Abstract
We report a case of syphilitic aortitis complicated by multiple aortic aneurysms in a 50-year-old man with elevated rapid plasma reagin titer of 1:128 and positive Treponema pallidum particle agglutination test. 256-slice MDCT depicted two saccular aneurysms in the descending thoracic aorta with a markedly thick mural thrombus causing the trachea and esophagus to shift to the right. Thickening of the aortic wall was also noted. Stenting of the proximal descending thoracic aortic aneurysm and aorto-right common carotid artery bypass were performed. Operative findings revealed thickening of the descending thoracic aortic wall with a coarse luminal surface.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until the advent of antibiotic therapy, the rate of syphilitic aortic attacks was high. We report a rare case of a man with syphilitic aortitis complicated by multiple aortic aneurysms.
Case report
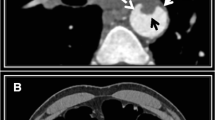
A 50-year-old man complaining of back pain was referred to our institution after he was diagnosed with multiple aortic aneurysms. He gave no history of hypertension, diabetes, smoking, or infectious diseases. The physical examination was unremarkable. Chest radiography showed a widened upper mediastinum with a tracheal shift to the right (Fig. 1a, b). Aortic CT angiography (CTA) using a 64-slice multidetector CT (MDCT) scanner confirmed two saccular aneurysms in the descending thoracic aorta (Fig. 1c, d). Among baseline pre-operative testing, the rapid plasma reagin (RPR) titer was 1:128, and the Treponema pallidum particle agglutination (TPPA) tests were positive. He received a course of antibiotics and continued supportive treatment with good control of his blood pressure. The patient’s symptoms improved with the medical treatment. One year later, the patient complained again of back pain, progressive dysphagia and hoarseness. The syphilitic serology showed a persistent positive RPR titer of 1:32. Subsequent imaging findings revealed a relatively wider upper mediastinum on chest radiograph (Fig. 2a, b). Aortic CTA using a 256-slice MDCT scanner depicted the proximal descending thoracic aortic aneurysm with a markedly thick mural thrombus causing the trachea and esophagus to shift to the right. Thickening of the aortic wall was also noted (Fig. 2c, d). Different reconstruction techniques also revealed occlusion of the innominate artery and stenosis of the celiac artery (Fig. 2e, f).
a Chest radiograph posteroanterior view showed widening of the upper mediastinum with tracheal shift to the right side (white arrow). b Chest radiograph lateral view shows a lobuted mass originating just distal to the aortic arch (black arrow), and the trachea displaced anteriorly (white arrow). c Aortic CTA axial view showed a thickened aortic wall, a large aneurysm in the proximal descending aorta with mural thrombus (arrow), and a mild tracheal (arrowhead) shift to the right. d Aortic CTA axial view showed a slightly thickened aortic wall (arrowhead) and a small aneurysm in the descending thoracic aorta (arrow)
a Chest radiograph posteroanterior view showed a wider upper mediastinum with a tracheal shift to the right side (white arrow). b Chest radiograph lateral view showed a lobulated mass originating at the level of the proximal descending aorta (black arrow), and the trachea is markedly shifted anteriorly (white arrow). c Axial CTA showed a thickened aortic wall (curved white arrow) and a proximal descending thoracic aortic aneurysm (curved black arrow) with a markedly thick mural thrombus (black star). Trachea (white star) and esophagus (white arrow) were seen to be markedly shifted to the right. d Curved planar reconstruction (CPR) CT image showed two aneurysms in the descending thoracic aorta. The larger one (curved black arrow) with a thick mural thrombus (white arrowhead) pushed the trachea (white star) and esophagus (white arrow) to the right and the smaller one (curved white arrow) is at the level of the diaphragm. e Axial CTA showed occlusion of the innominate artery (black star). f Axial CTA showed significant stenosis of the celiac artery (white arrow). g Volume rendering image showed the large aneurysm (white star), small aneurysm (arrowhead), the occlusion of the innominate artery (curved white arrow), and the significant stenosis of the celiac artery (white arrow)
Stenting of the proximal descending thoracic aortic aneurysm and aorto-right common carotid artery bypass were performed by vascular surgeons. Operative macroscopic findings revealed thickening of the descending thoracic aortic wall with a coarse luminal surface (Fig. 3).
Scanning protocols
The scan was obtained using a 64-slice MDCT scanner (Brilliance 64; Philips Healthcare, Cleveland, OH, USA) in the first scan and a 256-slice MDCT scanner (Brilliance iCT; Philips Healthcare) in the second scan. The patient was examined in the supine position with both arms extended above the head. A frontal scout view was acquired at 120 kV and 50 mA. The angiography scan was obtained in the craniocaudal direction. The imaging volume extended from the level of the subclavian arteries to the level of the origin of the femoral arteries. A collimation of 64 × 0.625 mm in the first scan or 128 × 0.625 mm in the second scan was used, with a gantry rotation speed of 0.75 s and a pith factor of 0.8. Patients were scanned with a kilovoltage of 120 kV and z-axis automatic tube current modulation in the first scan and with a kilovoltage of 80 kV and 490 mAs in the second scan. A contrast agent bolus of iopamidol 370 (80 ml; Bracco Diagnostics, SpA, Italy) was injected in the first scan and 40 ml of iopamidol 370 was injected in the second scan. The contrast agent was administered in an antecubital vein via a 20-G cannula at an injection rate of 5 ml/s using a dual-head power injector (Medrad, Indianola, PA, USA) in the first scan and 3 ml/s in the second scan. For timing purposes, automated bolus-tracing software (Bolus Pro Ultra; Philips Healthcare) was used, starting the scan automatically 6–8 s after contrast agent density in the descending aorta at the level of the aortic root reached a predefined threshold of 120 HU. The contrast material was administered followed by a 40-mL saline flush (5.0 ml/s).
