Abstract
Anxiety of childhood is a common and serious condition. The past decade has seen an increase in treatment-focussed research, with recent trials tending to give greater attention to parents in the treatment process. This review examines the efficacy of family-based cognitive behaviour therapy and attempts to delineate some of the factors that might have an impact on its efficacy. The choice and timing of outcome measure, age and gender of the child, level of parental anxiety, severity and type of child anxiety and treatment format and content are scrutinised. The main conclusions are necessarily tentative, but it seems likely that Family Cognitive Behaviour Therapy (FCBT) is superior to no treatment, and, for some outcome measures, also superior to Child Cognitive Behaviour Therapy (CCBT). Where FCBT is successful, the results are consistently maintained at follow-up. It appears that where a parent is anxious, and this is not addressed, outcomes are less good. However, for children of anxious parents, FCBT is probably more effective than CCBT. What is most clear is that large, well-designed studies, examining these factors alone and in combination, are now needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anxiety in childhood is common and serious
In recent years, there has been growing awareness of the problem that childhood anxiety presents. Epidemiological studies indicate that a sizeable proportion of the young population suffer from anxiety disorders. Even very conservative estimates (Ford, Goodman, & Meltzer, 2003) suggest that around 3% of children will have an anxiety disorder (and associated impairment) at any one time. Indeed, in a recent review, anxiety was found to be the most common psychological disorder of childhood, in most studies eclipsing both depression and behaviour disorders in its frequency (Cartwright-Hatton, McNicol, & Doubleday, 2006). Moreover, anxiety is more serious than it was once thought to be. Anxious children are at increased risk of having social and academic difficulties (Pine, 1997; Wood, 2006), are at increased risk of becoming anxious adults (Kim-Cohen et al., 2003), and are also at increased risk of developing serious secondary psychological disorder, in particular substance misuse (Kushner, Sher, & Beitman, 1990), and major depression (Kovacs, Gatsonis, Paulauskas, & Richards, 1989).
The development of treatments
Before the mid-1990s there was very little high quality treatment research investigating interventions for this population. However, the past decade has seen major developments in this field, with major trials being published every year.
The vast majority of these trials have reported on Cognitive Behaviour Therapy (CBT). The key reason for this focus on CBT has been the success that this treatment has been found to have in treating adults with a range of disorders, including anxiety (Butler, Chapman, Forman, & Beck, 2006). For pragmatic reasons, therefore, its adoption by the child field has been understandable. However, CBT with adults, even for fairly simple anxiety conditions, can be a complex affair. CBT necessarily involves the intellectual manipulation of complex verbal material, and some authors have cast doubt on the wisdom of trying to use it, without major modifications, with children (e.g. Grave & Blissett, 2004). In these early days of CBT for children, few modifications to the therapy have yet been made. Typically, anxious children work directly with a therapist, and will be required to identify and challenge their anxiogenic thoughts (albeit using simplified techniques) and they will be required to undergo difficult exposure to their feared stimuli. Given the problems that are clearly inherent in this, how successful have the early attempts at CBT with anxious children been? A systematic review of the treatment literature (Cartwright-Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004) included 10 of the first trials of CBT. This review showed that 57.5% of those children and adolescents receiving CBT recovered from their anxiety diagnosis by the end of treatment. The authors concluded that this was a somewhat disappointing result, especially when compared with the remission rate of 34.8% in the participants who were ‘wait list controls’ (i.e. who did not receive any treatment).
New developments in the treatments of child anxiety
In tandem with developments in treatment research, there has been progress in our understanding of the basic processes that drive and maintain anxiety in children. We now have a fuller understanding of the cognitive and behavioural processes that underlie early anxiety (e.g. Alfano, Beidel, & Turner, 2002) and, in particular, we are learning much about processes that may be present in the families of anxious children (Wood, McLeod, Sigman, Hwang, & Chu, 2003). Moreover, we are beginning to develop a picture of how anxiety is transmitted from parent to child (Murray, Cooper, Creswell, Schofield, & Sack, 2007). Unfortunately, many of these theoretical and basic science developments have not yet been translated into developmentally appropriate interventions for this younger population. In particular, although many treatment trials have now attempted to include the parents in treatment, to date, this has often been done in an idiosyncratic and atheoretical fashion, leading to inconsistent and confusing results.
Over the last 10 years a growing evidence base has formed to compare individual CBT administered with children to similar treatments with accompanying sessions for parents. Table I summarises features of a number of randomised controlled trials that have compared standard child-focussed CBT (henceforth CCBT) to CCBT with an added family component, or different forms of family-based CBT (henceforth FCBT). The results to date present a very mixed picture, with some studies reporting statistically significant improvements from the addition of a family component (e.g. Barrett, Dadds, & Rapee, 1996; Heyne et al., 2002; Mendlowitz et al., 1999) and others reporting no added value of FCBT over and above CCBT (e.g. Barrett, 1998; Nauta, Scholing, Emmelkamp, & Minderaa, 2003; Spence, Donovan, & Brechman-Toussaint, 2000). We will now review some of the possible explanations for the discrepant results, in order to consider how to best involve parents in treatment so that optimal therapeutic outcomes for highly anxious children might be achieved.
Inclusion Criteria
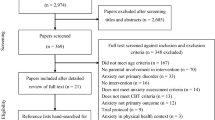
We sought to find all trials that conducted a formal randomised trial, comparing FCBT with CCBT for the treatment of childhood anxiety. Trials that exclusively treated participants with obsessive-compulsive disorder, post-traumatic stress disorder, or simple phobia were excluded on the grounds that the outcomes and clinical demands of these disorders may differ significantly from those for more typical anxiety disorders (generalised anxiety disorder, separation anxiety disorder, social phobia, agoraphobia with/out panic disorder). The following databases were searched: Medline (1950–August 2006); Psycinfo (1967–August 2006). The following search terms were used: Every combination of: Phobia / Panic / Anxious / Anxiety and Child / youth / adolescent and Trial; School refuser and trial; School refusal and trial. Where the authors were also aware of trials conducted since the publication of a case series these were also included (Bodden et al. (submitted) following Bögels & Siqueland, 2006). This yielded nine trials comparing FCBT and CCBT, which have formed the core of this review. However, in addition, we also included papers that reported a trial of FCBT, but did not carry out a formal randomised comparison of this with CCBT. Whilst these studies are not informative as to whether and in what circumstances CCBT or FCBT is more favourable, they do allow an investigation of the factors that might be associated with the success or otherwise of FCBT. This yielded a further ten papers. Most of the trials included children who met criteria for a formal anxiety diagnosis. However, two studies (Dadds, Spence, Holland, Barrett, & Laurens, 1997; Rapee, Kennedy, Ingram, Edwards, & Sweeney, 2005) also included a proportion of children who whilst severely anxious, did not meet formal criteria for a diagnosis. We took the decision to include these studies, as they are large and well-conducted, and cast considerable light on the issues in question.
Review Methods
Most of the studies discussed in this paper are very small, and their conclusions are necessarily tentative. One solution to this problem is to combine the results of these studies in a ‘meta-analysis’ (Field, 2006, submitted). However, it was decided that a meta-analysis was not appropriate at this stage in the development of the field, because of the very substantial method variance that was apparent between the papers. It would not have been possible to carry out a single meta-analysis of all studies, and instead, a number of smaller analyses, combining small groups of studies with comparable designs would have been necessary. It is likely that a formal meta-analysis, as soon as this is appropriate, will cast considerable light on some of the issues discussed in this paper.
What impacts on the success of FCBT?
How is Outcome Measured?
A range of measures are typically administered to participants before and after treatment, including: diagnostic interviews; clinician ratings of improvement; parent-report questionnaires and child-report questionnaires. Conclusions often differ depending on which outcome measure is being referred to (questionnaires, diagnostic interviews, clinician ratings of improvement, teacher reports or observational measures) so we now provide a summary of the findings, according to each of these types of outcome measure.
Questionnaire Measures
Based on child self-report questionnaire measures, a fairly consistent picture emerges in the randomised trials, in which no treatment differences (FCBT vs. CCBT) are found post-treatment across all the studies using a range of measures: Multidimensional Anxiety Scale for Children (MASC-C) (Wood, Piacentini, Southam-Gerow, Chu, & Sigman, 2006); Revised Children’s Manifest Anxiety Scale (RCMAS) (Barrett et al., 1996; Cobham, Dadds, & Spence, 1998; Heyne et al., 2002; Mendlowitz et al., 1999; Spence et al., 2000); Fear Survey Schedule for Children – Revised (FSSC-R/II) (Barrett, 1998; Barrett et al., 1996; Heyne et al., 2002); State Trait Anxiety Inventory for Children (STAIC) (Bodden, Bogels, Nauta et al., submitted; Cobham et al., 1998); Social Worries Questionnaire – Pupil version (SWQ-PU) Spence Children’s Anxiety Scale (SCAS; social phobia subscale) (Spence et al., 2000); Fear Thermometer, (Heyne et al., 2002); Screen for Child Anxiety Related Emotional Disorders (SCARED-71) and Children’s Automatic Thoughts Scale (CATS) (Bodden, Bogels et al., submitted). There were only two exceptions. First, the finding of Heyne et al. (2002) that children in the parent and teacher intervention reported significantly less ‘Fear of the Unknown’, ‘Physiological anxiety’ and ‘Worry and oversensitivity’ on these specific subscales compared to children in the ‘child treatment only’ condition in the study of school-refusing children, although as in the other studies, no differences were found on questionnaire total scores. Interestingly, in this study, child self-reports reduced the most in the condition in which the child was not involved in treatment at all. This will be discussed further below. Second, the finding that children in Barrett’s (1998) study of group CBT with family involvement gave lower fear scores on the FSSC-R than controls at the 12-month follow-up assessment (but no other time points).
