Abstract
Pancreatic cancer is critical for developed countries, where its rate of diagnosis has been increasing steadily annually. In the past decade, the advances of pancreatic cancer research have not contributed to the decline in mortality rates from pancreatic cancer—the overall 5-year survival rate remains about 5% low. This number only underscores an obvious urgency for us to better understand the biological features of pancreatic carcinogenesis, to develop early detection methods, and to improve novel therapeutic treatments. To achieve these goals, animal modeling that faithfully recapitulates the whole process of human pancreatic cancer is central to making the advancements. In this review, we summarize the currently available animal models for pancreatic cancer and the advances in pancreatic cancer animal modeling. We compare and contrast the advantages and disadvantages of three major categories of these models: (1) carcinogen-induced; (2) xenograft and allograft; and (3) genetically engineered mouse models. We focus more on the genetically engineered mouse models, a category which has been rapidly expanded recently for their capacities to mimic human pancreatic cancer and metastasis, and highlight the combinations of these models with various newly developed strategies and cell-lineage labeling systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Pancreatic cancer is one of the leading causes of cancer death in developed countries. Histologically, the majority of human pancreatic cancer is presented as pancreatic ductal adenocarcinoma (PDAC), which can arise from either a PanIN (pancreatic intraepithelial neoplasias) or IPMN (intraductal papillary mucinous neoplasms) precursor lesion. Other non-endocrine variants include acinar cell carcinoma, medullary cancer, colloid/mucinous non-cystic cancer, adenosquamous carcinoma, pancreatoblastomas, undifferentiated carcinoma, etc.; with only 1% as endocrine tumors. Three major histologically defined precursors to invasive adenocarcinoma of the pancreas have been described. These include pancreatic intraepithelial neoplasias (PanINs), which primarily derive from the small ducts and give rise to PDAC; IPMNs, which occur in the main pancreatic duct or branch ducts; and MCNs, where cystic lesions are featured by lining with mucinous tall columnar epithelia and surrounding with an associated ovarian-type stroma [1–5]. The progress from pancreatic preneoplastic lesions to invasive carcinoma is a very long process in humans [6], which usually takes multiple steps to accumulate a series of gene mutations including activation of oncogenes and inactivation of tumor-suppressor genes. For example, the various grades of PanINs ranging from low-grade PanIN-1A and 1B to PanIN-2 and high-grade PanIN-3 display a correlative relationship between accumulating clonal mutations in Kras, p16, p53, and Smad4 with increasing cellular atypia in human samples [4, 7–14]. Activation of Kras oncogene is virtually a universal event in advanced pancreatic ductal carcinoma but also can be detected as early as in ~40% of PanIN-1A and 1B lesions [7, 15]. Inactivation of tumor-suppressor gene p16 can be frequently detected in PanIN-2. Mutations of p53 and Smad4 occur relatively later in PanIN-3 [13, 16]. Similar but not identical overall genetic profiles were also observed in the development and progression of IPMNs and MCNs [17–20]. Unfortunately, advances achieved in our understanding of pancreatic genetic profile have not altered the survival rates of patients with PDAC. The challenges are that patients are frequently diagnosed with pancreatic cancer at advanced stage with metastasis and most patients are refractory to available chemotherapies. Thus, animal modeling of this disease remains in huge demand for better understanding of the molecular mechanism of pancreatic tumorigenesis, establishment of practical approaches for early detection, and testing novel compounds of chemoprevention and chemotherapy.
In this paper, we summarize three major categories of animal models for human pancreatic cancer: (1) carcinogen-induced; (2) xenograft and allograft; and (3) genetically engineered. We focus more on the genetically engineered mouse models (GEMM) because they better mimic precancerous lesions, advanced human pancreatic ductal cancer, and metastasis at both molecular and histologic levels and possess an immunocompetent tumor microenvironment. These characteristics render the GEMMs a valuable platform for investigations on the cellular origin and molecular pathways of pancreatic cancer development and metastasis. The GEMMs can also serve as an important tool in the development of early detection methods and evaluation of potential therapeutic strategies.
2 Carcinogen-induced animal models of pancreatic cancer
Several carcinogens have been reported to induce a variety of focal proliferative lesions and degenerative changes as well as carcinoma in the pancreas of multiple animal species. Most of those chemical carcinogens are mutagenic at the same time. They usually reach the pancreas through bloodstream after absorption. The administration of carcinogens can initiate preneoplastic lesions such as acinar to ductal metaplasia. Additional genetic mutation is assumed to be required for the further progression of cells from a preneoplastic state to a fully malignant phenotype. It is noted that animal species may contribute to the pancreatic cellular tumor types induced by those carcinogens. For example, development of acinar cell carcinoma is most likely to arise in rats following treatment with carcinogens. In contrast, hamsters develop carcinomas with ductal phenotype after carcinogen administration, while acinar cell carcinomas are extremely rare in this species. Relatively fewer carcinogens have been studied in mice, and both ductal carcinomas [21] and acinar cell carcinomas [22] have been reported.
The most widely used and studied model is Syrian gold hamsters intraperitoneally injected with N-nitrosobis(2-oxopropyl)amine [23–25]. More recent approaches involve the uses of azaserine in rats [26–28] and 7,12-dimerthylbenzanthracene in mice [29]. Table 1 is a summary of major chemicals that have been employed to induce pancreatic carcinoma in various animal species. Some of these models have been shown to resemble human PDAC histologically.
However, the genetic profile of PDAC induced by carcinogens in mice is not yet defined and thus limits their applications in studies involving molecular genetics and signaling pathway analyses. Moreover, the carcinogens often produce adverse effects on tissues other than the pancreas, thus reducing the value of carcinogen-induced mouse models in preclinical trials. However, chemical-induced tumorigenesis can simulate the spontaneous process of human tumorigenesis by inducing cell death or tissue injury, culminating with genetic mutations and the initiation of tumor formation. Thus, the carcinogen-induced animal models continue to serve as valuable tools in assessing the impacts of environmental risk factors, including diet and chemoprevention, on pancreatic tumorigenesis [54–64].
3 Xenograft and allograft pancreatic cancer mouse models
3.1 Xenograft pancreatic cancer mouse models
Implantation of cultured human pancreatic cancer cells or a patient’s tumor mass into mouse pancreas or other tissue sites has been widely used for generations of human pancreatic cancer mouse models, largely due to their comparatively low cost and rapid and predictable tumor growth. Based on the location of the implanted tumor or tumor cells, xenograft mouse models can be divided into two categories: heterotopic xenograft (extra-pancreatic) and orthotopic xenograft (intra-pancreatic). Both are commonly used in cancer research to better understand the genesis of pancreatic cancer and to test novel drug efficacies in vivo but with advantages and limitations in their applications.
Graft rejection is always an issue in immunocompetent mice, thus, immunodeficient mice must be chosen for such approaches. The selection of appropriate types of immunodeficient mice (nude mice, severe combined immunodeficient mice (SCID), NOD/SCID, etc.) for pancreatic cancer xenograft mouse models depends on the experimental requirements. Athymic nude mice (only T cell-deficient) have been widely used for the establishment of orthotopic and heterotopic human pancreatic cancer xenograft mouse models, especially when working with established human pancreatic cancer cell lines [65], because of their low cost and easy breeding. SCID are defective in the immunoglobulin gene and T cell receptor gene rearrangements, and thus lack mature B and T lymphocytes [66]. Therefore, if the preservation of the primary pancreatic tumor heterogeneity is the priority of the xenograft mouse models, more severe combined immunodeficient mice like NOD/SCID (lack of T, B, and NK cells) are better options because there is less immune pressure in these multiple immunodeficient mouse hosts [67]. Other benefits include fewer numbers of tumor cell inoculums and easy tumor formation [68]. The disadvantages for using severe combined immunodeficient mice are their relatively high cost and increased incidence of surgical, anesthetic, and infectious complications.
Through the heterotopic or orthotopic xenograft mouse modeling platform, many promising anti-pancreatic cancer agents, including plant-derived nature agents [69] and novel targeting therapies [70–73], have recently been discovered. More detailed disadvantages and advantages of these two types of xenograft mouse models are discussed below.
3.1.1 Heterotopic xenograft models for pancreatic cancer
Most of heterotopic pancreatic cancer xenograft models are generated by subcutaneously injecting cultured tumor cells into the skin of nude mice, usually along the back of the mice or upper portion of their legs. Nude mice lack not only T lymphocytes but also hair [74]. Therefore, the size and volume of an initiated tumor can be easily monitored by measuring the tumor dimensions in temporal manner in nude mice. The operation is simple and easily manageable. For their ease in applications, subcutaneous pancreatic cancer model is often employed as the first step in validating in vitro research results. For example, a subcutaneous pancreatic xenograft mouse model has recently been used to validate the in vitro synergistic effects of combining a first-line agent for pancreatic cancer, gemcitabine, with a monoclonal antibody TRA-8 to human death receptor 5 expressed on human pancreatic cancer cells [75].
Subcutaneous xenografts can also be accomplished by directly implanting patients’ primary tumor tissues under the skin of nude mice. As little as 1–2 mm3 tumor fragment resected from pancreatic cancer patients is needed for this approach. Direct subcutaneous xenograft is often used to expand a patient tumor mass, to propagate it in vivo, or as an intermediate step prior to establishing it into a cell line in culture. Direct pancreatic cancer xenografts have a number of advantages over cultured cell xenografts. First, the biological features of the xenograft tumors (e.g., histopathology, desmoplastic reaction, tumor heterogeneity) more closely resemble those of the primary tumors than cultured cell lines [76–78]. Secondly, direct xenografts can be used to identify and enrich distinct subpopulations, such as tumor-initiating cells (cancer stem cells), from various solid tumors including pancreatic cancer [79]. Finally, direct pancreatic cancer xenografts may be used to efficiently assess drug efficacy and screen novel therapeutic agents or novel combination of chemotherapies over a broad range of heterogeneous patient tumors [77, 80]. Eventually, this model system could be used as a preliminary step to select appropriate chemotherapies for personalized treatment due to its rapid, affordable, and feasible techniques [81].
It’s important to recognize the limitations of this model system. For example, the alteration of the tumor cell microenvironment can induce changes in the gene expression profiles, which may not reflect the same state of the original tumor. More importantly, subcutaneous xenograft tumors usually exhibit extensive local growth but rarely metastasize and thereby not a feasible model to study metastasis [82]. Furthermore, subcutaneous xenograft models usually do not display the signs and symptoms that may be caused by the consequences of significant tumor burden in the internal organs [83]. These limitations may have contributed to the ineffectiveness of translating treatment success observed in subcutaneous xenograft models to clinical efficacy.
3.1.2 Orthotopic pancreatic cancer xenograft models
Although subcutaneous heterotopic mouse model is relatively rapid, low-cost, and not technically challenging, shortcomings of this type of model have become evident recently, especially in preclinical studies. For instance, drug reagents shown to be highly promising in subcutaneous mouse models often are subsequently demonstrated to have little impacts in human patients. As mentioned previously, subcutaneous xenograft mouse models also rarely develop metastasis [84]. In contrast, in orthotopic xenograft models, in which tumors or tumor cells are either implanted or injected into the equivalent organ from which the tumors originated, frequent metastases are observed. Up to 60% of orthotopic xenografted pancreatic tumors can disseminate to other organ sites [85]. The tumor microenvironments of orthotopic xenograft models are also more comparable to those in humans and therefore rendering the models more relevant in predicting clinical outcomes in humans. Because of their increased clinical relevance, orthotopic xenograft models have emerged as a preferred tool for pancreatic cancer researchers over subcutaneous mouse models, or as a necessary second step to further validate results established in subcutaneous xenograft mouse models [80].
Although orthotopic mouse models offer numerous advantages, the generation of orthotopic pancreatic cancer mouse models is labor-intensive, expensive, and technically challenging. Tumor burden is also challenging to measure and monitor in orthotopic mouse models, which can complicate the assessment of treatment responses. This difficulty can be lessened but not entirely overcome by incorporating in vivo imaging methods. In addition, orthotopic implantation of tumor cells or mass into an organ such as the pancreas would cause remarkable injury to the host animals, which require significant time for post-operative recovery. Although an ultrasound-guided method of injecting tumor cells into the pancreas has recently been established for the orthotopic pancreatic cancer mouse model in order to minimize the surgical wound of the recipient animals, it also raises the technical difficulties and expenses of utilizing this model [86]. The size and volume of implanted tumors can be dynamically measured by ultrasound examination during a treatment test trial in orthotopic pancreatic cancer mouse models [87]. Magnetic resonance imaginer (MRI) has also been employed to monitor tumor growth and metastasis in orthotopic pancreatic tumor mouse models [88]. However, using MRI for long-term follow-up in preclinical studies, especially with a large number of mice, is extremely expensive and time-consuming (it takes about 1 h to scan one mouse).
When only cultured tumor cells are used for orthotopic implantation, labeling tumor cells prior to the implantation provides an alternative method to visualize and track tumor growth in vivo. A number of approaches have been reported to label tumor cells for in vivo imaging. High signal strength, specificity, resolution, and physiological conditions are all important considerations in developing a labeling method to report tumor progression and metastasis on a real-time basis. The green fluorescent protein (GFP) gene is selected based on these criteria and because its applicability as a cellular marker has been previously demonstrated [89–91]. A major advantage of the GFP labeling approach is that imaging GFP-expressing tumor cells requires no preparative procedures, contrast agents/substrates injection, anesthesia administration, or light-tight box as other imaging techniques do [92, 93]. Bouvet et al. have reported in vivo monitoring of GFP-expressing pancreatic cancer orthotopically implanted in nude mice [94, 95]. They have also described monitoring a highly metastatic model of pancreatic cancer that utilizes red fluorescent protein (RFP)-expressing pancreatic cancer cells [96–100]. These RFP-expressing pancreatic tumors have also been implanted into the pancreas of transgenic GFP-expressing nude mice to create dual-color models to study tumor–host interactions [101–103].
Another common approach involves the incorporation of the luciferase gene into tumor cells [104]. When a pancreatic cancer cell line is stably labeled with a luciferase reporter gene, the tumor burden including metastasis in an orthotopic pancreatic mouse model could be monitored by utilizing bioluminescence imaging systems such as the IVIS instrument (Xenogen Corp) [105]. In a drug testing trial, tumor growth can be dynamically assessed, and the tumor burden of the control and treatment mice can be compared by measuring the bioluminescence signals of the tumor cells. Figure 1 provides an example of using luciferase imaging to monitor tumor growth in a preclinical investigation in our laboratory.
Representative examples of tumor growth and tumor burden dynamically being monitored and compared by measuring the bioluminescent signals. a The growth of pancreatic tumor mass in a control mouse was precisely recorded at different time points; b the tumor burden in the control panel was relatively bigger than that in the treatment group at 4 weeks after orthotopic implantation
3.2 Allograft pancreatic cancer mouse models
In the xenograft modeling, human tumors or cell lines are implanted either subcutaneously or orthotopically into the mice. In these models, the host animals have to be immunocompromised (nude or SCID mice) to avoid graft rejection, and therefore, the models do not necessarily recapitulate the original human tumor microenvironment. It is well accepted now that host immune cells in the tumor microenvironment play critical roles in tumor progression and metastasis. Therefore, an orthotopic mouse model with an intact immune system would be much more desirable than an immunocompromised one. Because it is possible to perform allograft using syngeneic hosts, implanting murine pancreatic cancer cells in a syngeneic immunocompetent host to generate an orthotopic pancreatic mouse model is a logical progression in the field. Recently, several GEMM have been reported to mimic human pancreatic tumorigenesis at both molecular and histologic levels [106–108]. Not only are these GEMMs excellent tools to the field of pancreatic cancer research (which will be discussed below), but cancer cell lines derived from the invasive tumors developed in the GEMMs are also good resources for generating immunocompetent orthotopic pancreatic mouse models [109–112]. In our laboratory, hundreds of primary pancreatic ductal adenocarcinoma cell lines derived from mouse models with engineered mutant Kras G12D activation and p16 deletion have been established recently [113]. In our experiences, these tumor cell lines grow extremely aggressively upon implantation as manifested by progressive growth in the pancreas, peritoneal dissemination, and distant metastases to multiple organs including the liver and lungs. These clonal tumor cell lines, originated from 11 distinct individual genetic mutant mice with pancreatic ductal adenocarcinomas and two metastases, are useful resources for future investigations on the molecular mechanisms for pancreatic tumorigenesis, in vitro screening of novel chemotherapeutical compounds, and the generation of syngeneic heterotopic or orthotopic mouse models. Allograft mouse models are the closest model system to GEMMs because of their intact tumor microenvironment. They hold several advantages over GEMMs in terms of their lower costs, faster tumor growth, and the ease to incorporate tumor cell labeling for in vivo imaging. Therefore, immunocompetent allograft mouse models may have great potential and may play a greater role in the future research [114].
