Abstract
The purpose of our study was to investigate the impact of temporal uniformity and adjustment by the contrast opacification enhancement in the aorta on the performance of transluminal attenuation gradient (TAG) for obstructive coronary artery disease. A total of 274 coronary arteries from 94 patients who underwent both multi- and single-beat scan using 128-slice scanner at the same time were enrolled. TAG and corrected coronary opacification (CCO) of both scan technique were compared against obstructive coronary arteries defined by diameter stenosis ≥50%. In per-vessel analysis, both TAG and CCO were slight but significantly different between multi- and single-beat scan in overall (−13.3 vs. −14.3 HU/10 mm; 0.31 vs. 0.38; p < 0.05, all). However, the difference was evident only in right coronary artery (p < 0.05) but not in left coronary arteries (p = NS). Correlation coefficient value are more than 0.8 for all coronary arteries (0.84) and each of the three vessels (RCA: 0.87, LAD: 0.84, LCX: 0.81) in TAG in single-beat versus multi-beat scans (p < 0.0001). Radiation exposure was significantly lower in single-beat scan compared to multi-beat scan (0.9 vs. 3.7 mSv, p < 0.001). TAGs of multi- and single beat scans well correlated each other in all coronary arteries and were not affected by temporal non-uniformity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with coronary artery disease (CAD), clinical benefit of coronary revascularization was associated with more favorable outcomes in patients with a significant amount of myocardial ischemia [1]. Coronary revascularization guided by physiological ischemia showed better clinical outcome compared to revascularization guided by anatomical stenosis [2]. Meanwhile, the yield of diagnostic invasive coronary angiography (ICA) for detection of coronary artery disease is not satisfactory [3]. Therefore non-invasive functional evaluation of coronary artery stenosis is highly warranted to reduce unfruitful ICA and to guide revascularization in a sagacious manner [4].
Coronary computed tomography angiography (CCTA) is increasingly used as a noninvasive diagnostic work-up and showed high sensitivity and negative predictive value in screening of CAD [5, 6]. However, the inherent limitation of anatomical imaging is moderate diagnostic performance for functionally significant stenosis which needs revascularization [7]. To overcome this limitation, myocardial perfusion imaging, non-invasive computational hemodynamics (FFR-CT), vessel-specific myocardial mass, and transluminal attenuation gradient (TAG) have been investigated to enable non-invasive functional assessment. Myocardial perfusion imaging is hampered by additional radiation exposure contrast burden [8, 9]. Non-invasive calculation of computational hemodynamics requires significant computational time, that at present can only be performed off-site [10]. Vessel-specific myocardial mass needs dedicated software module and depends on the quantitation of vessel luminal dimension [11–13]. On the other hand, TAG, which is an intraluminal attenuation gradient along the vascular axis that reflects contrast kinetics, is readily available from conventional CCTA image without additional radiation or long off-site computation [14–20].
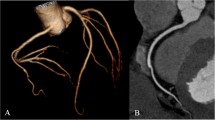
TAG has been validated in both animal and human studies against anatomical and functional stenosis [14–20]. TAG theoretically depends on the temporal uniformity of Z-axis coverage and the timing of acquisition with respect to the contrast enhancement curve in the CT image acquisition. Therefore, unlike TAG assessed from a 320-slice CT scanner with 16 cm width detector which enables isotemporal single-beat whole-heart image acquisition, TAG assessed from 64- to 256-slice CT scanner with 4–8 cm width detectors might be hampered from multi-beat image acquisition and lack of temporal uniformity. Adjustment with descending aortic opacification (corrected contrast opacification, CCO) or exclusion of nonlinear values caused by stented or calcified segment has been proposed but with mixed results [17, 20–22] (Fig. 1). Therefore the theoretical importance of the temporal uniformity warrants validation by direct comparison of multi-best scan with single-beat scan. We investigated the impact of temporal uniformity and the performance of TAG and CCO assessed from multi- and single-beat scan in the same patients.
