Abstract
Background: The ability to track dynamic changes in myocardial blood flow (MBF) and wall motion with serial gated perfusion imaging may be a limiting factor in assessing new therapies. The purpose of this study was to determine whether gated Tc-99 m sestamibi (MIBI) SPECT imaging can track small changes in MBF in a model of progressive ischemia. Methods: Eight pigs (20 kg) underwent lateral thoracotomy for placement of an ameroid constrictor on the left circumflex coronary artery (LCX) and indwelling femoral and left atrial catheters for serial microsphere determinations of absolute MBF. Animals underwent concurrent left atrial microsphere and Tc-99 m sestamibi (0.3 mCi/Kg IV) injections at weekly intervals over 6 weeks per animal. Gated SPECT imaging was acquired for each injection using high resolution collimation and standard processing. The animals were sacrificed on day 42. Mean signal intensity (SI) from regions of interest (ROI) corresponding to control and ischemic MBF by microspheres was measured for three SPECT short-axis images. Mean contrast ratio (MCR) was calculated from the ratio of ischemic to control SI per slice. Regional wall motion (RWM) from gated images was scored 1–5 using a 16 segment model and a score index (RWMI) was calculated. Results: MBF decreased progressively (27% below resting values [P < 0.0001]) but with a clear and significant partial recovery by day 42 (13% improvement from peak ischemia, [P < 0.01]). SPECT perfusion and gated RWM closely paralleled the dynamic pattern of MBF caused by the ameroid constrictor. SPECT MCR decreased 21% from baseline scans in the LCX territory (P < 0.0001) and improved 11% from peak ischemia (P < 0.01) while the gated RWMI (1.0 at baseline) peaked at 1.36 and improved to 1.13 by day 42. Conclusion: Gated SPECT-a technique readily available-tracks dynamic changes in MBF closely with both perfusion and RWM. For trials of new therapies for the alleviation of chronic ischemia, these findings have direct implications for measuring efficacy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The augmentation of myocardial blood flow (MBF) with novel approaches continues to evolve at a rapid pace. The increases achieved in MBF with these techniques may be less than those seen with percutaneous coronary interventions and bypass surgery [1] and so present quantitative challenges. Perfusion imaging is commonly employed clinically as a serial testing tool but controlled temporal reproducibility data is limited [2–4]. Investigators have extrapolated the use of clinical serial perfusion imaging to assess new anti-ischemic therapies with mixed results [5–9]. The purpose of this study was to determine whether serial imaging with gated Tc-99 m sestamibi SPECT can accurately reflect the relatively small changes in MBF in the setting of chronic myocardial ischemia as compared to myocardial blood flow determined by microsphere injection.
Methods
Model preparation
All animals received humane care and all members of the animal care team underwent animal care and use training. This study was reviewed by the Mayo Clinic Institutional Animal Care and Use Committee and complied with all institutional guidelines of the Mayo Clinic for animal research. Sus scrofa swine (n = 10) were anesthetized with IV xylazine and pentabarbitol and intubated for mechanical ventilation. The femoral artery was isolated and an indwelling silastic catheter introduced and externalized to the skin surface. A lateral thoracotomy was performed for surgical dissection of the left circumflex artery (LCX) for placement of an ameroid constrictor [10]. This is a ring like structure (with a gap to allow placement around a vessel) with a rigid outer surface and a soft porous inner surface. The inner material swells over time on exposure to fluid, progressively narrowing the bore of the ring and producing passive vessel constriction. A silastic catheter was placed in the left atrium and externalized for subsequent microsphere injections during the course of the experiment. The animals were allowed to recover and were housed 42 days at which time they were sacrificed. Two pigs died during surgery to give a total of eight animals who completed the protocol. The left atrial catheter clotted off on one animal precluding a final MBF determination.
