Abstract
Purpose
Dyslipidemia is common in type 2 diabetes (T2D) and contributes to cardiovascular disease (CVD) by exacerbating atherosclerosis and hypercoagulability. Statins can stabilize atherosclerotic plaque and reduce prothrombotic status. In the present study we aimed to evaluate the coagulation activity and the effect of statins on procoagulant state of T2D patients using a novel activated protein C (APC)-dependent thrombin-generation assay.
Methods
Procoagulant status (by HemosIL ThromboPath (ThP) assay) and in vivo platelet activation (by plasma soluble (s)CD40L levels) were analyzed in a retrospective, cross-sectional study of 198 patients with long-standing T2D and 198 controls.
Results
Procoagulant status of T2D patients was enhanced when compared to control subjects (p < 0.0001). Similarly, sCD40L levels were increased in T2D (p < 0.0001). When testing ThP as the dependent variable in a multivariate regression model, sCD40L (p < 0.0001) and statin treatment (p = 0.019) were independent predictors of the procoagulant state of T2D patients. Subgroup analysis showed a significant improvement of coagulability in T2D patients on statins (p = 0.012).
Conclusions
The use of a standardized, easy-to-run, and commercially available APC-dependent thrombin-generation assay detected the presence of a procoagulant status in a large series of patients with long-standing T2D and demonstrated a significant impact of statins in the coagulation status of patients with T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic dyslipidemia describes the alteration in blood lipid profiles that is commonly seen in patients with T2D [1], and that is thought to contribute, along with other consequences of insulin resistance, to the elevated cardiovascular risk in these patients [1]. Both hyperglycemia and dyslipidemia are components of the metabolic syndrome and well established risk factors for cardiovascular disease (CVD) including myocardial infarction (MI), stroke and peripheral vascular diseases (PVD) [2]. CVD is caused by atherosclerosis trough formation of atheromatous plaque, known as atherogenesis. Amongst the several mechanisms leading to atherothrombosis, hypercoagulation plays a main role [3].
An imbalance of coagulation promoting the development of the atherosclerotic process in patients with T2D involves coagulation cascade, endothelial function, platelet and monocyte adhesiveness, macrophage function, and fibrinolysis [4]. An hypercoagulable state, detected by thrombin generation tests, was reported in a study conducted in sixty patients with T2D, explaining, at least partially, the high incidence of vascular events in these patients [5]. Similarly to T2D, dyslipidemia has been associated with altered coagulation leading to an increased risk of hypercoagulability through mechanism linked to insulin resistance [6].
Several studies have demonstrated that 3-Hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins) may prevent thrombogenesis and maintain atherosclerotic plaque stability through their pleiotropic effects [7]. Accordingly, statins have been proposed as treatment of choice to prevent vascular events in patients with T2D [8].
Conventional tests for coagulation as well as single pro- or anti-coagulants are not specific in detecting hypercoagulability [5]. Aim of the present study was to evaluate the performance of a novel activated protein C (APC)-dependent thrombin-generation assay (HemosIL ThromboPath) in an unselected population of patients with T2D representative of a general practice cohort enrolled in the Interinstitutional Multidisciplinary Biobank project of the Scientific Institute for Research, Hospitalization and Health Care (IRCCS) San Raffaele Pisana (SR-BioBIM). The effect of statins on the procoagulant state of T2D patients was also analyzed.
Patients and methods
Subjects
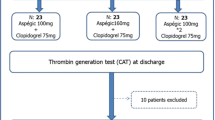
A sample size of one hundred ninety-eight Caucasian patients (89 females and 109 males, aged 70 ± 8 years) with T2D enrolled between June 2010 and May 2011 was retrospectively selected for this study from the SR-BioBIM database [9, 10]. Patients were diagnosed according to the American Diabetes Association (ADA) criteria. T2D was the primary inclusion criteria and was defined as fasting blood glucose ≥126 mg/dL or patient's self-reported history of diabetes or of diabetes medications. All patients with a previous history of CAD were under aspirin treatment at time of study entry. Ninety-three (47 %) patients were treated with superimposable doses of statins (atorvastatin n = 57, 40 mg/daily; simvastatin n = 22, 40 mg/daily; rosuvastatin n = 14, 10 mg/daily) at time of enrollment [11, 12].
