Abstract
Purpose
The purpose of this study was to evaluate whether adherence to the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) cancer prevention recommendations was associated with colorectal cancer incidence in the Black Women’s Health Study (BWHS).
Methods
In this ongoing prospective cohort of African American women (analytic cohort n = 49,103), 354 incident colorectal cancers were diagnosed between baseline (1995) and 2011. Adherence scores for seven WCRF/AICR recommendations (adherent = 1 point, non-adherent level 1 = 0.5 points, non-adherent level 2 = 0 points) were created using questionnaire data and summed to an overall adherence score (maximum = 7). Recommendation adherence and colorectal cancer incidence were evaluated using baseline and time-varying data in Cox regression models.
Results
At baseline, 8.5 % of women adhered >4 recommendations. In time-varying analyses, the HR was 0.98 (95 % CI 0.84–1.15) per 0.5 point higher score and 0.51 (95 % CI 0.23–1.10) for adherence to >4 compared to <3 recommendations. Adherence to individual recommendations was not associated with colorectal cancer risk. Results were similar in models that considered baseline exposures only.
Conclusions
Adherence to cancer prevention recommendations was low and not associated with colorectal cancer risk among women in the BWHS. Research in diverse populations is essential to evaluate the validity of existing recommendations, and assess whether there are alternative recommendations that are more beneficial for cancer prevention in specific populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
African American women are more likely to be diagnosed with colorectal cancer than women from other racial/ethnic groups [1]. Compared to Caucasian Americans, which is the racial/ethnic group with the second highest incidence and mortality rates, colorectal cancer incidence rates are 25 % higher and mortality rates 50 % higher among African Americans [2]. A portion of this difference is likely attributable to differences in colorectal cancer screening [3]. However, several lifestyle factors are associated with colorectal cancer risk, including diet, physical activity, and body weight [4–8], and important differences in dietary intake, physical activity levels, and body size across racial/ethnic groups likely also contribute to disparities.
Previous studies have consistently shown adherence to a greater number of cancer prevention recommendations, such as the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) recommendations (outlined in Table 1), to be associated with lower overall cancer incidence (any type) [9–13] and specific types of cancer [10–15]. The WCRF/AICR recommendations encompass diet, physical activity, and body weight recommendations based on findings from the WCRF/AICR Continuous Update Project: an ongoing systematic review of the literature [16]. While the goal of cancer prevention recommendations is to lower the risk of all types of cancer, adherence may be particularly beneficial for reducing the risk of colorectal cancer, which has been consistently associated with diet, physical activity, and body weight in previous studies [4–8]. Four prior studies investigated adherence to diet, physical activity, and body weight cancer prevention recommendations and colorectal cancer risk in largely Caucasian study populations [10–13]. Among the three studies with sufficient sample size, higher adherence to cancer prevention recommendations was significantly associated with lower risk of colorectal cancer in both genders combined [10] and when evaluated among women only [12, 13]. None of the studies presented data on associations with individual recommendations, and only one explored colon and rectal cancers separately [13]. Current evidence suggests that risk factors may differ between colon and rectal cancer, with stronger evidence of an association with colon cancer risk [5, 17].
Available data indicate that adherence to diet, physical activity, and body weight cancer prevention recommendations is likely poor among African American women. Adherence to diet, physical activity, and body weight recommendations is generally low in the USA and tends to be lower among African Americans. African Americans are less likely to meet US Dietary Guideline recommendations for intake of fruits, vegetables, dairy, and added sugars [18], more likely to be obese (58.5 % compared to 32.3 % in Caucasians and 41.4 % in Hispanics), and less likely to meet physical activity recommendations [19–21] than other racial/ethnic groups. The disparities in adherence to diet, physical activity, and body weight recommendations are consistent with the potential for lifestyle-related factors to influence colorectal cancer disparities among African Americans.
In the Women’s Health Initiative (WHI), adherence to the ACS cancer prevention recommendations was associated with a lower risk of cancer (any type) among African American women [12]. However, this study did not evaluate adherence levels among African American women, or whether adherence was associated with colorectal cancer incidence among African American women. Studies that investigate levels of adherence and potential benefits of adherence to cancer prevention recommendations among African American women are needed. The objective of this analysis was to address this gap by assessing adherence to WCRF/AICR cancer prevention recommendations in relation to colorectal cancer risk among African American women in the Black Women’s Health Study (BWHS).