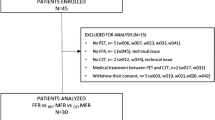
Protocol (Fig. 1)
Following the completion of surgery, pigs were injected with 1 ml of sonicated microspheres (IMT Stason Labs, Irvine, CA) for myocardial blood flow measurement at baseline. Within 10–15 min, Tc-99 m sestamibi (0.3 mCi/Kg) was injected IV and imaging commenced 10 min later. This process was repeated after day 21 and then weekly until sacrifice, for a total of five SPECT determinations per animal. Constriction of the ameroid was inferred from microsphere values in the LCX territory and subsequent myocardial necrosis by triphenlytetrazolium chloride (TTC) staining.
A. Infarct size measurement
Because myocardial necrosis impacts upon sestamibi uptake and retention [11–13], it was considered important to observe the degree of infarction that a proximal ameroid may produce. Following sacrifice, the heart was excised and sliced into 1 cm thick short-axis slices. These were stained with 1% TTC, digitally photographed and displayed on a high resolution monitor. Infarct area was planimetered using an image analysis software package (NIH Image) and expressed as a percentage of the left ventricle [14].
B. Microsphere determination of absolute MBF
Approximately 5 million fluorescent colored microspheres (1 ml) with a diameter of 15 μm (Nu Flow, IMT labs, Irvine CA) were injected into the left atrium with simultaneous withdrawal of a reference sample at a rate of 7.75 ml/min × 2 min from the descending aorta with a different color for each determination of MBF. Following sacrifice, the 1 cm thick short-axis slices were sectioned radially and further divided into endocardial and epicardial zones. Segments and reference samples were sent for ultracentrifugation and analysis by an outside commercial laboratory (IMT Labs, Irvine CA). Calculation of absolute MBF was done using conventional formulae [15, 16] with the use of a reference blood sample withdrawn at a known rate during microsphere injection. The values per segment were plotted circumferentially for all five determinations and the ischemic region of the lateral wall was identified. Occlusion MBF was taken as the average of two segments for three short-axis slices (apical, mid-ventricle, and base) unless the zone was confined to one segment. Epicardial and endocardial values were averaged to obtain transmural MBF. Control zone values were taken from the unaffected inferoseptal region. Because rest control MBF can change as a result of ischemia and indwelling catheter line infection/inflammation, MBF values were normalized in all cases to the control zone at midventricle for each determination.
C. Tc-99 m Sestamibi gated SPECT
Images were acquired 10 min following injection of the tracer with a dual headed camera (El-Scint Cardial, GE, Milwaukee, WI) equipped with high resolution collimators. Each head rotated 90 degrees acquiring 15 images at 60 s per image. Acquisition was gated to R wave and acquired into 16 temporal frames which were subsequently merged into eight frames over the cardiac cycle [17]. Perfusion SPECT images were reconstructed using standard filtered background projection and displayed in vertical and horizontal long axis views and short-axis views. Attenuation correction was not available on the imaging system.
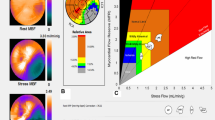
All analyses were performed off three short-axis views which were selected from landmarks previously described [18] using a quantitative image software package (Cine, GE Medical Systems, Milwaukee, WI). The mean contrast ratio (MCR) was calculated from the mean signal intensity (SI) from a region of interest (ROI) in each SAX slice within the area of occlusion divided by the mean SI in the control zone taken at midventicle (Fig. 2). Three values were generated from the three short-axis slices per animal for each time point.
Method of determining the mean contrast ratio (MCR) from SPECT short-axis images. Mean SI from the ischemic zone is contrasted to mean SI from a control zone to form the ratio of the two zones. Three slices (apex, mid-ventricle and base) were analyzed per animal. The same procedure and locations were used for the microsphere measures to normalize MBF SI = signal intensity, ROI = region of interest, Occl = coronary occlusion zone
Regional wall motion analysis
A 16 segment model based was scored subjectively by a single blinded observer for both motion and brightening (as a surrogate for thickening). To be scored normal [1] a segment had to show both motion and brightening. Motion without brightening was scored 2–5 depending on the degree on motion abnormality (2 = normal or mild hypokinesis, 3 = moderate, 4 = severe, 5 = akinesis or dyskinesis). A global score (RWMI) was calculated per study by summing the scores of each segment and dividing by the total.
