Abstract
Cardiovascular magnetic resonance (CMR) imaging is often considered the reference method to assess cardiac tumors. However, little data exists concerning the effectiveness of CMR for the accurate diagnosis of cardiac masses. We sought to understand the diagnostic value of CMR for evaluation of suspected cardiac mass. A total of 249 consecutive CMR cases performed at a single center from January 2005 to June 2013 for evaluation of masses found on echocardiography or computed tomography (CT) were included. All the clinical data and imaging features of these patients were retrospectively reviewed and medical records were verified for follow up care. More than half of the patients referred for evaluation of masses found at echocardiography or CT were found to have no evidence of mass by CMR. CMR correctly differentiated between thrombus and myxoma in 88.4 % cases. Malignant masses were accurately diagnosed on CMR. However, CMR missed or misdiagnosed a few cases of benign masses. Diagnosing cardiac masses remains an important use for imaging, despite technical difficulties with current imaging modalities. CMR can play a key role in confirming presence or absence of a mass. Additionally, in the presence of a mass, CMR can provide accurate differentiation of pseudomasses, benign and malignant masses. However, the limitations of CMR must be recognized.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac masses are rare, with an autopsy incidence ranging from 0.001 to 0.030 % [1]. However, even benign cardiac masses can cause clinical symptoms due to mass effect or embolism. Most cardiac masses are first detected on transthoracic or transesophageal echocardiograms (TTE or TEE) and some on chest computed tomography (CT) performed for other indications. Cardiovascular magnetic resonance (CMR) imaging is the preferred method for evaluation of cardiac masses detected by other modalities due to its multiplanar capabilities, superior spatial resolution, and ability to characterize tissue [2–4]. Differentiating benign from malignant masses is crucial as an accurate diagnosis can affect the work up and management of the patient [2, 3]. To date, very few studies have evaluated the effectiveness of CMR in aiding the diagnosis of masses found by echocardiography or CT, or have discussed the limitations of CMR for this use [5]. In this work, we perform a retrospective single-center analysis of 249 patients to evaluate the effectiveness of CMR for the accurate diagnosis of cardiac masses.
Methods
A retrospective review of CMR exams performed from January 2005 to June 2013 at University of Pennslyvania was conducted with waiver of consent, which was approved by our institutional review board. A total of 249 consecutive patients who underwent CMR for evaluation of mass found on echocardiography or CT were included. Most of the patients were referred to our hospital from outside physicians exclusively for CMR. All the clinical data and imaging features for this cohort of patients were retrospectively reviewed and medical records were verified for follow up care, including any available pathology or follow up imaging.
CMR imaging was performed on 1.5 Tesla scanners (Avanto or Espree, Siemens, Germany) using a 16 channel body surface array anteriorly and portions of a 12 channel spine array posteriorly, with electrocardiographic gating. Either 0.20 mmol/kg of gadiodamide (Omniscan, GE Healthcare, Little Chalfont, UK), 0.20 mmol/kg gadopentate (Magnevist, Bayer HealthCare,Germany) or 0.14 mmol/kg gadobenate (Multihance, Bracco Imaging, USA) was administered. All patients were imaged following the same protocol—after localizers, serial axial steady-state free precession (SSFP) sections were obtained through the entire chest, followed by half Fourier acquisition single shot turbo spin echo (HASTE) axial and short axis imaging covering the entire heart. SSFP cines in the vertical long axis, four chamber, and short axis planes were followed by rest perfusion with dynamic contrast enhanced 2D gradient echo imaging focusing on the identified mass if present. Finally, delayed inversion recovery prepped gradient echo sequences were performed 12–15 min after the contrast injection. The main components of CMR evaluation included (1) confirming the presence or absence of mass, (2) identifying any anatomical variants or benign findings simulating mass on echocardiography, (3) in the presence of a mass on CMR, characterizing the lesion as thrombus, benign, or malignant based upon imaging features.
Descriptive data is reported as percentages and medians as appropriate. A Student’s t test was used to detect significant differences in patient characteristics. P < 0.05 is considered statistically significant. All statistical analyses were performed on STATA 13 (StatCorp, Texas).