Materials and methods
The Black Women’s Health Study is an ongoing prospective cohort study of African American women in the United States (n = 59,000) [22]. In 1995, subscribers to Essence magazine were mailed health questionnaires. A small number of women were also recruited from several professional organizations or were friends or relatives of early respondents. Women who were aged 21–69 years, self-identified as Black, and completed the study questionnaire comprised the cohort. Participants have been followed subsequently through mailed questionnaires sent every 2 years. Deaths are identified by reports from family members, US Postal Service and via the National Death Index. Follow-up of the baseline cohort is complete for 88 % of potential years of follow-up through 2013. The study was approved by the Institutional Review Board of Boston University Medical Center, and informed consent was obtained from all participants.
Data collection
On the baseline questionnaire, data on demographics, medical and reproductive history, smoking and alcohol usage, physical activity, sedentary behavior, current weight and height, weight at age 18, and medication usage were collected. Follow-up questionnaires updated information on lifestyle factors and health status. For the variables included in score creation, additional data on alcohol intake (all questionnaires), physical activity level (1997, 1999, 2001, 2007, 2009), time sitting (1997, 1999, 2001), and weight (all questionnaires) were collected on follow-up questionnaires. Physical activity questions ascertained typical hours spent engaging in vigorous activity and walking for exercise per week. In a validation study among a subset of participants, objectively measured activity levels were associated with self-reported physical activity levels (vigorous activity on questionnaire vs. 7-day actigraph measured, r = 0.40) [23]. Participants also answered questions on the typical number of hours per day spent doing sedentary activities, including sitting at work, sitting while commuting to work and watching television. Height (1995) and current weight were used to calculate body mass index (BMI) (kg/m2), and adult weight change was calculated by subtracting weight at age 18 from participant-reported current weight. Self-reported weight (Spearman correlation = 0.97) and height (Spearman correlation = 0.93) were highly correlated with technician measurements in a BWHS validation study [23].
Block Food Frequency Questionnaires (FFQ) were administered at baseline (68 item) and in 2001 (85 item). Participants selected their typical frequency of intake from nine options (foods: ‘never’ to ‘2 + per day; beverages: ‘never’ to ‘6 or more per day’) for commonly consumed foods and beverages. For each food item, typical portion size relative to a defined medium size was selected from three size options in 1995 (‘small’, ‘medium’, and ‘large’) and four options in 2001 (added ‘super’ size). Servings of foods and beverages (sugar beverages, red and processed meat, and fruit and vegetables) were calculated by summing reported frequency of intake weighted by reported typical serving size. Portion size weights were defined relative to a standard medium size for each food or beverage item (small = 0.5 times; large = 1.5 times; super = 2.0 times). Nutrient estimates for caloric, fiber, and sodium intakes were calculated using the National Cancer Institute’s DietCalc software [24]. The baseline FFQ was previously validated in the BWHS [25].
Data on covariates (smoking, family history of colorectal cancer, education, menopausal status, diabetes, insulin usage, aspirin usage, and screening by colonoscopy/sigmoidoscopy) were also collected by questionnaire. Menopausal status was defined by the presence/absence of menstruation and age. Women who reported their periods had ceased due to natural causes, had both ovaries removed or had a hysterectomy but retained one or both ovaries, and were older than 56 years, were classified as postmenopausal. Premenopausal status was defined as ongoing menstrual cycles or a hysterectomy with retention of one or both ovaries among women less than 43 years of age.
WCRF/AICR score creation
Questionnaire data were used to construct scores for adherence to the WCRF/AICR cancer prevention recommendations for BMI, physical activity, and diet (Table 1). Seven of the eight recommendation categories were included in the adherence score for this analysis. The recommendation to limit foods that promote weight gain (energy dense foods, and sugary drinks) was only partially operationalized (sugary beverage intake only) due to insufficient data necessary to calculate energy density. The dietary supplement recommendation was not included due to limited information on supplement use.
