Abstract
Purpose
To assess the pattern of corpus uteri cancer (CUC) in individual states of the USA according to ethnicity.
Methods
Population-based cancer registries from 29 states and the District of Columbia with information on ethnicity for African-American women (AA) and Caucasian-American women (CA) were extracted from the Cancer Incidence in Five Continents (1998–2002, 2003–2007) and the Surveillance, Epidemiology, and End Results Program (SEER; 2008–2010) databases. Rate ratios (RRs) were calculated with respect to ethnicity, age, state, and region.
Results
In southern states, AA had a lower CUC burden among women aged <60 years (AA/CA RR = 0.67; 95 % CI 0.64–0.70), whereas it was higher among women aged ≥60 years (AA/CA RR = 1.22; 95 % CI 1.19–1.26). In other regions, the lower CUC burden among AA aged <60 years was true in all states; however, the CUC burden among AA aged ≥60 years was similar to that of CA. Data for the most recent period (2008–2010) indicate that the age-dependent crossover in CUC burden was not anymore restricted to the South, but also occurred in other regions. Overall, women in the South have had the lowest CUC burden compared with that in all other regions, irrespective of ethnicity and age.
Conclusions
Significant geographic and ethnic variations in the CUC burden exist in the USA. The incidence of hysterectomy could be a factor underlying the geographic variations in CUC burden and particular attention should be given to older AA in southern states.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Corpus uteri cancer (CUC) is the most invasive gynecological cancer among females in the USA, and approximately, 95 % of CUC is diagnosed as endometrial cancer [1, 2]. African-American women (AA) generally experience a lower incidence of CUC, but they have a higher mortality rate compared with Caucasian-American women (CA) [3, 4]. It has been suggested that this higher mortality is partially due to a lower socioeconomic status, which prevents AA from accessing health care and treatment, and also due to a higher prevalence of an aggressive CUC subtype [4–9]. Similar to breast cancer (BC), CUC is a multisubtype disease (subtype I and subtype II) [10] that is differentially influenced by environmental factors, and with a prevalence that varies according to ethnicity [11]. Subtype I (endometrioid adenocarcinoma) is less aggressive and is influenced by exposure to estrogen; this subtype is most likely to occur among younger women and is more prevalent among CA. Subtype II (primarily serous or clear cell histology) is more aggressive, less hormonally dependent, more likely to occur among older women, and more prevalent among AA [5, 12–14].
As with most female cancers, the etiology of CUC remains unknown. However, the risk factors for CUC and BC correlate with reproductive life and anthropometric factors. Late menopause, hormonal-replacement therapy, nulliparity, and obesity are well-established risk factors for CUC. Some of these risk factors such as obesity and parity are modifiable, and their prevalence varies across states and ethnicities in the USA [15–17]. Other factors such as hysterectomy (the surgical removal of the uterus) vary across ethnicities and states. Women who underwent hysterectomy are no longer at risk of endometrial cancer. Therefore, it is possible that the pattern of this cancer might differ from one state to another and might reveal a need for state-specific adaptation of cancer-control strategies. In the USA, there is no clear screening policy for early detection of CUC [18, 19].
The present study aims to assess the CUC pattern across the USA with respect to ethnicity, state, and age group. This was assessed by extracting and analyzing relevant data from the databases of the Cancer Incidence in Five Continents (CI5) volumes IX (CI5-IX; 1998–2002) and X (CI5-X; 2003–2007), and the Surveillance, Epidemiology, and End Results Program (SEER; 2008–2010).
