking behavior and attitudes. Journal of Community Psychology, 38(3), 350–368.
Bulanda, J. J., Bruhn, C., Byro-Johnson, T., & Zentmyer, T. (2014). Addressing mental health stigma among young adolescents: evaluation of a youth-led approach. Health and Social Work, 39(2), 73–80.
Burns, J. R., & Rapee, R. M. (2006). Adolescent mental health literacy: Young people’s knowledge of depression and help seeking. Journal of Adolescence, 29(2), 225–239.
Bussing, R., Gary, F. A., Mills, T. L., & Garvan, C. W. (2003). Parental explanatory models of ADHD. Social Psychiatry and Psychiatric Epidemiology, 38(10), 563–575.
Bussing, R., Koro-Ljungberg, M., Mason, D., Mayerson, G., Noguchi, K., & Garvan, C. W. (2012). Willingness to use ADHD treatments: A mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Social Science and Medicine, 74(1), 92–100.
Carrillo, J. E., Green, A. R., & Betancourt, J. R. (1999). Cross-cultural primary care: A patient-based approach. Annals of Internal Medicine, 130(10), 829–834.
Castro, F. G., Barrera, M., & Steiker, L. K. H. (2010). Issues and challenges in the design of cultural adapted evidence-based interventions. Annual Review Clinical Psychology, 6, 213–239.
Cauce, A. M., Domenech-Rodríguez, M., Paradise, M., Cochran, B. N., Shea, J. M., Srebnik, D., et al. (2002). Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology, 70(1), 44–55.
Chan, Y., Leung, D., Fong, D., Leung, C., & Lee, A. (2010). Psychometric valuation of the Hospital Anxiety and Depression Scale in a large community sample of adolescents in Hong Kong. Quality of Life Research, 19(6), 865–873.
Chan, R. Y. K., & Lau, L. B. Y. (2001). Explaining green purchasing behavior: A cross-cultural study on American and Chinese consumers. Journal of International Consumer Marketing, 14, 9–40.
Chang, D. F., & Berk, A. (2009). Making cross-racial therapy work: A phenomenological study of clients’ experiences of cross-racial therapy. Journal of Counseling Psychology, 56(4), 521.
Chavez, L., Shrout, P., Alegría, M., Lapatin, S., & Canino, G. (2010). Ethnic differences in perceived impairment and need for care. Journal of Abnormal Child Psychology, 38(8), 1165–1177.
Cheung, F. M., Lee, S., & Chan, Y. (1983). Variations in problem conceptualizations and intended solutions among Hong Kong students. Culture, Medicine and Psychiatry, 7(3), 263–278.
Chhim, S. (2012). Baksbat (broken courage): The development and validation of the inventory to measure baksbat, a Cambodian trauma-based cultural syndrome of distress. Culture, Medicine and Psychiatry, 36(4), 640–659.
Choi, K. H. (2002). Psychological separation-individuation and adjustment to college among Korean American students: The roles of collectivism and individualism. Journal of Counseling Psychology, 49(4), 468–475.
Chorpita, B. F., Yim, L. M., Donkervoet, J. C., Arensdorf, A., Amundsen, M. J., McGee, C., et al. (2002). Toward large-scale implementation of empirically supported treatments for children: A review and observations by the Hawaii Empirical Basis to Services Task Force. Clinical Psychology: Science and Practice, 9(2), 165–190.
Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S., Bezborodovs, N., et al. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45(1), 11–27.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46.
Cohen, B. Z. (1999). Measuring the willingness to seek help. Journal of Social Service Research, 26(1), 67–82.
Cohen, D., Yoon, D. P., & Johnstone, B. (2009). Differentiating the impact of spiritual experiences, religious practices, and congregational support on the mental health of individuals with heterogenous medical disorders. International Journal for the Psychology of Religion, 19(2), 121–128.
Cohen, J., & Struening, E. L. (1962). Opinions about mental illness in the personnel of two large mental hospitals. Journal of Abnormal and Social Psychology, 64(5), 349–360.
Coleman, D., Walker, J. S., Lee, J., Friesen, B. J., & Squire, P. N. (2009). Children’s beliefs about causes of childhood depression and ADHD: A study of stigmatization. Psychiatric Services, 60(7), 950–957.
Coles, M., Ravid, A., Gibb, B., George-Denn, D., Bronstein, L., & McLeod, S. (2016). Adolescent mental health literacy: Young people’s knowledge of depression and social anxiety disorder. Journal of Adolescent Health, 58(1), 57–62.
Collins, N. L., & Miller, L. C. (1994). Self-disclosure and liking: a meta-analytic review. Psychological Bulletin, 116(3), 457.
Comas-Díaz, L. (2006). Cultural variation in the therapeutic relationship. In C. D. Goodheart, A. E. Kazdin, & R. J. Sternberg (Eds.), Evidence-based psychotherapy: Where practice and research meet (pp. 81–105). Washington, DC: American Psychological Association.
Conger, R. D., Wallace, L. E., Sun, Y., Simons, R. L., McLoyd, V. C., & Brody, G. H. (2002). Economic pressure in African American families: a replication and extension of the family stress model. Developmental Psychology, 38(2), 179–193.
Constantino, M. J., Castonguay, L. G., & Schut, A. J. (2002). The working alliance: A flagship for the “scientist-practitioner” model in psychotherapy. In G. S. Tryon (Ed.), Counseling based on process research: Applying what we know (pp. 81–131). Boston: Allyn & Bacon.
Converse, L., Barrett, K., Rich, E., & Reschovsky, J. (2015). Methods of observing variations in physicians’ decisions: The opportunities of clinical vignettes. Journal of General Internal Medicine, 30(3), 586–594.
Cooper, L. A., Brown, C., Vu, H. T., Palenchar, D. R., Gonzales, J. J., Ford, D. E., et al. (2000). Primary care patients’ opinions regarding the importance of various aspects of care for depression. General Hospital Psychiatry, 22(3), 163–173.
Corrigan, P. W. (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614–625.
Corrigan, P. W. (2005). On the stigma of mental illness: Practical strategies for research and social change. Washington, DC: American Psychological Association.
Corrigan, P. W., Edwards, A., Green, A., Diwan, S. L., & Penn, D. L. (2001). Prejudice, social distance, and familiarity with mental illness. Schizophrenia Bulletin, 27(2), 219–226.
Corrigan, P. W., Gause, M., Michaels, P. J., Buchholz, B. A., & Larson, J. E. (2015). The California Assessment of Stigma Change: A short battery to measure improvements in the public stigma of mental illness. Community Mental Health, 51(6), 635–640.
Corrigan, P. W., Larson, J. E., & Ruesch, N. (2009). Self-stigma and the “why try” effect: Impact on life goals and evidence-based practices. World Psychiatry, 8(2), 75–81.
Corrigan, P. W., & Miller, F. E. (2004). Shame, blame, and contamination: A review of the impact of mental illness stigma on family members. Journal of Mental Health, 13(6), 537–548.
Corrigan, P. W., & Penn, D. L. (1999). Lessons from social psychology on discrediting psychiatric stigma. American Psychologist, 54(9), 765–766.
Corrigan, P. W., Rowan, D., Green, A., Lundin, R., River, P., Uphoff-Wasowski, K., et al. (2002). Challenging two mental illness stigmas: Personal responsibility and dangerousness. Schizophrenia Bulletin, 28(2), 293–309.
Corrigan, P. W., & Watson, A. C. (2002). The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice, 9(1), 35–53.
Corrigan, P. W., & Watson, A. C. (2007). The stigma of psychiatric disorders and the gender, ethnicity, and education of the perceiver. Community Mental Health Journal, 43(5), 439–458.
Cozby, P. C. (1973). Self-disclosure: A literature review. Psychological Bulletin, 79(2), 73.
Crisp, A. H., Gelder, M. G., Rix, S., Meltzer, H. I., & Rowlands, O. J. (2000). Stigmatisation of people with mental illness. The British Journal of Psychiatry, 177(1), 4–7.
D’Avanzo, C. E., & Barab, S. A. (1998). Depression and anxiety among Cambodian refugee women in France and the United States. Mental Health Nursing, 19(6), 541–556.
Davidson, K. H., & Fristad, M. A. (2006). The Treatment Beliefs Questionnaire (TBQ): An instrument to assess beliefs about children’s mood disorders and concomitant treatment needs. Psychological Services, 3(1), 1–15.
de Crane, R. S., & Spielberger, C. D. (1981). Attitudes of Hispanic, Black, and Caucasian university students toward mental illness. Hispanic Journal of Behavioral Sciences, 3(3), 241–253.
