Abstract
Increased aortic pulse wave velocity (PWV) results from loss of arterial compliance and is associated with unfavorable outcomes. Applanation tonometry (AT) is the most frequently applied method to assess PWV and deduce aortic compliance. The goal of this study was to compare the reproducibility of PWV measurements obtained with: (1) cross-correlation analysis of phase contrast magnetic resonance (PCMR) velocity data, and (2) applanation tonometry (AT). PWV was measured twice with each modality in 13 normal young volunteers (controls) and 9 older patients who had undergone a CT exam to evaluate coronary artery calcium. The coefficient of variation (CoV) between measurements was computed for each modality. There was no significant difference in PWV values obtained with AT and PCMR in controls or patients. The inter-scan reproducibility of PCMR was superior to AT in the controls (CoV: 3.4 ± 2.3% vs. 6.3 ± 4.0%, P = 0.03) but not in the older patients (7.4 ± 8.0% vs. 9.9 ± 9.6%, P = 0.32). PWV values were higher in patients than controls (5.6 ± 1.2 vs. 9.7 ± 2.8, P = 0.002). PCMR and AT yielded similar values for PWV in patients and volunteers. PCMR showed a superior reproducibility in young subjects but not in older patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The reduction in aortic compliance seen with aging and observed in hypertensive patients is the likely result of progressive deposition of collagen fibers in the interstitium of the vessel wall and fragmentation of elastic fibers [1]. Similar vascular remodeling processes take place during the development of atherosclerosis, in diabetes mellitus, and in chronic kidney disease [2–6]. PWV, a surrogate marker of vascular compliance via the Moens–Korteweg relationship, has been used in human studies because it does not require a pressure measurement [7, 8]. Increased PWV is a marker of cardiovascular risk [9–14] and decreases in PWV have been associated with a favorable response to various therapeutic interventions [15] and improved patient outcomes [16, 17]. The most frequently used method to measure PWV is applanation tonometry (AT), although many other methods are also available, including magnetic resonance-based methods [18–22]. We recently demonstrated the feasibility of PWV measurement in the aorta using cross-correlation analysis of phase contrast magnetic resonance (PCMR) in-plane velocity measurements [23]. In the current study, we compared the reproducibility of PCMR and AT measurements of PWV in healthy volunteers and patients asymptomatic for cardiovascular disease but who had elevated calcium scores on a screening CT exam.
Materials and methods
Subjects selection and study protocol
Subjects were either healthy, young volunteers recruited at our institution (n = 13, mean age: 33 ± 8 years) or patients undergoing CT screening for coronary artery calcium (mean age: 62 ± 4 years, Table 1). None of the patients or volunteers had a history of cardiovascular disease and all were asymptomatic at the time of imaging. All subjects signed an informed consent to participate in the study, and the study was approved by the University’s Institutional Review Board (IRB). Each subject underwent a PCMR scan followed by measurement of PWV by AT, and then the sequence was repeated the same day. This protocol allowed us to obtain two non-consecutive PWV estimates with each technique per individual within a few hours of each other.
Applanation tonometry measurements
PWV was assessed with the Sphygmocor Vx (AtCor Medical, Sydney, Australia) according to a standard protocol. First, the distance on the body surface between the sternal-notch and the femoral artery pulse was measured in centimeters. Then, the distance between the sternal-notch and the carotid artery pulse was measured and subtracted from the femoral-sternal-notch distance. This provided an approximation of the distance between the heart and the femoral artery. With the use of the tonometer, we then determined the timing of the carotid and femoral artery pulse upstroke in relation to the R-wave on a simultaneously acquired electrocardiogram. The time between the R-wave and pressure upstroke at each arterial site was then computed by the Sphygmocor Vx software and used in the calculation of the velocity of the traveling pulse wave (velocity = distance between the heart and femoral artery/time difference between R-wave and pressure upstroke at each site). The brachial arterial blood pressure was measured in the supine position with a sphygmomanometer in all patients.