Control group included 198 age and sex matched individuals with a prevalence of major atherosclerotic risk factors close to that of patients, but without history or evidence of impaired glucose metabolism or any type of diabetes (89 females and 109 males, aged 68 ± 8 years) whose samples were stored in the facilities of the SR-BioBIM, which enrolls individuals with major cardiovascular risk factors (including T2D) with or without overt vascular disease. Clinical and laboratory features of both study groups are detailed in Table 1.
All study participants underwent a standard clinical examination. Waist circumference (WC) was measured and BMI calculated. Information on risk factors for CVD was obtained by means of interviews, physical examination, laboratory and instrumental (x-ray, cardiac echo ultrasound, and 12-lead ECG) tests in all subjects. Hypertension was defined as a systolic/diastolic blood pressure (BP) ≥140/90 mmHg or anti-hypertensive treatment. Dyslipidemia was defined in accordance with the Third Report of the National Cholesterol Education Program–Adult Treatment Panel (NCEP-ATP) III criteria [13]. Cigarette smoking was dichotomized into ‘ever’ (defined as having smoked >5 cigarettes daily for ≥1 years) versus ‘never’. Diabetic nephropathy was defined by the presence of persistent microalbuminuria (30–300 mg/24 h) in at least 2 of 3 consecutive 24-h urine collections. Retinopathy was assessed by performing fundoscopic examination. Presence of macrovascular complications was substantiated by previous history of cerebrovascular accidents, MI, coronary artery disease (CAD), or PVD. Patients were excluded if they were aged below 18 years, or if they had T1D or confounding conditions such as active cancer, previous episodes of thromboembolism or immunological disease. Patients with renal insufficiency or proteinuria (by serum creatinine levels and urinalysis), altered hepatic function (by liver enzymes), acute or chronic inflammatory diseases, or alcohol abuse were also excluded. The study was performed under the appropriate institutional ethical approvals and in accordance with the principles embodied in the Declaration of Helsinki. Written informed consent was obtained from each participating subject.
Study design and laboratory methods
A cross-sectional comparison of ThromboPath values was performed between subjects with T2D and controls. Plasma sCD40L levels were also evaluated as a marker of platelet activation [14]. The study was specifically designed as a cross-sectional analysis between patients with T2D and control subjects with a prevalence of all other mayor risk factors but without any kind of diabetes (Table 1), in order to minimize possible confounders due to the presence of different risk factors or vascular disease, known to be associated with haemostatic alterations.
Subjects attended the clinic at 8:00 a.m. after an overnight fast. Patients under treatment with statins had taken the last dose the day before the blood analysis. Following a rest period of at least 20 min, blood samples were drawn from each consenting subject, without stasis using a 20 G needle and either non anti-coagulated, for serum recovery, or anti-coagulated in Na citrate 3.8 % (1:9, v:v) or in K2EDTA, for plasma separation. For serum preparation, blood was allowed to clot at room temperature for 2 h and then centrifuged at 2,000 g for 10 min at 4 °C. Citrated plasma was obtained by 10-min centrifugation at 1,500 g, aliquoted, coded and stored at -80 °C for batch analysis of ThromboPath and sCD40L.
Complete and differential blood cell counts were obtained from K2EDTA-treated whole blood using a routine hematology analyzer (Coulter LH 750; Beckman Coulter, Miami, FL). Routine coagulation studies were performed on fresh samples using an ACL-TOP automated coagulometer (Instrumentation Laboratory Co., Lexington, MA, USA). Routine blood chemistry was immediately analyzed on an Architect c8000 (Accelerator Total Lab Automation, Abbott Laboratories, Abbott Park, IL, USA). HbA1C level was measured by automated HPLC (Tosoh Bioscience, Rivoli, TO, Italy).
Plasma sCD40L levels were determined using a commercially available enzyme-immunoassay (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s protocol. Measurements were ascertained while blinded to the sample origin. All samples were assayed in duplicate and those showing values above the standard curve were re-tested with appropriate dilutions.
