Abstract
Background
This meta-analysis aimed to evaluate the efficacy and safety of non-vitamin K antagonist oral anticoagulants (NOACs) versus vitamin K antagonists (VKAs) in secondary stroke prevention in atrial fibrillation (AF) patients.
Methods
PubMed and Embase electronic databases were systematically searched from January 2009 to July 2019 for relevant randomized clinical trials and observational studies. A random-effects model was applied in the pooled analysis.
Results
A total of 14 studies (4 randomized clinical trials and 10 observational studies) were included. Based on the randomized clinical trials, compared with VKA use, the use of NOACs was associated with decreased risk of stroke and systemic embolism, major bleeding, and intracranial bleeding. Based on the observational studies, compared with VKAs, the subgroup analysis showed that dabigatran and rivaroxaban were associated with a reduced risk of stroke or systemic embolism, whereas dabigatran and apixaban were associated with a decreased risk of major bleeding.
Conclusion
Based on current data, the use of NOACs is at least non-inferior to the use of VKAs in AF patients for secondary stroke prevention irrespective of NOAC type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral anticoagulants are the first-line therapy for atrial fibrillation (AF) in the prevention of stroke. Vitamin K antagonists (VKAs) such as warfarin have been widely used in AF patients for decades. Previous studies have indicated that warfarin can achieve a two-thirds reduction in the primary prevention of stroke [1,2,3], and a similar risk reduction has been shown in secondary stroke prevention observational studies. Since 2009, non-vitamin K antagonist oral anticoagulants (NOACs; dabigatran, apixaban, edoxaban, and rivaroxaban) have provided an alternative therapy that is at least non-inferior to warfarin for thromboprophylaxis. AF is associated with the incidence of stroke-related death and disability in up to 15–25% of cases [4, 5]. A history of stroke/transient ischemic attack (TIA)/stroke or systematic embolism (SSE) is considered a risk factor for embolism in AF patients. Early recurrence of stroke is common when AF patients have a history of stroke/TIA/SSE. They are also more prone to hemorrhagic events after being prescribed oral anticoagulants. It is thus of great importance to evaluate the application of anticoagulants in AF patients regarding secondary stroke prevention.
In 2012, Ntaios et al. [6] pooled the data from randomized clinical trials (RCTs) comparing different NOACs (dabigatran, rivaroxaban, and apixaban) versus warfarin in AF patients with previous stroke/TIA. Their results indicated that NOACs produced significant reductions in systemic embolism, major bleeding, and hemorrhagic stroke compared with warfarin, and a subsequent study that included data from edoxaban confirmed these findings of Ntaios et al. [7]. In addition, there are no differences in the effects of rivaroxaban and warfarin in patients with mild AF-related acute ischemic stroke [8]. However, the evidence generated from RCTs lacks broad generalizability to patients in real-world settings. Therefore, this meta-analysis aimed to compare the efficacy and safety outcomes of NOACs versus VKAs in AF patients with previous stroke/TIA/SSE using data from both RCTs and observational studies.
Eligibility Criteria
Studies were included if they met the following criteria: (1) study population: non-valvular AF patients with previous stroke/TIA/systemic embolism who received at least one NOAC compared to those who received VKAs. (2) Interventions: any NOACs and VKAs. (3) Outcomes: studies reported at least one of the efficacy or safety outcomes. Efficacy outcomes included stroke or SSE, ischemic stroke (IS), and all-cause death, and safety outcomes included major bleeding, intracranial hemorrhage (ICH), and gastrointestinal (GI) bleeding. (4) Study design: RCTs or observational studies. (5) Effect estimates: propensity score-matched or adjusted risk ratios (RRs) and 95% confidence intervals (CIs). Studies that reported AF patients with certain interventions (e.g., cardioversion, catheter ablation, coronary interventions, or left-atrial appendage closure) or with specific diseases (e.g., coronary artery disease, peripheral artery disease, liver disease, diabetes, or cancer) were excluded. Publications with no data, such as reviews, case reports, case series, editorials, letters, guidelines, and conference abstracts, were also excluded. If the AF subjects in multiple studies were from the same data source, the study with the longest study period or the largest sample size was included.
