Abstract
Background
Patients with chronic kidney disease (CKD) are at high risk for developing cardiovascular events. However, limited evidence is available regarding the use of aspirin in CKD patients to decrease cardiovascular risk and to slow renal disease progression.
Study Design
Prospective, multicenter, open-label randomized controlled trial.
Setting and Participants
One hundred eleven patients with estimated glomerular filtration rate (eGFR) 15–60 ml/min/1.73 m2 without previous cardiovascular events.
Intervention
Aspirin treatment (100 mg/day) (n = 50) or usual therapy (n = 61). Mean follow-up time was 64.8 ± 16.4 months.
Outcomes
The primary endpoint was composed of cardiovascular death, acute coronary syndrome (nonfatal MI, coronary revascularization, or unstable angina pectoris), cerebrovascular disease, heart failure, or nonfatal peripheral arterial disease. Secondary endpoints were fatal and nonfatal coronary events, renal events (defined as doubling of serum creatinine, ≥ 50% decrease in eGFR, or renal replacement therapy), and bleeding episodes.
Results
During follow-up, 17 and 5 participants suffered from a primary endpoint in the control and aspirin groups, respectively. Aspirin did not significantly reduce primary composite endpoint (HR, 0.396 (0.146–1.076), p = 0.069. Eight patients suffered from a fatal or nonfatal coronary event in the control group compared to no patients in the aspirin group. Aspirin significantly reduced the risk of coronary events (log-rank, 5.997; p = 0.014). Seventeen patients in the control group reached the renal outcome in comparison with 3 patients in the aspirin group. Aspirin treatment decreased renal disease progression in a model adjusted for age, baseline kidney function, and diabetes mellitus (HR, 0.272; 95% CI, 0.077–0.955; p = 0.043) but did not when adjusted for albuminuria. No differences were found in minor bleeding episodes between groups and no major bleeding was registered.
Limitations
Small sample size and open-label trial.
Conclusions
Long-term treatment with low-dose aspirin did not reduce the composite primary endpoint; however, there were reductions in secondary endpoints with fewer coronary events and renal outcomes. ClinicalTrials.gov Identifier: NCT01709994.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salicylates have been used since ancient times to relieve pain, fever, and inflammation. It was not until the mid-twentieth century when physicians recognized the potential antithrombotic properties of aspirin therapy and began to use it to prevent myocardial infarction (MI) [1]. Aspirin is an effective antithrombotic agent that inhibits the production of thromboxane (TxA2) and other prostaglandins by blocking the enzyme cyclooxygenase (COX-1). The antiplatelet action of acetylsalicylic acid (ASA) is achieved by a specific inhibition of COX-1 through an irreversible acetylation of serine-529. Inhibition of COX-1 results in complete inhibition of synthesis the pro-aggregating factor TxA2. As platelets are anucleated, aspirin-induced TxA2 inhibition will be fully restored only through the synthesis of new platelets approximately 7 days after aspirin discontinuation [2].
In comparison to the general population, individuals with chronic kidney disease (CKD) are at increased risk for cardiovascular disease (CVD) and death due to cardiovascular events (CVE) [3]. CVD is the leading cause of mortality in patients with any CKD stage [4]. Therefore, preventive measures for CVE are essential in patients of great importance in patients with CKD. Aspirin has been shown to be effective in reducing cardiovascular morbidity and mortality in high-risk patients who have experienced MI or stroke and is recommended as a primary prevention strategy for individuals with multiple risk factors such as hypertension, dyslipidemia, obesity, diabetes, or a family history of ischemic heart disease [5]. However, aspirin use for the primary prevention of CVD is controversial. In 2014, the Food and Drug Administration (FDA) warned that current evidence does not support the routine use of aspirin for primary prevention of heart attack or stroke in the general population [6]. This statement was based on the lack of strong evidence on a sufficient cardiovascular risk reduction, as well as on the potential harm derived from bleeding. In contrast, the US Preventive Services Task Force (USPSTF) recently issued guidelines endorsing aspirin use for primary prevention of CVD and colorectal cancer in specific populations [7].