The HemosIL ThromboPath (ThP) assay (kindly provided by Instrumentation Laboratory Co.) was performed on citrated plasma samples using an ACL-TOP automated coagulometer as previously reported [15]. The assay is based on the ability of endogenous activated protein C (APC), generated after activation of protein C (PC) by a snake venom extract (Protac), to reduce the thrombin generation induced by a reagent containing tissue factor. The amount of thrombin is evaluated by recording changes in optical density (OD) at 405 nm in the presence (OD-A) or absence (OD-B) of Protac after adding a thrombin-specific chromogenic substrate. Test results are expressed as the Protac-Induced Coagulation Inhibition percentage (PICI%) calculated by dividing [OD-B minus OD-A] by OD-B and multiplying by 100. Intra- and inter-assay coefficients of variation determined in our laboratory were 0.6 % and 2.2 %, respectively. Cut-off value for categorization was locally defined on the basis of the mean minus 1 SD of the results obtained in control subjects, as previously suggested [15], and was set at 80 % PICI% (corresponding to the 10th percentile of controls). Samples with PICI% below this cut-off were categorized as pathologic.
Statistical analysis
Sample size of the study was based on the agreement to inclusion criteria and willingness to provide informed consent rather than on sample size calculations. However, estimation was later performed and showed that, given the observed means for patients (μ1) and control (μ2) groups for ThP PICI% values and using a type I error probability of 0.05, a sample size of 198 subjects per group yielded a statistical power greater than 95 %.
Data are expressed as mean ± SD or median and interquartile range (IQR). Student’s unpaired t-test and Pearson Product moment correlation analysis were used for normally distributed continuous variables. Appropriate non-parametric tests (Mann Whitney U test and Spearman Rank correlation test) were employed for all the other variables. Multiple linear regression analysis was performed by forward stepping to characterize the relationship between clinical and biochemical variables. Two-tailed probabilities were used for testing statistical significance and P values <0.05 were regarded as statistically significant. All calculations were made using a computer software package (Statistica 8.0, StatSoft Inc., Tulsa, OK).
Results
Median disease duration was 11 years and all patients with T2D were in good metabolic control, as demonstrated by a mean HbA1c of 7.1 % (54 mmol/mol). Clinical and laboratory features are summarized in Table 1. Patients with T2D significantly differ from controls in terms of BP, HDL or triglyceride levels, and had a larger mean WC (97 ± 16 vs. 83 ± 14, respectively; p = 0.04). On the other hand, control subjects displayed increased LDL levels compared to those with T2D (p < 0.0001), probably due to the lower number of subjects under statins treatment (Table 1). Smoking habit did not significantly differ between patients and controls, but subjects with T2D were characterized by higher rates of clinically diagnosed hypertension, dyslipidemia or macrovascular complications, mainly represented by CAD, leading to a significantly higher proportion of individuals treated with anti-platelet, statins or anti-hypertensive drugs (Table 1). Retinopathy and microalbuminuria were found in 6 % and 29 %, respectively, of 198 patients with T2D compared to none of controls.
Overall, the procoagulant status of patients with T2D, as reflected by ThP PICI% values, was significantly enhanced when compared to control subjects (82 ± 13 vs. 86 ± 6, p < 0.0001) (Table 1). Similarly, platelet activation, as reflected by sCD40L levels normalized by platelet count, was significantly increased in the T2D group when compared to controls [Median (IQR): 0.248 (0.154–0.373) pg/103Plt vs. 0.006 (0.003–0.018) pg/103Plt, respectively; <0.0001] (Table 1). A significant correlation was also observed between platelet activation and the procoagulant state of subjects with T2D (Rs = −0.184; p < 0.05) (Table 2). Furthermore, ThP PICI% values were associated with advanced age, diastolic BP and HbA1c on univariate analysis (Table 2). As expected, ThP PICI% values were reduced in patients treated with oral anticoagulants (owing to inhibition of vitamin K-dependent protein C synthesis) and correlated with INR target (Rs = −0.48), however the number of individual was too low (10 patients with T2D vs. 5 control subjects) to substantiate any statistical analysis. No differences were observed among patients with T2D who were taking antiplatelet drugs compared to those who did not (p = 0.84). Once ThP was tested as the dependent variable in a multivariate regression model, including as predictor variables all those listed in Table 3, platelet activation, age and treatment with statins were all independent predictors of the procoagulant state of subjects with T2D.
Table 4 summarizes the clinical and laboratory features of subjects with T2D treated or not with statins. As shown, the two groups of patients had similar age and gender distribution as well as comparable disease duration. As expected, LDL levels were lower in the group of patients treated with statins. Notably, a tendency toward a condition of hypercoagulability was observed in subjects with T2D not treated with statins, as demonstrated by lower ThP PICI% values compared to patients with T2D treated with different HMG-CoA reductase inhibitors (Anova test: F = 3.5, p = 0.02) (Table 4). ThP PICI% value distribution within the different classes of statins used in the study are reported in Table 4. No significant differences were observed for sCD40L (Table 4) irrespectively of the type of statin.