Concept of TAG and TAG-CCO. Concept of transluminal attenuation gradient (TAG) and corrected coronary opacification (CCO) in single-beat (a) and multi-beat scan (b). To measure TAG, the mean Hounsfield Unit (HU) value is assessed from each region of interest (ROI, shown as red circles). TAG of vessel with significant stenosis is lower that TAG of vessel with insignificant stenosis. For the assessment of CCO, the quotient of the mean intraluminal HU of the normal-looking coronary segment and the descending aorta in the same axial plane was calculated in the intracoronary segment most proximal to stenosis and most distal to the stenosis in axial slices. Then CCO was defined as the difference between two quotients. CCO of vessel with significant stenosis is higher than CCO of vessel with insignificant stenosis
Methods
Patient population
From November 2009 to November 2014, we retrospectively enrolled patients who underwent CCTA of heart and thoracic aorta for non-urgent evaluation of known or suspected coronary artery disease, concomitant valvular, or aortic disease. Patients with acute coronary syndrome within 90 days, significant ventricular dysfunction with left ventricular (LV) ejection fraction ≤40% or aneurysm, history of coronary artery bypass graft surgery, and any coronary anomaly such as coronary artery aneurysm or ectasia were not included. This retrospective image-analysis study was approved by our institutional review board, and written informed consent was waived.
CT acquisition
CT scans were performed using a 128-slice DSCT system (SOMATOM Definition Flash; Siemens Healthcare) with 2 mm × 64 mm × 0.6 mm detector collimation and the z-axis flying focal spot technique, resulting in 2 × 128 sections. Metoprolol 50 mg was administered 1 h before the examination If the patient’s heart rate was >70/min. Nitroglycerin 0.4 mg was administered sublingually 1 min before scanning.
CT imaging consisted of coronary imaging using retrospective electrocardiography (ECG)-gated helical mode and aorta imaging using prospective ECG-gated high-pitch helical mode at the same time using 128-slice dual source CT (DSCT).
Multi-beat scan of coronary artery was dedicated standard-pitch coronary artery imaging with the full radiation dose window set at 68–78% of the R–R interval in patients with heart rates ≤65/min, and 200–400 msec after the R peak in patients with a heart rate >65/min. A reduced dose (4% of the dose during acquisition window) was used for the rest of the R–R interval to minimize the radiation dose. Acquisition direction was cranio-caudal. The typical interval between proximal and distal coronary artery was 6 to 8 s.
Single-beat scan of coronary artery was reconstructed from prospective ECG-gated high-pitch (pitch = 3.2–3.4) helical scan of aortic imaging with cardiac data acquisition window set at 60% of the R–R interval in patients with heart rates ≤65 bpm, and 30% of the R–R interval in patients with a heart rate >65 bpm. Acquisition was cranio-caudal from mid level of common carotid artery to proximal superficial femoral artery. In both acquisitions, 60 mL of iomeprol 400 (Bracco, Milan, Italia) was injected from antecubital vein followed by 30 mL of saline chaser at 4 mL/sec. The interval between proximal and distal coronary artery was less than 1 s.
The CT acquisition delay time was calculated as the time of peak contrast medium attenuation in a region of interest in the ascending aorta plus 11 s. Acquisition parameters of both scans were 2 × 64 × 0.6 mm detector collimation resulting in 2 × 128 × 0.6 mm sections, 280 ms gantry rotation time, and 100 kV tube voltage. A real-time tube current modulation was performed with 320 reference mAs according to the precise shape of patient’s body (CAREDose4D; Siemens Healthcare). The effective radiation dose was derived by multiplying the dose-length product by the conservative conversion coefficient (0.017 mSv/mGy/cm).
Image reconstruction and analysis
Each CT data were reconstructed according to the FOV of CCTA. The range of FOV was from 14\(\mathrm{ }\times \mathrm{ }\)14 to 18 \(\times \mathrm{ }\)18 cm according to the body size. Images were reconstructed using a soft kernel (B26f) with 0.6 mm slice thickness and 0.4 mm reconstruction increment.
The quality of images on a 4-point scale; poor, poor but can measure, good, excellent. Only images with good to excellent quality in both multi- and single-beats scan were enrolled. Coronary artery tree was evaluated according to the 17-segment model according to Society of Cardiovascular Computed Tomography (SCCT) guideline [23]. To establish the variation in contrast enhancement in the aorta, which affects the intracoronary contrast, the intra-aortic enhancement of aortic root at the same level of left main and descending thoracic aorta at the same level of posterior descending artery (PDA) level was assessed. Significantly obstructive coronary artery was defined by visually assessed diameter stenosis ≥50%.
