Abstract
Accurate predictors of appropriate implantable cardioverter defibrillator (ICD) therapy in hypertrophic cardiomyopathy (HCM) patients are lacking. Both left atrial volume index (LAVI) and global longitudinal strain (GLS) have been proposed as prognostic markers in HCM patients. The specific value of LAVI and GLS to predict appropriate ICD therapy in high-risk HCM patients was studied. LAVI and 2-dimensional speckle tracking-derived GLS were assessed in 92 HCM patients undergoing ICD implantation (69 % men, mean age 50 ± 14 years). During long-term follow-up, appropriate ICD therapies, defined as antitachycardia pacing and/or shock for ventricular arrhythmia, were recorded. Appropriate ICD therapy occurred in 21 patients (23 %) during a median follow-up of 4.7 (2.2–8.2) years. Multivariate analysis revealed LAVI (p = 0.03) and GLS (p = 0.04) to be independent predictors of appropriate ICD therapy. Both LAVI and GLS showed higher accuracy to predict appropriate ICD therapy compared to presence of ≥1 conventional sudden cardiac death (SCD) risk factor(s) [area under the curve 0.76 (95 % CI 0.65–0.87) and 0.65 (95 % CI 0.54–0.77) versus 0.52 (95 % CI 0.43–0.58) respectively, p < 0.001]. No patient with both LAVI <34 mL/m2 and GLS <−14 % experienced appropriate ICD therapy. Assessment of both LAVI and GLS on top of conventional SCD risk factors provided incremental clinical predictive value for appropriate ICD therapy, as shown by likelihood ratio test (p < 0.001) and integrated discrimination improvement index (0.17, p < 0.001). LAVI and GLS provide high negative predictive value for appropriate ICD therapy in high-risk HCM patients. Additionally to conventional SCD risk factors, both parameters may be useful to optimize criteria and timing for ICD implantation in these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Implantable cardioverter defibrillator (ICD) is currently recommended in patients with hypertrophic cardiomyopathy (HCM) at high risk for sudden cardiac death [1]. In particular, ICD implantation is a class I indication for secondary prevention in HCM patients who survive cardiac arrest or present with sustained ventricular tachycardia. In addition, the presence of one or more sudden cardiac death (SCD) risk factors, including family history of SCD, left ventricular (LV) hypertrophy ≥30 mm, non-sustained ventricular tachycardia (nsVT), recent unexplained syncope and/or abnormal blood pressure response during exercise testing qualifies patients for ICD implantation as primary prevention [2]. Although appropriate ICD therapy in this high-risk population occurs at a yearly rate of 3.3 %, inappropriate ICD therapy or other device-related complications are seen in 4.8 and 3.4 % of patients per year, respectively [3]. Hence, weighting risk–benefit of ICD implantation in HCM patients is of paramount importance and has created a currently unmet clinical need for accurate predictors of appropriate ICD therapy that may optimize candidate selection and timing criteria for ICD implantation [2, 4].
Impaired myocardial mechanics are commonly observed in HCM patients, despite normal LV ejection fraction [5, 6]. Global longitudinal strain (GLS), which reflects the active deformation of all LV myocardial segments, has been proposed as a sensitive marker of LV systolic function and can be currently quantified by speckle tracking echocardiography [7]. In addition, HCM patients are often characterized by abnormal myocardial relaxation and significant LV diastolic dysfunction, ultimately resulting in increased left atrial volume index (LAVI) [8]. Both GLS and LAVI, as a sensitive marker of LV systolic function and a specific marker of LV diastolic function respectively, have therefore been identified as prognostic factors in HCM patients [9–14]. However, their potential role to predict appropriate ICD therapy is unexplored. Therefore, the aim of our study was (1) to evaluate the value of SCD risk factors, GLS and LAVI to predict appropriate ICD therapy in high-risk HCM patients and (2) to explore whether LAVI and GLS assessment provide incremental prognostic value over SCD risk factors.
Methods
Patient population
HCM patients who underwent ICD implantation for primary or secondary prevention in our centre during the last decade were evaluated. HCM was defined as presence of a non-dilated and hypertrophic LV with wall thickness ≥15 mm in the absence of any other cardiac or systemic disease that could account for the magnitude of LV hypertrophy [2]. All patients underwent extensive clinical, electrocardiographic and echocardiographic evaluation before implantation and patients’ data were prospectively collected in the departmental Cardiology Information System (EPD-Vision®, Leiden University Medical Center, Leiden, the Netherlands) and retrospectively analyzed. Patients were excluded from the analysis if 2-dimensional (2D) echocardiography was not available prior to ICD implantation. Patients with severe mitral regurgitation or prior extensive myocardial infarction were also excluded.