To allow for differentiation between barely missing the cut-point for adherence and missing the adherence cut-point by a wide margin, three-level scores were used rather than a binary variable of adherences versus non-adherence. This approach has been used in several previous study populations [10, 26, 27]. For each individual recommendation, 1 point was assigned for complete adherence, 0.5 points for non-adherence level 1 (missed cut-point, but closer to recommendation) and 0 points for non-adherence level 2 (missed cut-point and further from recommendations). Individual recommendation scores were summed to an overall WCRF/AICR adherence score (range 0–7). To separately evaluate adherence to diet-specific recommendations, WCRF/AICR diet recommendations were summed to create a diet-specific adherence score (range 0–5). Cut-points for levels of adherence were based on WCRF/AICR recommendations when explicit numbers were provided in either the outlined public health goals or personal goal recommendations. A lower sodium intake of 1,500 mg/day was chosen because this is the recommended intake for African Americans in the Dietary Guidelines [28]. When specific cut-points were not provided, we used numbers from other standard dietary recommendations, such as the 2010 Dietary Guidelines for Healthy Americans.
Case ascertainment
Colon and rectal cancer cases (ICD-10 colon cancer: C18.0–C18.9 and C26.0; ICD-10 rectal cancer: C19.9 and C20.9) were identified through self-report on the follow-up questionnaires and through linkage with cancer registries in 24 states in which 95 % of participants live. Pathology data were obtained from hospitals or registries for >85 % of cases (99.4 % were confirmed). All self-reported cases were included unless found to be incorrectly reported based on pathology data.
Analytic cohort
The analytic cohort included 49,103 women (681,125 person-years through 2011). Exclusions for the present analysis were: a history of cancer prior to baseline other than non-melanoma skin cancer (n = 1,256, including 138 colorectal cancer cases), pregnant at baseline (n = 1,002), reported implausible energy intake (<600 or >3,800 kcal) or left more than ten FFQ items blank (n = 7,640). To utilize the largest amount of data, women who were missing baseline data for any of the exposure variables for adherence scores were excluded only in the specific analyses for which they were missing data (WCRF/AICR score: n = 6,311; diet score: n = 1,619; fruit and vegetable intake: n = 1,323; body weight: n = 900; physical activity: n = 4,335; alcohol intake: n = 298; sodium intake: n = 19). Average follow-up time between 1995 and 2011 was 15.1 years, and 354 primary colorectal cancer cases (colon = 277; rectal = 77) were identified.
Statistical analysis
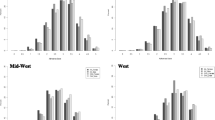
Baseline age-standardized means (continuous variables) and proportions (categorical variables) were calculated across baseline WCRF/AICR score categories for population characteristics. Adherence scores were evaluated as both continuous (unit size = 0.5 point) and categorical variables (three-level variables). Category cut-points for the WCRF/AICR overall score (category boundaries: <3.0 points, 3.0–4.0 points, >4.0 points) and diet score (category boundaries: <2.0 points, 2.0–3.0 points, >3.0 points) were chosen to reflect adherence to less than half, approximately half and more than half of the recommendations. Categories for individual recommendations were adherence (1.0 point), partial adherence (0.5 point) and non-adherence (0 points).
Associations between WCRF/AICR cancer prevention recommendation adherence scores and colorectal cancer were evaluated using Cox proportional hazards regression (PROC PHREG). Person-years were calculated from baseline until the occurrence of colorectal cancer, loss to follow-up, death, or the end of follow-up in 2011. Adherence to WCRF/AICR recommendations and colorectal cancer incidence was evaluated in two ways: using only baseline (1995) exposure and covariate data and using the Andersen–Gill data structure to update the score variables and covariates in a time-varying analysis [29]. The time-varying analytic approach accounts for variability in adherence over time, while the evaluation of baseline data is consistent with the approaches of previously published studies [9–11, 14, 15, 30]. In the time-varying analysis, scores and covariate data were updated at each time point where new data were collected. Test for trend was evaluated by analyzing a variable as continuous. Since the role of diet, physical activity, and body weight may be more strongly associated with colon versus rectal cancers, all analyses conducted with colorectal cancer as the outcome were repeated for colon cancer only [5, 17].