Limited data exists regarding the use of antiplatelet agents in primary and secondary cardiovascular prevention in patients with CKD. This is partly due to the systematic exclusion of these patients from randomized clinical trials [8]. A meta-analysis by Palmer et al. [9] evaluated the effects of aspirin and clopidogrel in nine trials (all post hoc subgroup analyses for CKD) involving 9969 patients who had acute coronary syndrome or who were undergoing percutaneous coronary intervention and in 31 trials involving 11,701 patients with stable or no CVD. These authors concluded that the use of antiplatelet agents in patients with CKD had little or no effect on all-cause or cardiovascular mortality or on myocardial infarction. However, these authors acknowledged the limitations of low-quality or very low-quality evidence (i.e., significant heterogeneity in the study populations, considerable variation among the studies, and variations in the post hoc subgroup analyses of the trials). The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches-Chronic Kidney Disease Trial (ISCHEMIA-CKD; NCT01985360; http://www.ischemiackd.org/) is recruiting patients with moderate to severe ischemic heart disease and stage 4 to 5 CKD or end-stage renal disease comparing an initial management strategy of optimal medical therapy (OMT) alone with coronary revascularization in addition to OMT.
The American Diabetes Association and the American Heart Association recommend low-dose aspirin for adults with diabetes who have no previous history of vascular disease, a 10-year risk of CVD events that is greater than 10%, and no increased risk of bleeding [10], but no data are available about the primary cardiovascular prevention in diabetic CKD patients.
Additionally, there is concern over the chronic use of aspirin potentially increasing the risk of bleeding, particularly in patients with CKD who have abnormal platelet function [11]. Finally, scarce data are available on the relationship between low-dose aspirin and progression of renal disease. Thus, there is substantial uncertainty regarding the risk/benefit balance associated with the use of aspirin by CKD patients. Accordingly, the purpose of this randomized clinical trial (RCT) was to evaluate the effects and safety of low-dose aspirin for the primary prevention of CVD in CKD patients and its effect on renal disease progression.
Methods
Trial Design
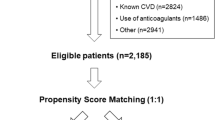
The AASER study is an interventional randomized, controlled, multicenter, open-label clinical trial to assess the potential effect of low-dose aspirin (100 mg/day) in the reduction of cardiovascular events in patients with CKD (ClinicalTrials.gov Identifier: NCT01709994). The study population included patients without previous CVE with stage 3 or 4 CKD (eGFR 15–60 ml/min/1.73 m2 of body surface area), according to the four-variable Modification of Diet in Renal Disease (MDRD4) equation. Patients were randomly assigned 1:1 to receive either aspirin 100 mg per day or standard care. Randomization was stratified by the presence of diabetes mellitus, since the diabetic patient has a higher cardiovascular risk, to avoid a disproportion in the number of diabetics included in each group. The study flow chart is shown in Fig. 1. Inclusion and exclusion criteria are detailed in ESM Appendix A.
Seven centers of the Community of Madrid participated in the study. However, due to logistical problems, the recruitment was not as expected. The majority of patients (all but twenty) were recruited in the same center. One hundred eleven patients were included in the clinical trial: 41 stage 3a (eGFR 45–59 ml/min/1.73 m2), 47 stage 3b (eGFR 30–44 ml/min/1.73 m2), and 23 stage 4 (15–29 ml/min/1.73 m2). Fourteen diabetic patients were randomized in standard therapy group and 19 in ASA group.
Visits were performed every 6 months. The following data was collected in all participants:
-
Anthropometric/clinical data (at every visit): age, gender, height, weight, body mass index, systolic and diastolic blood pressure, and heart rate.
-
Medical history including data on diabetes mellitus and cardiovascular risk factors such as dyslipidemia and hypertension.
-
Concomitant medication at each visit: renin-angiotensin system blockers, statins, and allopurinol. The dosage of antihypertensive drugs and lipid-lowering and uric acid-lowering agents was adjusted following the clinical criteria.
