Abstract
Interleukin-6 (IL-6) has been found to be a predictor of heart attack. We aimed to investigate the relationship of risk factor IL-6 with extent and severity of the coronary artery disease (CAD) evaluated using coronary computed tomography angiography (CCTA). A total of 303 participants without history of CAD undergoing CCTA were enrolled. Using the model of risk-adjusted Cox proportional-hazards, the association of IL-6 level with major adverse cardiac events (MACE) was detected. The participants were assigned into three study groups based on serum IL-6 level. Compared with those in the lowest tertile, patients with highest IL-6 level displayed higher atherosclerotic burden such as plaque extent defined as prevalence of obstructive CAD and segments with any plaque. After a median 3.0 year follow-up period, we also found that patients with highest IL-6 level experienced higher MACE risk and all-cause death compared with those from the lowest tertile. Among participants without CAD history who underwent CCTA, patients with high level of IL-6 had increased burden of atherosclerosis and higher MACE risk compared to participants of low level of IL-6.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Inflammation is an important factor in the progression and initiation of atherosclerosis, and involved in various cardiovascular diseases [1]. The predictive value of those inflammation biomarkers, such as interleukin-6 (IL-6), has been shown in patients of coronary artery disease (CAD) and also in healthy individuals [2]. Previously study supported the involvement of chronic inflammation in the initiation and development during atherosclerosis [3]. Increasing levels of inflammatory agents, such as IL-6, have been reported to associate with acute ischemia and serve as the indicators of recurrent CAD among patients [4, 5]. Furthermore, some studies showed that increased serum levels of IL-6 and/or other inflammatory cytokines, which trigger and sustain systemic inflammatory status, are predictors of various chronic conditions and causes of death in elderly patients [6, 7]. Moreover, interleukin-6 receptor (IL-6R) has been reported to be elevated in acute myocardial infarction (AMI) [8–10]. Right now, it is unclear whether IL-6 is a significant indicator of cardiovascular events for Chinese patients without history of CAD who underwent coronary computed tomography angiography (CCTA).
Imaging is a useful technique to assist in risk stratification [11]. In recent decades, CCTA has been shown to be a well-established imaging technique for detection atherosclerotic plaques and to evaluate the extent of coronary artery stenosis with high sensitivity and specificity [12, 13]. Several studies have demonstrated that CCTA can provide diagnostic capability and, most importantly, incremental prognostic value than calcium scoring for patients with suspected coronary heart disease (CHD) [14]. To our knowledge, no CCTA-based image analysis studies have focused IL-6 level and its relationship with MACE in asymptomatic population.
In this study, our aimed to investigate the potential role of serum IL-6 level as a useful biomarker in clinic to predict future cardiovascular risk in patients without CAD history who underwent CCTA.
Materials and methods
Study population
We retrospectively enrolled 383 patients without history of CAD undergoing CCTA evaluation. For the present study, we included only those patients with available serum IL-6 level data. Patients with CAD history, active inflammatory and malignancy disease, or those lacking serum IL-6 level were excluded. As a result, 303 participants were finally included in the study. The ethics committee of The Second Hospital of Shandong University approved the study procedure, and written informed consent forms were given by all participants. Patients were assigned into three groups based on serum IL-6 levels (<1.77, 1.78–3.07, and >3.08 pg/mL) [15]. Demographic data and coronary risk factors, such as smoking history, diabetes, dyslipidemia, hypertension and family history, were acquired before the CCTA evaluations by directly interviewing patient by investigators and/or by standardized site questionnaires. Dyslipidemia was determined by low-density lipoprotein cholesterol (LDL-C) higher than 140 mg/dL and high-density lipoprotein (HDL-C) lower than 40 mg/dL. Diabetes was defined as hemoglobin A1c (HbA1c) higher than 6.5%. Hypertension was defined as self-reported hypertension history and/or administration of antihypertensive medicines, or blood pressure higher than 140/90 mm Hg. Smoking history was defined as at least one cigarette per day for a period of at least 6 months, and smoking status was classified as never, past or current smoker.
