Abstract
Accurate assessment of pulmonary capillary wedge pressure (PCWP) is essential for physicians to effectively manage patients with acute decompensated heart failure. The ratio of early transmittal velocity to tissue Doppler mitral annular early diastolic velocity (E/E′) is used to estimate PCWP noninvasively in a wide range of cardiac patients. However, it remains contentious as to whether mitral E/E′ is a reliable predictor of PCWP. In the present study, acute heart failure patients were divided into two groups on the basis of left ventricular (LV) systolic function: those with preserved ejection fraction (HFpEF) and those with reduced ejection fraction (HFrEF). The usefulness of mitral E/E′ in estimating PCWP was compared between the two groups. Fifty consecutive patients who were admitted with acute decompensated heart failure and underwent both right-sided cardiac catheterization and transthoracic echocardiography during hospitalization were analyzed retrospectively. Pearson’s correlation was used to evaluate associations between Doppler parameters and PCWP. E/E′ was positively correlated with PCWP (r = 0.56, P = 0.01) in the heart failure with preserved ejection fraction group. However, no significant relationship was observed between PCWP and mitral E/E′ (P = 0.85) in the heart failure with reduced ejection fraction group. There were no significant correlations between any of the conventional parameters considered (LVEF, left atrial dimension, E/A, IVRT, and DT) with PCWP in either group. In conclusion, mitral E/E′ is useful for estimating PCWP in patients with acute heart failure with preserved ejection fraction but may not in those with reduced ejection fraction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessing pulmonary capillary wedge pressure (PCWP) is vital in determining the therapeutic strategy for patients with acute decompensated heart failure [1, 2]. Right-sided cardiac catheterization allows direct measurement of PCWP; however, there has been a reduction in hemodynamic assessments via pulmonary artery catheters because of the invasive nature of this technique. Echocardiography plays a crucial role in the management of acute heart failure because it is a noninvasive bedside tool that can be used to determine abnormalities in cardiac structure and performance. In addition, transmitral flow velocities and other Doppler variables are used as noninvasive estimates of intracardiac filling pressures, despite having some limitations. Indeed, the ratio of early transmitral velocity to tissue Doppler mitral annular early diastolic velocity (E/E′) has been used to estimate PCWP in a wide range of cardiac patients [3–7]. However, the results of previous studies into the relationship between mitral E/E′ and PCWP are contentious. For example, several studies have reported that E/E′ correlates well with PCWP in systolic and diastolic heart failure [3, 8, 9], whereas, others have not found any correlation between mitral E/E′ and PCWP in either advanced systolic dysfunction or healthy volunteers [10, 11]. Therefore, assessing the diagnostic usefulness of mitral E/E′ in estimating PCWP is an important topic for research.
Recent studies have reported that heart failure with preserved ejection fraction (HFpEF) accounts for nearly half of all heart failure cases [12, 13]. Although HFpEF is currently an important cause of morbidity and mortality, the pathophysiological differences between HFpEF and heart failure with reduced ejection fraction (HFrEF) remain unclear.
In the present study, patients admitted for acute decompensated heart failure were divided into two groups, namely HFpEF and HFrEF, on the basis of left ventricular (LV) systolic function, and the diagnostic usefulness of mitral E/E′ in assessing PCWP was compared between the two groups.
Methods
Study population
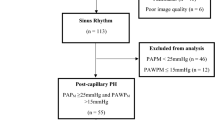
Fifty consecutive patients who had been admitted to Kyorin University Hospital between April 2010 and January 2013 for acute decompensated heart failure and who underwent both right-sided cardiac catheterization and transthoracic echocardiography during hospitalization were evaluated retrospectively. The study exclusion criteria were mitral valve replacement, mitral valve repair, and constrictive pericarditis. A past history of hypertension, dyslipidemia, or diabetes mellitus was determined from patient interviews regarding past health checks, diagnoses made by family doctors, and/or the use of medications for these conditions. This study was approved by the institutional Ethics Review Board of Kyorin University School of Medicine, Japan.
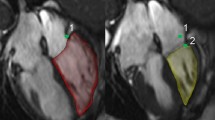
Echocardiography
All patients were examined by transthoracic echocardiography. Conventional measurements (two-dimensional, M-mode, pulsed Doppler, color flow imaging) were made in the parasternal and apical views. LV ejection fraction (LVEF) was determined using the modified biplane Simpson’s method [14]. Patients with LVEF ≥ 50 % were classified as having HFpEF, whereas those with LVEF ≤ 50 % were classified as having HFrEF. The peak velocities of early (E) and late (A) mitral flow, and the deceleration time of the E wave (DT) were measured using pulsed-wave Doppler with the sample volume at the tip of the mitral valve leaflets. Pulsed-wave Tissue Doppler Imaging (TDI) was applied to the apical four-chamber view to determine the early (E′) and late (A′) velocities. The peak early diastolic myocardial velocities at both the septal and lateral annuli were measured and averaged to calculate mean early velocity (E′).
