Abstract
Purpose
To examine whether the documented association of suboptimal cognitive function with total and cardiovascular (CVD) mortality also applies to cancer mortality and probe whether the explanation for this association is biomedical or health care related.
Methods
In a subsample of 733 participants of the EPIC-Greece cohort from Athens and surrounding area, we assessed cognitive function at age 65 or older in the period 2004–2006, using the Mini-Mental State Examination (MMSE). Incidence of cancer, mortality from cancer and CVD, and overall mortality were ascertained through active follow-up for a median of 4 years after MMSE assessment using Cox proportional hazards models.
Results
A total of 86 participants died during follow-up. A 2-point decrease in MMSE score was associated with increase in overall (hazard ratio (HR) 1.26, 95 % confidence interval (CI) 1.11–1.43), CVD (HR 1.26, 95 % CI 1.02–1.56), and cancer (HR 1.32, 95 % CI 1.02–1.70) mortality. In contrast, there was no noticeable difference in cancer incidence associated with a 2-point decrease in MMSE score (HR 1.07, 95 % CI 0.79–1.45).
Conclusions
Cognitive function appears to be inversely associated not only with CVD and overall, but also with cancer mortality. Although for CVD mortality there is a biomedical explanation invoking vascular mechanisms, for cancer mortality we may need to focus on socially conditioned factors, such as compromised ability to identify early signs and suboptimal compliance to treatment. Our hypothesis-generating results need to be confirmed in larger studies, as the issue is of major importance, since cognitive decline is not uncommon among the elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since 1990, several studies, using variable designs, have reported that low cognitive performance or decline in cognition is associated with increased mortality [1–6]. The association is consistent across studies, but the focus has been on cardiovascular diseases (CVD) [3, 4, 6–10]. Frailty [5], biological aging [11, 12], reduced efficiency of processing information [13], and underlying cardiovascular conditions [7] have been invoked as possible underlying mechanisms. Little work has been done on a possible relation between cognitive function and cancer mortality or on comparing the association across causes of death, thus allowing additional insight into the possible underlying mechanisms.
In the present paper, we evaluated the association of cognitive performance with overall and cause-specific mortality in a subsample of the Greek segment of the European Prospective Investigation into Cancer and nutrition (EPIC-Greece). Our study population comprised men and women aged 65 years or older when cognition was evaluated (6–12 years after their enrollment in EPIC-Greece) and who were followed up afterwards for a median of 4 years.
Subjects and methods
Study subjects
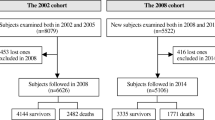
The European Prospective Investigation into Cancer and nutrition (EPIC) is conducted in 10 European countries and investigates the relationships of diet and other lifestyle and environmental factors, as well as genetic factors, with the risk of cancer and other chronic diseases [14]. The Greek segment of EPIC, EPIC-Greece, is a cohort consisting of 28,572 volunteers, women and men, who were recruited from several regions of Greece between 1993 and 1999 (age at recruitment 20–86 years). Active follow-up started in January 1997 and has been repeated every 2–4 years [15, 16].
The present study was conducted in a sub-sample of the EPIC–Greece cohort [17]. Inclusion criteria included residence in the Attica region that surrounds and includes Athens and age at enrolment around 60 years or more. A total of 1,225 eligible subjects were identified. Beginning in March 2004, subjects were invited for assessment of cognitive function and emotional status. Of them, 165 refused to participate, 151 had died during follow-up, 25 had a new permanent residence outside Attica and another 68 could not be traced. Of the 816 volunteers who agreed to participate in the study, 3 with missing information on one or more of the studied variables and 80 without further information on their vital status after their cognitive assessment were excluded from the analysis. Thus, 733 participants were included in the final analyses.
The study was conducted in accordance with the Helsinki Declaration; all participants provided written informed consent before enrolment in the EPIC study and again before enrolment in the study of cognitive function. The study protocol was approved by the Bioethics Committee University of Athens Medical School.
Lifestyle and anthropometry
Baseline socioeconomic, medical and lifestyle characteristics, notably age, years of schooling (as an indicator of socio-economic status), and tobacco smoking were recorded with the help of trained interviewers. Diet was assessed through a validated interviewer-administered FFQ including approximately 150 foods and beverages commonly consumed in Greece [18–20].