Literature Search
PubMed and Embase electronic databases were systematically searched from January 2009 (since the first available NOAC, dabigatran, was applied to AF patients) to July 2019 for studies that compared the effect between any reduced-dose NOAC and VKAs in AF patients with previous stroke/TIA/systemic embolism. As shown in Supplemental Table I, the search strategy combined three kinds of search terms using the Boolean operator “and”: “atrial fibrillation OR atrial flutter” AND “non-vitamin K antagonist oral anticoagulants OR NOACs OR direct oral anticoagulants OR DOACs OR new oral anticoagulants OR novel oral anticoagulants OR oral thrombin inhibitors OR factor Xa inhibitors OR dabigatran OR rivaroxaban OR apixaban OR edoxaban” AND “vitamin K antagonists OR warfarin”. We applied no linguistic restrictions in the literature search. The literature search strategy is shown in Supplemental Table I. To ensure a comprehensive literature search, the reference lists of the retrieved studies were screened to identify additional reports.
Study Selection and Data Extraction
All the retrieved studies were independently screened by two reviewers (Xin Liu and Zi-Xuan Xu). According to the inclusion and exclusion criteria, we first read the titles and abstracts to identify potentially eligible studies, the full texts of which were reviewed in more detail. Disagreements were resolved by consensus or by a discussion with other authors (Ping Yuan and Wen-Gen Zhu). For each study, we collected the following data: the first author and publication year, country, study design, inclusion period, data source, type of NOACs, follow-up time of NOAC cohorts, and outcomes used in the study. If one study reported adjusted RRs in multiple models, the mostly adjusted one was included.
Risk of Bias Assessment
For the RCTs, the bias risk was evaluated according to the Cochrane risk of bias assessment tool [9]. The bias risk of each study was scored as “low”, “unclear”, or “high” in each section. A “low risk” was considered when three out of five biases were “low” [11]. For the observational studies, the modified Newcastle–Ottawa Scale (NOS) tool was applied to evaluate the methodological quality [12, 13]. This scoring scale involved three domains: the selection of cohorts, the comparability of cohorts, and the assessment of the outcome. A study with a NOS score of <6 was defined as low quality [14].
Statistical Analysis
The Cochrane Q test and I2 statistic were the most commonly reported statistical methods to assess heterogeneity, where P < 0.1 and I2 > 50% indicated a substantial heterogeneity, respectively. The natural logarithms of RRs and standard errors of included studies were calculated and then pooled by a random-effects model using an inverse variance method. The publication bias was assessed by using the funnel plots and further calculated by using the Egger and Begg tests. Sensitivity analysis and subgroup analysis were performed where appropriate.
All statistical analyses were performed using the Review Manager 5.3 software (the Nordic Cochrane Center, Rigshospitalet, Denmark) and Stata software (version 15.0, Stata Corp LP, College Station, TX, USA).
Results
Study Selection
The process for electronic retrievals is shown in Supplemental Fig. I. A total of 16 studies (5 sub-analyses of RCTs [8, 15,16,17,18] and 11 observational studies [19,20,21,22,23,24,25,26,27,28,29]) were potentially qualified. In order to show the reliability of all the included studies, the source and the size of participants have been listed in Supplemental Table II. In addition, two studies focusing on AF patients with acute ischemic stroke were excluded [8, 21]. Finally, four sub-analyses of RCTs and 10 observational studies were included in this meta-analysis. The baseline characteristics of the included studies are shown in Supplemental Table II. Analysis of four post-proof-of-concept (PoC) RCTs provided the initial anticoagulation therapy. All patients were randomized after day 7 post-stroke in ARISTOTLE [30] and after day 15 in both RE-LY [31] and ROCKET [32]. The ENGAGE AF-TIMI 48 trial [33] excluded patients with any ischemic stroke type up until day 30. Regarding the observational studies, the information of anticoagulation agents was list in the Supplemental Table II, without details about the initial NOACs available. For the quality assessment, the four sub-analyses of RCTs had a low risk of bias, whereas the 10 observational cohorts had an acceptable quality with a NOS score of ≥6.
NOACs Versus VKAs Based on RCTs
Efficacy
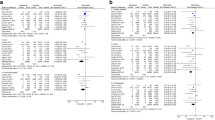
Compared with VKA use, the use of NOACs was associated with decreased risk of SSE (with stroke/TIA: RR, 0.82, 95% CI 0.71–0.94; without stroke/TIA: RR, 0.80, 95% CI 0.70–0.92; Pinteraction = 0.88; Supplemental Fig. II). A similar rate of IS was observed in patients with and without previous stroke/TIA (Supplemental Fig. III). As shown in Table 1, there was no difference in the risk of all-cause death between patients without previous stroke/TIA (RR, 0.91, 95% CI 0.85–0.97) and those with previous stroke/TIA (RR, 0.91, 95% CI 0.82–1.01) (Pinteraction = 0.99; Supplemental Fig. IV) (Fig. 1).