The weight of evidence certainly suggests that based on child self-report questionnaires, there is no significant difference between CCBT and FCBT.
Whilst it has been suggested that perhaps child self-report questionnaires (such as the RCMAS and STAI-C) lack sufficient sensitivity to detect differences between interventions (e.g. Barrett et al., 1996; Dadds et al., 1997), more recently, specific symptom-based measures (e.g. SCARED and SCAS) as well as more idiosyncratic measures (e.g. Fear thermometer) have been developed, yet differences between interventions have still not been found. Another explanation is that young people may not be reliable reporters of change over time, which requires a consistent ‘yardstick’ against which to measure oneself. However, if this were the case, we may expect to find age-effects on pre–post differences in those studies that have particularly broad age ranges, but these have not been found (Bodden, Bogels et al., submitted). In fact, for the most part, parent-report questionnaire measures also fail to distinguish between CCBT and FCBT, again using a variety of different measures: Child Behavior Checklist Internalising Scale (CBCL-internalising) (Barrett, 1998; Barrett et al., 1996—mothers and fathers report; Bodden, Bogels et al., submitted; Cobham et al., 1998); SCARED-71(p) (Bodden, Bogels et al., submitted); State Trait Anxiety Inventory – Parents’ Version (STAIC-P) (Bodden, Bogels et al., submitted); Social Skills Questionnaire (parent) (Spence et al., 2000). There are two notable exceptions to this pattern, however. In their study of children with anxiety-based school refusal, Heyne et al (2002) reported that mothers rated a greater decrease in internalising scores on the widely used CBCL for both of the treatment conditions that involved parents and teachers, compared to the treatment involving children alone (although no differences were found based on fathers’ reports). Second, in a recent study by Wood et al. (2006) there was a faster decline (‘medium’ effect size) in parent report scores on the Multidimensional Anxiety Scale for Children – Parent Report Version (MASC(p)) following FCBT in comparison to CCBT. However, there are some notable features to the content of these studies that differentiate them from other studies, as will be discussed below.
In summary, based on both child and parent reports on questionnaire measures, the bulk of evidence fails to find significant differences between treatments with and without family components, with a few notable exceptions. Both of these methods of assessment will, however, be subject to reporter bias. For example, parent and child reports of anxiety commonly differ (e.g. Federer, Stuber, Margraf, Schneider, & Herle, 2001). Significant discrepancies can also be found between two adults’ reports on a child’s level of anxiety (e.g. mother–teacher; mother–father) and in some cases discrepancies between ratings have been found to relate to parental anxiety (e.g. Briggs-Gowan, Horwitz, Schwab-Stone, Leventhal, & Leaf, 2000; Treutler & Epkins, 2003 see below). In order to overcome this difficulty, a number of studies have also included measures that are designed to provide a more objective rating of child anxiety.
‘Objective’ Measures of Child Anxiety
To achieve more objective ratings of anxiety, data have also been gathered based on clinician and teacher reports and on observable behaviours. Diagnosis according to a structured interview is typically considered to be the ‘gold-standard’ outcome measure.
Accordingly, these data, specifically the proportion of children free of an anxiety diagnoses on completion of treatment, are presented in Table I.
Anxiety Disorder Diagnosis
Of the seven listed RCTs that compared CCBT to FCBT and provided diagnostic data following treatment, only one study reported a statistically significant difference between the number of children in each condition who were free of an anxiety disorder diagnosis following treatment (Barrett et al., 1996). However, as shown in Table I, in five of the seven studies, the pattern of results favours FCBT. Certainly, the lack of statistical significance in the majority of these studies needs to be considered in relation to the power of the given sample sizes to detect differences between treatment groups where effects would be expected to be smaller than when comparing treatment and no-treatment conditions. For example, a meta-analysis of comparisons of CBT to wait-list controls has concluded that 56% of patients are likely to be free of an anxiety diagnosis following CBT (e.g. Cartwright-Hatton et al., 2004). To detect an absolute difference between treatment conditions, with a moderate effect size (i.e. 30%) with 80% power at the 5% significance level, would require 135 patients per treatment group—a condition that is far from met by any of the trials conducted to date. It is notable that the largest RCT to be carried out to date with children with anxiety disorders (Bodden, Bogels et al., submitted) was in fact the only to find that more children were free of an anxiety diagnosis following CCBT than FCBT. Specific characteristics of the family component of this study are discussed in more detail below.
Whilst it is helpful that all the trials described above used a uniform measure (the Anxiety Disorder Interview Schedule for Children – Child/Parent Report Versions (ADIS-C/P); Silverman & Nelles, 1988) to assign diagnoses, the extent to which this is in fact an ‘objective’ measure is questionable. When using this measure, diagnoses are based on children and/or parents reporting the presence of a specified set of symptoms and a clinician awarding a severity rating (based on the child and parent interviews) over or above a given cut off value (4 out of 8) for either the child or parent report. Allocation of diagnostic status is, therefore, like questionnaire measures, based primarily on parent or child report and may be subject to bias. Furthermore, although the majority of the studies report acceptable reliability for clinician severity ratings within studies (e.g. Barrett et al., 1996; Bodden, Bogels et al., submitted; Cobham et al., 1998; Spence, Donovan, & Brechman-Toussaint, 1999; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002; Wood et al., 2006) it is not clear whether the ratings that are reported are reliable across centres or trials. An honourable exception to this is the recent study by Bodden, Bogels et al. (submitted) in which ADIS interviewers were required to establish reliable ratings with experienced interviewers from another centre, namely the Child and Adolescent Anxiety Disorder Clinic at Temple University, Philadelphia, USA.
Clinician Ratings of Improvement
Although subject to similar limitations, a number of the studies have also included clinicians’ ratings of improvement, conducted by assessors blind to the treatment condition. Barrett et al. (1996), for example, rated improvement (on a scale from 0 to 6) based on the ADIS-C/P reports and direct questions about the following dimensions: (a) clinical global impression; (b) overall functioning; (c) overall anxiety; (d) avoidant behaviours; (e) family disruption; (f) parental perceived ability to deal with the child and (g) child’s perceived ability to deal with the feared situations. At post-treatment, mean ratings were higher for the FCBT condition for clinical global impression, change of family disruption by the child’s behaviour and change in parent’s perception of their own ability to deal with their child’s behaviour. In other words, following treatment where parents were involved in treatment, those scales that relate to how parents manage the child’s anxiety improve. Over the longer term, however, these advantages seem to generalise, with superiority for FCBT for all seven of the dimensions at the 6- and 12-month follow-up assessments. In terms of the clinical significance of these findings, however, it is notable that the actual difference in mean scores for these scales was small, with means falling around 5.0 for CBT and 5.4 for FCBT. Similar findings were reported by Barrett (1998) based on the results of her CCBT or FCBT group interventions. Specifically, at post-treatment, group FCBT was superior for change in family disruption as a result of the child’s behaviour and change in the parent’s perception of their own ability to deal with the child’s behaviour; and at 12-month follow-up this was true of six out of seven of the dimensions assessed. Using a more general rating scale, Wood et al. (2006) provided ratings of the Clinical Global Impression (CGI) Improvement Scale and found that three times more children in the FCBT condition were rated as ‘completely recovered’; or ‘very much better’ by independent assessors, than in the CCBT condition, and this was a highly significant finding. In contrast, using the scales developed by Barrett et al (1996), and Cobham et al (1998), and the Global Assessment of Functioning (GAF) Scale (American Psychiatric Association, 1994), Heyne et al (2002) did not find group differences at post-treatment or follow-up assessment. Once again, we are left with a mixed set of findings, which does not seem to be fully accounted for by measurement differences.
Teacher Report
In order to attempt to overcome the difficulties inherent in child and parent report, and, as a result, clinician ratings based on parent and/or child report, an additional approach is to draw on other reporters who are in a position to observe the impact of child anxiety, for example, school personnel. The primary limitation of this method, however, is that correlations are typically low between parents, children and teachers (e.g. Federer et al., 2001) and teachers have been found to underreport emotional symptoms amongst their pupils (e.g. Youngstrom, Loeber, & Stouthamer-Loeber, 2000). It is perhaps unsurprising, therefore, that Heyne et al. (2002) found no group differences based on teacher report questionnaires administered to school teachers or counsellors.
Observational Measures
Two studies are notable for the inclusion of observational data to provide more clearly objective outcome measures. Spence et al. (2000), in their study of children with Social Phobia, used both observations of peer interactions in the classroom and playground and a clinic-based role-play to assess children’s social skills pre- and post-treatment. Although treated children showed slight improvements in assertiveness compared to the wait-list group, these differences failed to reach significance and no clear differences between treatment conditions were apparent. In contrast, Heyne et al. (2002) found a significant effect of treatment group on their school-based measure: percentage of school attendance. In this study, participants were children who were refusing school due to anxiety-related difficulties. Specifically, children in the child plus parent and teacher training group were attending school significantly more than children in the child-treatment only condition. Children in the parent and teacher training (with no child treatment) condition were also attending school more than the child treatment only group, but differences between this group and the other two groups did not reach significance.
While these are isolated sets of results that require further exploration, these studies are to be lauded for their use of objective outcome measurements that target variables specific to the objectives of the particular study.
