Abstract
Objective
To examine if survival has changed over the last 20 years in patients with base of tongue and tonsil cancers in the United States.
Methods
Using SEER data, we employed Kaplan–Meier method to draw survival curves and calculate survival rates, and estimated adjusted hazard ratios (HR).
Results
From the 1980s to the 2000s, the 5-year overall survival rates statistically significantly improved by 100% from 25 to 51% among patients with one primary base of tongue cancer and 28–60% among those with one primary tonsil cancer (p values for trend <0.001). In addition, the 5-year cancer-specific survival improved by 222.4 and 276%, respectively, among two types of patients. Survival improvement was more pronounced among male patients than among female patients regardless of young or old age, while the improvement was generally consistent among patients with different tumor stages and treatment methods. In contrast, however, those patients with subsequent multiple cancers showed no improvement in overall survival over time.
Conclusions
The survival of patients with base of tongue and tonsil cancer has significantly improved over the last decades in the United States. Whether the improvement is associated with HPV infection, screening, or early detection is worthy to study in future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence rates of tongue and tonsil cancers have significantly increased in recent decades in the United States, particularly among younger patients [1–4]. The rising trends of these cancers are a contradiction to the stable or decreasing trends of other smoking-related oral and pharyngeal cancers. The cause for this increase has not been clearly established. It is controversial for the effect of early oral screening in the increases because the incidences of other oral cancers did not increase within the same period [2, 5]. Some investigators suspected that marijuana use might play a role for the increases [2], but the evidence of association is weak and has not yet been proved. Many studies have shown overwhelming evidence for a strong association between HPV infection and tongue and tonsil cancers [6–8]. In addition, HPV infection has also been substantially increasing in the US populations [9]. HPV has been found to be most strongly associated with base of tongue cancer and tonsil cancer, the reported patient infection rate being 45–100% [6, 10]. Most importantly, the prevalence of HPV infection was found to be increasing with time in populations [11] and in patients with base of tongue cancer [8]. Thus, HPV infection was considered as the responsible factor for the increasing incidence in tongue and tonsil cancer.
The survival of patients with base of tongue and tonsil cancers was previously very low: 5-year survival rate of 28–50% [3, 12, 13]. With an increased incidence of HPV-positive tumors and HPV infections, a change in survivability in these particular head and neck subsites would be anticipated. Clinically, HPV-positive oropharyngeal tumors were found to be very distinct from HPV-negative tumors, and patients with HPV-positive tumor were consistently demonstrated to have a better prognosis than those with HPV-negative tumor [10, 14–16]. In addition, patients with HPV-positive tumors had higher response rates (84%) after chemoradiation therapy, comparing to patients with HPV-negative tumors (57%), and their two-year overall survival rates were also higher (95% vs. 62%) [17]. However, studies examining survival change over time have been scarce. An Australian study reported that the 5-year survival rate of tongue cancer did not improve over the 24 years from 1977–1985 to 1986–1993 to 1994–2001 [18]. In addition, a US study indicated that the 2-year survival rate of base of tongue and tonsil cancers increased from 1973–1982 to 1983–1992 to 1993–2004 [19].
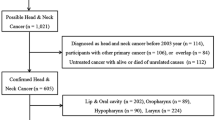
In this study, SEER data were used to examine the time trends of change of survival rate among patients with base of tongue, tonsil, and other tongue cancer in recent decades. To better observe the trend of survival, we separated patients into those with one primary cancer and those with subsequent multiple cancers, and then compared trend using three non-overlapped periods of 1980–1982, 1990–1992, and 2000–2002.
Patients and methods
Patient data and inclusions
Patient data from the SEER 1973–2006 registry system were used for analysis. The data was released on April 2009, based on the November 2008 submission [20].
Eligible patients were those aged 20 years or older and with squamous tongue and tonsil cancer, who were identified by the International Classification of Disease-Oncology (ICD-O) morphological and topography codes. The ICD morphological codes of squamous tumor were 8050 to 8090, and the ICD site codes of base of tongue cancer were C019, other tongue cancers C020 to C029, and tonsil cancer C090 to C099. We excluded lingual tonsil tumor (C024) from other tongue cancers since this tumor was considered to have the same etiological cause as base of tongue and tonsil cancers.