De Leon, G., Melnick, G., Kressel, D., & Jainchill, N. (1994). Circumstances, motivation, readiness, and suitability (The CMRS Scales): Predicting retention in therapeutic community treatment. American Journal of Drug and Alcohol Abuse, 2(4), 495–515.
Dempster, R., Davis, D. W., Jones, V. F., Keating, A., & Wildman, B. (2015). The role of stigma in parental help—Seeking for perceived child behavior problems in urban, low-income African American parents. Journal of Clinical Psychology in Medical Settings, 22(4), 265–278.
Derr, A. S. (2016). Mental health service use among immigrants in the United States: A systematic review. Psychiatric Services, 67(3), 265–274.
Dietrich, S., Beck, M., Bujantugs, B., Kenzine, D., Matschinger, H., & Angermeyer, M. C. (2004). The relationship between public causal beliefs and social distance toward mentally ill people. Australian and New Zealand Journal of Psychiatry, 38(5), 348–354.
Dinh, K. T., Weinstein, T. L., Kim, S. Y., & Ho, I. K. (2008). Acculturative and psychological predictors of academic-related outcomes among Cambodian American high school students. Journal of Southeast Asian American Education & Advancement, 3, 1–25.
Dishion, T. J., & Stormshak, E. A. (2007). Intervening in children’s lives: An ecological, family-centered approach to mental health care. Washington, DC: American Psychological Association.
Downs, M. F., & Eisenberg, D. (2012). Help seeking and treatment use among suicidal college students. Journal of American College Health, 60(2), 104–114.
Dumas, J. E., Nissley-Tsiopinis, J., & Moreland, A. D. (2007). From intent to enrollment, attendance, and participation in preventive parenting groups. Journal of Child and Family Studies, 16(1), 1–26.
Dunkle, J. H., & Friedlander, M. L. (1996). Contribution of therapist experience and personal characteristics to the working alliance. Journal of Counseling Psychology, 43(4), 456.
Edwardraj, S., Mumtaj, K., Prasad, J. H., Kuruvilla, A., & Jacob, K. S. (2010). Perceptions about intellectual disability: A qualitative study from Vellore, South India. Journal of Intellectual Disability Research, 54(8), 736–748.
Eisenbruch, M. (1990). Classification of natural and supernatural causes of mental distress: Development of a Mental Distress Explanatory Model Questionnaire. The Journal of Nervous and Mental Disease, 178(11), 712–719.
Eisenbruch, M. (1991). From post-traumatic stress disorder to cultural bereavement: Diagnosis of Southeast Asian refugees. Social Science and Medicine, 33(6), 673–680.
Fan, C. (1999). A comparison of attitudes towards mental illness and knowledge of mental health services between Australian and Asian students. Community Mental Health Journal, 35(1), 47–56.
Farber, B. A., Berano, K. C., & Capobianco, J. A. (2004). Clients’ perceptions of the process and consequences of self-disclosure in psychotherapy. Journal of Counseling Psychology, 51(3), 340.
Farber, B. A., & Hall, D. (2002). Disclosure to therapists: What is and is not discussed in psychotherapy. Journal of Clinical Psychology, 58(4), 359–370.
Farina, A. (2000). The few gains and many losses for those stigmatized by psychiatric disorders. In J. H. Harvey & E. D. Miller (Eds.), Loss and Trauma: General and close relationship perspectives (pp. 183–204). Philadelphia, PA: Brunner-Routledge.
Fekadu, Z., & Kraft, P. (2001). Self-identity in planned behavior perspective: Past behavior and its moderating effects on self-identity-intention relations. Social Behavior and Personality: An International Journal, 29(7), 671–685.
Feldman, D. B., & Crandall, C. S. (2007). Dimensions of mental illness stigma: What about mental illness causes social rejection? Journal of Social and Clinical Psychology, 26(2), 137–154.
Feng, Y., Wu, Z., Zhou, X., Zhou, Z., & Fan, W. (2006). Knowledge discovery in traditional Chinese medicine: State of the art and perspectives. Artificial Intelligence in Medicine, 38(3), 219–236.
Fischer, E. H., & Turner, J. I. (1970). Orientations to seeking professional help: Development and research utility of an attitude scale. Journal of Consulting and Clinical Psychology, 35(1, pt. 1), 79–90.
Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach. New York: Psychology Press.
Fisher, J. D., Nadler, A., & Whitcher-Alagna, S. (1982). Recipient reactions to aid. Psychological Bulletin, 91(1), 27–54.
Fox, C. K., Eisenberg, M. E., McMorris, B. J., Pettingell, S. L., & Borowsky, I. W. (2013). Survey of Minnesota parent attitudes regarding school-based depression and suicide screening and education. Maternal Child and Health Journal, 17(3), 456–462.
Fung, K., & Wong, Y. L. R. (2007). Factors influencing attitudes towards seeking professional help among East and Southeast Asian immigrant and refugee women. International Journal of Social Psychiatry, 53(3), 216–231.
Furnham, A., & Wardley, Z. (1990). Lay theories of psychotherapy: Attitudes towards and beliefs about psychotherapy and therapists. Journal of Clinical Psychology, 46, 878–890.
Gabbidon, J., Brohan, E., Clement, S., Henderson, R. C., Thornicroft, G., & MIRIAD Study Group. (2013). The development and validation of the Questionnaire on Anticipated Discrimination (QUAD). BMC Psychiatry. doi:10.1186/1471-244X-13-297.
Garratt, A. M., Bjertnaes, O. A., Holmboe, O., & Hanssen-Bauer, K. (2011). Parent experiences questionnaire for outpatient child and adolescent mental health services (PEQ-CAMHS Outpatients): reliability and validity following a national survey. Child and Adolescent Psychiatry and Mental Health. doi:10.1186/1753-2000-5-18.
Garvey, C., Julion, W., Fogg, L., Kratovil, A., & Gross, D. (2006). Measuring participation in a prevention trial with parents of young children. Research in Nursing & Health, 29(3), 212–222.
Gaylord-Harden, N. K., & Cunningham, J. A. (2009). The impact of racial discrimination and coping strategies on internalizing symptoms in African American youth. Journal of Youth and Adolescence, 38(4), 532–543.
Gerdes, A. C., & Hoza, B. (2006). Maternal attributions, affect, and parenting in attention deficit hyperactivity disorder and comparison families. Journal of Clinical Child and Adolescent Psychology, 35(3), 346–355.
Gil, A. G., Wagner, E. F., & Vega, W. A. (2000). Acculturation, familism, and alcohol use among Latino adolescent males: Longitudinal relations. Journal of Community Psychology, 28(4), 443–458.
Gilens, M. (1999). Why Americans hate welfare: Race, media, and the politics of antipoverty policy. Chicago: University of Chicago Press.
Gitlin, L. N., Chernett, N. L., Dennis, M. P., & Hauck, W. W. (2012). Identification of and beliefs about depressive symptoms and preferred treatment approaches among community-living older African Americans. American Journal of Geriatric Psychiatry, 20(11), 973–984.
Givens, J. L., Katz, I. R., Bellamy, S., & Holmes, W. C. (2007). Stigma and the acceptability of depression treatments among African Americans and whites. Society of General Internal Medicine, 22(9), 1292–1297.
Goffman, E. (1963). Behavior in public place. New York: Glencoe.
Golberstein, E., Eisenberg, D., & Gollust, S. E. (2008). Perceived stigma and mental health care seeking. Psychiatric Services, 59(4), 392–399.
Gopalan, G., Goldstein, L., Klingenstein, K., Sicher, C., Blake, C., & McKay, M. M. (2010). Engaging families into child mental health treatment: Updates and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 19(3), 182–196.
Green, G., Bradby, H., Chan, A., & Lee, M. (2006). “We are not completely Westernized”: Dual medical systems and pathways to health care among Chinese migrant women in England. Social Science and Medicine, 62(6), 1498–1509.
Greenberg, J. S., Kim, H. W., & Greenley, J. R. (1997). Factors associated with subjective burden in siblings of adults with severe mental illness. American Journal of Orthopsychiatry, 67(2), 231–241.
Griffiths, K. M., Batterham, P. J., Barney, L., & Parsons, A. (2011). The generalised anxiety stigma scale (GASS): Psychometric properties in a community sample. BMC Psychiatry. doi:10.1186/1471-244X-11-184.
Griffiths, K. M., Christensen, H., & Jorm, A. F. (2008). Predictors of depression stigma. BMC Psychiatry. doi:10.1186/1471-244X-8-25.
