Abstract
Community dwelling military families from the National Guard and Reserve contend with deployment-related stressors in relative isolation, living in communities where mental health providers may have little knowledge of military culture. When they are community residents, active duty service members and families tend to live in close proximity to their military installations. This article will focus primarily on the challenges to quality mental health care for reserve component (RC) families. Where studies of RC families are absent, those of active component (AC) families will be highlighted as relevant. Upon completion of a deployment, reintegration for RC families is complicated by high rates of symptomatology, low service utilization, and greater barriers to care relative to AC families. A paucity of providers skilled in evidence-based treatments (EBTs) limits community mental health capacity to serve RC military families. Several emergent programs illustrate the potential for better serving community dwelling military families. Approaches include behavioral health homes, EBTs and treatment components, structured resiliency and parent training, military informed schools, outreach methods, and technology-based coping, and psychoeducation. Methods from implementation science to improve clinical skill acquisition and spread and sustainability of EBTs may advance access to and quality of mental health treatment and are reviewed herein. Recommendations related to research methods, military knowledge and treatment competencies, and transition to a public health model of service delivery are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The paucity of well-validated interventions for RC families represents a serious limitation in our national capacity to address effectively the needs of service members and their families as they return to home communities where there is scant recognition of the challenges of reintegration. Service members’ exposure to combat and other forms of war zone stress contributes substantially to the development of posttraumatic stress disorder (PTSD), co-morbid mental health symptoms and disorders, and functional impairments (Thomas et al. 2010). Since the beginning of Operations Iraqi and Enduring Freedom (OIF/OEF), 21.8 % of first-time users of Department of Veterans Affairs (VA) health care facilities were diagnosed with PTSD and 17.4 % with a depressive disorder (Seal et al. 2009). Mental health care needs were identified for 20.3 % of active component and 42.4 % of reserve component service members 3–4 months following deployment (Milliken et al. 2007). Service members who deployed after September 11, 2001 were 26 % more likely to develop posttraumatic stress and other psychiatric symptoms and disorders relative to those deployed prior to the global war on terror (Wells et al. 2012). As multiple deployments and shorter dwell times have become a norm, levels of combat engagement and exposure to traumatic events have multiplied; by one estimate, more than 80 % of combat deployed service members have been attacked or ambushed, and approximately 25 % have witnessed, often at close range, the shooting of a comrade. Concurrently, clinical symptomatology, disorder, and service needs have increased.
Research is accumulating to suggest that deployment and reintegration stressors take a toll on civilian family members, more so with multiple cycles of deployment and reunion (Thomas et al. 2010). Mental health problems and diagnoses among deployed service members and their families occur at rates well above those observed among nondeployed military and civilian families. Spouses of deployed service members experience higher levels of psychological distress and perceive their relationships as having lower quality relative to spouses of the nondeployed (Lambert et al. 2012). Challenges for families include lengthy and sometimes traumatic separations, anxiety about service member injury and death, and moves that disrupt social relationships, school, and community resources. Although RC families are not reassigned to different duty locations, families not infrequently relocate to be closer to relatives who can provide assistance and support while a spouse is deployed. Across the deployment cycle, children’s functioning is associated significantly with the mental health of civilian caregivers.
Deployment-related stress and trauma disproportionately affect RC families. Specific incidence is difficult to estimate due to samples that comprise AC, RC, or an admixture of both. In a National Guard sample, 40 % of service members and 34 % of spouses reported mental health difficulties (Gorman et al. 2010, 2011). Other research has linked increases in PTSD symptoms among RC service members following combat theater deployment with adjustment problems between spouses and parenting challenges (Gewirtz et al. 2010). Despite these concerning rates, in each instance, those experiencing clinically significant problems remain a minority, albeit a substantial one. Thus, concern should be tempered with recognition that most military families adjust to deployment without significant symptomatology.
Of the more than 1.9 million children of military parents, greater than 700,000 have experienced the overseas deployment of at least one parent. Most military children are resilient and adjust well to the deployment experience (Lester et al. 2010). Yet, studies indicate that some children experience significant deployment-related stress and behavior problems. Relatively, few studies have stratified samples by age. Most have relied on convenience samples. The largest proportion of RC children are between ages 6 and 11 (52 %) compared to 32 % in this age range within AC families (Sogomonyan and Cooper 2010, May). Three-to-eight-year-old children of AC members experienced higher levels of anxiety, behavior, and stress disorders relative to children of nondeployed parents (Gorman et al. 2010). Youth, aged 11–17, with a deployed parent experienced levels of distress that exceeded national civilian norms. Regression analyses controlled for demographic and deployment covariates. Greater age, living in civilian housing, poor caregiver mental health, and deployment duration were associated with greater problems adapting to deployment and reintegration. Girls’ problems exceeded those of boys during reintegration but not during the deployment itself. RC families reported less social support and more mental health problems, although these differences were small relative to the other factors (Chandra et al. 2009, 2011; Gibbs et al. 2007) Similarly, service member injury, severity, and death exerted a negative effect on children (Gibbs et al. 2007; Mansfield et al. 2011).
In studies with samples that are not stratified according to AC and RC status, a similar pattern of deployment-related difficulties emerges. The authors of one mixed sample study (Siegel et al. 2013) highlighted children of deployed parents as experiencing higher rates worry (>33 %), poor coping and academic skills (20 %), and more mental health diagnoses relative to children of nondeployed parents. Among an admixture of AC and RC families enrolling in the National Military Family Association Operation Purple camps, parent deployment was associated with higher rates of depression relative to peers whose parents were not deployed. These patterns were evident during and subsequent to deployment (Chandra et al. 2009).
Studies of AC families have documented similar patterns of elevated child difficulties. For example, children in AC families experienced higher rates of ICD-9 (United States. Health Care Financing Administration 2004) diagnoses related to acute stress and adjustment reactions, depressive disorders, and behavior disorders with severity increasing with deployment duration (Mansfield et al. 2011). Child maltreatment within active duty families increases with length and number of combat deployments (Fullerton et al. 2011; Gibbs et al. 2007; Milliken et al. 2007). Since mothers and other female caregivers typically are civilian, primary caregivers opportunities for maltreatment reports exist that are not present for the deployed spouse. Relative to nondeployed service members, maltreatment was more prevalent for families overall and for mothers specifically contending with parental combat deployment with risk ratios (RR) of 1.42 and 3.33, respectively. The family RR for moderate to severe maltreatment was 1.61. Physical abuse rates were lower at the family level (RR = .76) and higher for female, civilian caregivers (RR = 1.91). Elevated neglect rates were observed among deployed families (RR = 1.95) and by civilian caregivers who were female with a RR of 3.88 (Gibbs et al. 2007). The relationship of parental combat and child problems was further supported by the observation predeployment stress and family distress following a service member injury resulted in odds ratios for child distress of 8.11 and 21.25, respectively (Cozza et al. 2010). For RC families, these data must be interpreted with notable caution as they are drawn from samples of active duty Army families.
Although the evidence tends to be sparse and inconsistent in terms of AC, RC, or combined samples, a proportion of children of military families experience significant challenges related to deployment. Children of RC families appear to experience greater difficulty while having fewer opportunities to avail themselves of quality, evidence-based treatments (EBTs). This paper will address unique aspects of community dwelling military families, barriers to care, a resiliency perspective on military child and family adjustment, emerging approaches to improve service utilization and outcomes, implementation methods that may improve practice quality and sustainability, limitations in the research base, suggestions for improved care, and a recommendation for a public health approach toward the needs of family members living across our nation’s communities.
Reserve Component Families in Communities
The deployment cycle has been characterized as three sequential, albeit overlapping, phases of predeployment, separation, and reintegration. The phases encompass a set of emotional, cognitive, and relational aspects of the deployment experience that vary according to the role of a particular family member (e.g., parent, child, and extended family), setting in which adjustment is considered (e.g., home, school, and work), service and branch, and individual and environmental characteristics (e.g., development, ethnicity, prior stress, finances, and social support (DeVoe and Ross 2012; Houston et al. 2009; Huebner et al. 2009; Tunac De Pedro et al. 2011). Each may be complicated by the nature of deployment, its rapid tempo, and recurring nature. Predeployment involves preparation for a deployment over a timespan ranging from days to months. In addition to the practical aspects of deployment, children and their service member and civilian parents prepare psychologically for the separation, its attendant worry about safety, anxiety about impending changes in family role functioning, and varied emotional reactions to the separation. Deployment involves the actual separation when family members adjust to the absence of the service member and contend with the actuality of the concerns from the earlier phase. The reintegration phase involves the return of the service member, often characterized by a new set of adjustments about family roles and responsibilities, possible changes in the psychological or physical functioning of a service member, and efforts to adapt and establish new routines of civilian life.
Although eligible, RC seldom accesses services available during their time of active duty. If they seek services at all, they likely rely on limited community resources, which usually are not equipped to address the unique needs of military families. Families of active duty service members may live off base, yet they tend to reside in proximal communities that have a strong military awareness and culture. Service members are dispersed across rural, suburban, and urban areas in roughly equal proportions (Sogomonyan and Cooper 2010, May). Postdeployment reintegration for RC families may be complicated by distance from military installations and dispersion across many communities with scant awareness of the military involvement of their citizens (Krier et al. 2011; Proctor et al. 2011). For such community dwelling military families, especially those from the National Guard or Reserve, status as a military family and possible effects of deployment may remain unknown and hidden from the larger populace.