Clinical data included demographics, medications and identification of co-morbidities. Echocardiographic evaluation consisted of conventional measurements and included 2D-speckle tracking echocardiography for LV deformation analysis. The SCD risk profile of HCM patients was determined based on clinical and echocardiographic parameters, according to current guidelines [2]. In particular, conventional SCD risk factors were defined as secondary prevention ICD indication, family history of SCD (≥one 1st or 2nd degree relative), maximal LV wall thickness ≥30 mm, unexplained syncope or documented nsVT (≥3 beats at ≥120 bpm) prior to ICD implantation. Blood pressure response during exercise testing was not included as it was not part of clinical routine in the early years of our study period. In addition LV resting gradient ≥30 mmHg was determined.
The patient population was dichotomized based on occurrence or absence of appropriate ICD therapy at follow-up and the incremental prognostic value of LAVI and GLS was evaluated over conventional SCD risk factors.
ICD implantation and settings
All defibrillator systems used were implanted via transvenous approach. During the implant procedure, sensing and pacing threshold was determined and defibrillation threshold testing was performed. Used systems were manufactured by Biotronik (Berlin, Germany), Boston Scientific [Natick, MA, USA, formerly CPI, Guidant (St Paul, MN, USA)], Medtronic (Minneapolis, MN, USA), and St Jude Medical/Ventritex (St Paul, MN, USA). The antitachycardia settings in all devices were programmed with three consecutive zones with limits varying slightly per manufacturer: a monitor zone (lower limit between 150 and 155 bpm; upper limit between 185 and 190 bpm), an antitachycardia pacing (ATP) shock zone (lower limit between 185 and 190 bpm; upper limit between 205 and 210 bpm), and an initial shock zone (≥205–210 bpm). In the monitor zone, no therapy was programmed unless ventricular arrhythmia was detected during follow-up. In the ATP-shock zone, two bursts of ATP were administered and, if arrhythmia continued, defibrillator shocks were used. In case of ventricular arrhythmia faster than the ATP shock zone, device shocks were the initial therapy. Therapy settings were adapted only when clinically indicated.
Echocardiography
Transthoracic 2D-echocardiography was performed with the patient in left lateral decubitus position using commercially available ultrasound machines (Vivid-5, Vivid-7 and E9, GE-Vingmed, Milwaukee, WI) equipped with a 3.5 MHz transducer. ECG-triggered standard 2D gray-scale and color-Doppler images were acquired in cine-loop format and transferred to a workstation for off-line analysis (EchoPAC 110.0.0, GE Medical Systems, Horten, Norway). Chamber quantification was performed conform to current recommendations [15]. Maximal LV end diastolic wall thickness was assessed by LV evaluation in short axis view at basal, mid and apical level. LV volumes were assessed by Simpson biplane method, indexed to body surface area and used to calculate LV ejection fraction.
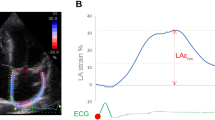
Assessment of LV GLS was performed as previously described [16]. In summary, a region of interest covering the LV myocardium in a two-, four- and apical long-axis view was selected to perform automated frame-by-frame 2D-speckle tracking throughout the cardiac cycle. Manual correction was performed to optimize tracking results when appropriate. GLS was calculated as the average peak longitudinal strain value of the two-, four- and apical long-axis view (Fig. 1). Mean frame rate for deformation analysis was 61 frames/s.
