Abstract
Purpose
Cardiotoxicity is a well-known side effect of chloroquine. Several studies have proposed chloroquine as a potential anti-diabetic treatment but do not address this problem. The current study investigated the effect of ex vivo chloroquine treatment on (1) heart function and glucose uptake, (2) mitochondrial function and (3) in vivo treatment on heart function.
Methods
Control or obese male Wistar rats were used throughout. Dose responses of increasing chloroquine concentrations versus vehicle on cardiac function were measured using isolated, Langendorff-perfused hearts whilst glucose uptake and cell viability were determined in ventricular cardiomyocytes. Mitochondrial function was assessed with a Clark-type oxygraph (Hansatech) after ex vivo perfusion with 30 μM chloroquine versus vehicle. Animals were treated orally with 5 mg/kg/day chloroquine for 6 weeks.
Results
Acute chloroquine treatment of 10 μM was sufficient to significantly decrease heart function (p < 0.05) whilst 30 μM significantly reduced heart rate (p < 0.05). Chloroquine became toxic to isolated cardiomyocytes at high concentrations (100 μM), and had no effect on cardiomyocyte glucose uptake. Ex vivo treatment did not affect mitochondrial function, but chronic low-dose in vivo chloroquine treatment significantly decreased aortic output and total work in hearts (p < 0.005).
Conclusion
Low and intermediate chloroquine doses administered either chronically or acutely are sufficient to result in myocardial dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chloroquine and its synthetic analogue hydroxychloroquine are widely used for anti-malarial treatment, and more recently also for the effective treatment of autoimmune diseases such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) [1]. Clinical studies have shown that both chloroquine and hydroxychloroquine can improve glucose metabolism in patients with insulin-resistant diabetes mellitus [2]. Moreover, patients treated with chloroquine for RA or SLE showed a decreased incidence of developing diabetes mellitus [3, 4].
The metabolic effects of chloroquine include increased insulin secretion, decreased insulin clearance, improved peripheral glucose uptake and decreased dyslipidaemia [5,6,7]. Chloroquine is an acidotropic, lysosomotropic agent that prevents endosomal acidification and consequently inhibits lysosome-autophagosome fusion and degradation [8], effectively protecting insulin against endosomal degradation [9]. The drug increases cellular glucose uptake through the promotion of GLUT4 trafficking to, and fusion with, the cellular plasma membrane by increasing cellular Ca2+ uptake [10]. Moreover, chloroquine is a potent activator of the insulin-responsive protein, protein kinase B (PKB, also known as Akt), and significantly enhances glycogen synthesis through the phosphorylation of glycogen synthase kinase 3β (GSK-3β), which makes it an attractive potential anti-diabetic drug [11].
However, chloroquine toxicity has been observed at both therapeutic and high doses, especially when administered rapidly, and include cardiovascular effects such as vasodilation, hypotension, suppressed myocardial function and cardiac arrhythmias [12]. Moreover, hypoglycaemia has been reported in non-diabetic patients and is considered a rare, but serious side effect [13]. Interestingly, low-dose chloroquine treatment (3.5 mg/kg twice a week for 8 weeks that equates to approximately 40 mg/kg/week for a 70-kg human) mitigated the development of atherosclerosis in ApoE−/− knockout mice and improved metabolic abnormalities in ob/ob and db/db mice [14]. Conversely, a more recent study has shown that chloroquine treatment (10 mg/kg for 14 days) worsened cardiac performance in type 1 diabetes, whilst hearts from db/db mice exhibited poorer diastolic function when compared to hearts obtained from either control or heterozygous db/+ mice [15]. The study concluded that chloroquine decreased diastolic function in type 2 diabetes (T2D), and noted that this could be due to suppressed autophagy in the diabetic heart. Left ventricular (LV) diastolic dysfunction is also prominent in T2D patients without any history of heart disease [16].
Autophagy plays an important role in cardiovascular homeostasis [17] and has been found to be upregulated in cardiac pressure overload (PO) hypertrophy [18]. Moreover, both chloroquine and hydroxychloroquine can bind phospholipids within myocytes and lead to the accumulation of pathological metabolic products, such as glycogen [19]. Although it has been shown that high dosage chloroquine treatment can decrease cardiac PO hypertrophy, it also resulted in significant impairments in cardiac relaxation and contractility [18]. On a cellular level, chloroquine treatment increased mitochondrial fragmentation and cristae destruction which was associated with increased oxidative stress and mitochondrial dysfunction [18]. Similar results were noted in cortical neurons where chloroquine treatment significantly increased mitochondrial DNA damage, inhibited key mitochondrial functions and, consequently, resulted in significant alterations in cellular metabolism [20]. When translating the chloroquine concentrations used by [18, 20] to human doses, using the body surface area [21] to calculate an equivalent human dose in milligram per kilogram per day, the dosage used in these studies are equivalent to 4.05 mg/kg/day and 3.24 mg/kg/day respectively. This falls within the prescribed range of 2.3 mg/kg/day chloroquine and 5 mg/kg/day for hydroxychloroquine in patients treated for SLE to prevent the development of retinopathy at higher doses [22]. However, Kanamori et al. [15] noted diastolic dysfunction in mice treated with a human-equivalent dose of as little as 0.81 mg/kg/day (10 mg/kg/day in mice), and raises the question whether the low doses of chloroquine, as reported by [11, 14], can also induce cardiotoxicity.
More than 70 cases of cardiotoxicity in patients, primarily due to chloroquine treatment, have been reported in literature [23], and it is suggested that cardiotoxicity is often not reported due to difficult diagnosis [24]. An increasing number of chloroquine cardiotoxicity cases at low doses are being reported and have led to the suggestion that an electrocardiogram (ECG) should be included with annual ophthalmological check-ups in patients that use chloroquine for SLE and RA [25, 26]. Moreover, detection of chloroquine-induced cardiotoxicity through ECG can improve the patient outcome, if detected early [27].