Cost-effectiveness
To date, only one study has considered the cost-effectiveness of CBT in comparison to FCBT for the treatment of anxiety disorders (Bodden, Dirksen, Bogels et al., submitted). In this study, societal and healthcare costs were found to be comparable for CCBT and FCBT. However, the costs per anxiety-free child and costs per Quality Adjusted Life Year (QALY) favoured individual CCBT. As this study is based on data from the only study in which the pattern of results has favoured CCBT over FCBT, it will be important for other studies to assess whether these findings can be generalised.
Outcomes in the Non-comparative Trials
In the non-comparative studies of FCBT, a similar picture emerges, with outcome being dependent upon the measure that is selected. In all but one of the studies where diagnoses were used, these showed the predicted positive effects of FCBT at post-treatment. The single study that did not show a significant reduction of anxiety diagnoses as a result of FCBT (Dadds et al., 1997) was an early intervention/prevention project, which screened schoolchildren and offered FCBT to those with significantly elevated anxiety scores. Notably, significant improvements did occur at some follow up points (discussed below) and on other indices of anxiety (mostly on parent and clinician ratings of child and family functioning). The limited success of FCBT according to post-treatment diagnoses in this study may have arisen for a number of reasons: First, the families in this study were identified as part of a screening process, and had not chosen to present themselves for assistance. The motivation of the families in this study may, therefore, have been different to those in the other studies. Second, for ethical reasons, many of the children who presented the most severe difficulties during the screening process were offered individual treatment, rather than the FCBT under scrutiny, meaning that only 75% of participating children had a full anxiety diagnosis. This removal of children with the most room for improvement is likely to have impacted negatively on overall outcomes.
The majority of the non-comparative studies of FCBT, like the FCBT vs. CCBT studies, used parent and child questionnaire measures, and a number-used teacher or clinician ratings too. The response on these measures was variable. The majority of studies found no significant effect of FCBT on at least one of their measures, the exception being Rapee (2000) which showed positive outcomes of FCBT on all measures. However, in examining which instruments/indices/reporters are most and least sensitive to change in FCBT, no clear pattern is yet emerging.
With regards to observational measures, two non-comparative studies of FCBT have employed observational measures of outcome. King et al. (1998) used school attendance as an outcome measure, in their study of FCBT for school refusal. They reported that according to this indicator, outcomes for FCBT were superior to those of a control group, whereas no difference was apparent for some less objective measures (particularly those rated by children and by teachers). Rapee et al. (2005) employed five laboratory measures of behavioural inhibition (including interactions with peers, adults, acceptance of medical procedures and novel toy). Unfortunately, although the trial did result in reduction in parent-reported anxiety, these benefits did not manifest on these measures of inhibition.
When is Outcome Assessed?
The results summarised so far have all been from immediately or soon after the completion of treatment. Clearly this introduces a source of variation in the time between initial assessment and treatment completion as the length of treatment packages differs, for example, from 8 sessions (although the time period during which this took place is not specified; Heyne et al., 2002) to up to 16 sessions (Wood et al. 2006).
Where studies have included longer-term follow-up assessments, these do generally indicate that treatment effects continue to accrue after treatment completion, a process that Nauta and colleagues (2003) refer to as ‘sowing and reaping’, i.e. during treatment, skills are trained, which can be used to overcome the child’s anxiety after treatment. In the one study in which the CCBT condition performed better than FCBT (Bodden, Bogels et al., submitted) this appeared particularly to be the case for FCBT, which did not significantly differ from CCBT in terms of proportion of children who were free of an anxiety disorder diagnosis at the 3-month follow up. Other studies have reported maintenance of therapeutic outcome (e.g. Cobham et al., 1998; Spence et al., 2000) or, where gains have been made, these were fairly equivalent for participants in CCBT and FCBT conditions at 6 and 12 months (e.g. Barrett, 1998; Barrett et al. 1996). In the one study that has followed children beyond one year, Barrett et al. (2001) reported that the proportion of children that were free of an anxiety disorder diagnosis at 6-year follow-up was exactly the same for the CCBT and FCBT conditions.
A number of the non-comparative FCBT studies have also examined the maintenance of treatment effects over the longer term. In most cases, the benefits that were apparent at post-treatment were maintained, or slightly improved at 12-month follow-up (King et al., 1998; Manassis et al., 2003; Rapee, 2000; Shortt, Barrett, & Fox, 2001; Silverman et al., 1999). In the single study that did not show greater reductions in anxiety diagnoses, compared to a control group, at post-treatment (Dadds et al., 1997), significantly greater improvement for FCBT was apparent at the six-month follow up. Interestingly, this superiority of FCBT over the control group then phased in and out over the next 18 months, disappearing at 12 months, but re-emerging at 24 months, although it should be noted that not all children in this study met criteria for a full anxiety disorder at intake.
Taken as a whole, the results seem to suggest that at longer-term follow-up there is little difference in outcome for CCBT or FCBT (regardless of which performed better at post-treatment). This is not to say, however, that shorter-term treatment outcomes should not be taken in to account, as the presence of anxiety in childhood presents a clear social and emotional risk. Effective treatment of child anxiety has been found, for example, to be associated with improved school performance and school functioning (Wood et al., 2006). It makes sense, therefore, that the sooner treatment makes an impact, the more associated risks can be prevented from becoming established.
It does appear, however, that when gains are achieved using FCBT, these can be expected to persist into the short or medium term, at the very least. There is also some evidence that the treatment may have a ‘slow release’ effect, whereby benefits accrue as the child (and their parents) develop.
Who Does the Treatment Work For?
Age Effects
As shown in Table I, the majority of treatment trials have recruited children from 7 years of age (±1 year), with upper age limits ranging between 10 and 18 years. As discussed above, on the whole the studies are short on statistical power to address their main effects, so their ability to reliably detect age effects and interactions between age and treatment conditions are limited. In the majority of cases, age effects are not reported (Barrett, 1998; Heyne et al., 2002; Mendlowitz et al., 1999; Spence et al., 2000; Wood et al., 2006) although there are a few notable exceptions: Barrett et al. (1996) divided their participants into younger (7–10 years) and older (11–14 years) groups for analysis. Most striking was that for the younger group, 100% of participants were free of an anxiety disorder diagnosis post-treatment in the FCBT condition, in comparison to 55.6% in the CCBT condition. For older children, however, there was no advantage for FCBT over CCBT. The same pattern of results was found at the 12-month follow-up assessment. These findings were not, however, replicated by Bodden, Bogels et al. (submitted) or Nauta et al. (2003) who found no difference in efficacy for FCBT when comparing older and younger children. In fact, in the Bodden et al. study, CCBT was significantly more effective amongst younger (7–12 years) than older children (13–18 years).
In the studies of FCBT in comparison to wait list, a number of investigators examined the effect of age on outcome. Shortt et al. (2001) although studying a comparatively small age range (6.5–10 years) reported that age was not a moderator of treatment outcome—i.e. that the intervention was equally effective for the younger and older participants. Similarly, in their study of FCBT for 7- to 14-year-old children, Dadds et al. (1997) reported that there were no effects of age, when comparing 7–10 year olds and 11–14 year olds. A similar result was reported by Berman, Weems, Silverman, and Kurtines (2000) in their study of factors influencing FCBT outcome across a number of trials where FCBT was compared to wait list. In children aged between 6 and 17 years, age was found to have no effect on success of treatment, where success was defined as withdrawal of DSM diagnosis or ‘major reduction in severity’ of anxiety. On examination of the means from the ‘success’ and ‘failure’ groups, there was a one year age difference, with younger children doing better than the older ones. However, this difference was not statistically significant, and no firm conclusions can, therefore, be drawn. Silverman et al. (1999) also showed that age did not moderate the effects of FCBT in their sample of 6–16 year olds, when entered as a covariate into their analyses. Similar results were reported by Rapee (2000) and, finally, by Dadds et al. (1997) who found no difference comparing 7–10 year olds with 11–14 year olds. It should be noted, however, that this latter study found no significant effect of FCBT on anxiety diagnoses when compared to a control group at the immediate post-treatment assessment, and also treated a proportion of children who did not meet full criteria for an anxiety disorder.
Only one study has focussed on the needs of very young children. Rapee et al. (2005) used a parent-only intervention in an attempt to modify behavioural inhibition in children aged 36–62 months. Although the intervention did not have a substantial effect on behavioural inhibition, it was found to substantially reduce post-treatment anxiety diagnoses in those who received the treatment (although only 90% of children had diagnoses at the outset of the study), indicating that family-based CBT may be effective for young children, despite (or perhaps because of) not involving the children in treatment.
In many of the studies, the division between ‘older’ and ‘younger’ has been made at the mid-point of the sample, rather than based on a theoretical rationale, and due to the differences in the age ranges used, the definitions of ‘older’ and ‘younger’ in these studies differ markedly. It is likely that the actual age ranges considered in these analyses is of crucial importance. Certainly, the influence of significant others appears to vary with the age of the child. For example, adults tend to hold greater authority for younger children, whereas peers have increasing influence over adolescents (Rosenberg, 1979). More specifically, 9–11 year olds have been reported to depend more on parents for social support and appraisal information than on peers (Furman & Buhrmester, 1985) or teachers (Baker & Entwisle, 1987). Later relationships with parents, however, are more conflictual and less supportive, and relationships with peers become more important sources of social support (Buhrmester & Furman, 1990). The relative influence of parents and others on the development, maintenance and recovery of anxiety problems in children remains unclear. However, literature from broader areas of developmental psychology points us to more theoretically defined age groups by which to assess interactions between treatment condition and development.