Discussion
T2D is a well recognized major risk factor for CVD, mainly leading to progression of atherosclerotic lesions through mechanisms involved in atherothrombosis [4]. T2D is a very common disease in the Western World with its prevalence likely to increase dramatically during the next decades, especially in the developing countries. To date, 15 % of the whole population is considered at high risk to develop T2D [16].
T2D is a complex prothrombotic state to which factors such as insulin resistance, dyslipidemia, endothelial dysfunction, systemic inflammation, increased platelet activation, increased thrombin generation, elevated levels of plasma fibrinogen, altered fibrin network structure and hypofibrinolysis may contribute.
In this study, carried on a cohort of patients with long-standing T2D and using a new APC-based thrombin generation assay to evaluate the coagulation activity, we found significant differences in procoagulant status between patients with T2D and greater CVD burden, and a group of control subjects. Although the HemosIL ThP assay was developed and validated for globally screening protein C (PC) pathway abnormalities [15], several reports have recently highlighted its value as a novel “marker” of hypercoagulability, independent of its sensitivity to each individual PC pathway abnormality [17, 18]. In the present study, we did not observe any PC deficiency and only 4.9 % patients were heterozygous or Factor V Leiden, leading to activated PC resistance, which is consistent with the data reported in the literature (data not shown) [19]. Nonetheless, we found abnormal PICI% values in approximately 26 % of patients with T2D compared to 6 % controls (possibly due to activation of coagulation and, in turn, consumption of the counteracting factors of the anticoagulant PC pathway), which allow to hypothesize that the HemosIL ThP assay is capable of identifying a procoagulant status, as already suggested by Toulon et al. [15].
Of interest, in patients with T2D, treatment with a statin drug was associated with a statistically significant decrease in hypercoagulability, as indicated by higher PICI% values. T2D is frequently associated with dyslipidemia, including the presence of a high concentration of small, dense LDL particles, that may accelerate the progression of atherosclerotic disease and the development of CVD [1]. Dyslipidemia, hyperglycemia and hypercoagulability are known to be major modifiable factors in the process of atherogenesis [2], however, the links between insulin resistance, dyslipidemia, and hypercoagulability are complex and to date have been only partially delineated. Nonetheless, it is well accepted that insulin resistance contributes to abnormalities of plasma lipids in patients with T2D [20].
Clinical trials have failed to show that glycemic control per se significantly reduces macrovascular endpoints such as MI [21–24]. On the other hand, statin trials have consistently demonstrated significant reductions in morbidity and mortality from CVD, including in patients with diabetes [25]. Nevertheless, many patients with diabetic dyslipidemia who achieve their LDL goal still carry residual CVD risk, possibly due to both increased concentration of atherogenic apolipoprotein B-containing lipoproteins that can persist despite normalized LDL levels, and low HDL levels [26].
Both T2D and insulin resistance have been shown to be associated with hypercoagulability [5, 6]. Hypercoagulability is characterized by increased levels of procoagulants and/or decreased levels of anti-coagulants. Unfortunately not enough is known regarding the characteristics of hypercoagulability in T2D, and what data is available mainly reports the measurement of single pro- or anti-coagulants levels in this patient population [27, 28]. A recent study demonstrated that plasma from patients with T2D display an imbalance of pro- versus anti-coagulation factors resulting in hypercoagulability detected by thrombin generation tests when compared to healthy subjects [5]. Our data are in agreement with these findings, and confirm the presence of a procoagulant state in a large series of T2D patients using a standardized, easy-to-run, and commercially available thrombin-generation assay. Moreover, differently from the study by Tripodi et al. [5], our study compared T2D patient with a control population not only similar for age, gender, but also including a substantial proportion of individuals with major risk factors or macrovascular complications, albeit in a lower percentage when compared to patients with T2D. The rationale behind our choice was to match the two experimental groups and to eliminate as much as we could potential selection bias not linked to the presence of T2D. Notably, the occurrence of an increased procoagulant state in T2D was confirmed despite the inclusion of individuals with risk factors, or overt CVD in the control group. Of interest, procoagulant status of T2D patients was significantly associated to the occurrence of in vivo platelet activation, a condition that has been already described in T2D (reviewed in [3]), here demonstrated by an increase of sCD40L in patients with T2D. These findings extend previously published observation demonstrating the presence of elevated levels of plasma sCD40L in both type 1 and 2 diabetes [29, 30], which expression might be triggered by advanced glycation end products [31], including HbA1c [32, 33], and could be lowered by thiazolidinediones [34]. Our results are also in agreement with the findings by other authors, who demonstrated that sCD40L levels in patients with T2D were not reduced by either simvastatin [35] or atorvastatin [36, 37], although rosuvastatin was capable to reduce sCD40L levels in a short-term study of hypercholesterolemic patients with T2D [35].
