Abstract
To evaluate the effects of age and pulmonary hypertension on phasic right atrial function we measured right atrial volumes at 3 different points in the cardiac cycle in 57 healthy subjects and 33 patients with pulmonary arterial hypertension. Right atrial reservoir function was assessed by systolic filling volume and passive and active emptying by passive and active emptying volume and fraction of total emptying. We compared these phases of right atrial function in 30 healthy subjects <60 and 27 ≥ 60 years old, and in a separate analysis, in 33 patients with pulmonary arterial hypertension and 33 matched controls. Healthy subjects ≥60 years had lower passive emptying fraction (46.0 ± 23.3% vs 59.9 ± 15.4%, P = 0.011) and larger active emptying volume (7.0 ± 3.5 vs 4.9 ± 2.5 ml/m2, P = 0.013 ) and fraction (54.0 ± 23.3% vs 40.1 ± 15.4%, P = 0.011) compared to those <60. Patients with pulmonary arterial hypertension had larger right atrial volumes, systolic filling volume (18.3 ± 6.9 vs 12.3 ± 4.9 ml/m2, P ≤ 0.001) and active emptying volume and fraction (11.2 ± 6.9 vs 5.4 ± 3.0 ml/m2, P ≤ 0.001; 60.7 ± 29.9 vs 44.9 ± 19.0%, P = 0.017 ) and smaller passive emptying fraction (39.3 ± 29.9% vs 55.1 ± 19.0%, P = 0.017) compared to controls. Aging and pulmonary arterial hypertension are associated with a decrease in passive right atrial emptying and an increase in right atrial active emptying.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The right and left atria perform 3 different functions during the various phases of the cardiac cycle, serving as reservoirs during systole, passive conduits during early diastole, and booster pumps during late diastole [1]. Recently there have been multiple studies of phasic left atrial function using either Doppler flow or echocardiographic changes in left atrial area and volume during the cardiac cycle [2–10]. These investigations have reported that the relative contribution of the components of phasic left atrial function to left ventricular filling are affected by several factors including age, [2–5] hypertension [6–7] and left ventricular dysfunction [8–10]. A smaller number of studies, primarily using conventional or tissue Doppler imaging, have shown that right atrial active emptying is also affected by some of these factors with an increase in right atrial pump function reported in the elderly [3,11–14] and pulmonary arterial hypertension patients [15–16]. Another study used acoustic quantification to measure right atrial areas continously during the cardiac cycle and evaluate both the passive and active phases of right atrial emptying. This study reported that right atrial passive emptying was reduced and active emptying elevated in patients with pulmonary arterial hypertension compared to normal controls, but only studied 11 pulmonary arterial hypertension patients [17]. Although increased right atrial reservoir function has been reported in an animal model of pulmonary arterial hypertension, [18] the effects of age and pulmonary arterial hypertension on right atrial reservoir function have not been extensively studied in humans. The current study examines the efffects of age and pulmonary arterial hypertension on all 3 phases of right atrial function by measuring changes in right atrial volume during the cardiac cycle using 2-dimensional transthoracic echocardiography.
Methods
Subjects
This study consists of 2 parts. For the first part which evaluated the effects of age on right atrial function, we reviewed the clinical records of 1,186 patients 20–85 years old referred to a university-affiliated echocardiography laboratory for standard indications between July 2004 and June 2005. From these patients, we identified 62 healthy subjects without cardiovascular disease, renal failure, diabetes or hypertension. Subjects classified as healthy were required to be in in normal sinus rhythm and to not have a history of myocardial infarction, angina pectoris, heart failure, atrial fibrillation, left bundle branch block, previous surgical or percutaneous coronary revascularization, coronary artery stenosis ≥50% at angiography, or previous abnormal stress test. Subjects were excluded if the index echocardiogram showed any valvular regurgitaion greater than trivial, any degree of valve stenosis, pulmonary artery systolic pressure ≥40 mm Hg, pericardial disease, right or left ventricular regional wall motion abnormalities or ejection fraction <50% determined qualitatively, and if undergoing stress echocardiography, exercise induced electrocardiographic or wall motion abnormalities. Other exclusion criteria included fasting blood sugar >126 mg/dl or the use of glucose lowering medication or diet, systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg during at least 1 clinic visit or use of antihypertensive medication, and renal replacement therapy or serum creatinine ≥2.0 mg/ml.
