Abstract
Background
Patients with head and neck squamous cell carcinoma (HNSCC) are at significantly elevated risk of second primary malignancies (SPM), most commonly within the head and neck, lung, and esophagus (HNLE). Our objectives were to quantify the excess risk of SPM across all anatomic sites in which SPM risk is meaningfully elevated, including non-HNLE sites, in a large cohort of US patients.
Methods
Population-based analysis of 75,087 patients with HNSCC in the SEER program, quantifying excess SPM risk by integrating relative (standardized incidence ratio; SIR) and absolute (excess absolute risk per 10,000 person-years at risk; EAR) statistics.
Results
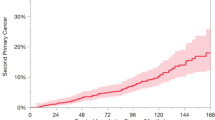
In HNSCC patients, the SIR of a second primary solid cancer was 2.2 (95% CI 2.1–2.2), corresponding to EAR of 167.7 additional cases per 10,000 person-years at risk. Over 1 year, 60 patients would need to be followed to observe one excess SPM. Lung cancer burden was most markedly elevated in absolute terms (EAR = 75.2), followed by HN (EAR = 59.8), esophageal (EAR = 14.2), and colorectal (EAR = 4.3) cancers. Lesser but significant excess risks were also observed for cancers of the bladder, liver, stomach, pancreas, kidney, salivary glands, nasopharynx, uterine cervix, and lymphoma.
Conclusions
Data from a large population-based US cohort reveals that HNSCC patients experience markedly excess risk of SPM, predominantly in the HNLE sites. Furthermore, the risk of SPM is also meaningfully elevated, although to a lesser degree, in multiple other tobacco-associated sites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The elevated risk of second primary malignancy (SPM) in patients with head and neck squamous cell carcinoma (HNSCC) is well established. The incidence of SPM in this population has been estimated at 2–6% per year [1–4]. Recent pooled international epidemiologic analyses have reported a cumulative SPM incidence of 36% at 20 years among patients with HNSCC [5]. Despite the advances in locoregional control achieved with modern surgery and chemoradiation, survival with HNSCC has not meaningfully improved, in part due to the continuing risk of development of SPMs in these patients. SPMs represent the leading long-term cause of mortality in head and neck cancer patients [6]. Approximately one-third of HNSCC deaths are attributable to SPMs [2, 3], triple the number of deaths due to distant metastases [7].
SPMs arising in the upper aerodigestive tract after HNSCC illustrate concepts of “field cancerization,” first proposed by Slaughter in 1953, in which environmental carcinogens such as tobacco and alcohol may induce a field of mucosa afflicted with premalignant disease, and are believed to elevate epithelial cancer risk throughout the head and neck, lungs, and esophagus [8, 9]. More generally, SPMs also provide useful information regarding common etiologies and epidemiological trends [10, 11].
The canonical sites of elevated SPM risk after an index HNSCC are the head and neck, lung, and esophagus (HNLE sites) [2–5, 8, 10, 12–18]. More recent epidemiologic data support a weaker association with SPMs of the cervix and anogenital region, likely related to oncogenic human papillomavirus (HPV) [5, 19]. Investigators in the 13-cis-retinoic acid chemoprevention trial also observed a notable incidence of SPM in the bladder, another tobacco-related site, although an elevated risk of bladder cancer after HNSCC has not been demonstrated [20, 21]. Other sites with elevated SPM risk attributable to HNSCC have not been defined. A recent pooled analysis of international cancer registry data suggested that several other non-HNLE sites associated with tobacco or alcohol exposure may carry elevated SPM risk, although individual risk data for specific anatomic sites were not analyzed [5].
To date, SPM risk after HNSCC has not been analyzed in a large population-based cohort in the United States, and the excess risk of SPM in contemporary US patients has not been comprehensively described. Also, it remains unknown whether there are non-HNLE anatomic sites at elevated risk of SPM in HNSCC patients. The objectives of our study were to describe SPM excess risk in a US cancer registry and to identify anatomic sites (beyond HNLE) in which SPM risk is meaningfully elevated following an index HNSCC.
Methods
Cases in the SEER program
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program is considered the gold standard cancer registry, having collected data continuously since 1973 and now capturing 26% of the United States population. Cancer incidence registries are population-based data sets, facilitating epidemiologic analysis of the incidence of second primary malignancy. All cancers, primary and subsequent, occurring among residents of the defined geographic registries comprising the SEER program are reportable. Near-universal follow-up is achieved by actively tracing all patients. However, second cancers developing in patients who migrate out of a SEER registry may not be reliably captured. An additional limitation of national cancer incidence registries, including SEER, is lack of information on risk factors such as tobacco use, alcohol use, or human papillomavirus status. Quality control is an integral part of the SEER program, and comparison studies have confirmed that pathologic, surgical, and radiation data are accurately recorded [22, 23]. The National Cancer Institute does not require institutional board approval for use of this deidentified data set.