Methods
Database and study populations
The CI5 reports data in a series of monographs published every 5 years by the International Agency for Research on Cancer, which is a specialized branch of the World Health Organization. CI5 is a reference source of cancer incidence data in populations around the world and provides data with respect to gender, age group, race/ethnicity, and subpopulations living in the same geographic area. To date, 10 monographs have been published. The current study utilized data published in the CI5-IX (http://www.iarc.fr/en/publications/pdfs-online/epi/sp160/index.php) and CI5-X (http://ci5.iarc.fr/CI5-X/ci5-X.htm) monographs. CI5-IX and CI5-X compile cancer incidence data from 290 population-based cancer registries in 68 countries for 5 year periods, 1998–2002 (CI5-IX) and 2003–2007 (CI5-X), published in 2007 and 2013, respectively. These data include five registries from five countries in Africa, 42 registries from 15 countries in Asia, 11 registries from Central and South America, 94 registries from 27 countries in Europe, 11 registries from four countries in Oceania, 11 registries from Canada, and 44 registries from 35 states in the USA (for a total of 55 registries from North America) (http://ci5.iarc.fr/CI5i-ix/ci5i-ix.htm; http://ci5.iarc.fr/CI5-X/ci5-X.htm).
The CI5-IX and CI5-X databases contained registries from 29 states and the District of Columbia (DC) that provided information with respect to the African-American and Caucasian-American ethnicities of interest. Data from these registries were analyzed with respect to their location within the four regions defined by the United States Census Bureau: Northeast, South, Midwest, and West (http://www.census.gov/prod/1/gen/95statab/preface.pdf). Figure 1 shows the states that were included in the study categorized into four regions. The Northeast region includes New York, New Jersey, Connecticut, Pennsylvania, Massachusetts, and Rhode Island. The South region includes Florida, Alabama, Texas, Louisiana, Georgia, South Carolina, North Carolina, Virginia, Arkansas, Tennessee, Delaware, Oklahoma, and the District of Columbia. The Midwest region includes Missouri, Illinois, Michigan, Ohio, Indiana, Wisconsin, and Nebraska. The West region includes California, Arizona, Colorado, and Oregon. Of these 29 states and the DC, only 15 had information available regarding ethnicity during 1998–2007. These include New York, New Jersey, Connecticut, and Pennsylvania in the Northeast; Florida, Alabama, Texas, Louisiana, Georgia, and South Carolina in the South; Missouri, Illinois, Michigan, and Ohio in the Midwest; and California in the West. The DC had information regarding ethnicity only during 1998–2002.
SEER Program data for the period 2008–2010 were analyzed to include the most recent data for the states in our study. SEER databases include 20 registries (http://seer.cancer.gov/registries/list.html) that represent 28 % of the geographic area of the USA (http://seer.cancer.gov/about/overview.html). To compare the results obtained from analysis of CI5-IX and CI5-X with those obtained from SEER, we used data from New Jersey for the Northeast, Louisiana for the South, and San Francisco and Los Angeles for California in the West. Greater California was not combined with San Francisco and Los Angeles because the Greater California Cancer Registry became a SEER Registry in 2000, and thus does not contain data for 1998 and 1999. The site of Detroit-Michigan in the Midwest was not used to represent the Midwest because there were only a very small number of cases that did not permit statistically significant analysis. Due to Hurricane Katrina, data from Louisiana in 2005 were excluded from the CI5. In terms of state coverage, 2003–2007 was the most comprehensively inclusive and complete period.
Statistical analysis and modeling
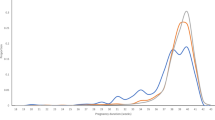
Age-standardized incidence rates (ASR) were adjusted to the world-standard population by 5 year age groups according to Segi [20] and calculated by direct standardization [21]. Population denominators for the periods 1998–2002 (CI5-IX), 2003–2007 (CI5-X), and 2008–2010 (SEER) were derived from US Census Bureau estimations. Population structures of the states and the DC included in the study showed strong differences when stratified by ethnicity Figure S1. Therefore, we modeled the expected number of cases by 5-year ranges in a standard population in which the age-specific rates were adjusted to the world-standard population, rather than expressing the age-specific rates per 100,000. This approach minimized the tendency to overestimate cancer burden in older age groups (where the denominator is low), and thus provided a more accurate distribution of cancer burden across different age groups Figure S2. We chose not to use the US standard population for normalization so that further comparison of these data with those of other countries of the world, including African and Caribbean countries, could be performed in future studies. The rate ratio (RR) and 95 % confidence interval (CI) were calculated with respect to ethnicity, age group, state, and region, to assess the statistical significance in the reported changes during the three study periods (1998–2002, 2003–2007, and 2008–2010). Two age categories were used, including <60 years and ≥60 years. The RRs for CA, AA, and AA/CA were calculated separately for each of the three study periods (1998–2002, 2003–2007, and 2008–2010), and then compared for analysis. Data analyses were conducted with Stata.12 software.