Results
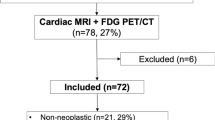
Of the 249 patients evaluated for cardiac mass, 96.4 % were referred with suspected mass on TTE or TEE, nine patients (3.6 %) were referred because of mass suspected on CT. The mean age of the patients was 55.9 ± 17.9 years and 43 % were male. A total of 56.2 % (140/249) patients referred with a suspicion of mass did not have a mass identified by CMR. Of these, 35.3 % (88/249) patients were found to have no evidence of mass or other finding corresponding to the 87 cases of echocardiogram abnormality and 1 case of CT abnormality, although one TTE confirmed mass was missed by CMR. The characteristics of the 249 patients separated into mass and no mass groups are shown in Table 1. Significant differences are present in the histories of thrombus and malignancy between the groups. Of these 140 patients, 65 patients had a median of 24 months of follow up with an interquartile range of 11 and 48 months. Of the 109 patients found to have a mass, 24 were lost to follow up and could not be included in further analysis. Of the remaining 85 with masses identified, 66 patients (including the previous mentioned case misdiagnosed as fibroelastoma but verified to be inflammation at surgery) had features of either a benign mass or thrombus and were managed accordingly(Fig. 1). CMR correctly characterized thrombus versus benign mass in 89.4 % (59/66) of cases (Fig. 1). Malignant masses were accurately diagnosed on CMR 100 % of the time (19/19) with confirmation by biopsy, surgery and/or positron emission tomography (PET).
Anatomic variants or benign findings
Of the 140 patients where no mass was found by CMR, 52 had anatomical variants/benign findings on CMR (Table 2). This is 20.9 % (52/249) of total patients (not including one case misdiagnosed as fibroelastoma by CMR, shown at surgery to represent chronic inflammation). The most common was lipomatous hypertrophy of interatrial septum (17/52). Prominent crista terminalis, prominent epicardial fat, mitral valve thickening/calcification, increased RV trabeculations or prominent moderator band, and aneurysm of interatrial septum are other common findings.
Thrombi
Twenty nine patients were diagnosed as having thrombus by CMR (5 referred from CT), corresponding to 34.1 % (29/85) of all confirmed masses. Twenty eight cases were verified as thrombus (16 males, 12 females, age range 26–79 years, mean age 48.0 years) in follow-up as evidenced by resolution or decrease in size with anticoagulation. One patient who did not have resolution went to surgery and a myxoma was found. This was a very small mass (0.6 × 0.8 cm) in the left atrial appendage and could only be seen as a non-enhancing defect on first-pass perfusion by CMR.
The incidence of thrombi was much higher in the right atrium (RA) compared to the left atrium (LA) in our study. Seventeen patients had thrombus in the RA, one in the LA, eight in the left ventricle (LV), and two in the right ventricle (RV). Of 17 RA thrombi, 13 cases (76.5 %, 13/17) were related to the presence of a catheter or history of a catheter used for chemotherapy, 2 cases were with a history of deep venous thrombus or pulmonary embolism, one case had a history of tricuspid repair with a hypercoagulable state and one case had a history of pulmonary hypertension with severe RA dilation. LV thrombi were seen in dilated cardiomyopathy (n = 3), myocardial infarction (n = 2), and cardiac sarcoid (n = 2, one of whom also had a history of myocardial infarction). One gastric carcinoma patient was found to have an LV apical thrombus.
Benign masses
In our cohort, 37/85 (43.5 %) patients were diagnosed with benign masses by CMR (3 referred from CT) (14 males, 23 females, age range 25–86 years, average age 59.3 years). Of these, 17 were managed conservatively and 20 underwent surgery.