Assessment of 2D-speckle tracking global longitudinal strain. Left ventricular (LV) global longitudinal strain (GLS) is calculated as the average of the peak longitudinal strain values obtained in the 3 apical echocardiographic views. The bull’s eye view is a color-coded representation of longitudinal strain values of all tracked LV segments (deep red reflects normal strain, light red and blue reduced and severely reduced strain, respectively). a Impaired GLS in a patient with hypertrophic cardiomyopathy that experienced appropriate implantable cardioverter defibrillator (ICD) therapy. b Preserved GLS in a patient without appropriate ICD therapy
In addition, end-systolic LA volume was measured using Simpson biplane method and indexed to body surface area. LV diastolic function was analyzed assessing mitral inflow peak E (early diastolic) velocity, peak A (late diastolic) velocity, E/A ratio and deceleration time [17]. In addition, E prime was derived from the lateral wall on a four-chamber color tissue-Doppler acquisition. The presence of a systolic anterior movement of the mitral valve was also evaluated by M-mode imaging at the level of the mitral leaflets in a parasternal long-axis view. Mitral regurgitation severity was semi-quantitatively assessed, based on conventional spectral and color-Doppler echocardiography as recommended [18]. Screening for presence of an intraventricular or LV outflow tract gradient at rest was systematically performed using pulsed wave Doppler and peak gradient was measured by continuous wave Doppler.
Endpoints
Occurrence of appropriate ICD therapy, defined as ATP and/or shock for ventricular tachycardia and/or ventricular fibrillation, was the main endpoint of this study. Inappropriate ICD therapy was noted when ATP and/or shock occurred despite absence of ventricular tachycardia and/or ventricular fibrillation. ICD device interrogation was scheduled every 3–6 months after implantation and data were included until occurrence of the study end point or until last date of ICD check-up during the last year (between February 2011 and March 2012) for patients that did not experience the study endpoint.
Statistics
Continuous variables are presented as mean ± standard deviation when normal and as median with inter-quartile ranges when not normally distributed. Categorical variables are given as absolute numbers and percentages. Baseline characteristics between groups with and without appropriate ICD therapy were evaluated by Student t test, Kruskall–Wallis or χ2-test, when appropriate. In order to evaluate the association between SCD risk factors and appropriate ICD therapy, only patients with primary prevention indication were considered, for which incidence rates of appropriate ICD therapy were calculated and expressed per 100-patient years. Difference in incidence rates according to the number of SCD risk factors were tested by Poisson regression, and expressed as incidence rate ratios.
In order to identify parameters potentially associated with appropriate ICD therapy, assessment of independent predictors of appropriate ICD therapy was initially performed using a staged multivariable Cox proportional-hazards regression analysis to avoid model over-fit, given the relatively low incidence of the end point. Significant univariable predictors at a threshold p < 0.2 were entered in a first multivariable analysis that used a backward elimination approach to identify predictors of appropriate ICD therapy. Variables with p < 0.05 in the first multivariable model were entered in a second multivariable model, now containing the variables of interest, LAVI and GLS. Second, the predictive value of LAVI and GLS and conventional SCD risk factors was evaluated by receiver operating characteristic (ROC) analysis and comparison of respective areas under the curve (AUC) [19]. To define cut-offs from ROC analysis, a high sensitivity (>85 %) was stipulated to ensure identification of patients who would experience the endpoint. These cut-offs were used for subsequent analysis. Sensitivity, specificity, negative and positive predictive values for appropriate ICD therapy were calculated for LAVI and GLS, as well as conventional SCD risk factors, assuming a realistic 20 % 5-year incidence of appropriate ICD therapy. Kaplan–Meier curves were constructed for LAVI and GLS for survival free of appropriate ICD therapy, and compared by log-rank test. Additionally, the potential incremental value of LAVI and GLS over SCD risk factors to predict appropriate ICD therapy was evaluated by likelihood ratio testing and assessment of integrated discrimination improvement index (IDI). Absolute IDI is a reclassification statistic that studies a new model`s discriminatory improvement to predict the outcome variable (appropriate ICD therapy), calculated by summing the IDI components (net true predictive probabilities) of cases (patients experiencing appropriate ICD therapy) and controls (patients without appropriate ICD therapy) [20]. Finally, a similar explorative analysis was performed to test the relation of both LAVI and GLS with occurrence of inappropriate ICD therapy.
Statistical analysis was performed using SPSS version 17.0. (SPSS Inc., Chicago, IL) and STATA version 12 (STATA Corp., College Station, TX) software. All tests were two-sided and a p value of <0.05 was considered statistically significant.