Comparing efficacy-related outcomes of NOACs with warfarin in AF patients with previous stroke or TIA based on RCTs. Abbreviations: SSE = stroke or systemic embolism; IS = ischemic stroke; AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; DA = dabigatran; RIV = rivaroxaban; API = apixaban; EDO = edoxaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
Safety
Compared with VKA use, the use of NOACs was associated with decreased rates of major bleeding (with stroke/TIA: RR, 0.85, 95% CI 0.73–0.98; without stroke/TIA: RR, 0.85, 95% CI 0.74–0.99; Pinteraction = 0.96; Supplemental Fig. V) and intracranial bleeding (with stroke/TIA: RR, 0.46, 95% CI 0.31–0.68; without stroke/TIA: RR, 0.43, 95% CI 0.35–0.53; Pinteraction = 0.76; Supplemental Fig. VI) in AF patients with or without previous stroke/TIA. There was a similar risk of GI bleeding in patients with and without previous stroke/TIA (Supplemental Fig. VII) (Fig. 2, Table 1).
Comparing the safety-related outcomes of NOACs with warfarin in AF patients with previous stroke or TIA based on RCTs. Abbreviations: ICH = intracranial hemorrhage; GI bleeding = gastrointestinal bleeding; AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; DA = dabigatran; RIV = rivaroxaban; API = apixaban; EDO = edoxaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
NOACs Versus VKAs Based on Observational Studies
Sensitivity analysis was performed by excluding the study of Lip GY et al. since the studied populations were AF patients with stroke/systemic embolism (SSE), and the results were not changed. (Supplemental Table III).
Efficacy
Compared with VKA use, the use of NOACs was associated with reduced risk of SSE (RR, 0.79, 95% CI 0.72–0.88; Fig. 3) and all-cause death (RR, 0.84, 95% CI 0.74–0.95; Supplemental Fig. VIII) but a comparable risk of IS (RR, 0.87, 95% CI 0.74–1.03; Supplemental Fig. IX) and myocardial infarction (MI) (RR, 1.08, 95% CI 0.81–1.43; Supplemental Fig. X).
Comparison of the outcome of SSE with NOACs versus VKAs in secondary stroke prevention in AF patients based on observational studies. Abbreviations: SSE = stroke or systemic embolism; AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; VKAs = vitamin K antagonists; DA = dabigatran; RIV = rivaroxaban; API = apixaban; EDO = edoxaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
Safety
Compared with the VKA users, the users of NOACs had reduced risk of major bleeding (RR, 0.70, 95% CI 0.57–0.84; Fig. 4) and ICH (RR, 0.44, 95% CI 0.34–0.57; Supplemental Fig. XI) in secondary stroke prevention in AF patients. We found a similar risk of GI bleeding (RR, 1.06, 95% CI 0.86–1.31; Supplemental Fig. XII) in these two groups.
Comparison of major bleeding with NOACs versus VKAs in secondary stroke prevention in AF patients based on observational studies. Abbreviations: AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; VKAs = vitamin K antagonists; DA = dabigatran; RIV = rivaroxaban; API = apixaban; EDO = edoxaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
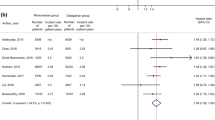
Subgroup Analysis
We performed a subgroup analysis based on the NOAC types. Compared with VKAs, dabigatran (RR, 0.83, 95% CI 0.75–0.93) and rivaroxaban (RR, 0.76, 95% CI 0.69–0.84), but not apixaban (RR, 0.78, 95% CI 0.60–1.02), reduced the risk of SSE (Fig. 5), and dabigatran (RR, 0.62, 95% CI 0.47–0.83) and apixaban (RR, 0.68, 95% CI 0.57–0.82), but not rivaroxaban (RR, 1.02, 95% CI 0.85–1.23), were associated with a decreased risk of major bleeding (Fig. 6). Data regarding other efficacy and safety outcomes suggested that NOACs had lower or similar rates of thromboembolic and bleeding events relative to VKAs (Supplemental Figs. XIII, XIV, XV, and XVI). Additional subgroup analysis was conducted regarding different prior stroke types. The results suggested that NOACs had lower or similar rates of thromboembolic and bleeding events compared with VKAs. There was no difference between AF and different types of previous stroke (all Pinteraction>0.5) (Supplemental Table IX).
