Abstract
Fractional flow reserve (FFR) is the gold standard in the assessment of severity of the coronary stenosis. The aim of the study was to compare optical coherence tomography (OCT) obtained intermediate coronary lesions lumen areas measurements with FFR assessments, with the goal to develop an OCT threshold to identify significant coronary stenosis. 48 patients (mean age 65 ± 10 years) was enrolled for the study. Within this population, 71 intermediate coronary lesions were investigated using both FFR and OCT. High dose bolus of Adenosine (120 μg) was used to obtain coronary hyperemia. OCT imaging was performed using non-occlusive technique to assess minimal lumen area (MLA) and diameter. The OCT cut-off value that showed the best correlation with the FFR cut-off of 0.80 was the MLA less than 2.05 mm2 (accuracy 87 %, sensitivity 75 %, specificity 90 %, p < 0.001). The study did not disclose any relationship between FFR value and the lesion length. Vessel size influenced the OCT cut-off values, with greater values being found in presence of arteries with a reference diameter greater than 3.0 mm. OCT derived minimal lumen area might be complementary to FFR measurement in identifying ischemia related lesions. Further studies are warranted to assess threshold values in relation to vessel size and location.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The assessment of stenosis severity in the presence of intermediate coronary lesion is mainly performed using fractional flow reserve (FFR), that provides a functional study of the target artery. Intravascular ultrasound (IVUS) [1, 2] or OCT [3] are alternative options offering morphological non-functional insights. Robust clinical data support the adoption of fractional flow reserve [4–6] that is nowadays the gold standard to decide whether to treat ambiguous lesions at angiography. Some operators however prefer to rely on IVUS or OCT as such technique also provide, during angioplasty, instrumental data on the adequacy of stent implantation in case of intervention [7]. These techniques are therefore applied as a surrogate of FFR to judge the severity of intermediate lesions. Some IVUS criteria have been adopted in the past to address the severity of intermediate lesions, including left main location [8–10] and a lumen area threshold of 4.0 mm2 was set to discriminate significant lesions, capable of causing myocardial ischemia. More recently new smaller cut-off have been proposed for both IVUS and OCT and particularly for the latter there is some uncertainty regarding the morphologic criteria to be applied [11–13].
The aim of the study was to compare in intermediate coronary lesions lumen areas measurements obtained with OCT with FFR assessments, with the goal to develop an OCT threshold to identify significant coronary stenosis.
Methods
Study population
Study design
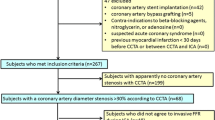
The study comprises 48 consecutive patients who were scheduled for diagnostic angiography in our Department and had angiographic intermediate coronary lesions defined as a 40–70 % reduction in percent of diameter stenosis at visual estimation. All patients were clinically stable and had FFR done to confirm or exclude the need of revascularization, applying the well validated cut-off value of 0.80 [4]. OCT imaging was performed in all cases in the effort to establish a correlation with FFR findings.
The study was approved by the local Ethics Committee.
Quantitative coronary angiography
The coronary angiography was performed using a trans-radial approach with 6 French guiding catheters. All patients received nitrates before FFR testing and after final angiography to obtain maximal coronary vasodilatation. The QCA analysis was performed offline with a computer-assisted system using an automated edge detection algorithm (QCA-CMS, MEDIS, Leiden, Netherlands) by observers unaware of OCT and FFR measurements. The studied segment was analyzed using two orthogonal views. The analysis included minimal lumen diameter (MLD), reference diameter (RD) and percent of diameter stenosis (%DS) as well as lesion length (LL).
Fractional flow reserve measurement
The FFR measurements were performed using commercially available PrimeWire (Volcano Corp. Rancho Cordoba, USA). The wire was first zeroed and advanced inside the guiding catheter until the pressure sensor reached the proximal segment of the target vessel. The aortic and wire’s pressures were normalized electronically, then the pressure wire was advanced and positioned at least 10 mm distal to the stenosis. Then, high dose bolus of adenosine was administered intracoronary (recommended dose of 120 μg). The FFR measurement was obtained as described previously, dividing distal coronary pressure (Pd) by aortic coronary pressure (Pa) (FFR = Pd/Pa). Lesions exhibiting values of 0.80 or less were considered significant and potentially causing ischemia. Measurements were repeated at least 2 times, with the lowest value being accepted for the study. The mean value of all obtained measurements was also calculated.