Results
Age-standardized rates and rate ratios for the three study periods
The current study included 103,197 women affected by CUC (93,185 CA and 10,012 AA) for the period 1998–2002; 151,941 (136,908 CA and 15,033 AA) for the period 2003–2007; and 10,431 (9,001 CA and 1,430 AA) for the period 2008–2010. The data included registries from 29 states and the District of Columbia.
During the periods 1998–2002 and 2003–2007, the CUC incidence rate increased for AA in the four regions under study, whereas it increased for CA only in the Northeast and Midwest. However, this increase was mild for CA. In the Northeast, the RR for AA was 1.12 (95 % CI 1.07–1.17), whereas the RR for CA was 1.04 (95 % CI 1.03–1.06). In the Midwest, the RR for AA was 1.13 (95 % CI 1.07–1.19), whereas the RR for CA was 1.03 (95 % CI 1.01–1.04) (Table S1). The median age at diagnosis was similar for both AA and CA and ranged between 62 and 64 years in the four study regions (Table S1).
To compare the results obtained from CI5 data (1998–2002 and 2003–2007) with those obtained from SEER data (2008–2010), we analyzed New Jersey in the Northeast, Louisiana in the South, and San Francisco and Los Angeles in the West. In New Jersey during 2008–2010, the incidence rates were 22.16 and 18.55 per 100,000 for AA and CA respectively. In Louisiana during 2008–2010, the incidence rates were 13.17 and 12.67 per 100,000 for AA and CA respectively. In San Francisco and Los Angeles during 2008–2010, the incidence rates were 17.71 and 19.14 per 100,000 for AA and CA respectively.
Age-specific burden by state and region
Northeast (New York, New Jersey, Connecticut, Pennsylvania, Massachusetts, and Rhode Island)
Figure 2 shows the age-specific CUC burden in the Northeast with respect to state and ethnicity for the periods 1998–2002 and 2003–2007. Overall, in all the northeastern states included in this analysis, AA had a lower CUC burden in all age groups compared with that of CA. The AA CUC burden was particularly low among women aged <60 years. The AA/CA RR among women aged <60 years ranged from 0.48 (95 % CI 0.38–0.61) in Massachusetts to 0.57 (95 % CI 0.50–0.65) in New Jersey for the period 2003–2007 (Table 1). Among women aged ≥60 years, the AA CUC burden was similar to that of CA. For the most comprehensively inclusive period (2003–2007), the pattern was comparable to that of 1998–2002, although some states such as New York, Connecticut, and Rhode Island had a slightly higher but statistically insignificant burden among older women. For New Jersey, during the period 2008–2010, the CUC burden among AA was lower than that of CA for women aged <60 years (AA/CA RR = 0.80; 95 % CI 0.66–0.98). Although an increase was observed in CUC burden among AA aged ≥60 years compared to that of CA, it was mild and not statistically significant (AA/CA RR = 1.07; 95 % CI 0.96–1.20). Overall, in northeastern states during the three study periods, the CUC burden was significantly lower among AA aged <60 years compared with that of CA. During the most comprehensively inclusive period (2003–2007), the AA/CA RR was 0.53 (95 % CI 0.50–0.56) for women aged <60 years. Among women aged ≥60 years, the AA/CA RR was 0.93 (95 % CI 0.90–0.97) (Table 1).
