Abstract
Purpose
There is a long-standing debate about whether statins have chemopreventive properties against colorectal cancer (CRC), but the results remain inconclusive. We therefore present a meta-analysis to investigate the association between statin use and risk of CRC.
Methods
A comprehensive literature search was undertaken through July 2013 looking for eligible studies. Pooled relative risk (RR) estimates and 95 % confidence intervals (CIs) were used to calculate estimated effect.
Results
Forty-two studies [18 case–control studies, 13 cohort studies, and 11 randomized controlled trials (RCTs)] were included in this analysis. Overall, statin use was associated with a modest reduction in the risk of CRC (RR = 0.90, 95 % CI 0.86–0.95). When the analyses were stratified into subgroups, a significant decreased association of CRC risk was observed in observational studies (RR = 0.89, 95 % CI 0.84–0.95), rectal cancer (RR = 0.81, 95 % CI 0.66–0.99), and lipophilic statin (RR = 0.88, 95 % CI 0.85–0.93), but not in RCTs (RR = 0.96, 95 % CI 0.85–1.08), colon cancer, and hydrophilic statin. However, long-term statin use (≥5 years) did not significantly affect the risk of CRC (RR = 0.96, 95 % CI 0.90–1.03). Cumulative meta-analysis showed that statin use significantly reduces the risk of CRC, which has been available between 2007 and 2013.
Conclusions
Our results suggest that statin use is associated with a modest reduced risk of CRC; apparent associations were found for lipophilic statin use. However, long-term statin use did not appear to significantly affect the risk of CRC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common cancers, and CRC-related deaths are highly prevalent worldwide, which has become a major public health challenge [1]. In 2013, there were 142,820 estimated new cases, and 50,830 estimated deaths from CRC occurred in the USA [2]. Moreover, the five-year survival rate remains low in advanced CRC [3]. Although improved oncological techniques and advanced treatment have certainly had a positive impact on CRC outcomes, further advances in outcomes should be possible with chemopreventive strategies [4]. Thus, prevention efforts merit additional consideration.
Statins (3-hydroxy-3-methyl glutaryl-coenzyme A reductase inhibitors), a group of cholesterol-lowering drugs, are used to manage and prevent coronary heart disease. Recent experimental evidence suggests that statins have an additional chemopreventive potential through inhibiting tumor growth and angiogenesis [5], attenuating metastatic potential [6], stimulating cellular immunity, and potentiating the antitumor effects of some cytokines [7]. A growing number of epidemiologic studies [8–38] have investigated the association between statin use and risk of CRC. There were also many randomized controlled trials (RCTs) of statins [39–53]. However, the results of these trials have been inconsistent, with some studies reporting reduced risk, some describing an increased risk, and others failing to identify any effect.
A previous meta-analysis done by Bonovas et al. [54] in 2007 did not support the hypothesis that statins strongly reduce the risk of CRC using six RCTs and twelve observational studies published between 1995 and 2007. The last study conducted by Bardou et al. [55], last updated in September 2009, suggests a small reduction in the risk (9 %) of CRC attributable to chronic statin use. Thirteen observational studies [19–25, 33–38] published after 2009 have also shown contrasting results, including decreased risk [19, 21, 24, 38], increased risk [22], and no probable association, which has added new evidence to the previous research.
In view of the widespread use of statins, more knowledge is needed on the association between statins and risk of CRC. Therefore, we performed a comprehensive meta-analysis of all published studies to better understand this issue.
Methods
Systematic search
A systematic literature search of PubMed, Embase, Web of Science, and Cochrane library databases was conducted by two investigators (Y. Liu and S. Li) independently for all relevant articles on the effects of statin use on CRC risk (last update on July 30, 2013). The MeSH and free text keywords search terms included the following: (1) statins: “HMG-CoA reductase inhibitor(s),” “statin(s),” “simvastatin,” “lovastatin,” “fluvastatin,” “atorvastatin,” “pravastatin,” “rosuvastatin,” “cerivastatin,” “mevastatin”; (2) colorectal cancer: “cancer,” “neoplasm(s),” “neoplasm,” “malignancies,” “malignancy”; (3) human study. No language restrictions were imposed. Additional studies were scanned by manual search through the reference lists of relevant articles. We followed the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines [56] and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement [57] to report our analysis.
