Abstract
Cancer metastasis is highly inefficient and complex. Common features of metastatic cancer cells have been observed using cancer cell lines and genetically reconstituted mouse and human tumor xenograft models. These include cancer cell interaction with the tumor microenvironment and the ability of cancer cells to sense extracellular stimuli and adapt to adverse growth conditions. This review summarizes the coordinated response of cancer cells to soluble growth factors, such as RANKL, by a unique feed forward mechanism employing coordinated upregulation of RANKL and c-Met with downregulation of androgen receptor. The RANK-mediated signal network was found to drive epithelial to mesenchymal transition in prostate cancer cells, promote osteomimicry and the ability of prostate cancer cells to assume stem cell and neuroendocrine phenotypes, and confer the ability of prostate cancer cells to home to bone. Prostate cancer cells with activated RANK-mediated signal network were observed to recruit and even transform the non-tumorigenic prostate cancer cells to participate in bone and soft tissue colonization. The coordinated regulation of cancer cell invasion and metastasis by the feed forward mechanism involving RANKL, c-Met, transcription factors, and VEGF-neuropilin could offer new therapeutic opportunities to target prostate cancer bone and soft tissue metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cancer metastasis is a highly inefficient process. Only a few cancer cells can successfully colonize metastatic sites [1–4]. Cancer cells increase the odds of colonizing metastatic sites by preparing themselves for increased local migration and invasion through interaction with their surrounding microenvironments, turning on genes that increase angiogenesis and survivorship for improved distant dissemination, and interacting and cooperating with cells at metastatic sites to augment the success of metastatic spread. A number of the molecular processes closely associated with metastasis have been investigated extensively, including epithelial to mesenchymal transition (EMT), which allows cancer cells to dissociate from each other by downregulating a cell adhesion molecule, E-cadherin, to gain increased migratory and invasive properties by synthesizing, releasing and responding to numerous soluble and insoluble factors in the tumor microenvironment via an enhanced cell signaling network that confers increased cell proliferation, survival and resistance to therapy. Cancer cells also induce angiogenesis by recruiting the host vasculogenic network [5] and enhance growth and survival potentials upon transition from primary to distant sites by genetically and epigenetically modifying their response to environmentally induced stress and metabolic derangements [6], evading host immune surveillance [7], enduring shear forces during their transit from primary or secondary sites of growth through the circulatory system [8], and ultimately arrive at metastatic sites by establishing reciprocal interaction and cooperation with host cells through soluble growth factors, extracellular matrices, and oncosomal communication [9]. This review focuses specifically on lethal bone metastasis, the source of mortality and morbidity in affected patients. We employ prostate cancer (PCa) as a model to illustrate the multiple steps of cancer metastasis and distant colonization. We focus on the receptor activator of NF-κB (RANK)-mediated signaling network because: (a) RANK receptor in PCa cells responds to the action of RANK ligand (RANKL), which drives PCa to undergo EMT and enhances the potential development of bone metastasis [10, 11]. (b) RANKL, one of the osteomimicry associated genes, is expressed in PCa cells and closely associated with PCa patient survival [12, 13]. This association reflects the potential roles of cancer osteomimicry and cancer metastasis. (c) RANKL, a paracrine factor that promotes bone turnover [14] and expands the stem cell compartment in the development of normal mammary gland [15], could be the driver for castration-resistant prostate cancer (CRPC) and the initiation of PCa skeletal metastasis. (d) RANKL expression is elevated in castrated hosts [16] and in experimental mice fed with high cholesterol, suggesting the pathogenesis of PCa metastasis may derive in part from a dysfunctional RANK-mediated signal network in PCa [17]. (e) The RANK-mediated signal network affects both cancer cells and cells in the cancer microenvironment [18]. (f) Targeting RANKL-RANK interaction has profound effects in reducing bone resorption in osteoporosis and reducing pain and skeletal related events in PCa patients [19, 20]. (g) The RANK-mediated signal pathway is closely linked to c-Met and its activation. Through increased expression of a family of transcription factors (TFs) and effector molecules, PCa cells exhibit various phenotypes with an enhanced ability to metastasize [21, 22]. In this review, we will first summarize the importance of signaling amplification as a recurring theme for cancer cells to gain a foothold at metastatic sites. We will then review the highly coordinated cell signal network established by cancer cells and cells in the tumor microenvironment. We will next discuss how cancer cells employ different strategies including amplifying cell signaling networks and recruiting bystander cells to increase their odds of success at metastatic sites. Among the mixed cell populations contributing to cancer metastasis, we discuss the possible contribution of bystander “dormant” cells or bone marrow-derived mesenchymal cells participating in the metastatic cascade. We discuss the potential transdifferentiation or transforming roles by which metastasis-initiating cells impinge on their neighbors so that metastasis can be fully established. Understanding the metastasis cascade can suggest a new therapeutic paradigm with treatment protocols that could help alleviate the pain and suffering of PCa patients who develop CRPC and skeletal lesions.
2 Osteomimicry in the PCa bone metastatic phenotype activates cell signaling networks: the potential role of β-2 microglobulin (β-2m)
Osteomimicry occurs when cancer cells begin to express genes normally restricted to bone cells, such as Runx2, osteocalcin, osteopontin, bone sialoprotein, osteonectin, RANK, RANKL, and parathyroid hormone-related peptide (PTHrP) [23, 24]. Changes in gene expression profiles in PCa toward the bone phenotype were first observed by Knerr et al. in 2004 using large-scale transcripts profiling PCa cells after exposing these cells to factors produced by osteoblasts. In response to osteoblast-derived factors, they validated the expression of cell adhesion and anchoring molecules by PCa that promoted cancer cells to colonize bone [25]. Osteomimicry was also found to be a common feature of human breast and lung cancer cells that could increase cancer cell growth, survival and ability to thrive in bone microenvironments [24, 26]. Soluble factors found to be involved in osteomimicry included BMP-2, RANKL, IGF-1, TGF-β, TNF-α, M-CSF, G-CSF, GM-CSF, 17β-estradiol, and miR218 [27, 28]. These factors likely mediate the osteogenic program in cancer cells through a complex of intracellular cell signal networks involving Twist, Wnt, NF-κB, Svep-1, RANK, and c-Met [21–23, 29, 30]. We found that β-2m, a pleiotropic factor, regulates osteomimicry through binding to a cell-surface receptor, HFE, a hemochromatosis gene known to regulate RANKL [10, 11] and iron flux in cells [31]. β-2m, best known for its function as a co-receptor for histocompatibility complex (MHC) class I antigen, also controls the stability of IgG, albumin in fetal development, and the proliferation, survival, apoptosis and metastasis of cancer cells. β-2m regulates a diverse array of cellular functions, including transcriptional regulation of osteocalcin (OC) and bone sialoprotein (BSP) in human prostate cancer cells [32, 33], promotes cell cycle progression resulting in increased cell growth and survival, drives PCa cells to undergo EMT and increase their migratory, invasive, and metastatic capability through transcriptional upregulation of RANKL expression and increased RANKL-RANK signaling [31], modulates AR-mediated signaling to enhance the development of a castration- and drug-resistance phenotype [32, 34], and increases metabolism by promoting lipogenesis and ROS production [34], known to enhance the degree of malignancy of PCa.
β-2m enhances OC and BSP gene expression by cAMP-dependent PKA activity through a cAMP-responsive element-binding protein, CREB. This activation can induce explosive tumor growth in mouse skeleton via a coordinated increase of pCREB and its activated target genes including OC, BSP, cyclin A, cyclin D1, and VEGF [32–34]. β-2m stimulates cell growth and enhances cancer cell ability to invade and migrate through EMT, and eventually supporting the lethal progression of cancer to bone and soft tissues in mice. PCa cells expressing β-2m show increased bone turnover, and generated mixed osteolytic and osteoblastic responses in mouse skeleton [31]. β-2m activated not only β-2m/PKA/CREB signaling but also activated its convergent cell survival signaling network, phosphatidylinositol 3-kinase (PI3K)/Akt/extracellular signal-regulated kinase (ERK). Furthermore, recombinant β-2m protein could phosphorylate the Bcl-xL/Bcl-2-associated death-promoting protein, Bad, via activated PI3K/Akt/ERK signaling pathways in human SN12C kidney cancer cells [35–37]. Human PCa, breast, lung and kidney cancer cells stably transfected with β-2m had consistently activated STAT3, Snail, LIV-1, and RANKL protein, showed EMT induction and promoted bone metastasis upon intracardiac administration [10, 31, 38]. These results collectively support the concept that EMT occurs subsequent to β-2m expression and that this phenotype is stable in vivo and can be induced by enhanced RANKL-RANK signaling which drives bone metastasis in multiple human tumors.