Statistical analysis
Data are expressed as mean ± standard deviation (SD). Analyses were performed for comparison of measures over five time periods using one-way analysis of variance. Post-hoc comparisons of paired time points were also performed using a Fischer’s LSD test. A two-tailed unpaired t-test was used to compare SPECT MCR values to microsphere-derived measures of MBF. A P value <0.05 was considered significant. Intraobserver reproducibility of the SPECT MCR measure was assessed by paired measures in four animals. MCR values were measured in apical, mid-ventricular and basal slice locations for three points in time: baseline, day 28, and day 42 for a total of 36 paired measures.
Results
A total of eight pigs were successfully completed. Initial animal weight was 21.7 ± 1.7 Kg and weight at sacrifice was 34.7 ± 6.8 Kg. There was a trend for heart rate (HR) to decrease over the course of the protocol but this was not statistically significant (HR baseline = 99 ± 21 bpm, HR sacrifice = 84 ± 16 bpm). Infarct size was 5.0 ± 4.9%LV with a range of 0–11.6%LV (Table 1) and usually demonstrated a mosaic pattern in that patches of necrosis were intermixed with viable tissue. There was no evidence of transmural infarction in any animal. One animal had no evidence of necrosis.
Myocardial blood flow results
The average myocardial segment mass for calculation of MBF from microspheres was 3.2 g (24 segments per pig). Absolute MBF at baseline was 0.73 ± 0.52 ml/min/g (endocardial MBF = 0.78 ± 0.53 ml/min/g, epicardial = 0.69 ± 0.51 ml/min/g). Control zone MBF increased significantly after initial surgery (week 3 mean MBF = 1.34 ml/min/g, final MBF = 1.48 ml/min/g). The ratio of occlusion MBF/Control MBF (normalized MBF) is shown in Fig. 3 and Table 1. Overall, MBF varied significantly from baseline through the protocol (ANOVA P < 0.0001). Peak ischemia was reached between weeks 4 and 5 and was significantly lower (27% decrease) than baseline MBF (0.99 ± 0.23–0.73 ± 0.15, P < 0.0001). There was a significant recovery of 13% in MBF by week 6 (0.73 ± 0.15–0.86 ± 0.11, P < 0.01).
Summary results of the the two imaging parameters and the microsphere-derived normalized myocardial blood flow (MBF) values over five points in time. Data points represent mean values and whiskers represent 95% confidence intervals of the mean. For all three measures, the overall values changed significantly over time (P < 0.0001 for all three). Significant differences by post-hoc analysis exist for all 3 measures at weeks 3–4 compared to baseline (P < 0.0001) and week 6 compared to weeks 3–4. (P < 0.01). MCR = SPECT mean contrast ratio, RWMI = regional wall motion index by gated SPECT imaging
SPECT perfusion
Technically satisfactory perfusion images and gated images were obtained on the eight surviving pigs approximately 20 min following completion of the microsphere MBF determinations. There was no significant change in HR between the two modalities. The intraobserver variability of the SPECT MCR measurement was 0.029 and the 95% confidence interval for a significant change for this measure was 0.048. There was no significant difference overall between MBF by microspheres and SPECT MCR (MBF = 0.85 ± 0.21, MCR = 0.85 ± 0.13, P = NS). This was true for all five time points and for slice location (Fig. 4). The MCR closely paralleled the changes in MBF over the five measurements (Fig. 3 and Table 1) with a significant decrease at peak ischemia of 21% compared to baseline (0.97 ± 0.11–0.76 ± 0.13, P < 0.001). Following peak ischemia there was a significant increase in the MCR value of 11% (0.76 ± 0.13–0.87 ± 0.11, P = 0.0017) which paralleled the increase in MBF. All eight animals had an increase in the SPECT MCR from the ischemic nadir to the final acquisition that was greater than the reproducibility of the MCR measurement (Table 1).