Eligible patients were also classified into two groups of one primary cancer and multiple cancers because patients with subsequent multiple cancers are complicated in etiology, and those with a cancer at other sites might have undergone more treatments and possibly affected in survival by other treatments. The one primary patient group included patients with only one primary base of tongue, tonsil, or other tongue cancer, while the multiple cancer patient group consisted of patients with subsequent primary cancers after an initial diagnosis of base of tongue, tonsil, or other tongue cancer, which excluded patients with base of tongue, tonsil, or other tongue cancer following a previous diagnosis of a cancer in any other part of the body.
Patient cohorts
To examine the time trend of survival, we used patients who were diagnosed in 1980–1982, 1990–1992, and 2000–2002. Three diagnostic periods were arbitrarily determined as the nature of SEER cancer registry data, and patients’ survivals during the time periods were assumed to represent the survivals of the 1980s, the 1990s, and the 2000s. The design of 3-year registry data for each period was done to obtain more patients for sub-group analyses. With the design, the possible mutual overlaps of survival curves, particularly those 5-year or 10-year curves, between two adjacent periods of time (a common problem when using cancer registry for survival rate trend analysis) were removed. For instance, the 1980–1982 patient cohort generated a maximum non-overlapped 8-year survival curve from 1980 to 1989, the 1990–1992 cohort from 1990 to 1999, and the 2000–2002 cohort from 2000 to 2009.
A total of 10,704 eligible patients were identified in all three time periods of the 1980s, the 1990s, and the 2000s as defined. Of them, 9,187 were those with one primary base of tongue, tonsil, or other tongue cancer, and 1,517 with subsequent multiple cancers after an initial diagnosis of base of tongue, tonsil, or other tongue cancer. Of 9,187 patients with one primary cancer, 2,619 were diagnosed with base of tongue cancer, 3,225 with tonsil cancer, and 3,343 with other sites of the tongue, while of 1,517 patients with subsequent multiple cancers, 450 were diagnosed with a previous diagnosis of base of tongue cancer, 514 with tonsil cancer, and 553 with other tongue cancer.
Statistical analysis
The Kaplan–Meier method was used to draw survival curves, and the statistical significance of difference of survival curves was tested by log-rank test. In the survival curve analysis, the overall survival of patients was defined. In addition, the 5-year overall survival rates were also calculated for the three periods of time, and the difference of trend of 5-year survival rate was tested by logistic regression model [21].
To control the influence of potential confounding factors, the time-dependent adjusted risks of mortality were estimated by the Cox proportional hazard model. Before model analysis, a data set containing covariates was initially established, which consisted of time periods (1980–1982, 1990–1992, and 2000–2002), age group (<60 and ≥60 years), gender (female and male), race (non-Hispanic white, Black, and other races), tumor grade (well differentiated, moderately differentiated, poorly differentiated, undifferentiated, and unknown), tumor stage (local, regional, distant, and unstaged), surgery (yes and no), radiation treatment (yes and no), follow-up time (months), and survival status (alive and dead). In the Cox model, the mortality rate of the 1980s was set as baseline for the comparison with the 1990s and the 2000s rates. The Cox model was run separately by subgroups. In the separate model, both univariate and multivariate-adjusted hazard mortality ratios and 95% confidence intervals (CI) were estimated, and the null hypothesis of no death risk difference for the three time periods was evaluated by the Wald Chi-Square test. A hazard mortality ratio less than one with a p value of less than 0.05 indicated a significantly improved survival in the 1990s or in the 2000s when compared to the baseline. In contrast, a ratio of larger than one conferred a worse survival in the later decades.