-
Laboratory data (at every visit): serum creatinine, hemoglobin, lipid parameters, serum fibrinogen, erythrocyte sedimentation rate, white cell count, and high-sensitivity C-reactive protein (CRP). The MDRD4 equation was used to estimate GFR. Albuminuria was measured in simple and 24-h urine samples. Plasma CRP was measured using a latex-based turbidimetric immunoassay on a Hitachi analyzer (Sigma Chemical Co.). Urine and blood parameters were assessed using standard laboratory methods in every single center. Participants were followed for a mean of 64.8 ± 16.4 months. The study was approved by the local ethics committees in accordance with the Declaration of Helsinki and all patients provided written informed consent.
Endpoints
The primary endpoint was composed of cardiovascular death, acute coronary syndrome (nonfatal MI, coronary revascularization, or unstable angina pectoris), cerebrovascular disease, heart failure, or nonfatal peripheral arterial disease (PAD). Secondary endpoints were fatal and nonfatal coronary events, renal events (defined as doubling of serum creatinine, ≥ 50% decrease in eGFR, or renal replacement therapy), and bleeding episodes. Renal event was defined as doubling of serum creatinine, an eGFR decrease ≥ 50%, or initiation of renal replacement therapy. The same independent researcher, blinded as to the therapeutic group, adjudicated renal and cardiovascular events in clinical documentation.
Cerebrovascular disease was defined as having a history of ischemic or hemorrhagic stroke, transient ischemic attacks (verified using computed tomography), or carotid artery stenosis > 70% (verified using a Doppler ultrasound). The diagnosis of PAD was based on the presence of intermittent claudication, angiography, or ultrasound-proven stenosis of the major arteries of the lower limbs, or ulcers caused by atherosclerotic disease or by surgery. Congestive heart failure was defined as left ventricular ejection fraction ≤ 40% in patients with congestive symptoms classified by the New York Heart Association (NYHA) in classes II to IV.
Safety
Bleeding events were collected during follow-up and divided in major and minor episodes according to the GUSTO (Global Use of Strategies to Open Coronary Arteries) classification [12]. Major bleeding included intracranial bleeding and bleeding associated with a hemoglobin decrease of more than 5 g/dl. Minor bleeding included spontaneous hematuria, hematemesis, and mild hemoglobin decreases less than 5 g/dl. Patients who suffered any bleeding episode during the clinical trial were censored.
Randomization List
The randomization list was generated by software that assigned the codes for all patients at each participating center in order of enrollment.
Statistical Analysis
Statistical analysis was performed by intention-to-treat. All statistical analyses were performed using IBM SPSS, version 21.0 (IBM Corp., Armonk, NY, USA) for Windows. Values are expressed as mean ± standard deviation (SD) or median (interquartile range) (IQR). Kaplan-Meier curves and the log-rank test were used to analyze renal and cardiovascular survival. Cox proportional hazard models were used to evaluate the risk of renal events, and the results were adjusted for several covariates. Univariate Cox regression (p < 0.1) was used to determine which covariates should be introduced in the multivariable model. Statistical significance is defined as a two-tailed p value of less than 0.05.
Results
Baseline characteristics, previous CVD history, concomitant medications, and laboratory parameters in each study group are shown in Table 1A, B.
Cardiovascular Outcomes
After a median follow-up of 64.8 months, 22 patients (17 (28%) in the control group and 5 (10%) in the ASA group experienced a primary composite endpoint. Primary composite endpoint included five congestive heart failure events, eight ischemic coronary events (one fatal MI), six stroke, and three cases of PAD. The distribution of primary endpoint in the two groups of patients during the trial is shown in Table 2. No significant differences were found in the primary composite endpoint between the ASA and standard care groups: HR 0.396 (0.146–1.076), p = 0.069 (Fig. 2a). However, regarding secondary endpoints, there were significant differences in fatal and nonfatal coronary events. Eight patients (13%) suffered a fatal or nonfatal coronary event in the control group in comparison to no events in the ASA group (log-rank, 5.997; p = 0.014) (Fig. 2b).
