Abstract
Acute kidney injury (AKI) is one of the most common complications during hospitalization in various clinical settings. The goal of this review was to assess the incidence of AKI in acute myocardial infarction patients (AMI), how this incidence is affected by the diverse definitions, and if there is variability in the reported rates over recent years. Additionally, we sought to appraise the impact of AKI on short- and long-term prognosis of these patients. Finally, we report on the current preventive measures as they are suggested in the current guidelines of various societies, we comment on the evidence that support them, and we review the literature for other proposed therapeutic strategies, which either failed to prove their efficacy or they are not adequately confirmed yet. Due to the heterogeneity in AKI definition and in the population studied of the published data, the incidence of AKI ranged from 5.2 to 59%. A recent meta-analysis reported a median value of 15.8%. All studies assessing AKI-related prognosis in AMI patients suggested that presence of AKI has detrimental effect on patients prognosis, raising mortality two- to threefold not only during the 30 first days but also during the first year after the acute event. Various treatment modalities have been proposed for prevention of AKI in AMI patients; however, the majority of them failed to prove their efficacy in the clinical trial arena. Hydration, use of iso- or low-osmolar agents at the lowest possible dose during coronary interventions, and use of statins have been proposed among others. Nonetheless, the prevalence of AKI after an AMI still remains high today and therefore it is crucial for the practicing physician to be aware of its presence and for the scientific community to identify novel measures for a more efficacious prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is known that acute kidney injury (AKI) is one of the most frequent complications during hospitalization of a patient, with detrimental effects on his prognosis in a variety of clinical scenarios including abdominal aortic aneurysm repair surgery [1], coronary angiography [2], cardiopulmonary bypass surgery [3], and critically ill patients in the intensive care unit [4]. Furthermore, recent evidence suggested a strong correlation between cardiac and kidney function, which engendered the term “cardiorenal syndrome” in the heart failure and in the acute coronary syndrome (ACS) setting [5]. Within this context, it is reasonable to assess the incidence and also the prognosis of AKI in patients with acute myocardial infarction (AMI).
A fair amount of research endeavored to answer the aforementioned query. However, one of the major problems one has to encounter when assessing the accumulated data is the heterogeneity in the definition of AKI, as more than 30 proposed terms were in use until the last decade [6]. In 2004, Acute Dialysis Quality Initiative (ADQI) developed the Risk, Injury, Failure, Loss, and End-stage kidney disease (RIFLE) criteria, which was the first attempt to reach a consensus [7]. In 2007, the Acute Kidney Injury Network (AKIN) published the AKIN criteria [8], and finally in 2012, the Kidney Disease Improving Global Outcomes (KDIGO) released their criteria which build off of the RIFLE criteria and the AKIN criteria [9]. The result is that there are at least three incumbent definitions and classifications for AKI (Table 1), not considering the contrast-induced nephropathy definition, ensuing in studies a lack of homogeneity, and hobbling the efforts to extract solid conclusions about the pathophysiology and the epidemiology of the disease.
Apart from assessing the incidence of AKI and its associated prognosis in patients with AMI, the identification of the preventive measures which can inhibit the occurrence of this detrimental complication is also of great importance. Numerous preventive strategies have been applied, with poor outcomes most of the time. This therapeutic shortcoming could be associated with the management strategies of AMI patients which include the quick transfer of the patient to the catheterization laboratory and the administration of contrast media. The use of contrast media is additionally per se nephrotoxic and furthermore the prompt response does not provide adequate time to implement the possible preventive measures. In that way, the conclusions regarding the true efficacy of these measures are less solid.
The goal of this review was to assess the incidence of AKI in AMI patients, how this incidence is affected by the diverse definitions, and if there is variability in the reported rates over recent years. Additionally, we sought to appraise the impact of AKI on short- and long-term prognosis of these patients. Finally, we reported on the current preventive measures as they are suggested in the current guidelines of various societies, we commented on the evidence that support them, and we reviewed the literature for other proposed therapeutic strategies, which either failed to prove their efficacy or they are not adequately confirmed yet.
Incidence of Acute Kidney Injury in Acute Myocardial Infarction Patients
The incidence of AKI in AMI patients as published in the medical literature fluctuates from 5.2 to 59%. This broad fluctuation is the result of the heterogeneity which characterizes the relevant clinical studies. The source of their heterogeneity stems not only from the AKI definition used but also from the clinical characteristics of the study population. A comprehensive presentation of the published studies which reported on AKI incidence in AMI patients is cited in Table 2 [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75].
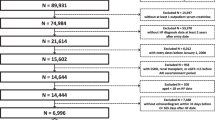
One of the largest studies was drawn from the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry-Get With the Guidelines (GWTG), a nationwide sample of AMI patients admitted to 383 hospitals in the United States. The study enrolled 59,970 patients hospitalized with AMI [59]. The researchers used the AKIN criteria and they concluded that for the period from July 2008 to September 2009 the incidence of AKI was 16.1%. Using the same database, other researchers had similar results regarding AKI incidence (16.5%) for the time span between 2008 and 2012 including 76,500 AMI patients from 581 hospitals [33]. In the largest observational study including 147,007 elderly Medicare patients admitted for AMI from January 1994 through February 1996 as a part of the Cooperative Cardiovascular Project, an incident rate of AKI of 19.4% was reported [69].
The patients who undergo urgent coronary artery bypass grafting (CABG) constitute a particular category of AMI patients rather susceptible to AKI. In the HORIZONS-AMI and ACUITY trials, the patients who underwent percutaneous coronary intervention (PCI) had 16.1% frequency rate of AKI [40]. In contrast, in a study in which AMI patients were treated with CABG, the incident rate was nearly doubled (31.9%) [25]. Other possible predictors of AKI development in patients with AMI are hemodynamic instability and ejection fraction levels. When researchers assessed patients with cardiogenic shock, they reported that the incidence rate of AKI surged to 55% [75]. By comparison, in two other studies that reported AKI rates in AMI patients with preserved ejection fraction, the incidence rates were only 12.9% [57] and 6.2% [16].
An interesting debate is whether AKI incidence depends on the definition used. Two studies addressed this issue and assessed the same patients using different criteria (AKIN and RIFLE criteria) yielding contradictory results. The first concluded that AKIN criteria provide greater sensitivity than RIFLE criteria (AKI incidence 9.6 vs. 3.9% in favor of AKIN criteria); however, the second reported opposite results (23.9 vs. 15.8% in favor of RIFLE criteria) [22, 76]. Similarly, other researchers applied the KDIGO and RIFLE criteria on AMI patients showing that KDIGO surpass RIFLE criteria in AKI detection (36.6 vs. 14.8%) [53]. Finally, the comparison between AKIN criteria and Contrast-Induced Acute Kidney Injury (CI-AKI) criteria favored the second as more sensitive (10.7 vs. 17.4%) [17]. It is more than obvious that applying different definitions each time (using more strict or more liberal criteria) yields different incidence rates increasing or decreasing sensitivity and specificity each time.
Based on our review, we identified only one meta-analysis, which investigated the occurrence of AKI in AMI patients [77]. This analysis comprised 36 studies, with incidence ranging from 6.3 to 36.6% and a median value of 15.8%. Furthermore, it is worthy to cite two more papers, which investigated the fluctuation of AKI prevalence over time. The first one included 31,532 AMI patients hospitalized from 2000 to 2008 and reported that it steadily declined from 26.6% in 2000 tο 19.7% in 2008 [78]. The decline was steeper among the patients treated with PCI (from 24.6 to 16.5%) in comparison with those treated conservatively (from 29.4 to 27%). The second one extracted data from a single center and reported a linear decline in the incidence of AKI (P value for trend 0.038) among 4307 ST elevation myocardial infarction patients from 2000 to 2015 [79].