Groleau, D., Young, A., & Kirmayer, L. J. (2006). The McGill Illness Narrative Interview (MINI): An interview schedule to elicit meanings and modes of reasoning related to illness experience. Transcultural Psychiatry, 43(4), 671–691.
Grover, S., Aneja, J., Sharma, A., Malhotra, R., Varma, S., Basu, D., et al. (2014). Explanatory models of somatoform disorder patients attending a psychiatry outpatient clinic: A study from North India. International Journal of Social Psychiatry, 60(5), 492–498.
Gulliver, A., Griffiths, K., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help seeking in young people: A systematic review. BMC Psychiatry Open Access. doi:10.1186/1471-244X-10-113.
Guzder, J., Yohannes, S., & Zelkowitz, P. (2013). Help seeking of immigrant and native born parents: A qualitative study from a Montreal child day hospital. Journal of Canadian Academy of Child and Adolescent Psychiatry, 22(4), 275–281.
Hacking, I. (2007). Making up people. In M. Lock & J. Farquhar (Eds.), Beyond the body proper: Reading the anthropology of material life (pp. 150–163). Durham, NC: Duke University Press.
Haidet, P., O’Malley, K. J., Sharf, B. F., Gladney, A. P., Greisinger, A. J., & Street, R. L., Jr. (2008). Characterizing explanatory models of illness in healthcare: Development and validation of the CONNECT instrument. Patient Education and Counseling, 73(2), 232–239.
Hartog, K., & Gow, K. M. (2005). Religious attributions pertaining to the causes and cures of mental illness. Mental Health, Religion & Culture, 8(4), 263–276.
Harwood, A. (1981). Ethnicity and medical care. Cambridge: Harvard University Press.
Hays, P. A. (1996). Addressing the complexities of culture and gender in counseling. Journal of Counseling and Development, 74(4), 332–338.
Heather, N., & Rollnick, S. (1993). Readiness to change questionnaire: User’s manual (revised version). National Drug and Alcohol Research Centre, Technical Report No. 19. https://ndarc.med.unsw.edu.au/sites/default/files/ndarc/resources/TR.019.pdf
Helms, J. E., & Carter, R. T. (1991). Relationships of White and Black racial identity attitudes and demographic similarity to counselor preferences. Journal of Counseling Psychology, 38(4), 446–457.
Helms, J. E., & Cook, D. A. (1999). Using race and culture in counseling and psychotherapy: Theory and process. London: Pearson Education.
Hill, D. J., & Bale, R. M. (1980). Development of the mental health locus of control and mental health locus of origin scales. Journal of Personality Assessment, 44(2), 148–156.
Hinkelman, L., & Granello, D. H. (2003). Biological sex, adherence to traditional gender roles, and attitudes toward persons with mental illness: An exploratory investigation. Journal of Mental Health Counseling, 25(4), 259–270.
Hinshaw, S. P. (2005). The stigmatization of mental illness in children and parents: Developmental issues, family concerns, and research needs. Journal of Child Psychology and Psychiatry, 46(7), 714–734.
Hinton, D. E., Kredlow, M. A., Pich, V., Bui, E., & Hofmann, S. G. (2013). The relationship of PTSD to key somatic complaints and cultural syndrome among Cambodian refugees attending a psychiatric clinic: the Cambodian Somatic Symptom and Syndrome Inventory (CSSI). Transcultural Psychiatry, 50(3), 347–370.
Hinton, D. E., Nickerson, A., & Bryant, R. A. (2014). Prolonged grief in Cambodian refugees following genocide: Rebirth concerns and avoidance of reminders. Journal of Loss and Trauma: International Perspectives on Stress & Coping, 18(5), 444–460.
Hinton, D. E., Rasmussen, A., Nou, L., Pollack, M. H., & Good, M. J. (2009). Anger, PTSD, and the nuclear family: A study of Cambodian refugees. Social Science and Medicine, 69(9), 1387–1394.
Hirai, M., & Clum, G. A. (2000). Development, reliability, and validity of the beliefs toward mental illness scale. Journal of Psychopathology and Behavioral Assessment, 22(3), 221–236.
Ho, M. K. (1984). Social group work with Asian Americans. Social Casework, 57(3), 195–201.
Hoagwood, K. E., Cavaleri, M. A., Olin, S. S., Burns, B. J., Slaton, E., Gruttadaro, D., et al. (2010). Family support in children’s mental health: A review and synthesis. Clinical Child and Family Psychology Review, 13(1), 1–45.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22.
Hom, M. A., Stanley, I. H., & Joiner, T. E., Jr. (2015). Evaluating factors and interventions that influence help seeking and mental health service utilization among suicidal individuals: A review of the literature. Clinical Psychology Review, 40, 28–39.
Horvath, A. O. (2001). The alliance. Psychotherapy: Theory, research, practice, training, 38(4), 365–372.
Horvath, A. O., & Bedi, R. P. (2002). The alliance. In J. C. Norcross (Ed.), Psychotherapy relationships that work (pp. 37–70). Oxford, UK: Oxford University Press.
Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36(2), 223–233.
Horvath, A. O., & Symonds, B. D. (1991). Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology, 38(2), 139–149.
Horwitz, A. (1978). Family, kin, and friend networks in psychiatric help-seeking. Social Science and Medicine, 12(4A), 297–304.
Hovey, J. D., & Magaña, C. G. (2002). Exploring the mental health of Mexican migrant farm workers in the Midwest: Psychosocial predictors of psychological distress and suggestions for prevention and treatment. The Journal of Psychology, 136(5), 493–513.
Howard, K. I., Cornille, T. A., Lyons, J. S., Vessey, J. T., Lueger, R. J., & Saunders, S. M. (1996). Patterns of mental health service utilization. Archives of General Psychiatry, 53, 696–703.
Hsiao, F. H., Klimidis, S., Minas, H. I., & Tan, E. S. (2006). Folk concepts of mental disorders among Chinese-Australian patients and their caregivers. Journal of Advanced Nursing, 55(1), 58–67.
Hsieh, D., & Kirk, S. (2003). The effect of social context on psychiatrists’ judgments of adolescent antisocial behavior. Journal of Child Psychology and Psychiatry, 44(6), 877–887.
Hutchinson, M., & Dorsett, P. (2012). What does the literature say about resilience in refugee people? Implications for practice. Journal of Social Inclusion, 3(2), 55–78.
Hwang, S. K., & Charnley, H. (2010). Making the familiar strange and making the strange familiar: Understanding Korean children’s experiences of living with an autistic sibling. Disability & Society, 25(5), 579–592.
Hwang, W., & Goto, S. (2008). The effects of racial discrimination on minority college students. Cultural Diversity and Ethnic Minority Psychology, 14(4), 326–335.
Insel, T. R. (2009). Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Archives of General Psychiatry, 66(2), 128–133.
Interian, A., Lewis-Fernández, R., & Dixon, L. B. (2013). Improving treatment engagement of underserved US racial-ethnic groups: a review of recent interventions. Psychiatric Services, 64(3), 212–222.
Interian, A., Martinez, I. E., Guarnaccia, P. J., Vega, W. A., & Escobar, J. I. (2007). A qualitative analysis of the perception of stigma among Latinos receiving antidepressants. Psychiatric Services, 58(12), 1591–1594.
Johnson, H. C., Cournoyer, D. E., Fisher, G. A., McQuillan, B. E., Moriarty, S., Richert, A. L., et al. (2000). Children’s emotional and behavioral disorders: Attributions of parental responsibility by professionals. American Journal of Orthopsychiatry, 70(3), 327–339.
Johnson, H. C., Cournoyer, D. E., Fliri, J., Flynn, M., Grant, A., Lant, M., et al. (2003). Are we parent-friendly? Views of parents of children with emotional and behavioral disabilities. Families in Society: The Journal of Contemporary Social Services, 84(1), 95–108.
Johnston, C., & Freeman, W. S. (1997). Attributions for child behavior in parents of children without behavior disorders and children with attention deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology, 65(4), 636–645.
Johnston, C., & Freeman, W. S. (2002). Parents’ beliefs about ADHD: implications for assessment and treatment. ADHD Report, 10(1), 6–9.
Johnston, C., Seipp, C., Hommersen, P., Hoza, B., & Fine, S. (2005). Treatment choices and experiences in attention deficit and hyperactivity disorder: Relations to parents’ beliefs and attributions. Child: Care, Health and Development, 31(6), 669–677.
Jorm, A. F. (2000). Mental health literacy: Public knowledge and beliefs about mental disorders. British Journal of Psychiatry, 177(5), 396–401.