Gated SPECT regional wall motion
The wall motion score (where 1 is normal wall motion and 5 is akinetic/dyskinetic) changed significantly over the 6 weeks following placement of the ameroid constrictor on the left circumflex artery (Fig. 3) with a significant increase in RWMSI (1.0 ± 0–1.36 ± 0.45, P < 0.0001 by ANOVA) by day 28 and significant recovery by day 42 (1.36 ± 0.45–1.13 ± 0.21 P < 0.01). This inversely paralleled the findings for MBF over the same period. The presence of necrosis did not preclude regional wall motion (RWM) recovery. Pigs with larger infarcts (9–11% LV) had the greatest recovery in RWM (Table 1). However, infarct size was small in all animals.
Discussion
Imaging of myocardial blood flow has evolved from a diagnostic tool for the detection of epicardial vessel obstruction to an efficacy end-point for trials examining novel approaches for revascularization. These therapies and their highly localized delivery place extraordinary demands on imaging techniques which were not designed to provide precise measurements of myocardial blood flow in small segments of myocardial tissue. The performance of low resolution conventional imaging methods in clinical trials for the measurement of induced changes in MBF by these agents has been mixed [5–9, 19]. The improvements in blood flow which occur following the administration of growth factors is generally believed to be generated in vessels less than 200 μm in diameter [20]. Evaluating efficacy is therefore a challenge for cardiac imaging and particularly for SPECT where resolution is 1–1.5 cm.
Visual estimates of isotope uptake have been used for quantifying the small changes in MBF from growth factors administered to patients [5–7, 19]. Isotopes cannot quantify MBF in absolute terms due to photon scatter, attenuation and low spatial resolution but there are semi-quantitative methods can be applied as in the present study.
This study demonstrates that SPECT perfusion imaging in combination with gated wall motion provides a fairly clear serial representation of dynamic changes in MBF as might be seen in patients with ischemic heart disease. The MCR from the perfusion images, which provides a measure of mean SI in an ROI compared to a control zone, tracked mean changes in MBF closely in both progressive ischemia and presumed collateral flow development.
The changes in MBF in this model were relatively modest with a maximum reduction at weeks 4–5 of 27% from baseline and a modest recovery to climb within 13% of baseline. These changes did exceed the reproducibility of the measure, however. Despite these modest changes, the changes in wall motion by gated SPECT were significant. The changes in RWMI have also been found by other researchers to be a strong indicator of both the damage and recovery phases in the ameroid-induced pig model of ischemia. Zhang et al. [21] found a very similar relationship between RWM determined by gated SPECT and the recovery of ischemic area and ejection fraction. Lopez et al. [22], using the ameroid-induced ischemic pig with open chest echocardiography, found a good relationship existed between wall motion and MBF during the recovery phase, with the addition of fibroblast growth factor. Sato et al. [23], also in the ameroid-induced pig, found that wall motion and wall thickening were indicators for the recovery phase of the model.
Other techniques can provide both perfusion and regional wall motion data regarding therapies targeted to alter myocardial blood flow. Echocardiography and magnetic resonance imaging have demonstrated significant improvements in wall motion score in chronic ischemic animal models in both control and target treated regions [24–26]. Contrast Echocardiography has demonstrated measurable improvements in chronically ischemic myocardium which have correlated reasonably well with microsphere determinations of flow out to 48 days [25]. These studies were confined to two imaging time points and did not track dynamic changes, as in the present study.