TAG and CCO
TAG and CCO were assessed as described previously [15–18, 24]. In brief, cross-sectional images perpendicular to the vessel centerline were reconstructed for each major coronary artery. The contour of the region of interest and the vessel centerline were manually corrected if necessary. From the ostium to the distal level where the vessel cross-sectional area fell below 2.0 mm2, lumen cross-sectional area (mm2), mean diameter (mm), and luminal radiological attenuation (Hounsfield Unit, HU) were measured. The linear regression coefficient between intraluminal radiological attenuation (HU) and length from the ostium (mm) was calculated. TAG was defined by the change in HU per 10-mm vessel length. CCO was defined as the gradient of the quotient of the intracoronary luminal attenuation and thoracic aortic luminal attenuation [20, 21]. The attenuation, area, distance measurements were made manually in a 3D workstation (iNtuition, TeraRecon).
Statistical analysis
Analyses were done per-patient or per-vessel basis, as indicated below for each result. In per-patient analysis, the most severe stenosis or the longest vessel was selected. Data were expressed as median with 1st–3rd quartile range or number with percentage. Continuous variables between two scan techniques were compared using paired Wilcoxon signed rank test. Linear fit equations and Pearson correlation values were used for comparison of TAG in single-beat and multi-beat scans, for all coronary arteries and for each of the three vessels separately. A p value < 0.05 was considered statistically significant. R version 3.3 (R foundation) was used for computational analyses.
Results
Patients
A total of 110 CCTA cases were enrolled. After assessment of image quality analysis, 16 cases with poor quality were excluded. Further analysis was performed with 94 cases. Baseline clinical characteristics of patients are shown in Table 1. The median age of patients was 61 year with male gender in 69% of population.
Coronary CT angiography
Significant stenosis defined by DS ≥ 50% and DS ≥ 70% was found in 69 (25.2%) and 13 (4.7%) vessels, and 43 (45.7%) and 11 (11.7%) patients, respectively (Online Resource 1). Compared to multi-beat scan, single-beat scan images showed slightly but significantly shorter right coronary artery (RCA) length measurement (139 vs. 141 mm, p = 0.015) but not left anterior descending artery (LAD) or left circumflex artery (LCX). Single-beat scan also showed lower proximal aortic enhancement compared to multi-beat scan (479 vs. 492 HU, p = 0.002) but not distal aortic enhancement (p = NS). Median radiation exposure was significantly lower in single-beat scan compared to multi-beat scan (0.88 vs. 3.67 mSv, p < 0.001) (Online Resource 2).
TAG and CCO with multi- and single-beat scan
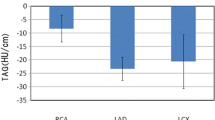
In per-vessel analysis, both TAG and CCO were significantly different between single-beat scan and multi-beat scan; TAG, −13.3 HU/10 mm (−20.2 to −6.6) versus −14.3 HU/10 mm (−21.4 to −7.9), p = 0.011; CCO, 0.31 (0.15–0.49) versus 0.38 (0.19–0.51), p < 0.001). In vessel-specific subgroup analysis, TAG and CCO was significantly different between two scan techniques in right coronary artery (RCA) (p < 0.01) but not in left anterior descending artery (LAD) or left circumflex artery (LCX) (p = NS). Per-patient analysis showed consistent results (Fig. 2; Table 2).
TAG and CCO between multi- and single-beat scan techniques. In per-vessel analysis, both TAG and CCO were significantly different between single-beat scan and multi-beat scan; TAG, −13.3 HU/10 mm (−20.2 to −6.6) versus −14.3 HU/10 mm (−21.4 to −7.9), p = 0.011; CCO, 0.31 (0.15–0.49) versus 0.38 (0.19–0.51), p < 0.001). However, the difference was evident only in right coronary artery (p < 0.05) but not in left coronary arteries (p = NS). *p < 0.05
TAG and CCO between non-obstructive and obstructive coronary artery, in both multi-beat and single-beat scan techniques
In both per-vessel and per-patient analysis, TAG showed significant difference between non-obstructive coronary artery and obstructive coronary artery irrespective of scan technique (p < 0.05, all). CCO was significantly different between non-obstructive coronary artery and obstructive coronary artery in RCA (p < 0.05, all). CCO was numerically different but statistically not consistent in LAD and LCX (Fig. 3; Table 3).