Discussion
Since the advent of the antibiotics, cardiovascular syphilis, a type of tertiary syphilis, has decreased drastically, especially in developed countries. The cardiovascular manifestations of cardiovascular syphilis usually appear after 10–40 years after the primary syphilitic infection. Cardiovascular manifestations occur in 30% of patients not treated during the primary syphilis episode, and among such patients, 10–15% are symptomatic [1]. The following 4 types of cardiovascular syphilis have been described: asymptomatic syphilitic aortitis; syphilitic aortic aneurysm (40%); aortic insufficiency (29%); and coronary ostial stenosis (26%) [2]. Syphilitic aortic aneurysms occur most often in the ascending aorta (50%) and the aortic arch (30%). The descending thoracic aorta and abdominal aorta are affected in 15 and 5% of cases, respectively [1, 2]. This finding is explained by the numerous lymphatic vessels in the ascending aorta and aortic arch compared to the rest of the distal aorta. In the initial phase of syphilitic infection, T. pallidum appears in the adventitious aorta and along the lymphatic vessels and the vasa vasorum, before reaching the media. In this acute phase, the vasa vasorum is surrounded by an inflammatory infiltrate of lymphocytes and plasmocytes causing endarteritis obliterans, which leads to patchy necrosis inside the aortic media. The elastic tissue is destroyed and replaced by fibrosis along with media thinning. Thus, in the weakened wall, a syphilitic aneurysm may develop [1]. Usually a single aneurysm is present, but in 7% of cases there may be multiple aneurysms [2]. Saccular aneurysms are more common than the fusiform-shaped aneurysms. Syphilitic aneurysms carry a high risk for rupture, with fatal outcomes in 40% of cases [3]. The presence of a medial scar makes aortic dissection less common [4].
The diagnosis of syphilitic aortitis is often delayed due to the insidious course of the disease. Syphilitic aortitis is often an incidental radiologic finding; the usual infectious signs, such as fever and hyperleukocytosis, are absent. Suspicion of syphilic aortic attacks should prompt the search of signs revealing a neurologic attack (tabes dorsalis and an Argyll Robertson pupil). Compressive signs can be associated with a large aneurysm [5]. Imaging findings are not very specific for the disease. Chest radiograph shows a widened upper mediastinum and linear calcifications along the ascending aorta. A CT can sometimes shows a double-ring appearance of the aortic wall with a hyperdense outer rim and a hypodense inner rim [6]. Syphilitic serology is the most reliable aid leading to the underlying etiology; however these tests are not always positive. Among non-specific non-treponemal tests are the RPR and Venereal Disease Research Laboratory (VDRL) tests; the latter is positive in only 40% of cases [1]. The T. pallidum hemaglutination assay (TPHA), TPPA, and fluorescent treponemal antibody absorption (FTA-ABS) are more specific, and positive in 90% of cases [1]. When both the VDRL and TPHA are positive, the syphilitic infection is active. If the TPHA is positive and the VDRL is negative, then the infection is healed. Thus, in the current case the aneurysm developed during the active phase of the syphilitic infection and evolved on its own.
The MDCT features of aortitis include the thickening or calcification of the aortic wall, and arterial enhancement is considered a sign of active disease [7]. Other signs include the presence of a perivascular fluid collection, periaortic lymph nodes, and an adjacent infectious focus [8]. MDCT can be used to assess the extent of aortic and arterial calcifications [9].
The therapeutic approach is both medical and surgical. After a course of antibiotics, usually from the penicillin group, surgery is generally necessary to treat the aortic aneurysm with placement of a vascular prosthesis. Aortic insufficiency can also be treated by valvular replacement.
References
Jackman JD Jr, Radolf JD (1989) Cardiovascular syphilis. Am J Med 87(4):425–433
Heggtveit HA (1964) Syphilitic aortitis. A clinicopathologic autopsy study of 100 cases, 1950 to 1960. Circulation 29:346–355
Kampmeier RH (1938) Saccular aneurysm of the thoracic aorta: a clinical study of 633 cases. Ann Intern Med 12:624–651
Chauvel C, Cohen A, Albo C et al (1994) Aortic dissection and cardiovascular syphilis: report of an observation with transesophageal echocardiography and anatomopathologic findings. J Am Soc Echocardiogr 7(4):419–421
Phillips PL, Amberson JB, Libby DM (1981) Syphilitic aortic aneurysm presenting with the superior vena cava syndrome. Am J Med 71(1):171–173
Kimura F, Satoh H, Sakai F et al (2004) Computed tomographic findings of syphilitic aortitis. Cardiovasc Intervent Radiol 27(2):179–181
Agarwal PP, Chughtai A, Matzinger FR et al (2009) Multidetector CT of thoracic aortic aneurysms. Radiographics 29(2):537–552
Gomes MN, Choyke PL (1992) Infected aortic aneurysms: CT diagnosis. J Cardiovasc Surg (Torino) 33(6):684–689
Takahashi T, Ando M, Okita Y et al (2005) Redo aortic valve replacement with ‘‘porcelain’’ aorta in an aortitis patient. A case report. J Cardiovasc Surg (Torino) 46(1):77–79
Conflict of interest
The authors do not have any possible conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, J., Yuan, Q., Golamaully, R. et al. Syphilitic aortitis complicated by multiple aortic aneurysms: findings of multidetector CT. Int J Cardiovasc Imaging 27, 695–699 (2011). https://doi.org/10.1007/s10554-011-9873-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-011-9873-7