Abstract
Age-related macular degeneration as one of the most common causes of worldwide vision loss needs a proper approach for treatment. Therein, cell therapy and regenerative medicine can hold a great promise to be an effective approach. Accordingly, some preclinical and clinical studies were conducted to search around the therapeutic influence of stem cells in Age-related macular degeneration models and subjects. Hereupon, the purpose of the current review is to discuss the mechanisms of age-related macular degeneration, appropriate animal models along with suitable dosage and route of stem cell administration for its treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The macula luteal (an oval-formed pigmented zone near the center of the eye retina) can participate in the central, high-resolution, and color vision. Macular degeneration is a disorder in which macula luteal deteriorates and results in the reduction or loss of central visual acuity. Different types of macular degeneration are including age-related macular degeneration (AMD), juvenile macular degeneration, and Stargardt’s disease (Bressler et al. 1988; Nowak 2006; de Jong et al. 2020). While a group of conditions can lead to macular degeneration, aging is the most common causes. Accordingly, AMD is a serious threat to the vision of older than 50 years of subjects (Veritti et al. 2012). Therefore, the evaluation of appropriate approaches to early diagnose and treatment is very worthwhile. In recent decades, the rationale of cell therapy and regenerative medicine for promoting tissue repair and treatment of different disease including AMD has been proven(Goodarzi et al. 2014, 2015; Soleimani et al. 2016, Goodarzi et al. 2018, Singh and MacLaren 2018; Waugh et al. 2018; Goodarzi et al. 2019; Larijani, Goodarzi et al. 2019). However, many uncertainties in conducting clinical trials such as the most suitable route and dosage of administration have existed. Herein, some preclinical investigations have also been prepared on the therapeutic application of stem cells (Djulbegovic 2007; Parekkadan and Milwid 2010; Isasi et al. 2016; Krause et al. 2019). For preclinical investigations, selection of the appropriate animal model and performing detailed molecular tests are necessary (Council 2006; Denayer et al. 2014; Goodarzi et al. 2019; Larijani et al. 2019). On the other hand, it is helpful to evaluate the mechanism of disease to prepare detailed molecular tests (Darbre and Darbre 1988). Since, current review aims to summarize the points about the AMD and its mechanisms along with consideration of the cell therapy importance through the evaluation of pre-clinical and clinical studies.
Age-related macular degeneration: symptoms, causes, and treatments
AMD as the common cause of poor vision in the elderly people of the industrialized countries is a multifactorial late-onset disorder (Swaroop et al. 2009; Villegas et al. 2017). Although the etiology of AMD is unknown, combination of hereditary (such as specific gene polymorphisms, lighter eye color and etc.) and non-hereditary factors (including over-exposure to sunlight, life style, drug side effects, aging and etc.) are considered as AMD risk factors. With regards to the growing old population in most part of the world, it is expected that the number of AMDs will be increased in the coming years. In this regard, a study has predicted the prevalence of AMDs will be reached to 196 million and 11 million of them will have severe visual difficulties by 2020 (Moore et al. 2017).
Two forms of macular degeneration are recognized: dry (non-neovascular) and wet (neovascular). While the wet form is more serious, fortunately the dry form is more common (Hussain and Ciulla 2017). Pathophysiology of dry (or geographic atrophy) form is reducing blood supply to macula which can be diagnosed by drusen deposits in and around the macula (Moore et al. 2017). Hereupon, abnormal overgrowth of choroidal blood vessels beneath the retina leads to the wet form of macular degeneration. Studies have shown the abnormal presence of vascular endothelial growth factor (VEGF) has more prominent role in vascular overgrowth than other factors such as angiopoietin, endothelin, and activin in the wet form (Semeraro et al. 2013; Campochiaro et al. 2016). While the available treatment agents for dry form are only preventive, the wet form has the food and drug administration (FDA)-approved treatments. Subsequently, anti-VEGF agents are the most common treatments of neovascularization form of macular degeneration (Table 1). Despite the various available treatments, presence of several complications such as different alternative angiogenic factors and pathways, local and systemic side effects of anti-VEGF intra-ocular injections, tolerance to common drugs in some patients, and financial difficulties lead to the need of new methods and treatments (Cabral et al. 2017; Hussain and Ciulla 2017). Recently, stem cell therapy as a pioneering method in regenerative medicine develops a promising therapeutics for disorders including macular degeneration (Goodarzi et al. 2019).