The frequency and duration of participation in occupational and leisure-time physical activities were recorded in the questionnaire [21] and allowed the calculation of a metabolic equivalent index (MET value) to each activity [22] and eventually an overall MET × hour sum, which indicates the amount of energy per kilogram of body weight expended during an average day by each participant. Body weight was measured to the nearest 100 g, and height was measured to the nearest 1 cm. Body mass index (BMI) was then calculated as the ratio of weight over the square of height (in kg/m2).
Cognitive function assessment
Subjects were examined by a team of specially trained staff, comprising a nurse, a social worker and a physician, from May 2004 to October 2006 [17], 6.4–12.6 years after enrolment in the EPIC–Greece cohort (median 8.0 years); when the assessment of cognitive function was performed, the participants were 65 years or older. All participants were requested to complete the Mini-Mental State Examination (MMSE). MMSE is a quantitative indicator of cognitive function widely used clinically and epidemiologically, and has been consistently validated as a good indicator of a person’s mental capacity for everyday activities, both internationally [23–26] and in Greece [27]. It consists of thirty questions that assess orientation, attention, immediate and short-term recall, language, and the ability to follow simple verbal and written commands, providing a score that places the individual on a scale of cognitive function from 0 (worst) to 30 (best) [28, 29]. In our analyses, MMSE score was considered in four categories [30]: (1) 25–30 (roughly equivalent to normal cognitive function), (2) 21–24 (mild cognitive impairment), (3) 10–20 (moderate cognitive impairment), and (4) <10 (severe cognitive impairment).
Statistical analysis
Distributions by sociodemographic, lifestyle, medical, and anthropometric variables of study participants were examined by different categories of MMSE scores separately for men and women.
In the main analysis, to evaluate the association of cognitive impairment with mortality (overall and cause-specific), as well as cardiovascular disease (CVD) and cancer incidence, we applied Cox proportional hazards models, assuming as entry time the date of MMSE measurement. In these models, we adjusted for age at MMSE assessment (continuously, in years), sex, BMI (continuously, in 1 kg/m2), height (continuously, in cm), marital status (cohabiting with partner vs alone), physical activity (continuously, in 1 MET × h increments), education level(categorically, <6, 6–11,12 and >12 years of schooling), smoking status(categorically, never/former/current smokers), alcohol intake (categorically, moderate consumption vs low/high consumption; moderate: if males and females consumed ≥10, ≤50 and ≥5, ≤25 g/day, respectively, low/high: if males and females consumed <10 or >50 and <5 or >25 g/day respectively [15], hypertension at enrollment (yes/no), diabetes at MMSE (yes/no), cancer prevalent at MMSE and CVD events prevalent at MMSE (yes/no). In the cancer incidence analysis, we exclude the prevalent at MMSE cancer cases. For BMI, marital status, physical activity and alcohol intake, we used information collected at recruitment. Tests were considered statistically significant when p values were less than 5 % (two-tailed). All statistical analyses were conducted using the Stata Statistical Software, release 11 (Stata Corp. 2009, Stata Corp LP).
Results
Table 1 presents the distributions of the characteristics of the participants by sex and different MMSE score categories. When comparing men with women, we see that men are generally more educated, had higher rates of smoking and hypertension at enrollment, whereas they also had higher prevalence at cognitive assessment of CHD and stroke. With respect to the MMSE score categories, we observe that, in both men and women, the participants with lower MMSE score were less educated, had higher prevalence of diabetes, CHD and stroke at cognitive assessment, as well as higher rates of hypertension at enrollment. Among men, 17 % (46 out of 265) were found to have mild cognitive impairment (MMSE: 21–24) and 5 % (12 out of 265) moderate cognitive impairment (MMSE: 10–20). The respective percentages for women were 19 and 11 %. No participant was found to have severe cognitive impairment (MMSE < 10). The small difference in cognitive function between men and women could be attributed to the difference in educational level.
Table 2 shows mortality ratios (hazard ratios, HR) overall, as well as from CVD and cancer, comparing subjects with mild and moderate cognitive impairment in relation to those with unaffected cognitive function. There are statistically significant trend associations of the same magnitude for all studied outcomes. A 2-point decrease in MMSE was associated with 26 % increase in overall mortality (HR 1.26, 95 % confidence interval (95 % CI) 1.11–1.43) and in CVD mortality (HR 1.26, 95 % CI 1.02–1.56) and with a 32 % increase in cancer mortality (HR 1.32, 95 % CI 1.02–1.70). We repeated the analyses also in a subsample of 508 subjects for whom blood levels of total and HDL cholesterol were also available, controlling also for these variables and the results remained essentially unchanged (data not shown).