The population for this study was drawn from the nine original SEER registries, comprising the states of Connecticut, Iowa, New Mexico, Utah and Hawaii, and the metropolitan areas of Detroit, San Francisco-Oakland, Seattle, and Atlanta. These geographic areas have been reported to represent a cross-section of the United States population with respect to race, ethnicity, income, and educational level. Patients included in the SEER program between 1975 and 2006 were included, extending follow-up for SPM to up to 31 years.
All patients with an index invasive squamous cell carcinoma (International Classification of Diseases for Oncology, 3rd edition [24] (ICD-O-3) histology codes 8070-8076, 8078) arising from subsites of the head and neck (oral cavity, oropharynx, larynx, and hypopharynx) were included. The oral cavity included ICD-O-3 codes corresponding to the upper and lower lip mucosa, oral tongue, upper and lower gums, floor of mouth, hard palate, and buccal mucosa. Oropharynx included the base of tongue, tonsils, soft palate, uvula, and posterior pharyngeal wall. Larynx included the supraglottis, glottis, and subglottis. Hypopharynx included the pyriform sinuses, postcricoid region, and posterior hypopharyngeal wall.
Definition of SPM risk
A second primary malignancy was defined as a subsequent invasive cancer developing after an index HNSCC. Multiple cancers within any of 194 anatomic sites were coded as SPMs only if several requirements were met, in accordance with Warren and Gates criteria [25] as modified by the National Cancer Institute [26]. We included only metachronous cancers, defined as those diagnosed at least six months after index HNSCC diagnosis. If the second cancer was of non-squamous cell origin, or developed in a different location (as defined by a different first or second digit in the ICD-O-3 topography code), it was coded as an SPM. If the second cancer was both SCC and developed in the same region as the index cancer, it was only coded as an SPM if more than 60 months had passed since the index diagnosis. If the primary medical records defined the second cancer as either recurrent or metastatic, it was not included. These criteria are intended to be conservative and to minimize classification of recurrences as SPMs. However, rare cases may be misclassified, as in clinical practice; for example, recurrences occurring at the margin of a prior treated cancer, but in a separate topographic subsite, may be coded as SPMs. Lung metastases may be misclassified as second primary lung cancers, or vice versa.
Crude incidence of SPM was calculated in order to allow comparison with prior studies [6, 21]. However, the crude incidence of SPM is not completely informative, as it simply reflects the number of cancers developing in the cohort, not the excess risk of cancer due to the index HNSCC. Therefore, the risk of SPM was defined as the standardized incidence ratio (SIR), first described by Schoenberg and Myers [27] and adapted to SEER registry analysis by Begg [28]. SIR is the ratio of observed to expected (O/E) second cancers, where the number of cancers expected is calculated for a reference SEER cohort of identical age, gender, race, and time period.
The excess absolute risk (EAR) represents the absolute number of additional second cancers attributable to the index HNSCC. EAR is calculated as the excess (observed—expected) number of second cancers in patients with an index HNSCC diagnosis, per 10,000 person-years at risk (PYR) [26]. Patients are actively followed in SEER and remain “at risk” until dying or lost to follow-up, so that multiple cancers (second, third, and subsequent cancers) are counted as they arise. For example, a patient with HNSCC who develops a second primary tumor in the lung and a third primary tumor in the esophagus would contribute to excess risk for each site.
Both SIR and EAR account for the number of patients at risk, as patients are lost to follow-up or die. While SIR is a relative measure of the strength of association between two cancers, EAR is an absolute measure of the clinical burden of additional cancer cases in a given population. The number needed to follow (NNF) is calculated as 10,000/EAR and represents the number of patients who would need to be followed for one year, assuming constant risk, in order to observe one additional case of SPM beyond the expected number of SPMs.
Statistical methods
Standardized incidence ratios were calculated using the formula above and 95% confidence intervals using Byar’s approximation to the Poisson distribution [29]. The SIR was considered significantly elevated if the 95% confidence intervals excluded 1.0.
To identify the most clinically meaningful anatomic sites of SPM, both relative and absolute statistics are needed. A common site for second cancers, such as the breast or prostate, may not be at elevated risk due to the index HNSCC. Conversely, the risk of a certain second cancer may be significantly associated with HNSCC, but be of such low prevalence such that it is clinically unimportant, e.g., anogenital squamous cell carcinoma [19].
Therefore, an integrative approach was used to identify clinically meaningful SPMs associated with HNSCC. First, four sites with prior epidemiologic evidence supporting elevated risk after HNSCC were included: head and neck, lung, esophagus, and uterine cervix [5]. Then, the remaining anatomic sites were screened for sites with SIR significantly greater than 1.0 and EAR greater than 1.0 per 10,000 PYR. The EAR threshold was chosen to correspond approximately to a minimum of one excess case observed in 1,000 patients followed for a decade. A list of clinically meaningful SPMs was constructed for each HNSCC subsite and NNF calculated for each.
All SIR and EAR values were calculated in SEER*Stat release 6.5.2 (July 2009; NCI Cancer Statistics Branch, Bethesda, MD). Additional statistical analyses were performed using SAS 9.2 (March 2008; SAS Institute, Cary, NC).