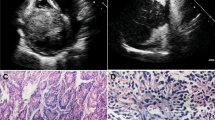
Thirteen of 15 masses diagnosed as myxoma by CMR underwent surgery and two were managed conservatively. Post-operative pathology reports revealed 10/13 to be myxomas (Table 3), 2 were found to be thrombi and one was a hemangioma. These confirmed myxoma cases (including the one diagnosed as thrombus described earlier) occurred in patients ranging from 22 to 81 years old, and were seen predominantly in females (2 males, 9 female, age range 22–81 years, average age 52.7 years). Seven myxomas were found in the LA and four in the RV; the sizes ranged from 0.6 to 7 cm. Ten myxomas diagnosed by CMR showed mild patchy or peripheral delayed enhancement (Table 3). In the conservatively managed group, the two cases diagnosed as myxoma on CMR were placed on anticoagulation therapy with follow-up imaging showing resolution of masses, suggesting that they were thrombi. Of the 4 misdiagnosed thrombus cases (two found in surgery, two had resolution on follow-up with anticoagulation), all had mild peripheral delayed enhancement on CMR imaging . One example is shown in Fig. 2 compared to a correctly diagnosed myxoma. Thus, 12.5 % (4/32) of proven thrombi in our study demonstrated mild delayed enhancement. Three out of four were found in the RA and one in a massively dilated LA. Two out of the three in the RA has a history of line placement. Considering all the confirmed thrombi and myxoma cases, CMR correctly differentiated between them in 88.4 % (38/43) cases.
Comparison of a thrombus misdiagnosed as a myxoma and a correctly diagnosed myxoma by CMR. Images a–e A mass is seen in the right atrium suggestive of myxoma, later proven a thrombus. Images f–j A mass diagnosed as myxoma in right ventricle, confirmed pathologically. Images a and f, steady-state free precession images showing the mass with higher signal intensity than the myocardium and lower than the blood pool. Images b and g, half Fourier acquisition single shot turbo spin echo images showed higher signal intensity in myxoma (g) than thrombus (b). Images c and h, rest perfusion images showed mobile thrombus appear to be perfused while less mobile myxoma was not. Images d and i, magnitude images of late gadolinium enhancement (LGE) imaging showed mild enhancement for both. Images e and j, LGE imaging with phase sensitive inversion recovery showing that the central enhancement in thrombus was no longer present, but the peripheral enhancement persist (e) and similar findings were present in the myxoma (j)
The mass verified to be hemangioma at surgery was at the junction of the RA and inferior vena cava. It had intermediate signal on SSFP sequences and high signal on HASTE sequences with early perfusion and significant late gadolinium enhancement (LGE).
Three lipomas present along the interatrial septum were surgically excised and one present in the sub-endocardium of the LV was managed conservatively. Two fibroelastomas were diagnosed by CMR on the aortic valve and both went to surgery, one proved to be fibroelastoma, the other showed chronic inflammatory changes. One hemangioma and one calcified amorphous tumor diagnosed by CMR were also verified by surgery.
Malignant masses
In patients with masses, 22.1 % (19/86; 11 males, 8 females, age range 27–93 years, average age 57.3 years) were diagnosed as malignant, of which 12 were primary and 7 were metastatic lesions. Primary malignancies included lymphoma (n = 5), sarcoma (n = 4), leukemic chloroma (n = 1), myxofibrosarcoma (n = 1) and malignant histiocytosis (n = 1). Metastatic lesions were from melanoma (n = 4), lung carcinoma (n = 1), metastatic neuroendocrine carcinoid (n = 1) and gastric carcinoma (n = 1).
The five cases of proven lymphoma all showed heterogeneous enhancing masses involving predominantly the right side of the heart. Bulky masses were noted in three cases and pericardial effusions in two cases. Tumors encased vessels including the right coronary artery (n = 3), superior vena cava (n = 2) and inferior vena cava (n = 1), however the vessel lumen remained patent in all cases.
Nine patients underwent cardiac biopsy, 4 patients had biopsies of other tissues including lymph nodes and liver and 1 patient underwent cardiac surgery. Of the 7 patients diagnosed as having cardiac metastases, 5 underwent PET for confirmation, one had a biopsy of a hepatic metastasis and one underwent cardiac surgery. Nine patients had follow up CMR 3 months to 1 year after initiation of therapy. Five masses showed decreases in size, two remained stable, one showed complete resolution and one had progressed.
CMR missed case
During follow-up, one benign mass, which was missed on CMR, was confirmed to be present by TTE. In this case, CMR showed pulmonic valve stenosis with a prominent jet in the pulmonary artery, which obscured a small mass in the main pulmonary artery (Fig. 3). This small mass was unchanged on multiple subsequent follow-up TTE studies.
