Abstract
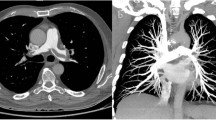
While lowering the radiation dose using a reduced tube potential (kVp) strategy for CT pulmonary angiography (CTPA) maintains accuracy for pulmonary embolism detection, there is no data regarding the effect of increased noise from lower kVp on both the accuracy of lung and mediastinum lesion detection in the same patient cohort. This study compares the accuracy and diagnostic confidence of lung nodules and enlarged mediastinal lymph nodes detection between low and standard kVp CTPA. The study cohort included 272 CTPA studies acquired at low kVp and 274 studies at standard kVp. Each patient had a routine chest CT acquired within 60 days of the CTPA that served as a reference standard for lung and mediastinum lesions. In additional to the evaluation of image quality, two radiologists independently interpreted lung nodules and mediastinal lymph nodes on CTPA and recorded confidence level for each interpretation. Multivariate models assessed effect of kVp settings on diagnostic accuracy and confidence level in interpretation. Low kVp CTPAs had higher image noise. A significant decrease in the confidence levels for evaluation of mediastinal lymph nodes was observed at low kVp by one of two readers, although there was no significant correlation between accuracy of interpretation and kVp settings for lung and mediastinum lesion detection (adjusted odds ratios = 0.67–1.22, p values >0.2). While increased image noise may decrease the diagnostic confidence of the radiologist, the detection of lung nodules and enlarged mediastinal lymph nodes was not compromised. Referring clinicians can expect that lower radiation dose CTPA answers questions related to lungs and mediastinum.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patient and overall population radiation exposure has increased significantly since multi-detector computed tomography (MDCT) has become mainstream for clinical diagnoses such as pulmonary embolism (PE). The additional radiation has provided diagnostic confidence since pulmonary artery filling defects are directly visualized, other important diagnoses (e.g. lymph node enlargement) are seen, and a clearly normal study is reassuring. However, as radiation concerns have escalated, clinicians have been charged with ordering studies only when appropriate, and radiologists have been charged with lowering the exposure for those studies that are appropriate.
This project focuses on lower radiation dose CT pulmonary angiography (CTPA) images; a highly impactful way to lower the MDCT photon flux is to decrease the X-ray CT tube potential, measured as the peak kiloVoltage (kVp) [1, 2]. This strategy has gained acceptance because while the images have more overall noise [3–5], the lower kVp does not compromise the iodine enhanced signal in the pulmonary artery and the accuracy of PE detection [1–4, 6–10]. However, the same accuracy in detecting lung nodules and mediastinal lesions, that are common findings on CTPA [11–15], using low kVp techniques, has not been systematically studied. If lower radiation dose compromises assessment of findings in lung or mediastinum, one potential implication will be the need for additional CT imaging to confirm suspected findings. Hence, the purpose of this study is to evaluate the effect of lower radiation dose CTPA images achieved by a reduced kVp on the detection and diagnostic confidence of lung nodules and enlarged mediastinal lymph nodes compared to standard dose CTPA.
Methods
Patient selection
The institutional human research committee approved this HIPAA-compliant retrospective study; informed consent was waived. Searching picture archiving communication systems (PACS) at a single, large, urban teaching hospital identified 5,816 consecutive CTPA studies performed between January 2008 and April 2010. This included patients scanned at standard radiation dose, based on higher kVp protocols (120–130 kVp) and those scanned after January 1, 2009 when the department adopted a change to weight-based low kVp techniques (80 kVp for patients weighing <80 kg and 100 or 110 kVp for those weighing ≥80 kg).
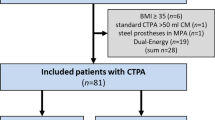
A total of 600 CTPA studies (300 low kVp plus 300 standard kVp, both of which were equally divided (n = 150) into <80 and ≥80 kg weight groups (Fig. 1) were randomly assembled from the 5,816 CTPA studies based on the criteria that cohort patients underwent additional chest CT imaging that was not a CTPA within 60 days of the CTPA. As detailed below, each of these studies was independently re-read for all imaging findings and served as a reference standard for the lung and mediastinum findings detected by CTPA studies. Fifty-four of the 600 patients were excluded from the analysis because the radiation dose could not be confirmed from the radiology records. Thus, the final population included 546 CTPA examinations stratified into four subpopulations.