Numerous studies have been published assessing possible predictors for AKI occurrence. Several risk scores have been developed in order to predict AKI; however, there are only a few that focused solely in patient with AMI. Among the most commonly cited risk factors for AKI are (a) reduced kidney function at presentation (defined as previous kidney disease, increased baseline creatinine levels, or decreased baseline glomerular filtration rate), (b) age, (c) hemodynamic instability (defined as the presence of shock, decreased systolic blood pressure, or use of intra-aortic balloon pump/inotropes), (d) heart failure (defined as previous history of heart failure, Killip class upon presentation, decreased ejection fraction, or increased left ventricular systolic ejection fraction), (e) coronary artery disease characteristics [defined as previous myocardial infarction, PCI, or CABG, presence of multi-vessel disease, anterior myocardial infarction, size of myocardial infarction, ST elevation or non-ST elevation myocardial infarction as an indication, catheterization that includes a PCI, emergency setting, thrombolysis in myocardial infarction (TIMI) flow post-PCI, or time to reperfusion], and (f) contrast volume used. Other predictors include various co-morbidities (anemia, diabetes mellitus, peripheral vascular disease, or hypertension) and possible nephrotoxic drugs (diuretics, metformin, or drugs that exert their action on renin-angiotensin-aldosterone axis, especially mineralocorticoid receptor antagonists) [80] (Fig. 1).
Risk factors for AKI occurrence. AKI, acute kidney injury; CABG, coronary artery bypass grafting; DM, diabetes mellitus; EF, ejection fraction; GFR, glomerular filtration rate; HF, heart failure; HTN, hypertension; IABP, intra-aortic balloon pump; LVEDP, left ventricular end-diastolic pressure; MI, myocardial infarction; MRA, mineralocorticoid receptor antagonist; NSTEMI, non-ST elevation myocardial infarction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; SBP, systolic blood pressure; STEMI, ST elevation myocardial infarction; TIMI, thrombolysis in myocardial infarction
For the last two decades, interventional (PCI) rather medical treatment is the preferred strategy among patients presenting with AMI. Therefore, the use of contrast agents is warranted in the majority of AMI patients rendering these agents among the most commonly present and more easily modifiable risk factors for AKI occurrence, especially the type and the volume of the agent used. Contrast agents have been shown to cause the following detrimental changes within the glomerular and tubular apparatus: renal vasoconstriction, resulting in a rise in intrarenal resistance (decrease in renal blood flow and glomerular filtration rate and medullary hypoxia); epithelial vacuolization and dilatation and necrosis of proximal tubules; potentiation of angiotensin II effects, reducing nitric oxide and causing direct constriction of descending vasa recta, leading to formation of reactive oxygen species; increasing active sodium re-absorption in the thick ascending limbs of Henle’s loop (increasing O2 demand and consequently medullary hypoxia); direct cytotoxic effects on endothelial and tubular epithelial cells; and reducing cell survival, due to decreased activation of kinases involved in cell survival/proliferation [81].
According to our knowledge, there are no published studies assessing differences in the incidence of AKI in AMI patients depending on the type of infarction (ST elevation vs. non-ST elevation myocardial infarction). Review of the published observational AKI studies did not reveal significant differences on AKI incidence rate between ST elevation and non-ST elevation myocardial infarction. The only reported difference is the effect of time to reperfusion on AKI incident rates. Regarding occurrence of AKI, ST elevation myocardial infarction patients are more sensitive to time to reperfusion. However, there is a bulk of evidence suggesting that large either in size (as assessed by circulating levels of necrotic myocardial enzymes) or by location (anterior) myocardial infarctions are associated with an increased incidence of AKI and are considered as possible risk factors for future AKI [82].
Short-Term and Long-Term Prognosis
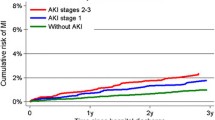
All studies investigating the toll that AKI might have on prognosis are suggesting a detrimental effect both for the short term and the long term in AMI patients. This detrimental effect was related neither with the follow-up period nor with AKI definition. As it was expected, it has been shown that AMI patients complicated with AKI have higher in-hospital mortality. Interestingly in these patients, this trend of increased mortality remains constant also out of hospital, even 3 years after their discharge [69]. The problem of heterogeneity among relevant studies still characterizes the assessment of AKI impact on prognosis. In Fig. 2 [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], these studies are summarized by reporting mean values for cumulative hazard ratios for mortality or major adverse cardiovascular events during hospitalization (7.9, 95% CI 2.5–13.2), up to 1 year since the index event (3.5, 95% confidence interval (CI) 2.7–4.3) and beyond 1 year (3.9, 95% CI 2.6–5.3).
Short-term and long-term prognosis of AMI patients complicated with AKI. Bars represent mean values for cumulative hazard ratios for mortality or MACE during hospitalization, up to 1-year follow-up since the index event and longer than 1 year using different criteria for AKI (AKIN, RIFFLE, CIN-AKI, and arbitrary criteria). For in-hospital prognosis, the following studies were used: [10, 15, 21, 26, 31, 32, 38, 43, 46, 49, 59, 61, 62, 64, 66, 71,72,73, 75]. For short-term prognosis, the following studies were used: [25, 28, 32,33,34,35, 41, 53, 55, 56, 60, 70]. For long-term prognosis, the following studies were used: [11, 15,16,17, 20, 22, 29, 31, 37, 40, 48, 50, 52, 65, 67,68,69, 71]. AKI, acute kidney injury; AKIN, Acute Kidney Injury Network; AMI, acute myocardial infarction; CIN, contrast-induced nephropathy; KDIGO, Kidney Disease Improving Global Outcomes; MACE, major adverse cardiovascular events; RIFLE, Risk, Injury, Failure, Loss and End-stage kidney disease
As expected, in-hospital mortality is higher in patients who develop AKI with reported hazard ratios (HR) from 2 to over 30. Regarding long-term mortality, data cited suggest that it increases additively with longer follow-up periods as well as with increasing AKI severity. In a study of Fox et al., who utilized data from the ACTION Registry-GWTG, from 383 hospitals in the USA between July 2008 and September 2009, it was shown that in-hospital mortality was higher in patients with more advanced AKI (mild AKI: HR 2.4, 95% CI 2–2.7; moderate AKI: HR 4.5, 95% CI 3.9–5.1; severe AKI: HR 12.6, 95% CI 11.1–14.3) [59]. In the same study, there was a progressive increase in mortality rates, even in patients with minor increases in serum creatinine of 0.1 mg/dL, below the threshold of 0.3 mg/dL which is used in AKIN/KDIGO criteria [59]. Utilizing more recent data from (from 2008 to 2012), Mody et al. similarly reported that 1-year mortality increased in a dose-dependent manner across increasing severity of AKI [33]. Another study encompassed patients from two multicenter randomized trials (HORIZONS-AMI and ACUITY) showing a temporal increase in mortality rate for patients undergoing PCI from 4.9% at 30 days to 9.8% at 1 year [35]. A similar temporal trend in increasing mortality was shown also for patients undergoing CABG from 6.7% at 30 days to 10.4% at 1 year [25]. Other researchers assessed AMI patients 10 years after their initial hospitalization and reported not only that mortality rates were proportionate to the corresponding AKI severity stage but also that this association continued to be significant even when death events occurring during the first 3 years were excluded from the analysis [69]. This finding may insinuate that the prognostic impact of AKI in AMI patients is not constraint only for the period of the acute event.
During recent years, an interesting notion has been postulated according which transient increases in creatinine (especially with that seen with diuretics or renin-angiotensin-aldosterone system medication use in heart failure patients) have no impact on patient prognosis. Several studies endeavored to elucidate this hypothesis. In the PREMIER study, only persistent AKI had statistically significant association with 4-year mortality compared to transient AKI (persistent AKI: HR 1.59, 95% CI 1.20–2.11 vs. transient AKI: HR 1.43, 95% CI 0.97–2.09) [65]. In contrast, other studies concluded that both transient and persistent AKI deteriorate patients’ prognosis [50, 72]. To complicate things further, when researchers in another study divided AKI patients not only according to its duration but additionally according to its severity, only patients with transient mild AKI had similar prognosis compared to patients who did not developed AKI (HR for 3-year mortality 1.2, 95% CI 0.6–2.3, P = 0.640) [68]. Patients with moderate/severe but transient AKI were characterized by a poorer prognosis (HR for 3-year mortality 1.7, 95% CI 1.1–2.8, P = 0.026) [68].