4 Genetically engineered mouse models for pancreatic cancer
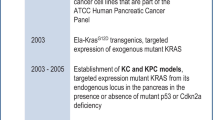
GEMM are the most sophisticated in their designs among the three categories. Common strategies include transgenic, conventional, and conditional gene knock-in and knock-out. In transgenic mouse models, target genes are randomly incorporated into the host mouse genome with uncertain number of gene copies. They are most likely to be ectopically overexpressed simply due to multiple copies of gene insertion. The expression pattern of a target gene can be restricted to particular tissues or cell lineages by placing the target genes under the control of a tissue/cell-specific promoter. In designing pancreas-specific mouse models, elastase (Ela), metallothionein-1, cytokeratin 19 (CK19), Pdx1, p48/Ptf1a, Mist1, and nestin have all been employed to restrict target gene expression to the pancreas (Fig. 2).
Schematics of pancreatic cell-lineage biomarkers that have been used or could be applied in the generation of genetically-modified mouse models-Elastase (Ela), metallothionein-1, cytokeratin 19 (CK19), Pdx1, p48/Ptf1a, Mist1, and nestin have all been employed to restrict target gene expression to the pancreas
The availability of these lineage-specific promoters is a crucial rate-limiting step for robust expressions of transgenes in the pancreas of these GEMMs. Because the majority of human pancreatic cancers are classified as PDAC, promoters that drive gene expressions specifically in pancreatic ductal epithelial or exocrine cells are most desirable when designing GEMM for pancreatic cancer. High levels of transgene expression in the acini can be accomplished by using the elastase promoter. Several other exocrine-specific promoters, including Mist1 and Nestin, are also available for targeting this compartment. Unfortunately, most promoters whose activities are restricted to the ductal epithelial cells in the pancreas often are also active in the epithelial cells of other organs. For example, cytokeratin 19 exhibits high expressions not only in the pancreatic ducts but also in the lung, bladder, and other epithelia [115]. Transgene expression driven by metallothionein-1 gene promoter is expressed not only in the pancreas but also in the mammary glands and liver [116]. A recent report showed that the keratin 7 promoter is more selective than the CK19 promoter in targeting pancreatic ductal cells [117]. However, CK7 is also expressed at low or undetectable levels in gastrointestinal epithelial cells, and its feasibility in pancreatic cancer modeling remains to be seen. Pdx1 is expressed in early embryonic stage of gastrulation, in a region that can give rise to both the duodenum and the pancreas in later stage [118]. Pdx1 is expressed as early as embryonic day 8.5 and therefore a biomarker for pancreatic progenitor cells. Pdx1+ progenitors contribute to adult ductal epithelial cells as well as acinar and endocrine cells, whereas Pdx1 promoter activity in the adult pancreas is largely confined to the islet cells.
Transgene expression can be further controlled temporally by Tet-on or Tet-off inducible expression control. Other inducible models include the uses of tamoxifen–ERTM and Cre–loxP systems. These inducible systems offer an additional regulation in restricting the transgene expression pattern or length of its expression in the pancreas when combined with tissue-specific promoters. Examples of their applications will be further discussed later in greater detail.
4.1 Transgenic mouse models for pancreatic cancer
The pathogenesis of PDAC remains incompletely defined, including its cell origin. Histological and molecular evidence support that human PDAC progress from PanIN lesions, which are thought to initiate in the small ducts of the pancreas [1, 4, 14]. Although morphological and molecular signatures associated with PanINs and PDA suggest that duct cells are responsible for these lesions, it remains unknown if other pancreatic cell types (acinar, islet, or stem cells) might also contribute to the pathogenesis of this disease. Recent evidence suggests that acinar cells could be the source of some ductal neoplasms through a process of acinar-to-ductal metaplasia [119]. Acinar-to-ductal metaplasia has been found associated with both human and mouse PanINs [119, 120]. Acinar cells have also been shown to directly transdifferentiate into duct-like cells in the presence of TGF-α [121]. Furthermore, targeted expression of Kras G12V to cells of the ductal compartment failed to produce mPanINs or PDA in the K19-Kras G12V mouse model [115, 122]. Together, these studies suggest that PanIN initiation and progression may involve cells from the acini compartment.
However, targeting the acinar cells alone would not lead to the development of PanIN or PDAC. Overexpressing oncogenes under control of acinar cell-specific elastase gene promoter, mice carrying the elastase promoter-SV40-T antigen (Ela-SV40-TAg), elastase-polyoma virus middle T antigen (Ela-PyMT), or elastase-H-ras (Ela-Hras) transgene [123–125] mainly developed acinar cell carcinomas at age of 4 to 8 months. More than half of the tumors ranged from well-differentiated acinar cell carcinoma to anaplastic carcinoma including moderately or poorly differentiated acinar cell carcinomas. Transgenic mice overexpressing oncogenic c-Myc controlled by the elastase gene promoter not only developed acinar cell carcinomas but also mixed neoplasms that exhibited both acinar-like neoplastic cells and duct-like neoplastic cells [126]. Acinar cell carcinoma of the pancreas occurred at 100% penetrance in those mice at 2 to 7 months of age. About half of the acinar cell tumors are mixed with regions of ductal differentiation associated with desmoplasia. Liver metastasis was reported in about 20% of the Ela-Myc transgenic mice by Liao et al. [127]. This is likely the first single-transgene mouse model for pancreatic cancer that produced liver metastasis. Such Myc-induced acinar-to-ductal metaplasia and focal acinar cell carcinoma were also observed in Ela-Myc transgenic rats [128].
Activating mutation of the KRAS oncogene is the most frequent and perhaps the earliest genetic alteration associated with pancreatic cancer [7, 15]. Naturally, transgenic mouse lines overexpressing mutant Kras have been generated in attempt to recapitulate human pancreatic tumorigenesis. Similar to those observed in Ela-SV40-TAg, Ela-PyMT, and Ela-Hras mice, transgenic mice carrying a mutant Kras G12D transgene driven by the elastase promoter displayed perinatal pancreatic acinar cell hyperplasia and dysplasia or preinvasive pancreatic neoplastic lesions like early mPanINs without adenocarcinoma formation [129]. Transgenic mice expressing the mutant Kras G12V allele in the pancreatic CK19+ compartment disappointingly exhibited even milder phenotypes characterized by lymphocytic infiltration surrounding the pancreatic ducts [115]. However, CK19-Kras G12V transgenic mice displayed mucous neck cell hyperplasia, a precursor lesion of gastric adenocarcinoma. The distinct phenotypes again may suggest that the development of PDAC requires the involvement of multiple cell lineages in the pancreas and acinar cells or acinar–ductal metaplasia is an essential piece of the process.
Hedgehog signaling, an essential pathway during embryonic pancreatic development, has been dysregulated in several cancer types including human PDAC [130]. Sonic hedgehog (Shh), a secreted hedgehog ligand, is abnormally expressed in PanINs as well as PDAC [131]. Overexpression of Shh in the Pdx-1+ compartment of the pancreas (Pdx1-Shh transgenic mice) led to the development of abnormal tubular complexes and PanIN-1 and PanIN-2, suggesting that the dysregulation of this pathway is an early and critical event in pancreatic tumorigenesis [131]. A transgenic mouse line expressing a dominant active form of the GLI2 transcription factor (CLEG2 transgene), a downstream mediator of the hedgehog signaling pathway that can be conditionally activated by Cre-mediated recombination, was also generated. Pancreatic tissue-specific activation of the transgene was achieved by crossing CAG-LSL-CLEG2 transgenic animals with Pdx1-Cre mice. The Pdx1-Cre; CLEG2 mice survived into adulthood without impaired exocrine or endocrine function, and 30% of these animals developed undifferentiated pancreatic tumors that are not commonly found in human patients [132]. Triple-transgenic Pdx1-Cre; CLEG2; LSL-Kras G12D mice exhibited extensive preneoplastic lesions, accelerated onset of tumor formation, and shortened survival in comparison to Pdx1-Cre; LSL-Kras G12D mice [132]. Together, these data support that activated hedgehog signaling favors pancreatic carcinogenesis and may play a role in early tumorigenesis.
Other than oncogenes and their pathways, growth factors are often selectively overexpressed in transgenic mouse modeling for pancreatic cancer because they have also been implicated in early pancreatic carcinogenesis. For example, elevated transforming growth factor-α (TGF-α) is consistently associated with pathological process of neoplastic transformation, and therefore transgenic mice carrying overexpression of TGF-α under the control of the metallothionein promoter (MT-TGFα) or the elastase promoter (EL-TGFα) in the pancreas were generated to investigate its potential role in pancreatic tumorigenesis [116, 133, 134]. MT-TGFα transgenic mice develop histopathological changes in multiple tissues including the breast, liver, the coagulation gland, and pancreas [135, 136]. Expectedly, pathogenesis of EL-TGF-α transgenic mice was restricted to the pancreas. Both models have similar histopathological characteristics in the pancreas—severe stromal fibrosis, tubular complex, acinar hyperplasia, and the absence of carcinoma formation. However, Liao et al. have reported that female MT100 line of MT-TGF-α transgenic mice developed ductal adenocarcinoma, albeit at low frequency [127], suggesting that gender and genetic background might influence the phenotypic outcomes in this model.
Chronic pancreatitis is a known risk factor for pancreatic adenocarcinoma [137]. Interleukin-1β (IL-1β) is a proinflammatory cytokine involved in pancreatic inflammation [138]. Expression of human IL-1β in the pancreas under the rat elastase promoter (Ela-IL-1β) led to chronic pancreatitis-associated histologic and molecular changes in mice. Breeding the Ela-IL-1β transgenic mice into p53 R172H/+ background increased the formation of precancerous lesions characterized by tubular complexes and acinar–ductal metaplasia [139]. Cyclooxygenase-2 (Cox-2), which is a key enzyme of prostaglandin biosynthesis, is also overexpressed in human pancreatic cancer [140]. Transgenic mice carrying murine keratin 5-promoter-driven expression of human Cox-2 gene developed IPMN-like lesions and serous cystadenomas. This phenotype can be reduced by feeding a Cox-2-selective inhibitor to the transgenic mice [141]. Skin phenotypes were also observed in these mice because keratin 5 promoter is also active in the skin [142]. In another similar transgenic mouse line, in which the mouse Cox-2 gene was expressed under the control of bovine keratin 5 promoter, chronic pancreatitis-like histopathological changes characterized by acinar-to-ductal metaplasia and a well-vascularized fibroinflammatory stroma were observed in the pancreas. Increased proliferation, cellular atypia, and loss of normal tissue architecture are typical features in the pancreases of these transgenic mice. The development of cancer was limited to local invasion with no metastasis. The abnormal pancreatic phenotype can also be completely prevented by maintaining mice on a diet containing celecoxib, a well-characterized Cox-2 inhibitor [143]. The presence of cholecystokinin (CCK)-B/gastrin receptors has been identified in the pancreas of higher mammals including humans [144], but their physiological function in the pancreas is unknown. A transgenic mouse strain expressing the human CCK-B/gastrin receptor in the pancreatic acinar cellular compartment (Ela-CCKB) displayed no pancreatic phenotype [145]. However, this transgenic model is sensitized to carcinogen azaserine-induced pancreatic neoplasia development, suggesting that activation of CCK-B receptor and azaserine result in cumulative effects to favor the emergence of a risk situation that is a potential site for carcinogenesis initiation [146].
TGF-β signaling pathway is commonly believed to play an important role in the development of pancreatic cancer because several mediators of its pathway are proven players in pancreatic tumorigenesis [12, 14, 130, 147]. Samd7 is generally considered as a specific inhibitor of TGF-β signaling. A transgenic mouse model with exogenous expression of Smad7 controlled by the elastase promoter mostly developed acinar to ductal metaplasia and some lesions similar to mPanIN at 6 months of age. This model demonstrated that in vivo inactivation of TGF-β signaling is implicated in the development of early stage of pancreatic cancers [148]. Since TGF-β signaling is known to play dual roles in oncogenesis, this Ela-Smad7 transgenic line can be valuable in distinguishing the biological roles of other mediators of the TGF-β signaling pathway in pancreatic carcinogenesis by crossbreeding to conditional Smad4 fl/fl knockout and/or Kras G12D mutant mouse models [106, 149].
4.2 Combination of transgenic mice and additional genetic alterations for accelerated development of invasive and metastatic pancreatic cancers
Most single-transgene mouse models do not histologically recapitulate the entire process of human pancreatic cancer progression, specifically from the initiation of PanINs to their progression to well-differentiated ductal adenocarcinoma. Transgenic expression of one single oncogene (TGF-α, c-Myc, Kras, etc.) is usually sufficient to evoke the formation of early preneoplastic lesions characterized as acinar to ductal metaplasia, mPanIN, or IPMN (Table 2), but their progression to invasive cancer requires a long latency if at all. Thus, it’s only desirable and logical to introduce additional genetic modifications, such as inactivation of tumor-suppressor genes such as p53, p16, and Smad4, into these transgenic mouse models to facilitate the progression to invasive and metastatic pancreatic cancer (Table 3). The generation of compound mutant mouse strains allows the evaluation of the relative roles of the target genes and their synergistic or compromised effects in tumor initiation and progression. Additionally, the multiple genetic mutant strains also provide good resources for dissecting the cross-talk of the molecular signal transduction pathways associated with these target genes.
To investigate the synergistic effects of cytokine TGF-α and oncogenes (viral oncogene SV40- Tag or cellular oncogene c-Myc) on tumor development in the pancreas, MT-TGF-α or Ela-TGF-α transgenic mice [133] were bred to Ela-SV40-Tag [123] or Ela-Myc transgenic mice [126] to generate double transgenic mice co-expressing TGF-α and SV40-TAg or TGF-α and c-Myc oncogenic proteins in the pancreatic acinar compartment. The results showed that TGF-α dramatically accelerated the growth of tumors initiated by either oncogene alone. Co-expression of TGF-α and SV40-TAg accelerated the formation of preneoplastic foci. Co-expression of TGF-α and c-Myc also enhanced tumor growth in situ and produced transplantable acinar cell carcinomas. Observed lesions are mostly restricted to the acinar cell compartment, although various ductal lesion, cysts, and adenocarcinomas in these double transgenic mice were reported by Liao et al. [127]. These findings demonstrate the importance of TGF-α expression during pancreatic multistage carcinogenesis [163]. Pancreatic tumor development in the EL-TGF-α transgenic mice can also be enhanced in a germline background of p53 insufficiency (Ela-TGF-α; p53 +/− or Ela-TGF-α;p53 −/−). These mice developed invasive pancreatic cancers, which expressed ductal epithelial biomarker cytokeratin 19 and increased the expression of Pdx1 [157, 158, 166]. Concomitants with partial or complete loss of p16 or Smad4 were detected in the tumors developed from the Ela-TGF-α;p53 +/− mice, probably due to increased genomic instability exhibited in these tumors [158, 167]. However, incorporation of inactivated tumor-suppressor genes does not always result in tumor promotion. Ela-TGF-α transgenic mice in conjunction of p16/p19 or p53 heterozygous deletion dramatically increased the incidence of serous cystadenomas, a benign form of pancreatic tumor that rarely progress to invasive state [159]. The inconsistencies regarding p53 reported by the two groups may be attributed to different mouse strains examined or the genetic status of p16 [157, 159]. Further investigations into the involvement of p16 would be desirable in bridging the discrepancy. Concomitant expression of TGF-α and mutant Kras G12D in Ela-TGF-α;p48 Cre/+; LSL-Kras G12D mice chiefly leads to the development of pancreatic IPMNs and significantly accelerates the progression from mPanIN to metastatic pancreatic cancer. Tissue microarray analyses showed that the protein profiles of the mouse IPMN are similar to human pancreatobiliary IPMNs. These data support that EGF signaling cooperates with oncogenic Kras to drive the initiation of IPMN and progression of pancreatic cancer [168].