Finally, our findings do demonstrate a significant association between ThP and age and statin treatment. The association of age with increase in hypercoagulability may be well explained by the increasing prevalence of vascular risk factors typical of older individuals [38]. On the contrary, statins reduce hypercoagulability in patients with T2D as demonstrated by an increase in ThP values. The pleiotropic effects of statins have been well established by several experimental studies showing their ability to modulate endothelial function, reduce inflammation, and decrease the risk of thrombosis thus mitigating acute vascular events [7]. Statins have been shown to lead to a significant downregulation of the blood coagulation cascade independently of changes in lipid profile as a result of decreased tissue factor expression, which leads to reduced thrombin generation. Statins may also enhance the activity of the PC anticoagulant pathway [39], which is in agreement with our observation of an enhancement of ThP values in patients with T2D receiving statins. ThP, indeed, is a chromogenic assay designed to globally evaluate the functionality of the PC pathway, with an overall test sensitivity to all PC pathway abnormalities of 95 % and a specificity of approximately 86 % [15]. Thus, statin treatment might improve test results directly through its enhancement of PC activity.
Different structure of statins has been shown to be related with differences in anti-inflammatory and pleiotropic properties that may help to account for variation in clinical efficacy [40]. In our analysis, after stratification for different type of statins, all of them were associated with an improvement of ThP values. However, we have to recognize the limitation of this analysis due to the small number of subjects in each subgroup.
Despite this limitation, our findings fit well into the current view of the antithrombotic effects of statins. The Collaborative Atorvastatin Diabetes Study (CARDS), involving 2,800 patients with T2D, clearly demonstrated that atorvastatin treatment significantly reduced incidence of MI, stroke and surgical procedures when compared to those receiving placebo [25]. Furthermore, a meta-analysis of 18,686 patients with diabetes taking statin therapy in the Cholesterol Treatment Trialists’ collaborators study found that, after a mean follow-up of 4.3 years there was a proportional 9 % decrease in all-cause mortality per mmol/L reduction in LDL, and a proportional 21 % reduction in major vascular events per mmol/L decrease in LDL, for patients on statin therapy. The effects of statin therapy were seen irrespective of baseline CVD risk, suggesting the use of an HMG-CoA reductase inhibitor in most patients with diabetes [41], despite these drugs are often under used [42].
Our findings are also consistent with current treatment recommendations from the NCEP-ATP III, which addresses the management of atherogenic dyslipidemia and recommends weight reduction, increased exercise, and lipid-lowering therapies (i.e., HMG-CoA reductase inhibitors, fibrates, and nicotinic acid) [13]. In terms of atherogenic dyslipidemia and diabetes, specifically those with T2D, both NCEP-ATP III and ADA recommend lifestyle modification and statin therapy regardless of baseline LDL for those with overt CVD and those without CVD who are age >40 years with one or more CVD risk factors [13, 43].
In conclusion, using a novel and well standardized APC-based thrombin generation assay, we showed a reduction in hypercoagulability in patients with long-standing T2D treated with statins. A better understanding the potential role of statins on coagulation may result in new therapeutic approaches, especially in patients with vascular risk factors, such as diabetes. Other studies, especially interventional study such as a randomized placebo-controlled study, are needed to further define the clinical implication of statins in modifying hypercoagulability in high risk patients.
References
Krentz AJ. Lipoprotein abnormalities and their consequences for patients with type 2 diabetes. Diabetes Obes Metab. 2003;5:S19–27.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32.
Ferroni P, Basili S, Falco A, Davi G. Platelet activation in type 2 diabetes mellitus. J Thromb Haemost. 2004;2:1282–91.
Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–81.
Tripodi A, Branchi A, Chantarangkul V, Clerici M, Merati G, Artoni A, et al. Hypercoagulability in patients with type 2 diabetes mellitus detected by a thrombin generation assay. J Thromb Thrombolysis. 2011;31:165–72.
Palomo I, Alarcon M, Moore-Carrasco R, Argiles JM. Hemostasis alterations in metabolic syndrome (review). Int J Mol Med. 2006;18:969–74.
Rubba P. Effects of atorvastatin on the different phases of atherogenesis. Drugs. 2007;67:17–27.
Ludwig S, Shen GX. Statins for diabetic cardiovascular complications. Curr Vasc Pharmacol. 2006;4:245–51.
Guadagni F, Albertini G, Barbanti P, Volterrani M, Palma E, Lancia A, et al. Foundation and Organization of a high-throughput technology-based Multidisciplinary and InterInstitutional Biobank at the IRCCS San Raffaele Pisana. Biopreserv Biobanking. 2010;7:201–2.
Guadagni F, Spila A, Nanni U, Somma P, Perrone V, De Angelis F, et al. Automated processing of biological samples. The experience of the InterInstitutional Multidisciplinary Biobank (BioBIM). Biopreserv Biobanking. 2010;7:230–1.
Wlodarczyk J, Sullivan D, Smith M. Comparison of benefits and risks of rosuvastatin versus atorvastatin from a meta-analysis of head-to-head randomized controlled trials. Am J Cardiol. 2008;102:1654–62.
Nicholls SJ, Brandrup-Wognsen G, Palmer M, Barter PJ. Meta-analysis of comparative efficacy of increasing dose of Atorvastatin versus Rosuvastatin versus Simvastatin on lowering levels of atherogenic lipids (from VOYAGER). Am J Cardiol. 2010;105:69–76.
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–421.
Riondino S, Martini F, La Farina F, Spila A, Guadagni F, Ferroni P. Increased plasma levels of soluble CD40 ligand correlate with platelet activation markers and underline the need for standardized pre-analytical conditions. Clin Biochem. 2010;43:666–70.
Toulon P, Smirnov M, Triscott M, Safa O, Biguzzi E, Bouziane K, et al. A new chromogenic assay (HemosIL ThromboPath) is sensitive to major prothrombotic risk factors affecting the protein C pathway. Results of a multicenter study. Thromb Res. 2009;124:137–43.
Adeghate E, Schattner P, Dunn E. An update on the etiology and epidemiology of diabetes mellitus. Ann NY Acad Sci. 2006;1084:1–29.
Ferroni P, La Farina F, Palmirotta R, Martini F, Raparelli V, Nigro C, et al. Predictive value of thrombopath determination in women with pregnancy complications. Clin Chim Acta. 2010;411:37–42.
Tripodi A, Legnani C, Lemma L, Cosmi B, Palareti G, Chantarangkul V, et al. Abnormal Protac-induced coagulation inhibition chromogenic assay results are associated with an increased risk of recurrent venous thromboembolism. J Thromb Thrombolysis. 2010;30:215–9.
De Stefano V, Finazzi G, Mannucci PM. Inherited thrombophilia: pathogenesis, clinical syndromes, and management. Blood. 1996;87:3531–44.
Krentz A. Type 2 diabetes and atherosclerotic cardiovascular disease: do they share common antecedents? Br J Diabetes Vasc Dis. 2002;2:370–8.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998; 352:837–53.
Gerstein HC, Miller ME, Byington RP, Goff Jr DC, Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Colhoun HM, Thomason MJ, Mackness MI, Maton SM, Betteridge DJ, Durrington PN, et al. Design of the Collaborative AtoRvastatin Diabetes Study (CARDS) in patients with type 2 diabetes. Diabet Med. 2002;19:201–11.
Vasudevan MM, Ballantyne CM. Advances in lipid testing and management in patients with diabetes mellitus. Endocr Pract. 2009;15:641–52.
Ceriello A, Quatraro A, Marchi E, Barbanti M, Dello Russo P, Lefebvre P, et al. The role of hyperglycaemia-induced alterations of antithrombin III and factor X activation in the thrombin hyperactivity of diabetes mellitus. Diabet Med. 1990;7:343–8.