Covariates in the adjusted model were chosen a priori based on factors known or suspected to be associated with colorectal cancer risk. All adjusted models included age, geographic region of residence (Northeast, South, Midwest, West, other), caloric intake (continuous), smoking (never, former, <15 cigarettes/day, ≥15 cigarettes/day), family history of colorectal cancer (yes/no), education (≤12, 13–15, ≥16 years), menopausal status (pre/post), diabetes (yes/no), insulin usage (yes/no), aspirin usage (yes/no), colonoscopy (yes/no), and sigmoidoscopy (yes/no). Diet score and individual recommendations were additionally adjusted for BMI (<25, 25-<30, ≥30 kg/m2), alcohol intake (<1, 1–6, 7–13, ≥14 drinks/week), physical activity level (high: ≥3–4 h/week vigorous activity or ≥5–6 h/week walking for exercise; moderate: 1–2 h/week vigorous exercise or 1–4 h/week walking for exercise; low: <1 h/week vigorous exercise or walking for exercise), and sitting time (≤5, 5–7, ≥8 h/day) when the variable was not part of the score being evaluated. For example, in the diet score model BMI, physical activity, and sitting time were included as covariates, but alcohol was not because it was included in the score.
Results did not change after excluding participants diagnosed with colorectal cancer within 4 years after baseline, so results with all cancer cases diagnosed after baseline are presented. Since associations between diet patterns and colorectal adenomas were stronger among women 50 years of age and older in a previously published BWHS project, sensitivity analyses restricted to women in this age group were performed [31]. Results did not differ and are not presented. While standard BMI definitions of normal weight, overweight, and obese may not be as appropriate in African American women compared to other American women [28], results did not change when different cut-points were chosen. Therefore, for comparability to previously published studies, we present results using standard BMI cut-points. Analyses were conducted using SAS 9.3 (SAS Institute, Inc.).
Results
Adherence to the WCRF/AICR cancer prevention recommendations was low (Table 1). At baseline, 8.5 % of women adhered to more than four recommendations compared to 5.6 % of women who later were diagnosed with colorectal cancer case and 4.9 % who developed colon cancer (data not shown). Less than 6 % of women in the BWHS adhered to more than three diet recommendations. Adherence to individual recommendations was highest for alcohol intake in the overall cohort (94.2 %). For other recommendations, adherence was generally less than 25 %. Descriptive statistics for baseline population characteristics by WCRF/AICR score category are presented in Table 2. Higher adherence was associated with higher education, lower BMI, lower caloric intake, and never smoking.
The results for guideline adherence and colorectal cancer risk are presented in Table 3. Regardless of modeling approach (continuous or categorical, baseline or time-varying), adherence to a greater number of WCRF/AICR recommendations was not significantly associated with colorectal cancer risk. In the continuous, time-varying model, a 0.5 unit higher score resulted in an adjusted HR of 0.98 (95 % CI 0.84–1.15). Results were similar in the baseline model. Adherence to more than four recommendations compared to less than three recommendations was not significantly associated with colorectal cancer incidence in either the baseline (Adjusted HR = 0.86, 95 % CI 0.52–1.44) or time-varying models (Adjusted HR = 0.51, 95 % CI 0.23–1.10). Similarly, adherence to a greater number of diet recommendations was not associated with colorectal cancer risk (>3 vs. <2 diet recommendations time-varying HR = 0.88, 95 % CI 0.48–1.58). No individual recommendation was associated with colorectal cancer incidence.
Results for colon cancer were similar to those for colorectal cancer (Table 4). In the continuous time-varying model, the HR for a 0.5 unit increase in WCRF/AICR score was 1.00 (95 % 0.83–1.19). Adherence to more than four recommendations compared to less than three recommendations was nonsignificantly associated with a lower colon cancer incidence (HR = 0.54, 95 % 0.23–1.26). Adherence to diet-specific recommendations and to any individual recommendation was not associated with colon cancer risk.
Discussion
Higher combined adherence to the WCRF/AICR cancer prevention recommendations was not associated with colorectal cancer risk in this large, prospective cohort of African American women, nor was adherence to any one individual recommendation associated with risk. The absence of association remained when rectal cancer cases were excluded. Adherence to recommendations was low in the BWHS and may have contributed to the lack of association.
Our results are inconsistent with findings from three prior cancer prevention guideline adherence studies that found an association between higher adherence to cancer prevention recommendations and lower risk of colorectal cancer [10, 12, 13]. While there may be differences by gender, associations with adherence remained consistent in the two studies that evaluated risk among women only [12, 13]. The only study to evaluate colon and rectal cancers separately observed lower incidence of both cancer types among participants who adhered to a greater number of recommendations [13]. None of these studies presented data on associations between adherence to individual recommendations and colorectal cancer incidence.