CT acquisition
All 546 CTPA examinations used 16-, 64- and 128 slice scanners of the same manufacture (Emotion, Definition/Sensation 64/Definition AS/Definition AS+, Siemens Healthcare, Erlangen. Germany) [16, 17] with standard imaging protocols (“Appendix”). The Dose Length Product (DLP) and average volume CT dose index (CTDIvol) were recorded from each CT scanner’s output as indexes of radiation exposure.
Clinically indicated non-CTPA chest CT scans evaluated as a reference for the findings detected by CTPA examinations included 517 studies (201 non-contrast and 316 contrast-enhanced chest CT scans); 25 chest CT studies were used as reference for 2 or more CTPA examinations. Details of the chest CT acquisition are described in the “Appendix”.
CTPA subjective image quality analysis
All images were anonymized and evaluated on a PACS workstation (Centricity, GE Healthcare, IL) identical to those used for clinical interpretation. Two thoracic radiologists with 8 and 6 years experience in thoracic imaging independently reviewed all 546 CTPA examinations without knowledge of the CT parameters. To simulate routine clinical interpretation, each reader individually adjusted window width/level to optimize the image quality for each study. Image quality was assessed using a 4-point scale in two areas: quality of contrast opacification (1-non diagnostic, 2-limited, only diagnostic in central pulmonary arteries, 3-grainy but no difficulty with diagnosis at all levels of the pulmonary arteries, and 4-excellent contrast opacification with no limitations) and image noise (1-non diagnostic, 2-interpretation possible, 3-minimal noise but diagnosis confident, and 4-no noise).
CTPA findings
The same two readers independently interpreted clinical findings on CTPA studies: presence of PE, presence of solid lung nodule/mass >5 mm in diameter, solid lung nodules ≤5 mm in diameter, ground glass nodules, and mediastinal lymph nodes >1 cm in short-axis diameter. Readers also recorded their confidence level for each interpretation using a 3-point scale (1-not confident, 2-fairly confident but some ambivalence, and 3-very confident).
Evaluation of reference chest CT examinations
Reference chest CT studies were reviewed by a third thoracic radiologist with 20 years of experience in thoracic imaging and without knowledge of the findings of the CTPA evaluations. Studies were evaluated for presence of solid lung nodule/mass >5 mm in diameter, solid lung nodules ≤5 mm in diameter, ground glass nodules, and mediastinal lymph nodes >1 cm in short-axis diameter. A forth radiologist with 6 years of experience reviewed official CT reports to determine findings at time of clinical interpretation. Final interpretation of each reference chest CT examination was determined after adjudication, and these data were used as a reference standard of each lung finding and enlarged mediastinal lymph node detected on the CTPA images.
Objective image quality analysis
The forth radiologist measured the vascular attenuation and image noise on CTPA: mean hounsfield unite (HU) values within a circular region of interest (ROI) were recorded from the left pulmonary arterial tree or on the right if obstructive PE or atelectasis in left lung. Background noise was defined as the standard deviation (SD) of the CT density HU in air. Background signal was measured using the pectoral muscle. The signal-to-noise ratio (SNR) was calculated as mean HU in the pulmonary artery divided by background noise, and CNR was calculated as mean HU in the pulmonary artery minus background signal, divided by the background noise.
Statistical analysis
Characteristics between different kVp groups were compared using unpaired Student’s t test, Chi square test, and Wilcoxon rank-sum test, as appropriate. Inter-observer agreement was assessed by Kappa test. Accuracy (the fraction of true positive and true negative cases) of each reader’s interpretation of the CTPA study was calculated using the findings from the chest CT as reference standard. Accuracy of interpretation and confidence level was compared between low and standard kVp settings using Chi square test.
Multivariate logistic/ordered logistic regression models were fitted to evaluate the effect of the kVp settings on the accuracy of interpretation and confidence level, while controlling for age, gender, body weight, time difference between the CTPA and reference chest CT, contrast versus non-contrast enhanced reference chest CT, tube current, and five different types of scanner (Emotion/Definition/Sensation 64/Definition AS/Definition AS+, Siemens Healthcare, Erlangen, Germany, details in Appendix) used for the CTPA study.
