Abstract
To compare cardiovascular magnetic resonance (CMR) characteristics between arrhythmogenic right ventricular cardiomyopathy (ARVC) patients with syncope and without syncope and explore CMR parameters related with syncope. A consecutive series of 80 patients with ARVC were divided in two groups according to history of syncope prior to CMR examinations. The biventricular function and volumes were calculated and indexed by body surface area. Fatty infiltration and late-gadolinium enhancement (LGE) were self-quantitatively analyzed according to segmental model. Patients with syncope had statistically significant greater left ventricular end-diastolic volume index (LVEDVI) (79.6 ± 23.0 vs. 69.0 ± 17.9 mL/m2, P = 0.030), right ventricular end-diastolic volume index (RVEDVI) (122.0 ± 30.0 vs. 107.4 ± 21.8 mL/m2, P = 0.017), and LGE incidence (52.2 vs. 21.1 %, P = 0.006) than that of patients without syncope. Patients with syncope had a trend towards greater number of segments with LGE (8.6 ± 4.2 vs. 6.6 ± 3.1, P = 0.199) than that of patients without syncope in subgroup analyses of patients with LGE, but no statistical significance was reached. Multivariate regression analysis showed the presence of LGE was independently associated with syncope in patients with ARVC (odds ratios 8.827, 95 % confidence interval 1.945–40.068, P = 0.005). CMR is helpful in detection and management of the patients with ARVC. Patients with syncope had significantly higher LVEDVI, RVEDVI and LGE incidence, and larger studies with follow-up data are needed to elucidate the relationship between LGE and syncope in patients with ARVC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) (also known as arrhythmogenic right ventricular dysplasia or ARVD) is a genetically determined cardiomyopathy characterized by fibrous and fatty replacement and presents as ventricular tachycardia (VT) and sudden cardiac death (SCD) [1–3]. Syncope is the most common presenting symptom and the greatest predictor of arrhythmic events and independently associated with cardiovascular deaths in ARVC [3–8]. It has been reported previously that syncope was an important predictor of life-saving implantable cardioverter defibrillator intervention in ARVC [9, 10]. Therefore, early detection at highest risk of experiencing syncope would be helpful in management of the patients with ARVC and may modify the natural history of the disease.
In comparison to the left ventricle (LV), the right ventricular (RV) evaluation is still a challenge because of the semi-lunar shape, complex geometry and thin wall. Cardiovascular magnetic resonance (CMR) imaging allows an accurate morphological and functional evaluation of the RV and is the standard imaging techniques for diagnosing ARVC. A potential role of CMR lies in its ability for tissue characterization to detect myocardial fibrofatty infiltration, a finding that can precede functional abnormalities thus allowing the disease detection at an earlier stage than the Task force criteria (TFC) [11–18]. Myocardial fibrosis identified using late-gadolinium enhancement (LGE) CMR has been shown to be a predictor of prognosis in patients with dilated, hypertrophic and ischemic cardiomyopathies [19–21]. The mechanistic studies have demonstrated that the presence of LGE is associated with ventricular arrhythmias and is an independent predictor of adverse outcomes in patients with ventricular arrhythmia [22, 23]. In this study, we sought to compare CMR characteristics between ARVC patients with syncope and without syncope and explore related risk factors for syncope.
Materials and methods
Study population
We collected consecutively a series of 80 patients with clinical diagnosis of ARVC at Fuwai hospital. The diagnosis of ARVC was made according to the modified TFC, if the patients either had two major criteria, one major and two minor criteria, or four minor criteria [18]. All patients underwent systematic clinical evaluation, including family and personal histories, physical examination, 12-lead electrocardiography, ambulatory 24-hour Holter monitoring, transthoracic echocardiography, and CMR. In addition, selective coronary angiography was performed in 9 patients with ARVC, and coronary computed tomography angiography was performed 37 patients. The whole patients were divided into two groups according to history of syncope before CMR scan. Syncope is defined as a transient loss of consciousness attributable to global cerebral hypo-perfusion, further characterized by rapid onset, brevity, and spontaneous recovery [24]. The study was performed in accordance with the Declaration of Helsinki and was approved by the committee on human research at our hospital.