Comparison of the outcome of SSE with different NOACs versus VKAs in secondary stroke prevention in AF patients based on observational studies. Abbreviations: SSE = stroke or systemic embolism; AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; VKAs = vitamin K antagonists; DA = dabigatran; RIV = rivaroxaban; API = apixaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
Comparison of major bleeding with different NOACs versus VKAs in secondary stroke prevention in AF patients based on observational studies. Abbreviations: AF = atrial fibrillation; NOACs = non-vitamin K antagonist oral anticoagulants; VKAs = vitamin K antagonists; DA = dabigatran; RIV = rivaroxaban; API = apixaban; TIA = transient ischemic attack; CI = confidence interval; SE = standard error; IV = inverse of the variance; RCTs = randomized clinical trials
Publication Bias
There were seemingly no potential publication biases indicated by the funnel plots (Supplemental Figs. XVII and XVIII). For the observational studies, Egger and Begg tests were also performed. The results for some reported outcomes indicated certain publication biases (Supplemental Fig. XIX). Nevertheless, the results from the trim-and-fill analysis showed no trimming performed, and the corresponding pooled results were not changed.
Discussion
Our meta-analysis pooled the data from 4 sub-analyses from RCTs and 10 observational studies to evaluate the comparisons of efficacy and safety outcomes for NOACs and VKAs in AF patients with stroke/TIA. The pooled RCT data show that the use of NOACs was associated with decreased risk of stroke or systemic embolism, major bleeding, and ICH when compared with VKA use. Similar efficacy and safety outcomes (NOACs versus VKAs) are indicated for AF patients with and without previous stroke. In addition, this is the first study to include observational study data to compare the outcomes of NOACs and VKAs in this population of interest. Compared with VKAs, subgroup analysis showed that dabigatran and rivaroxaban were associated with a reduced risk of stroke or systemic embolism, whereas dabigatran and apixaban were associated with a decreased risk of major bleeding. Overall, NOACs are at least non-inferior to VKAs in secondary stroke prevention in AF patients, irrespective of the NOAC type.
Data from both the RCTs [34,35,36,37,38] and observational studies [10, 39, 40] show the superiority of NOACs in the reduction of hemorrhagic-related adverse outcomes, including ICH and GI bleeding. In the present study, among AF patients with a history of stroke/TIA/SSE, NOACs show better reductions in the risk of SSE and ICH than VKAs. Among the mild AF-related acute ischemic stroke patients, rivaroxaban and VKAs show comparable effectiveness and safety profiles, as is reflected by the recurrence of IS and the incidence of ICH based on magnetic resonance imaging (MRI) diagnosis [8]. The specific-dose analysis of dabigatran from the RE-LY trial [17] was also included in this study. The regular dose (150 mg, bid) and low dose (110 mg, bid) of dabigatran did not show superiority but did show comparable efficacy compared with VKAs regarding SSE, while the low dose of dabigatran was safer with regard to major bleeding, ICH, and GI bleeding. In addition, NOACs showed advantages over VKAs regardless of the presence or absence of previous stroke/TIA in the RCTs.
Data from observational studies suggest that when compared with VKAs, NOACs show at least comparable effectiveness and greater safety among AF patients [29, 41]. Specifically, several meta-analyses indicated that when AF patients had other conditions, such as chronic kidney disease [42], percutaneous coronary intervention after myocardial infarction [43], or cancer [44], NOACs were more effective and safer for them than VKAs. However, there are limited data focusing on AF patients with a history of stroke/TIA/SSE, which is one of the most common complications in observational cohort studies. In a previous study, NOACs were found to be an independent factor negatively correlated with acute major cerebral artery occlusion in acute cardioembolic stroke with non-valvular AF when compared with either no anticoagulation or VKAs [45]. Another study reported that AF patients with a history of IS were more likely to experience TIA and partial anterior circulation infarct, which are usually indicators of less severe infarcts and better functional outcomes [46], when they were treated with NOACs versus VKAs. However, in the acute phase, thrombolysis was more common in the VKA group. Our meta-analysis data suggest that NOACs are associated with reduced risk of SSE and all-cause death, but have a comparable risk of IS. In terms of safety, NOACs reduce the rates of major bleeding and ICH, but have a similar risk of GI bleeding in AF patients with previous stroke/TIA/SSE when compared with VKAs.