Subgroup/sensitivity analyses
Because accuracy of the detection of enlarged mediastinal lymph nodes can be significantly affected by the use of iodinated contrast media, we added the subgroup analysis using CTPA studies for which the reference chest CT was contrast-enhanced (n = 316).
Of the 546 patients, body mass index (BMI) was available in 333 and in this sub-cohort (Fig. 1), the secondary analyses were performed to evaluate the feasibility of BMI-based low kVp protocol with a cutoff of 25 kg/m2 (i.e., 80 kVp for patients with <25 kg/m2 and 100/110 kVp for those with ≥25 kg/m2). The secondary analyses used the same methods as the index study where the patients were separated according to body weight.
For sensitivity analysis, we included the three different scanner types regarding the number of detectors (16, 64, or 128 detectors) as a covariate in the regression model, instead of the five scanner categories. All statistical analyses were performed on STATA version 11.2 (Stata Corp., College Station, TX).
Results
Patient demographics did not significantly differ between low and standard kVp groups, for both weight cohorts. Both DLP and CTDIvol were significantly higher for those patients imaged at the standard kVp (Table 1).
CTPA subjective image quality analysis
At both weight groups, inter-reader agreements were moderate to good for both contrast opacification (kappa = 0.59–0.66) and image noise (kappa = 0.57–0.69). There was no significant difference in contrast opacification scores between low and standard kVp groups, whereas low kVp images had significantly inferior image noise scores) (Table 1).
CTPA image findings
Among the 546 CTPA examinations, 80 studies (14.7 %) were positive for PE, with a similar positivity rate between low and standard radiation dose groups (Table 1). Inter-reader agreement of confidence level of CTPA interpretation was low (kappa = 0.00–0.26) and thus the analysis of confidence level was performed separately for reader 1 and 2. Images acquired at the standard kVp tended to have higher mean scores for the confidence level (i.e., more confident in interpretation) compared to the low kVp; this tendency was more obvious for reader 2 and in the patients <80 kg (Table 2). Multivariate ordered logistic regression showed a significant decrease in confidence level at low kVp for enlarged mediastinal lymph nodes interpreted by reader 2, while reader 1 had no significant association between the confidence level and kVp settings, for each finding (Table 3).
Evaluation of reference chest CT examinations
Median time difference between the CTPA examination and reference chest CT was 14.8 days (interquartile range: 7–29 days); 59.7 % of the reference chest CTs were performed before CTPAs (Table 1).
In univariate analysis, low kVp tended to result in lower accuracy for reader 2 regarding small (≤5 mm) solid lung nodule detection in the <80 kg group and ground glass nodule detection in the ≥80 kg group (Table 4). However, the multivariate analysis did not show a significant association between low kVp and a lower diagnostic accuracy for either reader (Table 3).
Objective image quality analysis
The image noise was higher at low kVp settings for both weight groups, but the difference was statistically significant in only the low weight group (Table 1). The SNR and CNR did not significantly differ between low and standard kVp groups for both weight groups.
Subgroup/sensitivity analyses
The subgroup analysis using CTPA studies with a contrast-enhanced reference chest CT showed the same results as those from the main analyses; a significant decrease in confidence level at low kVp for mediastinal lymph nodal detection was observed at the multivariate analyses for the reader 2 (coefficient = −2.91, p < 0.001), while reader 1 had no significant association between the confidence level and kVp settings. Accuracy of mediastinal lymph nodal detection was not affected by the kVp settings (adjusted odds ratios = 0.85, p = 0.628 for reader 1 and 0.99, p = 0.969 for reader 2).
Analysis using BMI < 25 kg/m2 as a cutoff (Fig. 1) between 80 kVp and 100/110 kVp showed qualitatively the same results as those using an 80 kg cutoff; reader 2 had a significantly decreased confidence for enlarged mediastinal lymph node detection (coefficient = −1.97, p < 0.001); the multivariate analyses did not prove an association between low kVp and lower accuracy of interpretation; lower kVp increased the background noise (32.0 ± 13.2 HU vs. 20.6 ± 6.3 HU, p < 0.001) and CT number in the main pulmonary artery (532.0 ± 194.2 HU vs. 361.3 ± 127.8 HU, p < 0.001) only for patients with a BMI < 25 kg/m2 patient group; there was no significant difference in SNR and in CNR for both BMI groups.