Eligibility criteria
Studies were included if they met all the following inclusion criteria: (1) The original studies evaluated exposure to statins and risk of CRC; (2) They provided a relative risk (RR) estimate (risk ratio, rate ratio, hazard ratio, or odds ratios) with the corresponding 95 % confidence intervals (95 % CIs) or sufficient data to calculate them; (3) They were full-text articles. Studies were excluded if (1) they did not fulfill the inclusion criteria; (2) they were reviews, letters, editorials, conference abstracts, or case reports; (3) they were animal trials. When multiple publications from the same population were identified, only the most recent study was included, unless the reported outcomes were mutually exclusive. Disagreements in the study selection were discussed among the co-authors until consensus was reached.
Data extraction
Data were independently abstracted onto a standardized form by two reviewers (S. Li and Y. Liu). Conflicts were resolved by consensus, referring back to the original article. The following data were collected from each study: first author’s name, study year, region of origin, study design, total number of persons in each group, exposure period of study, primary outcome reported, type of medication, dose and duration of statin use (if reported), follow-up period, information source for exposure measurement, multivariable-adjusted risk estimates and their 95 % CIs, and adjustment for confounding variables.
Statistical analysis
The use of statins is defined as ‘overall use’: all the reported intake levels of statin use. Pooled relative risks were used to estimate the effect and were calculated by two techniques: a random-effects model (the DerSimonian and Laird method) [59] and a fixed-effects model (the Mantel–Haenszel method) [60]. When heterogeneity is found, the random-effects model is considered more appropriate, although both models may be biased [61]. Statistical heterogeneity was assessed by performing Cochran Q and I 2 test [62, 63]. Sensitivity analyses were also conducted to assess the robustness of results by sequential omission of individual studies [64]. Additionally, the Galbraith plot was used to spot the outliers as the possible major sources of heterogeneity [65]. Cumulative meta-analysis was conducted to examine how the evidence has changed over time. Publication bias was assessed graphically using a funnel plot and quantitatively using the Begg rank correlation test [66] and the Egger regression asymmetry test [67]. All p < 0.05 (two-sided) was considered as significant unless otherwise specified. All analyses were performed using STATA, version 12.0 (StataCorp, College Station, TX).
Results
Study selection and characteristics
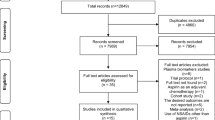
A total of 12,540 articles were identified during the initial search (Fig. 1). After removing the duplicates and reviewing the titles and abstracts, 9,201 were found to be ineligible as they were reviews, letters, editorials, conference abstracts, or case reports, or they were not relevant based on title or abstract. Fifty-one full-text articles were reviewed for more detailed evaluation. Seven articles were excluded for reasons. In particular, studies by Kushiro et al. [50], Matsushima et al. [53], and Limburg et al. [52] were post hoc analyses of primary studies. Finally, 42 studies [8–38] were identified as suitable for meta-analysis. Eighteen articles [8–25] used a case–control design, 13 articles [26–38] used a cohort design, and eleven studies were RCTs [39–49]. The publication dates of the studies included in the meta-analysis ranged from 1995 to 2013. The characteristics of case–control studies, cohort studies, and RCTs in this meta-analysis are presented in Tables 1, 2, and 3, respectively.
Overall analysis
We performed a combined analysis of observational studies and RCTs. Compared to non-use, the use of statins at any point in time was associated with a statistically significant 10 % reduction in the incidence of CRC (random-effects models: pooled RR = 0.90, 95 % CI 0.86–0.95; p < 0.001). Meanwhile, a moderate degree of heterogeneity was observed among all the studies (I 2 = 66.5 %; p < 0.001) (Fig. 2). Sensitivity analysis was performed to evaluate the robustness of the results. The omission of any individual study did not alter the direction and magnitude of the positive effect (data were not shown). This analysis demonstrated that no study influenced the overall results, confirming the stability of our results.