Gender Effects
Again, due to limited power, only a minority of studies have considered treatment outcome in relation to child gender. Barrett et al. (1996) found no differences for male participants across treatment conditions, however more female participants were diagnosis-free following FCBT than CCBT both at post-treatment and 12-month follow-up. This result was replicated by Cobham et al. (1998) but only for those children who had a parent who also experienced high levels of anxiety. This raises another important consideration when trying to assess for whom the different treatments work best, which will be discussed in the next section.
A number of non-comparative FCBT studies have examined the role of gender in outcomes of FCBT. In all cases, no moderating influence was found (Berman et al., 2000; Dadds et al., 1997; Manassis et al., 2003; Rapee, 2000; Shortt et al., 2001; Silverman et al., 1999).
It should be noted, however, that in the majority of the studies described here, the sample sizes did not give the studies adequate power to compare the efficacy of treatments for male and female participants. An additional factor that has, thus far, been neglected, has been the moderating role of participating parents’ gender on treatment outcome. There is some evidence from one study (Bögels & Phares, submitted) that male and female parents may have a different role to play in the development and maintenance of child anxiety. If this is the case, it is possible, that they also have different roles to play in the treatment of anxiety once it is established.
Is the Parent Highly Anxious?
It is well established that there is an increased rate of anxiety disorders amongst the parents of anxious children. Specifically, anxiety disorders amongst the mothers of anxious children are significantly raised above the base rate (Last, Hersen, Kazdin, Francis, & Grubb, 1987; Last, Hersen, Kazdin, Orvaschel, & Perrin, 1991). Indeed, a recent, bottom-up, family history study found that two thirds of the mothers of children presenting for treatment of an anxiety disorder themselves had a current anxiety disorder (Cooper, Fearn, Willetts, Seabrook, & Parkinson, 2006). Furthermore, in 1977, Windheuser demonstrated that where mothers themselves were diagnosed as being highly anxious, standard behavioural treatment for child phobias worked less well than when the behavioural treatment was preceded by treatment of the mother’s fear. Similar conclusions were drawn by Cobham et al. (1998) who divided parents into ‘high’ and ‘low’ anxiety groups based on their self-report on the Spielberger State-Trait Anxiety Inventory (trait version). Where both the child and parent were anxious, efficacy of the CBT intervention was dramatically reduced (82.4% recovered where parents were not highly anxious; 38.9% where child and parent were highly anxious). As highlighted above, this effect seemed to be primarily accounted for by outcomes for female participants. The effect also seemed to be particularly apparent amongst older children (11–14 years) for whom only 20% of those with an anxious parent were diagnosis-free following CBT, compared to 86% of children with low-anxious parents. By adding four sessions of ‘Parent Anxiety Management’ (PAM), however, the number of children who were diagnosis-free following treatment increased to 76.5% for children who had a highly anxious parent.
Recently, Wood et al. (2006) and Bodden, Bogels et al. (submitted) have both included more systematic diagnostic assessments of parental anxiety using the ADIS-IV (Brown, DiNardo, & Barlow, 1994). Wood et al. (2006) failed to find an association between children’s treatment outcome and parents’ anxiety status (although caution must be maintained as diagnostic assessments were only completed on a subgroup of parents, n = 32). With a much larger sample, Bodden, Bogels et al. (submitted), like Cobham et al. (1998) however, found that when one or both parents had an anxiety disorder, successful child treatment outcome was substantially reduced. Younger children (9–12 years) were particularly negatively effected, based on questionnaire scores, if one or both parents had an anxiety disorder, whereas older children (13–17 years) improved regardless of parental anxiety levels. In contrast to Cobham et al. (1998) they did not find an advantage for FCBT where parents suffered an anxiety disorder and, in fact, more of these children fell in to the normal range on questionnaire scores of anxiety symptoms following CCBT compared to FCBT.
Several of the studies that examined FCBT without comparison to CCBT examined the moderating role of parental anxiety upon treatment outcome. Rapee (2000) measured parental anxiety using the Beck Anxiety Inventory. It was shown that fathers’ anxiety was significantly related to outcome, with a positive correlation between fathers’ and children’s anxiety at the end of treatment and at follow up. Interestingly, no effect of mothers’ anxiety was found. Similarly, Crawford and Manassis (2001) found a significant association between fathers’ pre-treatment somatising symptoms and change in child self-reported anxiety. In both the study by Crawford and Manassis and a parallel paper from Rapee’s clinic (Creswell, Schneiring, & Rapee, 2005) a reduction in maternal anxiety was reported following FCBT. Change in maternal anxiety, therefore, represents a confound in both of these studies. Indeed the findings remain entirely consistent with the proposal that maternal anxiety acts against positive child treatment outcome, unless it is addressed clinically.
In the studies by Dadds and colleagues (Dadds et al., 1997, 1999) schoolchildren were screened for anxiety symptoms, and, unless very severely effected, were offered FCBT or a wait list control. Parental anxiety (as measured by the ‘Stress, Anxiety and Depression Scale’) was found to predict ‘severity of diagnosis’ at the post-treatment assessment, but not presence or absence of a diagnosis. This effect had disappeared at the two-year follow up point. Also, the analyses took the form of regressions, employing all participants, whether they were in the treatment or the control group. Therefore, it is not clear whether the deleterious impact of parental anxiety was equally present for both untreated and treated children.
Toren et al. (2000) reported an FCBT case series in which a number of treatment-moderating factors were explored. Children who had a mother with an anxiety disorder (diagnosed using a structured clinical interview—SADS-L) showed statistically greater reductions in their anxiety, as measured by the Revised Children’s Manifest Anxiety Scale, than children who did not have a clinically anxious mother. The mean reduction for children of anxious mothers was a substantial 9.5 points, compared to less than five points for children of non-anxious parents. This seemingly anomalous finding will be discussed further below, in relation to the type of maternal anxiety disorder suffered.
In their study of outcome predictors across two FCBT trials, Berman et al. (2000) found that parental psychological functioning had a significant impact on both the child’s diagnosis and severity of symptoms, post-treatment. In particular, higher parental scores on the ‘Fear Questionnaire’ were associated with poorer outcomes, as were high obsessive-compulsive, psychoticism, depression, hostility and paranoia scores. However, these outcome predictors were stronger for families that had received individual treatment than they were for families that had taken part in a group treatment. This is an intriguing finding, and suggests that group treatment may buffer against some of the damaging effects of parental mental ill-health. This study also indicated that the effects of parental mental health (in particular self-report depression scores) were more closely associated with outcome for younger children, than for older children.
A crucial factor in interpreting these findings is the nature of the family component that is delivered. There seem to be two ways in which parental anxiety could interfere with the child’s response to treatment. First, there is evidence to suggest that parental anxiety is associated with patterns of parenting that are themselves anxiogenic (Murray et al., 2007); so, an anxious mother’s expressed fear and avoidance of feared stimuli, for example, could militate against a treatment aimed at promoting her child’s approach of feared stimuli, or similarly, an anxious mother’s over-controlling parenting style could militate against a treatment aimed at promoting her child’s autonomy. In the study by Cobham et al. (1998) the family intervention aimed to isolate one component of other family programmes, namely PAM. Despite the positive effect on child treatment outcome, however, no reduction was found in parental self-reported trait anxiety following this intervention (in fact, the positive child outcome effect was found despite the fact that in some cases the parent who received PAM was not the anxious parent in the family). A key aspect of the PAM intervention was psychoeducation and it is possible that (rather than actually changing parent anxiety) this intervention increased parents’ sense of responsibility for change by alerting them to the role of parental anxiety in the development and maintenance of child anxiety, promoting parents to act in a less ‘anxiogenic manner’ around the child. This explanation may also account for the lack of an effect of parental anxiety in the study by Wood et al. (2006). In this study, parental anxiety was not addressed specifically, but instead, those parental behaviours that have been consistently found to be associated with child anxiety were targeted, i.e. high levels of intrusiveness, low levels of autonomy granting, and the frequent failure to model a solution-focussed approach to problems (e.g. Rapee, 1997; Wood et al., 2003). By changing these parental behaviours, the intervention may have effectively ‘trumped’ the potential negative effect of parental anxiety on child outcome. Whilst Bodden, Bogels et al. (submitted) included sessions aimed at modifying problematic family interactions and promote modelling of courageous behaviour, it is not clear whether this consistently involved specifically targeting anxiogenic parenting characteristics relating to intrusiveness and autonomy granting.
Second, family treatments commonly require the mother to provide support and encouragement for children’s exposure to feared stimuli (Dadds & Barrett, 2001) and the mother’s own anxiety may interfere with this requirement. According to this suggestion, it would be likely that different types of parental anxiety problems would create different degrees of interference with child outcome. For example, a mother with social phobia may well experience difficulties in encouraging her socially anxious child to engage in more social activities, whereas a mother with GAD may not show such clearly observable anxiety and avoidance. A recent study by Cooper et al. (submitted) provides tentative evidence for this suggestion. In this case series of children treated for anxiety disorders, in contrast to children whose mothers had GAD who did as well in treatment as children whose mothers were free from anxiety, children of mothers with social phobia responded particularly poorly. Similarly, the study by Toren et al. (2000) found that the children of the clinically anxious mothers (all but one of whom had GAD) showed more improvement after FCBT than those who did not have an anxious mother.