The sensitivity analysis including the three different scanner types in the multivariate models also showed the same results as those from the main analyses; a significant decrease in confidence level at low kVp for mediastinal lymph nodal detection was observed for reader 2 (coefficient = −2.33, p < 0.001).
Discussion
Diagnostic errors are an important cause of preventable adverse events which can directly cause patient morbidity and mortality, and include both missed and delayed diagnosis. Schiff et al. [18] analyzed 583 physician reported errors; two of the top three most common missed or delayed diagnoses included PE and lung cancer, both of which can be detected on CTPA images. Lowering the radiation dose using a reduced kVp strategy is validated for pulmonary arty filling defects [7, 19] and allows a reduction in the injected iodine mass [6] that is desired for patients who may require repeat studies who have multiple comorbidities such as cardiac and renal dysfunction. These benefits have generated enthusiasm for lowering the kVp of CTPA images, but for the transition to be clinically viable, data is needed to confirm that images acquired at a low kVp CTPA meet the overall clinical need in patient assessment. Hall et al. [11] reported that clinically relevant non-PE findings were identified in 24 % (136/589) of CTPA studies, a 2.5-fold increase when compared with the detection rate of PE (9 %). While previous non-CTPA studies showed an uncompromised accuracy of lung nodule detection on low-dose CT images [20, 21], findings were not confirmed on low kVp CTPA images. Moreover, no data is available regarding the detectability of mediastinal findings on a low-dose CT. While subjective image quality scores for mediastinum on 100 kVp CTPA images have been reported as comparative to the scores on 140 kVp CTPA images [4], this study provides the initial data regarding the diagnostic accuracy of mediastinal findings based on a reference standard imaging. The prevalence of malignancy is known to be high among those who have acute PE [22], and thus accurate diagnosis of lung nodules and/or mediastinal lymph nodes is critical to patient care. The current population had a prevalence of PE, lung nodules, and lymph nodes that is similar to previous reports[11, 23–25]. Our results suggest that the detection of lung nodules and enlarged mediastinal lymph nodes was not significantly compromised when lowering the radiation exposure with lower kVp settings: 80 kVp for small patients (<80 kg or BMI < 25 kg/m2) and 100/110 kVp for large patients (≥80 kg or BMI ≥ 25 kg/m2).
While the detection accuracy was similar between the different radiation exposure protocols, the confidence level decreased when the kVp was lowered, especially for enlarged mediastinal lymph nodal detection. We also observed the large inter-reader variability in confidence that could be due to differences in radiologists’ interpretation experience for images with increased image noise. Increased image noise is known to affect the low-contrast resolution (mediastinal window) [26, 27] but has little impact on the high-contrast resolution (lung window) [28]; this may reduce confidence in interpretation of the mediastinum while lung nodule detection confidence was maintained. Decreased confidence may result in increased rate of recommendation for additional imaging [29]. Since benefits of lower radiation exposure from low kVp protocols are likely to be significant, additional time and training may be needed to reduce the variability and increase the confidence level when reading low kVp studies with increased noise. It is also important to carefully consider the risk–benefit balance depending on the clinical scenario. Older patients with high risks of malignancy may sometimes need standard kVp settings for confidently identifying mediastinal abnormalities. We recommend vigilance and communication among both referring clinicians and radiologists as lower kVp CTPA images become routine at many institutions.
There are several additional strategies that can lower the radiation dose in CTPA images. Lowering tube current also decreases photon flux and lowers the radiation exposure, and important component of radiation dose reduction. For all CTPA studies in our cohort, we implemented tube current modulation that is readily available at the majority of recent CT scanners to avoid overexposure [30–32]. Iterative image reconstruction algorithms reduce noise, and this benefit is typically used to lower radiation exposure [33]. While the current data was acquired before these methods became available clinically, iterative methods should be incorporated when available.