While subjective scoring systems for perfusion changes may be successful, some degree of quantitation is likely necessary given the overall small changes in MBF reflected in this model and in human trials [9, 27, 28]. Rosengaart et al. found no change in perfusion in patients receiving vascular endothelial growth factor by SPECT as measured by a well validated subjective method employed for ischemic heart disease [19]. However, gated wall motion improved significantly suggesting the changes in perfusion are likely too subtle to be accurately reflected in purely subjective segmental analysis. The combination of semi-quantified SPECT perfusion with an index of subjective RWM may provide an effective combination to assess small degrees of MBF change.
The changes in SPECT perfusion were measurable despite the relatively low resolution of the technique in the setting of minimal infarction. Large chronic infarcts will not perform as well due to the dependence of viability for Tc-99 m sestamibi uptake [14]. Recently, serial gated SPECT imaging has been performed to evaluate the success of various stem-cell strategies in patients and animal models of infarction with mixed results [29–31]. This type of therapy is based on a different physiologic principle: the change in viability status through altering the cellular content of the infarct. The principles for the noninvasive quantitation for this change in viability [4] are quite different than the method used in the present study to track changes in MBF in a viable but ischemic zone. Altering viability may be the standard of care of the future and imaging methods designed to specifically target viability may provide effective measures. The animal model used in this study was based upon therapies that change blood flow and is not directly applicable to cellular therapies.
Limitations
No attenuation correction algorithms were used in the imaging protocol, which may assume more importance for clinical use where body habitus is more variable. Serial imaging of the same subject with the same tracer dose should produce a constant attenuation pattern. The infarcts generated in the present study were small. Performance of serial gated-SPECT for RWMI may not perform as well in the setting of large perfusion defects [32]. Anatomic analysis for collateral development was not performed to confirm the etiology for the increase in MBF from peak ischemia to sacrifice. However, the development of collateral circulation in this ameroid swine model has been demonstrated previously [27, 28] and the increase in MBF following an ischemic nadir in this study was likely to be the consequence of collateral development. While it is speculated that these results can be extrapolated to animal models and human trials where changes in regional myocardial blood flow can be invoked, there was no such therapeutic modality in this study.
Radionuclide perfusion SPECT imaging is a relative technique where the SI is scaled to the peak activity in the myocardium. Serial imaging assumes the peak region to which all activity is scaled does not change from one exam to the next. This may not hold for nonselective application of a therapeutic agent and needs further investigation. However, in the present study, SPECT was able to track fairly small changes in MBF in an untreated ameroid constrictor model of chronic ischemia. This is an encouraging result regarding both the clinical and experimental use of serial SPECT perfusion imaging.
References
Christian TF (1999) Detecting the effects of angiogenic therapy:how do we measure efficacy? Curr Interv Cardiol Rep 1:310–321
Dakik HA, Kleiman NS, Farmer JA et al (1998) Intensive medical therapyversus coronary angioplasty for suppression of myocardial ischemia insurvivors of acute myocardial infarction:a prospective, randomized pilot study. Circulation 98:2017–2023