Another interesting notion is whether the use of different AKI definitions has an effect in the accuracy of predicting AMI patients’ prognosis. When RIFLE and KDIGO criteria were compared, the later criterion not only classified more patients as suffering from AKI but also characterized patients with worse prognosis [53]. This could be clinically translated as KDIGO criteria having greater sensitivity without losing their prognostic importance. Under the same notion, comparison between RIFLE and AKIN criteria showed that they both signal poor prognosis for AMI patients (RIFLE: HR for 5-year mortality 6.49, 95% CI 1.98–21.29, P = 0.002 vs. AKIN: HR 6.68, 95% CI 2.06–21.6, P = 0.002); however, AKIN criteria detected more AKI cases (9.6 vs. 3.9%) [76]. In contrast, another similar study showed that even though patients classified as suffering from AKI by AKIN criteria had worse prognosis than those detected by RIFLE, the latter classification yielded greater sensitivity [22]. Finally, another study comparing AKIN criteria with the CI-AKI definition showed that AKIN criteria had better correlation with 1-year mortality than the CI-AKI definition (AUC 0.798 vs. 0.775, P = 0.033) [17]. Fuelling the debate, a recent study suggested that a relative increase in serum creatinine of more than > 35% compared to admission baseline levels has the best correlation with the patients’ mortality [29].
The only relevant meta-analysis showed that AKI-associated mortality in AMI patients is approximately threefold during the first 30 days (ΗR 3.1, 95% CI 2.6–3.6) and approximately twofold during the first year (ΗR 2.2, 95% CΙ 1.9–2.6) compared to patients who do not develop AKI [77]. Another interesting observation regarding the trend of AKI-related mortality in AMI patients is that the in-hospital mortality has declined steadily from 19.9% in 2000 to 13.8% in 2008 (P = 0.003) [78].
Preventive Strategies
The medical community in response to the frequent incidence of AKI in AMI patients and the detrimental impact on their prognosis applied numerous efforts in order to tackle this in-hospital complication. The main aim was to prevent the deterioration of kidney function and by those means to improve patients’ prognosis. Many pathophysiological hypotheses have been raised and numerous clinical studies have been conducted in order to apply measures against these hypotheses, but they usually failed to state efficacy. Therefore, despite the multitudinous preventive strategies that have been examined during the last two decades, only a few of them have been embraced by the practicing physicians. The current guidelines issued by the European Society of Cardiology, KDIGO, and other societies contain the following recommendations for prevention of contrast-induced nephropathy (Table 3) [9, 83,84,85,86,87,88,89].
All societies agree that renal replacement therapy (RRT) should be reserved for patients when life-threatening changes in fluid, electrolyte, and acid-base balance exist [hyperkalemia, metabolic acidosis, symptoms or complications of uremia (for example, pericarditis or encephalopathy), fluid overload/pulmonary edema not responding to standard medical treatment]. The main guidance is to consider the broader clinical context, the presence of conditions that can be modified with RRT, and trends of laboratory tests—rather than single urea and creatinine thresholds alone—when making the decision to start RRT.
According to all guidelines, the cornerstone for AKI prevention is optimal hydration. It has been suggested that optimal hydration achieves adequate intravascular volume and therefore adequate renal blood flow. Furthermore, the dilution of the nephrotoxic contrast agents and of the free radicals produced by the cellular necrosis attenuates their effect on kidney function [90]. Maioli et al. in a seminal paper showed that early hydration (before the procedure) of patients undergoing primary PCI reduced the incidence of AKI in comparison to patients with no or late hydration, albeit no effect on mortality or incidence of major clinical complications [90]. These results were corroborated by Jurado-Román et al., in a following study [91]. In the MYTHOS trial, the researchers investigated the effect of furosemide-forced diuresis and intravenous saline infusion matched with urine output on contrast-induced nephropathy (CIN) prevention in patients with chronic kidney disease (CKD) undergoing coronary procedures [92]. The researchers concluded that furosemide-induced high urine output with matched hydration significantly reduces the risk of CIN [relative risk (RR) 0.16, 95% CI 0.04–0.58, P = 0.003) and may be associated with improved in-hospital outcome [92]. In a slight different approach but under the same notion in the POSEIDON clinical trial, researchers used the end-diastolic pressure of the left ventricle (LV) as an index for the optimal infusion rate [93]. Results from the aforementioned study showed that guiding hydration by means of LV end-diastolic pressure could prevent CI-AKI (RR 0.41, 95% CI 0.22–0.79, P = 0.005) [93].
The efficacy of sodium bicarbonate in the prevention of AKI in the setting of AMI is not consolidated, since studies investigating its ability to prevent AKI enrolled a limited number of AMI patients. In detail, there are four published meta-analyses that suggest that its utilization may be beneficial; however, they encompass only two to three studies in the setting of AMI [94, 95]. Regarding the use of N-acetylcysteine (NAC), although there was an initial enthusiasm based on favorable initial results [96], following randomized clinical trials failed to replicate its efficacy in preventing AKI. Recently, four different published clinical trials reported that the use of NAC has no significant impact on AKI incidence [97,98,99,100]. In contrast, there are more robust data regarding the use of statins in prevention of AKI. The hypothesis underlying the use of statins in such a clinical setting is that their pleiotropic and anti-inflammatory actions of these drugs are responsible for the protection they provide to kidney function [101]. Three meta-analyses have been published recently which assessed the use of statins regarding their AKI prevention efficacy in the setting of AMI [102,103,104]. All three meta-analyses reported an AKI cumulative relative risk reduction between 50 and 60% with pretreatment with statins (OR 0.37, 95% CI 0.26–0.53 [102]; OR 0.39, 95% CI 0.25–0.61 [103]; and OR 0.48, 95% CI 0.35–0.66 [104]).
All societies agree that the volume and the composition of the contrast agent used during coronary angiography/intervention are very important regarding the incidence of kidney injury. Although initially it was the absolute amount of these agents which was thought to be responsible for inflicting kidney injury, later published evidence suggested that more significant was the ratio of absolute volume used to estimated GFR [105,106,107,108]. Multiple moderate-sized studies have initially supported the use of a threshold of a 5× body weight/serum creatinine as the safe upper limit for contrast, which is known as the maximal acceptable contrast dose (MACD) [109, 110]. However, contrast-induced injury has been anecdotally demonstrated at lower doses of contrast, and the need for better dosing strategy has been recognized for a long time. Therefore, the application of the ratio of the contrast volume used to estimate GFR was deemed more precise and practical. Three different approaches have been published regarding the cut-off of this ratio. Initially, it was recommended not to be bigger than 3.7 [105], a slightly different proposal defined the threshold at 3.6 [106], whereas other researchers proposed the ratio not to transcend above 2 [107]. In a similar way, recently it was suggested that the ratio of volume of contrast agent used to calculated creatinine clearance could yield accurate prediction for possible AKI and the threshold of this ratio should not exceed 3 [108]. This study showed that the association between the risk of AKI and the volume to GFR ratio is continuous and unfortunately AKI incidence is probable even in cut-offs < 2 especially in high-risk sub-populations [108]. Therefore, the authors recommended the use of as low as possible of contrast volume during PCI [108]. However, as AKI is a multifactorial complication, a preventive strategy should not focus on a single dimension such as the contrast volume used. Different predisposing aspects of this complex complication should be dealt with in a multi-dimensional strategy for these measures to be effective.
Additionally, the composition of the contrast agent is of major importance as far as it concerns its possible effect on kidney function. It has been shown that the use of high-osmolar agents has detrimental effects on kidney function and therefore they are not recommended. Furthermore, iso- and low-osmolar agents have been shown to be safer regarding AKI and also the comparison between iso-osmolar and low-osmolar agents failed to favor any of the two [111, 112]. Based upon these published data, latest guidelines recommend the use of either iso- or low-osmolar contrast agents.
During recent years, there was a significant shift in the practice of coronary angiography and or interventions, as nowadays the majority of interventional cardiologists prefer the radial access which proved to reduce mortality and periprocedural complications especially in the setting of an ACS [113]. A hypothesis has been raised according which the observed less bleeding events associated with radial access could have an impact on preserving kidney function as it well known that anemia may predispose to AKI [114]. This hypothesis has been corroborated in two meta-analyses that showed a cumulative relative risk reduction of 50–60% for AKI with the use of radial access in the clinical setting of AMI (OR 0.42, 95% CI 0.24–0.72 [115] and OR 0.49, 95% CI 0.32–0.75 [116]). Occurrence of bleeding complications after PCI has been associated with post-PCI AKI [117]. As transradial approach is associated with less bleeding complications compared to transfemoral approach, probably the reduction in bleeding rates is the link between radial access and its renal protective effects [117]. The speculated causative effect of bleeding may be related to the occurrence of AKI via the associated hypotension and subsequent renal hypoperfusion observed with larger bleeds [117]. Beyond hemorrhagic complications, microembolization has been observed in patients undergoing PCI and its role has been implicated in post-PCI AKI. PCI performed using transfemoral approach involves the transit of wires and catheters through a significantly long segment of the aorta, increasing the probability of atheroembolic renal injury leading to AKI. The reno-protective effect of radial access might be related to fewer atheroemboli in view of the lack of need to navigate through descending thoracic and abdominal aorta [117].