We acknowledge study trade-offs and limitations. First, while prospective studies incorporating reference standard imaging would mitigate the heterogeneity of the data, completion of a large trial would be difficult since patients would require additional scanning. As the benefit from lowering radiation exposure is huge, lower radiation dose CT protocols are often incorporated to clinical practice without prospective studies. Our retrospective data uses multiple CT scanners and parameters that were slightly different among scanners and influenced image noise; newer scanners in the standard kVp group with body weight ≥80 kg achieved superior objective image quality (“Appendix”). However the current data argue that despite this, the lower kVp images achieved comparable diagnostic accuracy to that from the standard kVp group. Second, we acknowledge that the reference chest CT scans included both non-contrast and contrast-enhanced CT studies, and attempted adjustments in the multivariate analysis as well as performed the subgroup analysis. Third, we note that among the two readers, we did not test for a possible learning curve. Future work should investigate the level of confidence after training with more than two readers. Fourth, we acknowledge that a number of body size metrics have been employed when tailoring kVp settings. We used body weight because it is easily obtainable at the time of CT scan and body weight-based kVp protocols are the routine clinical practice at our institution. BMI is another well-established metric of body habitus, but in this population, BMI was available only in 333 out of 546 patients. In the secondary analysis, we confirmed that the BMI cutoff and body weight cutoff give similar results. Finally, while the study design benefits from objective data regarding image quality, this approach by necessity used data from the pulmonary arteries, not the lungs and mediastinum. Objective image quality for subtle abnormalities such as small ground glass lesions is not reproducible. Thus, our approach was considered the best alternative for objective data [1, 6–8] since there would have been enormous variability from volume averaging among lesions that do not have distinct borders.
In conclusion, while increased image noise may decrease the diagnostic confidence of image interpretation by the radiologist, there was no compromise in accuracy for the detection of lung nodules and enlarged mediastinal lymph nodes using low radiation dose CTPA with low kVp settings. Hence, referring clinicians can expect that a single CTPA study can answer questions related to lung and mediastinum findings.
References
Szucs-Farkas Z, Strautz T, Patak MA, Kurmann L, Vock P, Schindera ST (2009) Is body weight the most appropriate criterion to select patients eligible for low-dose pulmonary CT angiography? Analysis of objective and subjective image quality at 80 kVp in 100 patients. Eur Radiol 19(8):1914–1922. doi:10.1007/s00330-009-1385-7
Sigal-Cinqualbre AB, Hennequin R, Abada HT, Chen X, Paul JF (2004) Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology 231(1):169–174. doi:10.1148/radiol.2311030191
Matsuoka S, Hunsaker AR, Gill RR, Oliva IB, Trotman-Dickenson B, Jacobson FL, Hatabu H (2009) Vascular enhancement and image quality of MDCT pulmonary angiography in 400 cases: comparison of standard and low kilovoltage settings. AJR Am J Roentgenol 192(6):1651–1656. doi:10.2214/AJR.08.1730
Schueller-Weidekamm C, Schaefer-Prokop CM, Weber M, Herold CJ, Prokop M (2006) CT angiography of pulmonary arteries to detect pulmonary embolism: improvement of vascular enhancement with low kilovoltage settings. Radiology 241(3):899–907. doi:10.1148/radiol.2413040128
Sodickson A, Weiss M (2012) Effects of patient size on radiation dose reduction and image quality in low-kVp CT pulmonary angiography performed with reduced IV contrast dose. Emerg Radiol 19(5):437–445. doi:10.1007/s10140-012-1046-z