Poor diet [8], low physical activity level [5], high BMI, and waist circumference [4, 7] are considered established risk factors for increased colorectal cancer risk [6], and few studies have evaluated these lifestyle factors among African Americans. Most large cohort studies include few racial/ethnic minorities, and to our knowledge no prospective studies have reported on whether BMI, waist circumference, or physical activity level is associated with colorectal cancer risk in African American women. In a case–control study among African American and Caucasian Americans, associations with dietary factors and colorectal cancer risk differed between African Americans and Caucasian Americans [32–35]. Among Caucasian American women, higher intake of refined carbohydrates and red meat was positively associated with colon cancer, while higher intake of fruits and vegetables was inversely associated with colon and rectal cancers. Conversely, among African American cases and controls, higher fiber intake was inversely associated, while high fruit and added sugar intakes were positively and diets high in legumes and dairy were inversely associated with rectal cancer risk. Increased risk of colorectal adenomas and polyps, potential precursors to colorectal cancer were associated with unhealthy diet patterns, higher body weight, and physical activity levels in the BWHS [31, 36, 37].
Low recommendation adherence likely contributed to the absence of association between adherence and colorectal cancer as only 8.5 % of the cohort met more than half the recommendations at baseline. Adherence to either the ACS or WCRF/AICR recommendations tended to be higher in other previous adherence studies compared with this study. Consistent with our results, adherence to ACS recommendations in the WHI tended to be lower among African American women than Caucasian women. However, adherence levels among African Americans were still higher than observed adherence levels in the BHWS [12]. Small numbers of high adherers may have limited our ability to detect associations in the present study. However, the lack of adherence to recommendations is an important finding on its own, lending support to the potential for low adherence to influence colorectal cancer disparities.
An additional potential reason for the differences in our study results compared to previous adherence studies is that all previous study populations were predominately Caucasian, and WCRF/AICR cancer prevention recommendations are largely based on research in Caucasian populations. The European Prospective Investigation into Cancer and Nutrition (EPIC) study includes few non-Caucasians [10]. The National Institute of Health-American Association of Retired Person (NIH-AARP) study includes <12 % classified as non-Caucasian (including African Americans) [13], and the WHI included 4,609 (7 %) African American women [12]. The WCRF/AICR cancer prevention recommendations, based largely on research in Caucasians, may not be equally applicable to African Americans for either cultural or biological reasons. For example, due to cultural reasons, alcohol intake may be a less effective target for reducing cancer risk in African American women, because alcohol intake is already very low in African American women [38]. Conversely, current recommendations related to body composition focus on BMI and weight gain and may not be appropriate targets for reducing cancer risk among African Americans for biological reasons [39, 40].
This is the first study to evaluate adherence to diet, physical activity, and body weight recommendations targeting cancer prevention and colorectal cancer risk among African American women. Among the strengths of this study is the high follow-up rate in this large prospective cohort. Diet, body weight, and physical activity habits change over time, and previous studies have not evaluated adherence to cancer prevention recommendations over time. The time-varying analytic approach, which accounts from changes in diet, body weight, and physical activity over time, is a major strength of this study.
Among the limitations of this study is the reliance on self-reported data, which are subject to measurement error. Previous validation studies indicate that self-reported diet, physical activity level, and body composition in the BWHS are reported with sufficient accuracy for use in epidemiologic analyses [23, 25], and these factors have been associated with outcomes in the expected manner [41–44]. Finally, a larger sample size would have increased our ability to detect an association, and we lacked the number of cases to evaluate colorectal (i.e., proximal, distal, etc.) cancer subtypes, which may be differentially associated with lifestyle behaviors [5].
Diet, physical activity, and body weight are associated with colorectal cancer risk in Caucasian women, but results on associations in African American women are sparse. The lack of associations with adherence to guidelines on these factors and colorectal cancer risk could reflect lack of relevance of the recommendation or cut-points specifically to African American women. Additionally, the observed low adherence levels support the potential for these factors to contribute to colorectal cancer disparities. Further research is needed to evaluate reasons for low adherence, and to determine whether there are recommendations that may be more relevant for preventing colorectal cancer in African American women.