Berman DS, Kang X, Schisterman EF, Gerlach J, Kavanagh PB, Areeda JS, Sharir T, Hayes SW, Shaw LJ, Lewin HC, Friedman JD, Miranda R, Germano G (2001) Serial changes on quantitative myocardial perfusion SPECT in patients undergoing revascularization or conservative therapy. J Nucl Cardiol 8(4):428–437
Christian TF (2006) Positively magnetic north. J Am Coll Cardiol 47:1646–1648
Henry TD, Annex BH, Azrin MA (1999) Double blind placebo controlled trial of recombinant human vascular endothelial growth factor—the VIVA trial. JACC 33:38A (Abstract)
Hendel RC, Henry TD, Rocha-Singh K, Isner JM, Kereiakes DJ, Giordano FJ, Simons M, Bonow RO (2000) Effect of intracoronary recombinant human vascular endothelial growth factor on myocardial perfusion: evidence for a dose dependent effect. Circulation 101:118–121
Vale PR, Losardo DW, Milleken CE, Maysky M, Esakof DD, Symes JF, Isner JM (2000) Left ventricular electromechanical mapping to assess efficacy of ph VEGF-165 gene transfer for therapeutic angiogenesis in chronic myocardial ischemia. Circulation 102:965–974
Udelson JE, Dilsizian V, Laham RJ, Chronos N, Vansant J, Blais M, Galt JR, Pike M, Yoshizawa C, Simons M (2000) Therapeutic angiogenesis with recombinant fibroblast growth factor-2 improves stress and rest myocardial perfusion abnormalities in patients with severe symptomatic chronic coronary artery disease. Circulation 102:1605–1610
Simons M, Bonow RO, Chronos NA, Cohen DJ, Giordano FJ, Hammond HK, Laham RJ, Li W, Pike M, Sellke FW, Stegmann TJ, Udelson JE, Rosengart TK (2000) Clinical trials in coronary angiogenesis: issues, problems, consensus: an expert panel summary. Circulation 102(11):E73–86
Harada K, Friedman M, Lopez JJ et al (1996) Vascular endothelial growth factor administration in chronic myocardial ischemia. Am J Physiol 270(5 Pt 2):H1791–802
Beanlands R, Muzik O, Nguyen N, Petry N, Schwaiger M (1992) The relationship between myocardial retention of technetium-99m teboroxime and myocardial blood flow. J Am Coll Cardiol 20(3):712–719
Piwnica-Worms D, Kronauge JF, Chiu ML (1990) Uptake and retention of hexakis (2-methoxyisobutyl isonitrile) technetium(I) in cultured chick myocardial cells. Mitochondrial and plasma membrane potential dependence. Circulation 82(5):1826–1838
Chareonthaitawee P, O’Connor MK, Gibbons RJ, Ritman EL, Christian TF (2000) The effect of collateral flow and myocardial viability on the distribution of tc-99m sestamibi in a closed chest model of coronary occlusion and reperfusion. Eur J Nucl Med 27:508–516
Christian TF, O’Connor MK, Schwartz RS, Gibbons RJ, Ritman EL (1997) Technetium-99m MIBI to assess coronary collateral flow during acute myocardial infarction in two closed-chest animal models. J Nuc Med 38:1840–1846
Prinzen FW, Bassingthwaighte JB (2000) Blood flow distributions by microsphere deposition methods. Cardiovasc Res 45:13–21
Domenech RJ, Hoffman JIE, Noble MIM, Saunders KB, Henson JR, Subijanto S (1969) Total and regional coronary blood flow measured by radioactive microsphere in conscious and anesthetized dogs. Circ Res 25:581–596
Kane GC, Hauser MF, Behrenbeck T, Miller TD, Gibbons RJ, Christian TF (2002) The impact of gender on Tc-99m sestamibi gated left ventricular ejection fraction. Am J Cardiol 89:1238–1241
Christian TF, Schwartz RS, Gibbons RJ (1992) Determinants of infarct size in reperfusion therapy for acute myocardial infarction. Circulation 96:81–90
Rosengart TK, Lee LY, Patel SR, Sanborn TA, Parikh M, Bergman GW, Hachamovitch R, Szulc M, Kligfield PD, Okin PM, Hahn RT, Devereaux RB, Post MR, Hackett NR, Foster T, Grasso TM, Lesser ML, Isom W, Crystal RG (1999) Angiogenesis gene therapy: phase 1 assessment of direct intramyocardial administration of an adenovirus vector expression VEGF 121 c DNA to individuals with clinically significant severe coronary artery disease. Circulation 100:468–474