The case with pulmonary mass missed by CMR due to turbulence in the pulmonary artery (PA). a 2D echocardiography image of mass (thick arrow) in the PA, located above pulmonary valve (PV) (thin arrow). b Systolic phase of the cine CMR showed pulmonary stenosis with prominent turbulence in the PA. c Diastolic phase of cine CMR image of main PA showed persistent flow turbulence. No mass was visible. RVOT right ventricular outflow tract. RV right ventricle. RA right atrium
Discussion
Although the incidence of cardiac masses is quite low [6, 7], CMR offers invaluable assessment, given its ability to assess each chamber of the heart in motion, the relationship of the heart to the adjacent structures, and superior tissue characterization. We have shown that CMR is excellent in excluding masses and differentiating between benign findings and malignant masses. However, limitations of CMR do exist and some cases could be missed or misdiagnosed.
Echocardiography is the primary initial mode of detection and evaluation of cardiac masses, however TTE can be limited due to poor acoustic windows and lack of soft tissue characterization [8]. The Eustachian valve at the junction of the IVC and RA [9], the Coumadin ridge (tissue between the left superior pulmonary vein and LA) [10], and a prominent moderator band in the RV [11] can all simulate a mass at echocardiography. Benign variants like lipomatous hypertrophy of the interatrial septum and aneurysms of the interatrial septum can appear as masses [12, 13]. In our study, the most common benign variant was lipomatous hypertrophy of the interatrial septum. The multiplanar capabilities and soft tissue characterization ability of CMR helps to identify these variants correctly.
Thrombus is one of the most common cardiac masses, representing 37.6 % of all confirmed masses in our study. Of these, 62.5 % were present in the RA (including the 4 misdiagnosed as myxomas) and 75 % of these RA thrombi were associated with presence or history of line placement. LV thrombi are associated with poor myocardial contractility and low ejection fraction, such as adherence to infarcted and scarred myocardium [14]. LA thrombi, predominantly in the form of LA appendage thrombi associated with atrial fibrillation are usually assessed by TEE and their low frequency in our patient population may represent a referral bias.
Thrombi have traditionally been described as hypointense masses adherent to chamber walls [15], without enhancement on either early post contrast or delayed imaging, although cases of findings of peripheral enhancement in chronic thrombus have been reported [16, 17]. In our study, 12.5 % of proven thrombi demonstrated mild delayed enhancement. Early imaging after contrast administration may aide the differentiation of myxoma versus thrombus [18], but it was not routinely performed during the study period at our institution.
Myxomas are the most common benign cardiac tumors; they are found predominantly in women, with reported occurrence of 75 % in the LA, 20 % in the RA, and 5 % in the ventricles [19]. We have found a similar gender distribution in myxomas, but a different distribution in locations with 63.6 % in the LA and 36.4 % in the RV; in contrast to thrombus, which were predominantly found in the RA (62.5 %) and LV (25 %) in our study. Myxomas are typically pedunculated and show high signal intensity on T2-weighted imaging, thought to be due to high water content in myxomatous tissue. On SSFP cine sequences, they appear hyperintense compared to myocardium and hypointense compared to the blood pool, which allows good visualization of mobility. Heterogeneous signal may be seen on other sequences depending on the presence of fibrosis and the fraction of fibrotic tissue. Myxomas in our study had similar CMR features to prior reports [4]. The case that was misdiagnosed as hemangioma showed early perfusion and more significant LGE. These indicated a highly vascularized mass, which should be an important feature to differentiate hemangioma from myxoma.
Other benign masses commonly encountered are lipomas and fibroelastomas. Lipomas are well defined, encapsulated tumors that follow the signal intensity of fat on the chest wall and appear hypointense on fat suppressed sequences. Lipomatous hypertrophy appears as thickening and is not encapsulated. Fibroelastomas are pedunculated tumors, generally smaller than 1.5 cm, that are usually associated with valves. They do not show early contrast enhancement on perfusion imaging, but show uniform delayed enhancement. The common differentials are vegetation or thrombus on valves, which do not show delayed enhancement [4, 20, 21]. However, the case of chronic inflammation on the aortic valve in our study was misdiagnosed as fibroelastoma due to its delayed enhancement.