A novel mouse model for pancreatic cancer targeting adult acinar cells was established through the somatic delivery of oncogene-bearing avian retroviruses to mice that express Tva, the receptor for avian leukosis sarcoma virus subgroup A, under the control of the elastase promoter [164]. Mice bearing the Ela-Tva transgene in combination with pancreatic-specific p53 knockout (p48 Cre/+;p53 fl/fl) resulted in a progressive and metastatic pancreatic cancer mouse model after the somatic and sporadic delivery of avian retroviruses encoding the mouse polyoma virus middle T antigen (RACS-PyMT) [165]. In this pancreatic metastasis model, the tumors metastasize most frequently to the liver, consistent with human pancreatic carcinomas. Further analysis of metastatic lesions demonstrated that concomitant loss of the p16 Ink4a/p19 Arf locus was not required for the metastasis. Delivery of RCAS-PyMT or RCAS-c-Myc vectors to the Ela-Tva;p16 −/−/p19 −/− mice induced the formation of pancreatic tumors. RCAS-PyMT-induced pancreatic tumors displayed histological features of acinar or ductal carcinomas, while RCAS-c-Myc induced endocrine tumors exclusively, indicating specific oncogenes can prompt the formation of particular pancreatic tumor types from one or more multipotential progenitor origins in a single transgenic line [125].
TGF-β signaling pathways are critically involved in human carcinogenesis including pancreatic cancer [12, 147, 169]. The roles of TGF-β signaling pathway in the development of PDAC have been intensively investigated through several thorough in vivo characterizations of relevant GEMMs [149, 160, 170–172]. Most of the research showed that the disruption of TGF-β signaling synergizes with mutant Kras in driving pancreatic tumorigenesis. However, when Elastase-Kras G12D mice were crossed with conventional Tgfbr1 (TGF-β receptor type 1) haploinsufficient mice to generate Ela-Kras G12D; Tgfbr1 +/− mice, phenotypic analyses showed that only 50% of Ela-Kras G12D; Tgfbr1 +/− mice developed preinvasive lesions compared with 100% of Ela-Kras G12D mice with wild-type Tgfbr1 genotype. The results suggest that inhibition of TGF-β signaling promotes the development of precancerous lesions in mice but the inhibition of Tgfbr1 expression may lead to a decreased risk of pancreatic cancer [160]. These contradicted observations may be attributed to the dual roles of TGF-β signaling in tumorigenesis [173].
The tumor microenvironment is known to be critical for tumor progression and invasion. Increased pancreatic fat in human pancreatic tumorigenesis is found to be associated with tumor invasion and metastasis [174]. Pigment epithelium-derived factor (PEDF) has been recently implicated in metabolism and adipogenesis [175]. PEDF deficiency in mice promotes pancreatic hyperplasia and visceral obesity. Mice with combined Ela-Kras G12D transgene and PEDF deficiency (Ela-Kras G12D; PEDF −/−) developed invasive pancreatic ductal carcinoma associated with increased peripancreatic fat with adipocyte hypertrophy and intrapancreatic adipocyte infiltration (pancreatic steatosis). These data highlight the importance of lipid metabolism in the pancreatic tumor development [161]. Desmoplasia is one of histopathological hallmarks of human pancreatic cancer and a visual reminder of the dynamic interactions between tumor and its microenvironment. Desmoplasia has been shown recently to limit delivery of chemotherapy in vivo [176]. The proteinase membrane type 1-matrix metalloproteinase (MT1-MMP) is believed to be required for tumor growth and invasion in the collagen-rich microenvironment. Krantz et al. crossed TRE-MT1-MMP transgenic mice, in which MT1-MMP expression is under the control of seven tet-responsive elements (TRE) upstream of a minimal CMV promoter [129, 177], with Ela-tTA mice [129] to generate Ela-tTA/TRE-MT1-MMP double transgenic mice. In Ela-tTA mice, the transactivator tTA is expressed downstream of elastase promoter, thus enabling targeting of MT1-MMP to pancreatic acinar cells. The double transgenic mice were further crossed to Ela-Kras G12D mice [177]. The results show that mice expressing both MT1-MMP and Kras G12D (Ela-Kras G12D;MT1-MMP) developed a greater number of large, dysplastic mucin-containing papillary lesions than littermate control mice (Ela-Kras G12D alone ). The data support that the collagenase MT1-MMP contributes to fibrosis in pancreas which may favor pancreatic tumorigenesis [162].
These compound mouse models demonstrated that targeting viral or cellular oncogenes like SV40-TAg, PyMT, c-Myc, and Kras in the pancreatic compartments may be sufficient to induce preneoplastic lesions such as acinar to ductal metaplasia and acinar hyperplasia, suggesting these genes play important roles in the initiation of pancreatic tumor. Those precursor lesions could be focally transformed into duct-like neoplastic lesions but may take a long latency. Combination with distinct genetically modified mouse models can accelerate the progression from the precancerous lesions to invasive disease and reduce the time of onset. More importantly, interactions between various cancer gene signaling pathways which are critically associated with invasive pancreatic cancer could be explored through the investigation of various combinations of these transgenic mouse models.
Traditional transgenic mice are relatively faster to generate and easy to crossbreed and can express human genes. However, the weaknesses of transgenic mouse modeling include ectopically overexpressing target genes under foreign promoters at non-physiological levels, multiple copies of an insertion, and random genomic loci of a gene insertion, which could lead to inconsistent phenotypes among the different transgenic mouse lines from the same transgenic construct. Due to these reasons, conditional gene knock-in or knock-out mouse models have become the preferred targeting strategies over the traditional transgenic animal modeling approach in the recent years for modeling pancreatic cancer.
4.3 Conventional and conditional gene knock-in animal models for pancreatic cancer
Transgenic animal models ectopically expressing oncogenes do not always accurately depict the in vivo functions of the oncogenes during tumorigenesis because they are not expressed at the physiological levels. Unpredictable positional effects can also influence the expression levels of the oncogenes in transgenic mice. Gene knock-in model strategy on the other hand can avoid these potential pitfalls by controlling both the gene copy number and the site of the insertion. Thus, knocking in a mutant oncogenic allele by homologous recombination to its native locus would more faithfully reflect the natural processes of oncogenesis in humans. This is particularly important when targeting mutant Kras in pancreatic tissue, because the effects of mutant Kras in pancreatic tumorigenesis appear to be dependent on both its cellular context and expression levels [113, 115, 122, 129, 178–180] .
Oncogenic point mutation of Kras is a frequent genetic alteration found in premalignant stages of PDAC [7, 15]. Several approaches have been reported to knock-in Kras mutant allele in vivo. One classic gene knock-in approach is homologous recombined the mutant Kras G12D cDNA to Mist1 locus. Mist1 protein is restricted to mature pancreatic acinar cells with no measurable expression in mature ductal or islet cells [181]. Mist1 −/− mice develop progressive acinar dysplasia and pancreatic fibrosis, whereas Mist1 +/− mice have no discernible phenotype [182]. Therefore, haploinsufficiency of Mist1 in the conventional Mist1 KrasG12D/+ knock-in mice did not result in developmental defects. However, Mist1 KrasG12D/+ knock-in mice experienced reduced overall survival, developed acinar–ductal metaplasia, and metastatic exocrine pancreatic carcinoma [183]. These data are in contrast to previously described mutant mice that ectopically expressed the Kras oncogene in either acinar or ductal compartments [115, 122, 129]. Interestingly, many of the Mist1 KrasG12D/+ mice also developed hepatocellular carcinoma. The p53 +/− haploinsufficiency can cooperate with this conventional knock-in Mist1 KrasG12D/+ allele to accelerate lethality and promote advanced and metastatic pancreatic adenocarcinoma [183]. Crossing Mist1 KrasG12D/+ mice to Mist1 LacZ/LacZ mice to generate the Mist1 KrasG12D/LacZ genotype would inadvertently result in the biallelic inactivation of the Mist1 gene. Mist1 KrasG12D/LacZ mice lost Mist1 expression but gained mutant Kras G12D expression under the endogenous Mist promoter. These Mist1 KrasG12D/LacZ mice exhibited accelerated mPanIN development and severe exocrine pancreatic defects that could be rescued by ectopic expression of Mist1 in acinar cells [184].
Guerra et al. created a distinct conditional LSL-Kras G12V knock-in mouse line by homologous recombining a mutant Kras (loxp-stop-loxp-Kras G12V-IRES-β-geo) allele into the native Kras locus under the control of the endogenous Kras promoter in mouse embryonic stem cells [179]. Expression of this conditional oncogenic allele requires removal of the floxed STOP transcriptional cassette by Cre recombinase. The effectiveness of the floxed stop elements have previously been demonstrated in suppressing transcriptions of other transgenes and reporter genes [185, 186] and in a similar Kras mutant knock-in model [106]. The expression of the Kras G12V oncoprotein can be monitored by the co-expression of β-galactosidase. Selective expression of the Kras G12V oncogene in acinar/centroacinar lineage by turning on the elastase-tTA/tetO-Cre during embryogenesis resulted in the formation of mPanINs and invasive PDAC. However, if the elastase promoter controlled Cre recombinase expression is not turned on until adulthood, these mice are refractory to Kras G12V-induced PanINs and PDAC development. Adult mice expressing Kras G12V throughout the body failed to induce proliferative phenotype or other growth abnormalities for up to 8 months. Chronic pancreatitis appears to be essential for the induction of PanINs and invasive PDAC in addition to the activation of the mutant Kras G12V allele in adult mice [177].
Hingorani et al. has also generated a Lox–Stop–Lox Kras conditional knock-in mouse strain with a strong gain of function mutation Kras G12D, which is the most commonly identified mutation in human PDAC (LSL-Kras G12D mice) [106, 187]. The expression of oncogenic KrasG12D protein at physiological level in murine pancreases, activated by crossing to either the Pdx1-Cre transgenic or p48 Cre/+ knock-in mouse line, is sufficient to initiate the development of precancerous lesions that recapitulate the full spectrum of human PanINs. Although at low frequency, these mPanINs in the Pdx1-Cre; LSL-Kras G12D mice can progress spontaneously to invasive and metastatic adenocarcinomas [106]. Korc et al. have demonstrated that activation of this oncogenic Kras G12D mutant allele in nestin-expressing cells also results in mouse PanIN formation in Nestin-Cre; Kras G12D mice [188]. Nestin is a marker of progenitor cells, and nestin-positive progenitors contribute to the formation of differentiated acinar cells [189]. Furthermore, nestin can be re-expressed in acinar cells upon “de-differentiation” during epithelial injury and regeneration [190]. Thus, activation of oncogenic Kras in the nestin-expressing lineage might be equivalent to targeting oncogenic Kras to progenitor and mature acinar cells.
The expression of the activated Kras mutant in these conditional Kras G12V and Kras G12D mouse lines can be further regulated in a temporal manner by using inducible Cre expression systems. There are three tamoxifen-inducible Cre mouse strains that can be used to study temporal activation of mutant Kras G12D in adult pancreas: Ela-CreERT2, Pdx1-CreERT2, and Mist1 CreERT2/+. The Ela-CreERT2 and Pdx1-CreERT2 strains harbor transgenic CreERT2 alleles, while the Mist1 CreERT2/+ mice contain a CreERT2 knock-in at the Mist1 locus. Habbe et al. have crossed these three inducible Cre lines with the LSL-Kras G12D mice to investigate the cell(s)-of-origin from which mPanIN lesions arise in Pdx1-Cre ; LSL-Kras G12D mice [106, 191]. In that study, both tamoxifen-induced Ela-CreERT2 and Mist1 CreERT2/+ targeted Kras G12D activation to the mature acinar cell compartment, while tamoxifen-induced Pdx1-CreERT2 restricted Kras G12D activation to Pdx1-expressing cells, predominantly islet β cells within the adult pancreas. The spontaneous development of mPanIN lesions of all histological grades was observed in the pancreases of adult mice with acinar-restricted Kras G12D expression (in tamoxifen-treated Ela-CreERT2; LSL-Kras G12D and Mist1 CreERT2/+; LSL-Kras G12D mice). Contrary to a previous report, concomitant exocrine injury was not required in inducing the preneoplastic lesions in these mice [177, 191]. Furthermore, no lesions were observed in the pancreases of the tamoxifen-treated Pdx1-CreERT2; LSL-Kras G12D population [191]. Acinar–ductal metaplasia areas were observed within the immediate vicinity of mPanIN lesions, with progressive transition from normal acinar parenchyma to metaplastic structures to mPanINs, in Ela-CreERT2; LSL-Kras G12D mice [191]. These findings provide informative insights to the cellular initiation of PDAC and suggest that acinar compartment might be the proximate source of mPanIN lesions. The possibility of acinar cell derivation of mPanIN lesions is also supported by Zhu et al., who also demonstrated the extensive acinar–ductal metaplasia preceding the onset of mPanIN lesions and the existence of “biphenotypic” cells expressing markers of acinar and ductal differentiation within the metaplastic ducts and mPanIN lesions in young p48 Cre/+; LSL-Kras G12D mice [120].
A number of GEMMs involving both mutant Kras knock-in allele and Cre mouse strain are listed in Table 4. The aforementioned conditional LSL-Kras G12D knock-in mouse is one of the most popularly utilized line for modeling human pancreatic carcinogenesis so far [106]. This model is preferred for several reasons: (1) The Kras G12D mutant allele is expressed under the control of its endogenous Kras promoter, which allows its expression at the native physiological level, mimicking the expression level of oncogenic KRAS in human tumorigenesis. (2) The LSL-Kras G12D knock-in mouse strain can be easily combined with assorted promoter controlled Cre transgenic or knock-in mouse lines to generate various tissue- or cell-specific Kras mutant mouse models. This strategy has been widely used for pancreatic cancer as well as in other cancer types [183, 192–195]. (3) The LSL-Kras G12D model is readily available through the NCI Mouse Repository for academic research. The prevalent use of LSL-Kras G12D over LSL-Kras G12V-IRES-β-geo model is more likely associated with the general accessibility of the LSL-Kras G12D model than scientific rationale or consideration. Both LSL-Kras G12D and LSL-Kras G12V-IRES-β-geo models when activated by Cre recombinase in the pancreases can develop mPanINs and PDAC spontaneously [122]. It is worth pointing out that extra-pancreatic phenotypes are frequently observed in the Pdx1-Cre; LSL-Kras G12D mice, mostly presenting as papilloma at the conjunction areas between skin and anal, mouth, or eye mucus. Lung adenoma was also frequently noted in this Pdx1-Cre-mediated mutant Kras G12D model [113].