Meta-analysis of RCTs
Eleven large RCTs of statins involving 95,984 participants were included in the analysis [39–49]. Meta-analysis of all eleven trials indicated a non-significant decrease in CRC risk in all statin users (random-effects models: pooled RR = 0.96, 95 % CI 0.85–1.08, p = 0.491; fixed-effects models: RR = 0.94, 95 % CI 0.86–1.04, p = 0.239). The Cochran’s Q test resulted a p = 0.238 and the corresponding I 2 = 21.6 %, both indicating the absence of heterogeneity (Fig. 2). Sensitivity analysis also demonstrated that no study apparently influenced the overall results (data were not shown).
Meta-analysis of observational studies
Eighteen case–control articles [8–25] and thirteen cohort articles [26–38] involving 7,812,690 participants evaluated exposure to any statins and CRC risk. Nine reports [11, 17, 19, 21, 23, 24, 29, 33, 38] indicated a significantly lower risk of CRC in the treatment group, while one report [22] found a significantly higher risk, and others did not obtain statistically significant results. A pooled analysis of 31 studies indicated that compared to non-use, ever having used statins was statistically significantly associated with a modest reduction in the risk of colorectal cancer (random-effects models: pooled RR = 0.89, 95 % CI 0.84–0.95; p < 0.001). Meanwhile, a high degree of heterogeneity was observed among all the studies (I 2 = 72.6 %; p < 0.001) (Fig. 2).
Sensitivity analysis demonstrated that study by Vinogradova et al. [22] apparently influenced the overall results. When the Galbraith plot was analyzed, seven outliers [11, 15, 21, 22, 24, 29, 32] were identified as the major sources of heterogeneity. By excluding these studies from the analysis, similar pooled RR and significance were obtained (RR = 0.93, 95 % CI 0.90–0.98; p < 0.001), and heterogeneity was decreased (I 2 = 15.9 %; p = 0.242) (data not shown). After stratifying the data into subgroups based on study design, we found a significant inverse association between statin use and risk of CRC in both case–control studies (RR = 0.84, 95 % CI 0.76–0.93; p = 0.001) and cohort studies (RR = 0.93, 95 %CI 0.87–0.99; p = 0.019), although both showed significant heterogeneity within the group (Fig. 2).
Other subgroup analysis
Colon and rectal cancer
We extracted the available data from studies that reported RR estimates for colon cancer and rectal cancer separately. There were 13 studies [8–13, 15, 25, 30, 32–34, 36] that evaluated exposure to any statins and colon cancer risk, and 11 studies [9–13, 15, 25, 30, 32, 33, 36] that evaluated rectal cancer risk. The pooled results indicated that statin use was statistically significantly associated with a modest reduction in the risk of rectal cancer (RR = 0.81, 95 % CI 0.66–0.99, p = 0.040; heterogeneity: I 2 = 69.6 %), but not colon cancer risk (RR = 0.97, 95 % CI 0.92–1.01, p = 0.142; heterogeneity: I 2 = 32.3 %). Funnel plots were presented in Online Resource 1.
Long-term statin use
Clinical studies require a longer-term follow-up after statin use to detect cancer outcomes for the long latency period of CRC [68]. We chose ≥5 years as a cutoff point of long term, according to the mean of follow-up and statin use in RCTs. Pooled results showed that long-term statin use did not significantly affect the risk of CRC (random effect model: RR = 0.96, 95 % CI 0.88–1.04, p = 0.297; fixed effect RR = 0.96, 95 % CI 0.90–1.03, p = 0.235). No statistical heterogeneity was observed among studies (I 2 = 26.5 %; p = 0.134) (Fig. 3). Stratification by study design showed that the direction and magnitude of estimate effect did not change essentially (case–control studies: RR = 0.95, 95 % CI 0.84–1.07, p = 0.399; cohort studies: RR = 0.98, 95 % CI 0.90–1.07, p = 0.715; RCTs: RR = 0.91, 95 % CI 0.78–1.07, p = 0.254). No statistical heterogeneity was observed among cohort studies and RCTs (I 2 = 0.0 %, p = 0.917 and I 2 = 0.0 %, p = 0.547, respectively), but moderate heterogeneity was observed among case–control studies (I 2 = 68.6 %, p = 0.004) (Fig. 3).