References
Division of Cancer Prevention and Control-United States Centers for Disease Control and Prevention (2015) Colorectal cancer rates by race and ethnicity. http://www.cdc.gov/cancer/colorectal/statistics/race.htm. Accessed 4 Dec 2015
Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64(2):104–117. doi:10.3322/caac.21220
Laiyemo AO, Doubeni C, Pinsky PF, Doria-Rose VP, Bresalier R, Lamerato LE, Crawford ED, Kvale P, Fouad M, Hickey T, Riley T, Weissfeld J, Schoen RE, Marcus PM, Prorok PC, Berg CD (2010) Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst 102(8):538–546. doi:10.1093/jnci/djq068
Moghaddam AA, Woodward M, Huxley R (2007) Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomark Prev 16(12):2533–2547. doi:10.1158/1055-9965.EPI-07-0708
Robsahm TE, Aagnes B, Hjartaker A, Langseth H, Bray FI, Larsen IK (2013) Body mass index, physical activity, and colorectal cancer by anatomical subsites: a systematic review and meta-analysis of cohort studies. Eur J Cancer Prev 22(6):492–505. doi:10.1097/CEJ.0b013e328360f434
World Cancer Research Fund/American Association for Cancer Research (2011) Continuous update project report. Food, Nutrition, Physical Activity, and the Prevention of Colorectal Cancer
Larsson SC, Wolk A (2007) Obesity and colon and rectal cancer risk: a meta-analysis of prospective studies. Am J Clin Nutr 86(3):556–565
Magalhaes B, Peleteiro B, Lunet N (2012) Dietary patterns and colorectal cancer: systematic review and meta-analysis. Eur J Cancer Prev 21(1):15–23. doi:10.1097/CEJ.0b013e3283472241
Cerhan JR, Potter JD, Gilmore JM, Janney CA, Kushi LH, Lazovich D, Anderson KE, Sellers TA, Folsom AR (2004) Adherence to the AICR cancer prevention recommendations and subsequent morbidity and mortality in the Iowa Women’s Health Study cohort. Cancer Epidemiol Biomark Prev 13(7):1114–1120
Romaguera D, Vergnaud AC, Peeters PH, van Gils CH, Chan DS, Ferrari P, Romieu I, Jenab M, Slimani N, Clavel-Chapelon F, Fagherazzi G, Perquier F, Kaaks R, Teucher B, Boeing H, von Rusten A, Tjonneland A, Olsen A, Dahm CC, Overvad K, Quiros JR, Gonzalez CA, Sanchez MJ, Navarro C, Barricarte A, Dorronsoro M, Khaw KT, Wareham NJ, Crowe FL, Key TJ, Trichopoulou A, Lagiou P, Bamia C, Masala G, Vineis P, Tumino R, Sieri S, Panico S, May AM, Bueno-de-Mesquita HB, Buchner FL, Wirfalt E, Manjer J, Johansson I, Hallmans G, Skeie G, Benjaminsen Borch K, Parr CL, Riboli E, Norat T (2012) Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr 96(1):150–163. doi:10.3945/ajcn.111.031674
Makarem N, Lin Y, Bandera EV, Jacques PF, Parekh N (2015) Concordance with World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) guidelines for cancer prevention and obesity-related cancer risk in the Framingham Offspring cohort (1991–2008). Cancer Causes Control 26(2):277–286. doi:10.1007/s10552-014-0509-9
Thomson CA, McCullough ML, Wertheim BC, Chlebowski RT, Martinez ME, Stefanick ML, Rohan TE, Manson JE, Tindle HA, Ockene J, Vitolins MZ, Wactawski-Wende J, Sarto GE, Lane DS, Neuhouser ML (2014) Nutrition and physical activity cancer prevention guidelines, cancer risk, and mortality in the women’s health initiative. Cancer Prev Res 7(1):42–53. doi:10.1158/1940-6207.CAPR-13-0258
Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, Rohan TE (2015) Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. Am J Clin Nutr 101(3):558–569. doi:10.3945/ajcn.114.094854
Catsburg C, Miller AB, Rohan TE (2014) Adherence to cancer prevention guidelines and risk of breast cancer. Int J Cancer. doi:10.1002/ijc.28887
Hastert TA, Beresford SA, Patterson RE, Kristal AR, White E (2013) Adherence to WCRF/AICR cancer prevention recommendations and risk of postmenopausal breast cancer. Cancer Epidemiol Biomark Prev. doi:10.1158/1055-9965.EPI-13-0210
World Cancer Research Fund/American Association for Cancer Research (2015) Recommendations for cancer prevention. http://www.aicr.org/reduce-your-cancer-risk/recommendations-for-cancer-prevention/. Accessed 11 Dec 2015