Mechanisms of age: related macular degeneration
AMD is known as a multifactorial disease in which multiple environmental, biological, and genetic factors are involved (Fig. 1). Better understanding of these risk factors and their mechanisms will help to develop novel effective treatment regimens.
Environmental factors
AMD is associated with different environmental risk factors including smoking (one of the strong risk factors as known inducer of oxidative stress), life style, diet include low omega3 fatty acids and antioxidants such as lutein and zeaxanthin, heavy alcohol intake, increase body mass index (BMI), over exposure to sunlight, increase the occurrence risk of AMD (Allikmets et al. 1997; Chong et al. 2008; Cano et al. 2010; Huang et al. 2014). There are evidences of association between hypertension and cardiovascular disease and AMD (Al-Zamil and Yassin 2017). However, more investigations are required to elucidate these and other new risk factors.
Cellular and molecular factors
Aging as a biological process affects the cells through different ways and these cellular and molecular alterations lead to age-related diseases such as AMD (Larijani et al. 2019). Studies have shown the accumulation of cholesterol, lipofuscin, and drusen deposits in various ocular layers increases as individuals get older. Subsequently, disordered protein metabolism, mitochondrial dysfunction and A2E increase in lipofuscins in aging process impair the normal apoptosis and activate the inflammatory response (Swaroop et al. 2009). In this regard, Ambati et al. has been reported that the mice deficient in monocyte chemoattractant protein-2 (CCL-2) and C–C chemokine receptor-2 (CCR-2) have shown some AMD characteristics through macrophage dysfunction which leads to accumulation the lipofuscin and drusen in the retina (Ambati et al. 2003). Generally, the different genetic variants are related to AMD. Among different relevant genes association of the complement factor H (CFH), CFB, and ARMS2/HTRA1 variants are more investigated. (Swaroop et al. 2009). Also, hepatic lipase (LIPC) is one of the main enzymes in the metabolism of triglycerides which its gene variants association with AMD has been studied (Seddon et al. 2010). A body of literatures have reported the relation between the increased levels of tissue inhibitor of metalloproeinase-3 (TIMP-3) and Immediate Early Response-3 (IER-3) and AMD (Vazquez-Chona et al. 2005; Strunnikova et al. 2010; Anand et al. 2016). Although there are other new unknown molecules and genes that further studies will indicate.
The importance of cell therapy in age: related macular degeneration treatment
Nowadays, new advancements in medicine especially breakthroughs in cell therapy help optimize the treatments of incurable diseases such as Parkinson, Alzheimer, and AMD (Goodarzi et al. 2019; Larijani et al. 2019). According to the ability of self-renewal and differentiation potential toward multiple lineages stem cells become a promising therapeutic choice in cell therapy. Various types of stem cells including embryonic stem cells (ESCs), adult stem cells, and induced Pluripotent Stem Cells (iPSCs) are identified (Öner 2018). Retinal cell transplantation as a promising therapeutic method in ophthalmology benefit a lot from stem cells. Herein, cell therapy provides limitless source of undifferentiated cells for cell transplantation. Furthermore, mesenchymal stem cells (MSCs) derived from different sources such as bone marrow and adipose tissue, ESCs, and iPSCs are the common studied stem cells in retinal degenerative diseases (Siqueira 2011; Guan et al. 2013; Sugitani et al. 2013; He et al. 2014; Tsuruma et al. 2014; Jian et al. 2015). Though some of these stem cells are more studied in macular cell therapies and they will be discussed subsequently.