In light of the role of chloroquine in glucose metabolism, improvement in metabolic syndrome symptoms in obesity and calls in literature for further investigation into the drug as a potential therapeutic agent for insulin resistance [11, 28], this study aimed to (1) evaluate the effects of chloroquine on (i) heart function and (ii) cardiomyocytes of young, lean male Wistar rats; (2) evaluate ex vivo low-dose treatment of the heart on mitochondrial function in diet-induced obese male Wistar rats as a potential underlying mechanism for cardiovascular dysfunction; and (3) examine the effect of low-dose, chronic treatment of rats on a high caloric diet on cardiac function.
Materials
Chloroquine diphosphate salt (C6628), insulin (I6634), propidium iodide (PI; P4864) and phloretin (P7912) were purchased from Sigma Aldrich. 2-Deoxy-D-[3H] glucose (2-DG; NET549005MC) was purchased from Perkin Elmer. Sodium pentobarbitone (Eutha-naze) was obtained from Bayer.
Methods
Animals
Adult male Wistar rats were housed at the Central Research Facility (Stellenbosch University) in a temperature-controlled (~ 23 °C) environment with a 12-h light/dark cycle. The rats were divided into three groups according to the aims: (1) Baseline controls consisting of adult male Wistar rats fed standard rat chow (bodyweight 200–300 g; n = 31), (2) male Wistar rats of approximately 7 weeks old weighing 190 ± 10 g fed either a high-sugar diet (DIO n = 17) or (3) a high-sugar plus high-fat diet (HFD n = 9) for 16 weeks and their age-matched controls fed standard rat chow for the duration (AMC_DIO, n = 15 and AMC_HFD n = 10 (Table 1). Only male rats were used during this study, based on the observation by [14] that low-dose chloroquine treatment did not result in any sex-based differences in their study that made use of both male and female mice.
Experimental Design
The animals were randomly assigned to control and diet groups. Within the baseline control group, animals were assigned to cardiomyocyte preparation for cell viability determination (n = 3), glucose uptake (n = 3) and acute ex vivo chloroquine perfusion to determine contractile strength and heart rate at increasing chloroquine concentrations (untreated n = 7; 10 μM, n = 7; 30 μM, n = 7; and 50 μM, n = 4).
Mitochondrial dysfunction in response to acute, ex vivo chloroquine treatment was determined in DIO with known insulin resistance that was randomly assigned to treated (30 μM chloroquine, n = 8) or non-treated (vehicle control n = 8) groups, whilst their age-matched controls were divided into treated (30 μM, n = 9) and non-treated (vehicle control n = 7) groups.
Lastly, the study aimed to determine the effect of chronic low dosage chloroquine treatment in a diet that induces insulin resistance. The animals were treated as follows: HFD (n = 4) and AMC_HFD (n = 6) received 5 mg/kg/day chloroquine in jelly cubes, whilst the non-treatment controls HFD (n = 5) and AMC_HFD (n = 4) received jelly cubes without chloroquine during the last 6 weeks of the diet.
Biometric Data Collection
The animals were anaesthetized with an intra-peritoneal administered overdose of 160 mg/kg sodium pentobarbitone and euthanized by exsanguination. Once the animals showed no pedal reflex following a foot pinch, the hearts were rapidly excised and arrested in ice-cold (4 °C) Krebs-Henseleit buffer (KHB; pH 7.4 containing in millimolar; 119 NaCl, 24.9 NaHCO3, 4.7 KCl, 1.2 KH2PO4, 0.6 MgSO4·7H2O, 0.59 Na2SO4, 1.25 CaCl2·12H2O and 10 glucose). After anaesthetizing, the animals were weighed and non-fasting glucose was measured by means of a tail prick and glucometer. Visceral (perirenal and perigonadal) fat deposits were removed and weighed post-exsanguination. The adiposity index was calculated as the ratio of visceral fat mass to total body mass (visceral fat/body mass) in grams and expressed as percentage (Table 2).
Oral glucose tolerance tests (OGTTs) were performed at week 10 on the HFD animals and AMC_HFD to determine insulin sensitivity prior to chloroquine treatment. Animals were fasted overnight; basal glucose levels for each rat were taken by means of a tail prick and glucometer prior to being gavaged with sucrose (1 g/kg). Glucose levels were monitored at intervals for a period of 2 h using blood from the same prick (Fig. 4).
Cell Viability Determination
Cell viability was determined with a PI staining assay in response to increasing chloroquine concentrations. Briefly, ventricular cardiomyocytes were isolated from basal, control hearts (n = 3). Isolated cardiomyocytes were prepared essentially as previously reported [29]. In brief, rats were anaesthetized with sodium pentobarbital (160 mg/kg); the hearts were quickly removed and retrogradely perfused with a calcium-free medium (HEPES buffer 6 mM KCl, 1 mM Na2HPO4, 0.2 mM NaH2PO4, 1.4 mM MgSO4, 128 mM NaCl, 10 mM HEPES, 5.5 mM glucose, 2 mM pyruvate, pH 7.4, 37 °C, equilibrated with oxygen) for 5 min. The perfusion was then switched to the second medium (HEPES buffer containing 0.7% bovine serum albumin (BSA), fraction V, fatty acid free, 1.1 mg collagenase/mL and 15 mM 2,3-butanedione monoxime (BDM)) for 15 min after which the calcium concentration was raised in two steps to 200 μM over the next 10 min. Perfusion was continued to a total time of approximately 35 min. The ventricles were then carefully separated from the atria, minced with tweezers and suspended in the second medium given above but containing 1% BSA, 1% BSA fraction V, fatty acid free and half the concentration of collagenase and BDM. The suspension was placed in a cell culture flask in a shaking benchtop incubator (37 °C) and digested for a further 15 min, where after the calcium concentration was gradually raised to 1.25 mM over the next 5 minutes. The isolated cells were filtered through a nylon net (mesh size 200 × 200 μm) and gently spun down (3 min, 100 rpm). The pellet obtained was re-suspended in HEPES buffer containing 1.25 mM CaCl2, 2% BSA (fraction V, fatty acid free) and the cells allowed to settle for 3–4 min. The supernatant was carefully aspirated, and the loose pellet re-suspended in the same buffer and allowed to recover from the trauma of isolation for 1 h before experimentation. The viability of the isolated cardiomyocytes routinely exceeded 80% as determined by the trypan blue exclusion method. The cells were treated with 10 μM (low dose), 50 μM (intermediate dose) and 100 μM (high dose) chloroquine for 45 min in duplicate. The use of a 100 μM chloroquine was chosen based on previous studies that showed that chloroquine can act as a potent activator of Akt and promote glucose uptake in vitro in L6-muscle cells [11, 14]. Pellets, obtained by gentle centrifugation, were re-suspended in fresh HEPES buffer prior to the addition of 5 μM PI. The samples were incubated in the dark at room temperature (~ 23 °C) for 15 min before fluorescence was measured. Twenty thousand events were acquired per condition using flow channel two of a Becton Dickinson FACSCalibur (BD Biosciences).