South (Florida, Alabama, Texas, Louisiana, Georgia, South Carolina, North Carolina, Virginia, Arkansas, Tennessee, Delaware, Oklahoma, and the District of Columbia)
Figure 3 shows the age-specific CUC burden in the South with respect to state and ethnicity for the periods 1998–2002 and 2003–2007. In southern states, the CUC burden for AA aged <60 years was lower than that of CA. For the period 2003–2007, the AA/CA RR ranged from 0.50 (95 % CI 0.33–0.74) in Delaware to 0.77 (95 % CI 0.65–0.92) in Louisiana (Table 1). However, in contrast to results for Northeastern states, AA had a higher CUC burden among women aged ≥60 years. Exceptions were observed for the District of Columbia and Virginia, where data were available for only one period (1998–2002 and 2003–2007, respectively).
For women aged ≥60 years during the period 2003–2007, the AA/CA RR ranged from 1.13 (95 % CI .03–1.23) in Texas to 1.49 (95 % CI 1.32–1.68) in Alabama. The same pattern was observed in the state of Louisiana for the period 2008–2010; the AA/CA RR was 0.80 (95 % CI 0.66–0.98) among AA aged <60 years and 1.26 (95 % CI 1.08–1.47) among AA aged ≥60 years. Overall, for the period 2003–2007, AA in southern states had a lower CUC burden among women aged <60 years, and a higher CUC burden among women aged ≥60 years, compared to that of CA. The AA/CA RR = 0.67 (95 % CI 0.64–0.70) for women aged <60 years, whereas the AA/CA RR = 1.22 (95 % CI 1.19–1.26) for women aged ≥60 years (Table 1). This same pattern was observed for the period 1998–2002.
Midwest (Missouri, Illinois, Michigan, Ohio, Indiana, Wisconsin, and Nebraska)
Figure 4 shows the age-specific CUC burden in the Midwest with respect to state and ethnicity for the periods 1998–2002 and 2003–2007. The disease burden pattern in the Midwest was similar to that of the Northeast. However, some states had different results. In Michigan, there was a slight increase in CUC burden among AA aged ≥60 years, but it was similar to that of CA, with AA/CA RR = 0.98 (95 % CI 0.89–1.08). Overall, for Midwestern states, the AA/CA RR was 0.54 (95 % CI 0.51–0.58) for women aged <60 years. For women aged ≥60 years, no statistically significant differences were observed between AA and CA; the AA/CA RR was 0.96 (95 % CI 0.92–1.01) (Table 1).
West (California, Arizona, Colorado, and Oregon)
Figure 5 shows the age-specific CUC burden in the West with respect to state and ethnicity for the periods 1998–2002 and 2003–2007. In Western states and particularly in California, the CUC burden among AA was lower in all age groups during 1998–2002 compared to that of CA. During 2003–2007, the CUC burden among AA aged 60–69 years was higher than that of CA. During 2008–2010, the CUC high burden among AA was extended to women aged ≥60 years, with AA/CA RR = 1.14 (95 % CI 1.02–1.28). In this last period, in California, the CUC burden among AA aged <60 years was lower than that of CA, with AA/CA RR = 0.67 (95 % CI 0.58–0.78). Similar to that observed in Northeast and Midwest regions, AA had a lower CUC burden among women aged <60 years compared to that of CA, whereas the CUC burden among women ≥60 years was similar for both AA and CA (Table 1).
Overall disease incidence rates with respect to age, ethnicity, and region
The strongest discrepancy in CUC incidence between AA and CA among women aged ≥60 years was observed in Southern states during the three study periods. However, Southern states had the lowest CUC incidence rates irrespective of ethnicity compared to those of the other three regions, even after stratifying the rates by age categories. For the most comprehensively inclusive period (2003–2007), the overall rate in the Northeast for CA was 1.60-fold higher (95 % CI 1.58–1.63) than that in the South; 1.53-fold higher (95 % CI 1.50–1.57) for women aged <60 years; and 1.67-fold higher (95 % CI = 1.64–1.70) for women aged ≥60 years. For AA, the overall rate in the Northeast was 1.25-fold higher (95 % CI 1.20–1.30) than that in the South; 1.21-fold higher (95 % CI 1.13–1.30) for women aged <60 years; and 1.27-fold higher (95 % CI 1.21–1.33) for women aged ≥60 years (Table 2).