Families and children who live far from military bases may lack military informed social support networks may struggle to find adequate, accessible mental health services should they seek care. Civilian providers often are lacking in their understanding of military culture. Therapists may not recognize the extent of stigma that service members associate with mental health services. They may lack critical knowledge elements that include differences between military and civilian culture, active and reserve components and service branches, rank structure, the psychological meaning of duty, unit cohesion, warrior culture and strength, chain of command, and a perspective on physical and psychological aspects of force readiness (Weiss and Coll 2011; Chandra et al. 2011). The obstacles to military competent mental health treatment are compounded in instances of fragmented or inaccessible public or private mental health systems.
As a result, civilian efforts toward outreach, engagement, and improving access may diverge from needs of community dwelling military families in need of assistance. Even when equipped with knowledge of military culture and attuned to barriers to care, practitioners frequently lack necessary clinical and assessment competencies to provide military and developmentally informed evidence-based treatment. Military competent service providers can, however, offset barriers when their work with families focuses on maximizing existing resources, coping skills, and resilience (Pietrzak et al. 2010).
Barriers to Effective Care
Myriad barriers constrain mental health treatment accessibility, engagement, and utilization. At best, one-third to just under half of service members and their family members seek mental health care when in need. Still fewer seek their care in traditional mental health settings and instead present to chaplains and clergy members, primary care physicians, or other professionals with whom they have a preexisting relationship. Expressed reasons for not seeking care include stigma, obstacles to career advancement if treatment were to become part of a service record, cost, inconvenience (e.g., inflexible appointment times, strict work hours), and lack of knowledge of how and where to seek assistance. Rural service members have reported more barriers to care (e.g., transportation, availability of mental health providers), negative attitudes about mental health treatment, and perception of their own needs as insufficient to warrant assistance relative to suburban and urban members. In contrast to AC members and despite low service utilization and multiple barriers, RC sometimes view mental health care in a somewhat more positive light, perhaps due to relatively less concern about negative career implications or their status in both military and civilian culture (Hoge et al. 2004).
Insurance status may be more fluid and insecure for community dwelling RC families. Tricare benefits for RC are time-limited following separation and may be restricted to the service member. Use of benefits may be stymied in remote communities where paneled providers are absent. Subsequent coverage is subject to the vagaries of employment and income status. Among families who were not affiliated with the military, parents of uninsured children reported greater unmet needs relative to parents of insured children (OR = 2.94). However, when children were enrolled in public health insurance programs, their reported need was actually lower (OR = 0.79) than for children with private health insurance (DeRigne et al. 2009). The results at first appear counterintuitive to common expectations that children from lower income backgrounds are less likely to receive sufficient quality care. Instead, they suggest that less than insurance status, benefits packages may play a crucial role, with public insurance frequently offering more generous mental health coverage.
In broad terms, barriers can be considered as environmentally or family influenced. As summarized in Table 1, environmental barriers include obstacles related to flexible appointments, inadequate transportation, or lack of military informed, affordable providers. Family influences include negative perceptions about mental health and concerns about career advancement. Treatment engagement has been related inversely to one’s belief in the importance of handling mental health problems on one’s own, an emphasis on self-reliance, and a negative perception of the mental health field (Vogt 2011).
Risk and Resilience
Theories of resilience have played a particularly strong role in conceptualizing how military families adjust to deployment. Despite variation, resilience theories and interventions highlight fairly consistent themes (Beardslee et al. 2011; Luthar et al. 2000). From a developmentally informed, biopsychosocial perspective, resilience (1) arises from environmental and genetic influences, (2) comprises multiple features that manifest differently across individuals, (3) evolves over time and may be context specific, and (4) is strengthened by prior experiences of effective coping in response to moderate stress. Resilience competencies critical to child functioning: effective coping skills, confidence and competence in successful planning and action, self-control and regulation, supportive parent, family, and community relationships, environmental advantage or adversity (e.g., socioeconomic status, social support for military activities), and how genetic vulnerabilities are expressed and modulated for different children (Betancourt and Khan 2008; Rutter 1985, 2012). As resilience and coping skills improve, children become more effective in their day-to-day lives with potential improvements in symptoms, school and interpersonal functioning, and capacity to cope with change or stress. When these competencies fail to develop or become ineffective in the face of stressors (e.g., deployment separation, posttraumatic stress, and caregiver functioning), children are at heightened risk of emotional, behavior, and interpersonal problems (Luthar et al. 2000).
From this perspective, resiliency interventions for military children and families are analogous to secondary prevention based on identified risk factors or provided subsequent to deployment-related stressors. Common techniques of resiliency interventions include child and family coping skills, problem solving, self and emotion regulation, parenting skills, attunement in the parent–child relationship, predictability in the presence of stress, social support within and beyond the family, addressing environmental advantage or disadvantage, and connection to formal and informal resources and services (Betancourt and Khan 2008; Bowen and Martin 2011; Friedberg and Brelsford 2011; Rutter 1985, 2012; Saltzman et al. 2011). As one example, children may learn and practice, within and outside of sessions, coping skills that provide accurate knowledge about deployment, opportunities to express specific deployment-related concerns, support skills for regulating anxiety and other distress, and assist with cognitive restructuring of inaccurate and maladaptive beliefs about the deployment.
Resiliency interventions offer developmentally appropriate pyschoeducation and attempt to restore a sense of meaning and predictability that has gone awry. Social support buffers youth against the disruptions of a parent’s deployment and military service, especially in the context of a responsive, military informed environment. For community dwelling military families without a close-knit, military informed community, connection to formal services (e.g., financial management, physical and mental health providers) and informal supports (e.g., faith communities, babysitters) can be critical to alleviating parents’ sense of isolation and burden. For those in rural communities, geographic isolation may potentiate this problem (Betancourt and Khan 2008; Cohen et al. 2010; Cohen and Mannarino 2011; Friedberg and Brelsford 2011; Saltzman et al. 2011). In the following section, we describe several programs and interventions to highlight the work being done to improve services for community military families. The approaches represent a combination of those that have been developed anew for military families and those that represent extensions of methods developed for civilian families. An exhaustive summary is neither our intent nor within the feasible scope of this article. Instead, we have tried to offer the reader with an appreciation of the myriad attempts to support military families.
Emerging Programs and Interventions
The state-of-the-science lags far behind the need of service and family members for well-validated interventions. Limited as the evidence may be, clinical providers in communities are increasingly interested in acquiring practice skills in EBTs, and many have recognized and responded to the needs of community dwelling military families. In recent years, access to EBTs has increased for civilian families. Access for military families, whether AC or RC, community or installation based, has not kept apace (Huebner et al. 2009; Kazdin 2011).
Efforts to redress this situation have received considerable attention among policy, practice, and research circles, including a presidential order mandating family-based responses for military families (Executive Order No. 13 2012). Some interventions have generated large clinical datasets that include standardized assessments conducted at regular intervals or are in the early stages of a randomized controlled trial (RCT). Most represent adaptations of EBTs that have been validated for civilian populations of youth who have experienced trauma. The concepts of adversity and trauma serve as intervention frameworks for assisting clinicians to support family adaptation related to military deployment. By no means should it imply that traumatic stress in the norm in response to deployment. Treatment quality may be assessed through an admixture of skill acquisition, treatment fidelity, and adaption and relevance for a specific military culture. Separately or in concert with treatment, programs attempt to improve access by expanding from facility and office-based treatment through community outreach with military provider and support systems and pyschoeducation to address the nature of deployment-related stress (Campbell et al. 2011). Fortunately, a number of interventions have the potential to address transitions and stress related to parental deployment and other aspects of military family life (Agency for Healthcare Research and Quality Effective Health Care Program 2012; Foa et al. 2009). The treatments and programmatic models highlighted herein serve as exemplars and should not be viewed as a complete catalog of available strategies.
Medical and Mental Health Colocation
Many civilian health care systems have embraced the concept of a consistent medical home that integrates or colocates behavioral health care in adult and pediatric primary care. The strategy is intended to improve access, utilization, and continuity of care, offer critical behavioral health services in a normative environment; and foster an interdisciplinary, integrative, efficient approach to care (Marshall et al. 2011; North Carolina Institute of Medicine 2011; Prinz et al. 2009; Rosenheck 2000). In early studies, service members and their families have reported a preference for receiving mental health care in a primary practice setting (Gould 2011). Some authors have emphasized graduated screening as an aspect of routine care, which at a basic level may involve inquiry about military connections as a standard aspect of care (Davis et al. 2012; Dubowitz et al. 2007; Forbes et al. 2010; Foy et al. 2010; Ward-Zimmerman and Cannata 2012). Others advocated strongly to extend beyond simple colocation to encompass care in which behavioral and medical services are well integrated (Davis et al. 2012; Dubowitz et al. 2007; Foy et al. 2010; Ward-Zimmerman and Cannata 2012).
Core Evidence-Based Techniques
With the plethora of new evidence-based and promising treatments for youth who have experienced adversity or trauma, some researchers have called for core clinical strategies or competencies that can be applied in a modular fashion as an alternative to multiple interventions designed narrowly for separate populations (Weisz et al. 2012). Friedberg and Brelsford (2011) suggest six cognitive behavioral modules (and accompanying strategies) that could assist children in adapting to a parent’s deployment: (1) pyschoeducation (e.g., online or printed materials), (2) self-monitoring (e.g., behavior logs), (3) behavioral interventions (e.g., relaxation training), (4) cognitive restructuring (e.g., altering maladaptive beliefs), (5) rational analysis (e.g., decatastrophizing), and (6) performance attainment (e.g., gradual exposure).