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rogers, B., & Pollitt, P. (1997). Mental health literacy: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal Australia, 166(4), 182–186.
Jourard, S. M. (1964). The transparent self: Self-disclosure and well-being. Cambridge, MA: Van Nostrand.
Kazdin, A., Holland, L., Crowley, M., & Breton, S. (1997). Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal for Child Psychology and Psychiatry, 38(8), 1051–1062.
Kellison, I., Bussing, R., Bell, L., & Garvan, C. (2010). Assessment of stigma associated with attention deficit hyperactivity disorder: Psychometric evaluation of the ADHD Stigma Questionnaire. Psychiatry Research, 178(2), 363–369.
Kelly, A. E., & Achter, J. A. (1995). Self-concealment and attitudes toward counseling in university students. Journal of Counseling Psychology, 42(1), 40–46.
Kessler, R. C., Berglund, P. A., Bruce, M. L., Koch, R., Laska, E. M., Leaf, P. J., et al. (2001). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6, pt.1), 987–1007.
Kim, G., Loi, C. X. A., Chiriboga, D. A., Jang, Y., Parmelee, P., & Allen, R. S. (2011). Limited English proficiency as a barrier to mental health service use: A study of Latino and Asian immigrants with psychiatric disorders. Journal of Psychiatric Research, 45(1), 104–110.
Kim, J. E., & Zane, N. (2016). Help-seeking intentions among Asian American and White American students in psychological distress: Application of the Health Belief Model. Cultural Diversity and Ethnic Minority Psychology, 22(3), 311–321.
King, M., Dinos, S., Shaw, J., Watson, R., Stevens, S., Passetti, F., et al. (2007). The Stigma Scale: Development of a standardised measure of the stigma of mental illness. British Journal of Psychiatry, 190(3), 248–254.
King, S., Rosenbaum, P., & King, G. (1996). Parents’ perceptions of caregiving: Development and validation of a measure of processes. Developmental Medicine and Child Neurology, 38(9), 757–772.
Kirk, S., & Hsieh, D. (2004). Diagnostic consistency in assessing conduct disorder: An experiment on the effect of social context. American Journal of Orthopsychiatry, 74(1), 43–55.
Kirk, S. A., Wakefield, J. C., Hsieh, D., & Pottick, K. J. (1999). Social context and social workers’ judgments of mental disorder. Social Service Review, 73, 82–104.
Kirmayer, L. J. (2001). Cultural variations in the clinical presentation of depression and anxiety: Implications for diagnosis and treatment. Journal of Clinical Psychiatry, 62(Suppl. 13), 22–30.
Kleinknecht, R. A., Dinnel, D. L., & Kleinknecht, E. E. (1997). Cultural factors in social anxiety: A comparison of social phobia symptoms and Taijin Kyofusho. Journal of Anxiety Disorders, 11(2), 157–177.
Kleinman, A. (1978). Concepts and a model for the comparison of medical systems as cultural systems. Social Science and Medicine, 12(2b), 85–93.
Kleinman, A. (1980). Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine, and psychiatry (Vol. 3). Berkeley, CA: University of California Press.
Kleinman, A. (1987). Anthropology and psychiatry: The role of culture in cross-cultural research on illness. The British Journal of Psychiatry, 151(4), 447–454.
Kleinman, A. (2004). Culture and depression. The New England Journal of Medicine, 351(10), 951–953.
Komiya, N., Good, G. E., & Sherrod, N. B. (2000). Emotional openness as a predictor of college students’ attitudes toward seeking psychological help. Journal of Counseling Psychology, 47(1), 138–143.
Koro-Ljungberg, M., & Bussing, R. (2009). The management of courtesy stigma in the lives of families with teenagers with ADHD. Journal of Family Issues, 30(9), 1175–1200.
Kuhl, J., Jarkon-Horlick, L., & Morrissey, R. F. (1997). Measuring barriers to help-seeking behavior in adolescents. Journal of Youth and Adolescence, 26(6), 637–650.
Kung, W. W. (2004). Cultural and practical barriers to seeking mental health treatment for Chinese Americans. Journal of Community Psychology, 32(1), 27–43.
Kuriyama, S. (2002). The divergence of Greek and Chinese medicine. New York: Zone Books.
Kushner, M. G., & Sher, K. J. (1989). Fear of psychological treatment and its relation to mental health service avoidance. Professional Psychology: Research and Practice, 20(4), 251–257.
LaFromboise, T., & Dixon, D. N. (1980). American Indian perception of trustworthiness in a counseling interview. Journal of Counseling Psychology, 28(2), 135–139.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174.
Lau, A. S. (2006). Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice, 13(4), 295–310.
Lawton, K. E., Gerdes, A. C., Haack, L. M., & Schneider, B. (2014). Acculturation, cultural values, and Latino parental beliefs about the etiology of ADHD. Administration and Policy in Mental Health and Mental Health Services Research, 41(2), 189–204.
Lee, J., Friesen, B. J., Walker, J. S., Colman, D., & Donlan, W. E. (2014). Youth’s help-seeking intentions for ADHD and depression: Findings from a national survey. Journal of Child and Family Studies, 23(1), 144–156.
Lee, S., Lee, M. T. Y., Chiu, M. Y. L., & Kleinman, A. (2005). Experience of social stigma by people with schizophrenia in Hong Kong. British Journal of Psychiatry, 186(2), 153–157.
Lee, S., & Wong, K. C. (1995). Rethinking neurasthenia: The illness concepts of shenjing shuairuo among Chinese undergraduates in Hong Kong. Culture, Medicine and Psychiatry, 19(1), 91–111.
Leong, F. T. L., & Lau, A. S. L. (2001). Barriers to providing effective mental health services to Asian Americans. Mental Health Services Research, 3(4), 201–214.
Lin, N., Dean, A., & Ensel, W. M. (1981). Social Support Scales: A methodological note. Schizophrenia Bulletin, 7(1), 73–89.
Lind, A. (2004). Legislating the family: Heterosexual bias in social welfare policy frameworks. Journal of Sociology and Social Welfare, 31(4), 21–35.
Link, B. G. (1987). Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations on rejection. American Sociological Review, 52(1), 96–112.
Liu, Z., Liu, Y., Zhang, Y., Chen, Z., & Hannak, W. (2014). Developing a Chinese PTSD Inventory (CPI) based on interviews with earthquake victims in Sichuan. PsyCh Journal, 3(2), 101–112.
Lloyd, K. R., Jacob, K. S., Patel, V., St. Louis, L., Bhurga, D., & Mann, A. H. (1998). The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychological Medicine, 28(5), 1231–1237.
Loo, C., Tong, B., & True, R. H. (1989). A bitter bean: Mental health status and attitudes in Chinatown. Journal of Community Psychology, 17(4), 283–296.
Mackenzie, C. S., Knox, V. J., Gekoski, W. L., & Macaulay, H. L. (2004). An adaptation and extension of the attitudes towards seeking professional psychological help scale. Journal of Applied Social Psychology, 33(11), 2410–2435.
Mah, J. W., & Johnston, C. (2007). Cultural variations in mothers’ attributions: Influence of child attention-deficit/hyperactivity disorder. Child Psychiatry and Human Development, 38(2), 135–153.
Mak, W. W., Cheung, R. Y., Law, R. W., Woo, J., Li, P. C., & Chung, R. W. (2007). Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Social Science and Medicine, 64(8), 1549–1559.
Mak, W. W. S. (2005). Integrative model of caregiving: How macro and micro factors affect caregivers of adults with severe and persistent mental illness. American Journal of Orthopsychiatry, 75(1), 40–53.
Mak, W. W. S., & Cheung, R. Y. M. (2008). Affiliate stigma among caregivers of people with intellectual disability or mental illness. Journal of Applied Research in Intellectual Disabilities, 21(6), 532–545.
Mak, W. W. S., & Cheung, R. Y. M. (2012). Psychological distress and subjective burden of caregivers of people with mental illness: The role of affiliate stigma and face concern. Community Mental Health Journal, 48(3), 270–274.
Makanjuola, R. O. A. (1987). Ode Ori’: A culture-bound disorder with prominent somatic features in Yoruba Nigerian patients. Acta Psychiatrica Scandinavica, 75(3), 231–236.
Malacrida, C. (2001). Motherhood, resistance and attention deficit disorder: Strategies and limits. Canadian Review of Sociology and Anthropology, 38(2), 141–165.
Markus, H. R., & Kitayama, S. (1991). Culture and the self: Implications for cognition, emotion, and motivation. Psychological Review, 98(2), 224–253.