Results
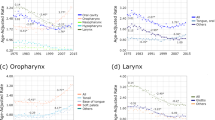
As shown in Fig. 1a–c, the 3-period survival curves differed significantly among patients with one primary cancer, regardless of the site being base of tongue, tonsil, or other tongue. The 5-year observed overall survival rates for the three time periods (1980–1982, 1990–1992, and 2000–2002) were 24.7, 29.9, and 50.5% for base of tongue cancer (p for trend <0.001), 28.2, 39.3, and 60.0% for tonsil cancer (p for trend <0.001), and 36.3, 44.6, and 52.4% for other tongue cancers (p for trend <0.001). From the 1980s to the 2000s, the 5-year observed survivals increased by 100% for both base of tongue and tonsil cancers, and 44% for other tongue cancer. The proportion of improvement of survival was noted to be greater between the 1990s and the 2000s than between the 1980s and the 1990s in both base of tongue cancer (68.9% in 1990s–2000s and 21.1% in 1980s–1990s) and tonsil cancer (52.7% vs. 39.4%). However, a similar trend was not observed in other tongue cancer, with the change between the decades being relatively equal. In contrast to patients with one primary cancer, the 3-period survival curves for those with multiple tumors in the base of tongue, tonsil, or other tongue sites were almost overlapped each other, and showed no improvement over time (Fig. 1d–f). More particularly, the survival of patients with multiple other tongue cancers reduced significantly between the 1980s and the 2000s (Fig. 1F, χ 2(2) = 11.58, p < 0.001). Our following analyses were focused on patients with one primary cancer because those with multiple cancers did not show significant survival difference over time.
Survival curves for patients with base of tongue, tonsil, and other tongue cancer during the periods of the 1980s, the 1990s, and the 2000s by whether patients had subsequent multiple cancers. The numbers on the right of the vertical dot line are the 5-year observed overall survival rate and 95% confidence interval
As shown in Fig. 2, from the 1980s to the 2000s, the 5-year cancer-specific survival increased by 222.4% (17.4% vs. 56.1%) for base of tongue, 292.3% (16.8% vs. 65.9%) for tonsil cancer, and 95.0% (29.9% vs. 58.3%) for other tongue cancer. In contrast, the increased magnitude of 5-year noncancer-specific survival was relatively small, which was 61.4% (51.5% vs. 83.1%) for base of tongue cancer, 46.9% (59.1% vs. 86.8%) for tonsil cancer, and 39.1% (60.1% vs. 83.6) for other tongue cancer.
Survival curves for patients with one primary base of tongue, tonsil, or other tongue cancer during the periods of the 1980s, the 1990s, and the 2000s by cancer-specific and noncancer-specific survivals. The numbers on the right of the vertical dot line are the 5-year observed overall survival rate and 95% confidence interval
To efficiently conduct subgroups analysis, we also combined patients with base of tongue and tonsil cancers together. Combining the two for further analysis is reasonable since these two tumors exhibit the similarity in survival curves and the same high rate of HPV-positivity. Figure 3 shows the overall survivals for the combined data of base of tongue and tonsil cancers according to gender and age. From the 1980s to the 2000s, the 5-year overall survival increased by 71.3% (p for trend <0.001) and 27% (p for trend =0.03) in the age groups of 20–59 years and 60 years or older among female patients. In contrast, the 5-year overall survival increased by 152.1% (p for trend <0.001) and 101.0% (p for trend <0.001) in the two age groups among male patients.
Figure 4 shows the time-dependent survival curves for the combined data of base of tongue and tonsil cancers according to tumor stage. From the 1980s to the 2000s, the survivals of base of tongue and tonsil cancers were found to improve significantly (p < 0.01), regardless of local, regional, distant, or unstaged tumor status. However, the largest improved proportion was found in regional stage tumor (125.8%), and the least in local stage tumor (52.7%).
The survival curves of the three time periods for the combined data were also examined according to treatment types (Fig. 5). As expected, survival curves were also significantly different for each type of treatment (p < 0.001), except for those who refused treatment, whose survival curves were not significantly different but 5-year observed survival rates were significantly different.