Gross et al. reported that β-2m is a downstream AR target gene [39]. Huang et al. showed a reciprocal β-2m regulation of AR and PSA in PCa cells [32, 34]. β-2m has been reported to interact with both classical and non-classical members of MHC class I [40, 41]. Josson et al. reported that HFE protein, a non-classical MHC class I member, interacts with β-2m to modulate iron homeostasis by interacting with the transferrin receptor (TFR) and its complex, TFRC, which together govern EMT and ROS in cancer cells. β-2m protected against the influx and accumulation of intracellular iron, and lower levels of intracellular iron activated HIF-1α and its target genes including EMT markers and VEGF [31, 36]. Knocking down either the HFE protein or β-2m resulted in mesenchymal to epithelial transition (MET), a reversal of EMT, decreased cell proliferation and increased apoptosis in PCa cells [42]. β-2m activates intracellular signaling axes mediated by ERK and sterol regulatory element-binding protein-1 (SREBP-1), that drive lipogenesis and lipid and lipid raft-mediated signaling and could potentially enhance the survival of cancer cells [34]. These results together with the demonstration that β-2m-mediated multiple downstream converging signaling pathways, including AR, lipid, iron and ROS [31, 36, 42, 43], could exert powerful influences on the fate of PCa cells and their clinical behavior.
Because genetic knockdown of β-2m or its receptor HFE drives the reversal of EMT with evidence of PCa cell death, we and others have employed anti-β-2m antibodies as reagents to treat both liquid [44, 45] and solid [32, 34, 36, 42] tumors in mice. While these antibodies have no observable effects on the growth of normal organs and cells, application of these antibodies caused remarkable remission of both liquid and solid tumors in experimental mice, compared to the effects of isotype-specific control antibodies [34, 44, 45]. β-2m and its receptor HFE constitute promising new therapeutic targets.
3 Amplification of the cell signaling network through a feed forward mechanism in metastatic cancer cells
While homeostasis in normal organisms is maintained by a negative feedback loop, cancer cells could become “addicted” to a feed forward or positive-feedback loop to survive. In breast cancer bone metastasis, signal amplification via a “vicious cycle” has been shown to maintain a metastatic phenotype. Bone acts as a storage site for growth factors, releasing TGF-β1 and inducing cancer cells to produce PTHrP, which enhanced osteoblast expression of RANKL, increased subsequent interaction with preosteoclast progenitor cells and further enhanced bone turnover and increased further growth factor release from bone to facilitate and support further cancer bone colonization [46]. In a search for new hedgehog signal downstream targets in basal cell carcinoma (BCC), Atwood et al. demonstrated the successful use of a protein screen comprised of scaffold protein MIM (missing in metastasis) which interacts and regulates GLI-1 [47, 48]. They uncovered aPKC-t/λ, an atypical protein kinaseCt/λ that mediates its action by binding to GLI-1 and breaking the positive feedback between GLI-1 and Prkci, both of which are elevated in BCC. During wound healing and tumor invasion and metastasis, Dunkel et al. [49] demonstrated that a new metastasis-associated Gα-interacting vesicle-associated protein, GIV, can be regulated by STAT3 in a feed forward loop by binding to a single cis-element in the GIV promoter region. Hassan et al. [50] observed that miR218 exerted a positive feedback action on Wnt signaling in osteoblasts and breast cancer cells but not normal breast epithelial cells. miR218 was found to stimulate the Wnt pathway by downregulating three Wnt signaling inhibitors, Sclerostin (SOST), Dickkopf2 (DKK2), and secreted frizzled-related protein2 (SFRP2) during osteogenesis. Activated Wnt signaling increased miR218 expression, which further exacerbated Wnt target gene transcription enhancing interactions of osteoblasts and breast cancer cells, potentially increasing breast cancer invasion and metastasis. Other studies, however, found that miR218 has tumor suppressive effects by targeting the focal adhesion pathway in cervical squamous cell carcinoma [51–55]. A feed forward loop could also operate in two lineage-unrelated stromal and epithelial cells. Tang et al. reported that matrix metalloproteinases (MMPs), a family of metal-dependent endopeptidases secreted primarily by tumor stromal cells, can be upregulated by a tumor cell-associated extracellular matrix metalloproteinase inducer, EMMPRIN [56–58]. By genetically engineering a human breast cancer cell line to overexpress recombinant EMMPRIN, they found the engineered cell line could induce breast cancer stromal fibroblasts to produce MMP-2, MMP-9, and EMMPRIN in co-culture. These results suggest that EMMPRIN-positive tumor cells could engage in cancer metastasis by a feed forward action on breast fibromuscular stromal cells. This example of an intercellular feed forward loop could account for increased breast cancer invasion through the degradation of extracellular matrices, ultimately causing increased tumor angiogenesis, tumor growth, and metastatic progression. It should be kept in mind, however, that the roles of MMPs or proteases can be cell context dependent. Maspin, a member of the serine protease inhibitor family, can be lost or gained dependent upon cancer cell type and the intracellular location of this protein seems to play a role in determining whether the overall protease activity alters cell adhesion to a local substratum [59].
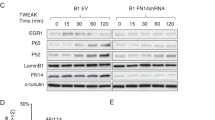
Using RANKL-overexpressing human prostate cancer cells as a model, we demonstrated markedly elevated bone and soft tissue metastatic potential in an indolent LNCaP PCa cell line [21]. The increased bone metastasis can be completely blocked by genetically deleting RANK receptor from RANKL-overexpressing LNCaP cells [60, 61]. We studied the molecular mechanisms underlying RANK-mediated signaling network and found a feed forward loop linking increased transcription of RANKL and c-Met with activation of a host of common transcription factors (TFs) orchestrating a wide range of cellular functions including EMT promotion, osteomimicry, stemness, and neuroendocrine differentiation in PCa cells (Fig. 1). These results, taken together, suggest the crucial roles of feed forward mechanism in conferring cell signaling amplification, which may be tightly regulated during cancer invasion, migration, and metastasis. To understand the potential clinical implications of the amplified RANKL-RANK and c-Met signaling in cell models, we performed multiplex quantum-dot based labeling (mQDL) of primary human PCa tissues with known survival properties [12, 13, 22]. Our results demonstrated that different components in the RANK-mediated cell signaling network predicts the survival of PCa patients in a racially dependent manner in patients of Caucasian-, African-American and Chinese background, confirming the roles of feed forward mechanism in both PCa models and in clinical PCa specimens [13]. The knowledge gained by these mechanistic studies could be applied in the future for more effective targeting of PCa bone and soft tissue metastases (see below).
RANK-mediated signal network in human prostate cancer cells. RNAseq was conducted using prostate cancer cells, with LNCaP background, overexpressing RANKL to compare with cells transduced with a control neo gene. The plot highlighted the interrelationship of differential gene expression between cells with high RANKL-mediated signal network as opposed to the control cells. Genes associated with EMT, stemness, neuroendocrine, osteomimicry, and metastasis were revealed in RANKL-mediated signal network, and these genes are known to be associated with the ability of PCa cells to develop aggressive phenotypes. In addition, we observed a number of LncRNAs either up- or downregulated. In this figure, genes marked in red represent the upregulated genes, whereas genes marked in blue represent the downregulated genes
4 Activation of a coordinated cell signal network by switching-on common TFs and regulatory RNAs
Metastatic cancer cells are evolved to resist hypoxia by efficiently generating new blood supply routes so nutrients can be delivered and toxic metabolites be removed. Metastatic cancer cells must also be able to adapt to their microenvironment so they can establish effective communication networks with their neighbors and gain functions by increasing plasticity and attracting protective and supporting stroma to alter their behaviors, increase growth and aggressiveness, resist therapy-induced cancer cell death, and evade host immunity. When cancer growth and expansion are threatened by failure to meet their minimal metabolic needs, metastatic cancer cells can undergo long-term dormancy to preserve their survivability. Metastatic cancer cells share the common mechanisms to achieve resistance to hypoxia, increased plasticity, cross-talk with cells in their microenvironments, and undergo dormancy. Metastatic cancer cells are able to activate, in a coordinated manner, the specific cell signal networks by switching TFs on or off, recruiting common and regulatory RNAs, and together regulating cancer and developmentally related genes to integrate cell signal networks and promote cancer metastasis.
4.1 Hypoxia resistance
In response to hypoxia, cancer cells survive and thrive by upregulating key TFs such as HIF-1α and HIF-2α that heterodimerize with their β-subunits to turn on more than 1,000 hypoxia-induced target genes, such as TFs, chromatin modifiers, receptors, kinases, transporters, small GTPases, and regulatory micorRNAs (miRNAs) that promote a broad range of cellular functions including neoangiogenesis, stemness, EMT, growth, survival, metastasis, and resistance to therapeutic inhibitory signals to protect the survival of cancer cells despite exposure to detrimental hypoxic conditions [62–64]. Specifically, for example, upregulation of Twist1, Snail, Slug, Zeb1, and Zeb2 could modify cellular EMT programs through either canonical or non-canonical pathways. Smith and Odero-Marah [65] showed that Snail regulates EMT by canonical signaling pathways but regulates bone turnover and neuroendocrine phenotypes by non-canonical pathways in PCa cells. HIF-mediated target genes also regulate inflammation, affecting many developmental pathways [66–70]. Brabletz et al. showed that Zeb1 and miR200 play a reciprocal role in a negative feedback loop controlling Notch signaling in cancer cells [71]. They found that the Zeb1-miR200 negative feedback loop regulates EMT, stem cell maintenance and therapeutic resistance in aggressive pancreatic adenocarcinoma and basal type mammary tumors. Their conclusions were largely supported by Guo et al. who greatly expanded the integrated signaling roles of two circuitries involving Stat3-coordinated Lin-28-let-7-HMGA2 and miR-200-ZEB1. Both are responsible for the initiation and maintenance of oncostatin M-driven EMT in breast cancer cell lines and xenograft models [72]. These data collectively suggest that cancer metastasis and therapeutic resistance, preceded by inflammation, EMT, and/or cancer cell stemness, can be co-targeted by modulating TFs, miRNAs, and specific factors regulating stem cell and EMT phenotypes.
