Abstract
Purpose
To test the effect of age on cancer-specific mortality (CSM) in most contemporary prostate cancer (PCa) patients of all stages and across all treatment modalities.
Methods
Within the Surveillance, Epidemiology, and End Results database (2004–2016), we identified 579,369 PCa patients. Cumulative incidence plots and multivariable competing-risks regression analyses (MCR) were used. Subgroup analyses were performed according to ethnicity (African-Americans), clinical stage (T1-2N0M0, T3-4N0M0, TanyN1M0, and TanyNanyM1), as well as treatment modalities.
Results
Patient distribution was as follows: 142,338 (24.6%) < 60 years; 113,064 (19.5%) 60–64 years; 127,158 (21.9%) 65–69 years; 94,782 (16.4%) 70–74 years; and 102,027 (17.6%) ≥ 75 years. Older patients harbored worse tumor characteristics and more frequently received no local treatment. Overall, 10-year CSM rates were 4.8, 5.3, 5.9, 7.6, and 14.6%, respectively, in patients aged < 60, 60–64, 65–69, 70–74 ,and ≥ 75 years (p < 0.001). In MCR focusing on the overall cohort and T1-2N0M0 patients, older age independently predicted higher CSM, but not in T3-4N0-1M0-1 patients.
Conclusions
Older age was associated with higher grade and stage and independently predicted higher CSM in T1-2N0M0 patients, but not in higher stages. Differences in diagnostics and therapeutics seem to affect elderly patients within T1-2N0M0 PCa and should be avoided if possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since overall life expectancy improved over the last decades and prostate cancer (PCa) incidence increases with older age, increased prevalence of PCa in older patients may be anticipated for the future [1]. Unfortunately, older patients are more likely to harbor higher-risk prostate cancer (PCa) at diagnosis and are less likely to receive local therapy according to several historical population-based as well as institutional analyses [1,2,3,4]. These differences in diagnosis and treatment of older patients have been widely discussed within the urologic community for many years now [5]. Several measures, such as careful assessment of life expectancy, as well as geriatric assessment have been suggested to select ideal candidates for diagnosis and treatment of PCa to avoid under- and over-treatment in older patients [6,7,8]. Therefore, we hypothesized that such ageist approach to diagnosis and treatment of PCa has been eliminated in contemporary patients. To address this hypothesis, we tested the effect of age on cancer-specific mortality (CSM) in most contemporary PCa patients. For purpose of all analyses, we relied on the most contemporary Surveillance, Epidemiology and End Results (SEER) database (2004–2016).
Patients and methods
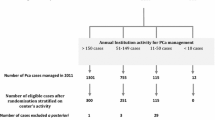
Study population
The SEER database samples 34.6% of the USA and approximates the USA in terms of demographic composition, as well as of cancer incidence [9]. Within the SEER database (2004–2016), we identified patients aged ≥ 18 years with histologically confirmed PCa diagnosis at biopsy (International Classification of Disease for Oncology [ICD-O-3] code 8140 site code C61.9) and available prostate-specific antigen (PSA) value (n = 580.033), while death certificate only or autopsy cases were excluded (n = 464). Moreover, clinical stage T0 patients were excluded (n = 200). This resulted in a cohort of 579,369 PCa patients.
Outcomes of interest
Our analyses focused on CSM which was defined as death attributable to PCa. Conversely, other-cause mortality (OCM) was defined as death attributable to other causes than PCa.
In all analyses, the predictor of interest consisted of age (categorized into < 60 vs. 60–64 vs. 65–69 vs. 70–74 vs. ≥ 75 years). First, we addressed the overall cohort to exclude any selection biases. Second, we performed five sets of subgroup analyses, namely, within African-American patients, within cT1-2N0M0 patients, cT3-4N0M0 patients, TanyN1M0 patients, and TanyNanyM1 patients. Finally, within each of the four stage subgroups, we further stratified testing according to treatment type (no local treatment [NLT], radical prostatectomy [RP], radiation therapy [RT], unknown treatment).