Wei EK, Giovannucci E, Wu K, Rosner B, Fuchs CS, Willett WC, Colditz GA (2004) Comparison of risk factors for colon and rectal cancer. Int J Cancer 108(3):433–442. doi:10.1002/ijc.11540
Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM (2012) Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. Journal of the Academy of Nutrition and Dietetics 112(5):624e626–635e626. doi:10.1016/j.jand.2011.11.012
Marshall SJ, Jones DA, Ainsworth BE, Reis JP, Levy SS, Macera CA (2007) Race/ethnicity, social class, and leisure-time physical inactivity. Med Sci Sports Exerc 39(1):44–51. doi:10.1249/01.mss.0000239401.16381.37
Neighbors CJ, Marquez DX, Marcus BH (2008) Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health 98(8):1460–1464. doi:10.2105/AJPH.2006.096982
U.S. Center for Disease Control (2014) Facts about physical activity. http://www.cdc.gov/physicalactivity/data/facts.html. Accessed 11 Apr 2014
Rosenberg L, Adams-Campbell L, Palmer JR (1995) The Black Women’s Health Study: a follow-up study for causes and preventions of illness. J Am Med Womens Assoc 50(2):56–58
Carter-Nolan PL, Adams-Campbell LL, Makambi K, Lewis S, Palmer JR, Rosenberg L (2006) Validation of physical activity instruments: Black Women’s Health Study. Ethn Dis 16(4):943–947
National Cancer Institute (2005) Diet*Calc analysis program, version 1.4.3. National Cancer Institute, Applied Research Program. http://appliedresearch.cancer.gov/DHQ/dietcalc/. Accessed 29 Apr 2015
Kumanyika SK, Mauger D, Mitchell DC, Phillips B, Smiciklas-Wright H, Palmer JR (2003) Relative validity of food frequency questionnaire nutrient estimates in the Black Women’s Health Study. Ann Epidemiol 13(2):111–118
Inoue-Choi M, Lazovich D, Prizment AE, Robien K (2013) Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations for cancer prevention is associated with better health-related quality of life among elderly female cancer survivors. J Clin Oncol 31(14):1758–1766. doi:10.1200/JCO.2012.45.4462
Inoue-Choi M, Robien K, Lazovich D (2013) Adherence to the WCRF/AICR guidelines for cancer prevention is associated with lower mortality among older female cancer survivors. Cancer Epidemiol Biomark Prev 22(5):792–802. doi:10.1158/1055-9965.EPI-13-0054
U.S. Department of Agriculture and U.S. Department of Health and Human Services (2010) Dietary guidelines for Americans. 7th edn. U.S. Goverment Printing Office, Washington, DC
Andersen PK, Gill RD (1982) Cox regression-model for counting-processes—a large sample study. Ann Stat 10(4):1100–1120. doi:10.1214/Aos/1176345976
Vergnaud AC, Romaguera D, Peeters PH, van Gils CH, Chan DS, Romieu I, Freisling H, Ferrari P, Clavel-Chapelon F, Fagherazzi G, Dartois L, Li K, Tikk K, Bergmann MM, Boeing H, Tjonneland A, Olsen A, Overvad K, Dahm CC, Redondo ML, Agudo A, Sanchez MJ, Amiano P, Chirlaque MD, Ardanaz E, Khaw KT, Wareham NJ, Crowe F, Trichopoulou A, Orfanos P, Trichopoulos D, Masala G, Sieri S, Tumino R, Vineis P, Panico S, Bueno-de-Mesquita HB, Ros MM, May A, Wirfalt E, Sonestedt E, Johansson I, Hallmans G, Lund E, Weiderpass E, Parr CL, Riboli E, Norat T (2013) Adherence to the World Cancer Research Fund/American Institute for Cancer Research guidelines and risk of death in Europe: results from the European Prospective Investigation into Nutrition and Cancer cohort study 1,4. Am J Clin Nutr 97(5):1107–1120. doi:10.3945/ajcn.112.049569
Makambi KH, Agurs-Collins T, Bright-Gbebry M, Rosenberg L, Palmer JR, Adams-Campbell LL (2011) Dietary patterns and the risk of colorectal adenomas: the Black Women’s Health Study. Cancer Epidemiol Biomark Prev 20(5):818–825. doi:10.1158/1055-9965.EPI-10-1213
Satia JA, Tseng M, Galanko JA, Martin C, Sandler RS (2009) Dietary patterns and colon cancer risk in Whites and African Americans in the North Carolina Colon Cancer Study. Nutr Cancer 61(2):179–193. doi:10.1080/01635580802419806