4.2 Increased plasticity and cross-talk in the tumor microenvironment
The concept that tumor–stroma interaction plays key roles in dictating cancer growth and differentiation came from a rich developmental biology literature. Local organ development can be profoundly programmed by embryonic connective tissue microenvironments [73–77]. The interaction is reciprocal and the consequence is largely cell context dependent. Cancer cells have remarkable ability to mimic bone (osteomimicry) [24, 26, 78–80], blood vessels (vasculogenic mimicry) [81–86], mesenchymal cells via EMT [87–89], stem cells [90–93], and neuroendocrine cells via upregulation of specific TFs [94–97], through their interaction with tumor microenvironments. These phenotypic transitions can be transient or permanent depending greatly on physical conditions in the environment, such as 2-D vs. 3-D growth [98–100] and the stiffness of the substratum [101, 102]. When ARCaPE PCa cells were exposed to soluble growth factors in 2-D culture, they underwent EMT reversibly but when the same cells were injected or metastasized to mouse bone, their EMT transition is permanent [103, 104]. Likewise, LNCaP cells cultured in rotary wall vessels under 3-D conditions in the presence of prostate or bone stromal cells exhibit permanent phenotypic and genotypic changes, and co-evolution of LNCaP and prostate and bone stromal cells were observed [105, 106]. These results suggest the possible roles of the in vivo environment, as cells cultured under 3-D conditions differed from cells grown in 2-D, and induced transdifferentiation or exerted “transforming” effects on PCa cells (see below). Our results are in agreement with a recently published review by Kaplun et al. who examined the binding of TFs to the promoter regions of the target genes of maspin, a tumor suppressor lost during PCa progression, by computational analysis [107]. Although PCa cells shared common maspin-induced TFs under different culture conditions, more common TFs either up- or down-regulated by maspin seemed to be shared between 3-D growth and PCa grown in vivo in bone microenvironments than with 2-D growth. Since maspin, identified as an endogenous peptide inhibitor of histone deacetylase-1, functions as a rheostat responsible for fine-tuning or reprogramming epithelial homeostasis, it is possible that the differences in TF profiles identified in PCa cell growth under different culture and in vivo conditions could be contributed epigenetically by histone and chromatin modifications. The participation of TFs in various key cellular functions believed to be the determinants of PCa bone metastasis was revealed in our recent studies of two bone metastatic human prostate cancer cell lines, ARCaPM, which endogenously expressed RANKL, and LNCaP, which was transfected genetically with constitutive RANKL expression vector. We found that both of these models exhibit high propensity for bone metastasis. Analyzing RNA-seq data by a computational method revealed that a RANKL-RANK signaling network in LNCaP cells with constitutive RANKL expression activated a number of master regulator TFs regulating EMT (Twist1, Slug, Zeb1, Zeb2), stem cells (Sox2, Myc, Oct3/4 and Nanog), neuroendocrine cells (Sox 9, HIF-1α and FoxA2) and osteomimicry (c-Myc/Max, Sox2, Sox9, HIF1α and Runx2). The RANK-mediated signal network apparently established a premetastatic niche through a feed forward loop by inducing RANKL and c-Met but repressing androgen receptor (AR) expression and downstream signal pathways through a common transcription factor complex, c-Myc/Max and AP4, which was identified by site-directed mutagenesis and transcription factor deletion/interference assays [21]. These data in aggregate suggest potential new targets focusing on TFs and cell signaling networks for the control of PCa bone metastasis. Figure 1 shows an extended RANK-mediated cell signaling network linking gene expression and cell behaviors in PCa cells. In this RANK-mediated network, we detected both up- (in red) or down- (in blue) regulated gene closely associated with EMT, stemness, neuroendocrine cell, androgen-independence, osteomimicry, and metastasis. In addition, a number of long non-coding RNAs (LncRNA) were also detected to be associated with PCa cell to develop aggressive phenotype.
4.3 Dormancy
Cancer dormancy has been observed frequently in patients. A tumor can be quiescent with no evidence of disease for years until the disease rebounds. Ruppender et al. [108] defined three types of dormancy: micrometastatic dormancy, angiogenic dormancy, and conditional dormancy, referring respectively to restrictive factors such as proliferation/apoptosis equilibrium, angiogenesis, and responsiveness to microenvironmental cues, preventing the cancer cells from colonizing metastatic sites. Coordinated gene expression involving specific sets of TFs has been shown in bacteria, plants and animal cells when they enter and exit from dormancy [109, 110]. In cancer cells, for example, hedgehog signaling could coordinate a response by releasing sonic hedgehog protein from stroma to activate epithelial gene expression via Patched-1 inhibitory receptor, which can release Smoothened to activate GLI-1 transcription factor and increase the expression of GLI-1 downstream target genes, and revive the growth signal in PCa cells [111, 112]. Many other versions of the roles of Hh signaling have been proposed in different cancer types such as GLI-2 as the TF target in breast cancer cells [113] and the involvement of normal prostate stroma as the Hh target in PCa cells [112]. Lu et al. [114] reported the transition of indolent micrometastasis to overt metastasis by overexpressing vascular cell adhesion molecule on the surface of breast cancer cells, which binds to their cognate receptor α4β1 and recruits monocytic osteoclast progenitors, expands the osteoclastogenesis program and results in increased tumor bone colonization. Taichman and colleagues [115, 116] demonstrated the functional link between the GAS6 (secreted by osteoblasts)/Mer, Tyro3 or Axl (receptors on the cell surface of tumor cells) axes in acute lymphoblastic leukemia (ALL) and PCa. In ALL, the GAS6-Mer signaling axis overcame dormancy by promoting cancer cell survival over apoptosis. In PCa, the functions of GAS6 are switched by the relative ratios of Axl and Tyro3 expression in which higher Axl/Tyro3 favors quiescence in a population of disseminated tumor cells (DTCs) in the skeleton whereas reversing these ratios favors the transition of DTCs from a dormant to an active state. LNCaP, a quiescent dormant PCa cell line when inoculated in experimental animals, can become highly metastatic upon the activation of the RANK-mediated cell signaling network [21, 22]. Based on differential gene expression profile analyses, we speculate that RANK-mediated signal activation can overcome all three restrictions surrounding dormancy, by increasing the ratios of proliferation/apoptosis, recruiting angiogenesis components, and enhancing the responsiveness of PCa cells to local derived growth factors and extracellular matrices (ECMs, see Fig. 1). Increasingly, research indicates that tumor dormancy is controlled by miRNAs. Lim et al. [117] showed that co-culture of breast cancer and bone stromal cells resulted in the transfer of miR-127, -197, -222, and -223 to breast cancer cells, mediated by gap junctions, decreasing their CXCL12 expression to restrict these cells to dormancy. Almog et al. [118, 119] found that miR190 enhances tumor dormancy by altering several transcriptional factors, tumor suppressor genes and interferon response pathways. This same group of investigators showed that a cluster of consensus sets of 19 dormancy related miRNAs (DmiRs), can govern the phenotypic switch of dormant human breast carcinoma, glioblastoma, osteosarcoma, and liposarcoma tumors to rapid growth. By upregulating DmiR-580, 588 or 190, they observed a transcriptional reprogramming of tumors while downregulating pro-angiogenic factors such as TIMP-3, bFGF and TGFα reversed fast-growing tumors to undergo dormancy.