Statistical analyses
Descriptive statistics included medians and interquartile ranges, as well as frequencies and proportions for continuous and categorical variables, respectively. The statistical significance of differences in medians and proportions was evaluated with the Kruskal–Wallis and chi-square tests. Temporal trend analyses were visualized with estimated annual percentage changes (EAPC).
In all analyses, we relied on cumulative incidence plots and subsequently fitted multivariable competing-risks regression models testing the effect of age on CSM and OCM [10]. All models were additionally adjusted for year of diagnosis (continuously coded), race (Caucasian vs. African-American vs. others), marital status (married vs. unmarried vs. unknown), PSA (continuously coded), biopsy grade group ([GG] GG I vs. GG II vs. GG III vs. GG IV vs. GG V vs. GG unknown) [11], clinical T stage (T1 vs. T2 vs. T3 vs. T4 vs. TX), clinical N stage (N0 vs. N1 vs. NX), clinical M stage (M0 vs. M1 vs. MX), as well as treatment type (no local treatment [NLT] vs. radical prostatectomy [RP] vs. radiation therapy [RT] vs. unknown treatment). For all statistical analyses, R software environment for statistical computing and graphics (version 3.4.3) was used. All tests were two sided with a level of significance set at p < 0.05.
Results
Patients’ characteristics and temporal trends
Overall, 579,369 PCa patients were identified. Patient distribution was as follows: 142,338 (24.6%) < 60 years; 113,064 (19.5%) 60–64 years; 127,158 (21.9%) 65–69 years; 94,782 (16.4%) 70–74 years; 102,027 (17.6%) ≥ 75 years (Table 1).
Older patients were more likely to harbor worse tumor characteristics. Specifically, older patients had higher pretreatment PSA values (9.3 vs. 5.7 ng/ml in ≥ 75 vs. < 60 years), more frequently harbored GG IV-V (28.9 vs. 10.5% in ≥ 75 vs. < 60 years), cT3-4 (5.6 vs. 3.9% in ≥ 75 vs. < 60 years), and M1 disease (8.8 vs. 3.1% in ≥ 75 vs. < 60 years). Moreover, they were more likely to receive no local treatment (47.6 vs. 18.4% in ≥ 75 vs. < 60 years). Median follow-up was 66 months (interquartile range 31–103 months). Analyses according to annual rates (2004–2016) showed a significant decrease of PCa diagnosis in patients aged ≥ 75 years (22.2–16.0%, EAPC: -3.7%) over time. However, within the subgroup of patients aged ≥ 75 years, analyses according to annual rates (2004–2016) showed a significant increase in the rates of higher stage PCa at diagnosis (T3-4N0M0: 2.4–7.0%, EAPC: 9.8%, TanyN1M0: 0.3–2.4%, EAPC: 17.1%, TanyNanyM1: 6.4–14.5, EAPC: 9.3%).
Cumulative incidence plots and competing-risks regression models in the main study population
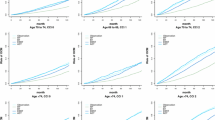
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up. In the main study population, 10-year CSM rates were 4.8, 5.3, 5.9, 7.6, and 14.6%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (p < 0.001, Fig. 1). In multivariable competing-risks regression models focusing on the main study population, older age represented an independent predictor of higher CSM (hazard ratio (HR) 1.05, 1.18, and 1.44 in patients aged 65–69 years, 70–74 years, and ≥ 75 years) relative to patients aged < 60 years (Table 2).
Subgroup analyses according to African-American ethnicity
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up in African-Americans (n = 87,597, 15.1%). Here, 10-year CSM rates were 6.5, 7.5, 8.9, 10.4, and 17.9%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (p < 0.001). In multivariable competing-risks regression models focusing on the main study population, older age represented an independent predictor of higher CSM (HR 1.11, 1.18, and 1.35 in patients aged 65–69 years, 70–74 years, and ≥ 75 years) relative to patients aged < 60 years.