As indicated in Table 1, the time-dependent changes of patient characteristics were generally consistent among two types of patients of one primary base of tongue and tonsil cancer. Younger, male, or white patients were pronounced more in the 2000s than in the 1980s. In addition, more patients were diagnosed with poorly differentiated tumor grade and regional stage tumor, and undergone with both surgery and radiation treatments in the 2000s than in the 1980s. Compared with the 1980s, the proportion of death reduced by 38.8 and 48.2% for base of tongue cancer and tonsil cancer in the 2000s.
Compared to the 1980s, the 5-year mortality risk during the 1990s fell 12% for both base of tongue and tonsil cancers after adjusting for the effects of age, gender, race, tumor grade, tumor stage, and treatment modality (Table 2). The risk of mortality during the 2000s decreased approximately 40% for base of tongue cancer (adjusted HR = 0.59, 95% confidence interval =0.5–0.7, p < 0.001) and tonsil cancer (adjusted HR = 0.60, 0.5–0.7, p < 0.001).
The 5-year mortality risks of the three periods were also compared for the combined data of base of tongue and tonsil cancer according to tumor stage, age, and treatment method (Table 3). This subgroup analysis was focused only on patients with regional stage tumor because the numbers of patients with local and distant stage tumors were too small to analyze. From the 1980s to the 2000s, the mortality risks for surgery alone, radiotherapy alone, and combined surgery and radiation therapy were found to reduce by 77% (adjusted HR = 0.23, 0.1–0.5, p < 0.001), 63% (adjusted HR = 0.37, 0.3–0.5, p < 0.001), and 62% (adjusted HR = 0.38, 0.3–0.5, p < 0.001) among younger patients of <60 years. However, the reductions over time for older patients ≥60 years with the three different treatment modalities were relatively small: 27% (adjusted HR = 0.73, 0.4–1.3, p = 0.312), 23% (adjusted HR = 0.77, 0.6–1.0, p = 0.042), and 40% (adjusted HR = 0.6, 0.4–0.8, p = 0.003), respectively.
Discussion
Our study demonstrated a significantly improved survival trend over the past decades for patients with one primary squamous cell cancer of the base of tongue, tonsil, and other tongue sites in the United States. The improvement of 5-year survival from the 1980s to the 2000s was found to be larger among patients with one primary base of tongue or tonsil cancer than among those with other tongue cancer (100% vs. 44%). In addition, the improvement was also pronounced more between the 1990s and the 2000s than between the 1980s and the 1990s, cancer-specific survival than noncancer-specific survival, among younger patients of <60 years, among male patients, and in regional stage tumors (versus local or distant stage tumors). Overall, the improvement of survival was relatively similar between patients who received surgery alone or those who underwent radiation therapy as their sole treatment modality.
The large improvement in survival for base of tongue and tonsil cancers has been unique when compared to the relative stable survival trends in other smoking-related cancers including cancers of the oral cavity [22], glottis [23, 24], and lung [25]. The divergence of trend of survival between HPV-related base of tongue and tonsil cancers and tobacco and alcohol related lip and oral cancers may indicate that the gradually decreased smoking rate since the mid-1960s [26, 27] did not play a role in the improving survival trends of base of tongue and tonsil cancers. To further analyze the relationship between the effects of HPV and tobacco and alcohol, we also estimated the 5-year cumulative mortality risks of the three periods for patients with cancers of the lip, floor of mouth, and gum and other mouth sites (Table 4). The results indicated that the mortality risk of lip or floor of mouth cancer decreased 18%, while that of gum and other mouth site 8% between the 1980s and the 2000s. The decreased proportions of these three tobacco and alcohol-related cancers were far lower than that of base of tongue and tonsil cancers, whose proportions decreased 40% during the same period (Table 2). It may indicate a possibility that HPV infection did not substantially affect lip and oral cavity tumors because both organs are not close to lymphoid tissue unlike the base of tongue and tonsil. On the other hand, it may also indicate a possibility that a downward trend of overall incidence of smoking-related tumors in the United States has slightly improved the survival of lip and oral cavity cancers.