5 Recruitment and cooperation with host bystander cells in cancer metastasis
In 2008, Bidard et al. reviewed how cancer cells cooperate in metastasis. They speculated that by means of microenvironment changes, metastatic colonization by non-metastatic primary cancer cells is possible [120]. Five years later, with technological advances including genetically tagged cancer cells and molecular imaging, we have documented that a class of metastasis-initiating or enabling PCa cells (MICs) can trigger microenvironment changes, such as increased osteoclastogenesis, and successfully recruit bystander non-tumorigenic cancer and host cells and promote their metastatic colonization in bone and soft tissues [21, 22]. Our studies used genetically tagged PCa cells as models. We observed the participation of bystander non-tumorigenic cancer cells with MICs to form skeletal and soft tissue metastases. We have advanced the concept proposed by Bidard et al. to show that bystander non-tumorigenic cancer cells [21, 22] or normal host mouse cells [121] can be reprogrammed by malignant cancer cells to exhibit their mimicry phenotypes (e.g. osteomimicry) and even undergo genetic transformation and gain the ability to colonize mouse skeleton through multiple steps, such as EMT, shedding, homing and colonization in bone and soft tissues (Fig. 2). This can be accomplished in part through specific TFs and effector molecules from malignant PCa cells which can turn on the same TFs and effector molecules in bystander cells via feed forward mechanisms. However, how the genetic changes are switched on in the non-tumorigenic cells after encountering MICs remains unknown at this time. Cancer metastasis can also be achieved thorough metabolic cooperation between cells. Liu et al. [122] characterized a PCa and bone mesenchymal model based on genome-wide expression analyses data and found that IL-1β derived from tumor cooperated with COX-2 produced by bone mesenchymal cells to support the growth and neuroendocrine differentiation of PCa cells. Giatromanolaki et al. [123] reported improved energy recycling between tumor-associated stroma (TAS) and cancer epithelium in which cancer epithelium predominately utilizes an anaerobic metabolism to drive the production of lactate whereas the TAS compartment picks up the lactate and converts it into pyruvate for aerobic metabolism and energy production to support the growth of PCa. However, tumor cells are heterogeneous and both aerobic and anaerobic metabolism takes place; hence lactate produced by stromal fibroblasts can also feed the metabolic needs of cancer epithelium. Additionally, Sotgia et al. [124] reported that caveolin-1 loss in the stroma could be used as a predictor for the lethal progression of breast cancer. They proposed a parasitic epithelial-stromal metabolic coupling via glutamine (produced by reactive stromal through autophagy that feeds the growth of cancer cells) and ammonia (produced by the cancer epithelium through an oxidative mitochondrial metabolism that helps maintain autophagy in the stromal compartment), resulting in metabolic collaboration facilitating the maintenance of breast cancer aggressiveness.
Cooperation of metastasis-initiating cells and bystander cancer and normal host cells. Cancer cells with activated RANKL-mediated signal network undergo EMT with increased migratory, invasive, and metastatic potential. These cells gain access to blood supply and intravasate into vascular space. Upon interaction with vascular endothelial sheath in the bone marrow, a small number of the circulating tumor cells are believed to extravasate into bone marrow space through transendothelial migration. Most of the tumor cells in bone, known as disseminated tumor cells, are dormant but can be activated upon the arrival of a poorly defined metastasis-initiating cell population. Positive signal amplification between the dormant cancer cells and normal host cells with metastasis-initiating cells create a favorable growth environment allowing non-tumorigenic cancer cells to break their dormancy. The cooperation with metastasis-initiating cells could provoke permanent gene expression and behavioral changes in the responding bystander cancer cells and normal host cells that are believed to contribute to bone and soft tissue metastases
6 Therapeutic paradigm for targeting bone metastasis based on an understanding of the RANK-mediated signal network
Metastatic castration-resistant PCa (mCRPC) is considered lethal and currently there are limited therapeutic options for managing this condition. Laboratory data support the hypothesis that the RANK-mediated signal network is the driving force for PCa bone metastasis. Based on current bone-directed targeting strategies, we suggest including the following targets downstream from the RANK-mediated signal network: (a) ß-2m. As a pleiotropic signaling molecule for cancer growth and survival, anti-ß-2m antibodies or drugs interfering with iron flux can be used in combination with chemotherapy or radiation therapy to enhance the cytotoxicity of antibodies or drugs in tumor cells [42]. (b) c-Met. Using ATP-competitive (PF 02341066, MK-2461) [125, 126] or non-competitive (ARQ-197) [127] c-Met inhibitors, or cabozatinib (XL-184) [128] which is a receptor tyrosine kinase inhibitor targeting both c-Met and VEGFR2. Additionally, ligand-independent c-Met activation can be blocked by Dasatinib, a Src-kinase inhibitor [129]. (c) Inhibition of c-Myc/Max heterodimerization. There are a number of the small molecules modified from the first generation of inhibitor, 10058-F4 [130, 131], and a newer inhibitor of 10074-GS is in the early stages of drug development. (d) Inhibition of EMT by small designed molecules has been shown to have potential for inhibiting epithelium transition to mesenchyme and stem cells [132, 133]. 5) Inhibition of VEGF-neuropilin complex. Small molecules such as EG0229, EG-3287 and VEGF (amino acid-111-165) are under development. In addition to RANK-mediated signal network components, it should be emphasized that agents interfering with stromal autophagy and miRNA regulators could be developed to interfere with RANK-mediated signal networks. These agents, once developed, can be used in combination with standard hormonal therapy, chemotherapy, immunotherapy, and radiation therapy.
7 Summary and conclusions
Cancer metastasis is a very inefficient process. Cancer cells must escape various host barriers before they can survive and establish metastatic colonization at distant sites. Cancer metastasis to the skeleton represents an advanced and lethal form of the disease. This review summarized how PCa cells mimic bone and establish communication with bone cells through secreted soluble factors. PCa cells amplify the RANK-mediated signal network and reciprocate these signals between metastatic and non-tumorigenic bystander cells. Remarkably, metastatic PCa cells not only amplify RANK-mediated signals in bystander cells, they are also capable of transforming these bystander cells through a feed forward loop to reprogram them from non-tumorigenic status to tumorigenic and bone colonizing PCa cells. Our understanding of the RANK-mediated cell signaling network and its downstream effectors suggests novel therapeutic approaches targeting PCa bone metastasis.
References
Chambers, A. F., Groom, A. C., & MacDonald, I. C. (2002). Dissemination and growth of cancer cells in metastatic sites. Nature Reviews Cancer, 2(8), 563–572. doi:10.1038/nrc865.
Fidler, I. J. (2003). The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nature Reviews Cancer, 3(6), 453–458. doi:10.1038/nrc1098.
Kang, Y., & Massague, J. (2004). Epithelial-mesenchymal transitions: twist in development and metastasis. Cell, 118(3), 277–279. doi:10.1016/j.cell.2004.07.011.
Alderton, G. K. (2012). Metastasis: Converging targets. Naturforschende Review Cancer, 12(12), 793. doi:10.1038/nrc3411.
Hardy, K. M., Kirschmann, D. A., Seftor, E. A., Margaryan, N. V., Postovit, L. M., Strizzi, L., et al. (2010). Regulation of the embryonic morphogen Nodal by Notch4 facilitates manifestation of the aggressive melanoma phenotype. Cancer Research, 70(24), 10340–10350. doi:10.1158/0008-5472.CAN-10-0705.
Cui, H., Grosso, S., Schelter, F., Mari, B., & Kruger, A. (2012). On the Pro-Metastatic Stress Response to Cancer Therapies: Evidence for a Positive Co-Operation between TIMP-1, HIF-1alpha, and miR-210. Frontiers in Pharmacology, 3, 134. doi:10.3389/fphar.2012.00134.
Qi, Y., Li, R. M., Kong, F. M., Li, H., Yu, J. P., & Ren, X. B. (2012). How do tumor stem cells actively escape from host immunosurveillance? Biochemical and Biophysical Research Communications, 420(4), 699–703. doi:10.1016/j.bbrc.2012.03.086.
Mitchell, M. J., & King, M. R. (2013). Computational and experimental models of cancer cell response to fluid shear stress. Frontiers Oncologica, 3, 44. doi:10.3389/fonc.2013.00044.
Di Vizio, D., Morello, M., Dudley, A. C., Schow, P. W., Adam, R. M., Morley, S., et al. (2012). Large oncosomes in human prostate cancer tissues and in the circulation of mice with metastatic disease. The American Journal of Pathology, 181(5), 1573–1584. doi:10.1016/j.ajpath.2012.07.030.
Odero-Marah, V. A., Wang, R., Chu, G., Zayzafoon, M., Xu, J., Shi, C., et al. (2008). Receptor activator of NF-kappaB Ligand (RANKL) expression is associated with epithelial to mesenchymal transition in human prostate cancer cells. Cell Research, 18(8), 858–870. doi:10.1038/cr.2008.84.
Zhau, H. E., Odero-Marah, V., Lue, H. W., Nomura, T., Wang, R., Chu, G., et al. (2008). Epithelial to mesenchymal transition (EMT) in human prostate cancer: lessons learned from ARCaP model. Clinical and Experimental Metastasis, 25(6), 601–610. doi:10.1007/s10585-008-9183-1.
Zhau, H. E., Li, Q., & Chung, L. W. (2013). Interracial differences in prostate cancer progression among patients from the United States, China and Japan. Asian Journal of Andrology. doi:10.1038/aja.2013.86.
Hu, P. Z., Chung, L. W., Berel, D., Frierson, H. F., Yang, H., Liu, C. Y., et al. (2013). Convergent RANK- and c-Met-mediated signaling components predict survival of patients with prostate cancer: an interracial comparative study. PLoS One., 8, e73081.
Roodman, G. D. (2012). Genes associate with abnormal bone cell activity in bone metastasis. Cancer and Metastasis Reviews, 31(3–4), 569–578. doi:10.1007/s10555-012-9372-x.