For the second part of this study which evaluated the effects of pulmonary arterial hypertension on right atrial function, we identified 33 patients from the pulmonary arterial hypertension clinic who had undergone transthoracic echocardiography by cross referencing the clinic lists with our echocardiographic data base. All pulmonary arterial hypertension patients had pulmonary artery systolic pressure ≥40 mm Hg on echocardiography. The etiology of pulmonary arterial hypertension in these patients was idiopathic pulmonary arterial hypertension in 15 (46%), scleroderma or other connective tissue disorder in 8 (24%), portopulmonary hypertension in 5 (15%), obstructive sleep apnea in 2 (6%) and chronic lung disease, atrial septal defect and chronic thromboembolic pulmonary hypertension in 1 (3%) each. For comparison with these patients, we selected 33 subjects from our healthy cohort who were matched for age, gender and body surface area with the pulmonary arterial hypertension patients to serve as controls.
Pemission to review patient records and echocardiograms was granted by the institutional review board of our facility.
Echocardiography
The subjects of this study had complete transthoracic 2-dimensional and Doppler echocardiography performed for standard clinical indications. Standard echocardiographic views were obtained in the left lateral decubitus position during quiet respirations after 10 min of rest as per our laboratory protocol using commercially available equipment (Sonos 5500 or IE33, Philips Medical Systems, Bothell, Washington or Vivid 7, GE Vingmed, Milwaukee, WI) and stored digitally. Digitally-stored echocardiograms were reviewed on off-line work-stations (Xcelera, Philips Medical Systems or Echopac 6, GE Vingmed) by a single reader (HJW) to avoid interobserver variability.
We measured right atrial volumes at 3 points in the cardiac cycle using single plane method of discs by manually tracing endocardial borders in the apical 4-chamber view (Fig. 1a–c). A straight line connecting the insertion points of the anterior and septal leaflets of the tricuspid valve to the annulus was drawn to define the inferior border of the right atrium. In cases of septal dropout, the interatrial septum was traced by reconstruction from the visualized segments. Measurements were made from 2 cardiac cycles and averaged. Maximum RA volume (RAmax) was measured at end systole from the frame immediately preceding tricuspid valve opening (Fig. 1a). Right atrial volume before atrial contraction (RAp) was measured at the onset of the P wave of the electrocardiogram (Fig. 1b). Minimum right atrial volume (RAmin) was measured at end diastole from the frame coinciding with tricuspid valve closure (Fig. 1c). Phasic right atrial function was evaluated by calculating changes in volume during the cardiac cycle. Right atrial reservoir function was assessed by systolic filling volume (RAmax-RAmin). Passive emptying during early diastole was evaluated by passive emptying volume (RAmax-RAp) and passive emptying fraction of total emptying (RAmax-RAp/RAmax-RAmin). Right atrial contractile function during late diastole was assessed by active emptying volume (RAp-RAmin) and active emptying fraction of total emptying (RAp-RAmin/RAmax- RAmin). To adjust for body size, all right atrial volumes and volumetric measures of phasic function were indexed to body surface area. To test for intraobserver variabilty, measurements were repeated in 15 randomly selected patients aproximately 7 days after the initial reading and coefficients of variation were calculated. The coefficients of variation were 4.6, 6.1 and 6.3% for RAmax, RAp and RAmin respectively.
Pulmonary artery systolic pressures were determined from the peak tricuspid regurgitant velocity recorded from multiple views averaged over 2 cardiac cycles plus estimated right atrial pressure. Right atrial pressure was estimated from the respiratory dynamics of the inferior vena cava [19].