As in other realms, much of this work has occurred with civilian children and families; generalization to military families reflects clinical judgment rather than a decision based on empirical support. Emphasizing the complexity of implementation, practice change, and policy development, Weisz et al. (2011) have advocated forcefully for the modular approach to training and practice as consistent with the complex presentations and comorbidities among mental health clientele, and potentially yielding better outcomes and receptivity among policy makers. They randomly assigned 84 clinicians to three service provision groups: (1) modular treatment using EBT techniques, (2) standard manualized treatment, and (3) usual care. Relative to children receiving manualized treatment or usual care, those treated with the modular approach improved more rapidly and had fewer psychiatric diagnoses at the conclusion of treatment. The manualized treatment condition was not significantly different from usual care (Weisz et al. 2012). The strength of evidence is insufficient for firm conclusions in favor of the component approach.
Clinicians are faced with a dilemma of balancing the quality of existing practice with an increasing emphasis treatment using evidence-based approaches. The latter inherently involves learning a number of EBTs commensurate with one’s scope of practice. EBTs typically share theoretical elements and strategies, yet for research purposes, most studies use a specific model applied to a relatively narrowly defined population. A tendency toward flexible use of EBT strategies is reflected in a recent survey of trauma-focused cognitive behavioral therapy (TF-CBT)-trained clinicians (Allen and Johnson 2011). Sixty-six percent indicated that they regularly used TF-CBT components; thirty-four percent routinely applied the entire model. Among favored techniques were relaxation and coping skills (95 %), pyschoeducation (93 %), behavior management (87 %), cognitive restructuring (86 %), and a trauma narrative (85 %). A similar pattern of flexible application of treatment techniques had been reported among Department of Veterans Affairs clinicians (Gifford et al. 2012).
The National Center for Child Traumatic Stress developed the Core Curriculum on Childhood Trauma as a precursor or accompaniment to training in EBTs (Layne et al. 2011a). The curriculum uses case-based learning in which students apply knowledge to civilian and military vignettes. In a small pilot study, social work students significantly improved their self-efficacy in applying the curriculum over the course of training (Layne et al. 2011b).
Families Over Coming Under Stress (FOCUS) Resiliency Training
Researchers from UCLA and Harvard adapted FOCUS from existing interventions already supported through RCTs (Beardslee et al. 2007; Lester et al. 2013; Rotheram-Borus et al. 2004) as a brief, resiliency-based intervention for military families experiencing parental deployment (Beardslee et al. 2011; Saltzman et al. 2011). Consistent with secondary or tertiary prevention, FOCUS consists of an eight session manualized intervention with parent, child, and family sessions devoted to key developmental capacities of emotion recognition and regulation, awareness among family members of multiple perspectives on deployment, enhancing family strengths and coping skills, engagement of community supports and services, creation of a shared narrative about the deployment experience, and collaborative problem solving and goal setting. The sessions are organized into three, broad segments of narrative construction, parent planning, and narrative sharing and skills practice. Attention to the program’s education and skill building approach places it squarely within the context of military experience where service members routinely receive education about relevant skills.
With a strong emphasis on family engagement, providers promote access and engagement through outreach activities, including briefings for military and civilian stakeholders (e.g., base command, chaplains, unit commanders, schools) and single session skills groups. FOCUS parallels the combat and operation stress control model (Nash 2011) for conceptualizing health, risk, injury, and illness as four categories analogous to physical injury and consistent with force readiness with family functioning viewed as an important component of force readiness (See Nash et al. this issue). In addition to use with AC Marine, Naval Special Warfare, and Navy Seal families, FOCUS has been applied with preschool children, combat injured service members, Wounded Warrior Regiments, military couples, and children who have experienced medical trauma. Each adaptation retains the core resiliency model and techniques. FOCUS-CI (combat injury) begins during a service member’s admission to a military hospital and continues following discharge via telemedicine.
The press for rapid scale up precluded an initial RCT. Instead, FOCUS was implemented with a standard system of data collection for clinical decision-making and outcomes evaluation. In a pre- and postoutcomes comparison with 331 families (Lester et al. 2012), active duty and civilian parents reported significant decreases in anxiety, depression, and overall symptomatology, as well as improvements in family functioning and child prosocial behavior. Seventy percent of families completed the intervention, a rate higher than in many community mental health settings. Approximately 18 % were unable to complete due to deployment or other military directed relocations.
In another clinical sample, the authors examined follow-up effects 1 and 4 months following service completion among 280 families with an AC-deployed service member, a civilian spouse, and at least one child aged 3–18 (Lester et al. 2013). Path analysis results indicated that boys and younger children experienced greater distress relative to girls and older children, respectively. Initial child distress directly predicted positive family change. Military and civilian parent distress predicted higher session attendance, which in turn predicted positive family change. Finally, improved family functioning coincided with reduced child distress; session attendance mediated the relationship of family functioning and child distress. Albeit based on clinical administrative data, the two studies suggest that FOCUS may be an effective way to prevent and diminish family, parent, and child difficulties related to military deployment. The results thus far are limited by the lack of a comparison group and follow-up beyond 4 months postcare.
Military Informed Schools
Children of AC families may attend between six and nine different schools prior to completing high school. The majority, approximately 1.3 million, are enrolled in public school; Department of Defense schools educate approximately 87,000 students (Esqueda et al. 2012). In response to their needs, the Department of Defense and Council of State Governments developed the Interstate Compact on Educational Opportunities for Military Children (a.k.a., the Compact) in order to improve consistency and flexibility during school transfers between states (Department of Defense-State Liaison Office 2010; Military Child Education Coalition 2012). The Compact applies to families of active duty service members, veterans within a year of medical discharge or retirement, and service members who died during active duty. RC families are included only during the time they are activated.
As one of few points of universal contact, schools that are military informed have been viewed as a context in which to buffer deployment stress and promote children’s resilience (Astor 2011; Tunac De Pedro et al. 2011). Although RC families relocate less frequently than their AC counterparts, they are less likely to reside in a community attuned to the nature of military service. Ninety-three percent of RC children attend public school, and research has seldom assessed their educational needs (Atuel et al. 2011; Card et al. 2011).
The Building Capacity in Military-Connected Schools program represents a military informed school model that attends to four experiences common to military children: (1) family transitions, (2) mobility and school changes, (3) deployment, and (4) traumatic experiences (Astor et al. 2012b). A consortium of public school districts, university researchers and graduate interns, and the Department of Defense Education Activity has piloted the program in eight school districts proximal a major military base. Key strategies involve student support, availability of evidence-based treatment, resource materials for educators, graduate training for future mental health clinicians, and work toward a school-wide, military-friendly climate (Astor et al. 2012a, b). However, this model has been applied neither in school districts that lack a high concentration of service members, nor has it been studied in controlled trials.
The Military Child Education Coalition (2012) has developed a suite of workshop materials to assist military parents to become better advocates for the educational needs of their children, students to provide peer support to one another, and disseminate resources related to education, transitions, and available services. Building on the acknowledged value to mutual peer support, the Student 2 Student program educates a core team of students who then become leaders and offer guidance to other students around transitions.
Parenting Skills
The After Deployment Adaptive Parenting Tools Program (ADAPT) applies the well-validated Parent Management Training-Oregon (PMTO) intervention to enhance parenting skills, emotional regulation, and child adjustment among RC families where a parent has been deployed (Forgatch and Martinez 1999; Gewirtz et al. 2011). ADAPT conceptualizes effective parenting as a mediator between deployment-related stress and children’s adjustment. Fourteen group sessions are supplemented with Web-based, interactive scenarios to reinforce group lessons and serve as a resource in instances of missed sessions. Parents learn about the deployment cycle and acquire means to maintain family routines, support children’s coping, respond empathically to children’s anxiety and distress, reduce and ameliorate disruptions due to life transitions (e.g., school, family residence), promote agreement and consistency about parenting strategies, improve emotional regulation and stress management, and apply positive behavior management and discipline techniques. An RCT comparing ADAPT to usual services has commenced. Early analyses suggest that deployment status is associated with difficulties involving emotional regulation and inconsistent discipline (Gewirtz and Davis, in press).
An extensive body of research, including multiple RCTs, supports the efficacy and effectiveness of parent–child interaction therapy (PCIT) for improving child behavior, parent–child relationship quality, discipline practices, and reduction of physical abuse recidivism. Follow-up studies indicate the endurance of treatment outcomes for up to 6 years (Hood and Eyberg 2003; Chaffin et al. 2011). The structured, training-oriented nature of PCIT may facilitate its implementation due to commonality with service members’ training assignments to acquire a range of other skills expected for a duty assignment. As with other EBTs, dissemination and implementation of PCIT in the military context have been limited. Extension of PCIT for military families mirrors other instances of cultural adaptation where model fidelity is maintained, and context is adapted for a particular culture (Gurwitch et al. 2013; Gurwitch and Pearl 2011; Gurwitch 2010). In another example, in an adaptation for American Indian and Alaska Native families, the tenets of PCIT are presented in the context of traditional beliefs about child rearing and children’s role in the extended community (Bigfoot and Funderburk 2011).