Results
Patient population
A total of 92 HCM patients (69 % men, mean age 50 ± 14 years) who underwent ICD implantation were included. Baseline characteristics of the study population are summarized in Table 1. Peri-procedural echocardiography was performed at a median of 11 days before ICD implantation and all patients were in sinus rhythm at the time of echocardiographic evaluation. Despite normal LV volumes and preserved LV ejection fraction, mean GLS was impaired in the HCM patients (−13.3 ± 3.5 %). In addition, an enlarged LA volume (LAVI) was observed in these patients [39 (31–49) mL/m2]. A total of 22 patients (24 %) that survived prior cardiac arrest, sustained ventricular tachycardia or ventricular fibrillation received an ICD for secondary prevention. The remaining 70 patients (76 %) had a primary prevention indication for ICD implantation, based on the presence of ≥1 conventional SCD risk factors (n = 63), or on additional factors such as complete heart block (n = 1), LV systolic dysfunction (n = 1), inducibility of ventricular fibrillation during electrophysiological study (n = 3) or abnormal blood pressure response during exercise testing (n = 2).
Long-term ICD end points
A total of 21 patients (23 %) experienced an appropriate ICD therapy during a median follow-up of 4.7 (2.2–8.2) years (shock only n = 6, shock after unsuccessful ATP n = 3, ATP only n = 12). According to ICD interrogation, appropriate ICD therapy was given for ventricular fibrillation (n = 5), fast ventricular tachycardia in the programmed ventricular fibrillation zone (n = 12) or ventricular tachycardia in the programmed ventricular tachycardia zone (n = 4).
As shown in Table 1, patients presenting with versus without appropriate ICD therapy were more likely to be men (p = 0.02) and were characterized by more impaired GLS (p = 0.03) and increased LAVI (p < 0.001). The overall HCM risk profile did not differ significantly between both groups (all p > 0.05), although there was a trend towards higher maximal LV wall thickness and increased prevalence of nsVT and syncope prior to ICD implantation in the group of patients with appropriate ICD therapy. Of note, incidence of appropriate ICD therapy did not differ between primary and secondary ICD indication patients (p = 1.0), nor it was significantly related to the number of conventional SCD risk factors in primary prevention ICD recipients. In particular, compared with primary prevention ICD recipients with 1 SCD risk factor, patients with 2 SCD risk factors had an incidence rate ratio of appropriate ICD therapy of 1.5 (95 % confidence interval (CI) 0.93–2.6) and patients with 3 SCD risk factors had an incidence rate ratio of 2.0 (95 % CI 0.60–6.4, p for trend = 0.06) (Fig. 2).
Predictors of appropriate ICD therapy
Univariable Cox proportional-hazards regression analysis revealed LAVI, GLS, male gender, presence of nsVT and unexplained syncope prior to ICD implantation as predictors of appropriate ICD therapy (all p < 0.2) (Table 2). Staged multivariable analysis showed that LAVI and GLS, and not any SCD risk factors, were independent predictors of appropriate ICD therapy (all p < 0.05). A resting LV gradient of ≥30 mmHg was not related to appropriate ICD therapy in this patient cohort.
ROC curve analysis indicated that the presence of ≥1 SCD risk factors had limited value to predict appropriate ICD therapy when compared to both LAVI and GLS [AUC 0.52, 95 % CI 0.43–0.58 vs. AUC 0.76, 95 % CI 0.65–0.87 and AUC 0.65, 95 % CI 0.54–0.77, respectively] (p < 0.001). LAVI ≥34 mL/m2 and GLS ≥−14 % provided high sensitivity of 95 and 86 % respectively to predict appropriate ICD therapy, reaching up to 100 % if at least one of both was present (Table 3). However, the same approach showed a modest positive predictive value of 24 %. More importantly, the combined presence of LAVI <34 mL/m2 and GLS <−14 % adequately ruled out likelihood of appropriate ICD therapy, reflected by a negative predictive value of 100 %.
Finally, the Kaplan–Meier survival curves for LAVI and GLS revealed a significant difference in time to survival free of appropriate ICD therapy for both LAVI ≥34 mL/m2 versus <34 mL/m2 (p < 0.001) and GLS ≥−14 % versus <−14 % (p = 0.003) (Fig. 3). In particular, after a median follow-up of 1, 3 and 5 years a respective 12, 24 and 32 % of patients with LAVI ≥34 mL/m2 reached the endpoint, whereas their counterparts showed significantly lower cumulative event rates (0, 4 and 4 %, respectively). HCM patients with GLS ≥−14 % experienced appropriate ICD therapy in 9, 23 and 32 % after 1, 3 and 5 years, respectively, while patients with GLS <−14 % showed lower cumulative event rates of 6, 9 and 9 %.