Type of statin
With respect to statin type, we categorized statins according to whether they were lipophilic (simvastatin, lovastatin, fluvastatin, and atorvastin) or hydrophilic (pravastatin and rosuvastatin), as it has been hypothesized that the preventive effect of statins against cancer may be more apparent to lipophilic than hydrophilic statins [69]. As expected, the pooled results only showed a significant association between lipophilic statin use and CRC risk (RR = 0.88, 95 % CI 0.85–0.93, p < 0.001) and a null association between hydrophilic statin use and CRC risk (RR = 0.88, 95 % CI 0.76–1.02, p = 0.088). Statistical heterogeneity for both was observed (I 2 = 94.0 %, p < 0.001 and I 2 = 75.5 %, < 0.001, respectively). Funnel plots were presented in Online Resource 1.
Cumulative meta-analysis
A cumulative meta-analysis of a total of 42 studies was carried out to evaluate the cumulative effect estimate over time. In 1995, Shepherd et al. [39] first reported a significant effect estimate of 0.90. Between 1995 and 2007, 20 studies were published, with a cumulative RR of 0.86 (95 % CI 0.79–0.94). Between 2007 and 2013, 22 more publications were added cumulatively, resulting in an overall effect estimate of 0.89 (95 % CI 0.84–0.95) (Fig. 4).
Publication bias
Begg’s funnel plot and Egger’s test were performed to access the publication bias of the literature included in this meta-analysis. The shapes of the funnel plot did not reveal obvious evidence of asymmetry for the overall analysis, and the p values for Begg’s test and Egger’s test were 0.416 and 0.113, respectively. The above results suggest that publication bias was not evident in this meta-analysis.
Discussion
There is a long-standing debate concerning the association between use of statins and cancer. As a result, statins are now being studied in clinical trials for cancer prevention. Several reviewed studies have discussed the potential chemoprevention of statin use against cancer at various sites, such as breast [70], prostate [71], pancreatic [72], and hepatocellular cancer [73]. This meta-analysis of 18 case–control studies, 13 cohort studies, and 11 RCTs involving more than 7.9 million patients demonstrates that the RR of CRC after statins use is 0.90 (95 % CI 0.86–0.95). In other words, summary estimates suggest that the use of statins is associated with a modest reduction in risk of CRC compared to non-users. Similar results were found in subgroup analyses of case–control and cohort studies. This effect was more pronounced and consistent in the rectal cancer and lipophilic statin users. However, our results do not support the hypothesis that long-term statin use may reduce the risk of CRC incidence. On the other hand, it provides evidence that long-term statin use is not associated with a substantially decreased or increased risk of CRC. The likelihood of important selection and publication bias in our meta-analysis is small.
Present findings were statistically significantly associated with a modest reduction of approximately 10 % in the risk of CRC, a more pronounced result than Bardou et al.’s [55] findings of a 9 % risk reduction. This is likely to be due to the inclusion of 13 new studies published after Bardou et al.’s [55] meta-analysis, which showed a positive association between statin use and a reduced risk of CRC [19, 21, 24, 38]. Cumulative meta-analysis showed a change in the trend of reporting risk to continue positive in statin users between 2007 and 2013 (Fig. 4).