Joshi, P. A., Jackson, H. W., Beristain, A. G., Di Grappa, M. A., Mote, P. A., Clarke, C. L., et al. (2010). Progesterone induces adult mammary stem cell expansion. Nature, 465(7299), 803–807. doi:10.1038/nature09091.
Li, X., Ominsky, M. S., Stolina, M., Warmington, K. S., Geng, Z., Niu, Q. T., et al. (2009). Increased RANK ligand in bone marrow of orchiectomized rats and prevention of their bone loss by the RANK ligand inhibitor osteoprotegerin. Bone, 45(4), 669–676. doi:10.1016/j.bone.2009.06.011.
Sanbe, T., Tomofuji, T., Ekuni, D., Azuma, T., Irie, K., Tamaki, N., et al. (2009). Vitamin C intake inhibits serum lipid peroxidation and osteoclast differentiation on alveolar bone in rats fed on a high-cholesterol diet. Archives of Oral Biology, 54(3), 235–240. doi:10.1016/j.archoralbio.2008.11.001.
Roodman, G. D., & Dougall, W. C. (2008). RANK ligand as a therapeutic target for bone metastases and multiple myeloma. Cancer Treatment Reviews, 34(1), 92–101. doi:10.1016/j.ctrv.2007.09.002.
Smith, M. R., Saad, F., Coleman, R., Shore, N., Fizazi, K., Tombal, B., et al. (2012). Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet, 379(9810), 39–46. doi:10.1016/S0140-6736(11)61226-9.
Dougall, W. C. (2012). Molecular pathways: osteoclast-dependent and osteoclast-independent roles of the RANKL/RANK/OPG pathway in tumorigenesis and metastasis. Clinical Cancer Research, 18(2), 326–335. doi:10.1158/1078-0432.CCR-10-2507.
Chu, C. Y. (2011). The role of RANKL in prostate cancer progression and bone metastasis. Ph.D Thesis., Georgia State University,
Hu, P., Chu, G. C., Zhu, G., Yang, H., Luthringer, D., Prins, G., et al. (2011). Multiplexed quantum dot labeling of activated c-Met signaling in castration-resistant human prostate cancer. PLoS One, 6(12), e28670. doi:10.1371/journal.pone.0028670.
Cox, R. F., Jenkinson, A., Pohl, K., O’Brien, F. J., & Morgan, M. P. (2012). Osteomimicry of mammary adenocarcinoma cells in vitro; increased expression of bone matrix proteins and proliferation within a 3D collagen environment. PLoS One, 7(7), e41679. doi:10.1371/journal.pone.0041679.
Koeneman, K. S., Yeung, F., & Chung, L. W. (1999). Osteomimetic properties of prostate cancer cells: a hypothesis supporting the predilection of prostate cancer metastasis and growth in the bone environment. Prostate, 39(4), 246–261.
Knerr, K., Ackermann, K., Neidhart, T., & Pyerin, W. (2004). Bone metastasis: Osteoblasts affect growth and adhesion regulons in prostate tumor cells and provoke osteomimicry. International Journal of Cancer, 111(1), 152–159. doi:10.1002/ijc.20223.
Rucci, N., & Teti, A. (2010). Osteomimicry: how tumor cells try to deceive the bone. Frontiers in Bioscience (Scholar Edition), 2, 907–915.
Kavitha, C. V., Deep, G., Gangar, S. C., Jain, A. K., Agarwal, C., & Agarwal, R. (2012). Silibinin inhibits prostate cancer cells- and RANKL-induced osteoclastogenesis by targeting NFATc1, NF-kappaB, and AP-1 Activation in RAW264.7 cells. Molecular Carcinogenesis. doi:10.1002/mc.21959.
Graham, T. R., Agrawal, K. C., & Abdel-Mageed, A. B. (2010). Independent and cooperative roles of tumor necrosis factor-alpha, nuclear factor-kappaB, and bone morphogenetic protein-2 in regulation of metastasis and osteomimicry of prostate cancer cells and differentiation and mineralization of MC3T3-E1 osteoblast-like cells. Cancer Science, 101(1), 103–111. doi:10.1111/j.1349-7006.2009.01356.x.
Yuen, H. F., Kwok, W. K., Chan, K. K., Chua, C. W., Chan, Y. P., Chu, Y. Y., et al. (2008). TWIST modulates prostate cancer cell-mediated bone cell activity and is upregulated by osteogenic induction. Carcinogenesis, 29(8), 1509–1518. doi:10.1093/carcin/bgn105.
Glait-Santar, C., & Benayahu, D. (2012). Regulation of SVEP1 gene expression by 17beta-estradiol and TNFalpha in pre-osteoblastic and mammary adenocarcinoma cells. The Journal of Steroid Biochemistry and Molecular Biology, 130(1–2), 36–44. doi:10.1016/j.jsbmb.2011.12.015.
Josson, S., Nomura, T., Lin, J. T., Huang, W. C., Wu, D., Zhau, H. E., et al. (2011). beta2-microglobulin induces epithelial to mesenchymal transition and confers cancer lethality and bone metastasis in human cancer cells. Cancer Research, 71(7), 2600–2610. doi:10.1158/0008-5472.CAN-10-3382.
Huang, W. C., Havel, J. J., Zhau, H. E., Qian, W. P., Lue, H. W., Chu, C. Y., et al. (2008). Beta2-microglobulin signaling blockade inhibited androgen receptor axis and caused apoptosis in human prostate cancer cells. Clinical Cancer Research, 14(17), 5341–5347. doi:10.1158/1078-0432.CCR-08-0793.
Huang, W. C., Wu, D., Xie, Z., Zhau, H. E., Nomura, T., Zayzafoon, M., et al. (2006). beta2-microglobulin is a signaling and growth-promoting factor for human prostate cancer bone metastasis. Cancer Research, 66(18), 9108–9116. doi:10.1158/0008-5472.CAN-06-1996.
Huang, W. C., Zhau, H. E., & Chung, L. W. (2010). Androgen receptor survival signaling is blocked by anti-beta2-microglobulin monoclonal antibody via a MAPK/lipogenic pathway in human prostate cancer cells. The Journal of Biological Chemistry, 285(11), 7947–7956. doi:10.1074/jbc.M109.092759.
Nomura, T., Huang, W. C., Seo, S., Zhau, H. E., Mimata, H., & Chung, L. W. (2007). Targeting beta2-microglobulin mediated signaling as a novel therapeutic approach for human renal cell carcinoma. The Journal of Urology, 178(1), 292–300. doi:10.1016/j.juro.2007.03.007.
Nomura, T., Huang, W. C., Zhau, H. E., Josson, S., Mimata, H., & Chung, L. W. (2013). beta2-Microglobulin-mediated signaling as a target for cancer therapy. Anticancer Agents Med Chem. doi:10.2174/18715206113139990092
Nomura, T., Huang, W. C., Zhau, H. E., Wu, D., Xie, Z., Mimata, H., et al. (2006). Beta2-microglobulin promotes the growth of human renal cell carcinoma through the activation of the protein kinase A, cyclic AMP-responsive element-binding protein, and vascular endothelial growth factor axis. Clinical Cancer Research, 12(24), 7294–7305. doi:10.1158/1078-0432.CCR-06-2060.
Lue, H. W., Yang, X., Wang, R., Qian, W., Xu, R. Z., Lyles, R., et al. (2011). LIV-1 promotes prostate cancer epithelial-to-mesenchymal transition and metastasis through HB-EGF shedding and EGFR-mediated ERK signaling. PLoS One, 6(11), e27720. doi:10.1371/journal.pone.0027720.
Gross, M., Top, I., Laux, I., Katz, J., Curran, J., Tindell, C., et al. (2007). Beta-2-microglobulin is an androgen-regulated secreted protein elevated in serum of patients with advanced prostate cancer. Clinical Cancer Research, 13(7), 1979–1986. doi:10.1158/1078-0432.CCR-06-1156.
Michaelson, J. (1983). Genetics of beta-2 microglobulin in the mouse. Immunogenetics, 17(3), 219–260.
Solheim, J. C. (1999). Class I MHC molecules: assembly and antigen presentation. Immunological Reviews, 172, 11–19.
Josson, S., Matsuoka, Y., Gururajan, M., Nomura, T., Huang, W. C., Yang, X., et al. (2013). Inhibition of beta2-Microglobulin/Hemochromatosis Enhances Radiation Sensitivity by Induction of Iron Overload in Prostate Cancer Cells. PLoS One, 8(7), e68366. doi:10.1371/journal.pone.0068366.
Josson, S., Matsuoka, Y., Chung, L. W., Zhau, H. E., & Wang, R. (2010). Tumor-stroma co-evolution in prostate cancer progression and metastasis. Seminars in Cell and Developmental Biology, 21(1), 26–32. doi:10.1016/j.semcdb.2009.11.016.
Yang, J., Qian, J., Wezeman, M., Wang, S., Lin, P., Wang, M., et al. (2006). Targeting beta2-microglobulin for induction of tumor apoptosis in human hematological malignancies. Cancer Cell, 10(4), 295–307. doi:10.1016/j.ccr.2006.08.025.