4.4 Combination of mutant Kras-driven oncogenesis and conditional inactivation of tumor-suppressor genes for invasive and metastatic pancreatic cancer mouse models
It is globally accepted that Kras mutation is sufficient to initiate pancreatic tumorigenesis. And the tumor malignant transformation and further progression to invasive and metastatic carcinoma require additional mutations of tumor-suppressor genes like p16, p53, and Smad4. These tumor-suppressor genes can be tissue-specifically inactivated in the pancreas by crossing the floxed target gene mouse lines to pancreatic-specific Cre-expressing mouse strains. Biallelic inactivation of a single tumor-suppressor gene in the pancreas is insufficient to induce pancreatic malignancy in most cases (Table 5). Oncogenic activation seems to play a key role especially in initiating pancreatic tumorigenesis. The combination of both oncogenic activation and tumor-suppressor inactivation appears to be most effective in generating invasive and metastatic pancreatic malignancy with short latency (Table 6).
In humans, inactivation of the tumor-suppressor gene p16 INK4A and oncogenic activation of KRAS occur in almost all pancreatic cancers [4, 8, 9, 14]. In mice, the sole inactivation of p16 Ink4a/p19 Arf failed to produce any preneoplastic or neoplastic lesions in the pancreases of mice with genotype Pdx1-Cre;p16/p19 fl/fl. Mice with both activated Kras G12D expression and p16 Ink4a/p19 Arf deficiency developed mPanIN at an early age, and these neoplasms progressed rapidly to highly invasive and metastatic cancers [211]. However, the deletion of the p16/p19 fl/fl allele inactivates both p16 and p19 tumor-suppressor genes simultaneously. To understand the importance of p16 in pancreatic tumorigenesis, we have generated a conditional p16 knockout mouse line (p16 fl/fl), in which p16 can selectively disrupted in a tissue-specific manner without affecting p19 expression. We have reported that p16 fl/fl; LSL-Kras G12D; Pdx1-Cre compound mutant mice can develop the full spectrum of mPanIN lesions, PDAC, and frequent metastases [113]. Using conventional p16 deletion mouse line [220], similar histological and gross phenotypes were observed in p16 −/−; LSL-Kras G12D; Pdx1-Cre mice as in p16 fl/fl; LSL-Kras G12D; Pdx1-Cre mice with slightly shortened survival [113, 204]. Interestingly, mutant Kras G12D in the context of p16 Ink4a or p16 Ink4a/p19 Arf inactivation in the presence of wild-type or heterozygous p53 deletion produced PDAC with longer latency and greater propensity for distant metastases relative to mice with homozygous deletion of p53 or p16 Ink4a/p19 Arf [113, 204]. Retinoblastoma 1 (RB) is a downstream gene of p16 signaling, a cell-cycle regulator that is functionally disrupted in most human cancers. Mice with pancreas-specific deletion of Rb (Pdx1-Cre; Rb fl/fl) displayed no pancreatic abnormalities, indicating that Rb inactivation does not affect pancreatic development or induce tumorigenesis. In the presence of oncogenic Kras G12D, loss of Rb in Pdx1-expressing pancreatic cells accelerated formation of mPanIN, increased the frequency of cystic neoplasms, and promoted rapid progression toward PDAC. Nearly 20% of the Pdx1-Cre; LSL-Kras G12D; Rb fl/fl compound mutant mice died during the first month of life. Overall median survival of Pdx1-Cre; LSL-Kras G12D; Rb fl/fl mice is only ~10 weeks. These data emphasize that the p16/Rb axis actively partakes in inhibiting pancreatic carcinogenesis and progression, further supporting the widely accepted concept that activated Kras serves to initiate PanIN lesions, and the removal of the p16 INK4A-controlled senescence is essential to the malignant conversion of these PanIN lesions into lethal ductal adenocarcinoma [221].
P53 mutation occurs in 50–70% of human PDAC [4, 11, 13, 14, 16]. Loss of the p53 tumor-suppressor gene has been associated with tumor progression and metastasis in several tumor types including pancreatic ductal adenocarcinoma. Conditional p53 knock-out mice in p48-expressing pancreatic epithelial cells (P48 Cre/+;p53 fl/fl) displayed no pancreatic phenotypes. In combination with elastase–Tva transgene, P48 Cre/+;p53 fl/fl mice can develop progressive and metastatic pancreatic cancers after the somatic and sporadic delivery of RACS-PyMT viral vector [165]. Analysis of metastatic lesions demonstrated that concomitant loss of the p16/p19 locus was not required for metastasis; however, pancreas-specific deletion of a single p16/p19 allele cooperated with p53 heterozygous deletion to accelerate tumor development and metastasis (P48 Cre/+; p53 fl/+;p16/p19 fl/+) [165]. Hingorani et al. has established a conditional p53 mutant mouse line that can conditionally express point mutant allele p53 R175H [107]. The concomitant expression of p53 R172H and Kras G12D in the mouse pancreas of Pdx1-Cre; LSL-Kras G12D;p53 R172H/+ mice revealed their synergy in promoting invasive and widely metastatic carcinoma [107]. This stood in contrast to the results obtained from Pdx1-Cre; LSL-Kras G12D;p53 f/f mice, where loss of p53 did not lead to the development of metastasis [204]. This functional difference between the expression of mutant p53 R175H and the complete loss of p53 protein expression in pancreatic metastasis became evident in a direct comparison of Pdx1-Cre; LSL-Kras G12D;p53 R172H/+ and Pdx1-Cre; LSL-Kras G12D;p53 fl/f+ mice showing that loss and mutation of p53 both drive rapid progression of premalignant lesions to PDAC, but only mutant p53 R172H appears to promote metastasis in comparison to loss of p53 [212]. The underlying mechanism is unknown presently.
TGF-β signaling is known to play an important role in PDAC development and progression. SMAD4, a central mediator downstream of TGF-β signaling, is deleted or mutated in about 50% of patients with pancreatic cancer [12, 169]. Using Pdx1-Cre or p48 Cre/+ mouse strains, three independent laboratories have reported that pancreas-specific deletion of Smad4 in mice showed no abnormal pathology within the pancreas, indicating that Smad4 is dispensable for normal pancreas development [149, 170, 172]. Although all three reports agreed that, in the presence of oncogenic Kras G12D, loss of Smad4 significantly enhanced the development of pancreatic invasive cancer in comparison to mice with Kras G12D activation alone, there were several discernible differences among them. The compound Pdx1-Cre; LSL-Kras G12D; Smad4 fl/fl mice exhibited a high incidence of IPMN and active fibrosis, and the IPMN occasionally progressed to locally invasive cancer with little evidence of metastases by 6 months of age and without loss of p53 or p16 Ink4A expressions detected [172]. However, in p48 cre/+; LSL-Kras G12D; Smad4 fl/fl mice, MCNs were the predominant precancerous lesions, and their progression to invasive disease was accompanied by the inactivation of p53 or p16 [149]. The histological differences observed in the two models cannot be simply attributed to the uses of two difference Cre-expressing mouse lines driven by two different promoters. In the study by Bardeesy et al., the precancerous lesions were characterized as IPMN in both Pdx1-Cre; LSL-Kras G12D; Smad4 fl/fl and p48 cre/+; LSL-Kras G12D; Smad4 fl/fl GEMMs [170]. In addition to SMAD4, the TGF-β receptor type II (TGFBR2) gene is also altered in a subset of human PDAC [147]. Pancreas-specific Tgfbr2 knockout mice alone (p48 cre/+; Tgfbr2 fl/fl) did not exhibit discernible phenotype in 1.5 years. Remarkably, in the context of mutant Kras G12D expression, Tgfbr2 knockout mice rapidly succumbed to well-differentiated PDAC with 100% penetrance and significantly reduced the median survival to 59 days [171]. One notable histological feature of this compound mutant model is that only differentiated ductal adenocarcinoma was observed and undifferentiated or sarcomatoid tumors were markedly absent. Undifferentiated and sarcomatoid tumors have been commonly documented in other compound GEMMs involving mutant Kras [107, 113, 204, 211] but are infrequently presented in human pancreatic cancers. These data would suggest that invasive pancreatic tumors in the p48 cre/+; LSL-Kras G12D; Tgfbr2 fl/fl model may have the closest histologic presentation to human PDAC of the existing GEMMs [171]. Recently transcriptional intermediary factor 1γ (TIF1γ) has been proposed to function as a regulator of the TGF-β signaling pathway [222]. Conditional inactivation of TIF1γ in the pancreas (Pdx1-Cre; Tif1γ fl/fl) did not impact its normal development. In combination with mutant Kras G12D expression, the loss of Tif1γ induced the growth of pancreatic precancerous lesions reminiscent of human IPMNs [213]. These mucinous cystic lesions resembled those observed in Pdx1-Cre; LSL-Kras G12D; Smad4 fl/fl mice [170, 172]. This particular model provides a useful tool to further interrogate the interaction of TIF1γ with TGF-β signaling during carcinogenesis. Activin receptor type 1B (ACVR1B) is a member of TGF-β superfamily. TheACVR1B gene was first identified by us as a bona fide tumor-suppressor gene in human PDAC [223]. Conventional knockout of the Acvr1b gene resulted in mouse embryonic lethality [224]. Thus, we have generated a conditional floxed Acvr1b mouse line to investigate its role in tumorigenesis [225]. We have found that disrupted activin signaling in the pancreas can result in focal chronic pancreatitis-like histopathological changes such as inflammatory cell infiltration, acinar to ductal metaplasia, and fibrosis in Pdx1-Cre; Acvr1b fl/fl mice older than 8 months of age. In compound Pdx1-Cre; LSL-Kras G12D; Acvr1b fl/fl mice, the dysregulated activin signaling particularly accelerated the development of IPMNs, but not mPanINs. The progression to invasive ductal carcinomas appears to require additional p16 inactivation. Our data provide the first critical evidence supporting a role for activin signaling in pancreatic tumorigenesis (unpublished data).
We have previously reported the involvement of the phosphatidylinositol 3-kinase (PI3K) signaling pathway in the development of human pancreatic tumor [226]. Tumor-suppressor gene PTEN is a negative regulator of PI3K signaling. Loss of PTEN expression is less frequently identified in human PDAC in comparing with tumor-suppressive genes p16, p53, and SMAD4 [227]. The loss of Pten in the pancreas was sufficient to evoke acinar to ductal metaplasia in Pdx1-Cre; Pten fl/fl mice [201]. A fraction of these mice can develop ductal carcinoma. These results indicate that dysregulation of the PI3K pathway in pancreatic progenitor cells can lead to the initiation of pancreatic carcinoma in vivo [201]. In combination with mutant Kras G12D, Pten fl/+ haploinsufficiency significantly accelerated the development of acinar-to-ductal metaplasia and mPanIN, and their progression to PDAC occurred in less than a year [228]. Mice with activated Kras G12D and homozygous deletion of Pten in the pancreas led to premature demise of the Pdx1-Cre; LSL-Kras G12D; Pten fl/fl mice from pancreatic cancer by 3 weeks of age [229]. Taken together, these data have demonstrated that the Pten-regulated signaling can affect the initiation and progression of pancreatic cancer.
Inherited heterozygous mutations in the BRCA2 tumor-suppressor gene have been associated with an increased risk of many cancer types including pancreatic cancer. These germline mutations in BRCA2 account for ~6% of familial pancreatic cancer [230, 231]. Mice with conditional Brca2 knockout in the pancreas (Pdx1-Cre; Brca2 fl/fl) developed mPanINs at 5 months of age, and about 15% of the cases progressed to invasive and metastatic PDAC at a latency of 15 months or greater [203]. In combination with p53 inactivation, mice carrying the genotype Pdx1-Cre; Brca2 fl/fl;p53 R172H/+ uniformly developed PDAC with variable histological features [203]. Another recent GEMM employing a conventional Brca2 +/− knockout strain to model familial pancreatic cancer in humans showed that germline heterozygosity of Brca2 was sufficient to promote PDAC initiated by oncogenic Kras G12D, irrespective of p53 status [214]. In this study, pancreatic tumors retaining a functional wild-type Brca2 allele were reported in this GEMM as well as in human specimens; loss of heterozygosity (LOH) at BRCA2 was deemed unessential for pancreatic tumorigenesis [214]. This new concept could potentially change the strategy for therapies targeting BRCA2 signaling pathway. Further confounding our understanding, Rowley et al. did not detect obvious abnormalities in the pancreas of Pdx1-Cre; Brca2 fl/fl mice. In combination with mutant Kras G12D, Brca2 deletion unexpectedly inhibited growth of premalignant lesions and tumors, but in the presence of disrupted p53, Brca2 inactivation promoted the development of premalignant lesions and pancreatic tumors [202]. These data indicate that the involvement of BRCA2 in pancreatic tumorigenesis is complex, and its dependency on p53 status remains to be further elucidated. Other than BRCA2, patients carrying germline mutations of LKB1/STK11 are also at greater risk of developing pancreatic cancer [230, 232, 233]. In mice, conventional Lkb1-knockout mice are not viable [234]. Conditional homozygous deletion of the Lkb1 gene in the pancreas (Pdx1-Cre; Lkb1 fl/fl) was sufficient to trigger total penetrance of pancreatic mucinous cystadenomas, a benign form of pancreatic tumor, but not PDAC. Heterozygous Pdx1-Cre; Lkb1 fl/+ mice were disease-free [209]. However, Lkb1 haploinsufficiency cooperated with oncogenic Kras G12D in vivo in increasing incidences of PanINs and PDAC and shortening medium survival significantly [209]. In addition to PDAC, tumors with cystic components were also observed in Pdx1-Cre; LSL-Kras G12D; Lkb1 fl/+ mice. This is not unexpected and is consistent with our previous reports that LKB1 germline and somatic mutations are more frequently detected in human pancreatic cancer associated with IPMN than in PDAC [17, 18, 232].
Inflammation has been documented to promote PDAC initiation and progression recently. For example, the receptor for advanced glycation end-products (RAGE) is a multi-ligand receptor and a member of the immunoglobulin superfamily of cell surface molecules, which has been be implicated in pancreatic tumorigenesis [235]. To evaluate the impact of RAGE deletion on the development of pancreatic cancer, we generated Pdx1-Cre; LSL-Kras G12D;p16 −/−; RAGE −/− mice. We found that RAGE gene deficiency inhibited the development of ductal neoplasia and prolonged survival. These data provide critical information for targeting the ligand–RAGE axis as a possible early intervention and prophylaxis for patients with high risk for developing pancreatic cancer [236]. The Stat3 transcription factor is an important regulator of inflammation. Conditional Stat3 knockout mice (Pdx1-Cre; Stat3 fl/fl) developed normally, and these mice did not exhibit evident physiologic alterations. Compound Pdx1-Cre; LSL-Kras G12D; Stat3 fl/fl mutant mice displayed drastically reduced incidences of acinar to ductal metaplasia and mPanINs in comparison to Pdx1-Cre; LSL-Kras G12D mice [205]. Similar results were reported in a similar model using p48Cre/+ (p48 Cre/+; Kras G12D; Stat3 fl/fl), thus supporting that Stat3 signaling is dispensable for pancreas development, but the ablation of Stat3 signaling can inhibit the development of mutant Kras-initiated preneoplastic formation [206]. The activation of NF–κB, a major transcription factor of inflammatory responses, has been reported to be a downstream target of oncogenic KrasG12D-induced transformation [237, 238]. Pancreas-specific deletion of inhibitor of κB kinase 2 (Ikk2), a component of the canonical NF–κB signaling pathway, substantially delayed the process of the Kras G12D-induced pancreatic tumorigenesis [215, 239]. Conditional deletion of TNF-α, an upstream stimulus of NF–κB, in combination with mutant Kras G12D activation yielded similar results observed in Pdx1-Cre; LSL-Kras G12D; Ikk2 fl/fl mice [215]. Notch and IL-1α are also reported to be involved in Kras G12D-induced NF–κB activation [215, 239], all supporting that inflammatory responses regulated by NF–κB is crucial to Kras G12D-initiated pancreatic tumorigenesis. MUC1, a membrane-tethered mucin glycoprotein, is overexpressed and aberrantly glycosylated in more than 80% of human ductal pancreatic adenocarcinomas [240]. Transgenic mice that express human MUC1 under its own promoter [241] when bred to p48 Cre/+; LSL-Kras G12D GEMM significantly enhanced the development of mPanINs and their progression to adenocarcinoma [218]. Tumors from the MUC1;p48 Cre/+; LSL-Kras G12D GEMM express higher levels of cyclooxygenase-2 (Cox-2); thus the model is ideally suited for testing novel therapeutic strategies against pancreatic cancer targeting MUC1 and/or Cox-2 [218]. Mukherjee et al. has recently shown that a triple therapy combining a novel MUC1-based vaccine, a Cox-2 inhibitor (celecoxib), and low-dose chemotherapy (gemcitabine) was effective in preventing the progression of preneoplastic intraepithelial lesions to invasive pancreatic ductal adenocarcinoma in the MUC1;p48 Cre/+; LSL-Kras G12D GEMM [219].