A meta-analysis of dose, duration, and type effects of statins was expected, because each of these drugs has its own side effect profile and so far, no single agent has been recommended for chemopreventive use in the general population. However, statin dose varied in each trial, making statistical analysis between these groups impossible. We were capable of investigating potentially different effects on risk by the long-term duration and type of statins used. The decreased risk of CRC in long-term statin users was found here to be non-significant. There are several plausible explanations of the discrepancy between the overall results and those for long-term statin use. First, the definition of ‘‘long-term use’’ varied among the studies, which could have led to non-significant results. Second, long-term users of statins tend to be healthier and more adherent to therapy. They have easier and more frequent access to preventive healthcare services such as screening colonoscopies, which theoretically could lower the incidence of colorectal cancer by removing colorectal adenomas. Moreover, statin users might have healthier lifestyle habits than non-users of statins, particularly after beginning to take the drugs. However, the long-term studies may have failed to adjust fully for these factors, possibly leading to residual confounding.
It is hypothesized that lipophilic statins (e.g., simvastatin, lovastatin) may have a greater chemoprotective effect than hydrophilic statins (e.g., pravastatin) due to greater lipid solubility and membrane permeability [74]. In this analysis, a significant reduction in CRC risk was observed in lipophilic statin users but not in hydrophilic statin users, which was consistent with previous research. This may shed light on recommending lipophilic statin for chemopreventive use in the specific population.
Use of statins is associated with a reduced risk of CRC in some, but not all, studies. Recent studies suggest this may be related to genetic variation in 3-hydroxy-3-methylglutaryl CoA reductase (HMGCR) activity [75]. Lipkin et al. [75] found that the genetic variant in the HMGCR gene significantly modified the protective association between statins and CRC risk and is associated with lower serum levels of low-density lipoprotein. Lee et al. [36] found that KRAS mutation status may also modified statins’ protective properties, while these required further confirmation. We anticipate that these data may advance the development of personalized statin use for reducing the risk of cancer.
Heterogeneity is a potential problem when interpreting the results of a meta-analysis, and finding sources of heterogeneity is one of the most important goals of meta-analysis [76]. In the present meta-analysis, significant between-study heterogeneity was observed in the pooled analyses of total eligible studies (I 2 = 72.6 %, p < 0.001). To find the sources of heterogeneity, we performed sensitivity, subgroup, and Galbraith plot analyses. The subgroup analyses based on different study designs could not explain the significant heterogeneity seen in the overall analysis. Colorectal cancer site and participants’ sex may be the sources of heterogeneity. Seven outliers (Poynter et al. [11], Boudreau et al. [15], Samadder et al. [21], Vinogradova et al. [22], Lakha et al. [24], Farwell et al. [29], and Haukka et al. [32]) were identified as the main contributors to heterogeneity by using Galbraith plot and sensitivity analyses. Five of them were case–control studies, which have limitations including different populations with different underlying CRC risks, different control groups, and insufficient statin exposure to detect a protective effect (some studies included patients with statin exposure of only 30 days [21]). Interestingly, when these studies were excluded from the analysis, similar pooled RR and significance were obtained (RR = 0.93, 95 % CI 0.90–0.98; p < 0.001) and heterogeneity was decreased (I 2 = 15.9 %; p = 0.242), indicating that our results were robust and reliable.
The strength of the present analysis lies in inclusion of 42 studies (31 observational studies and 11 RCTs) reporting data from more than 7.9 million participants, including 519,317 CRC cases. However, several limitations should be noted when interpreting our findings. First, observational studies, with their large, representative and ethnically diverse populations, have limitations, notably bias and unmeasured confounding. For the case–control studies, we cannot rule out the possibility of recall bias. However, in most of these studies, because pharmacy drug prescription information from population-based databases was used, the effects of this are likely minimal. Second, all studies did not adjust for the same confounders. They generally failed to account for one or more of the following risk factors for CRC: poor nutrition, physical inactivity, family history of colorectal cancer, inflammatory bowel disease, diabetes, use of nonsteroidal anti-inflammatory drugs, or check of colonoscopy. Third, the included studies were different in terms of definitions of drug exposure and long-term statin use, which could have led to heterogeneity. Fourth, colorectal cancer has never been a primary outcome in the included RCTs of statins; thus, most results of them were ambiguous because of inadequate power.