Renal Outcomes
eGFR decreased significantly in the standard group vs aspirin group (Tables 3 and 4). Seventeen patients (28%) in the control group (renal replacement therapy: nine patients and doubling of serum creatinine or ≥ 50% decrease in eGFR (Table 4): eight patients) reached the renal outcome in comparison with 3 patients (6%) (2 started dialysis therapy and 1 patient doubled serum creatinine) in the ASA group (log-rank, 5.849; p = 0.016) (Fig. 3).
Aspirin treatment was associated with a lower risk of renal disease progression in a model adjusted for age, baseline kidney function, and diabetes mellitus (HR, 0.272; 95% CI, 0.075–0.955; p = 0.042) (Table 5). But when we introduced the basal albuminuria into the model, the aspirin treatment did not significantly reduce the renal events (Table 6).
Safety
There were no differences in bleeding episodes (two in the standard care and three in the ASA group). No major bleeding episodes were observed during the trial.
Discussion
This is the first RCT to evaluate the role of aspirin in primary cardiovascular prevention and protection from renal disease progression in CKD patients. In the present study, no significant reduction in the primary composite endpoint could be demonstrated for aspirin. This is likely related to the small sample size and low number of events, as the p value approached significance. Nevertheless, it is striking that no patient treated with aspirin suffered from acute coronary events versus 8 patients who suffered them in the standard care group.
Aspirin is more effective in CVE prevention among patients with a higher cardiovascular risk. Thus, the greater the underlying risk, the greater the absolute benefit. For example, among patients enrolled in primary prevention trials, there was a nearly tenfold difference in the estimated absolute benefit, depending on baseline risk. For those with the lowest CVD risk, aspirin prevented approximately 0.15 nonfatal MI per 1000 person-years compared with 1.43 MI prevented per 1000 person-years in the highest risk populations [13]. In this sense, CKD patients have a very high cardiovascular risk, comparable to those patients who have had a prior cardiovascular event or diabetes, whose disease is considered a coronary artery disease risk equivalent [14]. Therefore, CKD patients may be hypothesized to represent a group of patients in whom the greatest benefit may be provided by the preventive use of aspirin. Nearly 30 years ago, the British Doctors Trial first evaluated whether aspirin can prevent MI. The trial, which randomized healthy male physicians to aspirin or placebo, reported a nonsignificant 3% reduction in the rate of nonfatal MI [15]. One year later, the Physicians’ Health Study reported a significant reduction in nonfatal MI (hazard ratio, 0.59; 95% CI, 0.47–0.74) [16]. Since those early studies, a total of ten high-quality trials have evaluated aspirin for the primary prevention of MI. The systematic review of these studies reported a reduction in the relative risk (RR) of nonfatal MI among those taking aspirin (RR, 0.78; 95% CI, 0.71–0.87) [10]. Taken together, these results suggest that primary prevention with aspirin reduces the risk of nonfatal MI. A retrospective propensity score (PS)-matched analysis of the effect of low-dose aspirin therapy on the development of CVD in CKD patients was recently published [17]. The incidence of a primary endpoint of any atherosclerotic CVD was significantly higher in aspirin users than in the non-users (p < 0.001). However, this was an observational study rather than a controlled interventional trial, in which coronary event was defined as significant coronary artery disease that required angioplasty, and fatal and nonfatal MI prevention with low-dose aspirin was not analyzed. To date, the only clinical trial that evaluated the use of aspirin in primary cardiovascular prevention and enrolled CKD patients was the HOT (Hypertension Optimal Treatment) study. In a post hoc analysis of this trial, the protection afforded by aspirin for MI increased as kidney function declined. The results suggested that for every 1000 persons with eGFR < 45 ml/min/1.73 m2 treated for 3.8 years, 76 major cardiovascular events and 54 all-cause deaths will be prevented while 27 excess major bleeds will occur [18].
The optimal management of ischemic heart disease remains controversial, which even more limited evidence to guide clinical decision-making in patients with CKD. ISCHEMIA-CKD trial will seek to answer more definitively the role of revascularization in patients with CKD and evidence of ischemia on stress testing. In this trial, patients are randomized to an invasive strategy of cardiac catheterization and OMT or an OMT alone [4]. In our clinical trial, we demonstrated a probable benefit of aspirin in the prevention of MI in CKD, but the small sample size and low number of events prevent us from drawing definitive conclusions.