Gold standard cell type for treatment of age: related macular degeneration
Retinal pigment epithelium (RPE) cells as the most common target of cell therapy is one type of the cells damaged in retinal degenerative diseases. Different stem cells transplantation which differentiated into the RPE cells are studied in preclinical and clinical trials (Fox et al. 2014; Zarbin et al. 2019). Though, nowadays RPE and retinal progenitor cell (RPC) derived from ESCs and PSCs become the favorite sources for retinal cell therapy (Stern and Temple 2011; Buchholz et al. 2013; Leach and Clegg 2015; Nazari et al. 2015). Preclinical and clinical studies are applied these stem cells derived from various methods, with different cell amounts, and route of delivery.
Animal models for cell therapy in age: related macular degeneration
Until now, different animal models have been designed based on AMD genetic and environmental causative factors which can mimic the pathological features of disease. But generally, designing and selecting the most appropriate model for AMD is challenging because of the complexity of these factors (Zeiss 2010). Hereupon, the most appropriate animal model is an inexpensive, accessible model which is able to exhibit histological and functional changes and has a short-term growth and developmental period (Held 1983; Rabadán-Diehl and Nathanielsz 2013; Goodarzi et al. 2019). Accordingly, different animal models were used for AMD (Table 2).
Clinical trials
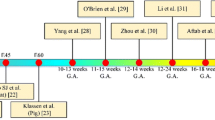
As discussed above, different stem cell sources are studied in vitro and in vivo in retinal degenerative disorders. However, clinical studies are demanded to translate the preclinical breakthrough into clinics. In this regard, some clinical trials are conducted to investigate the effectiveness of the cell therapy for ocular diseases. Two phase I/II, open-label, and nonrandomized clinical trials have shown the safety, tolerability, and efficacy of the Human Embryonic Stem Cell Derived Retinal Pigmented Epithelial (hESC-RPE) cells in patients with Stargardt’s Macular Dystrophy (SMD) and advanced dry AMD respectively in the United Kingdom and U.S. Accordingly, other trials are ongoing in transplantation of hESC-RPE cells in such cases (Schwartz et al. 2015; Schwartz et al. 2016; da Cruz et al. 2018). Also, there are some registered clinical trials in using MSCs derived from bone marrow and umbilical cord in treating the AMD or retinitis pigmentosa (RP). Another clinical trial in the United States has used an encapsulated RPE cell line in AMD or RP and Usher Syndrome patients. Results have shown the efficacy of the secreting neurotrophic factors from these cell lines for preservation (Jones et al. 2017). In addition, telomerase-mediated cell and gene therapy have been reviewed for the prevention of the RPE cell function devaluation during aging (Rowe-Rendleman and Glickman 2004; Immonen et al. 2009; Liu et al. 2019). However, still there is no FDA-approved stem cell therapy for macular degeneration and further trials and studies are required.
Route of cell administration
There are two common cellular delivery systems in retinal cell therapy: cell suspension and cellular sheets. Cell suspension including seeded cells on special substrates which inserted into the eye. In the second method, scaffolds provide a monolayer cell sheets implanted in the eye. Hu, Liu et al. has carried out an animal study to discuss the privilege of the second method. The scaffolds of the second method provide the cellular viability and stability, efficient cellular function and differentiation regulation, less migratory possibility, and effective cellular transplantation. (Lu et al. 2001; Schwartz et al. 2012; Aziz et al. 2019).