In conclusion, the findings of this meta-analysis of 42 studies suggest a modest decreased relative risk of CRC in statin users. This chemoprotective association is more pronounced in rectal cancer and lipophilic statin users. However, long-term statin use did not appear to significantly affect the risk of CRC.
References
Edwards BK, Ward E, Kohler BA et al (2010) Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116:544–573
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
O’Connell JB, Maggard MA, Ko CY (2004) Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst 96:1420–1425
Boghossian S, Hawash A (2012) Chemoprevention in colorectal cancer—where we stand and what we have learned from twenty year’s experience. Surgeon 10:43–52
Wong WWL, Dimitroulakos J, Minden MD, Penn LZ (2002) HMG-CoA reductase inhibitors and the malignant cell: the statin family of drugs as triggers of tumor-specific apoptosis. Leukemia 16:508–519
Guruswamy S, Rao CV (2008) Multi-target approaches in colon cancer chemoprevention based on systems biology of tumor cell-signaling. Gene Regul Syst Bio 2:163–176
Xiao H, Zhang Q, Lin Y, Reddy BS, Yang CS (2008) Combination of atorvastatin and celecoxib synergistically induces cell cycle arrest and apoptosis in colon cancer cells. Int J Cancer 122:2115–2124
Blais L, Desgagne A, LeLorier J (2000) 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors and the risk of cancer: a nested case-control study. Arch Intern Med 160:2363–2368
Graaf MR, Beiderbeck AB, Egberts AC, Richel DJ, Guchelaar HJ (2004) The risk of cancer in users of statins. J Clin Oncol 22:2388–2394
Kaye JA, Jick H (2004) Statin use and cancer risk in the general practice research database. Br J Cancer 90:635–637
Poynter JN, Gruber SB, Higgins PD et al (2005) Statins and the risk of colorectal cancer. N Engl J Med 352:2184–2192
Coogan PF, Smith J, Rosenberg L (2007) Statin use and risk of colorectal cancer. J Natl Cancer Inst 99:32–40
Hoffmeister M, Chang-Claude J, Brenner H (2007) Individual and joint use of statins and low-dose aspirin and risk of colorectal cancer: a population-based case-control study. Int J Cancer 121:1325–1330
Vinogradova Y, Hippisley-Cox J, Coupland C, Logan RF (2007) Risk of colorectal cancer in patients prescribed statins, nonsteroidal anti-inflammatory drugs, and cyclooxygenase-2 inhibitors: nested case-control study. Gastroenterology 133:393–402
Boudreau DM, Koehler E, Rulyak SJ, Haneuse S, Harrison R, Mandelson MT (2008) Cardiovascular medication use and risk for colorectal cancer. Cancer Epidemiol Biomarkers Prev 17:3076–3080
Yang YX, Hennessy S, Propert K, Hwang WT, Sarkar M, Lewis JD (2008) Chronic statin therapy and the risk of colorectal cancer. Pharmacoepidemiol Drug Saf 17:869–876
Hachem C, Morgan R, Johnson M, Kuebeler M, El-Serag H (2009) Statins and the risk of colorectal carcinoma: a nested case-control study in veterans with diabetes. Am J Gastroenterol 104:1241–1248
Shadman M, Newcomb PA, Hampton JM, Wernli KJ, Trentham-Dietz A (2009) Non-steroidal anti-inflammatory drugs and statins in relation to colorectal cancer risk. World J Gastroenterol 15:2336–2339
Robertson DJ, Riis AH, Friis S, Pedersen L, Baron JA, Sorensen HT (2010) Neither long-term statin use nor atherosclerotic disease is associated with risk of colorectal cancer. Clin Gastroenterol Hepatol 8:1056–1061
Cheng MH, Chiu HF, Ho SC, Tsai SS, Wu TN, Yang CY (2011) Statin use and the risk of colorectal cancer: a population-based case-control study. World J Gastroenterol 17:5197–5202
Samadder NJ, Mukherjee B, Huang SC et al (2011) Risk of colorectal cancer in self-reported inflammatory bowel disease and modification of risk by statin and NSAID use. Cancer 117:1640–1648
Vinogradova Y, Coupland C, Hippisley-Cox J (2011) Exposure to statins and risk of common cancers: a series of nested case-control studies. BMC Cancer 11:409