Peer-to-Peer Outreach
Reserve component mental health needs continue to exceed service access and utilization. One result has been the growth of peer outreach programs with the hope that military-to-military engagement and support will improve receptivity and access to treatment. Programs often rely on veterans to conduct peer-to-peer outreach based on varied levels of training in outreach strategies, motivational interviewing, psychosocial support, and linkage to services. Few have collected systematic data beyond limited pilot data about self-reported change in knowledge, interactions with children, and perspectives on received services (Greden et al. 2010, 2011; Kudler and Straits-Tröster 2009). Programs developed specifically for AC service members have expanded gradually to address spouse and family concerns (e.g., Combat and Operational Stress First Aid, BATTLEMIND); again, data are lacking for the family adaptations.
Self-Directed Psychoeducation and Coping
Telemedicine and Web-based medicine offer psychoeducation about deployment-related challenges and lessen barriers related to accessibility and acceptability of treatment. Once again, most efforts target service members; several efforts to apply these modalities to children and families are underway. For example, PTSD Coach is an application designed to assist postdeployment service members who manage posttraumatic stress symptoms; a family version is under development (Veterans Administration National Center for PTSD and Department of Defense National Center for Telehealth and Technology 2011). FOCUS World educates children, parents, and families about the emotional regulation, goal setting, and communication skills of the FOCUS intervention through an interactive, secure Web format (Beardslee et al. 2011). Psychoeducation and support materials (e.g., print and downloadable information, Web-based training modules) are widely available. Popular series with family components include the Courage to Care series that includes children’s responses to deployment and effective parenting strategies (Uniformed Services University of Health Sciences Center for the Study of Traumatic Stress and Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury 2011). Sesame Workshop developed three sets of Talk, Listen, Connect video, and print materials in English and Spanish, which focus on assisting military families, whether AC or RC, to cope with deployment, grief, and divorce (Sesame Workshop 2006, 2008, 2010). Military Kids Connect offers military children and youth an online community and resources for interactive, secure communication among peers regardless to duty status and residential location (National Center for Telehealth & Technology 2012). Mobile Dad focuses on military fathers and care for their infants and young children (University of Michigan 2013). Other useful sources may include the Military Child Education Coalition, National Child Traumatic Stress Network, National Military Family Association, National Guard Family Program, and Military OneSource (Military Child Education Coalition 2012; National Guard Family Program 2012; Ohye et al. 2012; U. S. Department of Defense 2012; National Center for Child Traumatic Stress 2009). Each promotes awareness and knowledge of the challenges faced by military families contending with a fast-paced tempo of multiple combat deployments.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
With effectiveness documented through multiple randomized trials, TF-CBT for children aged three to eighteen has been identified as one of the most effective treatments for child posttraumatic stress (Chadwick Center for Children and Families 2004; Cohen 1998; Forbes et al. 2010; Goldman Fraser et al. 2013, May). Strong evidence supports its use with children who have been sexually abused (the original focus of TF-CBT), maltreated, exposed to domestic violence, and affected by traumatic grief. Its widespread dissemination for multiple populations in high, middle, and low income countries suggests its adaptability (The World Bank 2011).
Trauma-focused cognitive behavioral therapy has not been studied for effectiveness for military families. Researchers, including TF-CBT developers, have supported its likely utility for military families, particularly those experiencing traumatic grief (Cohen and Mannarino 2011; Campbell et al. 2011). Although the suggestions are based on clinical extrapolation, authors have suggested that the death of a service member and related childhood grief may be distinguished from the experiences of civilians by the deployment experience, service member death in combat or due to suicide, military protocols for death notification and return of remains, and subsequent changes in the family’s military connections (Cohen and Mannarino 2011).
Implementation Frameworks
The availability of well-established, efficacious, and promising treatments would represent a boon to mental health providers working with military families. Research has long supported that the efficacy of psychotherapy (Bergin and Garfield 1994), and more recently that structured, manualized interventions consistently yields modest effect sizes or results in more rapid resolution of clinical symptoms (Kazdin 2011; Silverman et al. 2008). Research thus far has emphasized treatment efficacy and effectiveness over implementation and sustainability (Aarons et al. 2011). One method to promote quality implementation has been characterized as “dissemination process research” (p. 1609) that illuminates contextual and organizational factors that will predict implementation quality and sustainability (Resnick and Rosenheck 2009; Rosenheck 2001). Critical requirements were extrapolated from national dissemination of VA community programs and consist of leadership and partnerships that support practice change, linkage between a new practice and existing organizational goals, fidelity monitoring over an extended time frame, and learning communities with a long-term commitment to practice improvement. Absent these qualities, implementation quality suffers, outcomes diminish, resources wane, and staff shift priorities elsewhere.
The National Implementation Research Network has developed a theoretical model of implementation that aptly differentiates intervention from its implementation (Fixsen et al. 2005). Implementation science makes clear that a treatment that is not well implemented cannot yield desired outcomes, regardless of its efficacy. Although not involving military samples, studies of implementation training highlight that clinical competence, organization change, and active leadership together drive practice change (Fixsen et al. 2011). Key learning strategies include in vivo coaching and prompt performance feedback. In contrast, traditional didactic instruction appears to have marginal influence at best (Fixsen et al. 2005; Joyce and Showers 2002).
A framework that is relevant to military culture must guide EBT implementation. For example, the COSC model, although developed for active duty Marine and Navy service members, represents a psychological health framework that is consistent with physical health and stresses force readiness. Four sequential levels involve (1) stress mastery and force readiness, (2) mild, reversible reactions to life stressors, (3) stress injuries of the mind, body or spirit that temporarily limit mission readiness, and (4) diagnosable stress illness that prevents mission readiness. Although not specific to military families, the Institute of Medicine (Springer and Phillips 2007) adapted a prevention continuum derived from public health models for managing physical illness. Intervention spans prevention, treatment, and maintenance and may be universal, selective, or indicated. At the indicated stage, treatment incorporates case identification and treatment, after which strategies focus on sustaining beneficial effects through after care, assistance to prevent symptom relapse, and rehabilitation of long-term or chronic conditions.
Implementation Strategies
Implementation collaboratives may potentiate the scope and pace of practice change by focusing on system collaboration, leadership that champions change, interactive groups of learners that participate over time, attention to quality and fidelity of implementation, and continuous, data-based feedback. Two related models have been adapted from methods used in quality improvement in medical and child welfare settings (Markiewicz et al. 2006). A Breakthrough Series Collaborative (BSC) represents a practice improvement model designed to advance quality and accomplish particular goals (e.g., military informed assessment, increased accessibility for military families) within existing practices or agencies. An expansion of the BSC involves the Learning Collaborative where the implementation approach is combined with training in a particular EBT to a high level of treatment fidelity (Ebert et al. 2012; Markiewicz et al. 2006; National Child Traumatic Stress Network 2008).
As is often the case and in the absence of military specific studies, we report on studies with civilian populations with the hope that researchers will accept the challenge of civilian to military translational research. In one of few studies to follow up on a BSC, 68 clinicians from 11 community agencies achieved high levels of fidelity in the practice of TF-CBT. Twelve months later, 463 youth had received treatment, and 96 % of the clinicians had maintained their TF-CBT practice. Eighty-four percent reported continued high levels of treatment fidelity, which was corroborated by reports from their supervisors (Ebert et al. 2012).
Breakthrough Series Collaborative for Improving Community Treatment for Military Families
The National Center for Child Traumatic Stress adapted quality improvement methodology (Schouten et al. 2008; Wilson et al. 2003) to improve the uptake, quality, and sustainability of best practices for children who have experienced adversity or trauma (Ebert et al. 2012; Markiewicz et al. 2006). The Duke Evidence-based Practice Implementation Center (EPIC) developed the Veteran Culture & Clinical Competence (V3C) Breakthrough Series Collaborative (BSC) to improve community mental health care for Veteran, Guard, and Reserve families (Welcome Back Veterans 2012). In a yearlong pilot, teams of clinicians, clinical supervisors, and senior administrators work under the guidance of faculty to develop, test, and refine short interval change strategies to increase access, utilization, and quality of military informed practice.
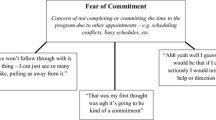
As indicated in Fig. 1, the BSC involves sequential activities designed to advance change in a particular area of practice. The method can be applied for a range of mental health issues, from quality improvement of existing services or delivery systems to implementation of EBTs to a high standard of practice fidelity. A first step for V3C was to convene an expert panel of clinical leaders, military researchers, RC service and family members, and government and community agency personnel to guide, refine, and finalize the project scope, goals, and objectives. After selection through a competitive application process, agency teams were challenged to identify gaps and barriers in their current service delivery and address them through well-supported strategies drawn from implementation science (Schouten et al. 2008; Wilson et al. 2003; Murphy et al. 2012).
Specifically, teams attended three face-to-face learning sessions, participated in intervening action periods to address implementation barriers, and utilized a virtual learning environment for mutual problem solving and peer support. In an early example, a team used a plan-do-study-act (PDSA) cycle to change their intake process to query new clientele about military service and affiliations. This revealed that 17–25 % of existing agency clientele were service members or had military affiliations. Team metrics document progress and barriers, and de-identified administrative clinical data document the intervention.