Phase contrast magnetic resonance
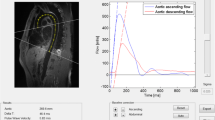
MR scans were performed on either a Philips 1.5T Intera CV (Philips Medical Systems, Best, The Netherlands) or Siemens 1.5T Avanto System (Siemens Medical Solutions, Erlangen, Germany). Patients were imaged in the supine position using a 5 or 6-element phased array cardiac coil. Survey images were acquired and used to plan oblique sagittal slices along the length of the descending aorta oriented perpendicular to the long-axis (“candy cane” view, Fig. 1a). A 2D phase contrast gradient echo sequence was acquired in this plane using a velocity encoding value of 2.0 m/sec in the foot-head direction. The sequence parameters were: TR = 3.4–4.7 ms, TE = 2.1–2.8 ms, flip angle = 15–30°, pixel size = 1.37 × 1.37 mm2 or 2.5 × 2.5 mm2, Slice thickness = 8–12 mm, acquisition matrix = 128 × 128, field of view = 17.5 cm × 17.5 cm or 32 cm × 32 cm. Using retrospective ECG-gated acquisition, 128 velocity images were reconstructed over the cardiac cycle.
a The centerline of the descending aorta was defined manually. b Cross-correlation analysis was used to compute the time shift between flow versus time waveforms at adjacent locations. c Weighted linear regression was used to fit a line to the plot of transit time versus the location along the descending aorta. The slope of this line is the pulse wave velocity
Image analysis
Image analysis was conducted with a custom-written program in MATLAB (The MathWorks, Natwick, MA). The centerline of the aorta was manually defined on a peak systolic frame for each set of phase contrast images. Velocity versus time waveforms over the cardiac cycle were generated using pixel values sampled at 30 equally-spaced locations along the user-defined centerline of the descending aorta. Using the waveform at the initial location as a reference, a cross correlation function was used to determine the time shift between the first waveform and each successive location’s waveform [23] (Fig. 1b). Using this cross-correlation analysis, the transit time of the pulse wave was computed for each location. A robust bi-square-weighted linear regression algorithm was used to fit a line to the plot of transit time versus location. The slope of this regression line is the pulse wave velocity (Fig. 1c).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD). Comparison of continuous variables was performed by means of a two-tailed t test. To assess variability we calculated the coefficient of variation for each method. The coefficient of variation was calculated as the standard deviation between two observations divided by the mean PWV measurement and expressed as a percentage. Bland–Altman plots were used to assess the average absolute difference between PCMR and AT and between two measurements obtained with each method. Statistical significance was set at a P value <0.05.
Results
In young volunteers, PCMR had a coefficient of variation 3.4 ± 2.3% compared to 6.3 ± 4.0% (P = 0.03) for AT, indicating superior reproducibility of PCMR. However, in the older patients, the coefficient of variation for PCMR (7.4 ± 8.0%) and AT (9.9 ± 9.6%) were not significantly different (P = 0.32).
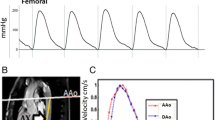
Bland–Altman analyses showed that AT had a higher PWV by 0.43 m/s (confidence interval: −2.2–3.0 m/s) compared to PCMR in young individuals. However, in older patients PCMR had a higher PWV by 0.64 m/s (confidence interval: −5.7–6.9 m/s) compared to AT (Fig. 2). The young subjects had a mean PWV of 6.1 ± 1.2 m/s using AT and 5.6 ± 1.2 m/s using PCMR (P = 0.27). Older patients had a higher PWV (9.0 ± 2.1 m/s using AT and 9.7 ± 2.8 m/s using PCMR; P = 0.57), and this was significantly higher than the PWV of young volunteers using either AT or PCMR measurements (P = 0.002 for both).
Discussion
The major findings in the current study were: (1) the reproducibility of PCMR is superior to AT in younger subjects, (2) the reproducibility of PCMR and AT was not significantly different in older patients, (3) PCMR and AT provide similar estimates of PWV in both young subjects and older patients, and (4) older patients have a higher PWV than younger subjects.