Broughton T, Sington J, Beales IL (2012) Statin use is associated with a reduced incidence of colorectal cancer: a colonoscopy-controlled case-control study. BMC Gastroenterol 12:36
Lakha F, Theodoratou E, Farrington SM et al (2012) Statin use and association with colorectal cancer survival and risk: case control study with prescription data linkage. BMC Cancer 12:487
Leung HW, Chan AL, Lo D, Leung JH, Chen HL (2013) Common cancer risk and statins: a population-based case-control study in a Chinese population. Expert Opin Drug Saf 12:19–27
Friis S, Poulsen AH, Johnsen SP et al (2005) Cancer risk among statin users: a population-based cohort study. Int J Cancer 114:643–647
Jacobs EJ, Rodriguez C, Brady KA, Connell CJ, Thun MJ, Calle EE (2006) Cholesterol-lowering drugs and colorectal cancer incidence in a large United States cohort. J Natl Cancer Inst 98:69–72
Setoguchi S, Glynn RJ, Avorn J, Mogun H, Schneeweiss S (2007) Statins and the risk of lung, breast, and colorectal cancer in the elderly. Circulation 115:27–33
Farwell WR, Scranton RE, Lawler EV et al (2008) The association between statins and cancer incidence in a veterans population. J Natl Cancer Inst 100:134–139
Flick ED, Habel LA, Chan KA et al (2009) Statin use and risk of colorectal cancer in a cohort of middle-aged men in the US: a prospective cohort study. Drugs 69:1445–1457
Singh H, Mahmud SM, Turner D, Xue L, Demers AA, Bernstein CN (2009) Long-term use of statins and risk of colorectal cancer: a population-based study. Am J Gastroenterol 104:3015–3023
Haukka J, Sankila R, Klaukka T et al (2010) Incidence of cancer and statin usage–record linkage study. Int J Cancer 126:279–284
Friedman GD, Flick ED, Udaltsova N, Chan J, Quesenberry CP Jr, Habel LA (2008) Screening statins for possible carcinogenic risk: up to 9 years of follow-up of 361,859 recipients. Pharmacoepidemiol Drug Saf 17:27–36
Hippisley-Cox J, Coupland C (2010) Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ 340:c2197
Jacobs EJ, Newton CC, Thun MJ, Gapstur SM (2011) Long-term use of cholesterol-lowering drugs and cancer incidence in a large United States cohort. Cancer Res 71:1763–1771
Lee JE, Baba Y, Ng K et al (2011) Statin use and colorectal cancer risk according to molecular subtypes in two large prospective cohort studies. Cancer Prev Res (Phila) 4:1808–1815
Simon MS, Rosenberg CA, Rodabough RJ et al (2012) Prospective analysis of association between use of statins or other lipid-lowering agents and colorectal cancer risk. Ann Epidemiol 22:17–27
Clancy Z, Keith SW, Rabinowitz C, Ceccarelli M, Gagne JJ, Maio V (2013) Statins and colorectal cancer risk: a longitudinal study. Cancer Causes Control 24:777–782
Shepherd J, Cobbe SM, Ford I et al (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med 333:1301–1307
Sacks FM, Pfeffer MA, Moye LA et al (1996) The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and recurrent events trial investigators. N Engl J Med 335:1001–1009
Downs JR, Clearfield M, Weis S et al (1998) Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 279:1615–1622
Group AOaCftACR (2002) Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT-LLT). JAMA 288:2998–3007
Group LS (2002) Long-term effectiveness and safety of pravastatin in 9014 patients with coronary heart disease and average cholesterol concentrations: the LIPID trial follow-up. Lancet 359:1379–1387
Heart Protection Study Collaborative G (2002) MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:7–22
Shepherd J, Blauw GJ, Murphy MB et al (2002) Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 360:1623–1630
Colhoun HM, Betteridge DJ, Durrington PN et al (2004) Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 364:685–696
Strandberg TE, Pyorala K, Cook TJ et al (2004) Mortality and incidence of cancer during 10-year follow-up of the Scandinavian Simvastatin Survival Study (4S). Lancet 364:771–777
Nakamura H, Arakawa K, Itakura H et al (2006) Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet 368:1155–1163