Primary cardiac malignancies include lymphomas, sarcomas and mesothelial tumors. Large, bulky masses with vascular encasement without obliteration of lumen are typical features of lymphoma [2, 22]. Sarcomas usually present as bulky masses with irregular margins and invasive features involving one or more chambers; they may show heterogeneous enhancement due to the presence of necrosis or hemorrhage. These tumors may be associated with pericardial effusions and metastasis to mediasternal nodes, lungs and other organs. Secondary metastasis to the heart occurs frequently from melanoma, lung, breast and gastric carcinomas [23]. They may show intramural or pericardial involvement and superior or inferior vena cava metastases [24]. Signal characteristics and contrast enhancement features are variable in metastatic lesions [3]. In our study, we were able to make correct diagnoses on all primary cardiac and metastatic malignancies using the combination of these features, with confirmation by histopathology or PET imaging.
One of the most important findings of this study is the demonstration of the limitations of CMR. CMR evaluation can be difficult in general in the presence of artifacts (for example, valve prosthesis and intracardiac leads) and arrhythmias (due to irregular motion and difficult cardiac gating). Evaluation of small masses adjacent to flow disturbances and associated with moving valves can be challenging as well, as shown in our case of missed small pulmonary artery mass in a patient with pulmonic stenosis.
Our study has several limitations. Lack of a gold standard diagnosis is a limitation for the diagnosis of thrombus. Resolution after anticoagulation served as a surrogate endpoint for the diagnosis of thrombus in our study, but it is possible that the masses were not there in the first place or decreased in size without treatment. Furthermore, a number of no mass and anatomic variants cases had no additional follow-up or further imaging studies (although one case with persistence on TTE was recognized). Therefore, we do not know the true positive or negative predictive value of CMR. In addition, referral bias has to be recognized as not all patients with masses found on echocardiography underwent CMR.
Conclusion
Diagnosing cardiac masses remains an important application for imaging, despite challenges for diagnosis using current imaging modalities. CMR can play a key role in making an accurate diagnosis and for confirming the presence of a mass or anatomic variants that may simulate masses. In the presence of a mass, CMR can provide accurate differentiation of benign and malignant lesions. However, the limitations of CMR must be recognized such as evaluating a small mass in turbulent flow.
References
Butany J, Nair V, Naseemuddin A, Nair GM, Catton C, Yau T (2005) Cardiac tumours: diagnosis and management. Lancet Oncol 6(4):219–228. doi:10.1016/S1470-2045(05)70093-0
Braggion-Santos MF, Koenigkam-Santos M, Teixeira SR, Volpe GJ, Trad HS, Schmidt A (2013) Magnetic resonance imaging evaluation of cardiac masses. Arq Bras Cardiol 101(3):263–272. doi:10.5935/abc.20130150
Fussen S, De Boeck BW, Zellweger MJ, Bremerich J, Goetschalckx K, Zuber M, Buser PT (2011) Cardiovascular magnetic resonance imaging for diagnosis and clinical management of suspected cardiac masses and tumours. Eur Heart J 32(12):1551–1560. doi:10.1093/eurheartj/ehr104
Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S (2013) MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology 268(1):26–43. doi:10.1148/radiol.13121239
Gulati G, Sharma S, Kothari SS, Juneja R, Saxena A, Talwar KK (2004) Comparison of echo and MRI in the imaging evaluation of intracardiac masses. Cardiovasc Intervent Radiol 27(5):459–469. doi:10.1007/s00270-004-0123-4
Lam KY, Dickens P, Chan AC (1993) Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med 117(10):1027–1031
Butany J, Leong SW, Carmichael K, Komeda M (2005) A 30-year analysis of cardiac neoplasms at autopsy. Can J Cardiol 21(8):675–680
Buckley O, Madan R, Kwong R, Rybicki FJ, Hunsaker A (2011) Cardiac masses, part 1: imaging strategies and technical considerations. AJR Am J Roentgenol 197(5):W837–W841. doi:10.2214/AJR.10.7260