Excluding cancers prevalent at MMSE assessment, we also calculated HR for incident cancer overall (21 cases) in Table 3 and we found that a 2-point decrease in MMSE had a non-significant association with cancer incidence in the same direction with mortality, but so weak (HR 1.07, 95 % CI 0.79–1.45) that it could be considered that MMSE decline was essentially unrelated to cancer occurrence.
Discussion
From a moderately sized cohort of 733 subjects aged 65 or more at cognitive function assessment and followed up a median of 4 years after this assessment, we found that lower cognitive function was associated with higher overall and CVD mortality, as well as higher mortality from cancer. We did not, however, find an association between cognitive function and cancer incidence.
An inverse association between cognitive function and mortality has been reported from several previous studies [3–6]. Explicitly or implicitly, the focus has been on CVD [3, 4, 6–10] with vascular conditions [7] suspected as the culprit mechanisms underlying both cognitive decline and mortality. Our results suggest that the inverse association is also present with respect to mortality from cancer. Since systematic conditions, like the vascular ones suspected for CVD, are unlikely to operate for cancer at initial stages, our findings are more compatible with an alternative explanation, i.e., that cognitive decline is associated with a delay in symptom recognition, or poor treatment compliance—both factors affecting mortality rather than incidence of cancer. Our findings, if confirmed in larger studies, would highlight the need for special attention to prompt recognition of symptoms and better treatment compliance among those with suboptimal cognitive function.
The weakness of the present study springs from its moderate sample size, notwithstanding the statistical significant results. However, the findings help to formulate a hypothesis of social conditioning of the association between cognitive decline and survival, which should be more rigorously evaluated in larger prospective investigations. Notwithstanding this limitation, our study also has strengths, including a prospective cohort design, validated instruments, application of these instruments by specially trained health professionals and confirmed outcomes.
In conclusion, the results of our study indicate that the inverse association of cognitive function with cancer mortality is likely to be as strong as that with CVD mortality. Although for CVD mortality a biomedical explanation invoking systematic vascular problems appears plausible, no such explanation is apparent with respect to mortality from cancer. Therefore, for cancer mortality, we may need to focus on socially conditioned factors, which may well apply also to other chronic conditions, including CVD, that substantially contribute to total mortality. Thus, our hypothesis-generating findings, if confirmed in larger studies, would help delineate an important issue, given the non-negligible prevalence of suboptimal cognitive function in aging populations. The implications of our findings with respect to health care and equity could be considerable.
References
Deeg DJ, Hofman A, van Zonneveld RJ (1990) The association between change in cognitive function and longevity in Dutch elderly. Am J Epidemiol 132(5):973–982
Liu IY, LaCroix AZ, White LR, Kittner SJ, Wolf PA (1990) Cognitive impairment and mortality: a study of possible confounders. Am J Epidemiol 132(1):136–143
Lavery LL, Dodge HH, Snitz B, Ganguli M (2009) Cognitive decline and mortality in a community-based cohort: the Monongahela Valley Independent Elders Survey. J Am Geriatr Soc 57:94–100. doi:10.1111/j.1532-5415.2008.02052.x
Batterham PJ, Mackinnon AJ, Christensen H (2012) The association between change in cognitive ability and cause-specific mortality in a community sample of older adults. Psychol Aging 27(1):229–236. doi:10.1037/a0024517
Cano C, Samper-Ternent R, Al Snih S, Markides K, Ottenbacher KJ (2012) Frailty and cognitive impairment as predictors of mortality in older Mexican Americans. J Nutr Health Aging 16(2):142–147
O’Donnell M, Teo K, Gao P et al (2012) Cognitive impairment and risk of cardiovascular events and mortality. Eur Heart J 33(14):1777–1786. doi:10.1093/eurheartj/ehs053
Gale CR, Martyn CN, Cooper C (1996) Cognitive impairment and mortality in a cohort of elderly people. BMJ 312:608
Hart CL, Taylor MD, Davey SG et al (2003) Childhood IQ, social class, deprivation, and their relationships with mortality and morbidity risk in later life: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Psychosom Med 65:877