Marlowe, J. (2009). Accessing authentic knowledge: Being and doing with the Sudanese community. Australian Community Psychologist, 21(1), 39–49.
Marsh, J., Burke, C., & De Los Reyes, A. (2016). The sweet spot of clinical intuitions: Predictors of the effects of context on impressions of conduct disorder symptoms. Psychological Assessment, 28(2), 181–193.
Martin, J. K., Pescosolido, B. A., Olafsdottir, S., & Mcleod, J. D. (2007). The construction of fear: Americans’ preferences for social distance from children and adolescents with mental health problems. Journal of Health and Social Behavior, 48(1), 50–67.
Martin, J., Romas, M., Medford, M., Leffert, N., & Hatcher, S. L. (2006). Adult helping qualities preferred by adolescents. Adolescence, 41(161), 127–140.
Masuda, A., Price, M., Anderson, P., Schmertz, S. K., & Calamaras, M. (2009). The role of psychological flexibility in mental health stigma and psychological distress for the stigmatizer. Journal of Social and Clinical Psychology, 28(10), 1244–1262.
Mathews, M. (2008). Explanatory models for mental illness endorsed by Christian clergymen: The development and use of an instrument in Singapore. Mental Health, Religion and Culture, 11(3), 287–300.
Mathews, M. (2011). Assessment and comparison of culturally based explanations for mental disorder among Singaporean Chinese youth. International Journal of Social Psychiatry, 57(1), 3–17.
Matsuoka, J. K., Breaux, C., & Ryujin, D. H. (1997). National utilization of mental health services by Asian Americans/Pacific Islanders. Journal of Community Psychology, 25(2), 141–145.
McCabe, K. M. (2002). Factors that predict premature termination among Mexican-American children in outpatient psychotherapy. Journal of Child and Family Studies, 11(3), 347–359.
McConnaughy, E. A., Prochaska, J. O., & Velicer, W. F. (1983). Stages of change in psychotherapy: Measurement and sample profiles. Psychotherapy: Theory, Research and Practice, 20(3), 368–375.
McKay, M. M., & Bannon, W. M., Jr. (2004). Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics of North America, 13(4), 905–921.
McKay, M. M., Chasse, K. T., Paikoff, R., McKinney, L. D., Baptiste, D., Coleman, D., et al. (2004). Family-level impact of the CHAMP Family Program: A community collaborative effort to support urban families and reduce youth HIV risk exposure. Family Process, 43(1), 79–93.
McLoyd, V. C. (1998). Socioeconomic disadvantage and child development. American Psychologist, 53(2), 185–204.
Mehta, S. I., & Farina, A. (1988). Associative stigma: Perceptions of the difficulties of college-aged children of stigmatized fathers. Journal of Social and Clinical Psychology, 7(2–3), 192–202.
Messent, P. (1992). Working with Bangladeshi families in the east end of London. Journal of Family Therapy, 14(3), 287–304.
Miller, W. R. (1985). Motivation for treatment: A review with special emphasis on alcoholism. Psychological Bulletin, 98(1), 84–107.
Milstein, G., Guarnaccia, P. J., & Midlarsky, E. (1995). Ethnic differences in the interpretation of mental illness: Perspectives of caregivers. Research in Community and Mental Health, 8, 155–180.
Min, S. K., Suh, S., & Song, K. (2009). Symptoms to use for diagnostic criteria of Hwa-Byung, an anger syndrome. Psychiatry Investigations, 6(1), 7–12.
Miville, M., & Constantine, M. (2007). Sociocultural predictors of psychological help-seeking attitudes and behavior among Mexican American college students. Peace Research Abstracts Journal, 44(3), 420–432.
Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma questionnaire. Journal of Nervous & Mental Disease, 180(2), 111–116.
Mollica, R. F., Donelan, K., Tor, S., Lavelle, J., Elias, C., Frankel, M., et al. (1993). The effect of trauma and confinement on functional health and mental health status of Cambodians living in Thailand-Cambodia border camps. Journal of the American Medical Association, 270(5), 581–586.
Moses, T. (2009). Stigma and self-concept among adolescents receiving mental health treatment. American Journal of Orthopsychiatry, 79(2), 261–274.
Moses, T. (2010). Adolescent mental health consumers’ self-stigma: Associations with parents’ and adolescents’ illness perceptions and parental stigma. Journal of Community Psychology, 38(6), 781–798.
Moses, T. (2011). Stigma apprehension among adolescents discharged from brief psychiatric hospitalization. The Journal of Nervous and Mental Disease, 199(10), 778–789.
Moskos, M. A., Olson, L., Halbern, S. R., & Gray, D. (2007). Utah youth suicide study: Barriers to mental health treatment for adolescents. Suicide and Life-Threatening Behavior, 37(2), 179–186.
Moss-Morris, R., Weinman, J., Petrie, K. J., Horne, R., Cameron, L. D., & Buick, D. (2002). The revised illness perception questionnaire (IPQ-R). Psychology and Health, 17(1), 1–16.
Muhlbauer, S. A. (2002). Navigating the storm of mental illness: phases in the family’s journey. Qualitative Health Research, 12(8), 1076–1092.
Mukolo, A., & Heflinger, C. A. (2011). Factors associated with attributions about child health conditions and social distance preference. Community Mental Health Journal, 47(3), 286–299.
Murdock, G. P., Wilson, S. F., & Frederick, V. (1980). World distribution of theories of illness. Transcultural Psychiatric Research Review, 17(1/2), 37–64.
Murguia, A., Zea, M. C., Reisen, C. A., & Peterson, R. A. (2000). The development of the cultural health attributions questionnaire (CHAQ). Cultural Diversity and Ethnic Minority Psychology, 6(3), 268–283.
Myers, H. F., Lesser, I., Rodriguez, N., Mira, C. B., Hwang, W., Camp, C., et al. (2002). Ethnic differences in clinical presentation of depression in adult women. Cultural Diversity of Ethnic Minority Psychology, 8, 138–156.
Nadler, A. (1986a). Help seeking as a natural phenomenon: Differences between city and kibbutz dwellers. Journal of Personality and Social Psychology, 51(5), 976–982.
Nadler, A. (1986b). Self-esteem and the seeking and receiving of help: Theoretical and empirical perspectives. In B. Maher & W. Maher (Eds.), Progress in experimental personality research (Vol. 14, pp. 115–163). New York: Academic Press.
Nash, M., Wong, J., & Trlin, A. (2006). Civic and social integration: A new field of social work practice with immigrants, refugees and asylum seekers. International Social Work, 49(3), 345–363.
Neubeck, K. J., & Cazenave, N. A. (2001). Welfare racism: Playing the race card against America’s poor. Hove: Psychology Press.
New Freedom Commission on Mental Health. (2003). Achieving the promise: Transforming mental health care in America. Final report (Pub No. SMA-03-3832). Bethesda, MD: US Department of Health and Human Services.
Nguyen, Q. C. X., & Anderson, L. P. (2005). Vietnamese Americans’ attitudes toward seeking mental health services: relation to cultural variables. Journal of Community Psychology, 33(2), 213–231.
Nickerson, K. J., Helms, J. E., & Terrell, F. (1994). Cultural mistrust, opinions about mental illness, and Black students’ attitudes toward seeking psychological help from White counselors. Journal of Counseling Psychology, 41(3), 378–385.
Nock, M. K., & Ferriter, C. (2005). Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review, 8(2), 149–166.
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73(5), 872–879.
Nock, M. K., & Photos, V. (2006). Parent motivation to participate in treatment: Assessment and prediction of subsequent participation. Journal of Child and Family Studies, 15(3), 345–358.
Norberg, M. M., Wetterneck, C. T., Sass, D. A., & Kanter, J. W. (2011). Development and psychometric evaluation of the Milwaukee psychotherapy expectations questionnaire. Journal of Clinical Psychology, 67(6), 574–590.
Norquist, G. S., & Regier, D. A. (1996). The epidemiology of psychiatric disorders and the de facto mental health care system. Annual Review of Medicine, 47(1), 473–479.
Okamoto, S. K., Helm, S., Po‘a-Kekuawela, K., Chin, C. I. H., & Nebre, L. H. (2009). Community risk and resiliency factors related to drug use of rural Native Hawaiian youth: An exploratory study. Journal of Ethnicity in Substance Abuse, 8, 1–15.
Orlinsky, D. E., Ronnestad, M. H., & Willutzki, U. (2004). Fifty years of psychotherapy process-outcome research: Continuity and change. In M. J. Lambert (Ed.), Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change (5th ed., pp. 307–389). New York: Wiley.