An interesting debate regarding AKI incidence in the clinical setting of AMI is whether the timing of coronary reperfusion could have an impact. It is logical to hypothesize that in patients with risk factors for AKI, a prudent approach would be to delay coronary reperfusion and the associated use of “nephrotoxic” contrast agents. However, data from published studies are contradictory. In one study, which enrolled ST elevation myocardial infarction patients, the incidence of AKI was increased in parallel with the delay of revascularization [118]. In another study enrolling non-ST elevation myocardial infarction patients, time to reperfusion had no prognostic value [28]. This data probably underline the hypothesis that AKI incidence in AMI patients is not only dependant on the known nephrotoxic effects of contrast agents but also on other factors such as hemodynamic stability, adequate kidney perfusion, baseline kidney function, hemoglobin levels, atherosclerosis of other vascular beds, and others. Timely coronary reperfusion may have a beneficial effect on most of these aforementioned factors.
Another novel approach regarding prevention of AKI in AMI patients was the application of remote ischemic conditioning [119]. Remote ischemic conditioning, including remote ischemic pre-conditioning and remote ischemic post-conditioning, is a method that applies brief non-lethal episodes of ischemia and reperfusion to an organ or tissue (heart/vasculature) that is remote from the target organ or tissue (kidney) [119]. The associated nephroprotective actions of this novel method were attributed to the increased nitric oxide (NO) production and the reduction of free oxygen radicals [119]. One recent meta-analysis showed the effectiveness of these methods to prevent AKI in patients undergoing elective coronary angiography but failed to demonstrate similar results in ACS patients, possibly due to the limited number of incorporated studies and the small study populations enrolled [120].
Withholding metformin has been suggested by some guidelines as a means to prevent the development of AKI. However, randomized clinical data do not show that chronic metformin treatment prior to primary PCI had a significant impact on CI-AKI [121, 122]. Finally, published data regarding the use of natriuretic peptides [123] and magnesium [124] as preventive measures for AKI were promising; however, the under-investigation study populations were rather small to draw definitive conclusions. Larger clinical studies are required in order to extrapolate these results to all AMI patients.
A very recent survey from the Society of Cardiovascular Angiography and Interventions (SCAI) investigated the contemporary practice patterns related to the risk of AKI in the catheterization laboratory. The majority of cardiologists participating in this survey reported practice patterns consistent with guideline and evidence-based recommendations. However, over 40% of responses to questions were inconsistent with these recommendations, suggesting continued opportunities for education and quality improvement concerning AKI prevention [125].
Discussion
AKI is a common complication in the setting of AMI, with detrimental effects on patients’ prognosis, not only during hospitalization but also for the long-term. According to our point of view, the rather disproportionate reference of AKI in current AMI guidelines may contribute to inadequate vigilance, under-diagnosis, and ineffective management. Additionally, under the same notion, many physicians might underestimate creatinine changes during hospitalization and falsely attribute them to laboratory measurement variability.
Physicians should not approach in-hospital changes in creatinine values as a product of laboratory or biologic variation or transient, not being associated with prognosis but rather as an adverse event which requires a more active and pre-emptive course of actions. Modern laboratory measurements minimize the effects of analytic variations, and furthermore, several studies suggest that a creatinine increase even below the threshold for AKI definition (0.3 mg/dL) may be associated with augmented mortality.
A common limitation of the majority of studies that assess the incidence and impact of AKI in the AMI patient population is to exclude patients with end-stage renal disease, patients who are very old-aged, and finally patients with cardiogenic shock. The aforementioned selection bias renders study populations to include more “healthy” AMI patients and therefore probably lead to an underestimation of the true AKI incidence and impact on prognosis. Moreover, this limitation hinders the assessment of proposed preventive strategies on patients who are more vulnerable that is patients with a history of chronic kidney disease, the very elderly, and those patients with hemodynamic instability.
An unresolved issue is the association between AKI and mortality. The remaining question is whether AKI could lead to mortality per se via distinct pathophysiologic pathways or mortality just a result of frailty? It is known that ischemic injury deteriorates kidney function progressively in time and also predisposes to hypertension [126, 127]. Additionally, kidney dysfunction is characterized by an inflammatory, pro-oxidative, and pro-thrombotic state [65]. In summary, AKI is associated with a high mortality that may be due to traditional and non-traditional complications. Traditional complications include well-recognized renal adverse events such as hyperkalemia, acidosis, and volume overload that could lead to increased mortality and morbidity through arrhythmogenicity and decompensation of heart failure. Non-traditional complications include an augmented inflammatory, oxidative, and apoptotic environment that could lead to a propensity for either thrombosis or bleeding. Platelet defects range from diminished responsiveness to platelet agonists like ADP, abnormal platelet adherence to foreign surfaces, reduced platelet pro-coagulant activity, decreased thromboxane and cyclic AMP (cAMP) production, decreased platelet membrane glycoprotein Ib (GPIb) expression, or in the other hand increased platelet turnover and overexpression of the thrombin receptor protease-activated receptor-1 (PAR-1) [128]. Moreover, in patients with compromised renal function, there is evidence of endothelial dysfunction characterized by an abnormal prostacyclin and thromboxane production and more importantly by an increased production and abnormal activity of von Willebrand factor [128]. Therefore, the possible association between AKI and increased mortality in patients with kidney failure may lie under two opposite hemostatic complications: a bleeding diathesis and a thrombotic predisposition [128]. Finally, the presence of reduced glomerular filtration rate could prohibit the use of treatment modalities that could otherwise be beneficial such as medication that have an effect on renin-angiotensin-aldosterone axis. More extensive research is required in this direction, in order to better understand the pathophysiologic consequences of AKI and their association with mortality.
Although there is a bulk of published evidence suggesting the importance of AKI, we must underscore that a great number of studies, especially in the setting of contrast-induced nephropathy, question not only the impact of AKI on prognosis but also whether AKI is a true “disease” state [129]. An argument against this hypothesis is that the pathophysiology of kidney injury after a myocardial infarction is far more complex than CI-AKI, and according to our point of view, it would not be appropriate to confound these two distinctly different kidney injuries, although some times the latter may add up to the former as in the setting of invasive management of myocardial infarction patients.
Under the same notion, regarding prediction of AKI the bulk of published evidence derive from studies investigating the predictive ability of risk scores for CI-AKI in mixed populations including stable and unstable (acute coronary syndromes) coronary artery disease patients after PCI in a variety of clinical settings [elective, emergent (< 24 h) or urgent (≥ 24 h) basis]. On the other hand, there is scarcity of available data regarding predictive risk scores for AKI in patients after a myocardial infarction irrespective of the use of contrast agents. Zambetti et al. published recently the UT-AKI index, a risk score incorporating variables such as the use of intra-aortic balloon pump, hypotension, ejection fraction, age, chronic kidney disease, left ventricular end-diastolic pressure, and estimated GFR with modest predictive ability [area under the curve (AUC) 0.760] [130]. Kul et al. published the predictive ability of Zwolle risk score (Killip class, TIMI flow, age, three-vessel disease, anterior myocardial infarction, and ischemic time) in AMI patients with good predictive ability (AUC 0.850) [38]. Liu et al. assessed the prognostics characteristics of the GRACE risk score for CI-AKI (age, Killip class, systolic blood pressure, heart rate, creatinine levels, myocardial necrosis enzyme levels, and presence of ST deviation on ECG) yielding moderate results also (AUC 0.668 to 0.788) [45]. Although Mehran’s risk score had not been derived and validated solely in AMI patients population, its application in patients presenting with AMI is characterized with a moderate predictive value (AUC 0.790 [130]; AUC 0.780 [131]). Very recently, a new risk score was developed for prediction of AKI in AMI patients incorporating variables such as cardiac arrest, decompensated heart failure on presentation, diabetes mellitus, hypertension, anemia, impaired renal function, and tachycardia on presentation with repeatedly moderate prognostic ability (AUC 0.760) [132]. Taken altogether, the practical utility of the above risk scores in prediction of AKI among AMI patients is limited since the clinical application of these tools is characterized with moderate sensitivity and specificity (approximately 70–80% for both) rendering false-negative and false-positive prediction rates high.