Glucose Uptake (2-DG)
Radiolabelled 2-deoxy glucose (2-DG) uptake by isolated cardiomyocytes was determined essentially as previously described [29]. After recovery, the cells were spun down into a loose pellet (3 min at 100 rpm), washed twice and suspended in a suitable volume of the substrate-free assay medium. Cardiomyocytes (approximately 0.5 mg protein) were assayed in a total volume of 750 μl of oxygenated medium containing (in mmol/L) KCl 6, Na2HPO4 1, NaH2PO4 0.2, MgSO4 1.4, NaCl 128, HEPES 10, CaCl2 1.25 plus 2% bovine serum albumin, fraction V, and fatty acid free (pH 7.4). The cells were pre-incubated for 15 min in a shaking benchtop incubator (37 °C) with or without phloretin (400 μM) for measurement of non-carrier-mediated glucose uptake. Phloretin was dissolved in DMSO and stored as 6.4 mM stock solution and diluted with medium immediately before use. Each experimental series was then incubated with or without 100 nM insulin or 10, 50 and 100 μM chloroquine under the same conditions for 30 min after which glucose uptake was initiated by addition of 2-deoxy-D-[3H]glucose (1.5 μCi/ml; final concentration 1.8 μM) (2-DG). Glucose uptake was allowed to progress for a further 30 min before the reaction was stopped by adding 50 μl phloretin to give a final concentration of 400 μM. The cells were then microfuged for 1 min; the pellet was washed twice in medium to remove extracellular 2-DG and dissolved in 1 M NaOH. Afterwards, samples were diluted with dH2O to 0.5 M NaOH. Fifty microlitre of this was used to assay protein of every aliquot with 3 technical repeats by the method of Lowry et al. [30] whilst the rest was counted for radioactivity. The specific activity of the radiolabelled solution was determined and the 2-DG uptake calculated as picomole 2DG/mg prot/30 min. Decay was counted with an LS 6500 multi-purpose scintillation counter (Beckman) (in duplicate). Uptake of 2-DG was calculated as ratio to basal values.
Rate Pressure Product and Heart Rate
Excised hearts from baseline, control animals were cannulated via the aorta and perfused retrogradely with KHB gassed with 95% oxygen and 5% carbon dioxide at a constant pressure of 100 cm H2O. A syringe inflatable balloon, constructed from compliant and non-elastic plastic cling wrap, was inserted into the left ventricle via the pulmonary vein and left atrium. The balloon was inflated with distilled water to achieve an end diastolic pressure of 10 mmHg. A pressure transducer connected to the balloon enabled the measurement of heart rate and pressure throughout the experiments. Hearts were stabilised for 20 min, after which they were perfused in a recirculating manner with KHB (untreated group, n = 7) or 10 μM (n = 7), 30 μM (n = 7) and 50 μM (n = 4) chloroquine for 10 min. Left ventricular developed pressure (LVDevP; diastolic pressure subtracted from systolic pressure) and rate pressure product (RPP; LVdevP multiplied by heart rate) were calculated.
Mitochondrial Function Analysis
Langendorff Perfusions (for Mitochondrial Analysis)
Excised hearts from the DIO and AMC_DIO were cannulated and perfused with KHB gassed with 95% oxygen and 5% carbon dioxide at a constant pressure of 100 cm H2O. Hearts were stabilised for 20 min, after which they were perfused in a recirculating manner with KHB: AMC_DIO, n = 7; DIO, n = 9; or 30 μM chloroquine: AMC_DIO, n = 8; DIO, n = 8 for 20 min. Perfusions were performed using sodium light due to chloroquine’s reported light sensitivity. Protein determination for the mitochondrial data was performed with a Lowry assay [30].
Mitochondrial Isolation and Oxidative Phosphorylation Determination
Immediately following the perfusion period, the atria were removed and the ventricles were placed in ice-old mitochondrial isolation buffer (0.018 M KCl, 0.01 M EDTA, pH 7.4). Mitochondrial isolation was performed with a standard differential centrifugation protocol [31]. Briefly, the heart tissue was homogenised with a Heidolph SilentCrusher M, followed by a slow centrifugation step (755×g for 10 min at 4 °C) in order to obtain a pellet containing the nuclei, cell membranes and remaining tissue. The supernatant was transferred to a clean centrifuge tube and centrifuged at 18800×g for 10 min at 4 °C to obtain a mitochondrial pellet. The pellet was re-suspended in ice-cold mitochondrial isolation buffer with a 2 cm3 Potter-Elvehjem glass-teflon homogeniser and stored on ice until use.