GEMMs targeting more than two genetic loci (Table 7) are useful strategies for investigating gene functions that may mitigate the progression and metastasis of Kras G12D-driven pancreatic cancer, especially genes potentially associated with tumor angiogenesis, cell adhesion, and motility. Glypican-1 (GPC1) was reported to be involved in the angiogenesis and metastasis of human pancreatic ductal adenocarcinoma [243]. To further examine its role in vivo, Whipple et al. generated a GPC1 null model in combination of pancreas-specific Cre-mediated activation of oncogenic Kras G12D and deletion of tumor-suppressive p16 INK4A/p19 Arf allele (Pdx1-Cre; LSL-Kras G12D;p16/p19 fl/fl; GPC1 −/− ). In comparison with Pdx1-Cre; LSL-Kras G12D;p16/p19 fl/fl mice that were wild-type for GPC1, the Pdx1-Cre; LSL-Kras G12D ;p16/p19 fl/fl; GPC1 −/− mice exhibited attenuated pancreatic tumor growth and invasiveness and decreased cancer cell proliferation and mitogen-activated protein kinase activation. These mice also exhibited suppressed angiogenesis. These in vivo data directly demonstrate that GPC1 promotes tumor growth, angiogenesis, and invasion in conjunction with oncogenic Kras-driven PDAC [242]. N-cadherin upregulation has been observed in many cancers including PDAC [244]. Pdx1-Cre; LSL-Kras G12D; p53 fl/fl mice with N-cadherin haploinsufficiency (N-cad +/−) had significant longer medium survival (177 versus142 days) than animals expressing two wild-type copies of the N-cadherin gene, indicating a role for N-cadherin in PDAC and its potential prognostic value [197]. RAS-related C3 botulinum substrate 1 (Rac1), which controls actin reorganization and can be activated by Ras, is upregulated in several human cancers [198]. Deletion of Rac1 in p48-expressing pancreatic progenitor cells did not result in pancreatic abnormalities. However, deletion of Rac1 reduced the formation of acinar to ductal metaplasias, PanINs, and pancreatic tumors in P48 Cre/+; LSL-Kras G12D;p53 R172H/+ mice, and significantly prolonged their survival [199]. Rac1 is required for early metaplastic changes and neoplasia-associated actin rearrangements in development of pancreatic cancer, suggesting that Rac1 has the potential as an early diagnostic marker or a chemopreventive target for PDAC [199].
GEMMs targeting more than two genetic loci have also been employed to demonstrate that genes associated with development are involved in pancreatic tumorigenesis. Notch receptor signaling is reactivated in a subset of PDACs [106], therefore the roles of individual Notch receptors in pancreatic tumorigenesis are of great interest to the field. Conditional deletion of Notch1 in the pancreas did not result in major pancreatic abnormalities in mice [200, 207]. But ectopic expression of activated Notch1 in the presence of mutant Kras G12D in the mouse pancreatic epithelial cells (Rosa26 NIC; LSL-Kras G12D; Pdx1CreERT) promoted rapid reprogramming of acinar cells to a duct-like phenotype and synergized in inducing PanIN formation, suggesting that Notch1 signaling may act as an oncogene in the pancreatic tumorigenesis [217]. However, in another mouse model in which Notch1 is deleted in conjunction of oncogenic Kras activation in the pancreas (Pdx1-Cre; LSL-Kras G12D; Notch1 fl/fl), the loss of Notch1 resulted in increased tumor incidence and progression, implying that Notch1 functions as a tumor-suppressor gene in the development of pancreatic tumor [216]. Notch2 is predominantly observed to in ductal cells and PanIN lesions in humans [208]. Pancreas-specific deletion of Notch2 in mice (p48 Cre/+; Notch2 fl/fl) did not induce obvious morphological or functional abnormalities. But focal exocrine atrophy was noted in mice older than 12 months of age [208]. In combination with mutant Kras G12D, loss of Notch2 in the pancreas mainly developed MCN-like lesions. The progression of mouse PanIN lesions induced by mutant Kras G12D was completely blocked by the Notch2 deficiency in the pancreas but not Notch1 [208]. The reasons for the discrepant phenotypes reported in these GEMMs are not apparent presently different Cre mouse lines and mouse genetic background are some potential factors that could have contributed to the differences but remain to be demonstrated. β-catenin is crucial for acinar cell development and is upregulated in mPanINs and PDAC [245]. Conditional knockout of β-catenin in murine pancreas (p48 Cre/+;β-catenin fl/fl) resulted in the severe reduction of acinar cells [246]. The β-catenin-deficient pancreas also displayed a significant decrease in the acinar area after caerulein treatment. Coexpressing stabilized β-catenin in the acinar compartment with mutant Kras G12D expression (β-catenin exon3/-; LSL-Kras G12D;p48 Cre/+) in mice led to pancreatic tumor development resembling human intraductal tubular tumors via the PanIN to PDAC path, indicating that the stabilized β-catenin signaling antagonized mutant Kras-driven acinar to ductal metaplasia and PanIN development [247]. Mist 1 expression is restricted to the acinar cells. To evaluate the impact of Mist1 loss in the presence of oncogenic Kras in the same compartment, mice with mutant KrasG12D knocking into the Mist 1 locus (Mist1 KrasG12D/+) were crossed to Mist1 LacZ/LacZ mice to generate Mist1 KrasG12D/LacZ mice. In this model, loss of the Mist1 expression and gain of the Kras G12D transcription under the endogenous Mist promoter occur simultaneously in the same pancreatic cells. These Mist1 KrasG12D/LacZ mice displayed accelerated mPanIN development and severe exocrine pancreatic defects that could be rescued by ectopic expression of Mist1 in acinar cells [184].
4.5 General considerations in generating GEMMs
Compound GEMMs have become more widely employed in preclinical trials and testing of potential novel target therapies [176, 248–252]. It is important to point out that, when generating a multiple conditional gene knockout mouse model, the chromosome loci of these target genes must be particularly considered, because secondary genomic DNA recombination could be induced by the Cre DNA recombinase. Each conditional recombined locus still carries one residual lox-P site, and if both residual lox-P sites are in the same chromosomal arm and in close enough proximity, a secondary recombination can occur. There are three different outcomes of DNA recombination induced by Cre recombinase, which depend on the orientation of two lox-P sites. The DNA sequence between the two lox-P sites would be recognized and incised by the Cre enzyme if the two 34-nucleotide base pairs of lox-p sites are in the same direction. If they are in the opposite orientation, the DNA sequence between the two lox-P sites would be reversed. When the two lox-P sites are in the same orientation at the same locus, but different alleles, the DNA sequences behind the lox-P sites will be translocated between the two alleles [253]. The efficiency of chromosomal rearrangement induced by the Cre enzyme is reversely associated with the genomic distance of two lox-P sites [254]. This means that longer the distance between two lox-P sites may result in less efficient DNA recombination. In addition, it is imperative to emphasize that mouse genetic background should be considered as a compulsory factor in the analysis of phenotypes in GEMMs [255]. Genetic susceptibility loci to pancreatic ductal adenocarcinoma have recently been identified in the Ela-Kras G12D mouse models in various mouse strains [256]. C57BL6, 129, and FVB strains are generally utilized for the generation of knockout, transgenic, and conditional GEMMs. These distinct mouse strains harbor different susceptibility loci to mutant Kras-driven pancreatic tumorigenesis [256]. GEMMs involving multiple target genes are usually mixed with various degrees of these mouse strain background simply due to different breeding steps and breeding strategies that may result in distinct genetic backgrounds. Because of this, mouse models with the same genotype generated in different laboratories may display divergent phenotypes. Thus, setting up the littermates as the control group for comparison is a minimal obligatory necessity [257].
5 Newly developed models that can be used for tracking mutant cell lineage and reversing expression of mutant allele in pancreatic tumor
Conditional gene knock-in and knock-out mouse lines, if combined with advanced cellular lineage labeling techniques, could help us better comprehend the dynamic process of pancreatic carcinogenesis. Metastasis is the leading cause of cancer-associated death, but many details of the metastatic process are still unknown. Rhim et al. applied a Rosa26YFP lineage-labeling technique to track pancreatic epithelial cells with genetic modifications by introducing a lox-stop-lox-Rosa26YFP allele into Pdx1-Cre; LSL-Kras G12D;p53 fl/fl or Pdx1-Cre; LSL-Kras G12D;p16/p19 fl/fl GEMM [258]. In these GEMMs, YFP+ cells consistently represent the Cre + pancreatic epithelial lineage which harbors recombined Kras G12D allele and deletion of p53 or p16/19 tumor-suppressor gene. Using this strategy, the YFP+ cells reportedly invaded and entered the bloodstream early, even before pancreatic malignant transformation. Furthermore, mesenchymal biomarkers were detected in these disseminated and circulating mutant pancreatic cells, suggesting that these cells lost their original pancreatic epithelial markers like CK19 and E-adhesion to achieve epithelial to mesenchymal transit for the invasion and dissemination. These results support the authors’ hypothesis that tumor cellular invasion could be a very early event that may occur before tumor formation [258].
Recently, a novel mutant Kras G12D knock-in mouse line was established by Collins et al. [259], in which the expression of mutant Kras G12D is double controlled by Cre enzyme expression and doxycycline administration as well. Oncogenic Kras G12D protein is exclusively transcribed in Cre-expressing cells with sustained doxycycline treatment. The expression of mutant Kras G12D oncogenic protein in those Cre+ cellular compartments would be suspended when doxycycline administration was withdrawn. In combination with p53 haploinsufficiency, mice receiving doxycycline administration would accelerate mutant Kras G12D-driven pancreatic cancer development and progression to invasive PDAC. The authors found that the inactivation of mutant Kras G12D in initiated precursor lesions or during progression to cancer through simply suspending the doxycycline administration would result in regression of the lesions, indicating that mutant Kras G12D was required for not only the initiation of pancreatic tumor but the maintenance of established neoplastic lesions. This is consistent with our recent finding that mutant Kras continues to partake in the progression to metastasis in pancreatic tumorigenesis [113]. Similar strategies have been employed to restore p53 tumor-suppressor function, which resulted in tumor growth inhibition and regression, supporting the rationale and benefits of novel therapies aiming to restore or mimic p53 function in tumors harboring altered p53 [260, 261].
6 Conclusions
In summary, although there are numerous strategies to model for human pancreatic cancer, it is commonly agreed that GEMMs better recapitulate the full spectrum of human pancreatic tumorigenesis. Furthermore, by crossbreeding existing GEMMs, versatile new models can be easily generated to serve as a useful platform to accommodate new research directions in investigations of cancer cell origin, molecular pathways for pancreatic cancer development, the processes of metastasis, etc. These GEMMs are also valuable tools in translational research, such as the development of early detection methods and the evaluation of potential therapeutic strategies. Needless to say, it is critical to choose proper animal models for successful completion of pancreatic cancer research projects, and the choice of a particular model depends on the specific emphasis of each experimental design. Briefly, xenograft mouse models are direct transplantation of already transformed tumor cells which completely lack precursor lesions and the conversion from premalignant state to invasive cancer, but offer rapid development of invasive tumors. GEMMs, on the other hand, can spontaneously develop precancerous lesions, but cannot recapitulate the process of mutagenesis. Carcinogen-induced cancer mouse models can mimic the entire process of pancreatic tumorigenesis but the lack of the tissue-specificity of the carcinogens and the uncharacterized genetic profiles of these tumors currently limit their utilities in testing target therapies. Thus, each model has its strengths and weaknesses, and we hope that this review has provided its audience insights into choosing the most appropriate animal model for any pancreatic cancer research project.
References
Hruban, R. H., et al. (2001). Pancreatic intraepithelial neoplasia: A new nomenclature and classification system for pancreatic duct lesions. The American Journal of Surgical Pathology, 25(5), 579–586.
Takaori, K., et al. (2006). Current topics on precursors to pancreatic cancer. Advances in Medical Sciences, 51, 23–30.
Adsay, N. V. (2003). The “new kid on the block”: Intraductal papillary mucinous neoplasms of the pancreas: Current concepts and controversies. Surgery, 133(5), 459–463.
Hruban, R. H., Wilentz, R. E., & Kern, S. E. (2000). Genetic progression in the pancreatic ducts. American Journal of Pathology, 156(6), 1821–1825.
Wilentz, R. E., Albores-Saavedra, J., & Hruban, R. H. (2000). Mucinous cystic neoplasms of the pancreas. Seminars in Diagnostic Pathology, 17(1), 31–42.
Yachida, S., et al. (2010). Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature, 467(7319), 1114–1117.
Almoguera, C., et al. (1988). Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell, 53(4), 549–554.
Caldas, C., et al. (1994). Frequent somatic mutations and homozygous deletions of the p16 (MTS1) gene in pancreatic adenocarcinoma. Nature Genetics, 8, 27–31.
Schutte, M., et al. (1997). Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas. Cancer Research, 57, 3126–3130.
Redston, M. S., et al. (1994). p53 mutations in pancreatic carcinoma and evidence of common involvement of homocopolymer tracts in DNA microdeletions. Cancer Research, 54, 3025–3033.
Pellegata, S., et al. (1994). K-ras and p53 gene mutations in pancreatic cancer: Ductal and nonductal tumors progress through different genetic lesions. Cancer Research, 54, 1556–1560.
Hahn, S. A., et al. (1996). DPC4, a candidate tumor suppressor gene at human chromosome 18q21.1. Science, 271(5247), 350–353.
Wilentz, R. E., et al. (2000). Loss of expression of Dpc4 in pancreatic intraepithelial neoplasia (PanIN): Evidence that DPC4 inactivation occurs late in neoplastic progression. Cancer Research, 60, 2002–2006.
Su, G. H., & Kern, S. E. (2000). Molecular genetics of ductal pancreatic neoplasia. Curr Opin Gastroenterology, 16, 419–425.
Klimstra, D. S., & Longnecker, D. S. (1994). K-ras mutations in pancreatic ductal proliferative lesions. American Journal of Pathology, 145(6), 1547–1550.
DiGiuseppe, J. A., et al. (1994). Overexpression of p53 protein in adenocarcinoma of the pancreas. American Journal of Clinical Pathology, 101(6), 684–688.
Sato, N., et al. (2001). STK11/LKB1 Peutz-Jeghers gene inactivation in intraductal papillary–mucinous neoplasms of the pancreas. American Journal of Pathology, 159(6), 2017–2022.