In summary, the balance of evidence seems to support the suggestion that parental anxiety militates against optimal treatment outcomes. Additional interventions may be useful in overcoming this. However, whether it is parental anxiety that needs to be targeted, or specific parenting behaviours that may be exacerbated by parental anxiety has yet to be established. To the authors’ knowledge, this has not been systematically examined in the anxiety literature. However, Crawford and Manassis (2001) provide evidence that family dysfunction and frustration predicted child treatment outcome. Furthermore there is evidence from other quarters that where parental mental health is associated with poor child outcomes, this relationship is mediated, in large part, by deficits in parenting (Berg-Nielsen, Vikan, & Dahl, 2002). This suggests that targeting either the parental mental illness, or modifying the parenting behaviour might have a positive impact on the child.
What Type of Anxiety Problem is the Child Experiencing?
With the exception of three studies, all of the studies summarised in Table I recruited children with a range of anxiety disorders. In most studies, these included a principal diagnosis of Separation Anxiety Disorder, Social Phobia, Overanxious Disorder (where DSM-III or earlier was used) and Generalised Anxiety Disorder. In some cases, principal diagnoses of Agoraphobia with or without Panic Disorder and Specific Phobias were also included. Where it has been examined, the FCBT/CCBT comparison trials have concluded that there is no difference in outcome according to child diagnosis (Barrett et al., 1996), although these studies have not been amongst those to include, for example, specific phobias as principal diagnoses. Certainly, a lack of difference for treatment outcomes for different anxiety disorders would be surprising given the substantial differences in therapeutic input provided for the different disorders in adult treatment programmes, the extreme example being successful treatments of specific phobias being conducted in single-sessions (e.g. Ost, 1996).
FCBT and CCBT have, however, been compared for two specific anxiety diagnoses: Social Phobia (Spence et al., 2000) and anxiety-based School Refusal (Heyne et al., 2002). For Social Phobia, the authors concluded that there was a non-significant trend towards superior results when parents were involved in treatment (although the differences were fairly substantial and arguably clinically significant). In contrast, for School Refusal, the attendance and adjustment of children who received parent and teacher training was equivalent, whether or not the children were involved in treatment.
In the non-comparative FCBT trials, a number of attempts have been made to examine the relationship of child’s type of diagnosis to the outcome of treatment. However, in the majority of cases (perhaps due to lack of power) no impact of type of diagnosis has been found (Berman et al., 2000; Shortt et al., 2001). However, in their comparison on FCBT and wait list for a range of childhood anxiety disorders, Manassis et al. (2003) reported that, according to mothers’ reports, there was more improvement for children with a diagnosis of GAD than for those with specific phobias (including separation anxiety disorder).
Who participates in treatment will be subject to further discussion below. However, the available evidence suggests that future studies need to consider the specific role that family factors may play in relation to the development and maintenance of specific disorders. A recent demonstration of this specificity has been given by Murray et al. (2007) who found that mothers with social phobia differed from mothers with GAD and control mothers in their encouragement of their infants’ interaction with a friendly stranger, and that this was significantly associated with the infants’ subsequent response to the stranger.
How severe is the child’s anxiety disorder?
In addition to the type of anxiety disorder, it may also be important to consider the level of anxiety severity the child experiences. Whilst studies have generally found that severity of child anxiety disorder is associated with treatment outcome for both CCBT (e.g. Southam-Gerow, Kendall, & Weersing, 2001) and FCBT (Dadds et al., 1997; Rapee, 2000), the non-comparative trial of FCBT by Dadds et al. (1997) showed that whether the child’s anxiety was at diagnosable, or only at sub-clinical levels, did not impact on outcome. Whether severity is an indicator of which type of treatment is most effective, has not been established. Studies are certainly likely to differ in terms of their severity and complexity, with some studies representing clinical referrals only (e.g. Bodden, Bogels et al., submitted; Mendlowitz et al., 1999) and others including self-referrals from community (e.g. Barrett, 1998; Barrett et al., 1996; Cobham et al., 1998; Nauta et al., 2003; Spence et al., 2000) or school-based (e.g. Wood et al., 2006) advertisements. Uniformity in measures used and methods of establishing reliability across centres will help clarify this situation, but it is notable that the one study that clearly states that participants were referrals to specialist mental health services and provide diagnostic data report by far the lowest levels of efficacy from FCBT (Bodden et al., submitted), perhaps reflecting the complexity of family circumstances of children referred to specialist mental health services.
Comorbidity
None of the controlled trials of CBT/FCBT have examined the effect of comorbidity on outcomes. However, some data (albeit mixed in its findings) is present in the non-comparative studies of FCBT. Specifically, in examining the effects of comorbidity in their trial of FCBT, Manassis et al. (2003) showed that when scores on the Social Anxiety Scale for children were considered, the most socially anxious children did better in individual treatment than they did in group treatment. It is notable that, these children were also found to be more anxious generally, and more depressed than the less socially anxious children, which may have accounted for these results. Certainly, Berman et al. (2000) showed that, whilst number and type of diagnoses was not associated with outcome, comorbid diagnosis of depression was, with depressed children fairing less well than those who were not depressed. Although the very small number of children who qualified for a diagnosis of depression made this comparison tentative, it was also shown that children’s self-report of depression symptoms on the Children’s Depression Inventory was associated with outcome, with high scorers recovering less often. Similarly, having high self-report trait anxiety, as measured by the Spielberger Children’s Anxiety Inventory was associated with poorer outcomes.
What does the treatment comprise?
Treatment Format—Group vs. Individual
Just one study has directly compared group and individual FCBT. Manassis et al. (2003) gave parents and children 12 sessions each, delivered in either group or individual format, for a range of anxiety disorders. The results indicated that, in general, differences between the conditions were minimal. However, there was an indication that clinician ratings of outcome were superior in the individual treatment, although the overall size of this difference between the two groups was rather small. Similarly, there may have been a slight benefit of individual treatment for children who had high social anxiety scores (although see above for an alternative interpretation of these results). Other data also suggest no advantage of either method of delivery. Although not directly comparing individual and group delivery, two studies by Paula Barrett and colleagues (Barrett, 1998; Barrett et al., 1996) used a very similar treatment package, delivered in one trial individually, and in the other in group format, and found a similar pattern of results, with an advantage for FCBT (albeit not statistically significant) in the case of Barrett (1998).
Although not directly comparing group and individual treatments, Berman et al. (2000) were able to compare the efficacy of these two approaches, in the treatment of a range of anxiety disorders across two related trials. They found that there was no significant difference in successful outcome in the two formats on any of their outcomes.
As we have discussed, the majority of studies have compared CBT conducted with the child, to a similar treatment with the addition of parent sessions. However, a small number of studies have now suggested that involving the child may not necessarily add to efficacy and conducting sessions with parents alone may be equally beneficial. For example, Heyne et al. (2002) reported equivalent improvements amongst school refusers in their Parent and Teacher Training conditions, regardless of whether the child also received treatment. Similarly, on measures of anxiety and depression, Mendlowitz et al. (1999) found no difference between child only, parent only and parent and child group conditions. Intriguing results have also been reported by Lyneham and Rapee (2005) who did not find significant differences between their FCBT treatment (comprising 10 sessions of parents and children attending parallel groups) and a bibliotherapy condition in which parents were provided with a book about managing their child’s anxiety with only five accompanying parent sessions.
As CBT comes from a tradition of individual work it is not surprising that this approach has been the default position in RCTs for child anxiety to date. However, there are a number of factors that suggest that, particularly when working with younger children, doing the bulk of the work with parents may be preferable. Certainly for younger children, the primary influences on anxious affect have been argued to be observation of others (e.g. de Rosnay, Cooper, Tsigaras, & Murray, 2006; Gerull & Rapee, 2002) fear information from others (e.g. Field & Lawson, 2003), expectations of others (Creswell, Brewin, & O’Connor, 2006) and associated parent–child interaction behaviours (e.g. Wood et al., 2003). One recent study has indicated that treatment directed entirely towards parents can be efficacious in the treatment of young anxious children. Rapee et al. (2005) identified young children (up to 62 months in age) who scored highly on measures of behavioural inhibition (90% also met criteria for an anxiety diagnosis). Their parents were offered six group sessions focussing on psychoeducation, management of the child’s anxiety symptoms, cognitive restructuring of parents’ own worries and principles of exposure. At the end of treatment, there was a reduction in anxiety diagnoses in both the intervention and the control group, which was slightly but significantly greater for the intervention group.
In addition, by working with parents to help them to overcome their child’s anxiety problems, therapists are able to promote the parents’ sense of control over their child’s mood and behaviour, both of which have been found to be associated with parents’ perceptions of their child’s anxiety (Wheatcroft & Creswell, in press); and counterproductive parental behaviours (e.g. Bugental & Johnston, 2000). This approach may also have the added advantages of facilitating parents to incorporate the strategies learned more widely in to the child’s lifestyle, reducing stigma on the child due to having to attend mental health services, and instead increasing the amount of time the child spends in age-appropriate surroundings (e.g. school rather than mental health clinics).
Examining a wider literature, it is clear that treatments for other childhood disorders, in particular those characterised by behaviour problems, and particularly those in younger children, are now heavily directed towards parents, in preference to treating the child directly. Both short- and long-term results for these approaches have been highly encouraging (e.g. Webster-Stratton, Hollinsworth, & Kolpacoff, 1989), and there is now evidence that even unmodified behavioural parenting interventions, such as the Webster-Stratton ‘Incredible Years’ Programme, may have substantial impacts on internalising as well as externalising symptoms (Cartwright-Hatton, McNally, White, & Verduyn, 2005).