Ridker PM, Danielson E, Fonseca FA et al (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359:2195–2207
Kushiro T, Mizuno K, Nakaya N et al (2009) Pravastatin for cardiovascular event primary prevention in patients with mild-to-moderate hypertension in the Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese (MEGA) Study. Hypertension 53:135–141
Bulbulia R, Bowman L, Wallendszus K et al (2011) Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20 536 high-risk individuals: a randomised controlled trial. Lancet 378:2013–2020
Limburg PJ, Mahoney MR, Ziegler KL et al (2011) Randomized phase II trial of sulindac, atorvastatin, and prebiotic dietary fiber for colorectal cancer chemoprevention. Cancer Prev Res (Phila) 4:259–269
Matsushima T, Nakaya N, Mizuno K et al (2012) The effect of low-dose pravastatin in metabolic syndrome for primary prevention of cardiovascular disease in Japan: a post hoc analysis of the MEGA study. J Cardiovasc Pharmacol Ther 17:153–158
Bonovas S, Filioussi K, Flordellis CS, Sitaras NM (2007) Statins and the risk of colorectal cancer: a meta-analysis of 18 studies involving more than 1.5 million patients. J Clin Oncol 25:3462–3468
Bardou M, Barkun A, Martel M (2010) Effect of statin therapy on colorectal cancer. Gut 59:1572–1585
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Greenland S (1987) Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 9:1–30
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–748
Midgette AS, Wong JB, Beshansky JR, Porath A, Fleming C, Pauker SG (1994) Cost-effectiveness of streptokinase for acute myocardial infarction: a combined meta-analysis and decision analysis of the effects of infarct location and of likelihood of infarction. Med Decis Making 14:108–117
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Copas J, Shi JQ (2000) Meta-analysis, funnel plots and sensitivity analysis. Biostatistics 1:247–262
Galbraith RF (1988) A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 7:889–894
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Moorman PG, Hamilton RJ (2007) Statins and cancer risk—What do we know and where do we go from here? Epidemiology 18:194–196
Demierre MF, Higgins PD, Gruber SB, Hawk E, Lippman SM (2005) Statins and cancer prevention. Nat Rev Cancer 5:930–942
Undela K, Srikanth V, Bansal D (2012) Statin use and risk of breast cancer: a meta-analysis of observational studies. Breast Cancer Res Treat 135:261–269
Bansal D, Undela K, D’Cruz S, Schifano F (2012) Statin use and risk of prostate cancer: a meta-analysis of observational studies. PLoS ONE 7:e46691
Cui XB, Xie Y, Chen M et al (2012) Statin use and risk of pancreatic cancer: a meta-analysis. Cancer Causes Control 23:1099–1111
Singh S, Singh PP, Singh AG, Murad MH, Sanchez W (2013) Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology 144:323–332
Hamelin BA, Turgeon J (1998) Hydrophilicity/lipophilicity: relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. Trends Pharmacol Sci 19:26–37
Lipkin SM, Chao EC, Moreno V et al (2010) Genetic variation in 3-hydroxy-3-methylglutaryl CoA reductase modifies the chemopreventive activity of statins for colorectal cancer. Cancer Prev Res (Phila) 3:597–603
Ioannidis JP, Patsopoulos NA, Evangelou E (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335:914–916
Acknowledgments
None.
Conflict of interest
There are no potential conflicts of interest among any of the authors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Yanqiong Liu and Weizhong Tang have contributed equally to this study and should be considered as co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Y., Tang, W., Wang, J. et al. Association between statin use and colorectal cancer risk: a meta-analysis of 42 studies. Cancer Causes Control 25, 237–249 (2014). https://doi.org/10.1007/s10552-013-0326-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0326-6