Another relevant result from our clinical trial is that aspirin treatment decreased renal events (doubling of serum creatinine and renal replacement therapy) over 5 years of follow-up in a model adjusted for age, baseline eGFR, and diabetes. It is true that this beneficial effect was not significant when we introduced the basal albuminuria in the model, but the study does probably not have enough statistical power to include many variables in the multivariate model, so larger clinical trials will be needed to confirm these findings.
In the kidney, COX enzymes exert their physiologic regulatory functions in the macula densa, medulla, and interstitium [19].The products of COX enzymes and in particular the balance between Tx and prostacyclin production are crucial for kidney homeostasis [20]. Experimental studies showed that in the macula densa, COX enzymes favor renin production and are involved in the regulation of renal blood flow. In particular, in animal models, the administration of either aspirin or Tx receptor inhibitors was associated with improvements in renal plasma flow and eGFR values, suggesting a pathogenic role for Tx in the progression of renal damage [21,22,23,24]. However, current available data on the long-term effects of low-dose aspirin on kidney function and progression of CKD in humans are scarce and inconclusive. The first United Kingdom Heart and Renal Protection (UK-HARP-1) trial showed that low-dose aspirin use for 1 year in a mixed population of patients with native kidney CKD or kidney transplantation was not associated with faster progression of CKD [25]. Subsequently, in the post hoc subgroup analysis of the HOT trial, Jardine et al. reported that aspirin use did not affect renal function in the overall study population, but it was not powered to observe effects of low-dose aspirin on the renal outcome in patients within eGFR categories [15]. HOT mainly included diastolic hypertensive patients, and only 2.9% had an eGFR< 45 ml/min/1.73 m2, in contrast to our study, and duration of follow-up was shorter. Some large observational studies support a potential nephroprotective effect of aspirin. In a prospective cohort of 4494 US male physicians, aspirin intake significantly reduced the risk for decline in kidney function compared with those who never used aspirin in the group of subjects without cardiovascular risk factors [26]. In a retrospective cohort study of 3585 patients with CKD undergoing cardiac surgery, preoperative aspirin use was associated with a significant decrease in postoperative acute kidney injury [27]. In a recent observational cohort study, involving 800 patients with non-valvular atrial fibrillation, the use of aspirin (100 mg/day) was significantly associated with a reduced risk of CKD progression over 2 years of follow-up. In particular, patients not on aspirin had a threefold higher risk of progressing to an eGFR value < 45 ml/min per 1.73 m2 at the end of follow-up compared with those on aspirin [28]. Furthermore, levels of urinary 11-dehydro-TxB2 excretion were inversely associated with aspirin use and strongly predicted the annual eGFR decline during the 2-year follow-up period. A Swedish cohort study that investigated the decline of renal function at 5–7 years in 801 patients with CKD showed that chronic administration of aspirin was associated with a slower decline of renal function compared with untreated patients (mean difference of 0.8 ml/min per 1.73 m2) [29]. Conversely, the JPAD2 cohort study showed no effect of aspirin on kidney function in 2536 Japanese patients, but the allocation of patients to aspirin (81 or 100 mg daily) or not was at the physician discretion [30]. The LEDA (The renaL disease progression by aspirin in Diabetic pAtients) trial will be the first multicenter, double-blind, placebo-controlled trial to examine whether treatment with aspirin (100 mg daily) may preserve kidney function in adult patients with type 2 diabetes mellitus by assessing the annual decline of eGFR. The trial will also examine whether the potential renoprotective effects of aspirin might be partly due to inhibition of TxB2 production [2]. According to the clinicaltrial.gov site, the trial is expected to be completed by September 2018 (https://clinicaltrials.gov/ct2/show/NCT02895113; accessed December 24, 2017). Patients with eGFR < 30 ml/min/1.73 m2 will be excluded.