OCT imaging
Time-domain optical coherence tomography (TD-OCT) studies was performed using a well validated non-occlusive technique [3]. Briefly, after wiring the artery with FFR guidewire as described previously, the ImageWire (LigthLab Co.) was advanced distally to the stenosis and during continuous contast media flush (Iodixanol, Visipaque GE Heathcare), the automatic pullback was performed. The commercially available console (M2 or M3 by LigthLab Co.) was used.
Optical coherence tomography images were obtained along the region of interest (ROI) which was the angiographically detected stenosis (measured from proximal reference segment to distal reference segment—no plaque on angiography) plus 5 mm both proximal and distal to the edges of the stenosis.
Off-line analysis was performed after careful re-calibration of acquired images along the reconstructed longitudinal segment. Calibration was obtained by adjusting the z-offset, the zero-point setting of the system [14]. The analysis of the ROI was performed applying a dedicated off-line software (St Jude Medical). Quantitative measurements of the minimal lumen area (MLA) and minimal lumen diameter (OCTMLD) were obtained in all consecutive frames along the ROI using semi-automated algorithm. The frame with the smallest MLA at OCT was considered for comparison with FFR. Additionally the mean value of all LA cross-sections measured inside the ROI was calculated (AvROI-LA). Additionally, lumen volume analysis was performed along ROI—all measured LA cross-sections were summed (LVol).
Proximal and distal reference sites areas were also obtained in each lesion, measuring the LA at the start and at the end of the ROI.
Statistical test
All statistical analyses were performed using SPSS (version 10.0, SPSS Inc., Chicago, IL, USA). Data were analyzed on a per-patient and per-lesion basis. Continuous variables were presented as means ± 1 standard deviation, whereas categorical variables were presented as percentages. Continuous variables were compared using the unpaired Student t test. Categorical variables were compared using the Chi square test or Fisher’s exact test. Linear regression analyses were performed to correlate the FFR value with OCT data. To assess an independent predictors of FFR to predict FFR < 0.8, multivariable logistic regression analysis was performed; the model included OCT parameters (MLA, OCTMLD, MinMLA etc.) that correlated with positive (<0.80) FFR value. Receiver operating curves (ROCs) were used to calculated the best cutoff values of OCT parameters to determine FFR < 0.80. Area under the ROC curve (AUC) values were presented. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with 95 % confidence intervals (CI) were calculated. p values <0.05 were considered significant.
Results
Study population
In total, seventy-one intermediate lesions were included in the final analysis. The mean patient age was 65 ± 10 years. Baseline demographic and angiographic characteristics are presented in Table 1.
In 16 cases of 71 lesions, (22.5 %) fractional flow reserve was less than 0.80 and coronary angioplasty was performed. Drug eluting stents were deployed in 81.5 % of patients. Table 2 summarizes patients’ data according to FFR values (<0.80 or >0.80).
OCT determinants for FFR
The correlation between OCT MLA and FFR < 80 during hyperemia was observed (r = 0.63, p < 0.05). Consistently, a correlation with FFR was found for the AvROI-LA index (r = 0.53, p < 0.05) and the MLD (r = 0.68, p < 0.01). Of note, the study did not disclose any relationship between FFR value and the lesion length (Fig. 1).
The multivariable logistic analysis did not reveal any correlation between FFR values and demographic, angiographic and OCT variables.
The best cut-off value for FFR < 0.80 was an MLA of 2.05 mm2 (accuracy 87 %, AUC 0.91, p < 0.001). A similar correlation was obtained for the OCT minimal lumen diameter threshold of 1.28 mm (accuracy 87 %, AUC 0.90, p < 0.001) (Fig. 2) and for the of 3.72 mm2 AvROI-LA value (accuracy 88 %, AUC 0.87, p < 0.001). No relationship was found between lesion length and FFR.
Analysis performed on lumen volume along ROI have showed that mean LVol was 64.40 ± 32.30 mm3 (mean ROI length 12.3 ± 4.3 mm). Table 2 depicts LVol according to FFR findings (<0.80 or >0.80) and showed that patients with positive FFR have lower lumen volume than patients with FFR > 0.80 (p < 0.05). The best cut-off value for FFR < 0.80 was LVol of 49.5 mm3 .