Mitochondrial oxygen consumption was analysed with a Clarke-type oxygraph (Hansatech, as described by Maarman et al. [31]) immediately following isolation. Two chambers containing a glutamate or palmitoyl-L-carnitine assay buffer (250 mM sucrose, 10 mM TRIS-HCl (pH 7.4), 8.5 mM K2HPO4-3H2O, 2 mM malate and 5 mM glutamate or 5 mM palmitoyl-L-carnitine; pH 7.4), equilibrated to ambient oxygen levels at 25 °C, were analysed in parallel. Data was captured with Hansatech Plus software. Oxygen consumption in the presence of ADP (state 3), oxygen consumption after complete utilisation of ADP (state 4) and state 3 oxygen consumption after 20 min anoxia followed by reoxygenation were noted.
Work Heart Perfusions
Aortic output (mL/min) and total work (mWatts) were determined with Morgan work heart perfusions. Briefly, excised hearts from insulin-resistant rats and their age-matched controls (HFD and AMC_HFD groups) that were treated with 5 mg/kg/day chloroquine over a 6-week period were mounted on a working heart perfusion system. After a 10-min stabilisation period in the retrograde mode, the hearts were perfused in working mode for 10 min. Working heart perfusion was performed at a preload of 15 cm H2O and an afterload of 100 cm H2O. A pressure transducer connected to the aortic line was used to determine heart rate and pressure development whilst aortic and cardiac output was measured manually and total work performed was calculated as described by Kannengiesser et al. [32].
Statistical Analysis
Data is presented as the mean ± standard deviation. Statistical analyses were performed using unpaired Student’s t tests, one-way analysis of variance (ANOVA) or two-way ANOVA with a Bonferroni post hoc test in GraphPad Prism 6.0. Differences with a p value of less than 0.05 were considered significant.
Results
The Effect of Chloroquine on Isolated Cardiomyocyte Viability and Glucose Uptake
This study tested chloroquine-induced cardiotoxicity (10 μM, 50 μM and 100 μM) on isolated adult ventricular cardiomyocytes. The cardiomyocytes were treated with increasing concentrations of chloroquine and stained with PI to determine cell viability (n = 4). Compared to the untreated group, the low (10 μM) and intermediate (50 μM) chloroquine concentrations had no effect on cell viability, expressed as percentage increase in PI uptake (107 ± 4.6%, p = 0.20 and 105.3 ± 3.0%, p = 0.15 respectively). Treatment with 100 μM chloroquine significantly decreased cell viability of isolated cardiomyocytes when compared to the untreated group (106.8 ± 2.1%, p = 0.03) (Fig. 1a).
a Percentage change in propidium iodide uptake in isolated ventricular cardiomyocytes in response to increasing concentrations of chloroquine (Ch). Asterisk indicates p = 0.03 versus untreated with unpaired t test (n = 3). b Glucose uptake, expressed relative to the basal group, in isolated ventricular cardiomyocytes in response to insulin and increasing chloroquine concentrations. Double asterisks indicate p = 0.009 versus untreated with one-way ANOVA (n = 3)
Glucose uptake was measured in response to increasing chloroquine concentrations (10 μM, 50 μM and 100 μM) in isolated ventricular cardiomyocytes (n = 3). Insulin was used as a positive control (1.72 ± 0.15 fold-change relative to untreated, p = 0.009). Chloroquine concentrations had no effect on 2-DG uptake (Fig. 1b) when compared to the control group.
Acute Ex Vivo Chloroquine Treatment Decrease Heart Rate Pressure Product and Heart Rate
Langendorff perfusions, using the balloon model, were conducted on hearts from control animals to assess cardiac function during drug delivery. Cardiac function was significantly reduced after 10 min of treatment with each of the chloroquine concentrations (n = 7 per group except 50 μM chloroquine treatment, n = 4) compared to the untreated vehicle group (n = 7) (Fig. 2a). The decrease in rate pressure product (RPP) was caused by a decrease in left ventricular developed pressure and heart rate (Fig. 2b, c respectively). Fifty percent of the hearts treated with 50 μM chloroquine ceased to function within the first 5 min of treatment and we therefore omitted the highest chloroquine concentration, namely 100 μM, from the perfusion experiments. We included an intermediate chloroquine concentration (30 μM) that resulted in a significant decrease in RPP, whilst maintaining heart function.
Cardiac function following treatment of hearts with increasing chloroquine concentrations. a Rate pressure product (mm Hg × beats/min). b Left ventricular developed pressure (mm Hg). c Heart rate (beats/min). Asterisk indicates p < 0.05, double asterisks indicate p < 0.005, triple asterisks indicate p < 0.0001 versus untreated with one-way ANOVA (n = 7 per group, except 50 μM n = 4)
Effect of Acute Single-Dose Chloroquine Treatment on Complex I-Linked Mitochondrial Respiration in Obesity
This study investigated the effect of a single, intermediate dose (30 μM) chloroquine on oxidative phosphorylation of hearts obtained from obese (as determined with adiposity index; Table 2), DIO male Wistar rats. Neither diet nor acute, intermediate-dose ex vivo chloroquine treatment (30 μM) altered the respiratory control index (RCI, state 3/state 4; Fig. 3a) or the ATP synthesis rate (Fig. 3b). Interestingly, chloroquine treatment significantly (p < 0.001) reduced complex I-linked respiration (state 3 oxygen consumption; glutamate plus malate [GM] buffer) in isolated mitochondria from obese hearts (DIO) when compared to chloroquine-treated controls (AMC_DIO, Fig. 3c). No significant differences were seen in fatty acid oxidation with palmitoyl-L-carnitine and malate (PCM) as a substrate (Fig. 3d).