Orloff, A. S. (2002). Explaining US welfare reform: Power, gender, race and the US policy legacy. Critical Social Policy, 22(1), 96–118.
Pan, D., Huey, S. J., Jr., & Hernandez, D. (2011). Culturally adapted versus standard exposure treatment for phobic Asian Americans: Treatment efficacy, moderators, and predictors. Cultural Diversity and Ethnic Minority Psychology, 17(1), 11–22.
Paradis, C., Friedman, S., Hinton, D. E., McNally, R. J., Solomon, L. Z., & Lyons, K. A. (2009). The assessment of the phenomenology of sleep paralysis: The unusual sleep experiences questionnaire (USEQ). CNS Neuroscience & Therapeutics, 15(3), 220–226.
Parcesepe, A. M., & Cabassa, L. J. (2013). Public stigma of mental illness in the United States: A systematic literature review. Administration and Policy in Mental Health and Mental Health Services Research, 40(5), 384–399.
Park, A. S. (1993). The wounded heart of god: The Asian concept of han and the christian doctrine of sin. Nashville, TN: Abingdon Press.
Park, Y. J., Ryu, H., Han, K. S., Kwon, J. H., Kim, H. K., Kang, H. C., et al. (2010). Anger, anger expression, and suicidal ideation in Korean adolescents. Archives of Psychiatric Nursing, 24(3), 168–177.
Patel, S., & Bakken, S. (2010). Preferences for participation in decision making among ethnically diverse patients with anxiety and depression. Community Mental Health Journal, 46(5), 466–473.
Patterson, G. R., & Forgatch, M. S. (1985). Therapist behavior as a determinant for client noncompliance: A paradox for the behavior modifier. Journal of Consulting and Clinical Psychology, 53(6), 846–851.
Pescosolido, B. A. (2013). The public stigma of mental illness what do we think; what do we know; what can we prove? Journal of Health and Social Behavior, 54(1), 1–21.
Pescosolido, B. A., Jensen, P. S., Martin, J. K., Perry, B. L., Olafsdottir, S., & Fettes, D. (2008). Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. Journal of the American Academy of Child and Adolescent Psychiatry, 47(3), 339–349.
Petrie, K. J., Jago, L. A., & Devcich, D. A. (2007). The role of illness perceptions in patients with medical conditions. Current Opinion in Psychiatry, 20(2), 163–167.
Phan, T., Steel, Z., & Silove, D. (2004). An ethnographically derived measure of anxiety, depression and somatization: The Phan Vietnamese Psychiatric Scale. Transcultural Psychiatry, 41(2), 200–232.
Phelan, J. C., Bromet, E. J., & Link, B. G. (1998). Psychiatric illness and family stigma. Schizophrenia Bulletin, 24(1), 115–126.
Phillips, M. R., Li, Y., Stroup, S., & Xin, L. (2000). Causes of schizophrenia reported by patients’ family members in China. British Journal of Psychiatry, 177(1), 20–25.
Pinfold, V., Toumin, H., Thornicroft, G., Huxley, P., Farmer, P., & Graham, T. (2003). Reducing psychiatric stigma and discrimination: Evaluation of educational interventions in UK secondary schools. BMC Psychiatry, 182(4), 342–346.
Pinto, M. D., Hickman, R., Logsdon, M. C., & Burant, C. (2012). Psychometric evaluation of the revised attribution questionnaire (r-AQ) to measure mental illness stigma in adolescents. Journal of Nursing Measurement, 20(1), 47–58.
Pirutinsky, S., Rosen, D. D., Shapiro Safran, R., & Rosmarin, D. H. (2010). Do medical models of mental illness relate to increased or decreased stigmatization of mental illness among Orthodox Jews? The Journal of Nervous and Mental Disease, 198(7), 508–512.
Portes, A. (1997). Immigration theory for a new century: Some problems and opportunities. International Migration Review, 31(4), 799–825.
Pottick, K. J., & Davis, D. M. (2001). Attributions of responsibility for children’s mental health problems: Parents and professionals at odds. American Journal of Orthopsychiatry, 71, 426–435.
Pottick, K. J., Kirk, S. A., Hsieh, D. K., & Tian, X. (2007). Judging mental disorder: Effects of client, clinician, and contextual differences. Journal of Consulting and Clinical Psychology, 75, 1–8.
Pottick, K. J., Wakefield, J. C., Kirk, S. A., & Tian, X. (2003). Influence of social workers’ characteristics on the perception of mental disorder in youths. Social Service Review, 77, 431–454.
Pottick, K.J., & Warner, L.A. (2002). More than 115,000 disadvantaged preschoolers receive mental health services (report #1-2). Update: Latest findings in children’s mental health. Retrieved from Rutgers University, Institute for Health, Health Care Policy and Aging Research. http://www.ihhcpar.rutgers.edu/downloads/fall2002.pdf. Accessed 20 February 2017.
Prelow, H. M., Danoff-Burg, S., Swenson, R. R., & Pulgiano, D. (2004). The impact of ecological risk and perceived discrimination on the psychological adjustment of African American and European American youth. Journal of Community Psychology, 32(4), 375–389.
Price, P. B., & Jones, E. E. (1998). Examining the alliance using the Psychotherapy Process Q-Set. Psychotherapy, 25(3), 392–404.
Prince, R. (1962). The “brain fag” syndrome in Nigerian students. The British Journal of Psychiatry, 106(443), 559–570.
Raftery, J. N., Steinke, C. M., & Nickerson, A. B. (2010). Engagement, residual treatment of staff cognitive and behavioral disputations, and youths’ problem-solving. Child & Youth Care Forum, 39(1), 167–185.
Rao, D., Feinglass, J., & Corrigan, P. (2007). Racial and ethnic disparities in mental illness stigma. The Journal of Nervous and Mental Disease, 195(12), 1020–1023.
Richardson, L. A. (2001). Seeking and obtaining mental health services: What do parents expect? Archives of Psychiatric Nursing, 15(5), 223–231.
Ridley, C. R. (1984). Clinical treatment of the nondisclosing Black client: A therapeutic paradox. American Psychologist, 39(11), 1234–1244.
Rodrigues, L., Calheiros, M., & Pereira, C. (2015). The decision of out-of-home placement in residential care after parental neglect: Empirically testing a psychosocial model. Child Abuse and Neglect, 49, 35–49.
Rose, A., Peters, N., Shea, J. A., & Armstrong, K. (2004). Development and testing of the health care system distrust scale. Journal of General Internal Medicine, 19(4), 57–63.
Rosenbloom, S. R., & Way, N. (2004). Experiences of discrimination among African American, Asian American, and Latino adolescents in an urban high school. Youth & Society, 35(4), 420–451.
Rostain, A. L., Power, T. J., & Atkins, M. S. (1993). Assessing parents’ willingness to pursue treatment for children with attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 32(1), 175–181.
Ruedell, K., Bhui, K., & Priebe, S. (2009). Concept development and application of a new mixed method assessment of cultural variations in illness perceptions. Journal of Health Psychology, 14(2), 336–347.
Ryan, R. M., Plant, R. W., & O’Malley, S. (1995). Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors, 20(3), 279–297.
Ryder, A. G., Yang, J., Zhu, X., Yao, S., Yi, J., Heine, S. J., et al. (2008). The cultural shaping of depression: Somatic symptoms in China, psychological symptoms in North America? Journal of Abnormal Psychology, 117(2), 300–313.
Salmán, E., Liebowitz, M. R., Guarnaccia, P. J., Jusino, C. M., Garfinkel, R., Street, L., et al. (1998). Subtypes of ataques de nervios: The influence of coexisting psychiatric diagnosis. Culture, Medicine and Psychiatry, 22(2), 231–244.
Sanders Thompson, V. L., Bazile, A., & Akbar, M. (2004). African Americans’ perceptions of psychotherapy and psychotherapists. Professional Psychology: Research and Practice, 35(1), 19–26.
Saunders, S. M. (1993). Applicants’ experience of the process of seeking therapy. Psychotherapy, 30(4), 554–564.
Scheff, T. J. (1966). Being mentally Ill: A sociological theory. Chicago, IL: Aldine.
Schnurr, P. P., & Green, B. L. (2004). Understanding relationships among trauma, post-tramatic stress disorder, and health outcomes. Advances in Mind-body Medicine, 20(1), 18–29.
Schomerus, G., Matschinger, H., & Angermeyer, M. C. (2014). Causal beliefs of the public and social acceptance of persons with mental illness: A comparative analysis of schizophrenia, depression and alcohol dependence. Psychological Medicine, 44(2), 303–314.