Sauls DL, Banini AE, Boyd LC, Hoffman M. Elevated prothrombin level and shortened clotting times in subjects with type 2 diabetes. J Thromb Haemost. 2007;5:638–9.
Santilli F, Davi G, Consoli A, Cipollone F, Mezzetti A, Falco A, et al. Thromboxane-dependent CD40 ligand release in type 2 diabetes mellitus. J Am Coll Cardiol. 2006;47:391–7.
Lim HS, Blann AD, Lip GY. Soluble CD40 ligand, soluble P-selectin, interleukin-6, and tissue factor in diabetes mellitus: relationships to cardiovascular disease and risk factor intervention. Circulation. 2004;109:2524–8.
Varo N, Libby P, Nuzzo R, Italiano J, Doria A, Schönbeck U. Elevated release of sCD40L from platelets of diabetic patients by thrombin, glucose and advanced glycation end products. Diab Vasc Dis Res. 2005;2:81–7.
Neubauer H, Setiadi P, Günesdogan B, Pinto A, Börgel J, Mügge A. Influence of glycaemic control on platelet bound CD40-CD40L system, P-selectin and soluble CD40 ligand in Type 2 diabetes. Diabet Med. 2010;27:384–90.
Bláha V, Andrýs C, Smahelová A, Knízek J, Hyspler R, Solichová D, et al. Effect of atorvastatin on soluble CD14, CD40 Ligand, sE- and sP-selectins and MCP-1 in patients with type 2 diabetes mellitus: relationship to cholesterol turnover. Pharmacol Res. 2006;54:421–8.
Varo N, Vicent D, Libby P, Nuzzo R, Calle-Pascual AL, Bernal MR, et al. Elevated plasma levels of the atherogenic mediator soluble CD40 ligand in diabetic patients: a novel target of thiazolidinediones. Circulation. 2003;107:2664–9.
Santini E, Madec S, Corretti V, Ferrannini E, Solini A. Effect of statins on soluble CD40 ligand in hypercholesterolemic Type 2 diabetic patients. J Endocrinol Invest. 2008;31:660–5.
Kinlay S, Schwartz GG, Olsson AG, Rifai N, Sasiela WJ, Szarek M, et al. Effect of atorvastatin on risk of recurrent cardiovascular events after an acute coronary syndrome associated with high soluble CD40 ligand in the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) Study. Circulation. 2004;110:386–91.
Jaumdally RJ, Lip GY, Varma C, Blann AD. Impact of high-dose atorvastatin on endothelial, platelet, and angiogenic indices: effect of ethnicity, cardiovascular disease, and diabetes. Angiology. 2011;62:571–8.
Kannel WB. Overview of atherosclerosis. Clin Ther. 1998;20:B2–B17.
Undas A, Brummel-Ziedins KE, Mann KG. Statins and blood coagulation. Arterioscler Thromb Vasc Biol. 2005;25:287–94.
Arnaboldi L, Corsini A. Do structural differences in statins correlate with clinical efficacy? Curr Opin Lipidol. 2010;21:298–304.
Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371:117–25.
Avogaro A, Guida P, Giorda C, Mannucci E, Medea G, Comaschi M, et al. The under-use of statin in type 2 diabetic patients attending diabetic clinics in Italy. Nutr Metab Cardiovasc Dis. 2007;17:32–40.
Kumar A, Singh V. Atherogenic dyslipidemia and diabetes mellitus: what’s new in the management arena? Vasc Health. Risk Manag. 2010;6:665–9.
Acknowledgments
This work was partially supported by the Italian Ministry of Health Grant ACC-WP 3/1b and MERIT RBNE08NKH7. The authors wish to thank Francesco De Angelis and Vincenzino Perrone (InterInstitutional Multidisciplinary BioBank, Department of Laboratory Medicine and Advanced Biotechnologies, IRCCS San Raffaele, Rome, Italy), for their excellent technical assistance.
Declaration of Competing Interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
P. Ferroni, D. Della-Morte for equal contribution
Rights and permissions
About this article
Cite this article
Ferroni, P., Della-Morte, D., Pileggi, A. et al. Impact of Statins on the Coagulation Status of Type 2 Diabetes Patients Evaluated by a Novel Thrombin-Generation Assay. Cardiovasc Drugs Ther 26, 301–309 (2012). https://doi.org/10.1007/s10557-012-6388-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-012-6388-y