Endpoints
The endpoints of this study was MACE, which included acute coronary syndrome (ACS), all-cause death and target vessel revascularization [16]. Clinical follow-up was conducted by medical chart reviews, telephone or direct interviews or with mailed questionnaires. Mortality rate was summarized from the medical records of deceased patients.
Imaging analysis
All scans, using 64 slice or greater CT scanners, were independently evaluated by two radiologists blind to the group assignment and clinical information. After independent assessments were made, a final CCTA diagnosis was obtained based on consensus interpretation. Plaques were detected using a modified version of 16-segment American Heart Association coronary tree model. Composition of the plaque on CCTA, including number, presence, characteristics and severity stenosis and, was assessed by level III equivalent investigators following SCCT guideline. To analysis the CCTA finding, we determined the presence of any plaque, their extent and severity, and type of plaques. Coronary plaque was defined as structures occupying at least 1 mm2. Severity of CAD was subgroup as none (no luminal stenosis), non-obstructive (less than 50% luminal stenosis), and obstructive stenosis (more than 50% luminal stenosis), the latter of which was then sub-categorized as 1-, 2- and 3-vessel disease (VD). A segment involvement score (SIS) was used to define extent of CAD, as the coronary artery segment number with any plaque [13], which was categorized into three sub-groups with SIS of 0, 1–5 and over 5. Plaque characteristics were categorized as non-calcified plaques (NCAP) with no calcification, mixed calcified plaques (MCAP) with both of calcification and NCAP, or calcified plaques (CAP) with only calcification [17, 18].
Statistical analysis
All statistical analyses were performed using STATACorp Version 12. Quantitative data were shown as the mean ± SD depending on their distribution. Intergroup comparisons across tertiles were analyzed using the Wilcoxon rank-sum test. The significance of differences was evaluated with unpaired and paired student t test for continuous variables and the χ2 test. Risk-adjusted Cox proportional-hazards model was employed to examine the relationship between IL-6 level and the endpoints of time to MACE or all-cause death, the latter adjusted for gender, age, body mass index (BMI), all other risk factors of CAD, including dyslipidemia, hypertension, diabetes, smoking status, family history of early CAD, existence of obstructive CAD and SIS. Incidences of events were compared by the log-rank test. Free survival curves of MACE or all-cause-death were generated across tertiles using multivariate Cox proportional-hazards model adjusted for the same set of parameters in each group of IL-6 tertile. CAD stenosis severity and SIS were evaluated across tertiles with relate to MACE by Cox proportional-hazards model adjusted for gender, age, diabetes, hypertension, dyslipidemia and family history of CAD. The assumption of the Cox proportional-hazards model was verified using Scaled Schoenfeld residuals. Hazard ratio (HR) and 95% confidence interval (CI) were determined by using the Cox model. A p < 0.05 was considered to be statistically significant.
Results
Baseline characteristics
Among 383 patients who without known CAD undergoing CCTA, IL-6 records were available for 303 patients (79.1%; Fig. 1). The baseline demographic, clinical and laboratory patient characteristics base on IL-6 tertiles are listed in Table 1. Several differences were observed across the tertiles. Comparing with patients with lowest IL-6, those with higher IL-6 were more commonly symptomatic. Patients with high IL-6 serum level displayed a higher rate of diabetes, hypertension and dyslipidemia compared with patients in lower IL-6 group. Furthermore, patients with the high IL-6 level exhibited significantly elevated rate of current smoking, higher baseline high sensitivity C-reactive protein (hs-CRP), LDL and lower HDL levels.
Extent, severity and plaque type of CAD
The extent and severity of CAD is showed in Table 2. Compared with patents with lowest IL-6, those with higher IL-6 displayed greater coronary plaque extent. For plaque severity, compared with patents with lower IL-6, those with higher IL-6 exhibited a greater obstructive CAD prevalence, as well as the obstructive CAD categories including 1-VD, 2-VD and 3-VD. The plaque type of CAD is shown in Table 3. Absence of plaque was frequently found in the lower IL-6 patients. Compared with patients in lower IL-6 patients, those with higher serum IL-6 had more prevalent of NCAP, CAP and MCAP.