Treatment Dosage
It is notable that the amount of treatment that families and/or children have received varies markedly across the trials (see Table I). Whilst the majority of trials include 12 sessions for children (60–120 min) and 12 sessions for parents (Barrett, 1998; Barrett et al., 1996; Mendlowitz et al., 1999; Spence et al., 2000), others have had from 8 sessions (Heyne et al., 2002) to a maximum of 16 sessions for both children and parents (Wood et al., 2006). Typically the number of child and parent sessions is equal, except for a few instances, for example the family CBT provided by Bodden et al. (submitted) involved 3 sessions for the child alone, 2 for the child and parent, 5 for the parents alone and 3 for the whole family. In this instance it could be suggested that a lack of continuity with specific family members may have diluted the effects of family treatment. However, the amount of therapist input per se does not appear to be clearly associated with therapeutic outcome, as illustrated dramatically by Nauta et al. (2003) who found no difference in the number of participants who were diagnosis-free following a family intervention with seven more sessions.
In the non-comparative trials, there is even greater variance in the dosage that families have received, and the amount of this that was ‘family’ CBT. The length of overall treatment varied from 6 sessions of 90 min (Rapee et al., 2005) to 24 sessions of 90 min (Manassis et al., 2002), with the amount of dedicated ‘family’ input varying from 3 session of 1 h (Dadds et al., 1997) to 12 sessions of 90 min (Manassis et al., 2002). In examining these data (which are outlined in Table I), there is some small indication that the dosage might partially account for the level of success achieved by the end of the trial. The two studies that had least impact on their primary outcome measures (Dadds et al., 1997; Rapee et al., 2005) were the two trials with the smallest amount of dedicated ‘family’ input (3 sessions of 60 min; and 6 sessions of 90 min, respectively). However, it should be noted that these two trials are distinguishable in other ways from the other studies (see above and below for details) and, therefore, the brevity of their interventions is likely to be no more than a partial explanation for their outcomes.
Content of Treatment
In the vast majority of studies, CCBT has been delivered based closely on the Coping Cat treatment package developed by Kendall and colleagues (Kendall & Hedtke, 2006), with varying degrees of abbreviation from 10 to 16 sessions. The content of FCBT, (across both the comparative and non-comparative trials) however, has not followed a standard approach. In some treatment packages, the parent sessions have been devised to parallel the CCBT programme closely (e.g. Mendlowitz et al., 1999; Silverman et al., 1999; Toren et al., 2000) with the primary aim of providing parents with the necessary information to facilitate their children in putting the programme in to practice. In others, parents are, in addition, explicitly given coaching in behaviour management (e.g. Dadds et al., 1997; Heyne et al., 2002; King et al., 1998; Rapee, 2000); managing their own emotions and modelling positive responses to anxiety (e.g. Barrett, 1998; Barrett et al., 1996; Bodden, Bogels et al., submitted; Cobham et al., 1998; Dadds et al., 1997; Heyne et al., 2002; Rapee, 2000; Shortt et al., 2001; Spence et al., 2000); modifying dysfunctional parents’ cognitions (e.g. Bodden, Bogels et al., submitted; King et al., 1998; Nauta et al., 2003); and improving family communication (e.g. Barrett, 1998; Barrett et al., 1996; Bodden, Bogels et al., submitted; Shortt et al., 2001). Because of the tendency for interventions to include a range of strategies, we currently lack any information about which components of the treatment are necessary and sufficient. An important exception to this is Cobham’s (1998) study, in which PAM was delivered as an isolated family treatment component, with notable success for families in which a parent also experienced high levels of anxiety.
What is most striking about these varied approaches is the common lack of explicit reference to developmental models of anxiety, which typically emphasise parental intrusiveness (e.g. Chorpita & Barlow, 1998; Ginsburg & Schlossberg, 2002; Hudson & Rapee, 2004; Rubin & Mills, 1991), in the selection and sequence of family intervention strategies. Parental intrusiveness refers to a tendency for parents to take over tasks at the expense of the child performing them independently. This is hypothesised to preclude children’s opportunities to develop competence in novel situations, restricting the development of cognitions associated with self-efficacy and confidence and, thereby, creating a risk for the development or maintenance of anxiety disorders (e.g. Chorpita & Barlow, 1998; Rubin & Mills, 1991). A number of well-conducted studies have now supported an association between parental intrusiveness and child anxiety (see Wood et al., 2003). Recently, however, Wood et al. (2006) have developed a family intervention based specifically on theory and research relating to these anxiogenic parenting styles (e.g. Rapee, 1997; Wood et al., 2003) to target parental intrusiveness and autonomy-granting by, for example, teaching parents to give children choices rather than making decisions for them, and allowing children to learn by trial and error. This study demonstrated an additional benefit of FCBT over and above CCBT, based on independent ratings of improvement and change in parents’ ratings of anxiety, although the results were comparable to other trials that have not had such specific targets. This begs the question, clearly, of whether the different treatments are associated with specific changes in family processes or more generic treatment effects (e.g. from parents feeling supported by engagement in treatment). To date there is a lack of reported evidence about processes of change in FCBT for anxious children. As reported above, despite a focus on parent anxiety management, Cobham et al. (1998) did not find a reduction in parental anxiety following treatment, yet found a significant advantage from including this component in terms of child anxiety outcome. This study was limited, however, by reliance on a general measure of parental trait anxiety (STAI: Spielberger, 1983) which may have lacked the sensitivity to detect change as a result of the intervention. Using a more clinically oriented measure (BAI: Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), Creswell, Schniering, and Rapee (2005) did find a significant reduction in maternal anxiety following FCBT. In this study, children’s and mothers’ threat interpretations were also assessed based on responses to ambiguous scenarios, and reductions in both children’s and their mothers’ anxious interpretation was found post-treatment. The authors argued that a change in maternal anxious cognitions may be of particular significance as a stronger association was found between parent and child anxious cognitions compared to parent and child anxiety more generally. This is consistent with the finding of Barrett et al. (1996) that children in the FCBT condition had lower scores post-treatment on threat interpretation in comparison with both the CCBT and waitlist conditions. There were no differences, however, between avoidant responses selected by children, in response to ambiguous scenarios, following CCBT or FCBT, suggesting that the effective inclusion of families in treatment may act, at least in part, through changing parental influences on children’s developing anxious cognitions. Whether this is a result of changes in parental behaviours (for example, by promoting autonomy and allowing children to challenge threat-related cognitions) remains to be investigated.
Conclusions and future directions
This overview of the extant literature has allowed us to draw few firm conclusions. It seems very likely that FCBT, in most cases, is better than nothing. However, it is less clear that it is significantly better or worse than CCBT alone. When FCBT has been found to have substantially different outcomes than CCBT, this has been for a restricted set of outcome measures only, although notably, when examining the gold standard outcome (i.e. diagnosis), as can be seen in Table I, there is a trend towards superiority for FCBT.
We have learnt that the positive results of FCBT, when seen at post-treatment assessment, are generally maintained or even improved at follow up. However, with a few notable exceptions, follow up has been for just 12 months. It is important that these studies continue to follow up their treated samples, in order that the efficacy of FCBT over the longer term may be established.
To our surprise, we have learnt very little about the relative efficacy of FCBT for older and for younger children. It seems sensible to hypothesise that FCBT might have more impact on younger children who are under greater influence from their family than older children and adolescents. However, this review was unable to confirm or disconfirm this most basic of hypotheses. The majority of studies did not attempt to compare the efficacy of FCBT for older and younger participants. In those studies that did, differences were rarely found, but it was not clear whether this was an accurate finding, or an artefact of low power in the studies. Only one study attempted to treat very young children (Rapee et al., 2005) but this study did not compare FCBT and CCBT (and not all children met criteria for an anxiety disorder) so although the results were promising, it is difficult to draw any firm conclusions about the necessity of the parental component. We hope that future studies will be powered in order that they might examine the utility of FCBT with respect to the age of the child, and that the whole range of childhood and adolescence might be considered.
The gender of the child, and indeed of the parent is, we hypothesise, likely to moderate the impact of FCBT. However, very few studies have examined this factor, and those that have, have generally been underpowered to do so. It is to be hoped that future studies will take this simple factor into account. However, we must also bear in mind that the finding that different treatments are indicated for boys and girls could be politically difficult, and it will always be necessary to consider the needs of the individual child. This will also be the case (perhaps even more so) if different interventions are indicated for the mother and the father and it will be essential to identify whether gender effects are accounted for by the individual’s parental role (i.e. who is the primary caretaker) or, for example, social learning effects relating to a mis/match between parent and child gender (e.g. Bandura, 1969).
The conclusions that may be drawn regarding the interaction of FCBT and parental anxiety upon outcome are much richer, though still somewhat confusing. We can probably conclude, with some degree of confidence, that where a parent is anxious and this is not addressed, outcome for the child is also likely to be worse. There is also some indication that where a parent is anxious, FCBT might be more beneficial to the child than CCBT, particularly if the child is pre-adolescent. Whether it is parental anxiety per se or associated cognitive (e.g. Wheatcroft & Creswell, in press) or behavioural (e.g. Murray et al., 2007) features of the parent–child relationship that need to be addressed within treatment requires systematic evaluation. We perhaps also need to pay more attention to the role of severity of child anxiety, other comorbid conditions and the child’s and the parent’s specific diagnosis. There is some emerging evidence to suggest that these have an impact on the efficacy of FCBT, but as yet, no clear conclusions are possible.