The question of whether the use of aspirin by patients with CKD increases the risk for bleeding is controversial. The UK-HARP-1 trial [22] and the Dialysis Outcomes and Practice Patterns Study (DOPPS) [31] showed no increased risk of major bleeding or gastrointestinal bleeding, respectively, in CKD patients on 100 mg/day aspirin. However, the meta-analysis by Palmer et al. [9] disclosed an increased risk of major and minor bleeding events with the use of antiplatelet agents in patients with CKD. These findings were generated using low-quality evidence, with considerable variation in trial duration, heterogeneity in the definitions and assessment of bleeding outcomes, and reliance on subgroup data from major trials. The incidence of a bleeding event in our study was lower than reported in the meta-analysis and no patient had a major bleeding episode. Thus, the results of the current trial regarding major bleeding risk are in line with those of the UK-HARP-1 and DOPPS studies.
Limitations and Strengths
The present study has some limitations. The main one is the relatively small sample size. In this regard, the low number of events precluded any definite conclusions. In addition, although the study was designed as a multicenter study, most of the patients were recruited in the same center. For this reason, the recruitment period had to be prolonged for 2 years and we cannot assure that the patients were recruited consecutively. Also, participants with diastolic heart failure were not accounted for in this study, and this fact could be a potential bias in the heart failure diagnosis. By last, the events were all site-reported and not independently adjudicated; this fact could influence in the collection of some events as PAD and could have influenced the results.
Despite these limitations, the study also has several strengths. This is the first published RCT addressing this important issue and recruitment of CKD patients without cardiovascular disease is extremely difficult. In addition, despite the low number of cardiovascular events, important differences were found in MI incidence between aspirin and standard treatment. Additionally, we present the first data derived from an RCT on the effect of low-dose aspirin on the progression of renal function decline.
In conclusion, low-dose aspirin did not prevent primary composite cardiovascular endpoint but may prevent MI in CKD patients and slow the rate of progression of renal disease. Further RCTs are warranted to confirm these findings.
References
Miner J, Hoffhines A. The discovery of aspirin’s antithrombotic effects. Tex Heart Inst J. 2007;34(2):179–86.
Violi F, Targher G, Vestri A, Carnevale R, Averna M, Farcomeni A, et al. Background effect of aspirin on renal disease progression in patients with type 2 diabetes: a multicenter, double-blind, placebo-controlled, randomized trial. The renaL disease progression by aspirin in diabetic patients (LEDA) trial. Rationale and study design. Am Heart J. 2017;189:120–7.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Mathew RO, Bangalore S, Lavelle MP, Pellikka PA, Sidhu MS, Boden WE, et al. Diagnosis and management of atherosclerotic cardiovascular disease in chronic kidney disease: a review. Kidney Int. 2017;91:797–807.
Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative metaanalysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
US Food and Drug Administration. Information for consumers (drugs): use of aspirin for primary prevention of heart attack and stroke. Available at: https:// www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm390574.htm. Accessed 17 Mar 2017.
Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: recommendations from the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):836–45.
Charytan D, Kuntz RE. The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int. 2006;70:2021–30.
Palmer SC, Di Micco L, Razavian M, et al. Effects of antiplatelet therapy on mortality and cardiovascular and bleeding outcomes in persons with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med. 2012;156:445–59.
Desai D, Ahmed HM, Michos ED. Preventing cardiovascular disease in patients with diabetes: use of aspirin for primary prevention. Curr Cardiol Rep. 2015;17(3):566.
Weigert AL, Schafer AI. Uremic bleeding: pathogenesis and therapy. Am J Med Sc. 1998;316:94–104.
Lenderink T, Boersma E, Ruzyllo W, GUSTO IV-ACS Investigators, et al. Bleeding events with abciximab in acute coronary syndromes without early revascularization: an analysis of GUSTO IV-ACS. Am Heart J. 2004;147(5):865–73.
Guirguis-Blake JM, Evans CV, Senger CA, O'Connor EA, Whitlock EP. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):804–13.
Cedeño Mora S, Goicoechea M, Torres E, Verdalles Ú, Pérez de José A, Verde E, et al. Cardiovascular risk prediction in chronic kidney disease patients. Nefrologia. 2017;37(3):293–300.
Peto R, Gray R, Collins R, Wheatley K, Hennekens C, Jamrozik K, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed). 1988;296(6618):313–6.
Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321(3):129–35.
Kim AJ, Lim HJ, Ro H, Ko KP, Han SY, Chang JH, et al. Low-dose aspirin for prevention of cardiovascular disease in patients with chronic kidney disease. PLoS One. 2014;9(8):e104179. Published online 2014 Aug 5
Jardine MJ, Ninomiya T, Perkovic V, Cass A, Turnbull F, Gallagher MP, et al. Aspirin is beneficial in hypertensive patients with chronic kidney disease: a post-hoc subgroup analysis of a randomized controlled trial. J Am Coll Cardiol. 2010;56(12):956–65.
Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–84.
Harris RC, Breyer MD. Physiological regulation of cyclooxygenase-2 in the kidney. Am J Physiol Renal Physiol. 2001;281(1):F1–11.
Okumura M, Imanishi M, Yamashita T, Yamamura Y, Kim S, Iwao H, et al. Renal production of thromboxane and prostaglandins in a rat model of type 2 diabetes. Life Sci. 2000;66(5):371–7.
Boffa JJ, Just A, Coffman TM, Arendshorst WJ. Thromboxane receptor mediates renal vasoconstriction and contributes to acute renal failure in endotoxemic mice. J Am Soc Nephrol. 2004;15(9):2358–65.
Lomnicka M, Karouni K, Sue M, Wessel LA, Bing RJ. Effects of nonsteroidal anti-inflammatory drugs on prostacyclin and thromboxane in the kidney. Pharmacology. 2003;68(3):147–53.
Boffa JJ, Just A, Coffman TM, et al. Thromboxane receptor mediates renal vasoconstriction and contributes to acute renal failure in endotoxemic mice. J Am Soc. 2004;15(9):2358–65.
Baigent C, Landray M, Leaper C, Altmann P, Armitage J, Baxter A, et al. First United Kingdom Heart and Renal Protection (UK-HARP-I) study: biochemical efficacy and safety of simvastatin and safety of low-dose aspirin in chronic kidney disease. Am J Kidney Dis. 2005;45:473–84.
Kurth T, Glynn RJ, Walker AM, Rexrode KM, Buring JE, Stampfer MJ, et al. Analgesic use and change in kidney function in apparently healthy men. Am J Kidney Dis. 2003;42(2):234–44.
Yao L, Young N, Liu H, Li Z, Sun W, Goldhammer J, et al. Evidence for preoperative aspirin improving major outcomes in patients with chronic kidney disease undergoing cardiac surgery: a cohort study. Ann Surg. 2015;261(1):207–12.
Pastori D, Pignatelli P, Perticone F, Sciacqua A, Carnevale R, Farcomeni A, et al. Aspirin and renal insufficiency progression in patients with atrial fibrillation and chronic kidney disease. Int J Cardiol. 2016;223:619–24.
Evans M, Fored CM, Bellocco R, Fitzmaurice G, Fryzek JP, McLaughlin JK, et al. Acetaminophen, aspirin and progression of advanced chronic kidney disease. Nephrol Dial Transplant. 2009;24(6):1908–18.
Okada S, Morimoto T, Ogawa H, Sakuma M, Soejima H, Nakayama M, et al. Is long-term low-dose aspirin therapy associated with renal dysfunction in patients with type 2 diabetes? JPAD2 Cohort Study. PLoS One. 2016;11(1):e0147635.
Ethier J, Bragg-Gresham JL, Piera L, et al. Aspirin prescription and outcomes in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2007;50:602–11.
Funding
AASER was supported by Sociedad Española de Nefrologia (SEN) and Sociedad Madrileña de Nefrología (SOMANE). MG, GFJ, DA, AO, and JL are supported by ISCIII RETIC REDINREN RD016/009 and FEDER funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Goicoechea, M., de Vinuesa, S.G., Quiroga, B. et al. Aspirin for Primary Prevention of Cardiovascular Disease and Renal Disease Progression in Chronic Kidney Disease Patients: a Multicenter Randomized Clinical Trial (AASER Study). Cardiovasc Drugs Ther 32, 255–263 (2018). https://doi.org/10.1007/s10557-018-6802-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-6802-1