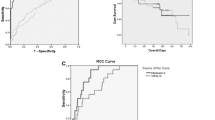
Rates and adjusted risk of MACE and all-cause death
After 3.0 ± 2.1 years of follow-up study, 28 subjects experienced MACE (9.24%). Incidence rate of MACE was significantly elevated in high IL-6 patients compared with those with lower IL-6. By unadjusted Cox model, MACE and all-cause death rates were found to be progressively increased with elevating IL-6 levels (both p < 0.0001 for trend). Using multivariable Cox proportional-hazards model, adjusted for gender, age, diabetes, hypertension, dyslipidemia, family history, smoking status, coronary stenosis ≥50% and SIS, patients with high IL-6 had higher risk of MACE than those with low IL-6 level subjects. After multivariate adjustment, HR was also found to be increased with elevating IL-6 levels (p < 0.0001 for trend). Furthermore, higher IL-6 was also associated with all-cause death (Table 4). Free survival curves also clearly showed increased MACE and all-cause death in patients with higher level of IL-6 (both p < 0.001; Fig. 2).
Risk of MACE and coronary plaque extent and severity
Table 5 demonstrated the results from Cox proportional-hazards model adjusted to risk for MACE by categories of SIS among IL-6 across tertiles. Compared with the lowest IL-6 patients with SIS of 0, highest IL-6 patients with SIS of 0 (HR 1.7, 95% CI 0.9–2.9, p < 0.01) exhibited increased risk of MACE. In the category of SIS 1–5, the MACE risk was higher than patients with SIS of 0 in all IL-6 tertiles. The risk among highest IL-6 level patients was much higher than low IL-6 groups (HR 3.0, 95% CI 2.1–4.2, p < 0.001). In the category of SIS > 5, the MACE risk was further elevated in all IL-6 tertiles. In the category of SIS 1–5, the MACE risk among highest IL-6 patients was much higher than low IL-6 groups (HR 4.2, 95% CI 3.2–5.9, p < 0.001).
Table 6 demonstrated the results from Cox proportional-hazards model adjusted to risk for MACE by categories of normal, non-obstructive, and obstructive CAD across all IL-6 tertiles. The risk of MACE among lowest IL-6 patients with non-obstructive CAD was higher than those with normal CCTA (HR 1.6, 95% CI 1.0–2.5, p < 0.01). This MACE risk was significantly elevated in highest IL-6 patients (HR 2.8, 95% CI 1.8–3.9, p < 0.001). Patients with obstructive CAD exhibited higher MACE rates than the lowest IL-6 patients with normal CCTA, regardless of their IL-6 levels (lowest IL-6: HR 2.7, 95% CI 1.8–3.9, p < 0.001; intermediate IL-6: HR 2.8, 95% CI 2.1–4.0, p < 0.001; highest IL-6: HR 4.3, 95% CI 3.0–5.8, p < 0.001).
Discussion
The main observation of our study are as following: (1) compared with patients of low IL-6, patients of higher IL-6 level exhibited significantly elevated MACE and all-cause death incidences; (2) adjusted for important covariates, high serum IL-6 level was strongly associated with increased incidences of MACE and all-cause death in patients without CAD history who underwent CCTA. To the best of our knowledge, it is the first report using CCTA in asymptomatic individuals to evaluate the correlations between the extent and severity of CAD, serum IL-6 levels, as well as the risks of MACE and all-cause death.