However, the results from the sub-analysis of different types of NOACs varied. When compared with VKAs, dabigatran and rivaroxaban, but not apixaban, significantly reduced the risk of SSE, while in terms of safety, dabigatran and apixaban, but not rivaroxaban, significantly decreased the risk of major bleeding. It has been observed that all three NOACs have similar anti-embolism effects, while both dabigatran and apixaban show a significantly reduced rate of major bleeding in real-world applications [27]. This indicates that the effectiveness and safety event rates for rivaroxaban treatment are higher in AF patients with prior stroke/TIA than in those without stroke [47]. We did not present the edoxaban data because only one study compared the effects of edoxaban and VKAs [25]. According to the data in the present meta-analysis, we can conclude that the use of NOACs is at least non-inferior to the use of VKAs in AF patients with previous stroke/TIA/SSE. Taking the advantages of NOAC application into consideration, including rapid onset/offset of action, few drug interactions, predictable pharmacokinetics, and eliminating the requirement for regular coagulation monitoring, NOACs would be a better choice in the clinical setting.
Limitations
This is the first meta-analysis evaluating the safety and efficacy of NOACs versus VKAs among AF patients with and without previous stroke/TIA that provides robust evidence to fill the gap in knowledge regarding primary and secondary stroke prevention in AF patients. However, several limitations should be noted. Patients with AF who had a stroke/TIA/SSE history were at high risk for recurrent ischemic stroke, especially in the early phase after stroke, and the incidence of ischemic stroke recurrence related to AF was found to be as high as 8% during the first 14 days [48]. Early prescriptions of NOACs do not increase the risk of ICH, but do decrease recurrent ischemic stroke. The timing of the initial secondary stroke prevention apart from anticoagulation agents should be taken into consideration. Due to the limited data regarding the initial time point of NOAC administration and early outcome in these specific patients, subgroup analysis was not available in this meta-analysis. Future studies are warranted to address the best treatment window. The baseline severity of stroke could be closely related to the prognosis. The National Institutes of Health Stroke Scale should be the primary assessment of AF patients with previous stroke before anticoagulation application. As such, subgroup analysis regarding the severity of stroke could not be performed due to the limited data. For the observational cohort studies, limitations arise from the bias of prescriptions from doctors and the lack of information about patient adherence and persistence. The proportion of patients treated with warfarin within the therapeutic range varied among the RCTs and was absent in most of the observational studies. Due to the lack of comparisons among different NOAC agents, it is too early to determine which one would be the best choice for AF patients with a history of ischemic stroke or TIA or systematic embolism.
Conclusions
In both RCTs and observational studies for secondary stroke prevention among AF patients, NOACs demonstrated a decreased risk of SSE and a lower rate of major bleeding and ICH compared with VKAs.
References
Warfarin versus aspirin for prevention of thromboembolism in atrial fibrillation: stroke prevention in atrial fibrillation ii study. Lancet. 1994;343:687–691.
Laupacis A, Albers G, Dalen J, Dunn M, Feinberg W, Jacobson A. Antithrombotic therapy in atrial fibrillation. Chest. 1995;108:352S–9S.
Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen afasak study. Lancet. 1989;1:175–9.
Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet. 1993;342:1255–1262.
Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001;32:2559–66.
Ntaios G, Papavasileiou V, Diener HC, Makaritsis K, Michel P. Nonvitamin-k-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298–304.
Ntaios G, Papavasileiou V, Diener HC, Makaritsis K, Michel P. Nonvitamin-k-antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and previous stroke or transient ischemic attack: an updated systematic review and meta-analysis of randomized controlled trials. Int J Stroke. 2017;12:589–96.
Hong K, Kwon SU, Lee SH, Lee JS, Kim Y, Song T, et al. Rivaroxaban vs warfarin sodium in the ultra-early period after atrial fibrillation–related mild ischemic stroke. JAMA Neurol. 2017;74:1206.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Xue Z, Zhang H. Non-vitamin k antagonist oral anticoagulants versus warfarin in Asians with atrial fibrillation: meta-analysis of randomized trials and real-world studies. Stroke. 2019;50:2819–28.