Szucs-Farkas Z, Kurmann L, Strautz T, Patak MA, Vock P, Schindera ST (2008) Patient exposure and image quality of low-dose pulmonary computed tomography angiography: comparison of 100- and 80-kVp protocols. Investig Radiol 43(12):871–876. doi:10.1097/RLI.0b013e3181875e86
Szucs-Farkas Z, Schaller C, Bensler S, Patak MA, Vock P, Schindera ST (2009) Detection of pulmonary emboli with CT angiography at reduced radiation exposure and contrast material volume: comparison of 80 kVp and 120 kVp protocols in a matched cohort. Investig Radiol 44(12):793–799. doi:10.1097/RLI.0b013e3181bfe230
Heyer CM, Mohr PS, Lemburg SP, Peters SA, Nicolas V (2007) Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study. Radiology 245(2):577–583. doi:10.1148/radiol.2452061919
Zamboni GA, Guariglia S, Bonfante A, Martino C, Cavedon C, Mucelli RP (2012) Low voltage CTPA for patients with suspected pulmonary embolism. Eur J Radiol 81(4):e580–e584. doi:10.1016/j.ejrad.2011.06.051
Bjorkdahl P, Nyman U (2010) Using 100- instead of 120-kVp computed tomography to diagnose pulmonary embolism almost halves the radiation dose with preserved diagnostic quality. Acta Radiol 51(3):260–270. doi:10.3109/02841850903505222
Hall WB, Truitt SG, Scheunemann LP, Shah SA, Rivera MP, Parker LA, Carson SS (2009) The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch Intern Med 169(21):1961–1965. doi:10.1001/archinternmed.2009.360
Schattner A (2009) Computed tomographic pulmonary angiography to diagnose acute pulmonary embolism: the good, the bad, and the ugly: comment on “The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism”. Arch Intern Med 169(21):1966–1968. doi:10.1001/archinternmed.2009.400
Sohns C, Amarteifio E, Sossalla S, Heuser M, Obenauer S (2008) 64-Multidetector-row spiral CT in pulmonary embolism with emphasis on incidental findings. Clin Imaging 32(5):335–341. doi:10.1016/j.clinimag.2008.01.028
Soye JA, Loughrey CB, Hanley PD (2008) Computed tomography pulmonary angiography: a sample of experience at a District General Hospital. Ulst Med J 77(3):175–180
McNulty K, Massouh L, Hughes NC, Ho TB (2010) Incidental findings of solitary pulmonary nodules on computed tomographic pulmonary angiography: a hidden workload. Clin Med 10(1):100
Hunsaker AR, Oliva IB, Cai T, Trotman-Dickenson B, Gill RR, Hatabu H, Rybicki FJ (2010) Contrast opacification using a reduced volume of iodinated contrast material and low peak kilovoltage in pulmonary CT angiography: objective and subjective evaluation. Am J Roentgenol 195(2):W118–W124. doi:10.2214/AJR.09.3342
Jaffe TA, Neville AM, Anderson-Evans C, Long S, Lowry C, Yoshizumi TT, Toncheva G (2009) Early first trimester fetal dose estimation method in a multivendor study of 16- and 64-MDCT scanners and low-dose imaging protocols. AJR Am J Roentgenol 193(4):1019–1024. doi:10.2214/AJR.08.2274
Schiff GD, Hasan O, Kim S, Abrams R, Cosby K, Lambert BL, Elstein AS, Hasler S, Kabongo ML, Krosnjar N, Odwazny R, Wisniewski MF, McNutt RA (2009) Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med 169(20):1881–1887. doi:10.1001/archinternmed.2009.333
Szucs-Farkas Z, Schibler F, Cullmann J, Torrente JC, Patak MA, Raible S, Hoppe H, Wyttenbach R, Vock P, Schindera ST (2011) Diagnostic accuracy of pulmonary CT angiography at low tube voltage: intraindividual comparison of a normal-dose protocol at 120 kVp and a low-dose protocol at 80 kVp using reduced amount of contrast medium in a simulation study. AJR Am J Roentgenol 197(5):W852–W859. doi:10.2214/AJR.11.6750
Oguchi K, Sone S, Kiyono K, Takashima S, Maruyama Y, Hasegawa M, Feng L (2000) Optimal tube current for lung cancer screening with low-dose spiral CT. Acta Radiol 41(4):352–356
Karabulut N, Toru M, Gelebek V, Gulsun M, Ariyurek OM (2002) Comparison of low-dose and standard-dose helical CT in the evaluation of pulmonary nodules. Eur Radiol 12(11):2764–2769. doi:10.1007/s00330-002-1368-4