Finally, it has been shown that AKI incidence has declined considerably during the last decade [78]. Of note, this declined occurred in the absence of a great array of preventive measures or of a significant shift in practice. So far, only volume loading for the prevention of contrast-induced AKI and avoidance of drugs that might contribute to AKI have proven to be of value, whereas results for other strategies are inconclusive (sodium bicarbonate, N-acetylcystein, ascorbic acid, theofyllin, statins and others) or indicate potential harm [132,134,134]. The majority of published data assessing the effects of preventive measures showed weak data regarding their ability to lower AKI incidence risk [135, 136]. Moreover, data regarding the ability of these preventive measures to lower cardiovascular mortality are either scarce are of low quality [135, 136]. Although occurrence of AKI is associated with increased mortality and morbidity, the association between lowering AKI incidence by preventive measures and the improvement on long-term cardiovascular prognosis is further complicated by the fact that the long-term prognosis after AKI varies depending on cause and clinical setting, but it may also, mostly, be explained by underlying post-AKI renal function and existing co-morbidities rather than the AKI episode itself [137]. With regards to the long-term effects, the consideration that outcome is a simple binary endpoint of dialysis or not, or survival or not, is overly simplistic, with the reality being much more complex [138]. All of the above underscore the need for larger and longer term studies focusing not just on short-term AKI but also long-term adverse cardiovascular events. To make matters worse, the cornerstone of the proposed preventive strategies, hydration, is under question, as a recent study failed to prove its usefulness in patients referred for an elective procedure requiring the administration of intravascular iodinated contrast material [139]. Moreover, the rate of hydration used is also debatable in the clinical setting of an AMI complicated with AKI as acute reductions in the systolic performance of the left ventricle in the presence of oliguria may lead to volume overload and congestion [135].
Are the preventive measures that already have been used so efficient or is something there concerning kidney protection eluding from us? Are differences in AKI definitions and in AKI reporting obscuring the picture or the large variation in AKI incidence among different hospitals and departments conceals truly preventive practices? Further studies are also needed in this direction.
An interesting clinical scenario has been identified in the clinical setting of an acute ST elevation MI. As according to current guidelines, the majority of these patients should be addressed invasively as soon as possible to first medical contact, the question prevailing is which reno-protective measures should be applied even before kidney function is known? The answer is far more straightforward; however, use of the lowest possible volume of low- or iso-osmolar contrast agent, adoption of staged procedures in patients with high complex coronary artery disease anatomy, avoidance of nephrotoxic drugs, and maintenance of adequate kidney perfusion are logical preventive measures to follow. Furthermore, prophylactic use of intravenous volume expansion with isotonic saline or sodium bicarbonate prior to the procedure and continuing for 6 h post-procedure is an additional alternative although systolic performance of the left ventricle should be taken into account.
Conclusions
AKI is one of the more common complications in the setting of AMI with significant detrimental impact on patients’ prognosis. Despite the limited number of practices and measures to prevent it, there is a steady decline in its incidence during the last years. However, further research is warranted in order to illuminate many “gray” areas regarding AKI pathophysiology, diagnosis, treatment, and prevention in the setting of AMI.
References
Tang Y, Chen J, Huang K, et al. The incidence, risk factors and in-hospital mortality of acute kidney injury in patients after abdominal aortic aneurysm repair surgery. BMC Nephrol. 2017;18:184.
James MT, Samuel SM, Manning MA, et al. Contrast-induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv. 2013;6:37–43.
Pickering JW, James MT, Palmer SC. Acute kidney injury and prognosis after cardiopulmonary bypass: a meta-analysis of cohort studies. Am J Kidney Dis. 2015;65:283–93.
García-Gigorro R, Dominguez Aguado H, Barea Mendoza JA, Viejo Moreno R, Sánchez Izquierdo JA, Montejo-González JC. Short- and long-term prognosis of critically-ill patients referred to the ICU from the Emergency Department of a tertiary hospital. Med Clin (Barc). 2017;148:197–203.
Ronco C, Lullo LD. Cardiorenal syndrome. Heart Fail Clin. 2014;10:251–80.
Rossaint J, Zarbock A. Acute kidney injury: definition, diagnosis and epidemiology. Minerva Urol Nefrol. 2016;68:49–57.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Lameire N, Kellum JA, Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Kuji S, Kosuge M, Kimura K, et al. Impact of acute kidney injury on in-hospital outcomes of patients with acute myocardial infarction―results from the Japanese Registry of Acute Myocardial Infarction Diagnosed by Universal Definition (J-MINUET) Substudy. Circ J. 2017;81:733–9.
Nakahashi H, Kosuge M, Sakamaki K, et al. Combined impact of chronic kidney disease and contrast-induced nephropathy on long-term outcomes in patients with ST-segment elevation acute myocardial infarction who undergo primary percutaneous coronary intervention. Heart Vessel. 2017;32:22–9.
Tziakas D, Chalikias G, Kareli D, et al. Spot urine albumin to creatinine ratio outperforms novel acute kidney injury biomarkers in patients with acute myocardial infarction. Int J Cardiol. 2015;197:48–55.
Yuan Y, Qiu H, Hu XY, et al. Risk factors of contrast-induced acute kidney injury in patients undergoing emergency percutaneous coronary intervention. Chin Med J. 2017;130:45–50.
Iwakura K, Okamura A, Koyama Y, Fujii K. Early prediction of acute kidney injury after acute myocardial infarction by a clinical score. J Am Coll Cardiol. 2016;67(Suppl):478.
Farhan S, Vogel B, Tentzeris I, et al. Contrast induced acute kidney injury in acute coronary syndrome patients: a single centre experience. Eur Heart J Acute Cardiovasc Care. 2016;5:55–61.
Shacham Y, Gal-Oz A, Ben-Shoshan J, Keren G, Arbel Y. Prognostic implications of acute renal impairment among ST elevation myocardial infarction patients with preserved left ventricular function. Cardiorenal Med. 2016;6:143–9.
Centola M, Lucreziotti S, Salerno-Uriarte D, et al. A comparison between two different definitions of contrast-induced acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Int J Cardiol. 2016;210:4–9.
Velibey Y, Oz A, Tanik O, et al. Platelet-to-lymphocyte ratio predicts contrast-induced acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology. 2017;68:419–27.
Neves D, Belo A, Damásio AF, et al. Acute kidney injury in acute coronary syndromes—an important multifactorial consequence. Rev Port Cardiol. 2016;35:415–21.
Park SD, Moon J, Kwon SW, et al. Prognostic impact of combined contrast-induced acute kidney injury and hypoxic liver injury in patients with ST elevation myocardial infarction undergoing primary percutaneous coronary intervention: results from INTERSTELLAR registry. PLoS One. 2016;11:e0159416.
Moriyama N, Ishihara M, Noguchi T, et al. Early development of acute kidney injury is an independent predictor of in-hospital mortality in patients with acute myocardial infarction. J Cardiol. 2017;69:79–83.
Kuboyama O, Tokunaga T. The prevalence and prognosis of contrast-induced acute kidney injury according to the definition in patients with acute myocardial infarction who underwent primary percutaneous coronary intervention. Clin Trials Regul Sci Cardiol. 2016;13:29–33.
Karamasis G, Al-Janabi F, Mohdnazri S, et al. Incidence and prevention of contrast induced acute kidney injury in ST elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. J Am Coll Cardiol. 2016;68(Suppl):B157.
Matějka J, Varvařovský I, Rozsíval V, et al. Heart failure is the strongest predictor of acute kidney injury in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction. Kardiol Pol. 2016;74:18–24.