Sahin, F., et al. (2003). Loss of Stk11/Lkb1 expression in pancreatic and biliary neoplasms. Modern Pathology, 16(7), 686–691.
Schonleben, F., et al. (2006). PIK3CA mutations in intraductal papillary mucinous neoplasm/carcinoma of the pancreas. Clinical Cancer Research, 12(12), 3851–3855.
Schonleben, F., et al. (2007). BRAF and KRAS gene mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/IPMC) of the pancreas. Cancer Letters, 249(2), 242–248.
Corbett, T. H., et al. (1984). Induction and chemotherapeutic response of two transplantable ductal adenocarcinomas of the pancreas in C57BL/6 mice. Cancer Research, 44(2), 717–726.
Zimmerman, J. A., et al. (1982). Pancreatic carcinoma induced by N-methyl-N′-nitrosourea in aged mice. Gerontology, 28(2), 114–120.
Gingell, R., et al. (1976). Metabolism of the pancreatic carcinogens N-nitroso-bis(2-oxopropyl)amine and N-nitroso-bis(2-hydroxypropyl)amine in the Syrian hamster. Journal of the National Cancer Institute, 57(5), 1175–1178.
Pour, P., et al. (1976). A further pancreatic carcinogen in Syrian golden hamsters: N-nitroso-bis(2-acetoxypropyl)amine. Cancer Letters, 1(4), 197–202.
Pour, P., et al. (1975). Pancreatic neoplasms in an animal model: Morphological, biological, and comparative studies. Cancer, 36(2), 379–389.
Roebuck, B. D., Baumgartner, K. J., & Thron, C. D. (1984). Characterization of two populations of pancreatic atypical acinar cell foci induced by azaserine in the rat. Laboratory Investigation, 50(2), 141–146.
Roebuck, B. D., & Longnecker, D. S. (1977). Species and rat strain variation in pancreatic nodule induction by azaserine. Journal of the National Cancer Institute, 59(4), 1273–1277.
Longnecker, D. S., & Curphey, T. J. (1975). Adenocarcinoma of the pancreas in azaserine-treated rats. Cancer Research, 35(8), 2249–2258.
Osvaldt, A. B., et al. (2006). Pancreatic intraepithelial neoplasia and ductal adenocarcinoma induced by DMBA in mice. Surgery, 140(5), 803–809.
Bax, J., et al. (1986). Adenosine triphosphatase, a new marker for the differentiation of putative precancerous foci induced in rat pancreas by azaserine. Carcinogenesis, 7(3), 457–462.
Roebuck, B. D., Baumgartner, K. J., & Longnecker, D. S. (1987). Growth of pancreatic foci and development of pancreatic cancer with a single dose of azaserine in the rat. Carcinogenesis, 8(12), 1831–1835.
Woutersen, R. A., van Garderen-Hoetmer, A., & Longnecker, D. S. (1987). Characterization of a 4-month protocol for the quantitation of BOP-induced lesions in hamster pancreas and its application in studying the effect of dietary fat. Carcinogenesis, 8(6), 833–837.
Mizumoto, K., et al. (1989). Cycles of repeated augmentation pressure in rapid production of pancreatic and cholangiocellular carcinomas in hamsters initiated with N-nitrosobis(2-oxopropyl)amine. Carcinogenesis, 10(8), 1457–1459.
Meijers, M., et al. (1989). Histogenesis of early preneoplastic lesions induced by N-nitrosobis(2-oxopropyl)amine in exocrine pancreas of hamsters. International Journal of Pancreatology, 4(2), 127–137.
Kilian, M., et al. (2006). Matrix metalloproteinase inhibitor RO 28–2653 decreases liver metastasis by reduction of MMP-2 and MMP-9 concentration in BOP-induced ductal pancreatic cancer in Syrian hamsters: Inhibition of matrix metalloproteinases in pancreatic cancer. Prostaglandins, Leukotrienes, and Essential Fatty Acids, 75(6), 429–434.
Kubozoe, T., et al. (2001). Absence of beta-catenin gene mutations in pancreatic duct lesions induced by N-nitrosobis(2-oxopropyl)amine in hamsters. Cancer Letters, 168(1), 1–6.
Kokkinakis, D. M., & Scarpelli, D. G. (1989). DNA alkylation in the hamster induced by two pancreatic carcinogens. Cancer Research, 49(12), 3184–3189.
Mangino, M. M., Scarpelli, D. G., & Kokkinakis, D. M. (1990). Metabolism and activation of the pancreatic carcinogen N-nitrosobis(2-oxopropyl)amine by isolated hepatocytes and pancreatic cells of the Syrian hamster. Carcinogenesis, 11(4), 625–631.
Sugio, K., et al. (1996). High yields of K-ras mutations in intraductal papillary mucinous tumors and invasive adenocarcinomas induced by N-nitroso(2-hydroxypropyl)(2-oxopropyl)amine in the pancreas of female Syrian hamsters. Carcinogenesis, 17(2), 303–309.
Longnecker, D. S., et al. (1985). Induction of pancreatic carcinomas in rats with N-nitroso(2-hydroxypropyl)(2-oxopropyl)amine: Histopathology. Journal of the National Cancer Institute, 74(1), 209–217.
Bockman, D. E., et al. (1978). Origin of tubular complexes developing during induction of pancreatic adenocarcinoma by 7,12-dimethylbenz(a)anthracene. American Journal of Pathology, 90(3), 645–658.
Rivera, J. A., et al. (1997). A rat model of pancreatic ductal adenocarcinoma: Targeting chemical carcinogens. Surgery, 122(1), 82–90.
Z’Graggen, K., et al. (2001). Promoting effect of a high-fat/high-protein diet in DMBA-induced ductal pancreatic cancer in rats. Annals of Surgery, 233(5), 688–695.
Wendt, L. R., et al. (2007). Pancreatic intraepithelial neoplasia and ductal adenocarcinoma induced by DMBA in mice: Effects of alcohol and caffeine. Acta Cirúrgica Brasileira, 22(3), 202–209.
Kimura, K., et al. (2007). Activation of Notch signaling in tumorigenesis of experimental pancreatic cancer induced by dimethylbenzanthracene in mice. Cancer Science, 98(2), 155–162.
Pour, P. M., & Rivenson, A. (1989). Induction of a mixed ductal-squamous-islet cell carcinoma in a rat treated with a tobacco-specific carcinogen. American Journal of Pathology, 134(3), 627–631.
Rivenson, A., et al. (1988). Induction of lung and exocrine pancreas tumors in F344 rats by tobacco-specific and Areca-derived N-nitrosamines. Cancer Research, 48(23), 6912–6917.
Schuller, H. M., et al. (1993). Transplacental induction of pancreas tumors in hamsters by ethanol and the tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Cancer Research, 53(11), 2498–2501.
Van Benthem, J., et al. (1994). Immunocytochemical identification of DNA adducts, O6-methylguanine and 7-methylguanine, in respiratory and other tissues of rat, mouse and Syrian hamster exposed to 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Carcinogenesis, 15(9), 2023–2029.
Hayashi, Y., et al. (1987). Induction of cells with acinar cell phenotype including presence of intracellular amylase. Treatment with 12-O-tetradecanoyl-phorbol-13-acetate in a neoplastic human salivary intercalated duct cell line grown in athymic nude mice. Cancer, 60(5), 1000–1008.
Reddy, J. K., & Rao, M. S. (1975). Pancreatic adenocarcinoma in inbred guinea pigs induced by n-methyl-N-nitrosourea. Cancer Research, 35(8), 2269–2277.
Rao, M. S., & Reddy, J. K. (1980). Histogenesis of pseudo-ductular changes induced in the pancreas of guinea pigs treated with N-methyl-N-nitrosourea. Carcinogenesis, 1(12), 1027–1037.
Chang, K. W., et al. (1994). Genomic p53 mutation in a chemically induced hamster pancreatic ductal adenocarcinoma. Cancer Research, 54(14), 3878–3883.
Al-Wadei, H. A., & Schuller, H. M. (2009). Nicotinic receptor-associated modulation of stimulatory and inhibitory neurotransmitters in NNK-induced adenocarcinoma of the lungs and pancreas. The Journal of Pathology, 218(4), 437–445.
Longnecker, D. S. (1991). Hormones and pancreatic cancer. International Journal of Pancreatology, 9, 81–86.
Lhoste, E. F., & Longnecker, D. S. (1987). Effect of bombesin and caerulein on early stages of carcinogenesis induced by azaserine in the rat pancreas. Cancer Research, 47(12), 3273–3277.
McGuinness, E. E., Morgan, R. G., & Wormsley, K. G. (1987). Fate of pancreatic nodules induced by raw soya flour in rats. Gut, 28(Suppl), 207–212.
Al-Wadei, H. A., Al-Wadei, M. H., & Schuller, H. M. (2009). Prevention of pancreatic cancer by the beta-blocker propranolol. Anti-Cancer Drugs, 20(6), 477–482.
Valentich, M. A., et al. (2006). Effect of the co-administration of phenobarbital, quercetin and mancozeb on nitrosomethylurea-induced pancreatic tumors in rats. Food and Chemical Toxicology, 44(12), 2101–2105.
Ouyang, N., et al. (2006). Nitric oxide-donating aspirin prevents pancreatic cancer in a hamster tumor model. Cancer Research, 66(8), 4503–4511.
Kuroiwa, Y., et al. (2006). Protective effects of benzyl isothiocyanate and sulforaphane but not resveratrol against initiation of pancreatic carcinogenesis in hamsters. Cancer Letters, 241(2), 275–280.
Heukamp, I., et al. (2005). Effects of the antioxidative vitamins A, C and E on liver metastasis and intrametastatic lipid peroxidation in BOP-induced pancreatic cancer in Syrian hamsters. Pancreatology, 5(4–5), 403–409.
Schuller, H. M., et al. (2002). The cyclooxygenase inhibitor ibuprofen and the FLAP inhibitor MK886 inhibit pancreatic carcinogenesis induced in hamsters by transplacental exposure to ethanol and the tobacco carcinogen NNK. Journal of Cancer Research and Clinical Oncology, 128(10), 525–532.
Strouch, M. J., et al. (2011). A high omega-3 fatty acid diet mitigates murine pancreatic precancer development. Journal of Surgical Research, 165(1), 75–81.
Gray, M. J., et al. (2005). Neuropilin-1 suppresses tumorigenic properties in a human pancreatic adenocarcinoma cell line lacking neuropilin-1 coreceptors. Cancer Research, 65(9), 3664–3670.
Bosma, M. J., & Carroll, A. M. (1991). The SCID mouse mutant: Definition, characterization, and potential uses. Annual Review of Immunology, 9, 323–350.
Ito, M., et al. (2002). NOD/SCID/gamma(c)(null) mouse: An excellent recipient mouse model for engraftment of human cells. Blood, 100(9), 3175–3182.
Quintana, E., et al. (2008). Efficient tumour formation by single human melanoma cells. Nature, 456(7222), 593–598.
Hafeez, B.B., et al., Plumbagin, a plant derived natural agent inhibits the growth of pancreatic cancer cells in in vitro and in vivo via targeting EGFR, Stat3 and NF-kappaB signaling pathways. Int J Cancer, 2012; 131:2175-2186.
Girgis, M. D., et al. (2011). Targeting CEA in pancreas cancer xenografts with a mutated scFv-Fc antibody fragment. EJNMMI Research, 1(1), 24.
Aurisicchio, L., et al., Novel anti-ErbB3 monoclonal antibodies show therapeutic efficacy in xenografted and spontaneous mouse tumors. J Cell Physiol, 2012;227:3381-3388.
Nakamura, M., et al., Targeting the hedgehog signaling pathway with interacting peptides to Patched-1. J Gastroenterol, 2012; 47:452-460.
Li, H., et al. (2011). STAT3 knockdown reduces pancreatic cancer cell invasiveness and matrix metalloproteinase-7 expression in nude mice. PLoS One, 6(10), e25941.
Fidler, I. J. (1986). Rationale and methods for the use of nude mice to study the biology and therapy of human cancer metastasis. Cancer Metastasis Reviews, 5(1), 29–49.
DeRosier, L. C., et al. (2006). Treatment with gemcitabine and TRA-8 anti-death receptor-5 mAb reduces pancreatic adenocarcinoma cell viability in vitro and growth in vivo. Journal of Gastrointestinal Surgery, 10(9), 1291–1300. discussion 1300.
Capella, G., et al. (1999). Orthotopic models of human pancreatic cancer. Annals of the New York Academy of Sciences, 880, 103–109.
Rubio-Viqueira, B., et al. (2006). An in vivo platform for translational drug development in pancreatic cancer. Clinical Cancer Research, 12(15), 4652–4661.
Trevino, J. G., et al. (2006). Inhibition of SRC expression and activity inhibits tumor progression and metastasis of human pancreatic adenocarcinoma cells in an orthotopic nude mouse model. American Journal of Pathology, 168(3), 962–972.
Li, C., et al. (2007). Identification of pancreatic cancer stem cells. Cancer Research, 67(3), 1030–1037.
Derosier, L. C., et al. (2007). TRA-8 anti-DR5 monoclonal antibody and gemcitabine induce apoptosis and inhibit radiologically validated orthotopic pancreatic tumor growth. Molecular Cancer Therapeutics, 6(12 Pt 1), 3198–3207.
Jimeno, A., et al. (2009). A direct pancreatic cancer xenograft model as a platform for cancer stem cell therapeutic development. Molecular Cancer Therapeutics, 8(2), 310–314.
Fogh, J., et al. (1980). Thirty-four lines of six human tumor categories established in nude mice. Journal of the National Cancer Institute, 64(4), 745–751.
Alisauskus, R., Wong, G. Y., & Gold, D. V. (1995). Initial studies of monoclonal antibody PAM4 targeting to xenografted orthotopic pancreatic cancer. Cancer Research, 55(23 Suppl), 5743s–5748s.
Killion, J. J., Radinsky, R., & Fidler, I. J. (1998). Orthotopic models are necessary to predict therapy of transplantable tumors in mice. Cancer Metastasis Reviews, 17(3), 279–284.
Loukopoulos, P., et al. (2004). Orthotopic transplantation models of pancreatic adenocarcinoma derived from cell lines and primary tumors and displaying varying metastatic activity. Pancreas, 29(3), 193–203.
Huynh, A. S., et al. (2011). Development of an orthotopic human pancreatic cancer xenograft model using ultrasound guided injection of cells. PLoS One, 6(5), e20330.
DeRosier, L. C., et al. (2007). Combination treatment with TRA-8 anti death receptor 5 antibody and CPT-11 induces tumor regression in an orthotopic model of pancreatic cancer. Clinical Cancer Research, 13(18 Pt 2), 5535s–5543s.
Partecke, I. L., et al. (2011). In vivo imaging of pancreatic tumours and liver metastases using 7 Tesla MRI in a murine orthotopic pancreatic cancer model and a liver metastases model. BMC Cancer, 11, 40.
Cheng, L., et al. (1996). Use of green fluorescent protein variants to monitor gene transfer and expression in mammalian cells. Nature Biotechnology, 14(5), 606–609.
Chalfie, M., et al. (1994). Green fluorescent protein as a marker for gene expression. Science, 263(5148), 802–805.
Astoul, P., et al. (1994). A “patient-like” nude mouse model of parietal pleural human lung adenocarcinoma. Anticancer Research, 14(1A), 85–91.
Budinger, T. F., Benaron, D. A., & Koretsky, A. P. (1999). Imaging transgenic animals. Annual Review of Biomedical Engineering, 1, 611–648.
Hoffman, R. M. (2005). The multiple uses of fluorescent proteins to visualize cancer in vivo. Nature Reviews. Cancer, 5(10), 796–806.