Cai B, Bedayat A, George E, Hunsaker AR, Dill KE, Rybicki FJ, Kumamaru KK (2013) Malignancy and acute pulmonary embolism: risk stratification including the right to left ventricle diameter ratio in 1596 subjects. J Thorac Imaging 28(3):196–201. doi:10.1097/RTI.0b013e3182870bf9
Ong CW, Malipatil V, Lavercombe M, Teo KG, Coughlin PB, Leach D, Spanger M, Thien F (2012) Implementation of a clinical prediction tool for Pulmonary Embolism diagnosis. In: a tertiary teaching hospital reduces the number of CT pulmonary angiograms performed. Intern med J. doi:10.1111/j.1445-5994.2012.02926.x
Prologo JD, Gilkeson RC, Diaz M, Asaad J (2004) CT pulmonary angiography: a comparative analysis of the utilization patterns in emergency department and hospitalized patients between 1998 and 2003. Am J Roentgenol 183(4):1093–1096
Raja AS, Ip IK, Prevedello LM, Sodickson AD, Farkas C, Zane RD, Hanson R, Goldhaber SZ, Gill RR, Khorasani R (2012) Effect of computerized clinical decision support on the use and yield of CT pulmonary angiography in the emergency department. Radiology 262(2):468–474. doi:10.1148/radiol.11110951
Baker ME, Dong F, Primak A, Obuchowski NA, Einstein D, Gandhi N, Herts BR, Purysko A, Remer E, Vachhani N (2012) Contrast-to-noise ratio and low-contrast object resolution on full- and low-dose MDCT: SAFIRE versus filtered back projection in a low-contrast object phantom and in the liver. Am J Roentgenol 199(1):8–18. doi:10.2214/AJR.11.7421
Rogalla P, Stover B, Scheer I, Juran R, Gaedicke G, Hamm B (1999) Low-dose spiral CT: applicability to paediatric chest imaging. Pediatr Radiol 29(8):565–569
Greess H, Nomayr A, Wolf H, Baum U, Lell M, Bowing B, Kalender W, Bautz WA (2002) Dose reduction in CT examination of children by an attenuation-based on-line modulation of tube current (CARE Dose). Eur Radiol 12(6):1571–1576. doi:10.1007/s00330-001-1255-4
Sistrom CL, Dreyer KJ, Dang PP, Weilburg JB, Boland GW, Rosenthal DI, Thrall JH (2009) Recommendations for additional imaging in radiology reports: multifactorial analysis of 5.9 million examinations. Radiology 253(2):453–461. doi:10.1148/radiol.2532090200
Kalra MK, Maher MM, Toth TL, Schmidt B, Westerman BL, Morgan HT, Saini S (2004) Techniques and applications of automatic tube current modulation for CT. Radiology 233(3):649–657. doi:10.1148/radiol.2333031150
Coche E, Vynckier S, Octave-Prignot M (2006) Pulmonary embolism: radiation dose with multi-detector row CT and digital angiography for diagnosis. Radiology 240(3):690–697. doi:10.1148/radiol.2402050580
Mastora I, Remy-Jardin M, Delannoy V, Duhamel A, Scherf C, Suess C, Remy J (2004) Multi-detector row spiral CT angiography of the thoracic outlet: dose reduction with anatomically adapted online tube current modulation and preset dose savings. Radiology 230(1):116–124. doi:10.1148/radiol.2301021408
Martillotti J, Silva N, Chhabra J, Molstrom C, Coughlin R, O’Loughlin M, Coughlin B (2013) Dose of reduced z-axis length of computed tomography angiography (CTA) of the chest for pulmonary embolism using 64-detector rows and adaptive iterative reconstruction techniques. Emerg Radiol 20(1):39–44. doi:10.1007/s10140-012-1065-9
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
CT pulmonary angiography acquisition
All 546 CTPA examinations used 16-, 64- and 128 slice scanners of the same manufacture (Emotion, Definition/Sensation 64/Definition AS/Definition AS+, Siemens Healthcare, Erlangen. Germany). Details of the CTPA parameters are described in the Table below. All patients received 75 ml iodinated contrast media intravenously (370 mg iodine per mL) at a rate of 3.5–4 mL/second without a saline chaser. The acquisition was timed using bolus tracking at the main pulmonary artery with a CT density threshold of 80 Hounsfield Units (HU). Axial images were reconstructed with 1 mm thickness with a 0.5 mm increment using standard soft tissue kernel for evaluation of PE, and contiguous 5 mm-thick slices in a high resolution algorithm for evaluation of the lung parenchyma.