A possibility for the improved survival trends is the effects of early oral screening and early diagnosis and early treatment of oral cancer. Many studies have attempted to assess the effectiveness of oral cancer screening in decreasing the morality of oral cancer. However, a recent review reported that more evidence needed to find out whether screening programs are effective in reducing the mortality of oral cancer [28]. In the United States, a national preventive service task force in 1996 recommended a careful screening for oral cancer for asymptomatic patients with a history of tobacco or alcohol use [29]. In our results, the improvements of survival of base of tongue and tonsil cancers were larger between the 2000s and the 1990s than between the 1990s and the 1980s. Therefore, whether the larger survival improvement of the 2000s partially reflects the effect of the recommendation is worthy to speculate. A UK study showed that the probability of visiting a dentist regularly was low in those at greatest risk of oral cancer and this was most striking in the case of smoking [30]. It is more plausible that cancers of the tongue and tonsil may be diagnosed easier and earlier during oral screening, thus increasing the survival of these two cancers to certain degree.
Another possibility is the influence of change of some treatment methods, particularly hyperfractionated radiotherapy [31–35] and concurrent chemotherapy [36, 37]. As noted by previous study, however, the substantial 5-year survival benefit was quite small for oral cavity cancer, only about 3 and 8%, if comparing hyperfractionated to conventional radiotherapy [19]. Such a small treatment benefit is apparently not proportional to the actual 80–100% survival improvement in base of tongue and tonsil cancers, as observed in our study. Furthermore, our result did not support the influence of change of radiation methods as well. For instance, patients with surgery alone who did not have radiotherapy also had the same improved survival trend as seen in those with radiotherapy alone. As to the effect of chemotherapy on survival trends, we could not evaluate it directly because SEER data do not provide information on chemotherapy to the public. However, we estimated that the effect of chemotherapy might be also unimportant for the significantly increased survival trend according to the reported small benefit for head and neck cancers [38].
The similar improved survival trends in surgical and radiation treatments may indicate a possibility of influence of other non-treatment factors. A particularly possible non-treatment factor is the influence of HPV infection. In our result, the improvement of survival was found to be larger in young patients than in old patients, particularly in those with regional stage tumor, which was consistent to the significant increase of incidence rate in young population in recent years [2, 3, 19]. Because of the strong association between HPV infection and base of tongue and tonsil cancers and having no clues or evidence from other factors, the effect of HPV infection on the improved survivals of both cancers is quite likely.
We noted that the improvement of survival was pronounced greater among patients with base of tongue or tonsil cancer than those with other tongue cancer (100% vs. 44%). The result seemed to be consistent with the higher frequency of HPV infection in the base of tongue and the tonsil sites than in the other tongue sites. It is unclear why HPV preferentially infects the base of the tongue and the tonsil. Perhaps it is related with the nature of the epithelium of the base of tongue and the tonsil and the infection is close to lymphoid tissue.
We classified patients as two types of single primary cancer and multiple cancers because we thought that patients with multiple cancers were complicated in etiology or in treatment. It is quite possible that patients with a cancer at other sites might have undergone more cancer treatments, and they were also more difficult to be treated than those with single primary cancer. Our results proved the necessity for distinguishing one primary cancer from multiple cancers, in which multiple cancer survival did not improve with time, and conversely it decreased in other tongue cancers excluding base of tongue cancer.
In the study, we used an equal 7-year observed time to describe survival curve for each period of 1980–1982, 1990–1992, and 2000–2002. The 7-year time frame is the length of time that patients were followed up for mortality events. The methodological consideration is necessary for survival trend analysis in the use of cancer registry patients, for whom follow-up time varies. For instance, the 1980s data contains 27 follow-up years from 1980 to 2006, the 1990s 17 years from 1990 to 2006, and the 2000s 7 years from 2000 to 2006. Our limitation to 7-year observational time helped to accurately observe 5-year survival because of a time lag between cancer diagnosis and reporting in SEER data.