Yang, J., Zhang, X., Wang, J., Qian, J., Zhang, L., Wang, M., et al. (2007). Anti beta2-microglobulin monoclonal antibodies induce apoptosis in myeloma cells by recruiting MHC class I to and excluding growth and survival cytokine receptors from lipid rafts. Blood, 110(8), 3028–3035. doi:10.1182/blood-2007-06-094417.
Guise, T. A., Kozlow, W. M., Heras-Herzig, A., Padalecki, S. S., Yin, J. J., & Chirgwin, J. M. (2005). Molecular mechanisms of breast cancer metastases to bone. Clinical of Breast Cancer, 5(2), S46–S53.
Atwood, S. X., Li, M., Lee, A., Tang, J. Y., & Oro, A. E. (2013). GLI activation by atypical protein kinase C iota/lambda regulates the growth of basal cell carcinomas. Nature, 494(7438), 484–488. doi:10.1038/nature11889.
Bershteyn, M., Atwood, S. X., Woo, W. M., Li, M., & Oro, A. E. (2010). MIM and cortactin antagonism regulates ciliogenesis and hedgehog signaling. Developmental Cell, 19(2), 270–283. doi:10.1016/j.devcel.2010.07.009.
Dunkel, Y., Ong, A., Notani, D., Mittal, Y., Lam, M., Mi, X., et al. (2012). STAT3 protein up-regulates Galpha-interacting vesicle-associated protein (GIV)/Girdin expression, and GIV enhances STAT3 activation in a positive feedback loop during wound healing and tumor invasion/metastasis. The Journal of Biological Chemistry, 287(50), 41667–41683. doi:10.1074/jbc.M112.390781.
Hassan, M. Q., Maeda, Y., Taipaleenmaki, H., Zhang, W., Jafferji, M., Gordon, J. A., et al. (2012). miR-218 directs a Wnt signaling circuit to promote differentiation of osteoblasts and osteomimicry of metastatic cancer cells. The Journal of Biological Chemistry, 287(50), 42084–42092. doi:10.1074/jbc.M112.377515.
Kinoshita, T., Hanazawa, T., Nohata, N., Kikkawa, N., Enokida, H., Yoshino, H., et al. (2012). Tumor suppressive microRNA-218 inhibits cancer cell migration and invasion through targeting laminin-332 in head and neck squamous cell carcinoma. Oncotarget, 3(11), 1386–1400.
Tatarano, S., Chiyomaru, T., Kawakami, K., Enokida, H., Yoshino, H., Hidaka, H., et al. (2011). miR-218 on the genomic loss region of chromosome 4p15.31 functions as a tumor suppressor in bladder cancer. International Journal of Oncology, 39(1), 13–21. doi:10.3892/ijo.2011.1012.
Uesugi, A., Kozaki, K., Tsuruta, T., Furuta, M., Morita, K., Imoto, I., et al. (2011). The tumor suppressive microRNA miR-218 targets the mTOR component Rictor and inhibits AKT phosphorylation in oral cancer. Cancer Research, 71(17), 5765–5778. doi:10.1158/0008-5472.CAN-11-0368.
Yamamoto, N., Kinoshita, T., Nohata, N., Itesako, T., Yoshino, H., Enokida, H., et al. (2013). Tumor suppressive microRNA-218 inhibits cancer cell migration and invasion by targeting focal adhesion pathways in cervical squamous cell carcinoma. International Journal of Oncology, 42(5), 1523–1532. doi:10.3892/ijo.2013.1851.
Yamasaki, T., Seki, N., Yoshino, H., Itesako, T., Hidaka, H., Yamada, Y., et al. (2013). MicroRNA-218 Inhibits Cell Migration and Invasion in Renal Cell Carcinoma through Targeting Caveolin-2 Involved in Focal Adhesion Pathway. The Journal of Urology, 190(3), 1059–1068. doi:10.1016/j.juro.2013.02.089.
Tang, Y., Kesavan, P., Nakada, M. T., & Yan, L. (2004). Tumor-stroma interaction: positive feedback regulation of extracellular matrix metalloproteinase inducer (EMMPRIN) expression and matrix metalloproteinase-dependent generation of soluble EMMPRIN. Molecular Cancer Research, 2(2), 73–80.
Tang, Y., Nakada, M. T., Kesavan, P., McCabe, F., Millar, H., Rafferty, P., et al. (2005). Extracellular matrix metalloproteinase inducer stimulates tumor angiogenesis by elevating vascular endothelial cell growth factor and matrix metalloproteinases. Cancer Research, 65(8), 3193–3199. doi:10.1158/0008-5472.CAN-04-3605.
Tang, Y., Nakada, M. T., Rafferty, P., Laraio, J., McCabe, F. L., Millar, H., et al. (2006). Regulation of vascular endothelial growth factor expression by EMMPRIN via the PI3K-Akt signaling pathway. Molecular Cancer Research, 4(6), 371–377. doi:10.1158/1541-7786.MCR-06-0042.
Marioni, G., Blandamura, S., Giacomelli, L., Calgaro, N., Segato, P., Leo, G., et al. (2005). Nuclear expression of maspin is associated with a lower recurrence rate and a longer disease-free interval after surgery for squamous cell carcinoma of the larynx. Histopathology, 46(5), 576–582. doi:10.1111/j.1365-2559.2005.02141.x.
Chu, G. C.-Y., Zhau, H. E., Wang, R. Rogatko, A., Feng, X., Zayzafoon, M., Liu, Y., Farach-Carson, M. C., You, S., Kim, J., Freeman, M. R., Chung, L. W. (2013). RANK- and c-Met-mediated signal network promotes prostate cancer metastatic colonization. Endocr Relat Cancer (in press).
Chu, G. C.-Y., Zhau, H. E., Wang, R. Rogatko, A., Feng, X., Zayzafoon, M., Liu, Y., Farach-Carson, M. C., Chung, L. W. (2013). Autocrine/paracrine RANKL-RANK signaling promotes cancer bone metastasis and establishes premetastatic niche recruiting bystander cancer cells to participate in the metastatic process. Washington, DC: American Association for Cancer Research.
Kaur, B., Khwaja, F. W., Severson, E. A., Matheny, S. L., Brat, D. J., & Van Meir, E. G. (2005). Hypoxia and the hypoxia-inducible-factor pathway in glioma growth and angiogenesis. Neuro-Oncology, 7(2), 134–153. doi:10.1215/S1152851704001115.
Kimbro, K. S., & Simons, J. W. (2006). Hypoxia-inducible factor-1 in human breast and prostate cancer. Endocrine-Related Cancer, 13(3), 739–749. doi:10.1677/erc.1.00728.
Powis, G., & Kirkpatrick, L. (2004). Hypoxia inducible factor-1alpha as a cancer drug target. Molecular Cancer Therapeutics, 3(5), 647–654.
Smith, B. N., & Odero-Marah, V. A. (2012). The role of Snail in prostate cancer. Cell Adhesion & Migration, 6(5), 433–441. doi:10.4161/cam.21687.
Jiang, J., Tang, Y. L., & Liang, X. H. (2011). EMT: a new vision of hypoxia promoting cancer progression. Cancer Biology and Therapy, 11(8), 714–723.
Konisti, S., Kiriakidis, S., & Paleolog, E. M. (2012). Hypoxia–a key regulator of angiogenesis and inflammation in rheumatoid arthritis. Nature Reviews. Rheumatology, 8(3), 153–162. doi:10.1038/nrrheum.2011.205.
McNamee, E. N., Korns Johnson, D., Homann, D., & Clambey, E. T. (2013). Hypoxia and hypoxia-inducible factors as regulators of T cell development, differentiation, and function. Immunologic Research, 55(1–3), 58–70. doi:10.1007/s12026-012-8349-8.
Shay, J. E., & Celeste Simon, M. (2012). Hypoxia-inducible factors: crosstalk between inflammation and metabolism. Seminars in Cell and Developmental Biology, 23(4), 389–394. doi:10.1016/j.semcdb.2012.04.004.
Tomita, S., Kihira, Y., Imanishi, M., Fukuhara, Y., Imamura, Y., Ishizawa, K., et al. (2011). Pathophysiological response to hypoxia - from the molecular mechanisms of malady to drug discovery:inflammatory responses of hypoxia-inducible factor 1alpha (HIF-1alpha) in T cells observed in development of vascular remodeling. Journal of Pharmacological Sciences, 115(4), 433–439.
Brabletz, S., & Brabletz, T. (2010). The ZEB/miR-200 feedback loop–a motor of cellular plasticity in development and cancer? EMBO Reports, 11(9), 670–677. doi:10.1038/embor.2010.117.
Guo, L., Chen, C., Shi, M., Wang, F., Chen, X., Diao, D., et al. (2013). Stat3-coordinated Lin-28-let-7-HMGA2 and miR-200-ZEB1 circuits initiate and maintain oncostatin M-driven epithelial-mesenchymal transition. Oncogene. doi:10.1038/onc.2012.573.
Chung, L. W. (1995). The role of stromal-epithelial interaction in normal and malignant growth. Cancer Surveys, 23, 33–42.