Inflammation plays a key role in the pathogenesis of atherosclerosis [19]. Elevated IL-6 level, an inflammation biomarker, has a relation to poor cardiovascular outcomes and IL-6 to be a potential for targeted drug therapy [20]. One of the mechanisms by which increased risk of CAD is thought to happen involves increased plaque vulnerability [21]. Beyond the role of triggering immunity in plaque deposition, a study also demonstrated the correlation between IL-6, impaired vasoreactivity and endothelial nitric oxide synthase inhibition in vitro [22]. IL-6 has also been implicated in the development of CHD, as blocking IL-6 receptor could alleviate systemic and articular inflammation [4], which was also consistent with a recent meta-analysis [10]. The above studies suggested that IL-6R may serve as a potential therapeutic target for the prevention and treatment of CHD. Our data also indicated that deceased patients had higher baseline serum IL-6 levels (data not shown), consistent with previous studies, suggesting that chronic inflammation may be involved in the pathogenesis and prognosis of atherosclerotic diseases. From the CCTA results, we were able to demonstrate that increased levels of IL-6 were correlated with elevated risk for the presence of any plaque of CAP, MCAP or NCAP. Furthermore, higher IL-6 levels were associated with greater extent and severity of CAD.
Previously studies demonstrated conflicting conclusions concerning the correlation between IL-6 and mortality. Among women with prevalent cardiovascular disease (CVD), those with higher serum levels of IL-6 had more than fourfold risk of death than patients with lower levels, but this correlation was absent among patients without CVD [23]. A study reported that TNF-α and CRP, but not IL-6, could serve as independent indicators of total mortality for male patients [24]. In addition, in elderly patients, serum IL-6 was also reported to be not associated with all-cause death [25, 26]. On the contrary, a great number of investigations have reported a positive correlation between serum IL-6 concentration and mortality, as well as between IL-6 and risk of CVD [3]. A study found that, compared to CRP, IL-6 was more strongly associated with all-cause death and CVD mortality [19]. In addition, long-term serum levels of IL-6 were found to be correlated with CHD [27]. In elderly patients with heart failure (HF), an increased level of IL-6 was reported to lead to higher mortality [28, 29]. In hemodialysis patients serum IL-6 was a stronger indicator of total and CVD mortality than CRP [30]. In patients with acute HF, serum IL-6 level was found to predict short and long-term mortality [28, 31]. Other studies have also indicated that increased serum IL-6 levels were useful for risk assessment of long-term CVD mortality [32]. The above conflicting studies may be due to limited sample size, heterogeneous populations and age of the participants in several of the studies. So, this situation may change as the follow up extends.
This study had several limitations. First, with relatively small sample population and incident cases, further investigations in a large number of clinical events are needed to confirm the present results. Second, high IL-6 may be attributed to inflammation caused by infection in some patients, however detailed information on inflammation sources and active infection were unavailable in the study. Third, because our current study included patients who underwent clinically indicated CCTA, it is questionable whether our present results can be generalized to larger population-based cohorts. Fourth, only Chinese patients were enrolled for this study, therefore future work with more diversified patient population should be considered. Finally, we only considered inflammatory diseases, but not other potential inflammation-associated factors including dietary habit.
Elevated serum IL-6 level was associated with long-term clinical outcome of patients without CAD history undergoing CCTA in the present study. Furthermore, the risk of MACE and all-cause death was elevated in the higher level IL-6 patients.