Incremental value of LAVI and GLS to predict appropriate ICD therapy
The addition LAVI ≥34 mL/m2 to a baseline model which included the presence of ≥1 SCD risk factor(s) provided incremental value to predict appropriate ICD therapy as indicated by the likelihood ratio test (p < 0.001) and an IDI of 0.13 (p < 0.001) (Fig. 4). Sequential addition of GLS further improved prediction of appropriate ICD therapy (likelihood ratio test p = 0.02 and IDI 0.04 with p = 0.02). Therefore, adding both LAVI and GLS on top of presence of ≥1 SCD risk factors provided the best calibration for appropriate ICD therapy prediction, reflected by the likelihood ratio test p < 0.001 and IDI 0.17 with p < 0.001. Importantly, the same results were observed (IDI 0.19, p < 0.001) when only considering IDI in primary prevention indication ICD recipients (n = 70), which is of particular clinical interest as ICD implantation is unlikely to be withheld in secondary prevention indication HCM patients. Importantly, assessing both LAVI and GLS on top of conventional SCD risk factors in primary prevention patients results in reclassification of about 1 out of 5 primary prevention ICD recipients into a very low-risk group, who experienced no appropriate ICD therapy during follow-up [12/70 pts (17 %) have both LAVI and GLS below the pre-specified cut-off values with presence of 0, 1 and 2 SCD risk factors in 3 (25 %), 6 (50 %) and 3 (25 %) patients respectively].
Likelihood ratio test bar graph. This test shows incremental value of sequential assessment of left atrial volume indexed to body surface area (LAVI) and left ventricular global longitudinal strain (GLS) over conventional sudden cardiac death risk factors (SCDRF) to predict appropriate implantable cardioverter defibrillator therapy. IDI integrated discrimination improvement
LAVI, GLS and inappropriate ICD therapy
During the median follow-up of 4.7 (2.2–8.2) years 19 patients (21 %) experienced at least one inappropriate ICD therapy event. Patients with versus without inappropriate ICD therapy had similar LAVI [37.4 (33.8–45.1) versus 39.3 (31.0–48.8) mL/m2, p = 0.806] and GLS (−13.8 ± 3.23 vs. −13.2 ± 3.56 %, p = 0.579) at baseline, respectively. In addition, at univariable Cox regression analysis LAVI did not relate to occurrence of inappropriate ICD therapy [HR 1.00 (95 % CI 0.98–1.03), p = 0.800], nor did GLS [HR 0.99 (0.88–1.13), p = 0.970]. Survival free of inappropriate ICD therapy during the follow-up period was similar between patients with baseline LAVI ≥34 versus <34 mL/m2 (log rank p = 0.330) as well as for patients with baseline GLS ≥−14 versus <−14 % (log rank p = 0.670).
Discussion
The main findings of the current study can be summarized as follows: (1) the value of conventional SCD risk factors to predict appropriate ICD therapy in high-risk HCM patients was limited, however, (2) LAVI and GLS were shown to be independent predictors of appropriate ICD therapy in this population and (3) assessment of both parameters provided significant incremental predictive value over conventional SCD risk factors, particularly to identify patients at very low risk of appropriate ICD therapy (100 % negative predictive value).
SCD risk factors and appropriate ICD therapy
Although conventional SCD risk factors are established criteria to recommend ICD implantation in HCM patients, no strong evidence is currently available that these factors can also accurately predict the occurrence of appropriate ICD therapy [2]. The largest multi-center HCM registry so far, which included 506 unrelated HCM patients who underwent ICD implantation, observed in fact that no single conventional SCD risk factor, nor the number of SCD risk factors, was associated with appropriate ICD therapy [1]. A recent observational study in 1606 HCM patients (of which 19 % with an ICD) also suggested that no single SCD risk factor could increase the risk of SCD or appropriate ICD shock, although aggregation of multiple SCD risk factors did increase this risk, however, with limited power to discriminate high versus low risk subjects [21]. Similar findings were also observed in smaller single-center series [22–24]. Only one study, evaluating 104 HCM patients, identified the presence of nsVT as an independent predictor of appropriate ICD therapy, although with wide confidence limits [HR 10.3 (95 % CI 1.13–92.99)] and modest positive predictive value (22 %) [25]. Although the independent predictive value of secondary prevention indication for appropriate ICD therapy has not been shown unequivocally, appropriate ICD therapy is highly prevalent amongst secondary prevention ICD recipients and recently showed a significant association to appropriate ICD therapy on a univariable level [1, 23, 26, 27].