Warren J, Mehran R, Baber U, et al. Incidence and impact of acute kidney injury in patients with acute coronary syndromes treated with coronary artery bypass grafting: insights from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) and Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trials. Am Heart J. 2016;171:40–7.
Marenzi G, Cosentino N, Moltrasio M, et al. Acute kidney injury definition and in-hospital mortality in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. J Am Heart Assoc. 2016;5:e003522.
Tung YC, Chang CH, Chen YC, Chu PH. Combined biomarker analysis for risk of acute kidney injury in patients with ST-segment elevation myocardial infarction. PLoS One. 2015;10:e0125282.
Kocas B, Abaci O, Cetinkal G, et al. Contrast-induced acute kidney injury in patients with non-ST-segment elevation myocardial infarction undergoing early versus delayed invasive strategy. Int J Cardiol. 2016;203:638–9.
Crimi G, Leonardi S, Costa F, et al. Incidence, prognostic impact, and optimal definition of contrast-induced acute kidney injury in consecutive patients with stable or unstable coronary artery disease undergoing percutaneous coronary intervention. Insights from the all-comer PRODIGY trial. Catheter Cardiovasc Interv. 2015;86:E19–27.
Vavalle JP, van Diepen S, Clare RM, et al. Renal failure in patients with ST-segment elevation acute myocardial infarction treated with primary percutaneous coronary intervention: predictors, clinical and angiographic features, and outcomes. Am Heart J. 2016;173:57–66.
Turan B, Erkol A, Gül M, Fındıkçıoğlu U, Erden İ. Effect of contrast-induced nephropathy on the long-term outcome of patients with non-ST segment elevation myocardial infarction. Cardiorenal Med. 2015;5:116–24.
Toso A, Servi SD, Leoncini M, et al. Acute kidney injury in elderly patients with non-ST elevation acute coronary syndrome: insights from the Italian elderly: ACS study. Angiology. 2015;66:826–30.
Mody P, Wang T, McNamara R, et al. Association of in hospital acute kidney injury with long term outcomes in survivors of acute myocardial infarction: insight from the NCDR. Circulation. 2015;132:A13975.
Gaskina A, Villevalde S, Kobalava Z, et al. Predictors and outcomes of contrast-induced acute kidney injury in patients with primary percutaneous intervention. J Hypertens. 2015;33(Suppl 1):e17.
Giacoppo D, Madhavan MV, Baber U, et al. Impact of contrast-induced acute kidney injury after percutaneous coronary intervention on short- and long-term outcomes. Circ Cardiovasc Interv. 2015;8:e002475.
Akin F, Celik O, Altun I, et al. Relation of red cell distribution width to contrast-induced acute kidney injury in patients undergoing a primary percutaneous coronary intervention. Coron Artery Dis. 2015 Jun;26(4):289–95.
Watabe H, Sato A, Hoshi T, et al. Association of contrast-induced acute kidney injury with long-term cardiovascular events in acute coronary syndrome patients with chronic kidney disease undergoing emergent percutaneous coronary intervention. Int J Cardiol. 2014;174:57–63.
Kul S, Uyarel H, Kucukdagli OT, et al. Zwolle risk score predicts contrast-induced acute kidney injury in STEMI patients undergoing PCI. Herz. 2015;40:109–15.
Shacham Y, Gal-Oz A, Leshem-Rubinow E, et al. Association of admission hemoglobin levels and acute kidney injury among myocardial infarction patients treated with primary percutaneous intervention. Can J Cardiol. 2015;31:50–5.
Narula A, Mehran R, Weisz G, et al. Contrast-induced acute kidney injury after primary percutaneous coronary intervention: results from the HORIZONS-AMI substudy. Eur Heart J. 2014;35:1533–40.
Kim JH, Lee JH, Jang SY, et al. Prognostic value of early acute kidney injury after primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2014;114:1174–8.
Menzorov MV, Shutov AM, Serov VA, Mikhaĭlova EV. Acute kidney injury in patients with myocardial infarction and efficacy of thrombolytic therapy. Kardiologiia. 2012;52:8–12.
Liao Y, Dong X, Chen K, Fang Y, Li W, Huang G. Renal function, acute kidney injury and hospital mortality in patients with acute myocardial infarction. J Int Med Res. 2014;42:1168–77.
Liu KL, Lee KT, Chang CH, Chen YC, Lin SM, Chu PH. Elevated plasma thrombomodulin and angiopoietin-2 predict the development of acute kidney injury in patients with acute myocardial infarction. Crit Care. 2014;18:R100.
Liu YH, Liu Y, Tan N, et al. Predictive value of GRACE risk scores for contrast-induced acute kidney injury in patients with ST-segment elevation myocardial infarction before undergoing primary percutaneous coronary intervention. Int Urol Nephrol. 2014;46:417–26.
Moriyama N, Ishihara M, Noguchi T, et al. Admission hyperglycemia is an independent predictor of acute kidney injury in patients with acute myocardial infarction. Circ J. 2014;78:1475–80.
Mizuno A, Ohde S, Nishizaki Y, Komatsu Y, Niwa K. Additional value of the red blood cell distribution width to the Mehran risk score for predicting contrast-induced acute kidney injury in patients with ST-elevation acute myocardial infarction. J Cardiol. 2015;66:41–5.
Hsieh MJ, Chen YC, Chen CC, Wang CL, Wu LS, Wang CC. Renal dysfunction on admission, worsening renal function, and severity of acute kidney injury predict 2-year mortality in patients with acute myocardial infarction. Circ J. 2013;77:217–23.
dos Santos LN, Conejo F, Filho FHF, et al. Impact of acute renal failure on in-hospital outcomes following percutaneous treatment of acute myocardial infarction. Rev Bras Cardiol Invasiva. 2013;21:344–50.
Choi JS, Kim YA, Kim MJ, et al. Relation between transient or persistent acute kidney injury and long-term mortality in patients with myocardial infarction. Am J Cardiol. 2013;112:41–5.
Marenzi G, Cabiati A, Bertoli SV, et al. Incidence and relevance of acute kidney injury in patients hospitalized with acute coronary syndromes. Am J Cardiol. 2013;111:816–22.
Kume K, Yasuoka Y, Adachi H, et al. Impact of contrast-induced acute kidney injury on outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Cardiovasc Revasc Med. 2013;14:253–7.
Rodrigues FB, Bruetto RG, Torres US, Otaviano AP, Zanetta DMT, Burdmann EA. Incidence and mortality of acute kidney injury after myocardial infarction: a comparison between KDIGO and RIFLE criteria. PLoS One. 2013;8:e69998.
Andò G, Morabito G, de Gregorio C, Trio O, Saporito F, Oreto G. Age, glomerular filtration rate, ejection fraction, and the AGEF score predict contrast-induced nephropathy in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Catheter Cardiovasc Interv. 2013;82:878–85.
Pyxaras SA, Sinagra G, Mangiacapra F, et al. Contrast-induced nephropathy in patients undergoing primary percutaneous coronary intervention without acute left ventricular ejection fraction impairment. Am J Cardiol. 2013;111:684–8.
Lazaros G, Tsiachris D, Tousoulis D, et al. In-hospital worsening renal function is an independent predictor of one-year mortality in patients with acute myocardial infarction. Int J Cardiol. 2012;155:97–101.
Lazzeri C, Valente S, Chiostri M, Picariello C, Attanà P, Gensini GF. ST-elevation myocardial infarction with preserved ejection fraction: the impact of worsening renal failure. Int J Cardiol. 2012;155:170–2.
Queiroz REB, de Oliveira LSN, de Albuquerque CA, et al. Acute kidney injury risk in patients with ST-segment elevation myocardial infarction at presentation to the ED. Am J Emerg Med. 2012;30:1921–7.
Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Wiviott SD. Short-term outcomes of acute myocardial infarction in patients with acute kidney injury: a report from the National Cardiovascular Data Registry. Circulation. 2012;125:497–504.
Bruetto RG, Rodrigues FB, Torres US, Otaviano AP, Zanetta DMT, Burdmann EA. Renal function at hospital admission and mortality due to acute kidney injury after myocardial infarction. PLoS One. 2012;7:e35496.
Hwang SH, Jeong MH, Ahmed K, et al. Different clinical outcomes of acute kidney injury according to acute kidney injury network criteria in patients between ST elevation and non-ST elevation myocardial infarction. Int J Cardiol. 2011;150:99–101.