Our study did not specifically list results on patients with lingual tonsil (C024) because the numbers of patients were very small in SEER data, only 6 patients in the 1980s, 7 in the 1990s, and 42 in the 2000s. Although the number of patients with lingual tonsil was small, the survival of patients with this cancer also tended to improve with time, whose 5-year survival rate was 54% in the 1980s and 79% in the 2000s.
In conclusion, survival has significantly improved from the 1980s to the 2000s among patients with base of tongue or tonsil cancer as well as among patients with other tongue cancer. The reason of the improvement has not been well understood. Because of the reported strong association of HPV infection with base of tongue and tonsil cancers in incidence and in prognosis, we suspect that the time-dependent improvement may be related with increased HPV infection among patients. In addition, screening or early detection may also contribute to the partial effect of the elevated survival. Our results of significantly improved survival provide important clinical implication for treating base of tongue and tonsil cancer, and possible HPV infection mechanism will help to study other cancer survivals.
References
Ryerson AB, Peters ES, Coughlin SS et al (2008) Burden of potentially human papillomavirus-associated cancers of the oropharynx and oral cavity in the US, 1998–2003. Cancer 113:2901–2909
Schantz SP, Yu GP (2002) Head and neck cancer incidence trends in young Americans, 1973–1997, with a special analysis for tongue cancer. Arch Otolaryngol Head Neck Surg 128:268–274
Shiboski CH, Schmidt BL, Jordan RC (2005) Tongue and tonsil carcinoma: increasing trends in the US population ages 20–44 years. Cancer 103:1843–1849
Frisch M, Hjalgrim H, Jaeger AB, Biggar RJ (2000) Changing patterns of tonsillar squamous cell carcinoma in the United States. Cancer Causes Control 11:489–495
Kingsley K, O’Malley S, Ditmyer M, Chino M (2008) Analysis of oral cancer epidemiology in the US reveals state-specific trends: implications for oral cancer prevention. BMC Public Health 8:87
Mellin H, Friesland S, Lewensohn R, Dalianis T, Munck-Wikland E (2000) Human papillomavirus (HPV) DNA in tonsillar cancer: clinical correlates, risk of relapse, and survival. Int J Cancer 89:300–304
Kreimer AR, Clifford GM, Boyle P, Franceschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomark Prev 14:467–475
Attner P, Du J, Nasman A et al (2010) The role of human papillomavirus in the increased incidence of base of tongue cancer. Int J Cancer 126:2879–2884
Dunne EF, Unger ER, Sternberg M et al (2007) Prevalence of HPV infection among females in the United States. JAMA 297:813–819
Dahlgren L, Dahlstrand HM, Lindquist D et al (2004) Human papillomavirus is more common in base of tongue than in mobile tongue cancer and is a favorable prognostic factor in base of tongue cancer patients. Int J Cancer 112:1015–1019
af Geijersstam V, Wang Z, Lewensohn-Fuchs I et al (1998) Trends in seroprevalence of human papillomavirus type 16 among pregnant women in Stockholm, Sweden, during 1969–1989. Int J Cancer 76:341–344
Zhen W, Karnell LH, Hoffman HT et al (2004) The National Cancer Data Base report on squamous cell carcinoma of the base of tongue. Head Neck 26:660–674
Brunin F, Mosseri V, Jaulerry C et al (1999) Cancer of the base of the tongue: past and future. Head Neck 21:751–759
Ritchie JM, Smith EM, Summersgill KF et al (2003) Human papillomavirus infection as a prognostic factor in carcinomas of the oral cavity and oropharynx. Int J Cancer 104:336–344
Schwartz SR, Yueh B, McDougall JK, Daling JR, Schwartz SM (2001) Human papillomavirus infection and survival in oral squamous cell cancer: a population-based study. Otolaryngol Head Neck Surg 125:1–9
Ang KK, Harris J, Wheeler R et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363:24–35
Fakhry C, Westra WH, Li S et al (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100:261–269
Lam L, Logan RM, Luke C (2006) Epidemiological analysis of tongue cancer in South Australia for the 24-year period, 1977–2001. Aust Dent J 51:16–22
Chaturvedi AK, Engels EA, Anderson WF, Gillison ML (2008) Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol 26:612–619