Finally, one of the difficulties in this review has been the lack of homogeneity in the FCBT that has been examined. Although this has naturally arisen in an attempt to explore and manipulate many of the factors that are thought to impact on children’s anxiety, it is far from clear what components are necessary and we now need a far more systematic approach, examining the additive effects of specific treatment components. Furthermore developmental models of anxiety (e.g. Chorpita & Barlow, 1998; Ginsburg & Schlossberg, 2002; Hudson & Rapee, 2004; Rubin & Mills, 1991) now exist which have been supported by emerging research over the last decade. The development of treatment trials in accordance with these models, and incorporating measures of change in cognitive, behavioural and family processes, offers us both benefits to clinical practice and to our scientific understanding of how environmental processes contribute to the maintenance of child anxiety disorder.
New Developments in Treatment Research
In concluding this review it seems fitting to mention, in addition to the trials described in this paper, a number of promising new developments in the treatment of childhood anxiety. In particular, a number of groups have attempted to incorporate the family into treatment in ways dictated by the theories of the development and maintenance of anxiety. One example is a recent case series, providing parent-only training for 12 families of young anxious children (aged 3–8 years) (Cartwright-Hatton, McNally, & White, 2005). In this study, parents received a modified behavioural parenting skills training programme, in which they were encouraged to engage in relationship building activities with their child (including a play technique in which control is handed to the child), to use standard, mild, consistent, behavioural techniques to encourage compliant and confident behaviour in their children, and were taught techniques for managing worry and fear. The results of the pilot study were promising, and a randomised controlled trial of this intervention is now underway.
Other promising family-based interventions that are in the early stages of development include ‘parent–child interaction therapy’ (PCIT—Choate, Pincus, Eyberg, & Barlow, 2005), and ‘Modular CBT’ (Chorpita, Taylor, Francis, Moffitt, & Austin, 2004). PCIT was initially designed as a technique for helping individual parents to manage their children’s oppositional behaviour. However, since it focuses on the interaction between the parent and child, and is thought to foster a sense of control in the child, the authors reasoned that it might be a useful intervention for younger children with separation anxiety. The results of a small case series supported this hypothesis. A similar approach, emphasising the parent–child interaction with a specific emphasis on anxiogenic parental cognitions and behaviours, has recently been piloted with children with mixed anxiety disorders and their primary caregiver with promising results (Creswell, Murray, Singhal, Willetts & Cooper, in submission).
Modular CBT (e.g. Chorpita, 2006) has also recently been developed to provide a more bespoke intervention for anxious children, whilst maintaining the integrity of a manual-based CBT. Children (and where necessary) their parents, are delivered a selection from 13 therapy ‘modules’, including a number of core modules that all cases receive. These modules are derived from well-validated manuals for the treatment of anxiety in adults and children, and the decision regarding which modules a child/family should receive is based on a formalised flowchart assessing their needs. An initial case series of seven children reported encouraging results (Chorpita et al., 2004). These novel approaches now warrant systematic investigation.
Future Research
In order to tease apart the many potential moderating factors and the complex interactions between them, much larger studies are now needed. These studies will need to employ multiple comparisons, manipulated or controlled across many cells. In so doing, we would like to strongly encourage researchers in the field to employ measures which can be used for direct comparison with existing trials but also to gather outcome data from multiple informants and from observational measures (see e.g. Heyne et al., 2002; Spence et al., 2000). On that basis, once a substantial number of trials employing similar methodology (and making similar comparisons) are available, a meta-analysis of their results would be appropriate and informative. Moreover, in order to refine the (still somewhat basic) theoretical understanding on which many of these interventions are predicated, future trials need to carefully measure the cognitive, behavioural and family processes that they are attempting to manipulate, and examine their mediating role in any improvement that is seen in children’s anxiety
References
Alfano C. A., Beidel D. C., Turner S. M. (2002). Cognition in childhood anxiety: Conceptual, methodological and developmental issues. Clinical Psychology Review, 22, 1209–1238
Baker, D. P., Entwisle, D. (1987). The influence of mothers on the academic expectations of young children. Social Forces, 65, 670–694.
Bandura A. (1969). Social learning of moral judgements. Journal of Personality and Social Psychology, 11, 275–279
Barrett P. M. (1998). Evaluation of cognitive-behavioral group treatments for childhood anxiety disorders. Journal of Clinical Child Psychology, 27(4), 459–468
Barrett P. M., Dadds M. R., Rapee R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342
Barrett, P. M., Duffy, A. L., Dadds, M. R., & Rapee, R. M. (2001). Cognitive-behavioral treatment of anxiety disorders in children: Long term (6 year) follow-up. Journal of Consulting and Clinical Psychology, 69(1), 135–141.
Beck, A. T., Ward C. H., Mendelson M., Mock J. E., Erbaugh J. K. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571
Berg-Nielsen T. S., Vikan A., Dahl A. A. (2002). Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical Child Psychology and Psychiatry, 7(4), 1359–1045
Berman S. L., Weems C. F., Silverman W. K., Kurtines W. M. (2000). Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy, 31, 713–731
Bodden, D. H. M., Bogels, S. M., Nauta, M. H., de Haan, E., Ringrose, J., Appelboom, C., et al. (submitted). Efficacy of individual versus family cognitive behavioural therapy in clinically anxious youth
Bodden, D. H. M., Dirksen, C. D., Bogels, S. M., Appelboom, C., Appelboom-Geerts, K. C. M. M. J., Brinkman, A. G., et al. (submitted). Cost and cost-effectiveness of family CBT versus individual CBT in clinically anxious children
Bögels, S. M., & Phares, V. (submitted). The role of the father in the etiology, prevention and treatment of child anxiety: A review and new model
Bögels S. M., Siqueland L. (2006). Family cognitive behavior therapy for children and adolescents with clinical anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45(2), 134–141
Briggs-Gowan M., Horwitz S., Schwab-Stone M. E., Leventhal J., Leaf P. (2000). Mental health in pediatric settings: Distribution of disorders and factors related to service use. Journal of the American Academy of Child & Adolescent Psychiatry, 39(7), 841–849
Brown, T. A., DiNardo P. A., Barlow D. H. (1994). Anxiety disorders interview schedule for DSM-IV. New York: Graywind
Bugental, D. B., Johnston C. (2000). Parental and child cognitions in the context of the family. Annual Review of Psychology, 51, 315–344
Buhrmester, D., Furman, W. (1990). Perceptions of sibling relationships during middle childhood and adolescence. Child Development, 61, 1387–1398
Butler A. C., Chapman J. E., Forman E. M., Beck A. T. (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26(1), 17–31
Cartwright-Hatton S., McNally D., White C. (2005). A new cognitive behavioural parenting intervention for families of young anxious children: A pilot study. Behavioural & Cognitive Psychotherapy, 33(2), 243–248
Cartwright-Hatton S., McNally D., White C., Verduyn C. (2005). Parenting skills training: An effective intervention for internalising symptoms in younger children? Journal of Child and Adolescent Psychiatric Nursing, 18(2), 45–52
Cartwright-Hatton S., McNicol K., Doubleday E. (2006). Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review, 26(7), 817–833
Cartwright-Hatton S., Roberts C., Chitsabesan P., Fothergill C., Harrington R. (2004). Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. British Journal of Clinical Psychology, 43, 421–436
Choate M. L., Pincus D. B., Eyberg S. M., Barlow D. H. (2005). Parent-child interaction therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice, 12, 126–135
Chorpita, B. F. (2006). Modular cogntive-behavioral therapy for childhood anxiety disorders. Guilford Press
Chorpita, B. F., Barlow, D. H. (1998). The development of anxiety: the role of control in the early environment. Psychological Bulletin, 124(1), 3–21
Chorpita, B. F., Taylor A. A., Francis S. E., Moffitt C., Austin A. A. (2004). Efficacy of modular cognitive behavior therapy for childhood anxiety disorders. Behaviour Therapy, 35, 263–287
Cobham, V. E., Dadds M. R., Spence S. H. (1998). The role of parental anxiety in the treatment of childhood anxiety. Journal of Consulting and Clinical Psychology, 66(6), 893–905
Cooper P. J., Fearn V., Willetts L., Seabrook H., Parkinson M. (2006). Affective disorders in the parents of anxious children. Journal of Affective Disorders, 93(1–3), 205–212
Cooper, P. J., Gallop, C., Willetts, L., & Creswell, C. (submitted). Treatment response in child anxiety is differentially related to the form of maternal anxiety disorder
Crawford A. M., Manassis K. (2001). Familial predictors of treatment outcome in childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 40(10), 1182–1189
Creswell C., Brewin C., O’Connor T. (2006). A longitudinal investigation of maternal and child ‘anxious cognitions’. Cognitive Therapy and Research, 30(2), 135–147
Creswell, C., Schniering C. A., Rapee R. M. (2005). Threat interpretation in anxious children and their mothers: Comparison with nonclinical children and the effects of treatment. Behaviour Research and Therapy, 43, 1375–1381