Lim DH, Jeong JH, Jeong JM, et al. One-year mortality of acute kidney injury in patients with acute myocardial infarction. Korean J Nephrol. 2011;30:141–7.
Wi J, Ko YG, Kim JS, et al. Impact of contrast-induced acute kidney injury with transient or persistent renal dysfunction on long-term outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart. 2011;97:1753–7.
Kim MJ, Choi HS, Oh SH, et al. Impact of acute kidney injury on clinical outcomes after ST elevation acute myocardial infarction. Yonsei Med J. 2011;52:603–9.
Amin AP, Spertus JA, Reid KJ, et al. The prognostic importance of worsening renal function during an acute myocardial infarction on long-term mortality. Am Heart J. 2010;160:1065–71.
Senoo T, Motohiro M, Kamihata H, et al. Contrast-induced nephropathy in patients undergoing emergency percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol. 2010;105:624–8.
Anzai A, Anzai T, Naito K, et al. Prognostic significance of acute kidney injury after reperfused ST-elevation myocardial infarction: synergistic acceleration of renal dysfunction and left ventricular remodeling. J Card Fail. 2010;16:381–9.
Goldberg, Kogan E, Hammerman H, Markiewicz W, Aronson D. The impact of transient and persistent acute kidney injury on long-term outcomes after acute myocardial infarction. Kidney Int. 2009;76:900–6.
Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008;168:987–95.
Passos RL, Siqueira DAA, Silva JFA, et al. Acute renal failure after primary percutaneous coronary intervention in acute myocardial infarction: predictors and long-term clinical evolution. Rev Bras Cardiol Invasiva. 2008;16:422–8.
Bouzas-Mosquera A, Vázquez-Rodríguez JM, Calviño-Santos R, et al. Contrast-induced nephropathy and acute renal failure following emergent cardiac catheterization: incidence, risk factors and prognosis. Rev Esp Cardiol. 2007;60:1026–34.
Latchamsetty R, Fang J, Kline-Rogers E, et al. Prognostic value of transient and sustained increase in in-hospital creatinine on outcomes of patients admitted with acute coronary syndrome. Am J Cardiol. 2007;99:939–42.
Buargub M, Elmokhtar ZO. Incidence and mortality of acute kidney injury in patients with acute coronary syndrome: a retrospective study from a single coronary care unit. Saudi J Kidney Dis Transpl. 2016;27:752–7.
Hsiao PG, Hsieh CA, Yeh CF, et al. Early prediction of acute kidney injury in patients with acute myocardial injury. J Crit Care. 2012;27:525.e1-7.
Marenzi G, Assanelli E, Campodonico J, et al. Acute kidney injury in ST-segment elevation acute myocardial infarction complicated by cardiogenic shock at admission. Crit Care Med. 2010;38:438–44.
Shacham Y, Leshem-Rubinow E, Ziv-Baran T, et al. Incidence and mortality of acute kidney injury in acute myocardial infarction patients: a comparison between AKIN and RIFLE criteria. Int Urol Nephrol. 2014;46:2371–7.
Pickering JW, Blunt IR, Than MP. Acute Kidney Injury and mortality prognosis in Acute Coronary Syndrome patients: A meta-analysis. Nephrology (Carlton) 2016. Epub ahead of print.
Amin AP, Salisbury AC, McCullough PA, et al. Trends in the incidence of acute kidney injury in patients hospitalized with acute myocardial infarction. Arch Intern Med. 2012;172:246–53.
Steinvil A, Garcia HG, Rogers T, et al. Acute kidney injury following primary percutaneous coronary interventions for ST-segment elevation myocardial infarction: trends in the past fifteen years. J Am Coll Cardiol. 2016;67:79.
Nie S, Tang L, Zhang W, Feng Z, Chen X. Are there modifiable risk factors to improve AKI? Biomed Res Int. 2017;2017:5605634.
Andreucci M, Faga T, Serra R, De Sarro G, Michael A. Update on the renal toxicity of iodinated contrast drugs used in clinical medicine. Drug Healthc Patient Saf. 2017;9:25–37.
Shacham Y, Steinvil A, Arbel Y. Acute kidney injury among ST elevation myocardial infarction patients treated by primary percutaneous coronary intervention: a multifactorial entity. J Nephrol. 2016;29:169–74.
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37:2999–3058.
Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267–315.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2017. 8pp. Epub ahead of print.
Schweiger MJ, Chambers CE, Davidson CJ, et al. Prevention of contrast induced nephropathy recommendations for the high risk patient undergoing cardiovascular procedures. Catheter Cardiovasc Interv. 2007;69:135–40.
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–619.
Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2012;79:453–95.
Thomas M, Davies A, Dawnay A, et al. National Institute of Clinical Excellence (NICE) Acute kidney injury: prevention, detection and management clinical guideline. August 2013 nice.org.uk/guidance/cg169.
Maioli M, Toso A, Leoncini M, Micheletti C, Bellandi F. Effects of hydration in contrast-induced acute kidney injury after primary angioplasty a randomized. Controlled Trial Circ Cardiovasc Interv. 2011;4:456–62.
Jurado-Román A, Hernández-Hernández F, García-Tejada J, et al. Role of hydration in contrast-induced nephropathy in patients who underwent primary percutaneous coronary intervention. Am J Cardiol. 2015;115:1174–8.
Marenzi G, Ferrari C, Marana I, et al. Prevention of contrast nephropathy by furosemide with matched hydration: the MYTHOS (Induced Diuresis With Matched Hydration Compared to Standard Hydration for Contrast Induced Nephropathy Prevention) trial. JACC Cardiovasc Interv. 2012;5:90–7.
Brar SS, Aharonian V, Mansukhani P, et al. Haemodynamic-guided fluid administration for the prevention of contrast-induced acute kidney injury: the POSEIDON randomised controlled trial. Lancet. 2014;383:1814–23.
Meier P, Ko DT, Tamura A, Tamhane U, Gurm HS. Sodium bicarbonate-based hydration prevents contrast-induced nephropathy: a meta-analysis. BMC Med. 2009;7:23.
Hoste EAJ, De Waele JJ, Gevaert SA, Uchino S, Kellum JA. Sodium bicarbonate for prevention of contrast-induced acute kidney injury: a systematic review and meta-analysis. Nephrol Dial Transpl. 2010;25:747–58.
Marenzi G, Assanelli E, Marana I, et al. N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006;354:2773–82.
Aslanger E, Uslu B, Akdeniz C, Polat N, Cizgici Y, Oflaz H. Intrarenal application of N-acetylcysteine for the prevention of contrast medium-induced nephropathy in primary angioplasty. Coron Artery Dis. 2012;23:265–70.
Tanaka A, Suzuki Y, Suzuki N, et al. Does N-acetylcysteine reduce the incidence of contrast-induced nephropathy and clinical events in patients undergoing primary angioplasty for acute myocardial infarction? Intern Med Tokyo Jpn. 2011;50:673–7.
Thiele H, Hildebrand L, Schirdewahn C, et al. Impact of high-dose N-acetylcysteine versus placebo on contrast-induced nephropathy and myocardial reperfusion injury in unselected patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: the LIPSIA-N-ACC (Prospective, Single-Blind, Placebo-Controlled, Randomized Leipzig Immediate Percutaneous Coronary Intervention Acute Myocardial Infarction N-ACC) Trial. J Am Coll Cardiol. 2010;55:2201–9.
Jaffery Z, Verma A, White CJ, et al. A randomized trial of intravenous n-acetylcysteine to prevent contrast induced nephropathy in acute coronary syndromes. Catheter Cardiovasc Interv. 2012;79:921–6.
Yoshida T, Hayashi M. Pleiotropic effects of statins on acute kidney injury: involvement of Krüppel-like factor 4. Clin Exp Nephrol. 2017;21:175–81.
Lee JM, Park J, Jeon KH, et al. Efficacy of short-term high-dose statin pretreatment in prevention of contrast-induced acute kidney injury: updated study-level meta-analysis of 13 randomized controlled trials. PLoS One. 2014;9:e111397.
Xie H, Ye Y, Shan G, et al. Effect of statins in preventing contrast-induced nephropathy: an updated meta-analysis. Coron Artery Dis. 2014;25:565–74.