Subgroup analyses according to stage
T1-2N0M0 patients
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up. Here, 10-year CSM rates were 2.2, 2.9, 3.5, 4.9, and 9.4%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (both p < 0.001). In multivariable competing-risks regression models, older age represented an independent predictor of higher CSM (HR 1.08, 1.16, 1.32 and 1.62 in patients aged 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years) relative to patients aged < 60 years (Table 3).
Further analyses relied on stratification according to treatment type. In multivariable competing-risks regression models within NLT patients, older age represented an independent predictor of higher CSM (HR 1.23 and 1.51 in patients aged 70–74 years and ≥ 75 years) relative to patients aged < 60 years. In multivariable competing-risks regression models within RP patients, older age represented an independent predictor of higher CSM (HR 1.15, 1.35, 1.55 and 2.75 in patients aged 60–64 years, 65–69 years, 70–74 years and ≥ 75 years) relative to patients aged < 60 years. In multivariable competing-risks regression models within RT patients, older age represented an independent predictor of higher CSM (HR 1.18 and 1.54 in patients aged 70–74 years and ≥ 75 years) relative to patients aged < 60 years. In multivariable competing-risks regression models within patients with unknown treatment type, older age represented an independent predictor of higher CSM (HR 1.84 in patients aged ≥ 75 years) relative to patients aged < 60 years.
T3-4N0M0 patients
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up. Here, 10-year CSM rates were 13.5, 14.6, 14.8, 16.4, and 24.0%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (both p < 0.001). In multivariable competing-risks regression models, older age did not represent an independent predictor of higher CSM (HR 1.06, 0.91, 0.99, and 1.11 in patients aged 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years) relative to patients aged < 60 years (Table 3). Further subgroup analyses relied on stratification according to treatment type. Here, no association was identified between age and CSM (data not shown).
TanyN1M0 patients
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up. Here, 10-year CSM rates were 25.1, 20.7, 25.9, 26.3, and 35.0%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (both p < 0.001). In multivariable competing-risks regression models, older age did not represent an independent predictor of higher CSM (HR 0.85, 0.90, 1.01, and 0.98 in patients aged 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years) relative to patients aged < 60 years (Table 3). Further subgroup analyses relied on stratification according to treatment type. Here, no association was identified between age and CSM (data not shown).
TanyNanyM1 patients
Cumulative incidence smoothed plots were generated and focused on CSM at 10 years of follow-up. Here, 10-year CSM rates were 73.2, 70.4, 66.6, 66.2, and 66.5%, respectively, in patients aged < 60 years, 60–64 years, 65–69 years, 70–74 years, and ≥ 75 years (both p < 0.001). In multivariable competing-risks regression models, older age did not represent an independent predictor of higher CSM (HR 098, 0.94, and 0.99 in patients aged 60–64 years, 65–69 years, and 70–74 years) relative to patients aged < 60 years, while it represented an independent predictor of higher CSM in patients aged ≥ 75 years (HR 1.06; Table 3). Further subgroup analyses relied on stratification according to treatment type. Here, no association was identified between age and CSM (data not shown).
Discussion
According to three population-based historical analyses from North America and Scandinavia, it could be postulated that ageism may deprive older PCa patients from timely diagnosis and treatment [1,2,3]. We tested this hypothesis in a contemporary PCa patient cohort of all stages and across treatment modalities. We aimed at including all patients within all disease stages as well as all treatment types to reduce any selection biases by excluding specific subgroups. Our analyses yielded several noteworthy findings.
First, 17.6% of patients in our cohort of 579,369 PCa patients diagnosed between 2004 and 2016 were ≥ 75 years old. Moreover, analyses according to annual rates showed a significant decrease of PCa diagnosis from 22.2 to 16.0% in patients aged ≥ 75 years (EAPC: − 3.7%) over time. However, in the subgroup of patients aged ≥ 75 years, analyses according to annual rates also showed a significant increase of higher stages at PCa diagnosis. The overall rate of older patients within the current study is in agreement with one previous North American population-based analysis, which reported 14.5% of patients older than 75 years within their cohort of 11,790 PCa patients [1]. Taken together, the findings of the current study indicate a decreasing rate of PCa diagnosis in the most elderly. However, the rate of higher stages at diagnosis is still on a rise, which is worrisome and may be interpreted as a result of voluntarily delayed diagnosis and/or treatment in elderly patients.