Conclusion and the future emerging landscape
Due to the emotional and economic burden of AMD along with the potential dangers related to vision problems, stem cell-based therapies considered as a very promising treatment approach. Accordingly, multiple types of stem cells were investigated to regenerate atrophic or damaged retinal tissue. However, applying stem cell-based therapeutic products are still needed preclinical investigations to support their innovative therapeutic effects (MacPherson and Kimmelman 2019; Riva and Petrini 2019). Indeed, preclinical studies can help to select the appropriate cell type, dosage, and administration methods for treatment. One of the most common parts of the preclinical studies involves the use of animal models. Considering that the use of animals in scientific research is highly controversial, it is better to use alternative methods based on the 3Rs (Replacement, Reduction, and Refinement) principles including the novel in vitro and computational in silico methods(Goodarzi et al. 2019; Hubrecht and Carter 2019; Larijani et al. 2019). On the other hand, the systemic biology approaches can be used for developing modern treatments designed for prevention(Schleidgen et al. 2017) and helping the AMD cure by evaluating AMD underlying mechanisms. It is generally hoped that all of these approaches will be effective in the road of treatment.
Abbreviations
- AMD:
-
Age-related macular degeneration
- VEGF:
-
Vascular endothelial growth factor
- FDA:
-
Food and drug administration
- BMI:
-
Body mass index
- CCL-2:
-
Chemoattractant protein-2
- CCR-2:
-
C-C chemokine receptor-2
- LIPC:
-
Hepatic lipase
- TIMP-3:
-
Tissue inhibitor of metalloproeinase-3
- IER-3:
-
Immediate early response-3
- ESCs:
-
Embryonic stem cells
- iPSCs:
-
induced pluripotent stem cells
- MSCs:
-
Mesenchymal stem cells
- RPE:
-
Retinal pigment epithelium
- RPC:
-
Retinal progenitor cell
- hESC-RPE:
-
Human embryonic stem cell derived retinal pigmented epithelial
- SMD:
-
Stargardt’s macular dystrophy
- RP:
-
Retinal pigment
References
Allikmets R, Shroyer NF, Singh N, Seddon JM, Lewis RA, Bernstein PS, Peiffer A, Zabriskie NA, Li Y, Hutchinson A (1997) Mutation of the Stargardt disease gene (ABCR) in age-related macular degeneration. Science 277(5333):1805–1807
Al-Zamil WM, Yassin SA (2017) Recent developments in age-related macular degeneration: a review. Clin Interv Aging 12:1313
Ambati J, Anand A, Fernandez S, Sakurai E, Lynn BC, Kuziel WA, Rollins BJ, Ambati BK (2003) An animal model of age-related macular degeneration in senescent Ccl-2-or Ccr-2-deficient mice. Nat Med 9(11):1390
Anand A, Sharma K, Sharma SK, Singh R, Sharma NK, Prasad K (2016) AMD genetics in India: the missing links. Front Aging Neurosci 8:115
Aziz K, Zarbin MA, Singh MS (2019) Clinical trials of retinal cell therapy. In: Zarbin MA, Singh MS, Casaroli-Marano RP (eds) Cell-based therapy for degenerative retinal disease. Springer, Berlin, pp 245–265
Bennis A, Gorgels TG, Jacoline B, Van der Spek PJ, Bossers K, Heine VM, Bergen AA (2015) Comparison of mouse and human retinal pigment epithelium gene expression profiles: potential implications for age-related macular degeneration. PLoS ONE 10(10):e0141597
Bressler NM, Bressler SB, Fine SL (1988) Age-related macular degeneration. Surv Ophthalmol 32(6):375–413
Buchholz DE, Pennington BO, Croze RH, Hinman CR, Coffey PJ, Clegg DO (2013) Rapid and efficient directed differentiation of human pluripotent stem cells into retinal pigmented epithelium. Stem Cells Transl Med 2(5):384–393