Hemodynamic study
All patients underwent right-sided cardiac catheterization. Mean PCWP was measured with a balloon-tipped pulmonary artery catheter connected to a fluid-filled transducer. The wedge position was verified by fluoroscopy and phasic changes in pressure waveform. Averaged values of three consecutive beats during end-expiratory apnea were used for analysis.
Statistical analysis
All data are expressed as the mean ± standard deviation (SD) for continuous data and as a ratio for categorical data. All statistical analyses were performed using Minitab version 16 (Minitab Inc., State College, PA, USA). Continuous variables were compared between the HFpEF and HFrEF groups using unpaired t tests, whereas categorical variables were compared using Chi squared tests or Fisher’s exact tests as appropriate. Pearson’s correlation was used to evaluate the correlations between Doppler parameters and PCWP. P < 0.05 was considered significant.
Results
The baseline characteristics of the study subjects are summarized in Table 1. Mean patient age was 65 ± 16 years, and 36 (72 %) were men. Mean plasma B-type natriuretic peptide (BNP) concentrations were 995 ± 829 pg/mL. The prevalence of hypertension, dyslipidemia, and diabetes was 56, 36, and 38 %, respectively. Of the entire study cohort, 32 % had HFpEF and 68 % had HFrEF. The results of comparative analyses between the HFpEF (EF ≥ 50) and HFrEF (EF < 50) groups are also given in Table 1. There were no significant differences between the groups in terms of age, gender, height, weight, creatinine, BNP, systolic blood pressure, diastolic blood pressure, heart rate, and the prevalence of hypertension, dyslipidemia, diabetes mellitus, dilated cardiomyopathy, coronary artery disease, acute myocardial infarction, atrial fibrillation/flutter, cardiac resynchronization therapy, or pacemaker use. Hemoglobin was significantly lower in the HFpEF compared with HFrEF group (P < 0.05).
Measured PCWP and conventional echocardiographic measurements in the HFpEF and HFrEF groups are summarized in Table 2. The length of time between echocardiographic assessment and invasive PCWP measurement did not differ significantly between the two groups. There was no significant difference in measured PCWP between the HFpEF and HFrEF groups, but LVEF was significantly higher and E/A was significantly lower in the HFpEF than HFrEF group (P < 0.05). There were no significant differences in left atrial dimensions, isovolumic relaxation time (IVRT), or DT between the two groups.
There was a positive correlation between mitral E/E′ and measured PCWP (r = 0.56, P = 0.01) in the HFpEF group (Fig. 1A), but not in the HFrEF group (P = 0.85; Fig. 1B).
Scatter plot of correlations between the ratio of the peak transmitral E velocity to the peak early diastolic velocity of the mitral annulus (E/E′) and the measured pulmonary capillary wedge pressure (PCWP) in heart failure patients with (A) preserved ejection fraction and (B) reduced ejection fraction
The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of E/E′ > 10 for measured PCWP > 15 mmHg are shown in Table 3. In the HFpEF group, E/E′ > 10 had a sensitivity of 71 %, specificity of 56 %, PPV of 56 %, and NPV of 71 % for detecting measured PCWP > 15 mmHg. On the other hand, E/E′ > 10 had a sensitivity of 71 %, specificity of 18 %, PPV of 46 %, and NPV of 38 % for detecting measured PCWP > 15 mmHg in the HFrEF group.
Results of correlation analyses between measured PCWP and other conventional Doppler measurements are given in Table 4. There was no significant correlation between any of the conventional parameters considered (LVEF, left atrial dimension, E/A, IVRT, and DT) and measured PCWP in either of the two groups (Table 4).
We further derived a calculated PCWP using a previously published formula: PCWP = 17 + (5.3 × E/A) − (0.11 × IVRT) [15] and compared it with the measured PCWP. Ten patients with atrial fibrillation/flutter were excluded (HFpEF, 4; HFrEF, 6); thus, 40 patients were included in the analysis (HFpEF, 12; HFrEF, 28). There was no significant correlation between the calculated and measured PCWP in either the HFpEF or HFrEF group (Fig. 2). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of calculated PCWP > 15 mmHg for measured PCWP > 15 mmHg are shown in Table 5. In the HFpEF group, calculated PCWP > 15 mmHg had a sensitivity of 20 %, specificity of 86 %, PPV of 50 %, and NPV of 60 % for detecting measured PCWP > 15 mmHg. On the other hand, calculated PCWP > 15 mmHg had a sensitivity of 47 %, specificity of 69 %, PPV of 64 %, and NPV of 53 % for detecting measured PCWP > 15 mmHg in the HFrEF group.
Discussion
In the present study, we report that E/E′ is a more reliable predictor of PCWP in patients with HFpEF than in those with HFrEF. We were not able to identify a direct correlation between PCWP and E/E′ in patients with HFrEF.