Second, older patients were more likely to harbor worse tumor characteristics. Specifically, older patients had higher pretreatment PSA values and more frequently harbored GG IV-V, cT3-4, and M1 disease relative to younger patients. Additionally, they were less likely to receive local treatment. Our observations are in line with previous reports. Pettersson et al. described similar findings in a population-based study of 121,392 Swedish men diagnosed with PCa between 1998 and 2012 [2]. Similarly, Bechis et al. reported on 11,790 PCa patients within a North American observational registry (Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) database). Here, older patients were also more likely to have high-risk disease at diagnosis and less likely to receive local therapy [1]. Likewise, Abdollah et al. described a decreasing rate of local treatment in older patients in a SEER cohort of 404,604 PCa patients diagnosed between 1988 and 2006 [3]. In conclusion, our results corroborate previous findings indicating that in current clinical practice, older patients may continue to receive insufficient diagnostic work-up that results in higher disease stage at presentation.
Third, univariable and multivariable analyses performed in the entire patient cohort demonstrated an increased risk of CSM in older patients. This also held true in the subgroup of African-American patients who accounted for 15% of the population. However, in stratified analyses, the association between increasing age and increasing CSM only applied to T1-2N0M0 patients, but not to higher stage patients. Moreover, treatment-specific subgroup analyses within T1-2N0M0 patients demonstrated that the relationship between increasing age and increasing CSM was universally applicable across all four examined treatment modalities, namely, NLT, RP, RT, and unknown treatment type. Taken together, these observations suggest that potential differences (i.e., poorer work-up, less aggressive treatment, or less PSA screening in older men) in diagnosis and treatment are predominantly operational in T1-2N0M0 patients, but not in patients with higher disease stages. It is possible that an ageist approach to PCa diagnosis and subsequent treatment is mostly operational at a localized stage, where definitive management options are considered with curative intent in mind. Conversely, the potential effect of ageism in diagnosis and treatment of more advanced stages of PCa is not evident. These differences are surprising in the light of cost differences between predominantly single-modality definitive therapy vs. life-long androgen deprivation therapy that is increasingly combined with additional systemic management in the setting of castration-resistant PCa or even castration-sensitive metastatic PCa [12,13,14]. These considerations should be used in everyday clinical practice with the intent of ideally establishing an early diagnosis at a localized stage even in elderly patients with potentially curative local treatment. An ideal example of such scenario corresponds to improved survival after RT in intermediate or high-risk elderly patients [15].
Taken together, our study demonstrates that the phenomenon of differences in diagnosis and potential under-treatment of elderly PCa patients is operational, even in most contemporary patients and foremost applies to those at risk of clinically localized disease (T1-2N0M0). Our results validate more historical reports and should be used to further sensitize the urologic community that chronological age per se should not be used to withdraw diagnostic and/or therapeutic considerations, even when clinically localized PCa diagnosis is contemplated [16].
There is certainly also the possibility that late-onset PCa may be biologically different (i.e., more aggressive) compared to early-onset disease independent of the classical pathological features. Weischenfeldt et al. demonstrated that men developing PCa at the age of < 50 years have a higher likelihood of a characteristic “androgen-type” pathomechanism compared to men who developed PCa at an older age [4]. However, while the authors described the mechanism of development of early-onset PCa to be different, it remains unknown whether this translates into a more aggressive biology. In consequence, further studies are needed to evaluate a potential difference in tumor biology according to age at diagnosis.