CMR protocol
All examinations were performed on a 1.5 Tesla MR scanner (Magnetom Avanto, Siemens Medical Solutions, Erlangen, Germany). All imaging acquisitions were captured under breath control. Scout transversal and sagittal images were acquired followed by a half-Fourier acquisition single shot turbo spin echo sequence (HASTE). Image parameters for HASTE were as follows: repetition time (TR) 1 R–R interval, echo time (TE) 42 ms, slice thickness 6 mm, imaging matrix 111 × 256, field of view (FOV) 34 cm. True imaging with steady-stage precession sequence (TrueFISP) was chosen for cine scan in the axial and short-axis planes. A true 4-chamber cine image was obtained in all patients, and the short-axis images were prescribed on the 4-chamber diastolic image. Image parameters for TrueFISP were as follows: TR 2.3 ms, TE 1.4 ms, slice thickness 6 mm, image matrix 256 × 192, FOV 34 cm, flip angle 60°. For delineation of fatty infiltration, fat-suppressed T1 and T2-weighted turbo spin echo sequence (TSE) were collected. 15–20 min after injection of 0.2 mmol/kg of gadolinium diethylenetriamine pentaacetic acid (Magnevist, Schering, Berlin, Germany), images of LGE were obtained in standard short axis covering the whole LV and RV, and in long axis views to detect areas of LGE using a phase-sensitive inversion recovery (PISR) spoiled gradient echo sequence. Imaging parameters for LGE were as follows: TR 8.7 ms, TE 3.4 ms, no gap between slice, imaging matrix 256 × 256, FOV 34 cm, flip angle 15°. For all scans the optimal inversion time to null the signal of normal myocardium was determined using an inversion-recovery steady-state free precession sequence with incrementally increasing inversion times.
CMR analysis
All magnetic resonance images were transferred to a dedicated workstation (Siemens Medical Systems) for analysis. Quantitative assessment was performed independently by an experienced radiologist (M.J.L.) blinded to the clinical and other diagnostic information, which had 13 years of experience in CMR studies. Biventricular ejective fraction (EF), end-diastolic volume index (EDVI), end-systolic volume index (ESVI), and cardiac index (CI) were obtained using Argus analytical software (version VE36A). Endocardial margins of the LV and RV were semi-automatically contoured on end-diastolic and end-systolic images. To analyze inter-observer variability, 20 randomly selected CMR images were reassessed by another CMR operator (G.Y.) with 6 years of experience.
To identify fatty infiltration, T1-weighted black blood imaging without and with fat saturation was utilized. The fatty infiltration was defined as an area of hyperintensity on T1-weighted imaging that was suppressed out on the corresponding fat saturation image. The same sequence was also used to differentiate partial volume effects from epicardial fat and LGE on the ventricular wall. For the detection of ventricular fibrosis, Long and short-axis images were scrutinized. LGE was considered present only if myocardial enhancement was confirmed on both short-axis and matching long-axis locations using a signal intensity threshold of >2 standard deviation (SD) above a remote reference region as previously reported. In order to rule out confounding effects from signal artifacts, we required an area of signal intensity corresponding to the region of interest in two orthogonal planes to confirm the presence of LGE. If there was no orthogonal plane exactly matching the region in question, an extra orthogonal slice was planned directly through the area in question. The RV was divided into three levels in the short-axis plane: basal, mid, and apical. Each of these three levels was further divided into three segments (superior, lateral, inferior), resulting in a nine-segment model for the RV [15]. The LV was assessed using the 17 segments model according to the American Heart Association recommendation [25]. The fatty infiltration and LGE were assessed in each segment using the following scale: 0 = none and 1 = presence. Global and regional wall motion abnormalities (akinesia, dyskinesia, or dyssynchronous contraction) of the RV were subjectively evaluated. Localized aneurysms of the RV were defined as akinetic regions showing bulging in diastole and systole. All qualitative assessments were performed by three observers who had no knowledge of clinical information. If there was a discrepancy, the majority opinion was used.