Tiered Dissemination
Once again, with the caveat that the research did not involve military families, modest evidence has supported rolling cohort and cascading dissemination methods for sustaining and spreading evidence-based interventions in domestic and foreign child welfare systems, and expert trainers gradually decrease their level of involvement and transfer responsibility for intervention, quality, and sustainability to a local team. Successful programs were those that integrated the new model into usual services and existing funding. Cascading dissemination takes similar approach of transferring responsibility from expert trainers to local providers in order to integrate the training and dissemination into local communities. This latter model involves a higher intensity and extended timeframe to training, monitoring, and consultation from model developers. In contrast to many instances that are associated with substantial decrements in intervention quality with each cohort of trainees, neither of these approaches were associated with diminished treatment outcomes (Daro and Donnelly 2002; Fixsen et al. 2005; Resnick and Rosenheck 2009; Sexton et al. 2010; Welsh et al. 2010).
Practice Scale Up
External forces can dictate the nature and pace of implementation, dissemination, and scale up (e.g., presence or absence of funds for an RCT, funder expectations for rapid implementation that alters training plans). As noted, FOCUS was launched with a demand for rapid scale across dispersed military installations, a method that favored a within subjects design relying on service-generated clinical data rather than an RCT (Beardslee et al. 2011; Lester et al. 2012). Other programs may benefit from an extended implementation timeframe that allows cohorts or BSC or LC cohorts. A well-validated or recently adapted treatment sometimes receives support to conduct an RCT, thereby blending rigorous research with tests of expected outcomes. Each could share common elements to study or promote the quality and scale of implementation, yet the methods will call for difference decisions in, for example, defining treatment populations, selecting assessment methods, and monitoring ongoing fidelity.
Recommendations
Implementation of EBTs represents a nascent field of inquiry; when considered in the context of military families living in communities, data are largely absent. Admittedly, implementation research represents a herculean effort, as does treatment outcome research, beset by myriad potential confounds and obstacles to rigorous inquiry. EBT transportability requires bridging divergent perspectives of researchers and practitioners. Otherwise, the sheer complexity of translating research from efficacy to effectiveness to implementation becomes exponentially complicated when well-specified study samples appear inconsistent with complex clinical presentations among community clientele (Sexton et al. 2010; Toth and Manly 2011). Early attention to mutual respect and valuation sets the stage for more effective partnership in which researchers and practitioners inform and enhance one another’s work and recognize areas where perceptions diverge.
Translational Research
Methodological issues warrant attention for the development of a robust scientific literature to guide effective practice with community dwelling military families. A major limitation, emphasized throughout this article, is the lack of intervention studies with military families, especially RC families. Intervention studies with civilian samples already are limited by factors that likely would be relevant to future studies with RC families: (1) few interventions are contrasted to an active treatment comparator or by independent research groups; (2) sample heterogeneity restricts generalizability of findings while sample size results in underpowered studies that may prohibit accurate conclusions; (3) attrition may be under-reported with scant information about reasons and barriers related to attrition; (4) most research has been unable to address possible mediators or moderators of outcomes; and (5) follow-up assessments are not always dictated by hypothesis about durability of effects and tend to reflect funding timelines. The implementation science field, like some others, lacks consistent, validated measures that facilitate cross-study comparison.
Translational implementation research is needed to understand how established or promising treatments can be adapted or developed to meet the pressing needs of community dwelling military families. A national research-practice network might overcome some of the extant methodological limits by allowing larger representative samples that can be assessed through common measures, applied in realistic community settings, include mediators and moderators, and identify essential and inessential aspects of training and implementation. A research-practice alliance may more effectively engage a range of potential audiences such as policy makers, other provider types and systems, and public and private funders. Running throughout is an unresolved question about whether existing interventions should be implemented in a military informed manner or interventions require extensive adaptation (or development) to be effective with military families. This question echoes the earlier mentioned tension between core treatment techniques or specific EBTs are a preferred route toward quality mental health care.
The scope of need among community dwelling military families, combined with the nascent state of implementation knowledge, calls for replacing the current ad hoc approach with one that is coordinated and integrated in order to bridge the multiple gaps that affect treatment uptake and dissemination, family access and utilization, and reliable outcomes. Implementation researchers should be charged and funded to meet the need for EBTs for community dwelling military children and families. An initiative should have a mandate to foster greater integration of research and practice, as well as collaboration among civilian, RC, and active duty providers and systems. These constituent groups should translate service delivery, research, and policy so that it is readily accessible across constituent groups. Models that address aspects of this type of initiative include the National Child Traumatic Stress Network, National Center for PTSD, and the Prevention Science and Methodology Group.
Military Knowledge, Screening/Assessment, and Treatment Competencies
Community mental health clinicians and other care providers can have a tremendous effect on the psychological and emotional well-being of RC members by becoming knowledgeable about working with service members, veterans, their families, and children. By routinely asking the question Have you—or a member of your family—ever served in the military? The clinician not only gains important information about a potentially critical mental health-related aspect of the patient’s occupational history, but signals that their practice is a military informed (Brown 2012). Perhaps unbeknownst to many practitioners, most communities are home to military families whose access to and engagement with mental health treatment can be enhanced by fostering a military-friendly practice. Despite coverage limitations for Guard and Reserve, Tricare enrollment can improve families’ access. Routine inquiry about family members who serve or have served in our military and educating oneself about available resources that might stabilize families at a critical time sends a message of interest and receptiveness, and can provide important clinical data.
Whether active or reserve component, installation or community dwelling, the US military represents a subculture with particular values and experiences that play a crucial role in force readiness, beliefs about service, and adjustment to deployment stress. As noted earlier, clinicians should acquire basic knowledge about the military and military families, including, although not limited to, service branches, rank structure, effects of deployment on service members, spouses, children, and other family members, and the extent to which a particular family views the military, or other cultures, as explanatory to their identity. Effective clinicians will acknowledge to themselves and families the limitations of their knowledge of the military environment. In a related vein, clinicians cannot assume that deployment or military service represent causal factors in distress, disorder, and treatment seeking. Instead, the military context is a crucial domain that should be considered in outreach, engagement, assessment, and treatment.
A second level of screening or assessment involves collecting information about the service member and his or her family, including children. Essential domains include symptomatology (e.g., posttraumatic stress, depression, anxiety, problem substance use), child emotional and behavior problems, individual child and adult strengths and challenges, coping skills and resiliency, and barriers to care. Clinicians will need to consider the extent to which the research literature is representative of their clientele in terms of civilian or military families, narrowly defined or multidimensional presenting problems, feasibility of delivering a particular intervention in a given community.
Unfortunately, the available literature offers little direct evidence for treatment effectiveness with community dwelling military populations and even less for the utility of implementation science as directly facilitating or achieving quality outcomes. Community implementation of services for military families seems to arise from one of three approaches: (1) direct transfer of an EBT from a civilian to military population, (2) adaptation of an existing intervention for military families, or (3) development of a new intervention, distinct from those already available. The first, direct transfer might occur when therapists who are confronted with a complex treatment need transfer an EBT or its components from civilian-to-military-oriented practice. The second has been the habitual approach, and several research groups have adapted existing EBTs. Entirely new interventions, the third approach, are exceeding rare, perhaps because of the complexity of developing a new intervention or the high degree of commonality across existing, effective interventions. Evidence that favors or disfavors these strategies is needed, especially involving military families dispersed across communities large and small.
Effective approaches to training pedagogy often are overlooked. Cost for quality training may exceed available resources. Commitment of substantial professional time involves opportunity cost decisions, for example foregoing billing revenue or decreased caseloads due to the time demand of training. We know that dissemination and implementation are most effective when they involve training to a high standard of treatment fidelity, ongoing coaching in the use of newly learned methods, consistent measurement that leads to useful, timely feedback, creation of a learning community or team, multisystem coordination (e.g., providers, service systems, policy makers, funders), proactive responses to barriers, and strategies for sustainability and spread. Incorporation of these elements is essential if we are to offer community dwelling military families quality treatment that can endure in their communities.
Practice standards will need to evolve to a point where benefits of an EBT relative to usual care are widely recognized and accepted. Provider systems will need to be accountable for use of and fidelity to EBTs, for outcomes rather than units of service, and for measurement of quality and outcome. For EBTs to be properly disseminated, implemented, and sustained, revenue streams must be reconciled with the true costs of service provision. Practitioners who are reliant on third party reimbursement have little or no financial incentive toward EBTs when potential revenue cannot meet the costs of training, consultation, foregone billable events, and the higher cost for providing EBTs relative to unstructured, open-ended treatments. One solution under consideration in many states and systems involves differential reimbursement strategies that would apply separate rates to either (1) use of EBTs, (2) submission of performance data, or (3) use outcome rather than service event-based payment.
Transition to a Public Health Model
With myriad barriers to sustained change and spread of EBTs, mental health care for community dwelling military families may improve with a transition from the longstanding disease model to a public health model (Straits-Troster et al. 2011; Defense of Defense Task Force on Mental Health 2007). For community dwelling service members and families, a public health approach fosters a continuum of services, including formal and informal supports; availability and accessibility of effective treatments in local communities, community capacity to screen and assess an array of military service-connected psychological health problems, provide appropriate EBTs, including EBTs, and expand prevention and resilience promotion for an entire community. A public health orientation engenders a thorough examination of available resources across multiple levels of care, an assessment of gaps and needs, and a strategy for solving service gaps.
Service members and their family members living in varied community settings, where RC families predominate, deserve comprehensive, effective care (EBTs) that has been well implemented and can be sustained over time. Key public health strategies should include: (1) public and provider outreach and education, (2) screening, (3) identifying risk and resilience, (4) decreasing stigma and health disparities, and (5) providing a range of effective treatments. The public health orientation should be infused with awareness and knowledge of military culture and the needs of military families. Inquiry about military service, and in some instances about deployment experiences and coping among family members, should become routine across settings. Prevention, resilience, and treatment interventions should not be restricted to tertiary care settings (e.g., mental health clinics), but occur in a range of accessible, normative settings (e.g., schools, primary care).