Discussion
CUC shares common risk factors with BC, but it is understudied in the USA. Evidence shows that both BC and CUC can be classified into subtypes that are influenced by estrogen exposure, and both have incidence rates that vary according to ethnicity. The most aggressive BC subtype is not responsive to hormones and is more prevalent among younger women and AA, whereas the hormone-dependent BC subtypes are more prevalent among older women and CA [23–26]. Similarly to that observed in BC, the present study identified an age-dependent CUC burden crossover among CA and AA; AA had a lower CUC burden among women aged <60 years and a higher CUC burden among women aged ≥60 years compared to that of CA, which is the inverse of that observed for BC. This observation was most pronounced for southern states, but the tendency was observed in some states of other regions during the most recent study period (2008–2010).
The lower CUC burden among younger AA might reflect the incidence of CUC subtype I, which is known to be more prevalent among CA and younger women [14]. The higher CUC burden among older AA might reflect the incidence of CUC subtype II, which is known to be more prevalent among AA and older women [14]. Anthropometric factors such as obesity, nulliparity, late menopause, and hormone-replacement therapy are well-established risk factors for CUC. These risk factors are more prevalent with the occurrence of subtype I, which correlates with excess estrogen and menopausal hormone therapy [12, 27, 28]. In the USA, AA have the highest prevalence of obesity compared to that of other ethnic/racial groups (39.2 % for AA vs 21.8 % for CA). The prevalence of AA obesity is highest in the South and Midwest (40.6 and 40.1 %, respectively) compared to that in the Northeast (36.1 %) and West (California; 23.8 %) [15]. AA have a reportedly decreased risk for CUC subtype I compared with that of CA; by contrast, AA have an increased risk for CUC subtype II [5, 14, 29].
Although granular data on the usage pattern of hormone-replacement therapy (HRT) in individual states and ethnicities are not available, it has been reported that CA are more likely to receive HRT than are AA [30, 31]. Thus, the CUC pattern among AA aged ≥60 years in the South might reflect an excess of CUC subtype II, which is associated with a worse outcome [32]. Detailed information on CUC mortality by state and ethnicity is not available; however, AA have a higher mortality from CUC compared with that of CA [33, 34].
The present study identified an overall lower CUC burden in the South compared with that of other regions, irrespective of ethnicity. The CUC burden among women aged <60 years was lower for AA in all states included in this study. Hysterectomy is the most effective method to prevent endometrial cancer; the prevalence of hysterectomy in USA varies with respect to geographical regions and ethnicity. The highest rate of hysterectomy was reported among women aged 30–54 years. Among women younger than 35, the hysterectomy rate was three times higher in the South compared with that in the Northeast and was overall higher among AA compared with that of CA [35, 36]. It has been suggested that an omission to correct for hysterectomy during calculation of CUC burden could lead to an underestimation of the incidence rate, particularly in the South where the hysterectomy rate is highest [37]. Hence, the low CUC burden observed in the South might be due to an artifact introduced by hysterectomy, which would cause underestimation of CUC burden particularly among women aged <60 years. However, the prevalence of hysterectomy in many Southern states is higher in CA compared to that in AA [37]. This might also explain why AA aged ≥60 years have a higher CUC burden in the South. However, the disease pattern observed in the South appears to be extending to other regions for the most recent study period.