Emotion 16 | Definition AS | Definition | Definition AS+ | p value | |
|---|---|---|---|---|---|
Lower kVp (Weight <80 kg, n = 138) | |||||
Number of patients | 92 | 8 | 18 | 20 | – |
Number of detector row | 16 | 64 | 64 | 128 | – |
Tube voltage | 80 | 80 | 80 | 80 | – |
Reference mAs for tube current modulation | 150 | 180 | 200 | 200 | – |
Gantry rotation time (s) | 0.6 | 0.5 | 0.5 | 0.5 | – |
Collimation (mm) | 0.6 | 0.6 | 0.6 | 0.6 | – |
Helical pitch factor | 1 | 0.9 | 1 | 0.75 | – |
Mean SNR at left main PA | 17.7 | 19.0 | 20.8 | 17.8 | 0.556 |
Mean CNR at left main PA | 16.0 | 17.3 | 18.9 | 15.8 | 0.559 |
Lower kVp (Weight ≥80 kg, n = 134) | |||||
Number of patients | 75 | 9 | 16 | 16 | – |
Number of detector row | 16 | 64 | 64 | 128 | – |
Tube voltage | 110 | 100 | 100 | 100 | – |
Reference mAs for tube current modulation | 150 | 180 | 200 | 200 | – |
Gantry rotation time (s) | 0.6 | 0.5 | 0.5 | 0.5 | – |
Collimation (mm) | 0.6 | 0.6 | 0.6 | 0.6 | – |
Helical pitch factor | 1 | 0.9 | 1 | 0.75 | – |
Mean SNR at left main PA | 13.2 | 11.7 | 12.2 | 13.3 | 0.814 |
Mean CNR at left main PA | 11 | 9.7 | 10.4 | 11.3 | 0.801 |
Emotion 16 | Definition | Sensation 64 | Definition AS+ | p value | |
|---|---|---|---|---|---|
Standard kVp (Weight <80 kg, n = 136) | |||||
Number of patients | 16 | 8 | 104 | 8 | – |
Number of detector row | 16 | 64 | 64 | 128 | – |
Tube voltage | 130 | 120 | 120 | 120 | – |
Reference mAs for tube current modulation | 150 | 200 | 200 | 200 | – |
Gantry rotation time (s) | 0.6 | 0.5 | 0.5 | 0.5 | – |
Collimation (mm) | 0.6 | 0.6 | 0.6 | 0.6 | – |
Helical pitch factor | 1 | 1 | 1 | 0.75 | – |
Mean SNR at left main PA | 15.9 | 15.5 | 18.1 | 17 | 0.636 |
Mean CNR at left main PA | 13.2 | 13.3 | 15.9 | 14.7 | 0.512 |
Standard kVp (Weight ≥80 kg, n = 138) | |||||
Number of patients | 18 | 7 | 84 | 29 | – |
Number of detector row | 16 | 64 | 64 | 128 | – |
Tube voltage | 130 | 120 | 120 | 120 | – |
Reference mAs for tube current modulation | 150 | 200 | 200 | 200 | – |
Gantry rotation time (sec) | 0.6 | 0.5 | 0.5 | 0.5 | – |
Collimation (mm) | 0.6 | 0.6 | 0.6 | 0.6 | – |
Helical pitch factor | 1 | 1 | 1 | 0.35–0.75* | – |
Mean SNR at left main PA | 10.4 | 10.4 | 12.3 | 16.7§ | 0.001 |
Mean CNR at left main PA | 8.4 | 8.3 | 10.3 | 14.2§ | 0.004 |
Reference chest CT acquisition
Acquisition parameters were optimized with tube voltage of 120–140 kVp and the tube current was determined using manufacturer automated software with a range between 100 and 500 mA. Reconstructions included contiguous 5 mm thick slices in both high resolution and soft tissue algorithms for evaluation of the lung parenchyma and mediastinum respectively. Thin section high resolution 1–1.25 mm thick slices were also obtained at 10 mm intervals.
Rights and permissions
About this article
Cite this article
Kumamaru, K.K., Rybicki, F.J., Madan, R. et al. Incidental findings detection using low tube potential for CT pulmonary angiography. Int J Cardiovasc Imaging 30, 1579–1588 (2014). https://doi.org/10.1007/s10554-014-0484-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0484-y