Conclusion
A robust public health system for military families in communities cannot exist or endure, nor can any specific EBT, without supporting public policies. Public policies that improve the availability and quality of EBTs for military families and their sustained implementation require leadership and commitment from public and private sectors: medicine, education, funders, politicians, and family stakeholders and consumers, to name a few. Mental health researchers and providers who are committed to quality care in the communities where service members and their families live have an obligation to educate others about research findings related to effective practice, their relevance and importance, and the conditions necessary for scale up and continuity over time. As Fairbank and Gerrity (p. 318) note, “The work of every scientist and clinician is linked to the world of policy, and there is not policy without politics (Fairbank and Gerrity 2007).” When this information is available and presented in an accessible manner, policy leaders are better prepared to support rules, procedures, policies, and laws that facilitate knowledge about the strengths and challenges faced by military families, effective treatment that can improve the lives of military families, and funding mechanisms that are consistent with the cost and effort required to provide EBTs. Mental health and research professionals must extend themselves beyond their traditional roles and responsibilities to understand and become comfortable operating in formal and informal political environments recognizing that with or without their input, policy makers will allocate scarce resources in the context of competing demands and diverse stakeholders and influencers.
References
Aarons, G. A., Hurlburt, M., & Horwitz, S. M. (2011). Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research, 38, 4–23.
Agency for Healthcare Research and Quality Effective Health Care Program. (2012). Grading the strength of a body of evidence when assessing health care interventions—AHRQ and the Effective Health Care Program: An Update <EPC> Evidence-based Practice Center, Contract No. <Contract Number>. (AHRQ to provide the remainder). Washington, DC: Agency for Healthcare Research and Quality.
Allen, B., & Johnson, J. C. (2011). Utilization and implementation of trauma-focused cognitive-behavioral therapy for the treatment of maltreated children. Child Maltreatment, 17, Advance online publication. doi:10.1177/1077559511418220.
Astor, R. A. (2011). The need to support students from military families. Education Week, 30(33), 32–33.
Astor, R. A., Benbenishty, R., Wong, M., & Jacobson, L. (2012a). Building capacity in military-connected schools. Los Angeles, CA: USC School of Social Work.
Astor, R. A., Jacobson, L., Benbenishty, R., Atuel, H., Gilreath, T., Wong, M., et al. (2012b). A teacher’s guide to supporting military students in the classroom. New York: Teachers College Press.
Atuel, H., Esqueda, M., & Jacobson, L. (2011). The military child within the public school education system. Los Angeles, CA: USC Center for Innovation and Research on Veterans & Military Families.
Beardslee, W., Lester, P., Klosinski, L., Saltzman, W., Woodward, K., Nash, W., et al. (2011). Family-centered preventive intervention for military families: Implications for implementation science. Prevention Science, 12, 339–348.
Beardslee, W. R., Wright, E. J., Gladstone, T. R. G., & Forbes, P. (2007). Long-term effects from a randomized trial of two public health preventive interventions for parental depression. Journal of Family Psychology, 21(4), 703–713.
Bergin, A. E., & Garfield, S. (Eds.). (1994). Handbook of psychotherapy and behavior change. Oxford, England: Wiley.
Betancourt, T. S., & Khan, K. T. (2008). The mental health of children affected by armed conflict: Protective processes and pathways to resilience. International Review of Psychiatry, 20(3), 317–328.
Bigfoot, D. S., & Funderburk, B. W. (2011). Honoring children, making relatives: The cultural translation of parent–child interaction therapy for American Indian and Alaska Native families. Journal of Psychoactive Drugs, 43(4), 309–318. doi:10.1080/02791072.2011.628924.
Bowen, G. L., Mancini, J. A., Martin, J. A., Ware, W. B., & Nelson, J. P. (2003). Promoting the adaptation of military families: An empirical test of a community practice model. Family Relations, 52(1), 33–44.
Bowen, G. L., & Martin, J. A. (2011). The resiliency model of role performance for service members, veterans, and their families: A focus on social connections and individual assets. Journal of Human Behavior in the Social Environment, 21, 162–178.
Brown, J. L. (2012). The unasked question. JAMA, 308(18), 1869–1870.
Campbell, C. L., Brown, E. J., & Okwara, L. (2011). Addressing sequelae of trauma and interpersonal violence in military children: A review of the literature and case illustration. Cognitive and Behavioral Practice, 18, 131–143.
Card, N. A., Bosch, L., Casper, D. M., Bracamonte Wiggs, C., Hawkins, S. A., Schlomer, G. L., et al. (2011). A meta-analytic review of internalizing, externalizing, and academic adjustment among children of deployed military service members. Journal of Family Psychology, 25(4), 508–520.
Chadwick Center for Children and Families. (2004). Closing the quality chasm in child abuse treatment: Identifying and disseminating best practices. San Diego, CA: Ewing Marion Kauffman Foundation.
Chaffin, M., Funderburk, B., Bard, D., Valle, L. A., & Gurwitch, R. (2011). A combined motivation and parent–child interaction therapy package reduced child welfare recidivism in a randomized dismantling field trial. Journal of Consulting and Clinical Psychology, 79(1), 84–95.
Chandra, A., Lara-Cinisomo, S., Jaycox, L. H., Tanielian, T., Burns, R. M., Ruder, T., et al. (2009). Children on the homefront: The experience of children from military families. Pediatrics, 125(1), 16–25.
Chandra, A., Lara-Cinisomo, S., Jaycox, L. H., Tanielian, T., Han, B., Burns, R. M., et al. (2011). Views from the homefront: The experiences of youth and spouses from military families. Santa Monica, CA: RAND Corporation.
Cohen, J. A. (1998). Practice parameters for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 37(10), 4S–26S.
Cohen, J. A., Berliner, L., & Mannarino, A. (2010). Trauma focused CBT for children with co-occurring trauma and behavior problems. Child Abuse and Neglect, 34, 215–224.
Cohen, J. A., & Mannarino, A. P. (2011). Trauma-focused CBT for traumatic grief in military children. Journal of Contemporary Psychotherapy, 41, 219–227.
Cozza, S. J., Guimond, J. M., McKibben, J. B. A., Chun, R. S., Arata-Maiers, T. L., Schneider, B., et al. (2010). Combat-injured service members and their families: The relationship of child distress and spouse-perceived family distress and disruption. Journal of Traumatic Stress, 23(1), 112–115.
Daro, D., & Donnelly, A. C. (2002). Charting the waves of prevention: Two steps forward, one step back. Child Abuse and Neglect, 26, 731–742.
Davis, B. E., Blaschke, G. S., & Stafford, E. M. (2012). Military children, families, and communities: Supporting those who serve. Pediatrics, 129(S3). doi:10.1542/peds.2010-3797c.
Defense of Defense Task Force on Mental Health. (2007). An achievable vision: Report of the defense of defense task force on mental health. Falls Church, VA: Defense Health Board.
Department of Defense-State Liaison Office. (2010). The interstate compact on educational opportunities for military children: An overview. Washington, DC: Author.
DeRigne, L., Porterfield, S., & Metz, S. (2009). The influence of health insurance on parent’s reports of children’s unmet mental health needs. Maternal and Child Health Journal, 13, 176–186.
DeVoe, E. R., & Ross, A. (2012). The parenting cycle of deployment. Military Medicine, 177(2), 184–190.
Dubowitz, H., Feigelman, S., Lane, W., Prescott, L., Blackman, K., Grube, L., et al. (2007). Screening for depression in an urban pediatric primary care clinic. Pediatrics, 119, 435–443.
Ebert, L., Amaya-Jackson, L., Markiewicz, J., & Fairbank, J. A. (2012). Development and application of the NCCTS learning collaborative model for the implementation of evidence-based child trauma treatment. In R. K. McHugh & D. H. Barlow (Eds.), Dissemination and implementation of evidence-based psychological interventions (pp. 97–123). New York, NY: Oxford University Press.
Esqueda, M. C., Astor, R. A., & Tunac De Pedro, K. M. (2012). A call to duty: Educational policy and school reform addressing the needs of children from military families. Educational Researcher, 41, 65–70. doi:10.3102/0013189X11432139.
Executive Order No. 13. (2012). Improving access to mental health services for veterans, service members, and military families. 77 FR 54783 (pp. 54783–54786). Washington, DC: United States Office of the Federal Register.
Fairbank, J. A., & Gerrity, E. T. (2007). Making trauma intervention principles public policy: Commentary on “Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence” by Hoffoll, Watson, et al. Psychiatry, 70(4), 316–319. doi:10.1521/psyc.2007.70.4.316.
Fixsen, D. L., Blase, K. A., & Van Dyke, M. K. (2011). Mobilizing communities for implementing evidence-based youth violence prevention programming: A commentary. American Journal of Community Psychology, 48, 133–137. doi:10.1007/s10464-010-9410-1.
Fixsen, D. L., Naoom, S. F., Blase, K. A., Friedman, R. M., & Wallace, F. (2005). Implementation research: A synthesis of the literature. (Vol. FMHI Publication #231). Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, the National Implementation Research Network.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (Eds.). (2009). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.). New York: Guilford Press.