Li H, Wang C, Liu C, Li R, Zou M, Cheng G. Efficacy of short-term statin treatment for the prevention of contrast-induced acute kidney injury in patients undergoing coronary angiography/percutaneous coronary intervention: a meta-analysis of 21 randomized controlled trials. Am J Cardiovasc Drugs Drugs Devices Interv. 2016;16:201–19.
Mager A, Vaknin Assa H, Lev EI, Bental T, Assali A, Kornowski R. The ratio of contrast volume to glomerular filtration rate predicts outcomes after percutaneous coronary intervention for ST-segment elevation acute myocardial infarction. Catheter Cardiovasc Interv. 2011;78:198–201.
Andò G, de Gregorio C, Morabito G, Trio O, Saporito F, Oreto G. Renal function-adjusted contrast volume redefines the baseline estimation of contrast-induced acute kidney injury risk in patients undergoing primary percutaneous coronary intervention. Circ Cardiovasc Interv. 2014;7:465–72.
Celik O, Ozturk D, Akin F, et al. Association between contrast media volume-glomerular filtration rate ratio and contrast-induced acute kidney injury after primary percutaneous coronary intervention. Angiology. 2015;66:519–24.
Gurm HS, Dixon SR, Smith DE, et al. Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2011;58:907–14.
Freeman RV, O’Donnell M, Share D, et al. Nephropathy requiring dialysis after percutaneous coronary intervention and the critical role of an adjusted contrast dose. Am J Cardiol. 2002;90:1068–73.
Brown JR, Robb JF, Block CA, et al. Does safe dosing of iodinated contrast prevent contrast-induced acute kidney injury? Circ Cardiovasc Interv. 2010;3:346–50.
Bolognese L, Falsini G, Schwenke C, et al. Impact of iso-osmolar versus low-osmolar contrast agents on contrast-induced nephropathy and tissue reperfusion in unselected patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention (From the Contrast Media and Nephrotoxicity Following Primary Angioplasty for Acute Myocardial Infarction [CONTRAST-AMI] Trial). Am J Cardiol. 2012;109:67–74.
Gül M, Turan B, Uğur M, et al. Nephrotoxicity of iodixanol versus iopamidol in patients with acute coronary syndrome. Turk Kardiyol Dern Ars. 2013;41:21–7.
Andò G, Capodanno D. Radial versus femoral access in invasively managed patients with acute coronary syndrome: a systematic review and meta-analysis. Ann Intern Med. 2015;163:932–40.
Ohno Y, Maekawa Y, Miyata H, et al. Impact of periprocedural bleeding on incidence of contrast-induced acute kidney injury in patients treated with percutaneous coronary intervention. J Am Coll Cardiol. 2013;62:1260–6.
Andò G, Costa F, Trio O, Oreto G, Valgimigli M. Impact of vascular access on acute kidney injury after percutaneous coronary intervention. Cardiovasc Revasc Med. 2016;17:333–8.
Trio O, Vizzari G, Piccione MC. Is STEMI presentation the link between vascular access and acute kidney injury after percutaneous coronary intervention? Int J Cardiol. 2016;223:83–5.
Pancholy MS, Skelding K, Scott T, Blankenship J, Pancholy SB. Effect of access site choice on acute kidney injury after percutaneous coronary intervention. Am J Cardiol. 2017;120(12):2141–5.
Shacham Y, Leshem-Rubinow E, Gal-Oz A, Arbel Y, Keren G, Roth A, et al. Relation of time to coronary reperfusion and the development of acute kidney injury after ST-segment elevation myocardial infarction. Am J Cardiol. 2014;114:1131–5.
Lim SY, Hausenloy DJ. Remote ischemic conditioning: from bench to bedside. Front Physiol. 2012;3:27.
Bei W, Duan C, Chen J, et al. Remote ischemic conditioning for preventing contrast-induced acute kidney injury in patients undergoing percutaneous coronary interventions/coronary angiography: a meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol Ther. 2016;21:53–63.
Zeller M, Labalette-Bart M, Juliard J-M, Potier L, Feldman LJ, Steg PG, et al. Metformin and contrast-induced acute kidney injury in diabetic patients treated with primary percutaneous coronary intervention for ST segment elevation myocardial infarction: a multicenter study. Int J Cardiol. 2016;220:137–42.
Posma RA, Lexis CP, Lipsic E, et al. Effect of metformin on renal function after primary percutaneous coronary intervention in patients without diabetes presenting with ST-elevation myocardial infarction: data from the GIPS-III trial. Cardiovasc Drugs Ther. 2015;29:451–9.
Zhang J, Fu X, Jia X, et al. B-type natriuretic peptide for prevention of contrast-induced nephropathy in patients with heart failure undergoing primary percutaneous coronary intervention. Acta Radiol Stockh Swed 1987. 2010;51:641–8.
Firouzi A, Maadani M, Kiani R, et al. Intravenous magnesium sulfate: new method in prevention of contrast-induced nephropathy in primary percutaneous coronary intervention. Int Urol Nephrol. 2015;47:521–5.
Prasad A, Sohn A, Morales J, et al. Contemporary practice patterns related to the risk of acute kidney injury in the catheterization laboratory: results from a survey of Society of Cardiovascular Angiography and Intervention (SCAI) cardiologists. Catheter Cardiovasc Interv. 2017;89:383–92.
Basile DP, Donohoe D, Roethe K, Osborn JL. Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol. 2001;281:F887–99.
Spurgeon-Pechman KR, Donohoe DL, Mattson DL, Lund H, James L, Basile DP. Recovery from acute renal failure predisposes hypertension and secondary renal disease in response to elevated sodium. Am J Physiol Ren Physiol. 2007;293:F269–78.
Best PJ, Lennon R, Ting HH, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002;39:1113–9.
Davenport MS, Khalatbari S, Dillman JR, Cohan RH, Caoili EM, Ellis JH. Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material. Radiology. 2013;267:94–105.
Zambetti BR, Thomas F, Hwang I, et al. A web-based tool to predict acute kidney injury in patients with ST-elevation myocardial infarction: development, internal validation and comparison. PLoS One. 2017;12:e0181658.
Chatterjee S, Kundu A, Mukherjee D, et al. Risk of contrast-induced acute kidney injury in ST-elevation myocardial infarction patients undergoing multi-vessel intervention-meta-analysis of randomized trials and risk prediction modeling study using observational data. Catheter Cardiovasc Interv. 2017;90:205–12.
Abusaada K, Yuan C, Sabzwari R, Butt K, Maqsood A. Development of a novel score to predict the risk of acute kidney injury in patient with acute myocardial infarction. J Nephrol. 2017;30:419–25.
Zhang B, Liang L, Chen W, Liang C, Zhang S. The efficacy of sodium bicarbonate in preventing contrast-induced nephropathy in patients with pre-existing renal insufficiency: a meta-analysis. BMJ Open. 2015;5:e006989.
Dong Y, Zhang B, Liang L, et al. How strong is the evidence for sodium bicarbonate to prevent contrast-induced acute kidney injury after coronary angiography and percutaneous coronary intervention? Medicine (Baltimore). 2016;95:e2715.
Vanmassenhove J, Kielstein J, Jörres A, Biesen WV. Management of patients at risk of acute kidney injury. Lancet. 2017;389:2139–51.
Silver SA, Siew ED. Follow-up care in acute kidney injury: lost in transition. Adv Chronic Kidney Dis. 2017;24:246–52.
Sawhney S, Mitchell M, Marks A, Fluck N, Black C. Long-term prognosis after acute kidney injury (AKI): what is the role of baseline kidney function and recovery? A systematic review BMJ Open. 2015;5:e006497.
Doyle JF, Forni LG. Acute kidney injury: short-term and long-term effects. Crit Care. 2016;20:188.
Nijssen EC, Rennenberg RJ, Nelemans PJ, et al. Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): a prospective, randomised, phase 3, controlled, open-label, non-inferiority trial. Lancet. 2017;389:1312–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Kaltsas, E., Chalikias, G. & Tziakas, D. The Incidence and the Prognostic Impact of Acute Kidney Injury in Acute Myocardial Infarction Patients: Current Preventive Strategies. Cardiovasc Drugs Ther 32, 81–98 (2018). https://doi.org/10.1007/s10557-017-6766-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-017-6766-6