Reproducibility differences between PCMR and AT
The reproducibility of the PCMR cross-correlation technique decreased at the higher pulse wave velocities seen in older patients. This decrease in reproducibility could be due to temporal sampling issues or spatial positioning difficulties. As the wavespeed increases, the pulse wave traverses the length of the descending aorta more rapidly. For example, in a 25 cm section of the aorta with a PWV of 10 m/sec, the pulse will travel through this section of the aorta in ~3 acquired time frames. Therefore, an error in one acquired time frame would cause a 33% error in the estimate of the wavespeed. This limitation is not present in AT due to the higher sampling rate. A second reason for decreased reproducibility of PCMR in older patients could be spatial positioning issues with the slice. The PCMR technique requires the operator to position a slice through the entirety of the aorta. In older patients, the aorta is often tortuous and it is difficult to keep the aorta in a single plane; therefore, both the distance used to compute the wavespeed and the PCMR data are a potential source of error. There was a trend toward better reproducibility of PWV measurements by PCMR even in older patients. However, using the standard deviations obtained in the older patients, a power analysis indicates that 198 subjects would be needed to show a 3% difference in the reproducibility of the two techniques (3% is the difference in reproducibility between PCMR and AT in the volunteers).
It is desirable to apply a PWV measurement technique with high reproducibility when assessing patients enrolled in clinical studies that determine the effect of medical interventions on vessel compliance. A more reproducible measurement technique will provide a more reliable estimate of PWV, and allow for a reduction in the required sample size to demonstrate a change in PWV. However, in a clinical setting, AT may be preferable to PCMR due to the cost of the test, inconvenience to the patient, and the amount of time required for acquisition and data analysis.
Technique differences between PCMR and AT
Although we demonstrated that the mean PWV assessed by PCMR and AT was not statistically different, differences exist in the underlying physics of each modality. AT estimates the time of arrival of a strain pulse caused by a wave of distension and recoil that propagates along the aorta after the ejection of blood from the left ventricle. PCMR measures the arrival of blood flow at multiple locations along the aorta using time-resolved blood velocity measurements.
Differences also exist between the implementation of PCMR and AT for measurement of PWV. Measurement of PWV using the AT technique requires estimation of the distance between the heart and the peripheral pulses of interest (carotid, femoral) on the body surface. The exact length of the vessel distance cannot be measured, therefore these estimates are potentially a source of error. PCMR computes the PWV in a specific vessel or vessel segment such as the descending aorta. AT computes PWV from carotid to femoral arteries. Since these territories may age and develop atherosclerosis differently [2], the two techniques do not measure exactly the same phenomenon, and this differential may increase with the patient’s age. This technical difference may explain the absolute difference between PCMR and AT reported in the current study.
Limitations
Currently, there is no gold standard for discerning a patient’s aortic pulse wave velocity. All techniques measure surrogates of pulse wave velocity. Even intravascular pressure measurements aren’t standardized due to the variety of methods used to determine the transit time of the pulse wave. To counter this limitation, Bland–Altman analysis was used to compare AT and PCMR in this study.
This study had a small sample size compared to other clinical studies of PWV. However, the sample size was large enough to see a statistically significant difference in the reproducibility of PWV measurement techniques in normal subjects.
In conclusion, we have shown that PCMR combined with cross-correlation analysis provides a significantly more reproducible estimate of aortic PWV than AT in younger patients, but not in older subjects. PWV measurement reproducibility using PCMR can be determined in a larger future study.