Forbes, D., Creamer, M., Bisson, J. I., Cohen, J. A., Crow, B. E., Foa, E. B., et al. (2010). A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress, 23(5), 537–552. doi:10.1002/jts.20565.
Forgatch, M. S., & Martinez, C. R., Jr. (1999). Parent management training: A program linking basic research and practical application. Parent Management Training, 36, 923–937.
Foy, J. M., Kelleher, K. J., Laraque, D., & American Academy of Pediatrics Task Force on Mental Health. (2010). Enhancing pediatric mental health care: Strategies for preparing a primary care practice. Pediatrics, 125(S87). doi:10.1542/peds.2010-0788E.
Friedberg, R. D., & Brelsford, G. M. (2011). Using cognitive behavioral interventions to help children cope with parental military deployment. Journal of Contemporary Psychotherapy, 41, 229–236.
Fullerton, C. S., McCarroll, J. E., Feerick, M., McKibben, J., Cozza, S., Ursano, R. J., et al. (2011). Child neglect in army families: A public health perspective. Military Medicine, 176, 1432–1439.
Gewirtz, A. H., & Davis, K. L. (in press). Parenting Practices and Emotion Regulation in National Guard and Reserve Families: Early Findings from the After Deployment Adaptive Parenting Tools/ADAPT study. In S. McDermid Wadsworth (Ed.), Stress in U.S. military families. New York: Springer.
Gewirtz, A. H., Erbes, C. R., Polusny, M. A., Forgatch, M. S., & DeGarmo, D. S. (2011). Helping military families through the deployment process: Strategies to support parenting. Professional Psychology: Research and Practice, 42(1), 56–62. doi:10.1037/a0022345.
Gewirtz, A. H., Polusny, M. A., DeGarmo, D. S., Khaylis, A., & Erbes, C. R. (2010). Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology, 78(5), 599–610. doi:10.1037/a0020571.
Gibbs, D. A., Martin, S. L., Kupper, L. L., & Johnson, R. E. (2007). Child maltreatment in enlisted soldiers’ families during combat-related deployment. Journal of the American Medical Association, 298, 528–535.
Gifford, E. V., Tavakoli, S., Weingardt, K. R., Finney, J. W., Peirson, H. M., Rosen, C. S., et al. (2012). How do components of evidence-based psychological treatment cluster in practice? A survey and cluster analysis. Journal of Substance Abuse Treatment, 42, 45–55.
Goldman Fraser, J., Lloyd, S. W., Murphy, R. A., Crowson, M., Zolotar, A. J., Coker-Schwimmer, E., et al. (2013, May). A comparative effectiveness review of parenting and trauma-focused interventions for children exposed to maltreatment. Journal of Developmental & Behavioral Pediatrics. doi:10.1097/DBP.0b013e31828a7dfc.
Gorman, L. A., Blow, A. J., Ames, B. D., & Reed, P. L. (2011). National Guard families after combat: Mental health, use of mental health services, and perceived treatment barriers. Psychiatric Services, 62(1), 28–34.
Gorman, G., Eide, M., & Hisle-Gorman, E. (2010). Wartime military deployment and increased pediatric mental and behavioral health complaints. Pediatrics, 126(6), 1–9.
Gould, M. (2011). Patient preferences for the delivery of military mental health services. Military Medicine, 176, 608–612.
Greden, J., Valenstein, M., Kees, M., & Spinner, J. (2011). Military support programs and networks for our service members, veterans, and their families. Paper presented at the Welcome Back Veterans Grantee Meeting, New York, NY, November 8, 2011.
Greden, J. F., Valenstein, M., Spinner, J., Blow, A., Gorman, L. A., Dalack, G. W., et al. (2010). Buddy-to-Buddy, a citizen soldier peer support program to counteract stigma, PTSD, depression, and suicide. Annals of the New York Academy of Sciences, 1208, 90–97. doi:10.1111/j.1749-6632.2010.05719.x.
Gurwitch, R. H. (2010). Improving relationships in military families. Paper presented at the 3rd Deployment Mental Health Symposium, Pensacola, FL.
Gurwitch, R. H., Fernandez, S., Pearl, E., & Chung, G. (2013). Utilizing parent–child interaction therapy to help improve the outcome of military families. Children, Youth and Families Newsletter.
Gurwitch, R. H., & Pearl, E. (2011). Application of parent–child interaction therapy to military families. Paper presented at the 2011DoD/USDA Family Resilience Conference, Chicago, IL.
Harpaz-Rotem, I., Murphy, R. A., Rosenheck, R. A., Berkowitz, S., & Marans, S. (2007). Clinical epidemiology of urban violence: Responding to children exposed to violence in ten communities. Journal of Interpersonal Violence, 22, 1479–1490.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. doi:10.1056/NEJMoa040603.
Hood, K., & Eyberg, S. (2003). Outcomes of parent–child interaction therapy: Mother’s reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology, 32(3), 412–429.
Houston, B. J., Pfefferbaum, B., Sherman, M. D., Melson, A. G., Jeon-Slaughter, H., Brand, M. W., et al. (2009). Children of deployed national guard troops: Perceptions of parental deployment to Operation Iraqi Freedom. Psychiatric Annals, 39, 805–811.
Huebner, A. J., Mancini, J. A., Bowen, G. L., & Orthner, D. K. (2009). Shadowed by war: Building community capacity to support military families. Family Relations, 58, 216–228.
Joyce, B., & Showers, B. (2002). Student achievement through staff development. In B. Joyce & B. Showers (Eds.), Designing training and peer coaching: Our needs for learning (3rd ed.). Alexandria, VA: Association for Supervision and Curriculum Development.
Kazdin, A. E. (2011). Evidence-based treatment research: Advances, limitations, and next steps. American Psychologist, 66, 685–698.
Krier, D., Stockner, C. R., & Lasley, P. (2011). The economic and cultural impacts of veterans on rural America: The case of IOWA. Journal of Rural Social Sciences, 26(3), 57–82.
Kudler, H., & Straits-Tröster, K. (2009). Partnering in support of war zone veterans and their families. Psychiatric Annals, 39(2), 64–70. doi:10.3928/00485713-20090201-04.
Lambert, J. E., Engh, R., Hasbun, A., & Holzer, J. (2012). Impact of posttraumatic stress disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology,. doi:10.1037/a0029341.
Layne, C. M., Ghosh Ippen, C., Strand, V., Stuber, M., Abramovitz, R., Reyes, G., et al. (2011a). The core curriculum on childhood trauma: A tool for training a trauma-informed workforce. Psychological Trauma: Theory, Research, Practice, and Policy, 3(3), 243–252. doi:10.1037/a0025039.
Layne, C. M., Ghosh, C., Strand, V., Stuber, M., Abromvitz, R., Reyes, G., et al. (2011b). The core curriculum on childhood trauma: A tool for training a trauma-informed workforce. Psychological Trauma: Theory, Research, Practice, and Policy, 3(3), 243–252. doi:10.1037/a0025039.
Lester, P., Peterson, K., Reeves, J., Knauss, L., Glover, D., Mogil, C., et al. (2010). The long war and parental combat deployment: Effects on military children and at-home spouses. Journal of the American Academy of Child and Adolescent Psychiatry, 49(4), 310–320. doi:10.1097/00004583-201004000-00006.
Lester, P., Saltzman, W. R., Woodward, K., Glover, D., Leskin, G. A., Bursch, B., et al. (2012). Evaluation of a family-centered prevention intervention for military children and families facing wartime deployments. American Journal of Public Health, 102(Supplement 1), S48–S54.
Lester, P., Stein, J. A., Saltzman, W., Woodward, K., MacDermid, S. W., Milburn, N., et al. (2013). Psychological health of military children: Longitudinal evaluation of a family-centered prevention program to enhance family resilience. Military Medicine, 178, X: 1.
Luthar, S. S., Cicchetti, D., & Becker, B. (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71(3), 543–562.
Mansfield, A. J., Kaufman, J. S., Engel, C. C., & Gaynes, B. N. (2011). Deployment and mental health diagnoses among children of US Army personnel. Archives of Pediatric and Adolescent Medicine, Online supplement, E1–E7. doi:10.1001/archpediatrics.2011.123.
Markiewicz, J., Ebert, L., Ling, D., Amaya-Jackson, L., & Kisiel, C. (2006). Learning collaborative toolkit. Los Angeles, CA: National Center for Child Traumatic Stress.
Marshall, R. C., Doperak, M., Milner, M., Motsinger, C., Newton, T., Padden, M., et al. (2011). Patient-centered medical home: An emerging primary care model and the military health system. Military Medicine, 176, 1253–1259.
McNally, R. J. (2012). Are we winning the war against posttraumatic stress disorder? Science, 336, 872–874.
Military Child Education Coalition. (2012). Education of the military child in the 21st century: Current dimensions of educational experiences for Army children. Harker Heights, TX: Author.
Milliken, C. S., Auchterlonie, J. L., & Hoge, C. W. (2007). Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA, 298, 2141–2148.
Murphy, R., Amaya-Jackson, L., Fairbank, J., Goetz, K., Ake, G., Potter, D., et al. (2012). Veteran culture and clinical competencies collaborative goals framework. Durham, NC: Duke University.
Nash, W. P. (2011). U.S. Marine Corps and Navy combat and operational stress continuum model: A tool for leaders. In E. C. Ritchie (Ed.), Combat and operational behavioral health (pp. 107–119). Washington, DC: Borden Institute Textbook of Military Psychiatry.