Statistical analysis
All values are given as mean ± SD or number (percent). Categorical variables were compared by the Chi square test or Fisher’s exact test. Comparisons in continuous variables were performed by t test. The inter-observer agreements for qualitative and quantitative assessments were measured with the Kendall’s W test and intra-class correlation coefficient (ICC), respectively. Multivariate regression analysis was used to determine associations between syncope and CMR parameters. The confidence interval (CI) estimated for odds ratios (OR) was calculated with 95 % probability levels. A two tailed P value of <0.05 was considered statistically significant. The statistical analysis was performed using SPSS for Windows 16.0 (Chicago, IL, USA).
Results
Patient baseline characteristics
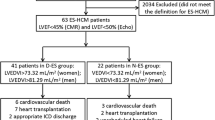
The study population consisted of 80 patients, 14–68 years (mean ± SD, 38.2 ± 15.1 years) of age, 56 (70 %) of whom were male. The diagnostic details of revised TFC are summarized in Table 1. All subjects had recorded ventricular arrhythmias. There were 56 (70 %) subjects with a sustained or nonsustained VT. Premature ventricular complexes were identified in 24 (30 %) patients. Ten (13 %) patients had family history with conformed ARVC or sudden death with suspected ARVC in a first-degree relative (<35 years of age). Four (5 %) patients underwent heart transplantation, and final diagnoses were proven by surgical pathology specimens (Fig. 1). In 46 patients with ARVC undergoing coronary angiography or coronary computed tomography angiography, coronary artery disease was excluded. The comparisons of demographic and clinical characteristics between two groups are shown in Table 2. There were no significant differences in sex, age, clinical presentation, heart failure symptoms, NYHA class, occurrence of VT, and family history between patients with syncope and patients without syncope.
CMR characteristics
Global and regional wall motion abnormality were found in 47 (59 %) and 24 (30 %) patients, respectively. The RV fatty infiltration and LGE were detected in 33 (41 %) and 24 (30 %) patients, respectively (Fig. 2). The LV involvement was identified in 22 (28 %) patients, and fatty infiltration and LGE were present in 7 (9 %) and 6 (8 %) patients, respectively. Comparative results of CMR parameters between two groups are independently shown in Table 3. Compared with patients without syncope, patients with syncope had significantly larger LVEDVI (mean ± SD, 79.6 ± 23.0 vs. 69.0 ± 17.9 mL/m2, P = 0.030), RVEDVI (mean ± SD, 122.0 ± 30.0 vs. 107.4 ± 21.8 mL/m2, P = 0.017) (Fig. 3). There was a higher LGE incidence (52.2 vs. 21.1 %, P = 0.006) in patients with syncope than in patients without syncope. There were no differences between patients with syncope and without syncope in fatty infiltration, LVEF, RVEF, LVESVI, and RVESVI (Fig. 3). Subgroup analyses were further performed in patients with fatty infiltration and with LGE, respectively. No statistical significances were reached in number of segments with fatty infiltration (8.9 ± 5.3 vs. 5.6 ± 3.1, P = 0.094) and with LGE (8.6 ± 4.2 vs. 6.6 ± 3.1, P = 0.199) between patients with syncope and without syncope.
Inter-observer variability
Kendall’s coefficient of concordance showed that there were excellent inter-observer agreements on the qualitative assessment for fatty infiltration (Kendall’s W = 0.91), LGE (Kendall’s W = 0.89,), and wall motion abnormality (Kendall’s W = 0.92, P < 0.001 for all). There were excellent correlations for LVEF (ICC = 0.92), LVEDVI (ICC = 0.94), RVEF (ICC = 0.82), and RVEDVI (ICC = 0.93, P < 0.001 for all) between two observers.
Multivariate analysis
Multivariate regression analysis revealed that the presence of LGE (OR 8.827, 95 % CI 1.945–40.068, P = 0.005) was the only CMR parameter that remained statistically significant with respect to syncope in patients with ARVC.
Discussion
The clinical and CMR features of ARVC in present study were consistent with the results of prior studies [3, 13–15]. Family history of ARVC or sudden death (<35 years of age) was observed in 10 (13 %) patients in our series and lower than that of previous reports [26, 27]. This likely represents an underestimate of true prevalence of familial pattern because systematic screening of all family members was not performed. Similar to what were previously observed [4, 28], 22 (28 %) patients had of LV involvement in the present study. Although ARVC is an inherited disease of the heart muscle involving the RV, there is now clinical and pathological evidence that the LV may be progressively affected thus resulting in a biventricular failure.