Several limitations of our study need to be mentioned. First, since SEER is an observational database, the current data are retrospective. Second, pathological assessment of biopsy samples and RP specimens did not benefit of central pathological review. Moreover, standardized staging information was not available. Similarly, staging methods and staging extent may have varied between patients. Moreover, only CSM was available for the purpose of outcome analyses. None of potentially important earlier cancer control outcomes such as biochemical recurrence or metastatic progression were available. Similarly, information regarding adjuvant or salvage treatment (i.e., RT, antiandrogen deprivation therapy, or chemotherapy) is not available within the SEER database. Additionally, no information regarding comorbidities is available in the SEER database. We compensated for this limitation by virtue of relying on competing-risks regression models that adjust for OCM and adjust for the most important comorbidities that resulted in OCM. Moreover, we could not account for selection biases related to primary treatment assignment. Finally, no information regarding PSA screening was available. However, it may be possible that the lead time bias introduced by PSA screening may partly explain the results. It is important to note that these limitations apply to all observational studies that rely on either the SEER database or similar population-based cohorts [1, 3].
Conclusions
Older age was associated with higher grade and stage. Moreover, older age was an independent predictor of higher CSM in T1-2N0M0 patients, but not in higher stages. This observation suggests that there are differences in diagnostic and therapeutic modalities in elderly patients within T1-2N0M0 PCa. Such practices should be avoided if possible.
References
Bechis SK, Carroll PR, Cooperberg MR (2011) Impact of age at diagnosis on prostate cancer treatment and survival. J Clin Oncol 29(2):235–241
Pettersson A, Robinson D, Garmo H, Holmberg L, Stattin P (2018) Age at diagnosis and prostate cancer treatment and prognosis: a population-based cohort study. Ann Oncol 29(2):377–385
Abdollah F, Sun M, Thuret R, Jeldres C, Tian Z, Briganti A et al (2011) A competing-risks analysis of survival after alternative treatment modalities for prostate cancer patients: 1988–2006. Eur Urol 59(1):88–95
Mandel P, Kriegmair MC, Kamphake JK, Chun FK-H, Graefen M, Huland H et al (2016) Tumor characteristics and oncologic outcome after radical prostatectomy in men 75 years old or older. J Urol 196(1):89–94
Bratt O, Folkvaljon Y, Hjälm Eriksson M, Akre O, Carlsson S, Drevin L et al (2015) Undertreatment of men in their seventies with high-risk nonmetastatic prostate cancer. Eur Urol 68(1):53–58
Narayan V, Jiang S, Warlick CA (2017) Early stage cancer in older adults: prostate-avoiding overtreatment and undertreatment. Cancer J Sudbury Mass 23(4):238–241
Lunardi P, Ploussard G, Grosclaude P, Roumiguié M, Soulié M, Beauval JB et al (2017) Current impact of age and comorbidity assessment on prostate cancer treatment choice and over/undertreatment risk. World J Urol 35(4):587–593
Ploussard G, Albrand G, Rozet F, Lang H, Paillaud E, Mongiat-Artus P (2014) Challenging treatment decision-making in older urologic cancer patients. World J Urol 32(2):299–308
About the SEER Program [Internet]. SEER. [cited 2019 Jun 2]. https://seer.cancer.gov/about/overview.html
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA et al (2016) The 2014 International Society of Urological Pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40(2):244–252
James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP et al (2017) Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med 377(4):338–351
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira AJ, Given R et al (2019) Apalutamide for Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med 381:13–24
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S et al (2019) Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med 381:121–131
Dell’Oglio P, Boehm K, Trudeau V, Tian Z, Larcher A, Leyh-Bannurah S-R et al (2016) Survival after conservative management versus external beam radiation therapy in elderly patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 96(5):1037–1045
Knipper S, Graefen M (2017) Clinical case discussion: primary treatment for prostate cancer in an elderly man-treatment of the primary tumor is necessary. Eur Urol Focus 3(4–5):326–327
Weischenfeldt J, Simon R, Feuerbach L, Schlangen K, Weichenhan D, Minner S et al (2013) Integrative genomic analyses reveal an androgen-driven somatic alteration landscape in early-onset prostate cancer. Cancer Cell 23(2):159–170
Funding
There was no external financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Knipper, S., Pecoraro, A., Palumbo, C. et al. The effect of age on cancer-specific mortality in patients with prostate cancer: a population-based study across all stages. Cancer Causes Control 31, 283–290 (2020). https://doi.org/10.1007/s10552-020-01273-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01273-5