Statistical analysis
Continuous variables are reported as means ± SD and categorical variables as number and percentages. Demographic and clinical characteristics were compared using unpaired t-test for continuous and chi-square tests for categorical variables. In order to evaluate the effects of age on right atrial function in the first part of the study, we divided the 57 healthy subjects into 30 subjects <60 years old and 27 ≥ 60 years. Right atrial size and function during the 3 phases of the cardiac cycle were compared in subjects < and ≥ 60 years old with unpaired t-test. Also, the association of age and the 3 phases of right atrial function were evaluated with Pearson’s correlation coefficients (r). In a separate analysis for the second part of the study, we compared right atrial size and phasic function in 33 pulmonary arterial hypertension patients and 33 healthy subjects matched for age, gender and body surface area using unpaired t-test. In this part of the study, the association of pulmonary artery systolic pressures with the 3 phases of right atrial function was evaluated with Pearson’s correlation coefficients (r). All test results with a 2-sided P-value <0.05 were considered statistically significant. All analyses were performed with the NCSS Statistical Software for Windows (Kaysville, Utah).
Results
The echocardiograms were of acceptable quality for measuring right atrial volumes in 57 of the 62 healthy subjects who form the study group for the first part of this study. Right atrial volumes could be measured in all 33 patients with pulmonary arterial hypertension and matched controls. The tricuspid regurgitation spectral Doppler signal was adequate for estimating pulmonary artery systolic pressure in all 33 patients with pulmonary arterial hypertension and in 21 of the 33 matched control subjects.
Effects of age on phasic right atrial function
Table 1 shows the demographic and clinical characteristics of healthy subjects ≥60 and <60 years old. Gender distribution, body surface area and heart rate did not significantly differ between the 2 groups. Table 2 reports the right atrial volumes and volumetric indexes of phasic right atrial function in subjects ≥ and <60 years old. There were no statistically significant differences in RAmax, RAmin, or systolic filling volume. RAp at end of passive emptying was significantly larger in subjects ≥60 years compared to the younger subjects (19.5 ± 8.8 vs 15.2 ± 6.0 ml/m2, P = 0.032). Active emptying volume and fraction of total emptying were significantly larger in those ≥60 years (7.0 ± 3.5 vs 4.9 ± 2.5 ml/m2, P = 0.013; 54.0 ± 23.3% vs 40.1 ± 15.4%, P = 0.011). Passive emptying fraction of total emptying was smaller in subjects ≥60 years compared to <60 (46.0 ± 23.3% vs 59.9 ± 15.4%, P = 0.011). Passive emptying volume was smaller in those <60 years although the difference was not statistically significant (P = 0.426).
Among the 57 healthy subjects, age correlated with active emptying volume and fraction of total emptying (r = 0.27, P = .048, r = 0.32, P = 0.017), respectively and inversely with passive emptying fraction of total emptying (r = −0.32, P = 0.017).
Effects of pulmonary arterial hypertension on phasic right atrial function
Table 3 presents the demographics, clinical variables and pulmonary artery systolic pressures of pulmonary arterial hypertension patients and age- and sex-matched controls. As required by the study criteria, there were no statistically significant differences in sex, age or body surface area between pulmonary arterial hypertension patients and matched healthy controls. However, heart rate and, as expected, pulmonary artery systolic pressure were significantly higher in the patients.
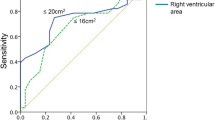
Table 4 presents the right atrial volumes and volumetric measures of phasic right atrial function in pulmonary arterial hypertension patients and controls. RAmax, RAp, RAmin, and systolic filling volume were all significantly larger in patients compared to controls (57.3 ± 28.0 vs 23.0 ± 7.4 ml/m2, P < 0.001; 50.2 ± 29.4 vs 16.1 ± 6.7 ml/m2, P < 0.001; 38.9 ± 27.5 vs 10.7 ± 4.4 ml/m2, P < 0.001; 18.3 ± 6.9 vs 12.3 ± 4.9 ml/m2, P < 0.001). Active emptying volume and fraction of total emptying were significantly larger in patients (11.2 ± 6.9 vs 5.4 ± 3.0 ml/m2, P ≤ 0.001; 60.7 ± 29.9 vs 44.9 ± 19.0%, P = 0.017). Passive emptying fraction of total emptying was lower in patients compared to controls (39.3 ± 29.9% vs 55.1 ± 19.0%, P = 0.017). There was no statistically significant difference in passive emptying volume between the 2 groups.