TAG and CCO in normal or obstructive coronary artery. TAG showed significant difference between non-obstructive coronary artery and obstructive coronary artery irrespective of scan technique (p < 0.05, all). CCO was significantly different between non-obstructive coronary artery and obstructive coronary artery in RCA (p < 0.05, all). CCO was numerically different but statistically not consistent in LAD and LCX. *p < 0.05, per-vessel analysis.
TAG in single-beat versus TAG in multi-beat scans
Correlation coefficient value are more than 0.8 for all coronary arteries (0.84) and each of the three vessels (RCA: 0.87, LAD: 0.84, LCX: 0.81) in TAG in single-beat versus multi-beat scans (p < 0.0001) (Fig. 4).
Discussion
This study is the first of its kind that directly compared TAG and CCO derived from multi- and single-beat scan. The performance of TAG for obstructive vessel was not affected by temporal uniformity or correction with thoracic aorta opacification (CCO). Our findings support the validity of TAG in detection of significant stenosis regardless of scan techniques.
TAG is based on the conceptual decline of contrast enhancement in vessel axial direction which reflects contrast kinetics. Therefore axial isochronism of image acquisition as well as a lot of factors including the time-density curve of intravascular contrast delivery, vessel-specific flow velocity, anatomical location, or length of vessel might affect the measured TAG value. These factors are too complex to be adjusted completely [25]. We focused on the temporal uniformity which depends on the CT scanning technique.
Only RCA was affected by the temporal uniformity of scan technique. RCA is the longest vessel but has slowest flow velocity [26]. RCA is curved and has lower ostium height compared to left ostium which results in shortest Z-axis compared LAD or LCX [27]. RCA is also known to have faster motion particulary in its mid-section, which nay also affect the temporal uniformity and result in statistically significant differences between single and multi-beat techniques when compared to the other coronaries. These distinctive characteristics of RCA can be explained by innate anatomical findings. The main body of RCA does not directly supply LV myocardium and functions as a conduit to posterior descending artery (PDA) and posterolateral branch without giving large branch and tapering, unlike LAD or LCX.
CCO is a adjustment of TAG with additional dephasing by thoracic aorta opacification but without vascular length information. CCO was not different between two scan techniques and also was not better than TAG for prediction of obstructive vessel. The Z-axis distance between ostium and distal end is not so different among three major coronary arteries. Thoracic aortic blood flow is pulsatile and much faster than the coronary artery [28], but a recent 64-slice CT study also showed very close time-density curve of thoracic aorta and mid segment of coronary artery [29]. Therefore thoracic aortic enhancement seems to have no major role in the analysis of TAG [17].
The followings are major limitations of this study. Our result is limited by inherent selection bias of retrospective analysis. Most patients had at least moderate degree of valvular stenosis or insufficiency, although LV dimension and systolic function was mostly normal range. TAG and CCO were compared to non-invasively assessed diameter stenosis ≥50%. However additional invasive coronary angiography or physiological assessment might be have little role considering our aim of study and the number of vessels analyzed.
Conclusions
TAGs of multi- and single beat scans well correlated each other in all coronary arteries and were not affected by temporal non-uniformity using 128-DSCT scanner. Therefore TAGs derived from both scan techniques with or without dephasing by thoracic aorta opacification might be utilized comparably.