Carson W, Chiu SS (1998) Image in cardiovascular medicine. Eustachian valve mimicking intracardiac mass. Circulation 97(21):2188
Gupta S, Plein S, Greenwood JP (2009) The Coumadin Ridge: an important example of a left atrial pseudotumour demonstrated by cardiovascular magnetic resonance imaging. J Radiol Case Reports 3(9):1–5. doi:10.3941/jrcr.v3i9.210
Mitta SR (2012) Moderator band wrongly interpreted as RV mass. J Assoc Phys India 60:42
Zarauza MJ, Alonso F, Hidalgo M, Hernando JP, Oliva MJ, Zueco J, Martin Duran R, Ochoteco A (1993) Lipomatous hypertrophy of the interatrial septum simulating an atrial mass in a patient with a pulmonary embolism: its diagnosis by transesophageal echocardiography and percutaneous biopsy. Rev Esp Cardiol 46(11):761–764
Castillo JA, Vilacosta I, Iniguez A, San Roman JA, Zamorano JL, Almeria C, Sanchez-Harguindey L (1993) A large aneurysm of the interatrial septum simulating an atrial mass. Its identification by transesophageal echocardiography. Rev Esp Cardiol 46(10):677–679
Ward TJ, Kadoch MA, Jacobi AH, Lopez PP, Salvo JS, Cham MD (2013) Magnetic resonance imaging of benign cardiac masses: a pictorial essay. J Clin Imaging Sci 3:34. doi:10.4103/2156-7514.117458
Jungehulsing M, Sechtem U, Theissen P, Hilger HH, Schicha H (1992) Left ventricular thrombi: evaluation with spin-echo and gradient-echo MR imaging. Radiology 182(1):225–229. doi:10.1148/radiology.182.1.1727287
Mollet NR, Dymarkowski S, Volders W, Wathiong J, Herbots L, Rademakers FE, Bogaert J (2002) Visualization of ventricular thrombi with contrast-enhanced magnetic resonance imaging in patients with ischemic heart disease. Circulation 106(23):2873–2876
Paydarfar D, Krieger D, Dib N, Blair RH, Pastore JO, Stetz JJ Jr, Symes JF (2001) In vivo magnetic resonance imaging and surgical histopathology of intracardiac masses: distinct features of subacute thrombi. Cardiology 95(1):40–47
Hoey ET, Mankad K, Puppala S, Gopalan D, Sivananthan MU (2009) MRI and CT appearances of cardiac tumours in adults. Clin Radiol 64(12):1214–1230. doi:10.1016/j.crad.2009.09.002
Grebenc ML, Rosado de Christenson ML, Burke AP, Green CE, Galvin JR (2000) Primary cardiac and pericardial neoplasms: radiologic-pathologic correlation. Radiographics 20 (4):1073–1103; quiz 1110–1071, 1112. doi:10.1148/radiographics.20.4.g00jl081073
Wintersperger BJ, Becker CR, Gulbins H, Knez A, Bruening R, Heuck A, Reiser MF (2000) Tumors of the cardiac valves: imaging findings in magnetic resonance imaging, electron beam computed tomography, and echocardiography. Eur Radiol 10(3):443–449. doi:10.1007/s003300050073
Vallurupalli S, Hayes K, Bhatti S (2014) Ventricular papillary fibroelastoma. J Am Coll Cardiol 63(20):2170. doi:10.1016/j.jacc.2013.12.060
Rogowitz E, Babiker HM, Krishnadasan R, Jokerst C, Miller TP, Bookman M (2013) Heart of lymphoma: primary mediastinal large B-cell lymphoma with endomyocardial involvement. Case Reports Oncol Med 2013:814291. doi:10.1155/2013/814291
Roberts WC (2001) Neoplasms involving the heart their simulators and adverse consequences of their therapy. Proceedings 14(4):358–376
Goldberg AD, Blankstein R, Padera RF (2013) Tumors metastatic to the heart. Circulation 128(16):1790–1794. doi:10.1161/CIRCULATIONAHA.112.000790
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Roja Tumma declares that she has no conflict of interest. Author Wei Dong declares that she has no conflict of interest. Author Jing Wang declares that she has no conflict of interest. Author Harold Litt declares that he has no conflict of interest. Author Yuchi Han declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived from individual participants included in the study for retrospective review of existing clinical data by the institutional review board.
Additional information
Roja Tumma and Wei Dong have contributed equally.
Rights and permissions
About this article
Cite this article
Tumma, R., Dong, W., Wang, J. et al. Evaluation of cardiac masses by CMR—strengths and pitfalls: a tertiary center experience. Int J Cardiovasc Imaging 32, 913–920 (2016). https://doi.org/10.1007/s10554-016-0845-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0845-9