Xue Z, Zhou Y, Wu C, Lin J, Liu X, Zhu W. Non-vitamin k antagonist oral anticoagulants in Asian patients with atrial fibrillation: evidences from the real-world data. Heart Fail Rev 2019.
Wells GA SBOC. The Newcastle Ottawa scale (nos) for assessing the quality of nonrandomized studies in meta-analyses. 2014.
Zhu W, Wan R, Liu F, Hu J, Huang L, Li J, et al. Relation of body mass index with adverse outcomes among patients with atrial fibrillation: a meta-analysis and systematic review. J Am Heart Assoc 2016;5.
Easton JD, Lopes RD, Bahit MC, Wojdyla DM, Granger CB, Wallentin L, et al. Apixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of the ARISTOTLE trial. Lancet Neurol. 2012;11:503–11.
Hankey GJ, Patel MR, Stevens SR, Becker RC, Breithardt G, Carolei A, et al. Rivaroxaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of ROCKET AF. Lancet Neurol. 2012;11:315–22.
Diener HC, Connolly SJ, Ezekowitz MD, Wallentin L, Reilly PA, Yang S, et al. Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE-LY trial. Lancet Neurol. 2010;9:1157–63.
Rost NS, Giugliano RP, Ruff CT, Murphy SA, Crompton AE, Norden AD, et al. Outcomes with edoxaban versus warfarin in patients with previous cerebrovascular events: findings from ENGAGE AF-TIMI 48 (effective anticoagulation with factor Xa next generation in atrial fibrillation-thrombolysis in myocardial infarction 48). Stroke. 2016;47:2075–82.
Xian Y, Xu H, O'Brien EC, Shah S, Thomas L, Pencina MJ, et al. Clinical effectiveness of direct oral anticoagulants vs warfarin in older patients with atrial fibrillation and ischemic stroke: findings from the patient-centered research into outcomes stroke patients prefer and effectiveness research (prosper) study. JAMA Neurol. 2019.
Seiffge DJ, Paciaroni M, Wilson D, Koga M, Macha K, Cappellari M, et al. Direct oral anticoagulants versus vitamin k antagonists after recent ischemic stroke in patients with atrial fibrillation. Ann Neurol. 2019;85:823–34.
Yoshimura S, Koga M, Sato S, Todo K, Yamagami H, Kumamoto M, et al. Two-year outcomes of anticoagulation for acute ischemic stroke with nonvalvular atrial fibrillation—SAMURAI-NVAF study. Circ J. 2018;82:1935–42.
Coleman CI, Peacock WF, Bunz TJ, Alberts MJ. Effectiveness and safety of apixaban, dabigatran, and rivaroxaban versus warfarin in patients with nonvalvular atrial fibrillation and previous stroke or transient ischemic attack. Stroke. 2017;48:2142–9.
Larsen TB, Rasmussen LH, Gorst-Rasmussen A, Skjoth F, Lane DA, Lip GY. Dabigatran and warfarin for secondary prevention of stroke in atrial fibrillation patients: a nationwide cohort study. Am J Med. 2014;127:1172–8.
Cho MS, Yun JE, Park JJ, Kim YJ, Lee J, Kim H, et al. Outcomes after use of standard- and low-dose non-vitamin k oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2018:A118023093.
Chan YH, Lee HF, See LC, Tu HT, Chao TF, Yeh YH, et al. Effectiveness and safety of four direct oral anticoagulants in Asian patients with nonvalvular atrial fibrillation. Chest. 2019.
Lee KH, Park HW, Lee N, Hyun DY, Won J, Oh SS, et al. Optimal dose of dabigatran for the prevention of thromboembolism with minimal bleeding risk in Korean patients with atrial fibrillation. Europace. 2017;19:v1–9.
Lip G, Keshishian A, Li X, Hamilton M, Masseria C, Gupta K, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients. Stroke. 2018;49:2933–44.
Lauffenburger JC, Farley JF, Gehi AK, Rhoney DH, Brookhart MA, Fang G. Effectiveness and safety of dabigatran and warfarin in real-world us patients with non-valvular atrial fibrillation: a retrospective cohort study. J Am Heart Assoc 2015;4.
Larsen TB, Skjoth F, Nielsen PB, Kjaeldgaard JN, Lip GY. Comparative effectiveness and safety of non-vitamin k antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Steffel J, Giugliano RP, Braunwald E, Murphy SA, Mercuri M, Choi Y, et al. Edoxaban versus warfarin in atrial fibrillation patients at risk of falling: engage af-timi 48 analysis. J Am Coll Cardiol. 2016;68:1169–78.