Scior, K., & Furnham, A. (2011). Development and validation of the Intellectual Disability Literacy Scale for assessment of knowledge, beliefs and attitudes to intellectual disability. Developmental Disabilities, 32, 1530–1541.
Scuglik, D. L., Alarcón, R. D., Lapeyre, A. C., Williams, M. D., & Logan, K. M. (2007). When the poetry no longer rhymes: Mental health issues among Somali immigrants in the USA. Transcultural Psychiatry, 44(4), 581–595.
Seaton, E. K., Caldwell, C. H., Sellers, R. M., & Jackson, J. S. (2008). The prevalence of perceived discrimination among African American and Caribbean Black youth. Developmental Psychology, 44(5), 1288–1297.
Seiffge-Krenke, I., & Shulman, S. (1990). Coping style in adolescence. A cross-cultural study. Journal of Cross-Cultural Psychology, 21(3), 351–377.
Shapiro, E. G. (1983). Embarrassment and help-seeking. In B. M. DePaulo, A. Nadler, & J. Fisher (Eds.), New directions in helping (Vol. 2, pp. 143–163)., Help seeking New York: Academic Press.
Shapiro, D., & Shapiro, D. (1987). Change processes in psychotherapy. Addiction, 82(4), 431–444.
Shibre, T., Negash, A., Kullgren, G., Kebede, D., Alem, A., Fekadu, A., et al. (2001). Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Social Psychiatry and Psychiatric Epidemiology, 36(6), 299–303.
Shin, J. K. (2002). Help-seeking behaviors by Korean immigrants for depression. Issues in Mental Health Nursing, 23(5), 461–476.
Shirk, S. R., & Karver, M. (2003). Prediction of treatment outcome from relationship variables in child and adolescent therapy: A meta-analytic review. Journal of Consulting and Clinical Psychology, 71(3), 452–464.
Shokoohi-Yekta, M., & Retish, P. M. (1991). Attitudes of Chinese and American male students towards mental illness. International Journal of Social Psychiatry, 37(3), 192–200.
Simon, D., Schorr, G., Wirtz, M., Vodermaier, A., Caspari, C., Neuner, B., et al. (2006). Development and first validation of the shared decision-making questionnaire (SDM-Q). Patient and Education Counseling, 63(3), 319–327.
Singh, I. (2004). Doing their jobs: Mothering with Ritalin in a culture of mother-blame. Social Science and Medicine, 59(6), 1193–1205.
Snowden, L. R. (2003). Bias in mental health assessment and intervention: Theory and evidence. American Journal of Public Health, 93(2), 239–243.
Sonuga-Barke, E. J. S., & Balding, J. (1993). British parents’ belief about the causes of three forms of childhood psychological disturbance. Journal of Abnormal Child Psychology, 21(4), 367–376.
Spencer, M. S., & Chen, J. (2004). Effect of discrimination on mental health service utilization among Chinese Americans. American Journal of Public Health, 94(5), 809–814.
Stacciarini, J. M., Shattell, M. M., Coady, M., & Wiens, B. (2011). Review: Community-based participatory research approach to address mental health in minority populations. Community Mental Health Journal, 47(5), 489–497.
Staudt, M. (1999). Barriers and facilitators to use of services following intensive family preservation services. The Journal of Behavioral Health Services & Research, 26(1), 39–49.
Staudt, M. (2007). Treatment engagement with caregivers of at-risk children: Gaps in research and conceptualization. Journal of Child and Family Studies, 16(2), 183–196.
Steel, Z., Silove, D., Phan, T., & Bauman, A. (2002). Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. The Lancet, 360(9339), 1056–1062.
Stefl, M. E., & Prosperi, D. C. (1985). Barriers to mental health service utilization. Community Mental Health Journal, 21(3), 167–177.
Stengler-Wenzke, K., Trosbach, J., Dietrich, S., & Angermeyer, M. C. (2004). Experience of stigmatization by relatives of patients with obsessive compulsive disorder. Archives of Psychiatric Nursing, 18(3), 88–96.
Stone, L., & Finlay, W. M. L. (2008). A comparison of African-Caribbean and white European young adults’ conceptions of schizophrenia symptoms and the diagnostic label. International Journal of Social Psychiatry, 54(3), 242–261.
Stormshak, E. A., Dishion, T. J., Light, J., & Yasui, M. (2005). Implementing family-centered interventions within the public middle school: Linking service delivery to change in problem behavior. Journal of Abnormal Child Psychology, 33, 723–733.
Strong, S. R., & Claiborn, C. D. (1982). Change through interaction: Social psychological processes of counseling and psychotherapy. New York: Wiley.
Struening, E. L., Perlick, D. A., Link, B. G., Hellman, F., Herman, D., & Sirey, J. A. (2001). Stigma as a barrier to recovery: The extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services, 52(12), 1633–1638.
Sue, S. (1977). Community mental health services to minority groups: Some optimism, some pessimism. American Psychologist, 32(8), 616–624.
Sue, S. (1998). In search of cultural competence in psychotherapy and counseling. American Psychologist, 53(4), 440–448.
Sue, S. (2006). Cultural competency: From philosophy to research and practice. Journal of Community Psychology, 34(2), 237–245.
Sue, S., Cheng, J. K. Y., Saad, C. S., & Chu, J. P. (2012). Asian American mental health: A call to action. American Psychologist, 67(7), 532–544.
Sue, S., & Sue, D. (1974). MMPI comparisons between Asian-American and non-Asian American students utilizing a student health psychiatric clinic. Journal of Counseling Psychology, 21(5), 423–427.
Sue, D. W., & Sue, D. (2003). Counseling the culturally diverse: Theory and practice. New York, NY: Wiley.
Sun, B., Fan, N., Nie, S., Zhang, M., Huang, X., He, H., et al. (2014). Attitudes toward people with mental illness among psychiatrists, psychiatric nurses, involved family members and the general population in a large city in Guangzhou, China. International Journal of Mental Health Systems. doi:10.1186/1752-4458-8-26.
Surgeon General. (2001). Mental health: Culture, race, and ethnicity. A supplement to mental health: a report of the Surgeon General. U.S. Department of Health and Human Services. Washington, DC: Government Printing Office.
Takeuchi, D. T., Leaf, P. J., & Kuo, H. (1988). Ethnic differences in the perception of barriers to help-seeking. Social Psychiatry and Psychiatric Epidemiology, 23(4), 273–280.
Tarakeshwar, N., Stanton, J., & Pargament, K. I. (2003). Religion an overlooked dimension in cross-cultural psychology. Journal of Cross-Cultural Psychology, 34(4), 377–394.
Taylor, S. M., & Dear, M. J. (1981). Scaling Community Attitudes toward the Mentally Ill. Schizophrenia Bulletin, 7(2), 225–240.
Terrell, F., & Terrell, S. (1981). An inventory to measure cultural mistrust among Blacks. Western Journal of Black Studies, 5(3), 180–185.
Terrell, F., & Terrell, S. (1984). Race of counselor, client sex, cultural mistrust level, and premature termination from counseling among Black clients. Journal of Counseling Psychology, 31(3), 371–375.
Tetley, A., Jinks, M., Huband, N., & Howells, K. (2011). A systematic review of measures of therapeutic engagement in psychosocial and psychological treatment. Journal of Clinical Psychology, 67(9), 927–941.
Thakker, J., & Ward, T. (1998). Culture and classification: The cross-cultural application of the DSM-IV. Clinical Psychology Review, 18(5), 501–529.
Thompson, E. H., Jr., & Doll, W. (1982). The burden of families coping with the mentally Ill: An invisible crisis. Family Relations, 31(3), 379–388.
Thurston, I. B., Phares, V., Coates, E. E., & Bogart, L. M. (2015). Child problem recognition and help-seeking intentions among black and white parents. Journal of Clinical Child & Adolescent Psychology, 44(4), 604–615.
Tinsley, H. E. A., Workman, K. R., & Kass, R. A. (1980). Factor analysis of the domain of client expectancies about counseling. Journal of Counseling Psychology, 27(6), 561–570.
Tsang, H. W. H., Fung, K. M. T., & Corrigan, P. W. (2006). Psychosocial treatment compliance scale for people with psychotic disorders. Australian and New Zealand Journal of Psychiatry, 40(6–7), 561–569.
Tseng, W. S., Asai, M., Jieqiu, L., Wibulswasdi, P., Suryani, L. K., Wen, J. K., et al. (1990). Multi-cultural study of minor psychiatric disorders in Asia: Symptom manifestations. International Journal of Social Psychiatry, 36(4), 252–264.