The results of the current evaluation are in line with previous studies, indicating rather limited predictive value of conventional SCD risk factors for appropriate ICD therapy [1]. Although conventional SCD risk factors remain mainstay to refer HCM patients for ICD implantation, additional markers are clinically needed to optimize candidate selection and allow accurate risk–benefit weighting of ICD implantation in these patients.
GLS and LAVI in HCM
HCM is a cardiomyopathy characterized by LV hypertrophy, myocardial fiber disarray and interstitial fibrosis [4, 28, 29]. These structural alterations are responsible for significant LV systolic dysfunction, which is often difficult to detect with conventional echocardiographic measures such as LV ejection fraction. Echocardiographic speckle tracking deformation imaging has been proposed as a highly sensitive technique which is able to accurately measure myocardial strain in a specific segment or in the overall LV [7]. With the use of this technique, a significant impairment of GLS was demonstrated in HCM patients, despite the presence of preserved LV ejection fraction [5, 9, 10]. In addition, impaired GLS in HCM patients has also been associated with occurrence of nsVT and adverse cardiac outcome [10].
The above-mentioned HCM structural alterations are also responsible for a significant LV diastolic dysfunction, due to impaired myocardial relaxation, and increased LV filling pressures. In addition to these factors, intra-ventricular gradients and mitral regurgitation severity are main determinants of increased LA size, a characteristic finding in many HCM patients [13, 30]. Increased LA size is therefore considered a marker of HCM disease severity and showed to be an independent predictor of adverse outcome in this population [11, 13]. Increased LA diameter has shown to be a strong mortality predictor in a study including 1491 HCM patients [31]. Most recently, O’Mahony et al. [32] reported on a large series of 3,675 relatively low-risk HCM patients (only 41 had baseline ICD, 1 %), showing LA diameter independently related to SCD or appropriate ICD shock. Asymmetric LA remodeling, however, may occur and therefore LAVI is currently recommended as the preferred parameter of LA size, as large variation in LA volume may coincide with little variation in LA diameter [11, 15, 33].
Studies in HCM patients evaluating ICD recordings prior to appropriate ICD discharge have shown that the vast majority of patients suffered from sustained monomorphic ventricular tachycardia or ventricular fibrillation, often preceded by increased heart rate due to sinus tachycardia and atrial fibrillation or late-coupled premature ventricular complexes, respectively [34, 35]. These findings indicate that coincidence of arrhythmogenic substrate (allowing for uni-directional conduction block and re-entry) as well as adequate modulators (including electrolyte disturbances, maladaptive autonomic responses affecting heart rate, intra-ventricular gradients or ischemia) are prerequisites for ventricular tachyarrhytmias in these patients [34, 35]. We hypothesize that both GLS and LAVI may indirectly reflect the underlying arrhythmogenic substrate, if not modulators, in HCM patients, including fibrosis and fiber disarray. These findings may contribute to the rationale for the independent and incremental value of both LAVI and GLS over SCD risk factors to predict appropriate ICD therapy in this population, as shown in current study.
Clinical implications
The present findings suggest that assessment of both LAVI and GLS on top of conventional SCD risk factors may optimize referral criteria and timing of ICD implantation in HCM patients at increased risk for SCD. All patients that experienced appropriate ICD therapy were identified by presence of LAVI or GLS above the cut-off value of ≥34 mL/m2 or ≥−14 % respectively (sensitivity 100 %). This strategy, however, showed a rather modest positive predictive value of 24 %, indicating that, although patients who may benefit from ICD are identified applying this approach, still a large number of ICD’s would be implanted in patients who will not experience any appropriate ICD therapy.
More importantly, when both LAVI and GLS were below the pre-specified cut-off values, a low-risk patient for appropriate ICD therapy was identified with a negative predictive value of 100 %. When applying this strategy, no single patient experienced appropriate ICD therapy during a median period of approximately 5 years. In particular, about 1 out of 5 patients (19 %) could be re-classified according to this approach as at low-risk and therefore eventually reassured that appropriate ICD therapy will not occur. These findings might therefore suggest considering the use of these parameters to delay ICD implantation in some HCM patients, with careful follow-up. This option might prevent these patients from exposure to potential adverse ICD-related events such as inappropriate therapy or device-related complications that might significantly impact on the quality of life or outcome of the ICD recipients.