Shipley BA, Der G, Taylor MD, Deary IJ (2008) Cognition and mortality from the major causes of death: the Health and Lifestyle Survey. J Psychosom Res 65(2):143–152. doi:10.1016/j.jpsychores.2008.02.017
Farid K, Zhang Y, Bachelier D, Gilson P, Teixeira A, Safar ME, Blacher J (2013) Cognitive impairment and malnutrition, predictors of all-cause mortality in hospitalized elderly subjects with cardiovascular disease. Arch Cardiovasc Dis 106(4):188–195. doi:10.1016/j.acvd.2012.12.006
Swan GE, Carmelli D, LaRue A (1995) Performance on the digit symbol substitution test and 5-year mortality in the Western Collaborative Group Study. Am J Epidemiol 141(1):32–40
Anstey KJ, Luszcz MA, Giles LC, Andrews GR (2001) Demographic, health, cognitive, and sensory variables as predictors of mortality in very old adults. Psychol Aging 16:3
Deary IJ, Der G (2005) Reaction time explains IQ’s association with death. Psychol Sci 16:64
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M et al (2002) European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 5(6B):1113–1124
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348(26):2599–2608
Dilis V, Katsoulis M, Lagiou P et al (2012) Mediterranean diet and CHD: the Greek European prospective investigation into cancer and nutrition cohort. Br J Nutr 108:699–709. doi:10.1017/S0007114512001821
Psaltopoulou T, Kyrozis A, Stathopoulos P, Trichopoulos D, Vassilopoulos D, Trichopoulou A (2008) Diet, physical activity and cognitive impairment among elders: the EPIC-Greece cohort (European Prospective Investigation into Cancer and Nutrition). Public Health Nutr 11:1054–1062. doi:10.1017/S1368980007001607
Gnardellis C, Trichopoulou A, Katsouyanni K, Polychronopoulos E, Rimm EB, Trichopoulos D (1995) Reproducibility and validity of an extensive semiquantitative food frequency questionnaire among Greek school teachers. Epidemiology 6:74–77
Trichopoulou A, Georga K (eds) (2004) Composition tables of simple and composite foods. Parisianos, Athens
Willett W, Stampfer M (1998) Implications of total energy intake for epidemiological analyses. In: Wilett W (ed) Nutritional epidemiology, 2nd edn. Oxford University Press, New York, pp 273–301
Trichopoulou A, Gnardellis C, Lagiou A, Benetou V, Trichopoulos D (2000) Body mass index in relation to energy intake and expenditure among adults in Greece. Epidemiology 11:333–336
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25:71–80
Monsch AU, Foldi NS, Ermini-Funfschilling DE, Berres M, Taylor KI, Seifritz E, Stahelin HB, Spiegel R (1995) Improving the diagnostic accuracy of the Mini-Mental State Examination. Acta Neurol Scand 92:145–150
Ishizaki J, Meguro K, Ambo H, Shimada M, Yamaguchi S, Hayasaka C, Komatsu H, Sekita Y, Yamadori A (1998) A normative, community-based study of Mini-Mental State in elderly adults: the effect of age and educational level. J Gerontol B Psychol Sci Soc Sci 53:359–363
Espino DV, Lichtenstein MJ, Palmer RF, Hazuda HP (2001) Ethnic differences in Mini-Mental State Examination (MMSE) scores: where you live makes a difference. J Am Geriatr Soc 49:538–548
Stewart R, Johnson J, Richards M, Brayne C, Mann A (2002) The distribution of Mini-Mental State Examination scores in an older UK African-Caribbean population compared to MRC CFA study norms. Int J Geriatr Psychiatry 17:745–751
Fountoulakis KN, Tsolaki M, Paulopoulos H, Kazis A (2002) Validation of the epidemiological dementia index in geriatric outpatients. Int Psychogeriatr 12:195–208
Folstein MF, Folstein SE, McHugh PR (1975) ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Crum RM, Anthony JC, Bassett SS, Folstein MF (1993) Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA 269:2386–2391
Rabadi MH, Rabadi FM, Edelstein L, Peterson M (2008) Cognitively impaired stroke patients do benefit from admission to an acute rehabilitation unit. Arch Phys Med Rehabil 89(3):441–448. doi:10.1016/j.apmr.2007.11.014
Acknowledgments
The research leading to these results has received funding from the European Union Seventh Framework Program (FP7/2007-2013) under CHANCES Project [grant agreement no. HEALTH –F3-2010-242244].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katsoulis, M., Kyrozis, A., Trichopoulou, A. et al. Cognitive impairment and cancer mortality: a biological or health care explanation?. Cancer Causes Control 25, 1565–1570 (2014). https://doi.org/10.1007/s10552-014-0460-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0460-9