Cardiovascular magnetic resonance is used as a part of the cardiac workup for ARVC and can be used to accurately identify the distribution of fibrofatty patterns, and this finding can precede functional abnormalities, potentially allowing for better detection of disease at an early stage than with the TFC [11–18, 29]. The study by te Riele et al. [30] showed recently that patients with electrical abnormalities on the basis of ECG and Holter assessment were significantly more likely to have higher RV volumes on CMR. Similar to their study, LVEDVI and RVEDVI were significantly higher in patients with syncope than in patients without syncope. This significant difference would be due to more severe disease states in patients with syncope.
The results of the current study showed the presence of LGE is independently related with syncope in patients with ARVC. Previous studies have shown that LGE CMR can reliably detect fibrotic substrate and predict VT in both ischemic and non-ischemic cardiomyopathies. The utility of LGE CMR has also been demonstrated as a diagnostic and prognostic tool in patients with ARVC [14–16]. Tandri et al. [15] reported LGE of the RV was observed in 67 % of patients with ARVC and correlated with inducibility of sustained monomorphic VT at electrophysiological study and demonstration of fibrofatty myocardial changes at endomyocardial biopsy. The authors concluded that LGE CMR may have a role in patients with ARVC as a noninvasive diagnostic test with added prognostic value. The extent of LGE is correlated with risk factors of SCD and the likelihood of inducible VT in hypertrophic and idiopathic dilated cardiomyopathies [19–23]. However, it’s worth noting that subgroup analysis of patients with LGE showed no difference in number of segments with LGE between patients with syncope and without syncope, which may be mainly attributable to a statistical bias of the insufficient sample in this study.
Syncope has often been regarded as surrogate for aborted sudden arrhythmic death in ARVC and an indication for intervention [9, 10]. Although a cause and effect relation is unproved, it is certainly plausible that ARVC patients with an underlying electrical instability from fibrofatty infiltration would be at increased risk. Since syncope may present in patients with ARVC at young age, and since the risk period for sudden arrhythmic death may be long, decision-making in patients with ARVC may be difficult, and have lifelong implications [4–6, 9]. Up to now there are no clear-cut guidelines to select the best management approach in patients with ARVC. There is no curative treatment for patients with ARVC, instead, the aim is to detect patients at high risk and prevent complications. Our study identifies the presence of LGE is associated with present of syncope in patients with ARVC; however, whether patients with ARVC may benefit from the identification of LGE is unknown, and larger studies with complete follow-up data are needed to test whether the present the LGE is valuable to assess the individual risk profile or can help identify high-risk patients with ARVC.
Study limitations
There are several limitations of the current study. Firstly, the major limitation is the lack of follow-up data from the study population. The presence of LGE for prediction of syncope needs further investigation in patients with ARVC. Secondly, there was a potential for selection and referral bias in our patient population, given most patients who had clinically overt disease at a tertiary care center that might not reflect the referral patterns of the community at large. Thirdly, the fatty and LGE size and surface area were not accurately measured because of the thinness of the RV wall.
Conclusions
Cardiovascular magnetic resonance is helpful in detection and management of the patients with ARVC. Patients with syncope had significantly higher LVEDVI, RVEDVI and LGE incidence, and larger studies with follow-up data are needed to elucidate the relationship between LGE and syncope in patients with ARVC.