Limitations
Several limitations to this study should be mentioned. The present evaluation most likely was underpowered to prove the absence of relationship between number of SCD risk factors and occurrence of appropriate ICD therapy, although our findings are in line with the largest HCM-ICD registry to date [1]. The specificity and negative predictive values of SCD risk factors to predict appropriate ICD therapy reported in the present evaluation should be interpreted with caution, as only an absolute minority of our patients presented without presence of conventional SCD risk factors. In addition, it should be emphasized that SCD risk factors are established markers and remain the cornerstone for a decision on ICD implantation in HCM patients [2]. The present results may not be generalizable to low-risk HCM patients for SCD. Therefore, given its retrospective observational single-center nature, this report should be considered as hypothesis generating and requires prospective validation in a larger HCM patient cohort.
Conclusions
Albeit conventional SCD risk factors are the cornerstone for clinical decision-making to implant ICD in HCM patients, these factors yield limited value to predict subsequent appropriate ICD therapy. Both LAVI and GLS are independent predictors of appropriate ICD therapy showing incremental benefit over conventional SCD risk factors, mainly attributed to high negative predictive value. Therefore, in addition to conventional SCD risk factors, assessment of both parameters may be clinically useful to optimize candidate selection and timing of ICD implantation, particularly to identify HCM patients at low risk for appropriate ICD therapy.
References
Maron BJ, Spirito P, Shen WK et al (2007) Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy. JAMA 298:405–412
Gersh BJ, Maron BJ, Bonow RO et al (2011) 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 124:e783–e831
Schinkel AF, Vriesendorp PA, Sijbrands EJ, Jordaens LJ, ten Cate FJ, Michels M (2012) Outcome and complications after implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy: systematic review and meta-analysis. Circ Heart Fail 5:552–559
Maron BJ (2010) Contemporary insights and strategies for risk stratification and prevention of sudden death in hypertrophic cardiomyopathy. Circulation 121:445–456
Serri K, Reant P, Lafitte M et al (2006) Global and regional myocardial function quantification by two-dimensional strain: application in hypertrophic cardiomyopathy. J Am Coll Cardiol 47:1175–1181
Kato TS, Noda A, Izawa H et al (2004) Discrimination of nonobstructive hypertrophic cardiomyopathy from hypertensive left ventricular hypertrophy on the basis of strain rate imaging by tissue Doppler ultrasonography. Circulation 110:3808–3814
Mor-Avi V, Lang RM, Badano LP et al (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr 24:277–313
Maron BJ, Maron MS (2012) Hypertrophic cardiomyopathy. Lancet 381:242–255
Paraskevaidis IA, Farmakis D, Papadopoulos C et al (2009) Two-dimensional strain analysis in patients with hypertrophic cardiomyopathy and normal systolic function: a 12-month follow-up study. Am Heart J 158:444–450
Saito M, Okayama H, Yoshii T et al (2012) Clinical significance of global two-dimensional strain as a surrogate parameter of myocardial fibrosis and cardiac events in patients with hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging 13:617–623
Losi MA, Betocchi S, Barbati G et al (2009) Prognostic significance of left atrial volume dilatation in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr 22:76–81
Tani T, Yagi T, Kitai T et al (2011) Left atrial volume predicts adverse cardiac and cerebrovascular events in patients with hypertrophic cardiomyopathy. Cardiovasc Ultrasound 9:34
Yang H, Woo A, Monakier D et al (2005) Enlarged left atrial volume in hypertrophic cardiomyopathy: a marker for disease severity. J Am Soc Echocardiogr 18:1074–1082
Yang WI, Shim CY, Kim YJ et al (2009) Left atrial volume index: a predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr 22:1338–1343
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Antoni ML, Mollema SA, Delgado V et al (2010) Prognostic importance of strain and strain rate after acute myocardial infarction. Eur Heart J 31:1640–1647
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133
Zoghbi WA, Enriquez-Sarano M, Foster E et al (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16:777–802