References
Sprague AH, Khalil RA (2009) Inflammatory cytokines in vascular dysfunction and vascular disease. Biochem Pharmacol 78:539–552. doi:10.1016/j.bcp.2009.04.029
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH (1997) Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 336:973–979. doi:10.1056/NEJM199704033361401
Li Y, Takemura G, Okada H, Miyata S, Maruyama R, Li L, Higuchi M, Minatoguchi S, Fujiwara T, Fujiwara H (2006) Reduction of inflammatory cytokine expression and oxidative damage by erythropoietin in chronic heart failure. Cardiovasc Res 71:684–694. doi:10.1016/j.cardiores.2006.06.003
Groot HE, Hartman MH, Gu YL, de Smet BJ, van den Heuvel AF, Lipsic E, van der Harst P (2015) Soluble interleukin 6 receptor levels are associated with reduced myocardial reperfusion after percutaneous coronary intervention for acute myocardial infarction. Cytokine 73:207–212. doi:10.1016/j.cyto.2015.02.004
Mendoza CE, Rosado MF, Bernal L (2001) The role of interleukin-6 in cases of cardiac myxoma. Clinical features, immunologic abnormalities, and a possible role in recurrence. Tex Heart Inst J 28:3–7
Lee JK, Bettencourt R, Brenner D, Le TA, Barrett-Connor E, Loomba R (2012) Association between serum interleukin-6 concentrations and mortality in older adults: the Rancho Bernardo study. PLoS ONE 7:e34218. doi:10.1371/journal.pone.0034218
Penninx BW, Kritchevsky SB, Yaffe K, Newman AB, Simonsick EM, Rubin S, Ferrucci L, Harris T, Pahor M (2003) Inflammatory markers and depressed mood in older persons: results from the health, aging and body composition study. Biol Psychiatry 54:566–572
Interleukin-6 Receptor Mendelian Randomisation Analysis, Swerdlow DI, Holmes MV, Kuchenbaecker KB, Engmann JE, Shah T, Sofat R, Guo Y, Chung C, Peasey A, Pfister R, Mooijaart SP, Ireland HA, Leusink M, Langenberg C, Li KW, Palmen J, Howard P, Cooper JA, Drenos F, Hardy J, Nalls MA, Li YR, Lowe G, Stewart M, Bielinski SJ, Peto J, Timpson NJ, Gallacher J, Dunlop M, Houlston R, Tomlinson I, Tzoulaki I, Luan J, Boer JM, Forouhi NG, Onland-Moret NC, van der Schouw YT, Schnabel RB, Hubacek JA, Kubinova R, Baceviciene M, Tamosiunas A, Pajak A, Topor-Madry R, Malyutina S, Baldassarre D, Sennblad B, Tremoli E, de Faire U, Ferrucci L, Bandenelli S, Tanaka T, Meschia JF, Singleton A, Navis G, Mateo Leach I, Bakker SJ, Gansevoort RT, Ford I, Epstein SE, Burnett MS, Devaney JM, Jukema JW, Westendorp RG, Jan de Borst G, van der Graaf Y, de Jong PA, Mailand-van der Zee AH, Klungel OH, de Boer A, Doevendans PA, Stephens JW, Eaton CB, Robinson JG, Manson JE, Fowkes FG, Frayling TM, Price JF, Whincup PH, Morris RW, Lawlor DA, Smith GD, Ben-Shlomo Y, Redline S, Lange LA, Kumari M, Wareham NJ, Verschuren WM, Benjamin EJ, Whittaker JC, Hamsten A, Dudbridge F, Delaney JA, Wong A, Kuh D, Hardy R, Castillo BA, Connolly JJ, van der Harst P, Brunner EJ, Marmot MG, Wassel CL, Humphries SE, Talmud PJ, Kivimaki M, Asselbergs FW, Voevoda M, Bobak M, Pikhart H, Wilson JG, Hakonarson H, Reiner AP, Keating BJ, Sattar N, Hingorani AD, Casas JP (2012) The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet 379:1214–1224. doi:10.1016/S0140-6736(12)60110-X