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: incidence—SEER 17 Regs limited-use + Hurricane Katrina Impacted Louisiana Cases, Nov 2008 Sub (1973–2006 varying), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2009, based on the November 2008 submission
Spiegelman D, Hertzmark E (2005) Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol 162:199–200
Shiboski CH, Shiboski SC, Silverman S Jr (2000) Trends in oral cancer rates in the United States, 1973–1996. Community Dent Oral Epidemiol 28:249–256
Cosetti M, Yu GP, Schantz SP (2008) Five-year survival rates and time trends of laryngeal cancer in the US population. Arch Otolaryngol Head Neck Surg 134:370–379
Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP (2005) Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer 114:806–816
Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W et al (eds) (2010) SEER cancer statistics review, 1975–2007, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER web site, 2010
US Department of Health and Human Services (1994) Preventing tobacco use among young people: a report of the surgeon general. US Dept of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking on Health, Atlanta
Centers for Disease Control and Prevention (CDC) (2002) Cigarette smoking among adults—United States, 2000. MMWR Morb Mortal Wkly Rep 51:642–645
Kujan O, Glenny AM, Duxbury J, Thakker N, Sloan P (2005) Evaluation of screening strategies for improving oral cancer mortality: a Cochrane systematic review. J Dent Educ 69:255–265
Cruz GD, Ostroff JS, Kumar JV, and Gajendra S (2005) Preventing and detecting oral cancer. Oral health care providers’ readiness to provide health behavior counseling and oral cancer examinations. J Am Dent Assoc 136:594–601. (quiz 681–682)
Netuveli G, Sheiham A, Watt RG (2006) Does the ‘inverse screening law’ apply to oral cancer screening and regular dental check-ups? J Med Screen 13:47–50
Pinto LH, Canary PC, Araujo CM, Bacelar SC, Souhami L (1991) Prospective randomized trial comparing hyperfractionated versus conventional radiotherapy in stages III and IV oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys 21:557–562
Horiot JC, Le Fur R, N’Guyen T et al (1992) Hyperfractionation versus conventional fractionation in oropharyngeal carcinoma: final analysis of a randomized trial of the EORTC cooperative group of radiotherapy. Radiother Oncol 25:231–241
Harrison LB, Lee HJ, Pfister DG et al (1998) Long term results of primary radiotherapy with/without neck dissection for squamous cell cancer of the base of tongue. Head Neck 20:668–673
Mendenhall WM, Stringer SP, Amdur RJ et al (2000) Is radiation therapy a preferred alternative to surgery for squamous cell carcinoma of the base of tongue? J Clin Oncol 18:35–42
Bourhis J, Le Maitre A, Baujat B, Audry H, Pignon JP (2007) Individual patients’ data meta-analyses in head and neck cancer. Curr Opin Oncol 19:188–194
Pignon JP, Bourhis J, Domenge C, Designe L (2000) Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-analysis of chemotherapy on head and neck cancer. Lancet 355:949–955
Pignon JP, le Maitre A, Bourhis J (2007) Meta-Analyses of Chemotherapy in Head and Neck Cancer (MACH-NC): an update. Int J Radiat Oncol Biol Phys 69:S112–S114
Budach W, Hehr T, Budach V, Belka C, Dietz K (2006) A meta-analysis of hyperfractionated and accelerated radiotherapy and combined chemotherapy and radiotherapy regimens in unresected locally advanced squamous cell carcinoma of the head and neck. BMC Cancer 6:28
Acknowledgments
Drs. Yu and Schantz had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Yu and Schantz developed study concept and design, interpreted analytic results, and drafted the manuscript. Drs. Zhang and Hashibe criticized and revised the manuscript for important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, GP., Mehta, V., Branovan, D. et al. Improved survival among patients with base of tongue and tonsil cancer in the United States. Cancer Causes Control 23, 153–164 (2012). https://doi.org/10.1007/s10552-011-9864-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-011-9864-y