Isolated mitochondrial oxidative phosphorylation from age-matched control (AMC_DIO) and diet-induced obese (DIO) hearts perfused with or without 30 μM chloroquine. a Respiratory control rate (RCR). b ATP synthesis rate in a glutamate+malate (GM) or palmitoyl-L-carnitine+malate (PCM). c Oxygen consumption rate with glutamate (GM) as substrate. d Oxygen consumption rate with PCM as substrate. Double asterisks indicate p < 0.005 versus untreated with two-way ANOVA and Bonferroni post hoc test (n values: untreated AMC_DIO = 7, untreated DIO = 9; chloroquine treated AMC_DIO = 8. Treated DIO = 8)
Biometric Data
Animals in the HFD group were found to be insulin resistant after 10 weeks on the high-fat diet compared to animals in the AMC_HFD group (Fig. 4). Both the HFD and the DIO diets caused a significant (p < 0.0001) increase in the adiposity index when compared to the relevant AMC groups (Table 2). Chloroquine treatment did not decrease the significant increase observed in the adiposity index (thus could not decrease visceral fat) in the HFD animals compared to AMC (p < 0.0106); however, within HFD animals, chloroquine treatment reduced the adiposity index, albeit not significantly (p < 0.0678). No differences were seen in adiposity index or non-fasting glucose levels after 6 weeks of chloroquine treatment in the HFD group.
Oral glucose tolerance tests were performed on untreated HFD and untreated AMC_HFD male Wistar rats at 10 weeks of diet prior to chronic, low-dose chloroquine treatment over a further 6-week period of diet. Asterisk indicates p < 0.05, double asterisks indicate p < 0.01 versus AMC_HFD determined with a repeated measures two-way ANOVA; n = 12 per group
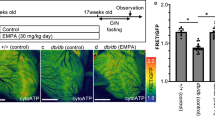
The Effect Chronic Chloroquine Treatment on Cardiac Function
In order to investigate the effect of long-term, low-dose chloroquine treatment in obese, insulin-resistant animals, aortic output and total work were determined as indicators of heart function. Low-dose chronic chloroquine treatment resulted in significantly reduced aortic output (Fig. 5a) and total work (Fig. 5b) in both the AMC_HFD and HFD groups.
Cardiac function in control (AMC_HFD) and high-fat diet (HFD) hearts in response to chloroquine treatment. a Aortic output (mL/min). b Total work (mWatts). Double asterisks indicate p < 0.005 versus untreated with two-way ANOVA and Bonferroni post hoc test; n values: Control untreated = 4, control chloroquine = 6. HFD untreated = 5, HFD chloroquine = 4
Discussion
Chloroquine and hydroxychloroquine treatment have previously been reported to improve lipoprotein metabolism abnormalities [6] as well as lower blood glucose in non-insulin–dependent diabetes mellitus in obese patients treated chronically for up to 18 months [33] or acutely (3 days, [6]). However, a small but significant reduction in fasting blood glucose levels (hypoglycaemia) was also noted in control patients compared to diabetic patients [2], and severe cardiotoxicity has been reported in SLE and RA patients [23, 24] as well as children with malaria [34] that were treated with chloroquine. Most studies that observed cardiotoxicity in animal models evaluated high chloroquine dosages, which correspond well with previous literature that reports cardiotoxicity in patients at high doses. Nonetheless, very few of the animal studies concerned with chloroquine-induced glucose uptake take the effect of heart function and different diets in account, and this study therefore aimed to address this. Moreover, a recent report of diastolic dysfunction has been noted in a type 2 diabetes mouse model [15] at a very low dose of chloroquine equivalent to a human dose of 0.81 mg/kg/day.
The DIO (high-sugar diet) is known to induce insulin resistance and have been associated with cardiovascular dysfunction [35], whilst the high-fat, high-sugar diet (HFD in our study) is strongly associated with metabolic alterations such as obesity and insulin resistance which can lead to cardiovascular dysfunction in mice [36]. Moreover, the chronic intake of high-fat compared to high-sucrose–fed mice results in different types of glucose intolerance [37], which highlights the importance of diet in drug evaluation studies. In this study, obesity was induced (as measured with an adiposity index) in both DIO and HFD rats, possibly due to the hyperphagic nature of the diets which result in increased caloric intake. Chronic chloroquine intake did not improve the non-fasting blood glucose levels in the treated HFD animals compared to their age-matched controls, but it did slightly improve the adiposity index of treated HFD animals compared to non-treated HFD animals (p = 0.0678; Table 2), albeit not significantly.
Previous studies have found that chloroquine can improve symptoms of metabolic syndrome in obesity [14], as well as increase cellular glucose uptake [10] and insulin-mediated PKB/Akt activity in HFD, insulin-resistant rats at low doses (7 mg/kg/week) [11]. Moreover, low-dose chloroquine treatment (7 mg/kg/week) has been shown to improve glucose tolerance, insulin sensitivity and hepatic PKB/Akt signalling, although it did not affect serum metabolites nor fasting blood glucose in rats fed a Western diet (42% fat-containing diet) for 8 weeks. Interestingly, the same study found that chloroquine could significantly decrease total aortic and aortic root atherosclerosis in an ApoE− atherosclerotic mouse model [28]. The dosages used in these studies are very low when equating it to the human-equivalent dose (39.73 mg/week) [21], and would suggest that the current clinical doses used for SLE and RA can be reduced considerably to induce anti-diabetic effects.