First-degree family history of BC has been reported to be positively associated with CUC subtype II (RR = 1.93; 95 % CI 1.27–2.93), whereas it was inversely associated with CUC subtype I (RR = 0.80; 95 % CI 0.67–0.96) [5]. Therefore, the possibility of an interaction between breast and corpus uteri cancers that could explain the disease burden among older AA should be investigated. The age-dependent crossover in BC disease burden between AA and CA is the inverse of what we observed for CUC in the present study.
Screening strategies for most female cancers such as breast and cervical cancers have been developed, but there is no clear strategy for CUC screening. The American Cancer Society concluded that there was not sufficient evidence to support recommendations for routine screening for endometrial cancer [18, 19]. However, our study indicates that more intervention should be performed for CUC, and particular attention should be given to older AA in the South.
In conclusion, this study showed that although southern states had an overall lower CUC burden, most likely due to artifact associated with hysterectomy rates, there was an age-dependent crossover in CUC burden in the South; AA aged <60 years had a lower disease burden, whereas AA aged ≥60 years had a higher disease burden. Although this tendency also was observed in states of other regions during 2008–2010, it was more prevalent in southern states during all three study periods (1998–2002, 2003–2007, and 2008–2010). The similar tumor characteristics between breast and corpus uteri cancers [38] suggest that their common risk factors might unfold differently according to the disease subtype.
References
Shingleton HM, Fowler WC, Jordan JA, Lawrence WD (1996) Gynecologic oncology: current diagnosis and treatment. W. B. Saunders, London
Platz CE, Benda JA (1995) Female genital tract cancer. Cancer 75:270–294
Aziz H, Hussain F, Edelman S et al (1996) Age and race as prognostic factors in endometrial carcinoma. Am J Clin Oncol 19:595–600
Connell PP, Rotmensch J, Waggoner SE, Mundt AJ (1999) Race and clinical outcome in endometrial carcinoma. Obstet Gynecol 94:713–720
Brinton LA, Felix AS, McMeekin DS et al (2013) Etiologic heterogeneity in endometrial cancer: evidence from a gynecologic oncology group trial. Gynecol Oncol 129:277–284
Byers TE, Wolf HJ, Bauer KR et al (2008) The impact of socioeconomic status on survival after cancer in the United States : findings from the National Program of Cancer Registries Patterns of Care Study. Cancer 113:582–591
Clegg LX, Reichman ME, Miller BA et al (2009) Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 20:417–435
Madison T, Schottenfeld D, James SA, Schwartz AG, Gruber SB (2004) Endometrial cancer: socioeconomic status and racial/ethnic differences in stage at diagnosis, treatment, and survival. Am J Public Health 94:2104–2111
Niu X, Pawlish KS, Roche LM (2010) Cancer survival disparities by race/ethnicity and socioeconomic status in New Jersey. J Health Care Poor Underserved 21:144–160
Bokhman JV (1983) Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 15:10–17
Kurman RJ, Zaino RJ, Norris HJ (1994) Endometrial carcinoma. In: Kurman RJ (ed) Blaustein’s pathology of the female genital tract. Springer, New York, pp 439–486
Ali AT (2013) Risk factors for endometrial cancer. Ceska Gynekol 78:448–459
Sonoda Y, Barakat RR (2006) Screening and the prevention of gynecologic cancer: endometrial cancer. Best Pract Res Clin Obstet Gynaecol 20:363–377
Yang HP, Wentzensen N, Trabert B et al (2013) Endometrial cancer risk factors by 2 main histologic subtypes: the NIH-AARP diet and health study. Am J Epidemiol 177:142–151
Anonymous(2009) Differences in prevalence of obesity among black, white, and Hispanic adults—United States, 2006–2008. MMWR Morb Mortal Wkly Rep 58: 740–4
Tinelli A, Vergara D, Martignago R, Leo G, Malvasi A, Tinelli R (2008) Hormonal carcinogenesis and socio-biological development factors in endometrial cancer: a clinical review. Acta Obstet Gynecol Scand 87:1101–1113