Cabral T, Mello LGM, Lima LH, Polido J, Regatieri CV, Belfort R, Mahajan VB (2017) Retinal and choroidal angiogenesis: a review of new targets. Int J Retina Vitr 3(1):31
Campochiaro PA, Aiello LP, Rosenfeld PJ (2016) Anti–vascular endothelial growth factor agents in the treatment of retinal disease: from bench to bedside. Ophthalmology 123(10):S78–S88
Cano M, Thimmalappula R, Fujihara M, Nagai N, Sporn M, Wang AL, Neufeld AH, Biswal S, Handa JT (2010) Cigarette smoking, oxidative stress, the anti-oxidant response through Nrf2 signaling, and age-related macular degeneration. Vis Res 50(7):652–664
Chen Y, Zeng J, Zhao C, Wang K, Trood E, Buehler J, Weed M, Kasuga D, Bernstein PS, Hughes G (2011) Assessing susceptibility to age-related macular degeneration with genetic markers and environmental factors. Arch Ophthalmol 129(3):344–351
Chen S, Popp N, Chan C-C (2014) Animal models of age-related macular degeneration and their translatability into the clinic. Expert Rev Ophthalmol 9(4):285–295
Chong EW-T, Kreis AJ, Wong TY, Simpson JA, Guymer RH (2008) Alcohol consumption and the risk of age-related macular degeneration: a systematic review and meta-analysis. Am J Ophthalmol 145(4):707–715
Council NR (2006) Overcoming challenges to develop countermeasures against aerosolized bioterrorism agents: appropriate use of animal models. National Academies Press, Washington, DC
da Cruz L, Fynes K, Georgiadis O, Kerby J, Luo YH, Ahmado A, Vernon A, Daniels JT, Nommiste B, Hasan SM (2018) Phase 1 clinical study of an embryonic stem cell–derived retinal pigment epithelium patch in age-related macular degeneration. Nat Biotechnol 36(4):328
Darbre PD, Darbre PD (1988) Introduction to practical molecular biology. Wiley, Hoboken
de Jong EK, Geerlings MJ, den Hollander AI (2020) Age-related macular degeneration. In: Gao XR (ed) Genetics and genomics of eye disease. Elsevier, Amsterdam, pp 155–180
Denayer T, Stöhr T, Van Roy M (2014) Animal models in translational medicine: validation and prediction. New Horiz Transl Med 2(1):5–11
Djulbegovic B (2007) Articulating and responding to uncertainties in clinical research. J Med Philos 32(2):79–98
Ebersberger I, Metzler D, Schwarz C, Pääbo S (2002) Genomewide comparison of DNA sequences between humans and chimpanzees. Am J Hum Genet 70(6):1490–1497
Fox IJ, Daley GQ, Goldman SA, Huard J, Kamp TJ, Trucco M (2014) Use of differentiated pluripotent stem cells in replacement therapy for treating disease. Science 345(6199):1247391
Goodarzi P, Aghayan HR, Soleimani M, Norouzi-Javidan A, Mohamadi-Jahani F, Jahangiri S, Emami-Razavi SH, Larijani B, Arjmand B (2014) Stem cell therapy for treatment of epilepsy. Acta Med Iran 52(9):651–655
Goodarzi P, Aghayan HR, Larijani B, Soleimani M, Dehpour A-R, Sahebjam M, Ghaderi F, Arjmand B (2015) Stem cell-based approach for the treatment of Parkinson’s disease. Med J Islam Repub Iran 29:168
Goodarzi P, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Mohamadi-Jahani F, Ranjbaran N, Payab M, Falahzadeh K, Mousavi M, Arjmand B (2018) Mesenchymal stem cells-derived exosomes for wound regeneration. In: Turksen K (ed) Cell biology and translational medicine, vol 4. Springer, Berlin, pp 119–131
Goodarzi P, Payab M, Alavi-Moghadam S, Larijani B, Rahim F, Bana N, Sarvari M, Adibi H, Heravani NF, Hadavandkhani M (2019) Development and validation of Alzheimer’s Disease Animal Model for the Purpose of Regenerative Medicine. Cell Tissue Bank 20(2):141–151