However, in light of the cardiotoxicity reported at low [15] and clinically relevant doses [18], the question remains whether cardiovascular dysfunction can be observed at the reported human equivalent low dose of 0.81 mg/kg/week [15] in an insulin resistant high-fat–fed rat model. The animal-based studies that have proposed the use of chloroquine as an anti-diabetic drug [11, 28] did not report on the cardiotoxic effect in either HFD, western diet–fed or age-matched control animals. This study did not aim to evaluate the efficacy of chloroquine as an anti-diabetic drug but rather compare heart function between chloroquine-treated obese, insulin-resistant and their age-matched controls. Due to the reported hypoglycaemic effect of chloroquine in non-diabetic patients, this study evaluated chronic, low-dose chloroquine treatment in a known, insulin-resistant (Fig. 4) obese male Wistar rat model (Table 2) with a human-equivalent dose of 0.81 mg/kg/day.
This study shows that chloroquine may only become cardiotoxic at high concentrations (100 μM), when administered in a single dose to isolated cardiomyocytes (Fig. 1a). Interestingly, chloroquine had no effect on cardiomyocyte glucose uptake (2DG) at low (10 μM), intermediate (50 μM) or high (100 μM) concentrations (Fig. 1a), in contrast to previous reports that showed a significant increase in glucose uptake in insulin-treated L6 myoblasts when compared to controls [11]. Similarly to the current study, a more recent report found that chloroquine did not increase glucose uptake in C2C12 cells, but rather resulted in decreased intracellular Ca2+ which was associated with a concomitant decrease in glucose transport [38]. This suggests that the increased glucose uptake observed by Halaby et al. [11] was mediated by the combination of chloroquine and insulin treatment rather than chloroquine alone, which, albeit sufficient to activate hepatic and muscle PKB/Akt [11, 28, 38], does not stimulate insulin secretion, as previously suggested [5]. The disparity between the use of high doses of chloroquine in vitro, compared to the effects seen in vivo at low dosages, was highlighted in a study that investigated the prevention of endosomal degradation of insulin [9] and suggested that the endosomal accumulation of chloroquine in vivo can result in micromole concentrations that would allow it to elicit the effects seen in vitro.
Increased PKB/Akt and GSK-3β activation were only measured in animals that were fed either a HFD [11] or Western diet [28] and were not compared to low-dose chloroquine treatment (3.5 mg/kg/day) in control animals. This study set out to determine whether a single dose of chloroquine is sufficient to influence heart function in chow-fed control male Wistar rats, and found that low (10 μM), intermediate (30 μM) and high (50 μM) chloroquine treatment significantly reduced heart rate and left ventricular pressure (presented as rate pressure product) in a Langendorff balloon model (Fig. 3). Interestingly, it has been suggested that the hypoglycaemic effect of most anti-malarial drugs is due to the closure of pancreatic beta cell K+ ATP channels which increases insulin secretion [39]. On the other hand, activation of these channels has been associated with cardioprotection [40]. It has also been suggested that the severe cardiac effects of anti-malarial drugs are due to their ion channel blocking properties, which in the case of chloroquine is on the transient outward K+ current in isolated ventricular cardiomyocytes [34, 41]. Moreover, the repolarisation of ventricular cardiomyocytes is mainly through outward currents of K+ ions, which, when impaired, can lead to an intracellular accumulation of K+ ions and a delay in polarisation resulting in a prolongation of the QT interval [34]. This could possibly explain the reduction in contractility that we observed in response to chloroquine treatment (Fig. 2).
Chloroquine has also been suggested to decrease metabolic syndrome symptoms associated with obesity. However, chloroquine is an autophagic inhibitor and can potentially result in the accumulation of dysfunctional mitochondria. This study thus set out to determine whether chloroquine can influence myocardial oxidative phosphorylation in obesity. Acute low-dose chloroquine treatment (30 μM) did not result in mitochondrial dysfunction in either AMC_DIO or DIO hearts (Fig. 3). This was unexpected in light of the role of chloroquine in autophagic suppression and the previously observed decrease in ATP content [15]. However, chloroquine treatment significantly (p < 0.001) reduced complex I–linked respiration (state 3 oxygen consumption; glutamate plus malate buffer) in isolated mitochondria from obese hearts (DIO) when compared to chloroquine-treated controls (AMC_DIO, Fig. 3c). No significant differences were seen in fatty acid oxidation with palmitoyl-carnitine and malate as a substrate (Fig. 3d). This could suggest a potential mechanism for the side effects observed in lean control patients such as hypoglycaemia, which is not observed in obese patients.
Chloroquine treatment is, however, often accumulative over time and can be prescribed for extensive periods in the case of RA and SLE. It has been argued that long-term chloroquine treatment can result in the accumulation of pathological metabolic products within lysosomes which contribute towards cardiovascular dysfunction [19]. Moreover, chloroquine is commonly used as an inhibitor of autophagy in the laboratory and was found to worsen cardiac function in both type 1 and T2D [15]. The suppression of autophagy, which plays an important role in cardiovascular homeostasis and insulin signalling in myocardial metabolism [17], has been associated with the development of diabetic cardiomyopathy. Kanamori et al. [15] showed that both AMPK activity as well as ATP content was reduced in T2D (db/db) mouse hearts when treated with chloroquine (10 mg/kg/day) for 14 days, and also found that it exacerbated insulin resistance, increased LV end diastolic pressure, dilated LV dimension and worsened both systolic and diastolic dysfunction. However, the latter study found that chloroquine did not significantly influence cardiac function in db/+ non-diabetic mice. Conversely to this, we found that chronic low-dose chloroquine (5 mg/kg/day) over a 6-week period significantly decreased heart function irrespective of diet (Fig. 5). The dose used in the study by Kanamori et al. [15] on mice, when adjusted to a human dose [21], is the same as the dose that was used in this study, when adjusted to an equivalent human dose (0.81 mg/kg/day).