The results of previous studies into the relationship between mitral E/E′ and PCWP are contentious, with some studies showing good correlations between E/E′ and PCWP in systolic and diastolic heart failure [3, 8, 9], but others failing to find any correlation between mitral E/E′ and PCWP in either advanced systolic dysfunction or healthy volunteers [10, 11]. These discrepancies may be related to the different clinical situations in these studies. Careful interpretation of each study is needed to evaluate this complicated index. In the present study, a low proportion of subjects were taking a renin-angiotensin system inhibitor (RASI) or beta blocker before admission. This finding could be related to the high proportion of patients in the present study presenting with de novo acute decompensated heart failure. We focused on patients admitted with acute decompensated heart failure in the present study. HFpEF currently accounts for approximately 50 % of heart failure cases and is an important cause of morbidity and mortality [12, 13]. Updated strategies for the diagnosis and treatment of HFpEF are crucial because of the epidemiological evolution towards a predominance of HFpEF. In the present study, E/E′ was significantly correlated with PCWP in patients with HFpEF.
Despite the controversy regarding the reliability of the relationship between E/E′ and PCWP, E/E′ is generally accepted as a noninvasive method to estimate PCWP in a variety of clinical conditions, including systolic heart failure. Of note, the aim of the present study was to compare the diagnostic utility of E/E′ for the assessment of PCWP between patients with HFpEF and HFrEF. Although we were not able to identify a significant correlation between E/E′ and PCWP in patients with HFrEF, this does not rule out the usefulness of E/E′ because the present study does have several limitations (see below). Similarly, Mullens et al. [11] reported that they were unable to identify a direct correlation between E/E′ and PCWP in decompensated patients with advanced systolic heart failure and speculated that patients with advanced systolic heart failure often had severe LV fibrosis and impaired cardiac output, which could restrict systolic and subsequent early diastolic mitral annular motion so that the relationship between left atrial driving pressure (E) and LV relaxation kinetics (E′) within the LV could become defective [11]. This could explain why, in the present study, the diagnostic usefulness of mitral E/E′ in estimating PCWP was superior in patients with HFpEF than in those with HFrEF. However, further studies are needed to evaluate this heterogeneity more precisely.
The present retrospective study has several limitations. First, the number of patients who underwent right-sided cardiac catheterization was small, despite the relatively large number of patients who were admitted for acute heart failure, because of the invasive nature of the technique. Thus, there was only a relatively small number of patients available for evaluation and so the power of the study to detect clinical correlations may be limited. Second, the length of time between echocardiographic assessment and invasive measurements may also limit the accuracy of our interpretation. Finally, other parameters that could influence the relationship between Doppler variables and PCWP, such as left atrial volume, left atrial strain, and pulmonary venous flow, were not evaluated in the present study. However, the Doppler parameters analyzed in this study are representative of the data obtained in most echocardiographic laboratories.
In conclusion, there is a good correlation between E/E′ and PCWP in patients admitted with HFpEF. However, E/E′ may not reflect PCWP accurately in patients with reduced ejection fraction. All available information, including other Doppler variables, chamber dimensions, and systolic function, should be considered when evaluating individual patients.
References
Nieminen MS, Böhm M, Cowie MR et al (2005) Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J 26:384–416
Weintraub NL, Collins SP, Pang PS et al (2010) Acute heart failure syndromes: emergency department presentation, treatment, and disposition: current approaches and future aims: a scientific statement from the American Heart Association. Circulation 122:1975–1996
Ommen SR, Nishimura RA, Appleton CP et al (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures : a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193
Oh JK, Park S-J, Nagueh SF (2011) Established and novel clinical applications of diastolic function assessment by echocardiography. Circ Cardiovasc Imaging 4:444–455
Nagueh SF, Mikati I, Kopelen HA et al (1998) DOPPLER estimation of left ventricular filling pressure in sinus tachycardia : a new application of tissue Doppler imaging. Circulation 98:1644–1650
Sohn DW, Song JM, Zo JH et al (1999) Mitral annulus velocity in the evaluation of left ventricular diastolic function in atrial fibrillation. J Am Soc Echocardiogr 12:927–931
Bruch C, Grude M, Müller J et al (2005) Usefulness of tissue Doppler imaging for estimation of left ventricular filling pressures in patients with systolic and diastolic heart failure. Am J Cardiol 95:892–895
Dokainish H, Zoghbi WA, Lakkis NM et al (2004) Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation 109:2432–2439
Firstenberg MS, Levine BD, Garcia MJ et al (2000) Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Coll Cardiol 36:1664–1669
Mullens W, Borowski AG, Curtin RJ et al (2009) Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation 119:62–70
Owan TE, Hodge DO, Herges RM et al (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355:251–259
Udelson JE (2011) Heart failure with preserved ejection fraction. Circulation 124:e540–e543
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiograph. J Am Soc Echocardiogr 18:1440–1463
Nagueh SF, Kopelen HA, Zoghbi WA (1995) Feasibility and accuracy of Doppler echocardiographic estimation of pulmonary artery occlusive pressure in the intensive care unit. Am J Cardiol 75:1256–1262
Acknowledgments
The authors thank Ms. Keiko Nishizawa for data collection. This work was supported, in part, by a Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (KAKENHI 26461086; to K. Matsushita).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Matsushita, K., Minamishima, T., Goda, A. et al. Comparison of the reliability of E/E′ to estimate pulmonary capillary wedge pressure in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction. Int J Cardiovasc Imaging 31, 1497–1502 (2015). https://doi.org/10.1007/s10554-015-0718-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0718-7