Bouvet, M., et al. (2000). Chronologically-specific metastatic targeting of human pancreatic tumors in orthotopic models. Clinical & Experimental Metastasis, 18(3), 213–218.
Bouvet, M., et al. (2002). Real-time optical imaging of primary tumor growth and multiple metastatic events in a pancreatic cancer orthotopic model. Cancer Research, 62(5), 1534–1540.
Katz, M. H., et al. (2003). A novel red fluorescent protein orthotopic pancreatic cancer model for the preclinical evaluation of chemotherapeutics. Journal of Surgical Research, 113(1), 151–160.
Katz, M. H., et al. (2004). An imageable highly metastatic orthotopic red fluorescent protein model of pancreatic cancer. Clinical & Experimental Metastasis, 21(1), 7–12.
Bouvet, M., et al. (2005). High correlation of whole-body red fluorescent protein imaging and magnetic resonance imaging on an orthotopic model of pancreatic cancer. Cancer Research, 65(21), 9829–9833.
Katz, M. H., et al. (2003). Selective antimetastatic activity of cytosine analog CS-682 in a red fluorescent protein orthotopic model of pancreatic cancer. Cancer Research, 63(17), 5521–5525.
Katz, M. H., et al. (2004). Survival efficacy of adjuvant cytosine-analogue CS-682 in a fluorescent orthotopic model of human pancreatic cancer. Cancer Research, 64(5), 1828–1833.
Amoh, Y., et al. (2006). Dual-color imaging of nascent blood vessels vascularizing pancreatic cancer in an orthotopic model demonstrates antiangiogenesis efficacy of gemcitabine. Journal of Surgical Research, 132(2), 164–169.
Amoh, Y., et al. (2006). Visualization of nascent tumor angiogenesis in lung and liver metastasis by differential dual-color fluorescence imaging in nestin-linked-GFP mice. Clinical & Experimental Metastasis, 23(7–8), 315–322.
Amoh, Y., et al. (2006). Dual-color imaging of nascent angiogenesis and its inhibition in liver metastases of pancreatic cancer. Anticancer Research, 26(5A), 3237–3242.
Sweeney, T. J., et al. (1999). Visualizing the kinetics of tumor-cell clearance in living animals. Proc Natl Acad Sci USA, 96(21), 12044–12049.
Kunnumakkara, A.B., et al., Zyflamend suppresses growth and sensitizes human pancreatic tumors to gemcitabine in an orthotopic mouse model through modulation of multiple targets. Int J Cancer 2012; 131:E292-E303.
Hingorani, S. R., et al. (2003). Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell, 4(6), 437–450.
Hingorani, S. R., et al. (2005). Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell, 7(5), 469–483.
Tuveson, D. A., & Hingorani, S. R. (2005). Ductal pancreatic cancer in humans and mice. Cold Spring Harbor Symposia on Quantitative Biology, 70, 65–72.
Tseng, W.W., et al., Development of an orthotopic model of invasive pancreatic cancer in an immunocompetent murine host. Clin Cancer Res. 16(14): p. 3684–95.
Partecke, L. I., et al. (2011). A syngeneic orthotopic murine model of pancreatic adenocarcinoma in the C57/BL6 mouse using the Panc02 and 6606PDA cell lines. European Surgical Research, 47(2), 98–107.
Wang, B., et al. (2001). A novel, clinically relevant animal model of metastatic pancreatic adenocarcinoma biology and therapy. International Journal of Gastrointestinal Cancer, 29(1), 37–46.
Tseng, W. W., et al. (2010). Development of an orthotopic model of invasive pancreatic cancer in an immunocompetent murine host. Clinical Cancer Research, 16(14), 3684–3695.
Qiu, W., et al. (2011). Disruption of p16 and activation of Kras in pancreas increase ductal adenocarcinoma formation and metastasis in vivo. Oncotarget, 2(11), 862–873.
Chu, Q.D. and R.H. Kim, Immunocompetent orthotopic pancreatic cancer murine model: A step in the right direction. J Surg Res, 2011 [Epub ahead of print]
Brembeck, F. H., et al. (2003). The mutant K-ras oncogene causes pancreatic periductal lymphocytic infiltration and gastric mucous neck cell hyperplasia in transgenic mice. Cancer Research, 63(9), 2005–2009.
Jhappan, C., et al. (1990). TGF alpha overexpression in transgenic mice induces liver neoplasia and abnormal development of the mammary gland and pancreas. Cell, 61(6), 1137–1146.
Pujal, J., et al. (2009). Keratin 7 promoter selectively targets transgene expression to normal and neoplastic pancreatic ductal cells in vitro and in vivo. The FASEB Journal, 23(5), 1366–1375.
Offield, M. F., et al. (1996). PDX-1 is required for pancreatic outgrowth and differentiation of the rostral duodenum. Development, 122(3), 983–995.
Aichler, M., et al. (2012). Origin of pancreatic ductal adenocarcinoma from atypical flat lesions: A comparative study in transgenic mice and human tissues. The Journal of Pathology, 226(5), 723–734.
Zhu, L., et al. (2007). Acinar cells contribute to the molecular heterogeneity of pancreatic intraepithelial neoplasia. American Journal of Pathology, 171(1), 263–273.
Means, A. L., et al. (2005). Pancreatic epithelial plasticity mediated by acinar cell transdifferentiation and generation of nestin-positive intermediates. Development, 132(16), 3767–3776.
Hruban, R. H., et al. (2006). Pathology of genetically engineered mouse models of pancreatic exocrine cancer: Consensus report and recommendations. Cancer Research, 66(1), 95–106.
Ornitz, D. M., et al. (1987). Pancreatic neoplasia induced by SV40 T-antigen expression in acinar cells of transgenic mice. Science, 238(4824), 188–193.
Quaife, C. J., et al. (1987). Pancreatic neoplasia induced by ras expression in acinar cells of transgenic mice. Cell, 48(6), 1023–1034.
Lewis, B. C., Klimstra, D. S., & Varmus, H. E. (2003). The c-myc and PyMT oncogenes induce different tumor types in a somatic mouse model for pancreatic cancer. Genes & Development, 17(24), 3127–3138.
Sandgren, E. P., et al. (1991). Pancreatic tumor pathogenesis reflects the causative genetic lesion. Proc Natl Acad Sci USA, 88(1), 93–97.
Liao, D. J., et al. (2006). Characterization of pancreatic lesions from MT-tgf alpha, Ela-myc and MT-tgf alpha/Ela-myc single and double transgenic mice. J Carcinog, 5, 19.
Grippo, P.J. and E.P. Sandgren. Acinar-to-ductal metaplasia accompanies c-myc-induced exocrine pancreatic cancer progression in transgenic rodents. Int J Cancer, 2012;131:1243-1248.
Grippo, P. J., et al. (2003). Preinvasive pancreatic neoplasia of ductal phenotype induced by acinar cell targeting of mutant Kras in transgenic mice. Cancer Research, 63(9), 2016–2019.
Jones, S., et al. (2008). Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science, 321(5897), 1801–1806.
Thayer, S. P., et al. (2003). Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature, 425(6960), 851–856.
Pasca di Magliano, M. (2006). Hedgehog/Ras interactions regulate early stages of pancreatic cancer. Genes & Development, 20(22), 3161–3173.
Sandgren, E. P., et al. (1990). Overexpression of TGF alpha in transgenic mice: Induction of epithelial hyperplasia, pancreatic metaplasia, and carcinoma of the breast. Cell, 61(6), 1121–1135.
Schmid, R. M., et al. (1999). Acinar-ductal-carcinoma sequence in transforming growth factor-alpha transgenic mice. Annals of the New York Academy of Sciences, 880, 219–230.
Liao, D. J., et al. (2000). Cell cycle basis for the onset and progression of c-Myc-induced, TGFalpha-enhanced mouse mammary gland carcinogenesis. Oncogene, 19(10), 1307–1317.
Thorgeirsson, S. S., Factor, V. M., & Snyderwine, E. G. (2000). Transgenic mouse models in carcinogenesis research and testing. Toxicology Letters, 112–113, 553–555.
Malka, D., et al. (2002). Risk of pancreatic adenocarcinoma in chronic pancreatitis. Gut, 51(6), 849–852.
Norman, J. G., et al. (1996). Transgenic animals demonstrate a role for the IL-1 receptor in regulating IL-1beta gene expression at steady-state and during the systemic stress induced by acute pancreatitis. Journal of Surgical Research, 63(1), 231–236.
Marrache, F., et al. (2008). Overexpression of interleukin-1beta in the murine pancreas results in chronic pancreatitis. Gastroenterology, 135(4), 1277–1287.
Yip-Schneider, M. T., et al. (2000). Cyclooxygenase-2 expression in human pancreatic adenocarcinomas. Carcinogenesis, 21(2), 139–146.
Muller-Decker, K., et al. (2006). Preinvasive duct-derived neoplasms in pancreas of keratin 5-promoter cyclooxygenase-2 transgenic mice. Gastroenterology, 130(7), 2165–2178.
Neufang, G., et al. (2001). Abnormal differentiation of epidermis in transgenic mice constitutively expressing cyclooxygenase-2 in skin. Proc Natl Acad Sci USA, 98(13), 7629–7634.
Colby, J. K., et al. (2008). Progressive metaplastic and dysplastic changes in mouse pancreas induced by cyclooxygenase-2 overexpression. Neoplasia, 10(8), 782–796.
Tang, C., Biemond, I., & Lamers, C. B. (1996). Cholecystokinin receptors in human pancreas and gallbladder muscle: A comparative study. Gastroenterology, 111(6), 1621–1626.
Saillan-Barreau, C., et al. (1998). Transgenic CCK-B/gastrin receptor mediates murine exocrine pancreatic secretion. Gastroenterology, 115(4), 988–996.
Mathieu, A., et al. (2005). Transgenic expression of CCK2 receptors sensitizes murine pancreatic acinar cells to carcinogen-induced preneoplastic lesions formation. International Journal of Cancer, 115(1), 46–54.
Goggins, M., et al. (1998). Genetic alterations of the transforming growth factor beta receptor genes in pancreatic and biliary adenocarcinomas. Cancer Research, 58, 5329–5332.
Kuang, C., et al. (2006). In vivo disruption of TGF-beta signaling by Smad7 leads to premalignant ductal lesions in the pancreas. Proc Natl Acad Sci USA, 103(6), 1858–1863.
Izeradjene, K., et al. (2007). Kras(G12D) and Smad4/Dpc4 haploinsufficiency cooperate to induce mucinous cystic neoplasms and invasive adenocarcinoma of the pancreas. Cancer Cell, 11(3), 229–243.
Wagner, M., et al. (1998). Malignant transformation of duct-like cells originating from acini in transforming growth factor transgenic mice. Gastroenterology, 115(5), 1254–1262.
Glasner, S., Memoli, V., & Longnecker, D. S. (1992). Characterization of the ELSV transgenic mouse model of pancreatic carcinoma. Histologic type of large and small tumors. American Journal of Pathology, 140(5), 1237–1245.
Bell, R. H., Jr., Memol, V. A., & Longnecker, D. S. (1990). Hyperplasia and tumors of the islets of Langerhans in mice bearing an elastase I-SV40 T-antigen fusion gene. Carcinogenesis, 11(8), 1393–1398.
Schaeffer, B. K., Terhune, P. G., & Longnecker, D. S. (1994). Pancreatic carcinomas of acinar and mixed acinar/ductal phenotypes in Ela-1-myc transgenic mice do not contain c-K-ras mutations. American Journal of Pathology, 145(3), 696–701.
Efrat, S., et al. (1988). Beta-cell lines derived from transgenic mice expressing a hybrid insulin gene-oncogene. Proc Natl Acad Sci USA, 85(23), 9037–9041.
Bottinger, E. P., et al. (1997). Expression of a dominant-negative mutant TGF-beta type II receptor in transgenic mice reveals essential roles for TGF-beta in regulation of growth and differentiation in the exocrine pancreas. EMBO Journal, 16(10), 2621–2633.
Yamaoka, T., et al. (2000). Diabetes and pancreatic tumours in transgenic mice expressing Pa x 6. Diabetologia, 43(3), 332–339.
Wagner, M., et al. (2001). A murine tumor progression model for pancreatic cancer recapitulating the genetic alterations of the human disease. Genes & Development, 15(3), 286–293.
Schreiner, B., et al. (2003). Pattern of secondary genomic changes in pancreatic tumors of Tgf alpha/Trp53+/− transgenic mice. Genes, Chromosomes & Cancer, 38(3), 240–248.
Bardeesy, N., et al. (2002). Obligate roles for p16(Ink4a) and p19(Arf)-p53 in the suppression of murine pancreatic neoplasia. Molecular and Cellular Biology, 22(2), 635–643.
Adrian, K., et al. (2009). Tgfbr1 haploinsufficiency inhibits the development of murine mutant Kras-induced pancreatic precancer. Cancer Research, 69(24), 9169–9174.
Grippo, P.J., et al., Concurrent PEDF deficiency and Kras mutation induce invasive pancreatic cancer and adipose-rich stroma in mice. Gut, 2012;61:1454-1464.
Krantz, S. B., et al. (2011). MT1-MMP cooperates with Kras(G12D) to promote pancreatic fibrosis through increased TGF-beta signaling. Molecular Cancer Research, 9(10), 1294–1304.
Sandgren, E. P., et al. (1993). Transforming growth factor alpha dramatically enhances oncogene-induced carcinogenesis in transgenic mouse pancreas and liver. Molecular and Cellular Biology, 13(1), 320–330.
Fisher, G. H., et al. (1999). Development of a flexible and specific gene delivery system for production of murine tumor models. Oncogene, 18(38), 5253–5260.
Morton, J. P., et al. (2008). Trp53 deletion stimulates the formation of metastatic pancreatic tumors. American Journal of Pathology, 172(4), 1081–1087.
Song, S. Y., et al. (1999). Expansion of Pdx1-expressing pancreatic epithelium and islet neogenesis in transgenic mice overexpressing transforming growth factor alpha. Gastroenterology, 117(6), 1416–1426.
Greten, F. R., et al. (2001). TGF alpha transgenic mice. A model of pancreatic cancer development. Pancreatology, 1(4), 363–368.
Siveke, J. T., et al. (2007). Concomitant pancreatic activation of Kras(G12D) and Tgfa results in cystic papillary neoplasms reminiscent of human IPMN. Cancer Cell, 12(3), 266–279.
Schutte, M., et al. (1996). DPC4 gene in various tumor types. Cancer Research, 56(11), 2527–2530.
Bardeesy, N., et al. (2006). Smad4 is dispensable for normal pancreas development yet critical in progression and tumor biology of pancreas cancer. Genes & Development, 20(22), 3130–3146.
Ijichi, H., et al. (2006). Aggressive pancreatic ductal adenocarcinoma in mice caused by pancreas-specific blockade of transforming growth factor-beta signaling in cooperation with active Kras expression. Genes & Development, 20(22), 3147–3160.
Kojima, K., et al. (2007). Inactivation of Smad4 accelerates Kras(G12D)-mediated pancreatic neoplasia. Cancer Research, 67(17), 8121–8130.
Akhurst, R. J. (2002). TGF-beta antagonists: Why suppress a tumor suppressor? The Journal of Clinical Investigation, 109(12), 1533–1536.
Mathur, A., et al. (2009). Pancreatic steatosis promotes dissemination and lethality of pancreatic cancer. Journal of the American College of Surgery, 208(5), 989–994. discussion 994–6.
Yamagishi, S., et al. (2010). Positive association of circulating levels of advanced glycation end products (AGEs) with pigment epithelium-derived factor (PEDF) in a general population. Pharmacological Research, 61(2), 103–107.
Olive, K. P., et al. (2009). Inhibition of hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science, 324(5933), 1457–1461.
Guerra, C., et al. (2007). Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell, 11(3), 291–302.