Cunha, G. R. (1994). Role of mesenchymal-epithelial interactions in normal and abnormal development of the mammary gland and prostate. Cancer, 74(3 Suppl), 1030–1044.
Donjacour, A. A., & Cunha, G. R. (1991). Stromal regulation of epithelial function. Cancer Treatment and Research, 53, 335–364.
Roberts, A. B., & Sporn, M. B. (1987). Transforming growth factor-beta: potential common mechanisms mediating its effects on embryogenesis, inflammation-repair, and carcinogenesis. International Journal of Radiation Applications and Instrumentation. Part B, 14(4), 435–439.
Sakakura, T. (1991). New aspects of stroma-parenchyma relations in mammary gland differentiation. International Review of Cytology, 125, 165–202.
Chung, L. W., Huang, W. C., Sung, S. Y., Wu, D., Odero-Marah, V., Nomura, T., et al. (2006). Stromal-epithelial interaction in prostate cancer progression. Clinical Genitourinary Cancer, 5(2), 162–170. doi:10.3816/CGC.2006.n.034.
Clezardin, P., & Teti, A. (2007). Bone metastasis: pathogenesis and therapeutic implications. Clinical and Experimental Metastasis, 24(8), 599–608. doi:10.1007/s10585-007-9112-8.
Tsubochi, H., Endo, S., Oda, Y., & Dobashi, Y. (2013). Carcinoid tumor of the lung with massive ossification: report of a case showing the evidence of osteomimicry and review of the literature. International Journal of Clinical and Experimental Pathology, 6(5), 957–961.
Bhatia, M. (2010). Developmental biology. Microenvironment mimicry. Science, 329(5995), 1024–1025. doi:10.1126/science.1194919.
Bissell, M. J. (1999). Tumor plasticity allows vasculogenic mimicry, a novel form of angiogenic switch. A rose by any other name? American Journal of Pathologists, 155(3), 675–679. doi:10.1016/S0002-9440(10)65164-4.
Folberg, R., Hendrix, M. J., & Maniotis, A. J. (2000). Vasculogenic mimicry and tumor angiogenesis. The American Journal of Pathology, 156(2), 361–381. doi:10.1016/S0002-9440(10)64739-6.
Folberg, R., & Maniotis, A. J. (2004). Vasculogenic mimicry. APMIS, 112(7–8), 508–525. doi:10.1111/j.1600-0463.2004.apm11207-0810.x.
Hendrix, M. J., Seftor, E. A., Hess, A. R., & Seftor, R. E. (2003). Vasculogenic mimicry and tumour-cell plasticity: lessons from melanoma. Nature Reviews Cancer, 3(6), 411–421. doi:10.1038/nrc1092.
McDonald, D. M., Munn, L., & Jain, R. K. (2000). Vasculogenic mimicry: how convincing, how novel, and how significant? The American Journal of Pathology, 156(2), 383–388. doi:10.1016/S0002-9440(10)64740-2.
Hugo, H., Ackland, M. L., Blick, T., Lawrence, M. G., Clements, J. A., Williams, E. D., et al. (2007). Epithelial–mesenchymal and mesenchymal–epithelial transitions in carcinoma progression. Journal of Cellular Physiology, 213(2), 374–383. doi:10.1002/jcp.21223.
Nauseef, J. T., & Henry, M. D. (2011). Epithelial-to-mesenchymal transition in prostate cancer: paradigm or puzzle? Nature Reviews. Urology, 8(8), 428–439. doi:10.1038/nrurol.2011.85.
van der Pluijm, G. (2011). Epithelial plasticity, cancer stem cells and bone metastasis formation. Bone, 48(1), 37–43. doi:10.1016/j.bone.2010.07.023.
Cogle, C. R., Theise, N. D., Fu, D., Ucar, D., Lee, S., Guthrie, S. M., et al. (2007). Bone marrow contributes to epithelial cancers in mice and humans as developmental mimicry. Stem Cells, 25(8), 1881–1887. doi:10.1634/stemcells.2007-0163.
Ping, Y. F., & Bian, X. W. (2011). Consice review: Contribution of cancer stem cells to neovascularization. Stem Cells, 29(6), 888–894. doi:10.1002/stem.650.
Timar, J., Tovari, J., Raso, E., Meszaros, L., Bereczky, B., & Lapis, K. (2005). Platelet-mimicry of cancer cells: epiphenomenon with clinical significance. Oncology, 69(3), 185–201. doi:10.1159/000088069.
Yao, X. H., Ping, Y. F., & Bian, X. W. (2011). Contribution of cancer stem cells to tumor vasculogenic mimicry. Protein & Cell, 2(4), 266–272. doi:10.1007/s13238-011-1041-2.
Danza, G., Di Serio, C., Rosati, F., Lonetto, G., Sturli, N., Kacer, D., et al. (2012). Notch signaling modulates hypoxia-induced neuroendocrine differentiation of human prostate cancer cells. Molecular Cancer Research, 10(2), 230–238. doi:10.1158/1541-7786.MCR-11-0296.
Eisinger-Mathason, T. S., & Simon, M. C. (2010). HIF-1alpha partners with FoxA2, a neuroendocrine-specific transcription factor, to promote tumorigenesis. Cancer Cell, 18(1), 3–4. doi:10.1016/j.ccr.2010.06.007.
McKeithen, D., Graham, T., Chung, L. W., & Odero-Marah, V. (2010). Snail transcription factor regulates neuroendocrine differentiation in LNCaP prostate cancer cells. Prostate, 70(9), 982–992. doi:10.1002/pros.21132.
Spiotto, M. T., & Chung, T. D. (2000). STAT3 mediates IL-6-induced neuroendocrine differentiation in prostate cancer cells. Prostate, 42(3), 186–195.
Lang, S. H., Sharrard, R. M., Stark, M., Villette, J. M., & Maitland, N. J. (2001). Prostate epithelial cell lines form spheroids with evidence of glandular differentiation in three-dimensional Matrigel cultures. British Journal of Cancer, 85(4), 590–599. doi:10.1054/bjoc.2001.1967.
Lang, S. H., Stark, M., Collins, A., Paul, A. B., Stower, M. J., & Maitland, N. J. (2001). Experimental prostate epithelial morphogenesis in response to stroma and three-dimensional matrigel culture. Cell Growth and Differentiation, 12(12), 631–640.
Winkenwerder, J. J., Palechek, P. L., Reece, J. S., Saarinen, M. A., Arnold, M. A., Cohen, M. B., et al. (2003). Evaluating prostate cancer cell culturing methods: a comparison of cell morphologies and metabolic activity. Oncology Reports, 10(4), 783–789.
Baker, E. L., Bonnecaze, R. T., & Zaman, M. H. (2009). Extracellular matrix stiffness and architecture govern intracellular rheology in cancer. Biophysical Journal, 97(4), 1013–1021. doi:10.1016/j.bpj.2009.05.054.
Docheva, D., Padula, D., Schieker, M., & Clausen-Schaumann, H. (2010). Effect of collagen I and fibronectin on the adhesion, elasticity and cytoskeletal organization of prostate cancer cells. Biochemical and Biophysical Research Communications, 402(2), 361–366. doi:10.1016/j.bbrc.2010.10.034.
He, H., Yang, X., Davidson, A. J., Wu, D., Marshall, F. F., Chung, L. W., et al. (2010). Progressive epithelial to mesenchymal transitions in ARCaP E prostate cancer cells during xenograft tumor formation and metastasis. Prostate, 70(5), 518–528. doi:10.1002/pros.21086.
Xu, J., Wang, R., Xie, Z. H., Odero-Marah, V., Pathak, S., Multani, A., et al. (2006). Prostate cancer metastasis: role of the host microenvironment in promoting epithelial to mesenchymal transition and increased bone and adrenal gland metastasis. Prostate, 66(15), 1664–1673. doi:10.1002/pros.20488.
Rhee, H. W., Zhau, H. E., Pathak, S., Multani, A. S., Pennanen, S., Visakorpi, T., et al. (2001). Permanent phenotypic and genotypic changes of prostate cancer cells cultured in a three-dimensional rotating-wall vessel. In Vitro Cell Dev Biol Anim, 37(3), 127–140. doi:10.1290/1071-2690(2001)037<0127:PPAGCO>2.0.CO;2.
Sung, S. Y., Hsieh, C. L., Law, A., Zhau, H. E., Pathak, S., Multani, A. S., et al. (2008). Coevolution of prostate cancer and bone stroma in three-dimensional coculture: implications for cancer growth and metastasis. Cancer Research, 68(23), 9996–10003. doi:10.1158/0008-5472.CAN-08-2492.
Kaplun, A., Dzinic, S., Bernardo, M., & Sheng, S. (2012). Tumor suppressor maspin as a rheostat in HDAC regulation to achieve the fine-tuning of epithelial homeostasis. Critical Reviews in Eukaryotic Gene Expression, 22(3), 249–258.
Ruppender, N. S., Morrissey, C., Lange, P. H., & Vessella, R. L. (2013). Dormancy in solid tumors: implications for prostate cancer. Cancer and Metastasis Reviews. doi:10.1007/s10555-013-9422-z.