Among the patients with pulmonary arterial hypertension and matched controls pulmonary artery systolic pressure correlated with active emptying volume and fraction of total emptying (r = 0.60, P < 0.001, r = 0.30, p = 0.038), respectively and inversely with passive emptying fraction of total emptying (r = −0.30, P = 0.038).
Discussion
Using volumetric indexes of right atrial size and phasic function determined by 2-dimensional transthoracic echocardiography, we observed that passive right atrial emptying in early diastole is decreased and active emptying in late diastole is increased in healthy subjects ≥60 years compared to those <60. We also observed that right atrial systolic filling volume and active emptying are increased and passive right atrial emptying is decreased in pulmonary arterial hypertension patients compared to matched controls. As expected RAmax, RAp, and RAmin were increased in our patients with pulmonary arterial hypertension.
Our observation of a redistribution of right atrial emptying with a greater dependence on booster pump function in healthy subjects ≥60 years is consistent with other studies that have shown a larger contribution of atrial contraction to right ventricular filling with age using conventional Doppler of transtricuspid and hepatic vein flow [11–14]. Our findings are also consistent with recent tissue Doppler imaging studies [3,13]. These studies reported a higher tissue Doppler-derived velocity of the mid right atrial free wall during late diastole in subjects ≥60 years [3] and an inverse relationship between age and ratio of early and late diastolic lateral tricuspid annular velocities [13].
Our observation of increased atrial active emptying volume and fraction and decreased passive emptying fraction in pulmonary arterial hypertension patients is also in agreement with the observations of other investigators who reported an increase in right atrial size and ratios of active atrial emptying to total atrial emptying and stroke volume in these patients [15–17]. We extend their findings about right atrial active and passive emptying in pulmonary arterial hypertension patients to reservoir function by describing higher systolic filling volume. This latter observation of greater reservoir contribution has also been reported in an experimental model of chronic pulmonary arterial hypertension in dogs created by progressive banding of their main pulmonary artery. In that study, reservoir volume assessed by directly measuring superior and inferior vena cava inflow during systole with ultrasonic flow probes was increased after 3 months of pulmonary arterial hypertension compared to baseline preoperative measurements [18].
The changes in right atrial phasic function observed in this study in subjects ≥60 and pulmonary arterial hypertension patients are also in accordance with reports on volumetric indexes of phasic left atrial function, which has been studied much more extensively. Studies of left atrial function have reported increased left atrial active emptying and decreased passive filling with aging [2–5], systemic arterial hypertension [6–7], and aortic stenosis [20]. Thus the response of both atria to age and increased after load to their respective ventricles appears analogous. The proposed mechanism of these changes in phasic left atrial function is impaired left ventricular relaxation associated with aging or cardiovascular disorders causing a decrease in rate of early diastolic emptying of the left atrium. This decrease is accompanied by increased volume at the onset of left atrial systole which augments atrial contraction through Frank-Starling law. This increases late left ventricular filling and pressure and maintains cardiac output [4]. Since there is also a decline in right ventricular diastolic function with age [11–14] and pulmonary arterial hypertension [16], it is tempting to speculate that similar mechanisms occur in the right sided cardiac chambers [16].
Studying changes in phasic right atrial function may be clinically important. While the increase in left atrial active emptying and volume in the elderly and patients with cardiovascular disorders is compensatory for maintaining cardiac output, it may also cause structural and electrophysiological changes in the left atrium that predispose to developing atrial fibrillation [21]. In patients with atrial fibrillation not triggered by ectopy, right atrial reentry may be an important mechanism for initiating and maintaining atrial fibrillation [22]. Whether the changes in right atrial emptying and volume with age and pulmonary arterial hypertension provide the substrate for developing right atrial reentry and atrial fibrillation warrants further study.