Bansilal S, Bloomgarden Z, Halperin JL, Hellkamp AS, Lokhnygina Y, Patel MR, et al. Efficacy and safety of rivaroxaban in patients with diabetes and nonvalvular atrial fibrillation: the rivaroxaban once-daily, oral, direct factor xa inhibition compared with vitamin k antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF trial). Am Heart J. 2015;170:675–82.
Avezum A, Oliveira G, Diaz R, Hermosillo J, Oldgren J, Ripoll EF, et al. Efficacy and safety of dabigatran versus warfarin from the RE-LY trial. Open Heart. 2018;5:e800.
Hohnloser SH, Hijazi Z, Thomas L, Alexander JH, Amerena J, Hanna M, et al. Efficacy of apixaban when compared with warfarin in relation to renal function in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2012;33:2821–30.
Nielsen PB, Skjoth F, Sogaard M, Kjaeldgaard JN, Lip GY, Larsen TB. Effectiveness and safety of reduced dose non-vitamin k antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510.
Forslund T, Wettermark B, Andersen M, Hjemdahl P. Stroke and bleeding with non-vitamin k antagonist oral anticoagulant or warfarin treatment in patients with non-valvular atrial fibrillation: a population-based cohort study. Europace. 2018;20:420–8.
Cha MJ, Choi EK, Han KD, Lee SR, Lim WH, Oh S, et al. Effectiveness and safety of non-vitamin k antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2017;48:3040–8.
Bai Y, Chen H, Yang Y, Li L, Liu XY, Shi XB, et al. Safety of antithrombotic drugs in patients with atrial fibrillation and non-end-stage chronic kidney disease: meta-analysis and systematic review. Thromb Res. 2016;137:46–52.
Lopes RD, Hong H, Harskamp RE, Bhatt DL, Mehran R, Cannon CP, et al. Safety and efficacy of antithrombotic strategies in patients with atrial fibrillation undergoing percutaneous coronary intervention: a network meta-analysis of randomized controlled trials. JAMA Cardiol 2019.
Deng Y, Tong Y, Deng Y, Zou L, Li S, Chen H. Non-vitamin k antagonist oral anticoagulants versus warfarin in patients with cancer and atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc. 2019;8:e12540.
Tomari S, Arima J, Yoshida T, Yamashita H, Sata R, Hamada R, et al. Effect of direct oral anticoagulant for acute major cerebral artery occlusion in cardioembolic stroke/transient ischemic attack patients with non-valvular atrial fibrillation. J Neurol Sci. 2019;402:162–6.
Zapata-Wainberg G, Masjuan J, Quintas S, Ximenez-Carrillo A, Garcia PA, Martinez ZM, et al. The neurologist's approach to cerebral infarct and transient ischaemic attack in patients receiving anticoagulant treatment for non-valvular atrial fibrillation: ANITA-FA study. Eur J Neurol. 2019;26:230–7.
Minematsu K, Ikeda T, Ogawa S, Kitazono T, Nakagawara J, Miyamoto S, et al. Real-world outcomes of rivaroxaban treatment in patients with both nonvalvular atrial fibrillation and a history of ischemic stroke/transient ischemic attack. Cerebrovasc Dis 2019:1–8.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–236.
Funding
The authors are thankful for the support of the National Natural Science Foundation of China (81760050) and Youth Science Fund of Jiangxi Provincial Department of Science and Technology (20192ACBL21037).
Author information
Authors and Affiliations
Contributions
Peng Yu, Wen-gen Zhu, and Ping Yuan designed the study. Xin Liu and Zi-Xuan Xu performed the literature search, study selection and data extraction, quality assessment, and statistical analysis. Xin Liu and Zi-Xuan Xu drafted the manuscript. Ping Yuan and Wen-Gen Zhu revised the draft. Peng Yu modified the English. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 3453 kb)
Rights and permissions
About this article
Cite this article
Liu, X., Xu, ZX., Yu, P. et al. Non-Vitamin K Antagonist Oral Anticoagulants in Secondary Stroke Prevention in Atrial Fibrillation Patients: An Updated Analysis by Adding Observational Studies. Cardiovasc Drugs Ther 34, 569–578 (2020). https://doi.org/10.1007/s10557-020-06961-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-06961-7