References
O’Rourke MF, Nichols WW (2005) Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension 45(4):652–658
Farrar DJ, Bond MG, Riley WA, Sawyer JK (1991) Anatomic correlates of aortic pulse wave velocity and carotid artery elasticity during atherosclerosis progression and regression in monkeys. Circulation 83(5):1754–1763
Farrar DJ, Green HD, Wagner WD, Bond MG (1980) Reduction in pulse wave velocity and improvement of aortic distensibility accompanying regression of atherosclerosis in the rhesus monkey. Circ Res 47(3):425–432
Haydar AA, Covic A, Colhoun H, Rubens M, Goldsmith DJA (2004) Coronary artery calcification and aortic pulse wave velocity in chronic kidney disease patients. Kidney Int 65(5):1790–1794
Raggi P, Bellasi A, Ferramosca E, Islam T, Muntner P, Block GA (2007) Association of pulse wave velocity with vascular and valvular calcification in hemodialysis patients. Kidney Int 71(8):802–807
Wada T, Kodaira K, Fujishiro K, Maie K, Tsukiyama E, Fukumoto T, Uchida T, Yamazaki S (1994) Correlation of ultrasound-measured common carotid artery stiffness with pathological findings. Arter Thromb J Vasc Biol Am Heart Assoc 14(3):479–482
Callaghan FJ, Geddes LA, Babbs CF, Bourland JD (1986) Relationship between pulse-wave velocity and arterial elasticity. Med Biol Eng Comput 24(3):248–254
Oliver JJ, Webb DJ (2003) Noninvasive assessment of arterial stiffness and risk of atherosclerotic events. Arter Thromb Vasc Biol 23(4):554–566. doi:10.1161/01.ATV.0000060460.52916.D6
Redheuil A, Yu WC, Wu CO, Mousseaux E, de Cesare A, Yan R, Kachenoura N, Bluemke D, Lima JA (2010) Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension 55(2):319–326. doi:10.1161/HYPERTENSIONAHA.109.141275
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM (1999) Impact of aortic stiffness on survival in end-stage renal disease. Circulation 99(18):2434–2439
Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG (2002) Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 106(16):2085–2090
Meaume S, Benetos A, Henry OF, Rudnichi A, Safar ME (2001) Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arter Thromb Vasc Biol 21(12):2046–2050
Safar ME, Henry O, Meaume S (2002) Aortic pulse wave velocity: an independent marker of cardiovascular risk. Am J Geriatr Cardiol 11(5):295–298
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J (2006) Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 113(5):664–670
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD, Thurston H, O’Rourke M (2006) Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation 113(9):1213–1225
Asmar RG, London GM, O’Rourke ME, Safar ME (2001) Improvement in blood pressure, arterial stiffness and wave reflections with a very-low-dose perindopril/indapamide combination in hypertensive patient: a comparison with atenolol. Hypertension 38(4):922–926
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM (2001) Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation 103(7):987–992
Reference Values for Arterial Stiffness’ Collaboration (2010) Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J 31(19):2338–2350. doi:10.1093/eurheartj/ehq165
DeLoach SS, Townsend RR (2008) Vascular stiffness: its measurement and significance for epidemiologic and outcome studies. Clin J Am Soc Nephrol (CJASN) 3(1):184–192
Laffon E, Marthan R, Montaudon M, Latrabe Vr, Laurent Fo, Ducassou D (2005) Feasibility of aortic pulse pressure and pressure wave velocity MRI measurement in young adults. J Magn Reson Imaging (JMRI) 21(1):53–58
Rogers WJ, Hu YL, Coast D, Vido DA, Kramer CM, Pyeritz RE, Reichek N (2001) Age-associated changes in regional aortic pulse wave velocity. J Am Coll Cardiol 38(4):1123–1129
van der Meer RW, Diamant M, Westenberg JJM, Doornbos J, Bax JJ, de Roos A, Lamb HJ (2007) Magnetic resonance assessment of aortic pulse wave velocity, aortic distensibility, and cardiac function in uncomplicated type 2 diabetes mellitus. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson 9(4):645–651
Fielden SW, Fornwalt BK, Jerosch-Herold M, Eisner RL, Stillman AE, Oshinski JN (2008) A new method for the determination of aortic pulse wave velocity using cross-correlation on 2D PCMR velocity data. J Magn Reson Imaging (JMRI) 27(6):1382–1387
Acknowledgments
This study was supported by National Institutes of Health (NIH) Training Grant 5-T32-EB005969 (Suever).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suever, J.D., Oshinski, J., Rojas-Campos, E. et al. Reproducibility of pulse wave velocity measurements with phase contrast magnetic resonance and applanation tonometry. Int J Cardiovasc Imaging 28, 1141–1146 (2012). https://doi.org/10.1007/s10554-011-9929-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-011-9929-8