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Pencina MJ, D’Agostino RB Sr., D’Agostino RB Jr., Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172; discussion 207–112
O’Mahony C, Tome-Esteban M, Lambiase PD et al (2013) A validation study of the 2003 American College of Cardiology/European Society of Cardiology and 2011 American College of Cardiology Foundation/American Heart Association risk stratification and treatment algorithms for sudden cardiac death in patients with hypertrophic cardiomyopathy. Heart 99:534–541
Bos JM, Maron BJ, Ackerman MJ et al (2010) Role of family history of sudden death in risk stratification and prevention of sudden death with implantable defibrillators in hypertrophic cardiomyopathy. Am J Cardiol 106:1481–1486
O’Mahony C, Lambiase PD, Quarta G et al (2012) The long-term survival and the risks and benefits of implantable cardioverter defibrillators in patients with hypertrophic cardiomyopathy. Heart 98:116–125
Prinz C, Vogt J, Bitter T et al (2010) Incidence of adequate ICD interventions in patients with hypertrophic cardiomyopathy supposed to be at high risk for sudden cardiac death. Acta Cardiol 65:521–525
Syska P, Przybylski A, Chojnowska L et al (2010) Implantable cardioverter-defibrillator in patients with hypertrophic cardiomyopathy: efficacy and complications of the therapy in long-term follow-up. J Cardiovasc Electrophysiol 21:883–889
Vriesendorp PA, Schinkel AF, Van Cleemput J et al (2013) Implantable cardioverter-defibrillators in hypertrophic cardiomyopathy: patient outcomes, rate of appropriate and inappropriate interventions, and complications. Am Heart J 166:496–502
Woo A, Monakier D, Harris L et al (2007) Determinants of implantable defibrillator discharges in high-risk patients with hypertrophic cardiomyopathy. Heart 93:1044–1045
Bruder O, Wagner A, Jensen CJ et al (2010) Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 56:875–887
O’Hanlon R, Grasso A, Roughton M et al (2010) Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol 56:867–874
Bauer F, Shiota T, White RD et al (2004) Determinant of left atrial dilation in patients with hypertrophic cardiomyopathy: a real-time 3-dimensional echocardiographic study. J Am Soc Echocardiogr 17:968–975
Nistri S, Olivotto I, Betocchi S et al (2006) Prognostic significance of left atrial size in patients with hypertrophic cardiomyopathy (from the Italian Registry for Hypertrophic Cardiomyopathy). Am J Cardiol 98:960–965
O’Mahony C, Jichi F, Pavlou M et al (2013) A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM Risk-SCD). Eur Heart J. doi:10.1093/eurheartj/eht439
Tsang TS, Abhayaratna WP, Barnes ME et al (2006) Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol 47:1018–1023
Cha YM, Gersh BJ, Maron BJ et al (2007) Electrophysiologic manifestations of ventricular tachyarrhythmias provoking appropriate defibrillator interventions in high-risk patients with hypertrophic cardiomyopathy. J Cardiovasc Electrophysiol 18:483–487
O’Mahony C, Lambiase PD, Rahman SM et al (2012) The relation of ventricular arrhythmia electrophysiological characteristics to cardiac phenotype and circadian patterns in hypertrophic cardiomyopathy. Europace 14:724–733
Acknowledgments
None.
Conflict of interest
Dr. Philippe Debonnaire is supported by a Sadra Medical Research Grant (Boston Scientific) and holds a European Association of Cardiovascular Imaging (EACVI) Research Grant for 2013. Dr. Darryl Leong is supported by the National Health and Medical Research Council and the National Heart Foundation of Australia. Dr. Emer Joyce holds a European Society of Cardiology Clinical Training Grant. Dr. Spyridon Katsanos is supported by the Hellenic Society of Cardiology. Dr. Victoria Delgado received consulting fees from St. Jude Medical and Medtronic. The Department of Cardiology of Leiden University Medical Centre received research grants from Biotronik, Medtronic, Boston Scientific, Lantheus Medical Imaging, Edwards Lifesciences, St. Jude Medical, GE Healthcare. No specific financial support for this work is involved.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Debonnaire, P., Thijssen, J., Leong, D.P. et al. Global longitudinal strain and left atrial volume index improve prediction of appropriate implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy patients. Int J Cardiovasc Imaging 30, 549–558 (2014). https://doi.org/10.1007/s10554-014-0378-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0378-z