Our results suggest that both low and intermediate chloroquine doses administered either chronically or acutely are sufficient to result in myocardial dysfunction, but not mitochondrial dysfunction irrespective of diet. We did, however, observe a significant increase in NADH-linked respiration (state 3, glutamate-malate substrate) in myocardial mitochondria from age-matched obese rats, which was not associated with an increase in the ATP synthesis rate (QO2 state3). Although this was not linked with mitochondrial dysfunction (as an output of the respiratory control index), it does suggest that an acute treatment of chloroquine can result in uncoupling in mitochondria from control but not obese rats. Moreover, the accumulative effect of chloroquine over a long term as well as autophagic suppression cannot be disregarded.
Conclusion
This study shows that single-dose chloroquine treatment only becomes cardiotoxic to isolated cardiomyocytes at high concentrations (100 μM, Fig. 2a), but has no effect on cardiomyocyte glucose uptake (2DG) at low (10 μM), intermediate (50 μM) or high (100 μM) concentrations (Fig. 2b). However, in line with previously reported suppressed myocardial function, we show that chronic low-dose chloroquine significantly decreases heart function irrespective of diet, and this highlights the need to include control as well as Western or HFD animal models when evaluating the effect of chloroquine treatment. Moreover, a single, intermediate chloroquine dose (30 μM) significantly decreased RPP in control hearts, but did not result in mitochondrial dysfunction in either AMC_DIO or DIO hearts. Although the chronic low-dose administered in this study is higher than was previously reported to alleviate insulin resistance [11] and metabolic syndrome [14], it is considerably lower than the current clinical dose prescribed for RA and SLE, and suggests that further research should be done with regard to clinically relevant chronic doses that can alleviate metabolic syndrome without resulting in cardiovascular dysfunction.
In conclusion, the role of chloroquine in cardiac toxicity still remains to be elucidated. Literature suggests that there are two potential mechanisms: short-term blockage of the K+ channels and accumulation of Ca2+ that can result in decreased heart function, tachycardia and prolongation of the QT interval; and long-term effects such as the accumulation of metabolic products and autophagy suppression that can result in mitochondrial dysfunction. These effects also appear to be diet dependent, and therefore, we suggest that chloroquine might not be a “one-size-fits all” anti-diabetic drug.
References
Hage MP, Badri MR, Azar ST. A favorable effect of hydroxychloroquine on glucose and lipid metabolism beyond its anti-inflammatory role. Ther Adv Endocrinol Metab. 2014;5:77–85.
Smith GD, Amos TA, Mahler R, Peters TJ. Effect of chloroquine on insulin and glucose homoeostasis in normal subjects and patients with non-insulin-dependent diabetes mellitus. Br. Med. J. (Clin. Res. Ed). 1987;294:465–7.
Wasko MCM, McClure CK, Kelsey SF, Huber K, Orchard T, Toledo FGS. Antidiabetogenic effects of hydroxychloroquine on insulin sensitivity and beta cell function: a randomised trial. Diabetologia. 2015;58:2336–43.
Chen Y-M, Lin C-H, Lan T-H, Chen H-H, Chang S-N, Chen Y-H, et al. Hydroxychloroquine reduces risk of incident diabetes mellitus in lupus patients in a dose-dependent manner: a population-based cohort study. Rheumatology. 2015;54:1244–9.
Asamoah KA, Robb DA, Furman BL. Chronic chloroquine treatment enhances insulin release in rats. Diabetes Res Clin Pract. 1990;9:273–8.
Powrie JK, Shojaee-Moradie F, Watts GF, Smith GD, Sönksen PH, Jones RH. Effects of chloroquine on the dyslipidemia of non-insulin-dependent diabetes mellitus. Metabolism. 1993;42:415–9.
Powrie JK, Smith GD, Shojaee-Moradie F, Sonksen PH, Jones RH. Mode of action of chloroquine in patients with non-insulin-dependent diabetes mellitus. Am J Physiol Metab Am Physiol Soc. 1991;260:E897–904.
Shintani T, Klionsky DJ. Autophagy in health and disease: a double-edged sword. Science (80-. ). 2004;306:990–5.
Bevan AP, Krook A, Tikerpae J, Seabright PJ, Siddle K, Smith GD. Chloroquine extends the lifetime of the activated insulin receptor complex in endosomes. J Biol Chem. 1997;272:26833–40.
Zhou Q, Yang X, Xiong M, Xu X, Zhen L, Chen W, et al. Chloroquine increases glucose uptake via enhancing GLUT4 translocation and fusion with the plasma membrane in L6 cells. Cell Physiol Biochem. 2016;38:2030–40.
Halaby M-J, Kastein BK, Yang D-Q. Chloroquine stimulates glucose uptake and glycogen synthase in muscle cells through activation of Akt. Biochem. Biophys. Res. Commun. Elsevier Inc. 2013;435:708–13.
Ben-Zvi I, Kivity S, Langevitz P, Shoenfeld Y. Hydroxychloroquine: from malaria to autoimmunity. Clin Rev Allergy Immunol. 2012;42:145–53.
Cansu DÜ, Korkmaz C. Hypoglycaemia induced by hydroxychloroquine in a non-diabetic patient treated for RA. Rheumatology. 2008;47:378–9.
Schneider JG, Finck BN, Ren J, Standley KN, Takagi M, Maclean KH, et al. ATM-dependent suppression of stress signaling reduces vascular disease in metabolic syndrome. Cell Metab. 2006;4:377–89.
Kanamori H, Takemura G, Goto K, Tsujimoto A, Mikami A, Ogino A, et al. Autophagic adaptations in diabetic cardiomyopathy differ between type 1 and type 2 diabetes. Autophagy. 2015;11:1146–60.
Poulsen MK, Henriksen JE, Dahl J, Johansen A, Gerke O, Vach W. Left ventricular diastolic function in type 2 diabetes mellitus prevalence and association with myocardial and vascular disease. Circ Cardiovasc Imaging. 2010;3:24–31.
Riehle C, Abel ED. Insulin regulation of myocardial autophagy. Circ J. 2014;78:2569–76.