Crosbie EJ, Zwahlen M, Kitchener HC, Egger M, Renehan AG (2010) Body mass index, hormone replacement therapy, and endometrial cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 19:3119–3130
Smith RA, Cokkinides V, Brawley OW(2012) Cancer screening in the United States, 2012: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin
Smith RA, Manassaram-Baptiste D, Brooks D et al (2014) Cancer screening in the United States, 2014: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 64:30–51
Segi M (1960) Cancer mortality for selected sites in 24 Countries. In: Sendai, Tohoku (eds) University School of Public Health, 1950–1957
International Agency for Research on Cancer (1991) Cancer registration principles and methods. IARC Press, Lyon
Sighoko D, Kamate B, Traore C et al (2013) Breast cancer in pre-menopausal women in West Africa: analysis of temporal trends and evaluation of risk factors associated with reproductive life. Breast 22:828–835
Griffiths CL, Olin JL (2012) Triple negative breast cancer: a brief review of its characteristics and treatment options. J Pharm Pract 25:319–323
Sturtz LA, Melley J, Mamula K, Shriver CD, Ellsworth RE (2014) Outcome disparities in African American women with triple negative breast cancer: a comparison of epidemiological and molecular factors between African American and Caucasian women with triple negative breast cancer. BMC Cancer 14:62
Sparano JA, Wang M, Zhao F et al (2012) Race and hormone receptor-positive breast cancer outcomes in a randomized chemotherapy trial. J Natl Cancer Inst 104:406–414
Yang XR, Chang-Claude J, Goode EL et al (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103:250–263
Ali AT (2014) Reproductive factors and the risk of endometrial cancer. Int J Gynecol Cancer 24:384–393
Amankwah EK, Friedenreich CM, Magliocco AM et al (2013) Anthropometric measures and the risk of endometrial cancer, overall and by tumor microsatellite status and histological subtype. Am J Epidemiol 177:1378–1387
Setiawan VW, Yang HP, Pike MC et al (2013) Type I and II endometrial cancers: have they different risk factors? J Clin Oncol 31:2607–2618
Brett KM, Chong Y (2011) Hormone replacement therapy knowledge and use in the United States, N.C.f.H. Statistics. CDC, Hyattsville
Brown AF, Perez-Stable EJ, Whitaker EE et al (1999) Ethnic differences in hormone replacement prescribing patterns. J Gen Intern Med 14:663–669
Alektiar KM, Venkatraman E, bu-Rustum N, Barakat RR (2003) Is endometrial carcinoma intrinsically more aggressive in elderly patients? Cancer 98:2368–2377
Olson SH, Atoria CL, Cote ML et al (2012) The impact of race and comorbidity on survival in endometrial cancer. Cancer Epidemiol Biomarkers Prev 21:753–760
Wright JD, Fiorelli J, Schiff PB et al (2009) Racial disparities for uterine corpus tumors: changes in clinical characteristics and treatment over time. Cancer 115:1276–1285
Kjerulff KH, Guzinski GM, Langenberg PW, Stolley PD, Moye NE, Kazandjian VA (1993) Hysterectomy and race. Obstet Gynecol 82:757–764
Sherman ME, Carreon JD, Lacey JV Jr, Devesa SS (2005) Impact of hysterectomy on endometrial carcinoma rates in the United States. J Natl Cancer Inst 97:1700–1702
Siegel RL, Devesa SS, Cokkinides V, Ma J, Jemal A (2013) State-level uterine corpus cancer incidence rates corrected for hysterectomy prevalence, 2004–2008. Cancer Epidemiol Biomarkers Prev 22:25–31
Lax SF (2004) Molecular genetic pathways in various types of endometrial carcinoma: from a phenotypical to a molecular-based classification. Virchows Arch 444:213–223
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sighoko, D. Ethnic and geographic variations in corpus uteri cancer burden: evidence based on data from 29 states and the District of Columbia. CI5 IX, X and SEER data (1998–2010). Cancer Causes Control 25, 1197–1209 (2014). https://doi.org/10.1007/s10552-014-0425-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0425-z