Collaboration IRGCERF, Sarwar N, Butterworth AS, Freitag DF, Gregson J, Willeit P, Gorman DN, Gao P, Saleheen D, Rendon A, Nelson CP, Braund PS, Hall AS, Chasman DI, Tybjaerg-Hansen A, Chambers JC, Benjamin EJ, Franks PW, Clarke R, Wilde AA, Trip MD, Steri M, Witteman JC, Qi L, van der Schoot CE, de Faire U, Erdmann J, Stringham HM, Koenig W, Rader DJ, Melzer D, Reich D, Psaty BM, Kleber ME, Panagiotakos DB, Willeit J, Wennberg P, Woodward M, Adamovic S, Rimm EB, Meade TW, Gillum RF, Shaffer JA, Hofman A, Onat A, Sundstrom J, Wassertheil-Smoller S, Mellstrom D, Gallacher J, Cushman M, Tracy RP, Kauhanen J, Karlsson M, Salonen JT, Wilhelmsen L, Amouyel P, Cantin B, Best LG, Ben-Shlomo Y, Manson JE, Davey-Smith G, de Bakker PI, O’Donnell CJ, Wilson JF, Wilson AG, Assimes TL, Jansson JO, Ohlsson C, Tivesten A, Ljunggren O, Reilly MP, Hamsten A, Ingelsson E, Cambien F, Hung J, Thomas GN, Boehnke M, Schunkert H, Asselbergs FW, Kastelein JJ, Gudnason V, Salomaa V, Harris TB, Kooner JS, Allin KH, Nordestgaard BG, Hopewell JC, Goodall AH, Ridker PM, Holm H, Watkins H, Ouwehand WH, Samani NJ, Kaptoge S, Di Angelantonio E, Harari O, Danesh J (2012) Interleukin-6 receptor pathways in coronary heart disease: a collaborative meta-analysis of 82 studies. Lancet 379:1205–1213. doi:10.1016/S0140-6736(11)61931-4
Gigante B, Strawbridge RJ, Velasquez IM, Golabkesh Z, Silveira A, Goel A, Baldassarre D, Veglia F, Tremoli E, Clarke R, Watkins H, Hamsten A, Humphries SE, de Faire U (2015) Analysis of the role of interleukin 6 receptor haplotypes in the regulation of circulating levels of inflammatory biomarkers and risk of coronary heart disease. PLoS ONE 10:e0119980. doi:10.1371/journal.pone.0119980
Forster O, Ansari AA, Sliwa K (2006) Current issues in the diagnosis and management of peripartum cardiomyopathy. Womens Health 2:587–596. doi:10.2217/17455057.2.4.587
Gitsioudis G, Katus HA, Korosoglou G (2014) Assessment of coronary artery disease using coronary computed tomography angiography and biochemical markers. World J Cardiol 6:663–670. doi:10.4330/wjc.v6.i7.663
Staniak HL, Bittencourt MS, Pickett C, Cahill M, Kassop D, Slim A, Blankstein R, Hulten E (2014) Coronary CT angiography for acute chest pain in the emergency department. J Cardiovasc Comput Tomogr 8:359–367. doi:10.1016/j.jcct.2014.08.001
Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, Lippolis NJ, Berman DS, Callister TQ (2007) Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 50:1161–1170. doi:10.1016/j.jacc.2007.03.067
Cesari M, Penninx BW, Newman AB, Kritchevsky SB, Nicklas BJ, Sutton-Tyrrell K, Tracy RP, Rubin SM, Harris TB, Pahor M (2003) Inflammatory markers and cardiovascular disease (the health, aging and body composition [health abc] study). Am J Cardiol 92:522–528
Goto K, Shiode N, Shirota K, Fukuda Y, Kitamura F, Tominaga K, Kato Y (2008) Impact of impaired renal function and diabetes on long-term prognosis in patients undergoing primary angioplasty for acute coronary syndrome. Intern Med 47:907–913
Staniak HL, Bittencourt MS, de Souza Santos I, Sharovsky R, Sabbag C, Goulart AC, Lotufo PA, Bensenor IM (2014) Association between psoriasis and coronary calcium score. Atherosclerosis 237:847–852. doi:10.1016/j.atherosclerosis.2014.11.004
Staniak HL, Salgado Filho W, Miname MH, Bensenor IM, Lotufo PA, Sharovsky R, Rochitte CE, Bittencourt MS, Santos RD (2014) Association between postprandial triglycerides and coronary artery disease detected by coronary computed tomography angiography. Atherosclerosis 233:381–386. doi:10.1016/j.atherosclerosis.2013.12.036
Sarojini A, Sai Ravi Shanker A, Anitha M (2013) Inflammatory markers-serum level of c-reactive protein, tumor necrotic factor-alpha, and interleukin-6 as predictors of outcome for peripartum cardiomyopathy. J Obstet Gynaecol India 63:234–239. doi:10.1007/s13224-013-0428-9