Our study has several important limitations. Although we and others [23] believe that the volumetric indexes we used provide a more direct and comprehensive assessment of right atrial function than Doppler measurements of tricuspid or hepatic vein flow, they are more dependent on acoustic windows and image quality than Doppler. We measured right atrial size and function in this study by retrospectively reviewing echocardiograms that were performed previously for clinical reasons. Gain and other technical factors may not have been adjusted to achieve the clearest definition of the right atrial endocardium. However, the 5 cases with inadequate visualization of right atrial endocardium were excluded from analysis. Also, the sonographers performing these clinical studies may not have oriented images of the right atrium to maximize its size. However, Doppler may also be influenced by technical factors including loading conditions during time of study, respiration, transducer position and angle of incidence. Another limitation is that the single plane planimetry method of discs used to estimate right atrial volumes makes several geometric assumptions about right atrial shape. This method has been less well validated than biplane methods used to measure the left atrium. However, this bias was maintained throughout the study. In addition our mean RAmax in healthy subjects <60 years was very close to the normal indexed value of 21 ml/m2 described in the recently published American Society of Echocardiography guidelines for chamber quantificiation [24, 25]. Sample size for both parts of our study was small but it is challenging to identify patients without any cardiovascular disease in a referral population and pulmonary arterial hypertension is not a common disease. Because our healthy subjects were referred to our laboratory for clinical reasons, our results may not be generalizable to all populations. Compared to controls, patients with pulmonary arterial hypertension had higher heart rates which are known to increase the contribution of active emptying to total right atrial emptying [3]. However, it is difficult to match the heart rates of controls and pulmonary arterial hypertension patients because of their different clinical and hemodynamic status. Finally, the changes in phasic right atrial function observed in pulmonary arterial hypertension patients might vary depending on disease duration and severity as well as the status of right ventricular function. Our sample size of pulmonary arterial hypertension patents was inadequate for sub group analysis to address these issues.
Despite these and other limitations, the most plausible interpretation of our data is that all 3 phases of right atrial function can be evaluated with transthoracic echocardiography by measuring changes in volume during the cardiac cycle. Passive right atrial emptying is lower and booster pump function greater in older healthy subjects and pulmonary arterial hypertension patients. Reservoir volume is higher in pulmonary arterial hypertension patients. This redistribution of the relative contribution of the phases of right atrial function to right ventricular filling is analogous to changes reported in the left atrium in response to similar stimuli. Whether these changes contribute to the development of atrial fibrillation and are a target for preventive therapy warrants further study.
Abbreviations
- RAmax:
-
Maximum right atrial volume
- RAp:
-
Right atrial volume before atrial contraction
- RAmin:
-
Minimum right atrial volume
References
Stefanadis C, Dernellis J, Toutouzas P (2001) A clinical appraisal of left atrial function. Eur Heart J 22:22–36
Spencer KT, Mor-Avi V, Gorscan J III et al (2001) Effects of aging on left atrial reservoir, conduit and booster pump function: a multi-institution acoustic quantification study. Heart 85:272–277
Zhang Q, Kum LCC, Lee P-W et al (2006) Effect of age and heart rate on atrial mechanical function assessed by Doppler tissue imaging in healthy individuals. J Am Soc Echocardiogr 19:422–428
Triposkiadis F, Tenolouris K, Androulakis A et al (1995) Left atrial mechanical function in the healthy elderly: new insights from a combined assessment of changes in atrial volume and transmitral flow velocity. J Am Soc Echocardiogr 8:801–809