Chauhan, S., & Tyagi, J. S. (2008). Interaction of DevR with multiple binding sites synergistically activates divergent transcription of narK2-Rv1738 genes in Mycobacterium tuberculosis. Journal of Bacteriology, 190(15), 5394–5403. doi:10.1128/JB.00488-08.
Vaistij, F. E., Gan, Y., Penfield, S., Gilday, A. D., Dave, A., He, Z., et al. (2013). Differential control of seed primary dormancy in Arabidopsis ecotypes by the transcription factor SPATULA. Proceedings of the National Academy of Sciences of the United States of America, 110(26), 10866–10871. doi:10.1073/pnas.1301647110.
Nadendla, S. K., Hazan, A., Ward, M., Harper, L. J., Moutasim, K., Bianchi, L. S., et al. (2011). GLI1 confers profound phenotypic changes upon LNCaP prostate cancer cells that include the acquisition of a hormone independent state. PLoS One, 6(5), e20271. doi:10.1371/journal.pone.0020271.
Shigemura, K., Huang, W. C., Li, X., Zhau, H. E., Zhu, G., Gotoh, A., et al. (2011). Active sonic hedgehog signaling between androgen independent human prostate cancer cells and normal/benign but not cancer-associated prostate stromal cells. Prostate, 71(16), 1711–1722. doi:10.1002/pros.21388.
Javelaud, D., Alexaki, V. I., Dennler, S., Mohammad, K. S., Guise, T. A., & Mauviel, A. (2011). TGF-beta/SMAD/GLI2 signaling axis in cancer progression and metastasis. Cancer Research, 71(17), 5606–5610. doi:10.1158/0008-5472.CAN-11-1194.
Lu, X., Mu, E., Wei, Y., Riethdorf, S., Yang, Q., Yuan, M., et al. (2011). VCAM-1 promotes osteolytic expansion of indolent bone micrometastasis of breast cancer by engaging alpha4beta1-positive osteoclast progenitors. Cancer Cell, 20(6), 701–714. doi:10.1016/j.ccr.2011.11.002.
Shiozawa, Y., Pedersen, E. A., & Taichman, R. S. (2010). GAS6/Mer axis regulates the homing and survival of the E2A/PBX1-positive B-cell precursor acute lymphoblastic leukemia in the bone marrow niche. Experimental Hematology, 38(2), 132–140. doi:10.1016/j.exphem.2009.11.002.
Taichman, R. S., Patel, L. R., Bedenis, R., Wang, J., Weidner, S., Schumann, T., et al. (2013). GAS6 receptor status is associated with dormancy and bone metastatic tumor formation. PLoS One, 8(4), e61873. doi:10.1371/journal.pone.0061873.
Lim, P. K., Bliss, S. A., Patel, S. A., Taborga, M., Dave, M. A., Gregory, L. A., et al. (2011). Gap junction-mediated import of microRNA from bone marrow stromal cells can elicit cell cycle quiescence in breast cancer cells. Cancer Research, 71(5), 1550–1560. doi:10.1158/0008-5472.CAN-10-2372.
Almog, N., Briggs, C., Beheshti, A., Ma, L., Wilkie, K. P., Rietman, E., et al. (2013). Transcriptional changes induced by the tumor dormancy-associated microRNA-190. Transcription, 4(4).
Almog, N., Ma, L., Schwager, C., Brinkmann, B. G., Beheshti, A., Vajkoczy, P., et al. (2012). Consensus micro RNAs governing the switch of dormant tumors to the fast-growing angiogenic phenotype. PLoS One, 7(8), e44001. doi:10.1371/journal.pone.0044001.
Bidard, F. C., Pierga, J. Y., Vincent-Salomon, A., & Poupon, M. F. (2008). A “class action” against the microenvironment: do cancer cells cooperate in metastasis? Cancer and Metastasis Reviews, 27(1), 5–10. doi:10.1007/s10555-007-9103-x.
Pathak, S., Nemeth, M. A., Multani, A. S., Thalmann, G. N., von Eschenbach, A. C., & Chung, L. W. (1997). Can cancer cells transform normal host cells into malignant cells? British Journal of Cancer, 76(9), 1134–1138.
Liu, Q., Russell, M. R., Shahriari, K., Jernigan, D. L., Lioni, M. I., Garcia, F. U., et al. (2013). Interleukin-1beta promotes skeletal colonization and progression of metastatic prostate cancer cells with neuroendocrine features. Cancer Research, 73(11), 3297–3305. doi:10.1158/0008-5472.CAN-12-3970.
Giatromanolaki, A., Koukourakis, M. I., Koutsopoulos, A., Mendrinos, S., & Sivridis, E. (2012). The metabolic interactions between tumor cells and tumor-associated stroma (TAS) in prostatic cancer. Cancer Biology and Therapy, 13(13), 1284–1289. doi:10.4161/cbt.21785.
Sotgia, F., Martinez-Outschoorn, U. E., Pavlides, S., Howell, A., Pestell, R. G., & Lisanti, M. P. (2011). Understanding the Warburg effect and the prognostic value of stromal caveolin-1 as a marker of a lethal tumor microenvironment. Breast Cancer Research, 13(4), 213. doi:10.1186/bcr2892.
Tumati, V., Kumar, S., Yu, L., Chen, B., Choy, H., & Saha, D. (2013). Effect of PF-02341066 and radiation on non-small cell lung cancer cells. Oncology Reports, 29(3), 1094–1100. doi:10.3892/or.2012.2198.
Pan, B. S., Chan, G. K., Chenard, M., Chi, A., Davis, L. J., Deshmukh, S. V., et al. (2010). MK-2461, a novel multitargeted kinase inhibitor, preferentially inhibits the activated c-Met receptor. Cancer Research, 70(4), 1524–1533. doi:10.1158/0008-5472.CAN-09-2541.
Munshi, N., Jeay, S., Li, Y., Chen, C. R., France, D. S., Ashwell, M. A., et al. (2010). ARQ 197, a novel and selective inhibitor of the human c-Met receptor tyrosine kinase with antitumor activity. Molecular Cancer Therapeutics, 9(6), 1544–1553. doi:10.1158/1535-7163.MCT-09-1173.
Yakes, F. M., Chen, J., Tan, J., Yamaguchi, K., Shi, Y., Yu, P., et al. (2011). Cabozantinib (XL184), a novel MET and VEGFR2 inhibitor, simultaneously suppresses metastasis, angiogenesis, and tumor growth. Molecular Cancer Therapeutics, 10(12), 2298–2308. doi:10.1158/1535-7163.MCT-11-0264.
Sen, B., Peng, S., Saigal, B., Williams, M. D., & Johnson, F. M. (2011). Distinct interactions between c-Src and c-Met in mediating resistance to c-Src inhibition in head and neck cancer. Clinical Cancer Research, 17(3), 514–524. doi:10.1158/1078-0432.CCR-10-1617.
Harvey, S. R., Porrini, M., Stachl, C., MacMillan, D., Zinzalla, G., & Barran, P. E. (2012). Small-molecule inhibition of c-MYC:MAX leucine zipper formation is revealed by ion mobility mass spectrometry. Journal of the American Chemical Society, 134(47), 19384–19392. doi:10.1021/ja306519h.
Kim, J., Roh, M., & Abdulkadir, S. A. (2010). Pim1 promotes human prostate cancer cell tumorigenicity and c-MYC transcriptional activity. BMC Cancer, 10, 248. doi:10.1186/1471-2407-10-248.
Carmody, L. C., Germain, A., Morgan, B., VerPlank, L., Fernandez, C., Feng, Y., et al. (2010). Identification of a Selective Small-Molecule Inhibitor of Breast Cancer Stem Cells - Probe 2. In Probe Reports from the NIH Molecular Libraries Program. Bethesda (MD).
Park, C. Y., Son, J. Y., Jin, C. H., Nam, J. S., Kim, D. K., & Sheen, Y. Y. (2011). EW-7195, a novel inhibitor of ALK5 kinase inhibits EMT and breast cancer metastasis to lung. European Journal of Cancer, 47(17), 2642–2653. doi:10.1016/j.ejca.2011.07.007.
Acknowledgments
This work was supported in part by a NCI PO-1 grant (2P01CA098912), RO-1 grant (1R01CA122602), Board of Governor's Distinguished Cancer Chair and PCF Challenge and 2013 Steve Wynn Young Investigator Awards. We thank Mr. Gary Mawyer from the University of Virginia for editorial assistance, Dr. Ruoxiang Wang from Cedars-Sinai Medical Center for his role in providing critical reading of this manuscript and manuscript processing, and Drs. John Lu and Murali Gururajan from Cedars-Sinai Medical Center for their help in the construction of RANK-mediated signal network in PCa cells.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, G.CY., Chung, L.W.K. RANK-mediated signaling network and cancer metastasis. Cancer Metastasis Rev 33, 497–509 (2014). https://doi.org/10.1007/s10555-013-9488-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-013-9488-7