References
Basso C, Corrado D, Marcus FI, Nava A, Thiene G (2009) Arrhythmogenic right ventricular cardiomyopathy. Lancet 373:1289–1300
Thiene G, Nava A, Corrado D, Rossi L, Pennelli N (1988) Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med 318:129–133
Dalal D, Nasir K, Bomma C, Prakasa K, Tandri H, Piccini J, Roguin A, Tichnell C, James C, Russell SD, Judge DP, Abraham T, Spevak PJ, Bluemke DA, Calkins H (2005) Arrhythmogenic right ventricular dysplasia: a United States experience. Circulation 112:3823–3832
Corrado D, Basso C, Thiene G, McKenna WJ, Davies MJ, Fontaliran F, Nava A, Silvestri F, Blomstrom-Lundqvist C, Wlodarska EK, Fontaine G, Camerini F (1997) Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol 30:1512–1520
Behr ER, Dalageorgou C, Christiansen M, Syrris P, Hughes S, Tome Esteban MT, Rowland E, Jeffery S, McKenna WJ (2008) Sudden arrhythmic death syndrome: familial evaluation identifies inheritable heart disease in the majority of families. Eur Heart J 29:1670–1680
Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G (2004) Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation 110:1879–1884
Migliore F, Zorzi A, Silvano M, Bevilacqua M, Leoni L, Marra MP, Elmaghawry M, Brugnaro L, Dal Lin C, Bauce B, Rigato I, Tarantini G, Basso C, Buja G, Thiene G, Iliceto S, Corrado D (2013) Prognostic value of endocardial voltage mapping in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ Arrhythm Electrophysiol 6:167–176
Turrini P, Corrado D, Basso C, Nava A, Thiene G (2003) Noninvasive risk stratification in arrhythmogenic right ventricular cardiomyopathy. Ann Noninvasive Electrocardiol 8:161–169
Corrado D, Calkins H, Link MS, Leoni L, Favale S, Bevilacqua M, Basso C, Ward D, Boriani G, Ricci R, Piccini JP, Dalal D, Santini M, Buja G, Iliceto S, Estes NA III, Wichter T, McKenna WJ, Thiene G, Marcus FI (2010) Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation 122:1144–1152
Corrado D, Leoni L, Link MS, Della Bella P, Gaita F, Curnis A, Salerno JU, Igidbashian D, Raviele A, Disertori M, Zanotto G, Verlato R, Vergara G, Delise P, Turrini P, Basso C, Naccarella F, Maddalena F, Estes NA III, Buja G, Thiene G (2003) Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation 108:3084–3091
Dalal D, Tandri H, Judge DP, Amat N, Macedo R, Jain R, Tichnell C, Daly A, James C, Russell SD, Abraham T, Bluemke DA, Calkins H (2009) Morphologic variants of familial arrhythmogenic right ventricular dysplasia/cardiomyopathy a genetics-magnetic resonance imaging correlation study. J Am Coll Cardiol 53:1289–1299
Puranik R, Gray B, Lackey H, Yeates L, Parker G, Duflou J, Semsarian C (2014) Comparison of conventional autopsy and magnetic resonance imaging in determining the cause of sudden death in the young. J Cardiovasc Magn Reson 16:44
Tandri H, Macedo R, Calkins H, Calkins H, Marcus F, Cannom D, Scheinman M, Daubert J, Estes M III, Wilber D, Talajic M, Duff H, Krahn A, Sweeney M, Garan H, Bluemke DA (2008) Multidisciplinary study of right ventricular dysplasia investigators role of magnetic resonance imaging in arrhythmogenic right ventricular dysplasia: insights from the North American arrhythmogenic right ventricular dysplasia (ARVD/C) study. Am Heart J 155:147–153
Keller DI, Osswald S, Bremerich J, Bongartz G, Cron TA, Hilti P, Pfisterer ME, Buser PT (2003) Arrhythmogenic right ventricular cardiomyopathy: diagnostic and prognostic value of the cardiac MRI in relation to arrhythmia-free survival. Int J Cardiovasc Imaging 19:537–543
Tandri H, Saranathan M, Rodriguez ER, Martinez C, Bomma C, Nasir K, Rosen B, Lima JA, Calkins H, Bluemke DA (2005) Noninvasive detection of myocardial fibrosis in arrhythmogenic right ventricular cardiomyopathy using delayed-enhancement magnetic resonance imaging. J Am Coll Cardiol 45:98–103
Hunold P, Wieneke H, Bruder O, Krueger U, Schlosser T, Erbel R, Barkhausen J (2005) Late enhancement: a new feature in MRI of arrhythmogenic right ventricular cardiomyopathy? J Cardiovasc Magn Reson 7:649–655
McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, Camerini F (1994) Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J 71:215–218