Chaanine AH, Gordon RE, Nonnenmacher M, Kohlbrenner E, Benard L, Hajjar RJ. High-dose chloroquine is metabolically cardiotoxic by inducing lysosomes and mitochondria dysfunction in a rat model of pressure overload hypertrophy. Physiol Rep. 2015;3:1–18.
Page RL II, O’Bryant CL, Cheng D, Dow TJ, Ky B, Stein CM, et al. Drugs that may cause or exacerbate heart failure. Circulation. 2016;134:e32–e69
Redmann M, Benavides GA, Berryhill TF, Wani WY, Ouyang X, Johnson MS, et al. Inhibition of autophagy with bafilomycin and chloroquine decreases mitochondrial quality and bioenergetic function in primary neurons. Redox Biol Elsevier B.V. 2017;11:73–81.
Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2007;22:659–61.
Marmor MF, Kellner U, Lai TYY, Melles RB, Mieler WF, Lum F. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology Elsevier. 2016;123:1386–94.
Costedoat-Chalumeau N, Hulot J-S, Amoura Z, Delcourt A, Maisonobe T, Dorent R, et al. Cardiomyopathy related to antimalarial therapy with illustrative case report. Cardiology. 2007;107:73–80.
Tönnesmann E, Stroehmann I, Kandolf R, Strach K, Musshoff F, Tiemann K, et al. Cardiomyopathy caused by longterm treatment with chloroquine: a rare disease , or a rare diagnosis? J Rheumatol. 2012;39:1099–103.
Cervera A, Espinosa G, Cervera R, Font J, Ingelmo M. Cardiac toxicity secondary to long term treatment with chloroquine. Ann Rheum Dis. 2001;60:301–4.
Yogasundaram H, Putko BN, Tien J, Paterson DI, Cujec B, Ringrose J, et al. Hydroxychloroquine-induced cardiomyopathy: case report, pathophysiology, diagnosis, and treatment. Can J Cardiol Can Cardiovasc Soc. 2014;30:1706–15.
Yogasundaram H, Hung W, Paterson ID, Sergi C, Oudit GY. Chloroquine-induced cardiomyopathy: a reversible cause of heart failure. ESC Hear Fail. 2018;5:372–5.
Razani B, Feng C, Semenkovich CF. P53 is required for chloroquine-induced atheroprotection but not insulin sensitization. J Lipid Res. 2010;51:1738–46.
Fischer Y, Rose H, Kammermeier H. Highly insulin-responsive isolated rat heart muscle cells yielded by a modified isolation method. Life Sci. 1991;49:1679–88.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin henol reagent. J Biol Chem. 1951;193:265–75.
Maarman G, Marais E, Lochner A, Toit EF. Effect of chronic CPT-1 inhibition on myocardial ischemia- reperfusion injury ( I / R ) in a model of diet-induced obesity. Cardiovasc Drugs Ther. 2012;26:205–16.
Kannengiesser GJ, Lubbe WF, Opie LH. Experimental myocardial infarction with left ventricular failure in the isolated perfused rat heart. Effects of isoproterenol and pacing. J Mol Cell Cardiol Elsevier. 1975;7:135–51.
Gerstein HC, Thorpe KE, Taylor DW, Haynes RB. The effectiveness of hydroxychloroquine in patients with type 2 diabetes mellitus who are refractory to sulfonylureas - a randomized trial. Diabetes Res Clin Pract. 2002;55:209–19.
White NJ. Cardiotoxicity of antimalarial drugs. Lancet Infect Dis. 2007;7:549–58.
Huisamen B, Dietrich D, Bezuidenhout N, Lopes J, Flepisi B, Blackhurst D, et al. Early cardiovascular changes occurring in diet-induced, obese insulin-resistant rats. Mol Cell Biochem. 2012;368:37–45.
Burchfield JG, Kebede MA, Meoli CC, Stöckli J, Whitworth PT, Wright AL, et al. High dietary fat and sucrose result in an extensive and time-dependent deterioration in health of multiple physiological systems in mice J Biol Chem. 2018;293:5731–5745.
Sumiyoshi M, Sakanaka M, Kimura Y. Nutrient physiology, metabolism, and nutrient-nutrient interactions chronic intake of high-fat and high-sucrose diets differentially affects glucose intolerance in mice. J Nutr. 2006;136:582–7.
Spears LD, Tran A V, Qin CY, Hobbs SB. Chloroquine increases phosphorylation of AMPK and Akt in myotubes. Heliyon. 2016 Mar;2(3):e00083.
Wagner M, Riepe KG, Eberhardt E, Volk T. Open channel block of the fast transient outward K+current by primaquine and chloroquine in rat left ventricular cardiomyocytes. Eur J Pharmacol Elsevier B.V. 2010;647:13–20.
Grover GJ, Garlid KD. ATP-sensitive potassium channels: a review of their cardioprotective pharmacology. J Mol Cell Cardiol. 2000;32:677–95.
Sánchez-Chapula JA, Salinas-Stefanon E, Torres-Jácome J, Benavides-Haro DE, Navarro-Polanco RA. Blockade of currents by the antimalarial drug chloroquine in feline ventricular myocytes. J Pharmacol Exp Ther. 2001;297:437–45.
Funding
We acknowledge funding from the South African National Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All applicable international, national, and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted. This study was approved by the Stellenbosch University Research Ethics Committee: Animal Care and Use (Protocol number SU-ACUM12-00040; SU-ACUD16-0079) and complied with the accepted national and international standards for the use of animals in research as stipulated in the South African National Standards 10386: 2008. This article does not contain any studies with human participants performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blignaut, M., Espach, Y., van Vuuren, M. et al. Revisiting the Cardiotoxic Effect of Chloroquine. Cardiovasc Drugs Ther 33, 1–11 (2019). https://doi.org/10.1007/s10557-018-06847-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-06847-9