Grisanti S, Ziemssen F (2007) Bevacizumab: off-label use in ophthalmology. Indian J Ophthalmol 55(6):417
Guan Y, Cui L, Qu Z, Lu L, Wang F, Wu Y, Zhang J, Gao F, Tian H, Xu L (2013) Subretinal transplantation of rat MSCs and erythropoietin gene modified rat MSCs for protecting and rescuing degenerative retina in rats. Curr Mol Med 13(9):1419–1431
He Y, Zhang Y, Liu X, Ghazaryan E, Li Y, Xie J, Su G (2014) Recent advances of stem cell therapy for retinitis pigmentosa. Int J Mol Sci 15(8):14456–14474
Held JR (1983) Appropriate animal models. Annals New York Acad Sci 406:13–19
Huang EJ, Wu S, Lai C, Kuo C, Wu P, Chen C, Chen C, King Y, Wu P (2014) Prevalence and risk factors for age-related macular degeneration in the elderly Chinese population in south-western Taiwan: the Puzih eye study. Eye 28(6):705
Hubrecht RC, Carter E (2019) The 3Rs and Humane Experimental Technique: implementing Change. Anim Open Access J MDPI 9(10):754
Humphray SJ, Scott CE, Clark R, Marron B, Bender C, Camm N, Davis J, Jenks A, Noon A, Patel M (2007) A high utility integrated map of the pig genome. Genome Biol 8(7):R139
Hussain RM, Ciulla TA (2017) Emerging vascular endothelial growth factor antagonists to treat neovascular age-related macular degeneration. Expert Opin Emerg Drugs 22(3):235–246
Immonen IJ, Saijonmaa O, Seitsonen S, Fyhrquist F (2009) Telomere length and age-related macular degeneration. Invest Ophthalmol Vis Sci 50(13):714
Isasi R, Rahimzadeh V, Charlebois K (2016) Uncertainty and innovation: understanding the role of cell-based manufacturing facilities in shaping regulatory and commercialization environments. Appl Transl Genomics 11:27–39
Ivandic BT, Ivandic T (2008) Low-level laser therapy improves vision in patients with age-related macular degeneration. Photomed Laser Surg 26(3):241–245
Jackson TL, Boyer D, Brown DM, Chaudhry N, Elman M, Liang C, O’Shaughnessy D, Parsons EC, Patel S, Slakter JS (2017) Oral tyrosine kinase inhibitor for neovascular age-related macular degeneration: a phase 1 dose-escalation study. JAMA ophthalmol 135(7):761–767
Jian Q, Li Y, Yin ZQ (2015) Rat BMSCs initiate retinal endogenous repair through NGF/TrkA signaling. Exp Eye Res 132:34–47
Jones MK, Lu B, Girman S, Wang S (2017) Cell-based therapeutic strategies for replacement and preservation in retinal degenerative diseases. Prog Retinal Eye Res 58:1–27
Krause M, Phan TG, Ma H, Sobey CG, Lim R (2019) Cell-Based Therapies for Stroke: are We There Yet? Front Neurol 10:656
Larijani BP, Goodarzi M, Payab A, Tayanloo-Beik M, Sarvari M, Gholami K, Gilany E, Nasli-Esfahani M, Yarahmadi M, Ghaderi F (2019) The design and application of an appropriate parkinson’s disease animal model in regenerative medicine. In: Turksen K (ed) Cell biology and translational medicine. Springer, Berlin
Leach LL, Clegg DO (2015) Concise review: making stem cells retinal: methods for deriving retinal pigment epithelium and implications for patients with ocular disease. Stem Cells 33(8):2363–2373
Liu Y, Weng W, Gao R (2019) New insights for cellular and molecular mechanisms of aging and aging-related diseases: herbal medicine as potential therapeutic approach. Oxidative Med Cell Longev J 2019:4598167
Lu L, Yaszemski MJ, Mikos AG (2001) Retinal pigment epithelium engineering using synthetic biodegradable polymers. Biomaterials 22(24):3345–3355