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DM, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, Zareba W (2010) Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Eur Heart J 31:806–814
Neilan TG, Coelho-Filho OR, Danik SB, Shah RV, Dodson JA, Verdini DJ, Tokuda M, Daly CA, Tedrow UB, Stevenson WG, Jerosch-Herold M, Ghoshhajra BB, Kwong RY (2013) CMR quantification of myocardial scar provides additive prognostic information in nonischemic cardiomyopathy. JACC Cardiovasc Imaging 6:944–954
Green JJ, Berger JS, Kramer CM, Salerno M (2012) Prognostic value of late gadolinium enhancement in clinical outcomes for hypertrophic cardiomyopathy. JACC Cardiovasc Imaging 5:370–377
Heidary S, Patel H, Chung J, Yokota H, Gupta SN, Bennett MV, Katikireddy C, Nguyen P, Pauly JM, Terashima M, McConnell MV, Yang PC (2010) Quantitative tissue characterization of infarct core and border zone in patients with ischemic cardiomyopathy by magnetic resonance is associated with future cardiovascular events. J Am Coll Cardiol 55:2762–2768
Prinz C, Schwarz M, Ilic I, Laser KT, Lehmann R, Prinz EM, Bitter T, Vogt J, van Buuren F, Bogunovic N, Horstkotte D, Faber L (2013) Myocardial fibrosis severity on cardiac magnetic resonance imaging predicts sustained arrhythmic events in hypertrophic cardiomyopathy. Can J Cardiol 29:358–363
Dawson DK, Hawlisch K, Prescott G, Roussin I, Di Pietro E, Deac M, Wong J, Frenneaux MP, Pennell DJ, Prasad SK (2013) Prognostic role of CMR in patients presenting with ventricular arrhythmias. JACC Cardiovasc Imaging 6:335–344
Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, Deharo JC, Gajek J, Gjesdal K, Krahn A, Massin M, Pepi M, Pezawas T, Ruiz Granell R, Sarasin F, Ungar A, van Dijk JG, Walma EP, Wieling W (2009) Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 30:2631–2671
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18:539–542
Nava A, Bauce B, Basso C, Muriago M, Rampazzo A, Villanova C, Daliento L, Buja G, Corrado D, Danieli GA, Thiene G (2000) Clinical profile and long-term follow-up of 37 families with arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol 36:2226–2233
Hamid MS, Norman M, Quraishi A, Firoozi S, Thaman R, Gimeno JR, Sachdev B, Rowland E, Elliott PM, McKenna WJ (2002) Prospective evaluation of relatives for familial arrhythmogenic right ventricular cardiomyopathy/dysplasia reveals a need to broaden diagnostic criteria. J Am Coll Cardiol 40:1445–1450
Pinamonti B, Dragos AM, Pyxaras SA, Merlo M, Pivetta A, Barbati G, Di Lenarda A, Morgera T, Mestroni L, Sinagra G (2011) Prognostic predictors in arrhythmogenic right ventricular cardiomyopathy: results from a 10-year registry. Eur Heart J 32:1105–1113
Looi KL, Edwards C, Hart H, Christiansen JP (2012) Utility of cardiac magnetic resonance in the evaluation of unselected patients with possible arrhythmogenic right ventricular cardiomyopathy. Clin Med Insights Cardiol 6:153–162
te Riele AS, Bhonsale A, James CA, Rastegar N, Murray B, Burt JR, Tichnell C, Madhavan S, Judge DP, Bluemke DA, Zimmerman SL, Kamel IR, Calkins H, Tandri H (2013) Incremental value of cardiac magnetic resonance imaging in arrhythmic risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy- associated desmosomal mutation carriers. J Am Coll Cardiol 62:1761–1769
Acknowledgments
The authors thank the staff and members of the departments of radiology, echocardiography, electrocardiogram and pathology for their assistance in various measurements, diagnosis, and other organizational aspects of this study.
This study was supported by Grants No. 81130029 from the key projects of National Natural Science Foundation of China and No. 2013CB531105 from National Basic Research Program of China (973 program projects).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cheng, H., Lu, M., Hou, C. et al. Comparative study of CMR characteristics between arrhythmogenic right ventricular cardiomyopathy patients with/without syncope. Int J Cardiovasc Imaging 30, 1365–1372 (2014). https://doi.org/10.1007/s10554-014-0481-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0481-1