Dadds, M. R., Barrett P. M. (2001). Psychological management of anxiety disorders in childhood. Journal of Child Psychology and Psychiatry, 42(8), 999–1011
Dadds M. R., Holland D. E., Spence S. H., Laurens K. R., Mullins M., Barrett P. M. (1999). Early intervention and prevention of anxiety disorders in children: Results at 2-year follow-up. Journal of Consulting and Clinical Psychology, 67(1), 145–150
Dadds M. R., Spence S. H., Holland D. E., Barrett P. M., Laurens K. R. (1997). Prevention and early intervention for anxiety disorders: A controlled trial. Journal of Consulting and Clinical Psychology, 65(4), 627–635
de Rosnay M., Cooper P. J., Tsigaras N., Murray L. (2006). Transmission of social anxiety from mother to infant: An experimental study using a social referencing paradigm. Behaviour Research and Therapy, 44(8), 1165–1175
Federer M., Stuber S., Margraf J., Schneider S., Herle J. (2001). Self report of child anxiety and rating by parents and teachers. Zeitschrift fur Differentialle und Diagnostische Psychologie, 22(3), 194–205
Field, A. P. (2006 submitted). How to do a meta-analysis
Field A. P., Lawson J. (2003). Fear information and the development of fears during childhood: Effects on implicit fear responses and behavioural avoidance. Behaviour Research and Therapy, 41, 1277–1293
Ford, T., Goodman R., Meltzer H. (2003). The British Child and Adolescent Mental Health Survey: The prevalence of DSM-IV disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 42(10), 1203–1211
Furman, W., Buhrmester, D. (1985). Children's perceptions of the qualities of sibling relationships. Child Development, 56, 448-461
Gerull F. C., Rapee R. M. (2002). Mother knows best: Effects of maternal modelling on the acquisition of fear and avoidance behaviour in toddlers. Behaviour Research and Therapy, 40, 279–287
Ginsburg G. S., Schlossberg M. C. (2002). Family based treatment of childhood anxiety disorders. International Review of Psychiatry, 42, 1203–1211
Grave J., Blissett J. (2004). Is cognitive behavior therapy developmentally appropriate for young children? A critical review of the evidence. Clinical Psychology Review, 24(4), 399–420
Heyne D., King N. J., Tonge B. J., Rollings S., Young D., Pritchard M., et al. (2002). Evaluation of child therapy and caregiver training in the treatment of school refusal. Journal of the American Academy of Child & Adolescent Psychiatry, 41(6), 687–695
Hudson J. L., Rapee R. M. (2004). From anxious temperament to disorder: An etiological model of Generalized Anxiety Disorder. In R. G. Heimberg, C. L. Turk, D. S. Mennin (Eds.), Generalized anxiety disorder: Advances in research and practice (pp 51–74). New York: Guilford Press
Kendall, P. C., & Hedtke, K. A. (2006). Coping cat workbook. Workbook Publishing Inc
Kim-Cohen J., Caspi A., Moffitt T. E., Harrington H., Milne B. J., Poulton R. (2003). Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry, 60(7), 709–717
King N. J., Tonge B. J., Heyne D., Pritchard M., Rollings S., Young D., et al. (1998). Cognitive-behavioral treatment of school refusing children: A controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 37(4), 395–403
Kovacs M., Gatsonis C., Paulauskas S., Richards C. (1989). Depressive disorders in childhood. IV. A longitudinal study of comorbidity with and risk for anxiety disorders. Archives of General Psychiatry, 46, 776–782
Kushner M., Sher K., Beitman B. (1990). The relation between alcohol problems and anxiety disorders. American Journal of Psychiatry, 147(6), 685–695
Last C. G., Hersen M., Kazdin A. E., Francis G., Grubb H. J. (1987). Psychiatric illness in the mothers of anxious children. American Journal of Psychiatry, 144, 1580–1583
Last C. G., Hersen M., Kazdin A. E., Orvaschel H., Perrin S. (1991). Anxiety disorders in children and their families. Archives of General Psychiatry, 48, 928–936
Lyneham, H. J., Rapee, R. M. (2005). Evaulation of therapist supported parent-implemented CBT for anxiety disorders in rural children. Behaviour Reserach and Therapy, 44(9), 287–300
Manassis K., Mendlowitz S. L., Scapillato D. C., Avery D. C., Fiksenbaum L., Freire M., et al. (2002). Group and individual cognitive-behavioral therapy for childhood anxiety disorders: A randomized trial. [Article]. Journal of the American Academy of Child & Adolescent Psychiatry, 41(12), 1423–1430
Manassis K., Mendlowitz S. L., Scapillato D., Avery D., Fiksenbaum L., Freire M., et al. (2003). Group and individual cognitive-behavioral therapy for childhood anxiety disorders: A randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 41(12), 1423–1430
Mendlowitz S. L., Manassis K., Bradley S., Scapillato D., Miezitis S., Shaw B. F. (1999). Cognitive-behavioral group treatment in childhood anxiety disorders: The role of parental involvement. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1223–1229
Murray L., Cooper P., Creswell C., Schofield E., Sack C. (2007). The effects of maternal social phobia on mother-infant interactions and infant social responsiveness. Journal of Child Psychology and Psychiatry, 48(1), 45–52
Nauta M. H., Scholing A., Emmelkamp P. M. G., & Minderaa R. B. (2003). Cognitive-behavioral therapy for children with anxiety disorders in a clinical setting: No additional effect of a cognitive parent training. Journal of the American Academy of Child & Adolescent Psychiatry, 42(11), 1270–1278
Ost L. (1996). One-session group treatment of spider phobia. Behaviour Research and Therapy, 34, 707–715
Pine D. S. (1997). Childhood anxiety disorders. Current Opinion in Pediatrics, 9, 329–339
Rapee R. M. (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17(1), 47–67
Rapee R. M. (2000). Group treatment of children with anxiety disorders: Outcome and predictors of treatment response. Australian Journal of Psychology, 52(3), 125–129
Rapee R. M., Kennedy S., Ingram M., Edwards S., Sweeney L. (2005). Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting & Clinical Psychology, 73(3), 488–497
Rosenberg, M. (1979). Conceiving the self. New York: Basic
Rubin, K. H., Mills, R. S. L. (1991). Conceptualizing pathways to internalizing disorders in childhood. Canadian Journal of Behavioral Science, 23(3), 300–317
Shortt A. L., Barrett P. M., Fox, T. L. (2001). Evaluating the FRIENDS Program: A cognitive-behavioral group treatment for anxious children and their parents. Journal of Clinical Child Psychology, 30(4), 525–535
Silverman W. K., Kurtines W. M., Ginsburg G. S., Weems C. F., White Lumpkin P., Hicks Carmichael D. H. (1999). Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67(6), 995–1003
Silverman W. K., Nelles W. B. (1988). The anxiety disorders interview schedule for children. Journal of the American Academy of Child and Adolescent Psychiatry, 27(6), 772–778
Southam-Gerow M. A., Kendall P. C., Weersing V. R. (2001). Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology, 30(3), 422–436
Spence S. H., Donovan C., Brechman-Toussaint M. (1999) Social skills, social outcomes, and cognitive features of childhood social phobia. Journal of Abnormal Psychology, 108(2), 211–221
Spence S. H., Donovan C., Brechman-Toussaint M. (2000). The treatment of childhood social phobia: The effectiveness of a social skills training based, cognitive-behavioural intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry, 41(6), 713–726
Spielberger C. D. (1983). State-trait anxiety inventory. Palo Alto, CA: Consulting Psychologist’s Press
Toren P., Wolmer L., Rosental B., Elder S., Koren S., Lask M., et al. (2000). Case series: Brief parent-child group therapy for childhood anxiety disorders using a manual-based cognitive-behavioral technique. Journal of the American Academy of Child and Adolescent Psychiatry, 39(10), 1309–1312
Treutler C. M., Epkins C. C. (2003). Are discrepancies among child, mother, and father reports on children’s behavior related to parents’ psychological symptoms and aspects of parent-child relationships? Journal of Abnormal Child Psychology, 31(1), 13–27
Webster-Stratton C., Hollinsworth T., Kolpacoff M. (1989). The long term effectiveness and clinical significance of three cost-effective training programs for families with conduct-problem children. Journal of Clinical Child Psychology, 57(4), 550–553
Wheatcroft, R., & Creswell, C. (in press). Parental cognitions and expectations of their preschool children: The contribution of parental anxiety and child anxiety. British Journal of Developmental Psychology
Windheuser H. J. (1977). Anxious mothers as models for coping with anxiety. Behavior Analysis and Modification, 2(1), 39–58
Wood J. (2006). Effect of anxiety reduction on children’s school performance and social adjustment. Developmental Psychology, 42(2), 345–349
Wood J., McLeod B. D., Sigman M., Hwang W.-C., Chu B. C. (2003). Parenting and childhood anxiety: Theory, empirical findings and future directions. Journal of Child Psychology & Psychiatry & Allied Disciplines, 44(1), 134–151
Wood J., Piacentini J., Bergman R. L., McCracken J., Barrios V. (2002). Concurrent validity of the anxiety disorders section of the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolescent Psychology, 31(3), 335–342
Wood J. J., Piacentini J. C., Southam-Gerow M., Chu B. C., Sigman M. (2006). Family cognitive behavioral therapy for child anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 45(3), 314–321
Youngstrom E., Loeber R., Stouthamer-Loeber M. (2000). Patterns and correlates of agreement between parent, teacher and male adolescent ratings of externalising and internalising problems. Journal of Consulting and Clinical Psychology, 68(6), 1038–1050
Acknowledgements
Sam Cartwright-Hatton was supported by MRC clinician scientist fellowship G108/604 during the preparation of this manuscript. The authors are grateful to two anonymous reviewers for their helpful comments on an earlier draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Creswell, C., Cartwright-Hatton, S. Family Treatment of Child Anxiety: Outcomes, Limitations and Future Directions. Clin Child Fam Psychol Rev 10, 232–252 (2007). https://doi.org/10.1007/s10567-007-0019-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-007-0019-3