Spencer KT, Mor-Avi V,Weinert L et al (1998) Age dependency of left atrial and left ventricular acoustic quantification waveforms for the evaluation of diastolic performance in left ventricular hypertrophy. J Am Soc Echocardiogr 11:1027–1035
Erol MK, Yilmaz M, Mahmut A et al (2002) Left atrial mechanical function in patients with essential hypertension. Acta Cardiol 57:323–327
Cioffi G, Mureddu GF, Stefenelli C et al (2004) Relationship between left ventricular geometry and left atrial size and function in patients with systemic hypertension. J Hypertens 22:1589–1596
Gottdiener JS, Kitzman DW, Aurigemma GP et al (2006) Left atrial volume, geometry,and function in systolic and diastolic heart failure of persons > 65 years of age (The Cardiovascular Health Study). Am J Cardiol 97:83–89
Dernellis JM, Stefanadis CI, Zacharoulis AA et al (1998) Left atrial mechanical adaptation to long-standing hemodynamic loads based on pressure-volume relations. Am J Cardiol 81:1138–1143
Prioli A, Marino P, Lanzoni L et al (1998) Increasing degrees of left ventricular filling impairment modulate left atrial function in humans. Am J Cardiol 82:756–761
Klein Al, Leung DY, Murray RD et al (1999) Effects of age and physiological variables on right ventricular filling dynamics in normal subject. Am J Cardiol 84:440–448
Spencer KT, Weinert L, Lang RM (1999) Effects of age, heart rate and tricuspid regurgitation on Doppler echocardiographic evaluation of right ventricular diastolic function. Cardiology 92:59–64
Kukulski T, Hubbert L, Arnold M et al (2000) Normal regional right ventricular function and its change with age: a Doppler myocardial imaging study. J Am Soc Echocardiogr 13:194–204
Yu CM, Sanderson JE (1997) Right and left ventricular diastolic function in patients with and without heart failure: effect of age, sex, heart rate, and respiration on Doppler-derived measurements. Am Heart J 134:426–434
Lambertz H, Krebs W, Schectem U et al (1985) Analysis of right atrium function in patients with chronic pressure overload of the right ventricle. Z Kardiol 74:402–408
Cioffi G, de Simone G, Mureddu G et al (2007) Right atrial size and function in patients with pulmonary hypertension associated with disorders of respiratory system or hypoxemia. Eur J Echocardiogr 8:322–31
Spencer KT, Garcia MJ, Weinart L et al (1999) Assessment of right ventricular and right atrial systolic and diastolic performance using automated border detection. Echocardiography 16:643–652
Gaynor SL, Maniar HS, Bloch JB et al (2005) Right atrial and ventricular adaptation to chronic right ventricular pressure overload. Circulation 112(suppl I):I-212–I-218
Kirchmer BJ, Himmelman RB, Schiller NB (1990) Noninvasive estimation of right atrial pressure from inspiratory collapse of the inferior vena cava. Am J Cardiol 66:493–496
Cioffi G, Stefenelli C (2002) Comparison of left ventricular geometry and left atrial size and function in patients with aortic stenosis versus those with pure aortic regurgitation. Am J Cardiol 90:601–6
Tsang TSM, Barnes ME, Bailey KR et al (2001) Left atrial volume: important risk marker for incident atrial fibrillation in 1655 older men and women. Mayo Clin Proc 76:467–475
Lin Y-J, Tai C-T, Kao T et al (2005) Electrophysiological characteristics and catheter ablation in patients with paroxysmal right atrial fibrillation. Circulation 112:1692–1700
Dernellis J. (2001) Right atrial function in hypertensive patients: effects of antihypertensive therapy. J Hum Hypertens 15:464–470
Lang RM, Bierig M, Devereux RB et al (2005) Chamber quantification writing group; American society of echocardiography’sguidelines and standards committee; European association of echocardiography.recommendations for chamber quantification: a report from the American society of echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European association of echocardiography, a branch of the European society of cardiology. J Am Soc Echocardiogr 18:1440–63
Wang Y, Gutman JM, Heilbron D et al (1984) Atrial volume in a normal adult population by two-dimensional echocardiography. Chest 86:595–601
Acknowledgments
This work was partially supported by the Schecter Family Foundation, Miami, Florida.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Willens, H.J., Fertel, D.P., Qin, J. et al. Effects of age and pulmonary arterial hypertension on the different phases of right atrial function. Int J Cardiovasc Imaging 24, 703–710 (2008). https://doi.org/10.1007/s10554-008-9306-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-008-9306-4