Abbreviations
- CAD:
-
Coronary artery disease
- CCO:
-
Corrected contrast opacification
- CCTA:
-
Coronary computed tomography angiography
- HR:
-
Heart rate
- LAD:
-
Left anterior descending coronary artery
- LCX:
-
Left circumflex artery
- LM:
-
Left main coronary artery
- RCA:
-
Right coronary artery
- TAG:
-
Transluminal attenuation gradient
References
Hachamovitch R, Hayes SW, Friedman JD et al (2003) Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 107(23):2900–2907
De Bruyne B, Fearon WF, Pijls NH et al (2014) Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 371(13):1208–1217
Patel MR, Peterson ED, Dai D et al (2010) Low diagnostic yield of elective coronary angiography. N Engl J Med 362(10):886–895
Shreibati JB, Baker LC, Hlatky MA (2011) Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 306(19):2128–2136
Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R et al (2007) Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology 244(2):419–428
Hamon M, Biondi-Zoccai GG, Malagutti P et al (2006) Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol 48(9):1896–1910
Meijboom WB, Van Mieghem CA, van Pelt N et al (2008) Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol 52(8):636–643
Kim SM, Choi JH, Chang SA et al (2013) Detection of ischaemic myocardial lesions with coronary CT angiography and adenosine-stress dynamic perfusion imaging using a 128-slice dual-source CT: diagnostic performance in comparison with cardiac MRI. Br J Radiol 86(1032):20130481
Kim SM, Choi JH, Chang SA et al (2013) Additional value of adenosine-stress dynamic CT myocardial perfusion imaging in the reclassification of severity of coronary artery stenosis at coronary CT angiography. Clin Radiol 68(12):e659–e668
Min JK, Leipsic J, Pencina MJ et al (2012) Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 308(12):1237–1245
Kim HY, Lim HS, Doh JH et al (2016) Physiological severity of coronary artery stenosis depends on the amount of myocardial mass subtended by the coronary artery. JACC 9(15):1548–1560
Kang SJ, Yang DH, Kweon J et al (2016) Better diagnosis of functionally significant intermediate sized narrowings using intravascular ultrasound-minimal lumen area and coronary computed tomographic angiography-based myocardial segmentation. Am J Cardiol 117(8):1282–1288
Kurata A, Kono A, Sakamoto T et al (2015) Quantification of the myocardial area at risk using coronary CT angiography and voronoi algorithm-based myocardial segmentation. Eur Radiol 25(1):49–57
Wong DT, Ko BS, Cameron JD et al (2014) Comparison of diagnostic accuracy of combined assessment using adenosine stress computed tomography perfusion + computed tomography angiography with transluminal attenuation gradient + computed tomography angiography against invasive fractional flow reserve. J Am Coll Cardiol 63(18):1904–1912
Choi JH, Kim EK, Kim SM et al (2014) Noninvasive evaluation of coronary collateral arterial flow by coronary computed tomographic angiography. Circ Cardiovasc Imaging 7(3):482–490
Yoon YE, Choi JH, Kim JH et al (2012) Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC 5(11):1088–1096
Choi JH, Koo BK, Yoon YE et al (2012) Diagnostic performance of intracoronary gradient-based methods by coronary computed tomography angiography for the evaluation of physiologically significant coronary artery stenoses: a validation study with fractional flow reserve. Eur Heart J Cardiovasc Imaging 13(12):1001–1007
Choi JH, Min JK, Labounty TM et al (2011) Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC 4(11):1149–1157
Steigner ML, Mitsouras D, Whitmore AG et al (2010) Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging 3(2):179–186
Stuijfzand WJ, Danad I, Raijmakers PG et al (2014) Additional value of transluminal attenuation gradient in CT angiography to predict hemodynamic significance of coronary artery stenosis. JACC 7(4):374–386
Chow BJ, Kass M, Gagne O et al (2011) Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol 57(11):1280–1288
Wong DT, Ko BS, Cameron JD et al. (2014) Comparison of diagnostic accuracy of combined assessment using adenosine stress CT perfusion (CTP) + computed tomography angiography (CTA) with transluminal attenuation gradient (TAG320) + CTA against invasive fractional flow reserve (FFR). J Am Coll Cardiol 63:1904–1912
Raff GL, Abidov A, Achenbach S et al (2009) SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 3(2):122–136
Choi JH, Kim EK, Kim SM et al. (2015) Non-invasive discrimination of coronary chronic total occlusion and subtotal occlusion by coronary computed tomography angiography. JACC 8:1143–1153
Bae KT (2010) Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 256(1):32–61
Gibson CM, Cannon CP, Daley WL et al (1996) TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 93(5):879–888
Knight J, Kurtcuoglu V, Muffly K et al (2009) Ex vivo and in vivo coronary ostial locations in humans. Surg Radiol Anat 31(8):597–604
Itskovich VV, Kraft KA, Fei DY (2001) Rapid aortic wave velocity measurement with MR imaging. Radiology 219(2):551–557
Bovenschulte H, Krug B, Schneider T et al (2013) CT coronary angiography: coronary CT-flow quantification supplements morphological stenosis analysis. Eur J Radiol 82(4):608–616
Funding
Authors received no funding for this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Authors report no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Informed consent
The written informed consent was waived.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, H.J., Kim, S.M., Choi, JH. et al. Influence of scan technique on intracoronary transluminal attenuation gradient in coronary CT angiography using 128-slice dual source CT: multi-beat versus one-beat scan. Int J Cardiovasc Imaging 33, 937–946 (2017). https://doi.org/10.1007/s10554-017-1078-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1078-2