Shields, J. M., et al. (2000). Understanding Ras: ‘It ain’t over ‘til it’s over’. Trends in Cell Biology, 10(4), 147–154.
Guerra, C., et al. (2003). Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell, 4(2), 111–120.
Tuveson, D. A., et al. (2004). Endogenous oncogenic K-ras(G12D) stimulates proliferation and widespread neoplastic and developmental defects. Cancer Cell, 5(4), 375–387.
Pin, C. L., Bonvissuto, A. C., & Konieczny, S. F. (2000). Mist1 expression is a common link among serous exocrine cells exhibiting regulated exocytosis. Anatomical Record, 259(2), 157–167.
Pin, C. L., et al. (2001). The bHLH transcription factor Mist1 is required to maintain exocrine pancreas cell organization and acinar cell identity. The Journal of Cell Biology, 155(4), 519–530.
Tuveson, D. A., et al. (2006). Mist1-KrasG12D knock-in mice develop mixed differentiation metastatic exocrine pancreatic carcinoma and hepatocellular carcinoma. Cancer Research, 66(1), 242–247.
Shi, G., et al. (2009). Loss of the acinar-restricted transcription factor Mist1 accelerates Kras-induced pancreatic intraepithelial neoplasia. Gastroenterology, 136(4), 1368–1378.
Mao, X., Fujiwara, Y., & Orkin, S. H. (1999). Improved reporter strain for monitoring Cre recombinase-mediated DNA excisions in mice. Proc Natl Acad Sci USA, 96(9), 5037–5042.
Lakso, M., et al. (1992). Targeted oncogene activation by site-specific recombination in transgenic mice. Proc Natl Acad Sci USA, 89(14), 6232–6236.
Jackson, E. L., et al. (2001). Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes & Development, 15(24), 3243–3248.
Carriere, C., et al. (2007). The nestin progenitor lineage is the compartment of origin for pancreatic intraepithelial neoplasia. Proc Natl Acad Sci USA, 104(11), 4437–4442.
Leach, S. D. (2005). Epithelial differentiation in pancreatic development and neoplasia: New niches for nestin and Notch. Journal of Clinical Gastroenterology, 39(4 Suppl 2), S78–S82.
Fendrich, V., et al. (2008). Hedgehog signaling is required for effective regeneration of exocrine pancreas. Gastroenterology, 135(2), 621–631.
Habbe, N., et al. (2008). Spontaneous induction of murine pancreatic intraepithelial neoplasia (mPanIN) by acinar cell targeting of oncogenic Kras in adult mice. Proc Natl Acad Sci USA, 105(48), 18913–18918.
Trobridge, P., et al. (2009). TGF-beta receptor inactivation and mutant Kras induce intestinal neoplasms in mice via a beta-catenin-independent pathway. Gastroenterology, 136(5), 1680–1688. e7.
Kim, W. Y., et al. (2009). HIF2alpha cooperates with RAS to promote lung tumorigenesis in mice. The Journal of Clinical Investigation, 119(8), 2160–2170.
Fan, H. Y., et al. (2009). Cell type-specific targeted mutations of Kras and Pten document proliferation arrest in granulosa cells versus oncogenic insult to ovarian surface epithelial cells. Cancer Research, 69(16), 6463–6472.
Dail, M., et al. (2010). Mutant Ikzf1, KrasG12D, and Notch1 cooperate in T lineage leukemogenesis and modulate responses to targeted agents. Proc Natl Acad Sci USA, 107(11), 5106–5111.
Sund, N. J., et al. (2001). Tissue-specific deletion of Foxa2 in pancreatic beta cells results in hyperinsulinemic hypoglycemia. Genes & Development, 15(13), 1706–1715.
Su, Y., et al., N-Cadherin haploinsufficiency increases survival in a mouse model of pancreatic cancer. Oncogene, 2012;31;4484-4489.
Karlsson, R., et al. (2009). Rho GTPase function in tumorigenesis. Biochimica et Biophysica Acta, 1796(2), 91–98.
Heid, I., et al. (2011). Early requirement of Rac1 in a mouse model of pancreatic cancer. Gastroenterology, 141(2), 719–730. 730 e1-7.
Nakhai, H., et al. (2008). Conditional ablation of Notch signaling in pancreatic development. Development, 135(16), 2757–2765.
Stanger, B. Z., et al. (2005). Pten constrains centroacinar cell expansion and malignant transformation in the pancreas. Cancer Cell, 8(3), 185–195.
Rowley, M., et al. (2011). Inactivation of Brca2 promotes Trp53-associated but inhibits KrasG12D-dependent pancreatic cancer development in mice. Gastroenterology, 140(4), 1303–1313. e1-3.
Feldmann, G., et al. (2011). Inactivation of Brca2 cooperates with Trp53(R172H) to induce invasive pancreatic ductal adenocarcinomas in mice: A mouse model of familial pancreatic cancer. Cancer Biology & Therapy, 11(11), 959–968.
Bardeesy, N., et al. (2006). Both p16(Ink4a) and the p19(Arf)-p53 pathway constrain progression of pancreatic adenocarcinoma in the mouse. Proc Natl Acad Sci USA, 103(15), 5947–5952.
Corcoran, R. B., et al. (2011). STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Research, 71(14), 5020–5029.
Fukuda, A., et al. (2011). Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma initiation and progression. Cancer Cell, 19(4), 441–455.
Siveke, J. T., et al. (2008). Notch signaling is required for exocrine regeneration after acute pancreatitis. Gastroenterology, 134(2), 544–555.
Mazur, P. K., et al. (2010). Notch2 is required for progression of pancreatic intraepithelial neoplasia and development of pancreatic ductal adenocarcinoma. Proc Natl Acad Sci USA, 107(30), 13438–13443.
Morton, J. P., et al. (2010). LKB1 haploinsufficiency cooperates with Kras to promote pancreatic cancer through suppression of p21-dependent growth arrest. Gastroenterology, 39(2), 586–597. 597 e1-6.
Murtaugh, L. C., et al. (2003). Notch signaling controls multiple steps of pancreatic differentiation. Proc Natl Acad Sci USA, 100(25), 14920–14925.
Aguirre, A. J., et al. (2003). Activated Kras and Ink4a/Arf deficiency cooperate to produce metastatic pancreatic ductal adenocarcinoma. Genes & Development, 17(24), 3112–3126.
Morton, J. P., et al. (2010). Mutant p53 drives metastasis and overcomes growth arrest/senescence in pancreatic cancer. Proc Natl Acad Sci USA, 107(1), 246–251.
Vincent, D. F., et al. (2009). Inactivation of TIF1gamma cooperates with Kras to induce cystic tumors of the pancreas. PLoS Genetics, 5(7), e1000575.
Skoulidis, F., et al. (2010). Germline Brca2 heterozygosity promotes Kras(G12D)-driven carcinogenesis in a murine model of familial pancreatic cancer. Cancer Cell, 18(5), 499–509.
Maniati, E., et al. (2011). Crosstalk between the canonical NF-kappaB and Notch signaling pathways inhibits Ppargamma expression and promotes pancreatic cancer progression in mice. The Journal of Clinical Investigation, 121(12), 4685–4699.
Hanlon, L., et al. (2010). Notch1 functions as a tumor suppressor in a model of K-ras-induced pancreatic ductal adenocarcinoma. Cancer Research, 70(11), 4280–4286.
De La, O. J., et al. (2008). Notch and Kras reprogram pancreatic acinar cells to ductal intraepithelial neoplasia. Proc Natl Acad Sci USA, 105(48), 18907–18912.
Tinder, T. L., et al. (2008). MUC1 enhances tumor progression and contributes toward immunosuppression in a mouse model of spontaneous pancreatic adenocarcinoma. Journal of Immunology, 181(5), 3116–3125.
Mukherjee, P., et al. (2009). Progression of pancreatic adenocarcinoma is significantly impeded with a combination of vaccine and COX-2 inhibition. Journal of Immunology, 182(1), 216–224.
Sharpless, N. E., et al. (2001). Loss of p16Ink4a with retention of p19Arf predisposes mice to tumorigenesis. Nature, 413(6851), 86–91.
Collado, M., et al. (2005). Tumour biology: Senescence in premalignant tumours. Nature, 436(7051), 642.
Yan, K. P., et al. (2004). Molecular cloning, genomic structure, and expression analysis of the mouse transcriptional intermediary factor 1 gamma gene. Gene, 334, 3–13.
Su, G. H., et al. (2001). ACVR1B (ALK4, activin receptor type 1B) gene mutations in pancreatic carcinoma. Proc Natl Acad Sci USA, 98(6), 3254–3257.
Gu, Z., et al. (1998). The type I activin receptor ActRIB is required for egg cylinder organization and gastrulation in the mouse. Genes & Development, 12(6), 844–857.
Qiu, W., et al. (2011). Conditional activin receptor type 1B (Acvr1b) knockout mice reveal hair loss abnormality. The Journal of Investigative Dermatology, 131(5), 1067–1076.
Schonleben, F., et al. (2008). PIK3CA, KRAS, and BRAF mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/C) of the pancreas. Langenbeck's Archives of Surgery, 393(3), 289–296.
Okami, K., et al. (1998). Analysis of PTEN/MMAC1 alterations in aerodigestive tract tumors. Cancer Research, 58(3), 509–511.
Ying, H., et al. (2011). Pten is a major tumor suppressor in pancreatic ductal adenocarcinoma and regulates an NF-kappaB-cytokine network. Cancer Discov, 1(2), 158–169.
Hill, R., et al. (2010). PTEN loss accelerates KrasG12D-induced pancreatic cancer development. Cancer Research, 70(18), 7114–7124.
Hruban, R. H., et al. (1999). Familial pancreatic cancer. Annals of Oncology, 4, 69–73.
Couch, F. J., et al. (2007). The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiology, Biomarkers & Prevention, 16(2), 342–346.
Su, G. H., et al. (1999). Germline and somatic mutations of the STK11/LKB1 Peutz-Jeghers gene in pancreatic and biliary cancers. American Journal of Pathology, 154, 1835–1840.
Giardiello, F. M., et al. (2000). Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology, 119(6), 1447–1453.
Ylikorkala, A., et al. (2001). Vascular abnormalities and deregulation of VEGF in Lkb1-deficient mice. Science, 293(5533), 1323–1326.
Grote, V.A., et al., The Associations of advanced glycation end products and its soluble receptor with pancreatic cancer risk: A case–control study within the prospective EPIC cohort. Cancer Epidemiol Biomarkers Prev, 2012;21:619-628.
DiNorcia, J., et al. (2012). RAGE gene deletion inhibits the development and progression of ductal neoplasia and prolongs survival in a murine model of pancreatic cancer. Journal of Gastrointestinal Surgery, 16(1), 104–112. discussion 112.
Meylan, E., et al. (2009). Requirement for NF-kappaB signalling in a mouse model of lung adenocarcinoma. Nature, 462(7269), 104–107.
Fendrich, V., et al. (2010). The angiotensin-I-converting enzyme inhibitor enalapril and aspirin delay progression of pancreatic intraepithelial neoplasia and cancer formation in a genetically engineered mouse model of pancreatic cancer. Gut, 59(5), 630–637.
Ling, J., et al. (2012). KrasG12D-induced IKK2/beta/NF-kappaB activation by IL-1alpha and p62 feedforward loops is required for development of pancreatic ductal adenocarcinoma. Cancer Cell, 21(1), 105–120.
Gendler, S. J., & Spicer, A. P. (1995). Epithelial mucin genes. Annual Review of Physiology, 57, 607–634.
Rowse, G. J., et al. (1998). Tolerance and immunity to MUC1 in a human MUC1 transgenic murine model. Cancer Research, 58(2), 315–321.
Whipple, C.A., A.L. Young, and M. Korc, A Kras(G12D)-driven genetic mouse model of pancreatic cancer requires glypican-1 for efficient proliferation and angiogenesis. Oncogene, 2012;31:2535-2544.
Aikawa, T., et al. (2008). Glypican-1 modulates the angiogenic and metastatic potential of human and mouse cancer cells. The Journal of Clinical Investigation, 118(1), 89–99.
Agbunag, C., & Bar-Sagi, D. (2004). Oncogenic K-ras drives cell cycle progression and phenotypic conversion of primary pancreatic duct epithelial cells. Cancer Research, 64(16), 5659–5663.
Pasca di Magliano, M. (2007). Common activation of canonical Wnt signaling in pancreatic adenocarcinoma. PLoS One, 2(11), e1155.
Morris, J. P., et al. (2010). Beta-catenin blocks Kras-dependent reprogramming of acini into pancreatic cancer precursor lesions in mice. The Journal of Clinical Investigation, 120(2), 508–520.
Heiser, P. W., et al. (2008). Stabilization of beta-catenin induces pancreas tumor formation. Gastroenterology, 135(4), 1288–1300.
Feldmann, G., et al. (2008). Hedgehog inhibition prolongs survival in a genetically engineered mouse model of pancreatic cancer. Gut, 57(10), 1420–1430.
Plentz, R., et al. (2009). Inhibition of gamma-secretase activity inhibits tumor progression in a mouse model of pancreatic ductal adenocarcinoma. Gastroenterology, 136(5), 1741–1749. e6.
Funahashi, H., et al. (2007). Delayed progression of pancreatic intraepithelial neoplasia in a conditional Kras(G12D) mouse model by a selective cyclooxygenase-2 inhibitor. Cancer Research, 67(15), 7068–7071.
Ijichi, H., et al. (2011). Inhibiting Cxcr2 disrupts tumor-stromal interactions and improves survival in a mouse model of pancreatic ductal adenocarcinoma. The Journal of Clinical Investigation, 121(10), 4106–4117.
Diep, C. H., et al. (2011). Synergistic effect between erlotinib and MEK inhibitors in KRAS wild-type human pancreatic cancer cells. Clinical Cancer Research, 17(9), 2744–2756.
Branda, C. S., & Dymecki, S. M. (2004). Talking about a revolution: The impact of site-specific recombinases on genetic analyses in mice. Developmental Cell, 6(1), 7–28.
Zheng, B., et al. (2000). Engineering mouse chromosomes with Cre-loxP: Range, efficiency, and somatic applications. Molecular and Cellular Biology, 20(2), 648–655.
Brayton, C. F., Treuting, P. M., & Ward, J. M. (2012). Pathobiology of aging mice and GEM: Background strains and experimental design. Veterinary Pathology, 49(1), 85–105.
Jorgenson, T. C., et al. (2010). Identification of susceptibility loci in a mouse model of KRASG12D-driven pancreatic cancer. Cancer Research, 70(21), 8398–8406.
Yu, R., et al. (2011). Pancreatic neuroendocrine tumors in glucagon receptor-deficient mice. PLoS One, 6(8), e23397.
Rhim, A. D., et al. (2012). EMT and dissemination precede pancreatic tumor formation. Cell, 148(1–2), 349–361.
Collins, M. A., et al. (2012). Oncogenic Kras is required for both the initiation and maintenance of pancreatic cancer in mice. The Journal of Clinical Investigation, 122(2), 639–653.
Wang, Y., et al. (2011). Restoring expression of wild-type p53 suppresses tumor growth but does not cause tumor regression in mice with a p53 missense mutation. The Journal of Clinical Investigation, 121(3), 893–904.
Ventura, A., et al. (2007). Restoration of p53 function leads to tumour regression in vivo. Nature, 445(7128), 661–665.
Acknowledgments
This work was supported by NCI R01 CA109525 and Pancreatic Cancer Action Network-AACR Innovative Grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qiu, W., Su, G.H. Challenges and advances in mouse modeling for human pancreatic tumorigenesis and metastasis. Cancer Metastasis Rev 32, 83–107 (2013). https://doi.org/10.1007/s10555-012-9408-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-012-9408-2