Satia-Abouta J, Galanko JA, Martin CF, Ammerman A, Sandler RS (2004) Food groups and colon cancer risk in African-Americans and Caucasians. Int J Cancer 109(5):728–736. doi:10.1002/ijc.20044
Satia-Abouta J, Galanko JA, Potter JD, Ammerman A, Martin CF, Sandler RS, North Carolina Colon Cancer S (2003) Associations of total energy and macronutrients with colon cancer risk in African Americans and Whites: results from the North Carolina colon cancer study. Am J Epidemiol 158(10):951–962
Williams CD, Satia JA, Adair LS, Stevens J, Galanko J, Keku TO, Sandler RS (2009) Dietary patterns, food groups, and rectal cancer risk in Whites and African-Americans. Cancer Epidemiol Biomark Prev 18(5):1552–1561. doi:10.1158/1055-9965.EPI-08-1146
Rosenberg L, Boggs D, Wise LA, Palmer JR, Roltsch MH, Makambi KH, Adams-Campbell LL (2006) A follow-up study of physical activity and incidence of colorectal polyps in African-American women. Cancer Epidemiol Biomark Prev 15(8):1438–1442
Wise LA, Rosenberg L, Palmer JR, Adams-Campbell LL (2008) Anthropometric risk factors for colorectal polyps in African-American women. Obesity 16(4):859–868. doi:10.1038/oby.2007.139
Collins LC, McNair LD (2002) Minority women and alcohol use. Alcohol Res Health 26(4):251–256
Heo M, Faith MS, Pietrobelli A, Heymsfield SB (2012) Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–2004. Am J Clin Nutr 95(3):594–602. doi:10.3945/ajcn.111.025171
Rahman M, Temple JR, Breitkopf CR, Berenson AB (2009) Racial differences in body fat distribution among reproductive-aged women. Metabolism 58(9):1329–1337. doi:10.1016/j.metabol.2009.04.017
Krishnan S, Rosenberg L, Djousse L, Cupples LA, Palmer JR (2007) Overall and central obesity and risk of type 2 diabetes in U.S. black women. Obesity 15(7):1860–1866. doi:10.1038/oby.2007.220
Krishnan S, Rosenberg L, Singer M, Hu FB, Djousse L, Cupples LA, Palmer JR (2007) Glycemic index, glycemic load, and cereal fiber intake and risk of type 2 diabetes in US black women. Arch Intern Med 167(21):2304–2309. doi:10.1001/archinte.167.21.2304
Boggs DA, Palmer JR, Spiegelman D, Stampfer MJ, Adams-Campbell LL, Rosenberg L (2011) Dietary patterns and 14-y weight gain in African American women. Am J Clin Nutr 94(1):86–94. doi:10.3945/ajcn.111.013482
Rosenberg L, Kipping-Ruane KL, Boggs DA, Palmer JR (2013) Physical activity and the incidence of obesity in young African-American women. Am J Prev Med 45(3):262–268. doi:10.1016/j.amepre.2013.04.016
Acknowledgments
S.J.O.N., L.L.A., L.R., and J.P. designed research; S.J.O.N. and J.Y. analyzed data; S.J.O.N., C.D., and L.R. wrote the paper; S.J.O.N. and L.R. had primary responsibility for final content. All authors read and approved the final manuscript. This work was supported by National Cancer Institute grants R01 CA058420 (L. Rosenberg) and UM1 CA164974 (L. Rosenberg). S.J.O.N. is supported by 5T32CA009686-19 (PI: A. Riegel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. Data on breast cancer pathology were obtained from several state cancer registries (AZ, CA, CO, CT, DE, DC, FL, GA, IL, IN, KY, LA, MD, MA, MI, NJ, NY, NC, OK, PA, SC, TN, TX, VA), and results reported do not necessarily represent their views. The authors are grateful to the participants and staff of the BWHS. This study was done in compliance with ethical standards with approval from the Institutional Review Board of Boston University Medical Center and informed consent was obtained from all participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Nomura, S.J.O., Dash, C., Rosenberg, L. et al. Is adherence to diet, physical activity, and body weight cancer prevention recommendations associated with colorectal cancer incidence in African American women?. Cancer Causes Control 27, 869–879 (2016). https://doi.org/10.1007/s10552-016-0760-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0760-3