To evaluate the impact of vessel size on the correlation between FFR and OCT, the angiographic reference diameter was considered. For the left anterior descending artery significant FFR values (<0.80) were best predicted by the OCT 2.96 mm2 MLA in large vessels (≥3 mm) (AUC 0.82, 95 % CI 0.55–0.96, specificity 61.5 %) and by the OCT MLA value of 1.85 mm2 in presence of small vessels (≤3 mm) (AUC 0.71, 95 % CI 0.54–0.94, specificity 100 %). The OCT MLA values for the circumflex artery were 2.96 and 2.03 mm2 respectively (AUC 0.72, 95 % CI 0.52–0.92, specificity 72.7 % and AUC 1.0, 95 % CI 0.66–1.0, specificity 100 %), whilst the OCT MLA values for the right coronary artery were 2.25 and 1.84 mm2 respectively (AUC 1.0, 95 % CI 0.69–1.0, specificity 72.7 % and AUC 1.0, 95 % CI 0.69–1.0, specificity 100 %) (Table 3).
Discussion
The present study has showed that the use of time-domain OCT can identify lesions potentially causing ischemia. OCT images coronary arteries at a resolution about 10 times higher than IVUS. In-fact the definition of the lumen-plaque border is significantly improved by OCT as compared to IVUS [3, 14]. In our group, we identified a 2.05 mm2 of MLA threshold to identify ischemia generating lesions, a value very closed to that recently identified by Gonzalo et al. [15] and Shiono et al. [16]. They identified a threshold value of 1.95 and 1.91 mm2, respectively. Some recent studies comparing IVUS and FFR [11–13] to address intermediate coronary stenosis identified new smaller morphologic criteria to indicate significant lesions. The MLA and MLD indicative of significant lesions are smaller than well known criteria developed more than a decade ago [8, 10]. According to Kang et al. [11] and Dor et al. [12] the IVUS MLA capable of revealing a significant lesions were 2.4 and 3.2 mm2, respectively. Additionally Koo et al. [13] showed that the MLA value to identify significant lesions is affected by lesion location, being larger for proximal lesions. Another variable that should be taken into account is vessel size. It was demonstrated by our study as well as by Gonzalo et al. [15] that cut-off values of OCT were smaller in vessels <3 mm by angiography than in larger ones. Taking it together (i.e. vessel size and location), one should remember that patients’ selection bias may play a role in final results. A study by Costa et al. [17] has showed that in small vessel lesions located nonproximally, there is no correlation between FFR and IVUS parameters. The opposite study by Lee et al. [18], showed a positive correlation between FFR and IVUS, but they have presented 59 % of patients with proximal, small reference diameter lesions. Artery distribution (left vs right coronary artery) may also influence final analysis results. In the present study, vessel location was distributed equally with 35 % of left anterior descending lesions while Shiono et al. [16] presented their work on 59 % patients with LAD lesion. Similarly, Kang et al. [11] analysed more than 67 % of lesion located in LAD. In their study, LAD location was a predictor of positive FFR value.
Based on the published evidence and results of the present study, it is difficult to indicate a single parameter that corresponds with negative FFR value. The variation of MLA is quite wide—from 1.59 [19] to 2.05 presented in this study. Of note, previously published reports showed that OCT derived MLA has moderate diagnostic efficiency to predict physiological significance of intermediate lesions. For example, Gonzalo et al. have proved that only MLA and MLD provided efficiency to predict a negative FFR while area stenosis by OCT or MLA by IVUS have low efficiency for FFR.
The present study has showed that in patients with positive FFR value, angiographic dimensions were quite similar like in patients with negative FFR findings, although a trend to smaller diameters in the first subgroup was observed. Comparable analysis was performed by Koo et al. [13] using intravascular ultrasound. They found that both groups were similar in terms of angiographically measured reference diameter but lumen area was significantly larger in patient s with negative FFR value. It is well known phenomenon of discrepancy between angiography and invasive imaging techniques [20]. It was also demonstrated that OCT provides smaller lumen diameters that IVUS [21], due to higher resolution.