White FC, Carroll SM, Magnet A, Bloor CM (1992) Coronary collateral development in swine after coronary artery occlusion. Circ Res 71:1490–1500
Zhang D, Luyue GAI, Fan R, Dong W, Wen Y (2002) Efficacy and safety of therapeutic angiogenesis from direct myocardial administration of an adenoviral vector expressing vascular endothelial growth factor 165. Chin Med J 115(2):643–648
Lopez JJ, Edelman ER, Stamler A, Hibberd M, Prasad P, Caputo RP, Carrozza JP, Douglas PS, Sellke FW Simons M (1997) Basic fibroblast growth factor in a porcine model of chronic myocardial ischemia: a comparison of angiographic, echocardiographic and coronary flow parameters. J Pharmacol Exp Ther 282(1):385–390
Sato K, Laham RJ, Pearlman JD, Novicki D, Sellke FW, Simons M Post MJ (2000) Efficacy of intracoronary versus intravenous FGF-2 in a pig model of chronic myocardial ischemia Ann Thorac Surg 70:2113–2118
Tse HF, Kwong YL, Chan JFK, Lo G, Ho CL, Lau CP (2003) Angiogenesis in ischemic myocardium by intramyocardial autologous bone marrow mononuclear cell implantation. Lancet 361:47–49
Villanueva FS, Abraham JA, Schreiner GF, Csikari M, Fischer D, Mills JD, Schellenberger U, Koci BJ, Lee JS (2002) Myocardial contrast echocardiography can be used to assess the microvascular response to vascular endothelial growth factor-121. Circulation 105(6):759–765
Horvath KA, Doukas J, Lu CY, Belkind N, Greene R, Pierce GF, Fullerton DA (2002) Myocardial functional recovery after fibroblast growth factor 2 gene therapy as assessed by echocardiography and magnetic resonance imaging. Ann Thorac Surg 74(2):481–486
Lopez JJ, Laham RJ, Stamler A et al (1998) VEGF administration in chronic myocardial ischemia in pigs. Cardiovasc Res 40(2):272–281 Harada K, Friedman M, Lopez JJ et al (1996) Vascular endothelial growth factor administration in chronic myocardial ischemia. Am J Physiol 270(5 Pt 2):H1791–802
Hariawala MD, Horowitz JR, Esakof D et al (1996) VEGF improves myocardial blood flow but produces EDRF-mediated hypotension in porcine hearts. J Surg Res 63:77–82
Zohlnhofer D, Ott I, Mehilli J, Schomig K, Michalk F, Ibrahim T, Meisetschlager G, von Wedel J, Bollwein H, Seyfarth M, Dirschinger J, Schmitt C, Schwaiger M, Kastrati A, Schomig A (2006) REVIVAL-2 Investigators. Stem cell mobilization by granulocyte colony-stimulating factor in patients with acute myocardial infarction: a randomized controlled trial. JAMA 295(9):1003–1110
Kim BO, Tian H, Prasongsukarn K, Wu J, Angoulvant D, Wnendt S, Muhs A, Spitkovsky D, Li RK (2005) Cell transplantation improves ventricular function after a myocardial infarction: a preclinical study of human unrestricted somatic stem cells in a porcine model. Circulation 112(9 Suppl):I96–104
Lim SY, Kim YS, Ahn Y, Jeong MH, Hong MH, Joo SY, Nam KI, Cho JG, Kang PM, Park JC (2006) The effects of mesenchymal stem cells transduced with Akt in a porcine myocardial infarction model. Cardiovasc Res 70(3):530–542
Yves GCJ, Bax JJ, Dibbets-Schneider P, Pauwels EKJ, Van Der Wall EE (2004) Evaluation of the Quantitative Gated SPECT (QGS) software program in the presence of large perfusion defects. Int J Cardiovasc Imaging 21:519–529
Acknowledgement
This work was funded by a grant from Procter and Gamble.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christian, T.F., Peters, K., Keck, B. et al. Gated SPECT imaging to detect changes in myocardial blood flow during progressive coronary occlusion. Int J Cardiovasc Imaging 24, 269–276 (2008). https://doi.org/10.1007/s10554-007-9255-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-007-9255-3