MacPherson A, Kimmelman J (2019) Ethical development of stem-cell-based interventions. Nat Med 25(7):1037–1044
Middleton S (2010) Porcine ophthalmology. Vet Clin North Am Food Anim Pract 26(3):557–572
Moore NA, Bracha P, Hussain RM, Morral N, Ciulla TA (2017) Gene therapy for age-related macular degeneration. Expert Opin Biol Ther 17(10):1235–1244
Mustari MJ (2017) Nonhuman primate studies to advance vision science and prevent blindness. ILAR J 58(2):216–225
Nazari H, Zhang L, Zhu D, Chader GJ, Falabella P, Stefanini F, Rowland T, Clegg DO, Kashani AH, Hinton DR (2015) Stem cell based therapies for age-related macular degeneration: the promises and the challenges. Prog Retinal Eye Res 48:1–39
Nowak JZ (2006) Age-related macular degeneration (AMD): pathogenesis and therapy. Pharmacol Rep 58(3):353
Öner A (2018) Stem cell treatment in retinal diseases: recent developments. Turk J Ophthalmol 48(1):33
Parekkadan B, Milwid JM (2010) Mesenchymal stem cells as therapeutics. Annu Rev Biomed Eng 12:87–117
Pennesi ME, Neuringer M, Courtney RJ (2012) Animal models of age related macular degeneration. Mol Asp Med 33(4):487–509
Rabadán-Diehl C, Nathanielsz P (2013) From Mice to Men: research models of developmental programming. J Dev Orig Health Dis 4(1):3–9
Riva L, Petrini C (2019) A few ethical issues in translational research for gene and cell therapy. J Transl Med 17(1):395
Rowe-Rendleman C, Glickman RD (2004) Possible therapy for age-related macular degeneration using human telomerase. Brain Res Bull 62(6):549–553
Schleidgen S, Fernau S, Fleischer H, Schickhardt C, Oßa A-K, Winkler EC (2017) Applying systems biology to biomedical research and health care: a précising definition of systems medicine. BMC Health Serv Res 17(1):761
Schmidt-Erfurth U, Hasan T (2000) Mechanisms of action of photodynamic therapy with verteporfin for the treatment of age-related macular degeneration. Surv Ophthalmol 45(3):195–214
Schwartz SD, Hubschman J-P, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, Mickunas E, Gay R, Klimanskaya I, Lanza R (2012) Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet 379(9817):713–720
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, Hubschman J-P, Davis JL, Heilwell G, Spirn M (2015) Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet 385(9967):509–516
Schwartz SD, Tan G, Hosseini H, Nagiel A (2016) Subretinal transplantation of embryonic stem cell–derived retinal pigment epithelium for the treatment of macular degeneration: an assessment at 4 years. Investig Ophthalmol Vis Sci 57(5):ORSFc1–ORSFc9
Seddon JM, Reynolds R, Rosner B (2010) Associations of smoking, body mass index, dietary lutein, and the LIPC gene variant rs10468017 with advanced age-related macular degeneration. Mol Vis 16:2412
Semeraro F, Morescalchi F, Duse S, Parmeggiani F, Gambicorti E, Costagliola C (2013) Aflibercept in wet AMD: specific role and optimal use. Drug Des Dev Ther 7:711
Sharma K, Sharma NK, Anand A (2014) Why AMD is a disease of ageing and not of development: mechanisms and insights. Front Aging Neurosci 6:151
Sharma A, Kumar N, Parachuri N, Sharma R, Bandello F, Kuppermann BD, Regillo CD (2020) Brolucizumab and fluid in neovascular age-related macular degeneration (n-AMD). Eye (Lond). https://doi.org/10.1038/s41433-020-0831-2
Singh MS, MacLaren RE (2018) Stem cell treatment for age-related macular degeneration: the challenges. Investig Ophthalmol Vis Sci 59(4):AMD78–AMD82