Zhou J, Chen X, Ye H, Peng P, Ba Y, Yang X, Huang X, Lu Y, Jiang X, Lian J, Duan S (2014) An association study between genetic polymorphism in the interleukin-6 receptor gene and coronary heart disease. Biomed Res Int. doi:10.1155/2014/504727
Clarke MC, Figg N, Maguire JJ, Davenport AP, Goddard M, Littlewood TD, Bennett MR (2006) Apoptosis of vascular smooth muscle cells induces features of plaque vulnerability in atherosclerosis. Nat Med 12:1075–1080. doi:10.1038/nm1459
Patterson CC, Smith AE, Yarnell JW, Rumley A, Ben-Shlomo Y, Lowe GD (2010) The associations of interleukin-6 (IL-6) and downstream inflammatory markers with risk of cardiovascular disease: the caerphilly study. Atherosclerosis 209:551–557. doi:10.1016/j.atherosclerosis.2009.09.030
Rao M, Guo D, Perianayagam MC, Tighiouart H, Jaber BL, Pereira BJ, Balakrishnan VS (2005) Plasma interleukin-6 predicts cardiovascular mortality in hemodialysis patients. Am J Kidney Dis 45:324–333
Tuomisto K, Jousilahti P, Sundvall J, Pajunen P, Salomaa V (2006) C-reactive protein, interleukin-6 and tumor necrosis factor alpha as predictors of incident coronary and cardiovascular events and total mortality. A population-based, prospective study. Thromb Haemost 95:511–518. doi:10.1160/TH05-08-0571
Arai Y, Takayama M, Gondo Y, Inagaki H, Yamamura K, Nakazawa S, Kojima T, Ebihara Y, Shimizu K, Masui Y, Kitagawa K, Takebayashi T, Hirose N (2008) Adipose endocrine function, insulin-like growth factor-1 axis, and exceptional survival beyond 100 years of age. J Gerontol A 63:1209–1218
Haugen E, Gan LM, Isic A, Skommevik T, Fu M (2008) Increased interleukin-6 but not tumour necrosis factor-alpha predicts mortality in the population of elderly heart failure patients. Exp Clin Cardiol 13:19–24
Zuo HP, Guo YY, Che L, Wu XZ (2016) Hypomethylation of interleukin-6 promoter is associated with the risk of coronary heart disease. Arq Bras Cardiol 107:131–136. doi:10.5935/abc.20160124
Haugen E, Tang MS, Isic A, Andersson B, Fu M (2008) TNFalpha antagonist upregulates interleukin-6 in rats with hypertensive heart failure. Int J Cardiol 130:64–68. doi:10.1016/j.ijcard.2007.08.047
Smart NA, Larsen AI, Le Maitre JP, Ferraz AS (2011) Effect of exercise training on interleukin-6, tumour necrosis factor alpha and functional capacity in heart failure. Cardiol Res Pract. doi:10.4061/2011/532620
Panichi V, Maggiore U, Taccola D, Migliori M, Rizza GM, Consani C, Bertini A, Sposini S, Perez-Garcia R, Rindi P, Palla R, Tetta C (2004) Interleukin-6 is a stronger predictor of total and cardiovascular mortality than C-reactive protein in haemodialysis patients. Nephrol Dial Transplant 19:1154–1160. doi:10.1093/ndt/gfh052
Li Y, Takemura G, Okada H, Miyata S, Esaki M, Maruyama R, Kanamori H, Li L, Ogino A, Misao Y, Khai NC, Mikami A, Minatoguchi S, Fujiwara T, Fujiwara H (2006) Treatment with granulocyte colony-stimulating factor ameliorates chronic heart failure. Lab Invest 86:32–44. doi:10.1038/labinvest.3700367
Ritschel VN, Seljeflot I, Arnesen H, Halvorsen S, Weiss T, Eritsland J, Andersen GO (2014) IL-6 signalling in patients with acute ST-elevation myocardial infarction. Results Immunol 4:8–13. doi:10.1016/j.rinim.2013.11.002
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Zhao, L., Wang, X. & Yang, Y. Association between interleukin-6 and the risk of cardiac events measured by coronary computed tomography angiography. Int J Cardiovasc Imaging 33, 1237–1244 (2017). https://doi.org/10.1007/s10554-017-1098-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1098-y