U. S. Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity. A supplement to mental health: A report of the surgeon general. Rockville, MD: US Department of Health and Human Services.
Uba, L. (1982). Meeting the mental health needs of Asian Americans: Mainstream or segregated services. Professional Psychology, 13(2), 215–221.
Uomoto, J. M., & Gorsuch, R. L. (1984). Japanese American response to psychological disorder: Referral patterns, attitudes, and subjective norms. American Journal of Community Psychology, 12(5), 537–550.
U.S. Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity. A supplement to mental health: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services.
Van der Helm, G. H. P., Wissink, I. B., De Jongh, T., & Stams, G. J. J. M. (2012). Measuring treatment motivation in secure juvenile facilities. International Journal of Offender Therapy and Comparative Criminology, 57(8), 996–1008.
Vega, W. A., & Gil, A. G. (1998). Drug use and ethnicity in early adolescence. Berlin: Springer.
Vega, W. A., Kolody, B., Aguilar-Gaxiola, S., & Catalano, R. (1999). Gaps in service utilization by Mexican Americans with mental health problems. American Journal of Psychiatry, 156(6), 928–934.
Vogel, D. L., Wade, N. G., & Haake, S. (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53(3), 325–337.
Vogel, D. L., & Wester, S. R. (2003). To seek help or not to seek help: The risks of self-disclosure. Journal of Counseling Psychology, 50(3), 351–361.
Wakefield, J. C., Kirk, S. A., Pottick, K. J., & Hsieh, D. (1999). Disorder attribution and clinical judgment in the assessment of adolescent antisocial behavior. Social Work Research, 23, 227–240.
Wang, J., & Lai, D. (2008). The relationship between mental health literacy, personal contacts and personal stigma against depression. Journal of Affective Disorders, 110(1–2), 191–196.
Wang, P. S., Lane, M., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 629–640.
Watson, A. C., Corrigan, P., Larson, J. E., & Sells, M. (2007). Self-stigma in people with mental illness. Schizophrenia Bulletin, 33(6), 1312–1318.
Webster-Stratton, C. (1984). A randomized trial of two parent training programs for families with conduct-disordered children. Journal of Consulting and Clinical Psychology, 52(4), 666–678.
Weiner, B., Perry, R. P., & Magnusson, J. (1988). An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology, 55(5), 738–748.
Weiss, M. (1997). Explanatory model interview catalogue (EMIC): Framework for comparative study of illness. Transcultural Psychiatry, 34(2), 235–263.
Westoby, P., & Ingamells, A. (2010). A critically informed perspective of working with resettling refugee groups in Australia. The British Journal of Social Work, 40(6), 1759–1776.
Whaley, A. L. (1997). Ethnic and racial differences in perceptions of dangerousness of persons with mental illness. Psychiatric Services, 48(10), 1328–1330.
Whitbeck, L. B., McMorris, B. J., Hoyt, D. R., Stubben, J. D., & LaFromboise, T. (2002). Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the upper Midwest. Journal of Health and Social Behavior, 43(4), 400–418.
Wilcox, C. E., Washburn, R., & Patel, V. (2007). Seeking help for attention deficit hyperactivity disorder in developing countries: A study of parental explanatory models in Goa, India. Social Science and Medicine, 64(8), 1600–1610.
Wilson, C. J., Deane, F. P., & Ciarrochi, J. (2005). Measuring help-seeking intentions: Properties of the general help-seeking questionnaire. Canadian Journal of Counselling, 39(1), 15–28.
Wong, J. L. (1994). Lay theories of psychotherapy and perceptions of therapists: A replication and extension of Furnham and Wardley. Journal of Clinical Psychology, 50(4), 624–632.
Wong, E. C., Collins, R. L., Cerully, J. L., Seelam, R., & Roth, E. (2016). Racial and ethnic differences in mental illness stigma and discrimination among californians experiencing mental health challenges. Santa Monica, CA: RAND Corporation.
Wong, C. A., Eccles, J. S., & Sameroff, A. (2003). The influence of ethnic discrimination and ethnic identification on African American adolescents’ school and socioemotional adjustment. Journal of Personality, 71(6), 1197–1232.
Wong, D. F. K., Tsui, H. K. P., Pearson, V., Chen, E. Y. H., & Chiu, S. N. (2004). Family burdens, Chinese health beliefs, and the mental health of Chinese caregivers in Hong Kong. Transcultural Psychiatry, 41(4), 497–513.
Wong, R., Wu, R., Guo, C., Lam, J. K., & Snowden, L. R. (2012). Culturally sensitive depression assessment for Chinese American immigrants: development of a comprehensive measure and a screening scale using an item response approach. Asian American Journal of Psychology, 3(4), 230–253.
Yang, L. H., Corsini-Munt, S., Phelan, J. C., & Link, B. G. (2009). Factors underlying beliefs of traditional Chinese medicine efficacy for psychiatric and physical disorders among Chinese Americans: Implications for mental health service utilization. The Journal of Nervous and Mental Disease, 197(3), 207–210.
Yang, L. H., Phelan, J. C., & Link, B. G. (2008). Stigma and beliefs of efficacy towards traditional Chinese medicine and Western psychiatric treatment among Chinese-Americans. Cultural Diversity and Ethnic Minority Psychology, 14(1), 10–18.
Yap, M. B. H., & Jorm, A. F. (2012). Young people’s mental health first aid intentions and beliefs prospectively predict their actions: Findings from an Australian National Survey of Youth. Psychiatry Research, 196(2), 315–319.
Yap, M. B. H., Mackinnon, A., Reavley, N., & Jorm, A. F. (2014). The measurement properties of stigmatizing attitudes towards mental disorders: Results from two community surveys. International Journal of Methods in Psychiatric Research, 23(1), 49–61.
Yasui, M., & Dishion, T. J. (2007). The ethnic context of child and adolescent problem behavior: Implications for child and family interventions. Clinical Child and Family Psychology Review, 10(2), 137–179.
Yasui, M., & Henry, D. B. (2014). Shared understanding as a gateway for treatment engagement: A preliminary study examining the effectiveness of the culturally-enhanced video feedback engagement intervention. Journal of Clinical Psychology, 70(7), 658–672.
Yasui, M., Hipwell, A. E., Stepp, S. D., & Keenan, K. (2015). Psychocultural correlates of mental health service utilization among African American and European American girls. Administration Policy and Mental Health, 42(6), 756–766.
Yeh, M., & Hough, R. L. (1997). Beliefs about the causes of child problems questionnaire. Dr. Yeh at myeh@casrc.org
Yeh, M., Hough, R. L., McCabe, K., Lau, A., & Garland, A. (2004). Parental beliefs about the causes of child problems: Exploring racial/ethnic patterns. Journal of the American Academy of Child and Adolescent Psychiatry, 43(5), 605–612.
Yeh, C. J., & Kwong, A. (2009). Asian American indigenous healing and coping. In N. Tewari & A. Alvarez (Eds.), Asian American psychology: Current perspectives (pp. 559–574). New York: Psychology Press.
Yeh, M., McCabe, K., Hough, R. L., Dupuis, D., & Hazen, A. (2003). Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Mental Health Services Research, 5, 65–77.
Yeh, M., Takeuchi, D. T., & Sue, S. (1994). Asian-American children treated in the mental health system: A comparison of parallel and mainstream outpatient service centers. Journal of Clinical Child Psychology, 23(1), 5–12.
Yong, F., & McCallion, P. (2004). Hwabyung as caregiving stress among Korean-American caregivers of a relative with dementia. Journal of Gerontological Social Work, 42(2), 3–19.
Young, A. (1976). Internalizing and externalizing medical belief systems: An Ethiopian example. Social Science and Medicine, 10(3), 147–156.
Young, A. S., & Rabiner, D. (2015). Racial/ethnic differences in parent-reported barriers to accessing children’s health services. Psychological Services, 12(3), 267–273.
Zung, W. W. K. (1965). A self rating depression scale. Archives of General Psychiatry, 12(1), 63–70.
Acknowledgements
This research was supported by a grant from the Agency of Healthcare Research and Quality to Dr. Yasui (AHRQ: 5K12 HS023007). The authors thank Jonathan M. Storm for editorial support and Lenna Nepomnyaschy for thoughtful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yasui, M., Pottick, K.J. & Chen, Y. Conceptualizing Culturally Infused Engagement and Its Measurement for Ethnic Minority and Immigrant Children and Families. Clin Child Fam Psychol Rev 20, 250–332 (2017). https://doi.org/10.1007/s10567-017-0229-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-017-0229-2