Historic studies, including study of Briguori et al. [8] had indicated that lesion length longer than 10 mm is responsible for ischemia. According to the Poisseuille’s law, pressure drop coefficient is inversely related to minimal lumen area (as derivative of vessel radius) and positively to lesion length [22]. The study of Kolozsvari et al. [22] have showed that plaque volume derived from three dimensional angiography reconstruction correlates with positive FFR value. Recently, Giuagliumi et al. [23] confirmed that volumentric OCT assessment is better than single cross section of lumen area to predict FFR value. On the other hand, Gonzalo et al. [15] has not confirmed that IVUS measured lesion length affects positive FFR value. The present study has not found any relationship with lesion length. It could be explained by the fact that lesion length is the one of many parameters influencing results of Poisseuille’s formula. It is possible that unwitting selection bias during collecting patients is responsible for different results.
From the theoretical point of view, there are several factors that influence coronary pressure drop and myocardium ischemia consequently. Minimal lumen area, lumen volume or lesion length describe in a limited way a substitute for fractional flow reserve. The impact of lesion location and vessel size are other factors that should be consider during intermediate lesion assessment. Based on the evidence collected so far [8, 11, 15, 16, 19], there is a need to perform a detailed analysis of several variations including lesion location and vessel size. On the other hand, it was strongly indicated that OCT has potential some advantages indentifying culprit lesions in acute coronary syndromes [19, 24] and provides morphological details for optimalisation for coronary angioplasty [24, 25]. It means that OCT may play a complementary role in daily practice, especially for assessment of intermediate coronary lesions.
Treatment of intermediate stenosis is a real challenge for every cardiologist. As mention, there is no single morphological parameter (IVUS or OCT) that is reliable for deferring coronary revascularization. The mass of viable myocardium distal to intermediate lesion is responsible for final result of FFR measurement and therefore the latest European Society of Cardiology guidelines [26] advices to perform FFR either in absence of non invasive testing or in case the latter are non-conclusive regarding the presence of effort induced ischemia.
Limitations
The study was performed a few years ago, before extensive use of Frequency-domain OCT but both recent studies [15, 16] have showed similar results.
We cannot extend our results to the occlusive modality of TD acquisition. Gonzalo et al. [21] showed that vessel occlusion during OCT imaging influences vessel size and affect lumen measurements.
The route of adenosine administration was intracoronary (high dose bolus) although it was demonstrated that there is no difference in achieving hyperemia using either intravenous or intracoronary route [27].
Conclusion
OCT derived minimal lumen area might be complementary to FFR measurement in identifying ischemia related lesions. Further studies are warranted to assess threshold values in relation to vessel size and location.
References
De Bruyne B, Sarma J (2008) Fractional flow reserve: a review. Heart 94:948–959
Mintz GS, Nissen SE, Anderson WD et al (2001) ACC Clinical Expert Consensus Document on Standards for the acquisition, measurement and reporting of intravascular ultrasound studies: a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents (Committee to Develop a Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies [IVUS]). J Am Coll Cardiol 37:1478–1492
Prati F, Cera M, Ramazzotti V, Imola F, Giudice R, Albertucci M (2007) Safety and feasibility of a new non-occlusive technique for facilitated intracoronary optical coherence tomography (OCT) acquisition in various clinical and anatomical scenarios. EuroIntervention 3:365–370
Tonino PA, De Bruyne B, Pijls NH et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224
De Bruyne B, Pijls NHJ, Bartunek J et al (2001) Fractional flow reserve in patients with prior myocardial infarction. Circulation 14:157–162
Pijls NH, De Bruyne B, Bech GJ et al (2000) Coronary pressure measurement to assess the hemodynamic significance of serial stenoses within one coronary artery: validation in humans. Circulation 102:2371–2377
Gil R, Pawlowski T, Dudek D et al (2007) Comparison of angiographically guided direct stenting technique with direct stenting and optimal balloon angioplasty guided with intravascular ultrasound. The multicenter, randomized trial results Am Heart J 154:669–675
Briguori C, Anzuini A, Airoldi F et al (2001) Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol 87:136–141