Siqueira RC (2011) Stem cell therapy for retinal diseases: update. Stem Cell Res Ther 2(6):50
Soleimani M, Aghayan HR, Goodarzi P, Hagh MF, Lajimi AA, Saki N, Mohamadi-Jahani F, Javidan AN, Arjmand B (2016) Stem cell therapy-approach for multiple sclerosis treatment. Arch Neurosci 3(1):e21564
Stein G, Rosenfeld PJ (2018) Next-Generation Therapies For Wet AMD: Upgrade 2.0; 2016: Retina fellows forum, 19 September
Stern JH, Temple S (2011) Stem cells for retinal replacement therapy. Neurotherapeutics 8(4):736–743
Strunnikova N, Maminishkis A, Barb J, Wang F, Zhi C, Sergeev Y, Chen W, Edwards A, Stambolian D, Abecasis G (2010) Transcriptome analysis and molecular signature of human retinal pigment epithelium. Hum Mol Genet 19(12):2468–2486
Sugitani S, Tsuruma K, Ohno Y, Kuse Y, Yamauchi M, Egashira Y, Yoshimura S, Shimazawa M, Iwama T, Hara H (2013) The potential neuroprotective effect of human adipose stem cells conditioned medium against light-induced retinal damage. Exp Eye Res 116:254–264
Sun Y-D, Dong Y-D, Fan R, Zhai L-L, Bai Y-L, Jia L-H (2012) Effect of (R)-α-lipoic acid supplementation on serum lipids and antioxidative ability in patients with age-related macular degeneration. Ann Nutr Metab 60(4):293–297
Swaroop A, Chew EY, Rickman CB, Abecasis GR (2009) Unraveling a multifactorial late-onset disease: from genetic susceptibility to disease mechanisms for age-related macular degeneration. Ann Rev Genomics Hum Genet 10:19-43
Tsuruma K, Yamauchi M, Sugitani S, Otsuka T, Ohno Y, Nagahara Y, Ikegame Y, Shimazawa M, Yoshimura S, Iwama T (2014) Progranulin, a major secreted protein of mouse adipose-derived stem cells, inhibits light-induced retinal degeneration. Stem Cells Transl Med 3(1):42–53
Twigger SN (2004) Of rats and men. Genome Biol 5(3):314
Vazquez-Chona FR, Khan AN, Chan CK, Moore AN, Dash PK, Hernandez MR, Lu L, Chesler EJ, Manly KF, Williams RW (2005) Genetic networks controlling retinal injury. Mol Vis 11:958
Veritti D, Sarao V, Lanzetta P (2012) Neovascular age-related macular degeneration. Ophthalmologica 227(Suppl 1):11–20
Villegas VM, Aranguren LA, Kovach JL, Schwartz SG, Flynn HW Jr (2017) Current advances in the treatment of neovascular age-related macular degeneration. Expert Opin Drug Deliv 14(2):273–282
Waugh N, Loveman E, Colquitt J, Royle P, Yeong JL, Hoad G, Lois N (2018) Treatments for dry age-related macular degeneration and Stargardt disease: a systematic review. Health Technol Assess 22(27):1–168
Zarbin M, Sugino I, Townes-Anderson E (2019) Concise review: update on retinal pigment epithelium transplantation for age-related macular degeneration. Stem Cells Transl Med 8(5):466–477
Zeiss C (2010) Animals as models of age-related macular degeneration: an imperfect measure of the truth. Vet Pathol 47(3):396–413
Zernii EY, Baksheeva VE, Iomdina EN, Averina OA, Permyakov SE, Philippov PP, Zamyatnin AA, Senin II (2016) Rabbit models of ocular diseases: new relevance for classical approaches. CNS Neurol Disord Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders) 15(3):267–291
Acknowledgements
The authors would like to thank Dr. Mohsen Khorshidi and Shokouh Slaimi for their considerable assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baradaran-Rafii, A., Sarvari, M., Alavi-Moghadam, S. et al. Cell-based approaches towards treating age-related macular degeneration. Cell Tissue Bank 21, 339–347 (2020). https://doi.org/10.1007/s10561-020-09826-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-020-09826-3