National Center for Child Traumatic Stress. (2009). Military families knowledge bank. http://mfkb.nctsn.org/cwis/index.php. Accessed March 3, 2012.
National Center for Telehealth & Technology. (2012). MilitaryKidsConnect.org. https://www.militarykidsconnect.org. Accessed December 17, 2012.
National Child Traumatic Stress Network. (2008). Empirically supported treatments and promising practices. Accessed April 17, 2009.
National Guard Family Program. (2012). National Guard Family Program: The gateway for service members and their families. http://www.jointservicessupport.org. Accessed October 31, 2012.
North Carolina Institute of Medicine. (2011). Honoring their service: A report of the North Carolina Institute of Medicine task force on behavioral health services for the military and their families. Morrisville, NC: Author.
Ohye, B., Rauch, P., & Bostic, J. (2012). Educator toolkit to increase awareness & support to military children in schools. Boston, MA: Red Sox Foundation and Massachusetts General Hospital Home Base Program & Massachusetts Child Psychiatry Access Project.
Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., Rivers, A. J., Morgan, C., et al. (2010). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of operations enduring freedom and Iraqi Freedom: The role of resilience, unit support, and post deployment social support. Journal of Affective Disorders, 120, 188–192.
Prinz, R. J., Sanders, M. R., Shapiro, C. J., Whitaker, D. J., & Lutzker, J. R. (2009). Population-based prevention of child maltreatment: The U.S. Triple P system population trial. Prevention Science, 10, 1–13.
Proctor, S. P., Wells, T. S., Jones, K. A., Boyko, E. J., & Smith, T. C. (2011). Examination of post-service health-related quality of life among rural and urban military members of the Millennium Cohort Study. Journal of Rural Social Sciences, 26(3), 32–56.
Resnick, S. G., & Rosenheck, R. A. (2009). Scaling up the dissemination of evidence-based mental health practice to large systems and long-term time frames. Psychiatric Services, 60(5), 682–685.
Rosenheck, R. (2000). Primary care satellite clinics and improved access to general and mental health services. Health Services Research, 35(4), 777–790.
Rosenheck, R. A. (2001). Organizational process: A missing link between research and practice. Psychiatric Services, 52(12), 1607–1612.
Rotheram-Borus, M. J., Lee, M., Lin, Y. Y., & Lester, P. (2004). Six-year intervention outcomes for adolescent children of parents with the Human Immunodeficiency Virus. Archives of Pediatric and Adolescent Medicine, 158, 742–748.
Rutter, M. (1985). Resilience in the face of adversity. Protective factors and resistance to psychiatric disorder. British Journal of Psychiatry, 147, 598–611.
Rutter, M. (2012). Annual research review: Resilience: Clinical implications. Journal of Child Psychology and Psychiatry, Advance publication,. doi:10.1111/j.1469-7610.2012.02615.x.
Saltzman, W. R., Lester, P., Beardslee, W. R., Layne, C. M., Woodward, K., & Nash, W. P. (2011). Mechanisms of risk and resilience in military families: Theoretical and empirical basis of a family-focused resilience enhancement program. Clinical Child and Family Psychology Review, 14, 213–230.
Schouten, L. M., Hulscher, M. E., van Everdingen, J. J., Huijsman, R., & Grol, R. P. (2008). Evidence for the impact of quality improvement collaboratives: Systematic review. BMJ, 336(7659), 1491–1494.
Seal, K. H., Metzler, T. J., Gima, K. S., Bertenthal, D., Maguen, S., & Marmar, C. R. (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care 2002–2008. American Journal of Public Health, 99(9), 1651–1658.
Sesame Workshop. (2006). Helping families during military deployment. Talk, listen, connect. New York: Sesame Workshop.
Sesame Workshop. (2008). Deployments, homecomings, changes. Talk, listen, connect. New York: Sesame Workshop.
Sesame Workshop. (2010). When families grieve. Talk, listen, connect. New York: Sesame Workshop.
Sexton, T. L., Chamberlin, P., Landsverk, J., Ortiz, A., & Schoenwald, S. K. (2010). Action brief: Future directions in the implementation of evidence based treatment and practices in child and adolescent mental health. Administration and Policy in Mental Health and Mental Health Services Research, 37, 132–134.
Siegel, B. S., Davis, B. E., & Committee on Psychosocial Aspects of Child and Family Health and Section on Uniformed Services (2013). Health and mental health needs of children in US military families. Pediatrics. doi:10.1542/peds.2013-0940.
Silverman, W. K., Ortiz, C. D., Viswesvaran, C., Burns, B. J., Kolko, D. J., Putnam, F. W., et al. (2008). Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology, 37(1), 156–183.
Sogomonyan, F., & Cooper, J. L. (2010). Trauma faced by children of military families: What every policymaker should know. New York: Columbia University National Center for Children in Poverty.
Springer, J. F., & Phillips, J. (2007). The Institute of Medicine Framework and its implication for the advancement of prevention policy, programs and practice. Washington, DC: Institute of Medicine of the National Academies.
Straits-Troster, K., Brancu, M., Goodale, B., Pacelli, S., Wilmer, C., Simmons, E. M., et al. (2011). Developing community capacity to treat post-deployment mental health problems: A public health initiative. Psychological Trauma: Theory, Research, Practice, and Policy, 1, 1–9. doi:10.1037/a0024645.
The World Bank. (2011). World Bank Atlas Method. http://go.worldbank.org/IEH2RL06U0. Accessed November 7, 2012.
Thomas, J. L., Wilk, J. E., Riviere, L. A., McGurk, D., Castro, C. A., & Hoge, C. W. (2010). Prevalence of mental health problems and functional impairment among active component and national guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67(6), 614–623.
Toth, S. L., & Manly, J. T. (2011). Bridging research and practice: Challenges and successes in implementing evidence-based preventive intervention strategies for child maltreatment. Child Abuse and Neglect, 35, 633–636.
Tunac De Pedro, K. M., Astor, R. A., Benbenishty, R., Estrada, J., Dejoie Smith, G. R., & Esqueda, M. C. (2011). The children of military service members: Challenges, supports, and future educational research. Review of Educational Research, 81, 566–618.
U. S. Department of Defense. (2012). Military OneSource. http://www.militaryonesource.mil. Accessed October 31, 2012.
Uniformed Services University of Health Sciences Center for the Study of Traumatic Stress, & Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. (2011). The impact of invisible injuries: Helping your family and children. Courage to Care. Bethesda, MD: Uniformed Services University of Health Sciences.
United States. Health Care Financing Administration. (2004). Volume 1 of the international classification of diseases, 9th revision, clinical modification: ICD-9-CM (Vol. 4). 1978: U.S. Dept. of Health and Human Services, Public Health Service, Health Care Financing Administration.
University of Michigan. (2013). Mobile Dad. https://mobiledadapp.org/about/. Accessed May 29, 2013.
Veterans Administration National Center for PTSD, & Department of Defense National Center for Telehealth and Technology. (2011). PTSD Coach. Washington, DC: Author.
Vogt, D. (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: A review. Psychiatric Services, 62(2), 135–142.
Ward-Zimmerman, B., & Cannata, E. (2012). Partnering with primary pediatric care: Lessons learned through collaborative colocation. Professional Psychology: Research and Practice, 43(6), 596–605.
Weiss, E., & Coll, J. E. (2011). The influence of military culture and veteran worldviews on mental health treatment: Practice implications for combat veteran help-seeking and wellness. The International Journal of Health, Wellness and Society, 1(2), 75–86.
Weisz, J. R., Chorpita, B. F., Palinkas, L. A., Schoenwald, S. K., Miranda, J., Bearman, S. K., et al. (2012). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth. Archives of General Psychiatry, 69(3), Advance online publication. doi:10.1001/archgenpsychiatry.2011.147.
Weisz, J. R., Ugueto, A. M., Herren, J., Afienko, S. R., & Rutt, C. (2011). Kernels vs. ears, and other questions for a science of treatment dissemination. Clinical Psychology Science and Practice, 18(1), 41–46.
Welcome Back Veterans. (2012). Welcome Back Veterans. http://web.welcomebackveterans.org/index. Accessed November 7, 2012.
Wells, T. S., Ryan, M. A. K., Jones, K. A., Hooper, T. I., Boyko, E. J., Jacobson, I. G., et al. (2012). A comparison of mental health outcomes in persons entering U. S. military service before and after September 11, 2001. Journal of Traumatic Stress, 25, 17–24.
Welsh, B. C., Sullivan, C. J., & Olds, D. L. (2010). When early crime prevention goes to scale: A new look at the evidence. Prevention Science, 11, 115–125.
Wilson, T., Berwick, D. M., & Cleary, P. D. (2003). What do collaborative improvement projects do? Experience from seven countries. Joint Commission Journal on Quality and Safety, 29(2), 85–93.
Acknowledgments
The authors wish to thank Karen Goetz for her consultation and advice. Funding was provided by Welcome Back Veterans, an initiative of Major League Baseball, The McCormick Foundation, and The Entertainment Industries Foundation, and by the Substance Abuse and Mental Health Services Administration National Child Traumatic Stress Initiative.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Murphy, R.A., Fairbank, J.A. Implementation and Dissemination of Military Informed and Evidence-Based Interventions for Community Dwelling Military Families. Clin Child Fam Psychol Rev 16, 348–364 (2013). https://doi.org/10.1007/s10567-013-0149-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-013-0149-8