De la Torre Hernandez JM, Hernandez FH, Alfonso F et al (2011) Prospective application of predefined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions: Results from the multicenter LITRO study. J Am Coll Cardiol 58:351–358
Takagi A, Tsurumi Y, Ishii Y, Kazuhito S, Kawara M, Kasanuki H (1999) Clinical potential of intravascular ultrasound for physiological assessment of coronary stenosis. Relationship between quantitative ultrasound tomography and pressure derived fractional flow reserve. Circulation 100:250–255
Kang S, Lee J, Ahn J et al (2011) Validation of intravascular ultrasound–derived parameters with fractional flow reserve for assessment of coronary stenosis severity. Circ Cardiovasc Interv 4:65–71
Dor I, Turguson R, Gaglia M et al (2011) Correlation between fractional flow reserve and intravascular ultrasound area in intermediate coronary artery stenosis. EuroIntervention 7:225–233
Koo B, Yang H, Doh J et al (2011) Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations. J Am Coll Cardiol Interv 4:803–811
Prati F, Regar E, Mintz G et al (2010) Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Euro Heart J 31:401–415
Gonzalo N, Escaned J, Alfonso F et al (2012) Morphometric assessment of coronary stenosis relevance with optical coherence tomography. A comparison with fractional flow reserve and intravascular ultrasound. J Am Coll Cardiol 59:1080–1089
Shiono Y, Kitabata H, Kubo T et al (2012) Optical coherence tomography-derived anatomical criteria for functionally significant coronary stenosis assessed by fractional flow reserve. Circ J. (advance publication; released: June 21)
Costa M, Sabate M, Staico R et al (2007) Anatomical and physiologic assessments in patients with small coronary artery disease: final results of the physiologic and anatomical evaluation prior to and after stent implantation in small coronary vessels (PHANTOM) trial. Am Heart J 153:296e1–296e7
Lee CH, Tai BC, Soon CY et al (2010) New set of intravascular ultrasound-derived anatomic criteria for defining functionally significant stenoses in small coronary arteries (results from Intravascular Ultrasound Diagnostic Evaluation of Atherosclerosis in Singapore [IDEAS] study). Am J Cardiol 105:1378–1384
Reith S, Battermann S, Jaskolka A, Lehmacher W, Hoffmann R, Marx N, Burgmaier M (2013) Relationship between optical coherence tomography derived intraluminal and intramural criteria and haemodynamic relevance as determined by fractional flow reserve in intermediate coronary stenoses of patients with type 2 diabetes. Heart 99(10):700–707. doi:10.1136/heartjnl-2013-303616
Moussa I, Kobayashi Y, Adamian M et al (2001) Characteristics of patients with a large discrepancy in coronary artery diameter between quantitative angiography and intravascular ultrasound. Am J Cardiol 88:294–296
Gonzalo N, Serruys P, García-García H et al (2009) Quantitative ex vivo and in vivo comparison of lumen dimensions measured by optical coherence tomography and intravascular ultrasound in human coronary arteries. Rev Esp Cardiol 62(6):615–624
Kolozsvári R, Tar B, Lugosi P, Sánta J, Béres Z, Ungvári T, Polgár P, Kőszegi Z (2012) Plaque volume derived from three-dimensional reconstruction of coronary angiography predicts the fractional flow reserve. Int J Cardiol 160(2):140–144
Guagliumi G, Sirbu V, Petroff C, Capodanno D, Musumeci G, Yamamoto H, Elbasiony A, Brushett C, Matiashvili A, Lortkipanidze N, Valsecchi O, Bezerra HG, Schmitt JM (2013) Volumetric assessment of lesion severity with optical coherence tomography: relationship with fractional flow. EuroIntervention 8(10):1172–1181
Stefano G, Bezerra H, Attizzani G et al (2011) Utilization of frequency domain optical coherence tomography and fractional flow reserve to assess intermediate coronary artery stenoses: conciliating anatomic and physiologic information. Int J Cardiovasc Imaging 2:299–308
Prati F, Di Vito L, Biondi-Zoccai G et al (2012) Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l’Infarto-Optimisation of Percutaneous Coronary Intervention (CLI-OPCI) study. EuroIntervention 8:823–829
Wijns W, Kolh P, Danchin N et al (2010) Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) European Association for Percutaneous Cardiovascular Interventions. Eur Heart J 31:2501–2555
Jeremias A, Whitbourn RJ, Filardo SD et al (2000) Adequacy of intracoronary versus intravenous adenosine-induced maximal coronary hyperemia for fractional flow reserve measurements. Am Heart J 140:651–657
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pawlowski, T., Prati, F., Kulawik, T. et al. Optical coherence tomography criteria for defining functional severity of intermediate lesions: a comparative study with FFR. Int J Cardiovasc Imaging 29, 1685–1691 (2013). https://doi.org/10.1007/s10554-013-0283-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-013-0283-x