Results
A total of 75,087 cases of HNSCC were identified in the SEER registry between 1975 and 2006. Patient and tumor characteristics are summarized in Table 1. Median follow-up time for HNSCC cases was 69.1 months, and 1,140 patients (1.5%) were lost to follow-up. Median age was 63.4 years.
The crude non-actuarial incidence of second primary malignancy (SPM) was then calculated. Among patients with an index diagnosis of HNSCC, 23.2% developed one or more multiple primary cancers: 19.6% developed one subsequent cancer, 2.8% developed 2 subsequent cancers, and 0.8% developed 3 or more subsequent cancers. The incidence and location of common SPMs are detailed in Table 2. The most common location of SPM was the lung (33.0% of SPMs), followed by the head and neck (22.6% of SPMs).
Crude SPM incidence data do not adjust for the expected number of second cancers in a reference population and do not adjust for the number of patients at risk. Therefore, the standardized incidence ratio (SIR) and excess absolute risk (EAR) of SPM were calculated. The landscape of relative and absolute SPM risk profiles across 194 anatomic sites is depicted in Fig. 1, which plots the SIR of each subsequent cancer site against the number of expected cases in the HNSCC cohort of 75,087 patients. The most meaningful SPM sites as determined by SIR > 1.0 and EAR > 1.0 are displayed in Fig. 2.
Scatterplot of the risk of SPM across 194 anatomic sites, with standardized incidence ratio (SIR) plotted against the expected number of cases in the cohort of 75,087 HNSCC cases. Cancers in anatomic sites above the curvilinear line had SIR > 1.0 and EAR > 1.0 per 10,000 person-years at risk. Cancers in sites below the line either did not have significantly elevated SIR or were of such low prevalence that elevated SIR did not translate to >1.0 excess cases per 10,000 PYR
Detailed information according to the subsite of the index HNSCC is provided in Table 3. Among patients with an index HNSCC, 16,605s primary solid cancers were observed over 535,469 person-years at risk. The expected value in a reference cohort was 7,617. Therefore, the SIR of a second primary solid tumor was 2.2 (95% CI 2.1–2.2), corresponding to 167.7 excess second solid cancers per 10,000 person-years at risk. The majority (89.0%) of the total excess number of second cancers was attributable to excess second cancers arising in the HNLE sites.
The highest relative risk of SPM was observed for second head and neck cancers, with a standardized incidence ratio of 12.4 (95% CI 12.0–12.7). The next highest SIR was for second primary esophageal cancer, with an SIR of 8.4 (95% CI 7.9–8.9), followed by lung cancer, with an SIR of 3.8 (95% CI 3.7–3.9). The excess burden of disease, as measured by EAR, was highest for lung (75.2 excess cases per 10,000 PYR), followed by head and neck (59.8 excess cases per 10,000 PYR), and then esophagus (14.2 excess cases per 10,000 PYR).
The SPM site with the 4th highest number of excess cases, after the HNLE sites, was colorectal cancer. Although the elevation in relative risk was modest compared to HNLE sites [SIR = 1.2 (95% CI 1.1–1.3)], the background prevalence of colorectal cancer in the United States is high, leading to 4.3 excess colorectal cancer cases per 10,000 PYR. Other anatomic sites with meaningfully elevated risk of SPM among all patients with HNSCC included the bladder, liver, stomach, salivary glands, and lymphoma.
While the SIR for cancer of the uterine cervix was significantly elevated at 1.7 (95% CI 1.2–2.4), this elevated relative risk in the context of a low background prevalence of cervical cancer translated to only 0.25 excess cases per 10,000 PYR, which failed to reach the threshold for a clinically meaningful SPM. Cervical cancer was most significantly associated with primary HNSCC of the oropharynx [SIR = 2.8 (95% CI 1.3–5.3)], but because of the low prevalence of cervical cancer, the burden of excess cases remained low (0.5 excess cases per 10,000 PYR).
Excess risk of a second solid cancer was elevated in both women (SIR = 2.9, 95% CI 2.8–3.0; EAR = 188.4) and men (SIR = 2.0, 95% CI 2.0–2.1; EAR = 163.4). Further context for EAR values is provided by the number needed to follow (NNF), representing the number of patients who would need to followed for one year in order to observe one additional SPM at that site. These values are detailed in Table 4 for the same list of SPM sites. Among SPM sites with meaningful elevation in risk, the NNF values range widely. Among all HNSCC patients, one additional second solid tumor was identified for every 60 patients followed for one year. One additional lung cancer was identified for every 133 patients, one additional head and neck cancer for every 167 patients, and one additional esophageal cancer for every 702 patients followed for one year. For colorectal cancer, the figure was 2,315; for cervical cancer, the figure was 40,000.
Discussion
In this population-based cohort study, we comprehensively describe excess risks of second primary malignancy after an index head and neck cancer using both relative and absolute statistics. We also report novel associations between HNSCC and the occurrence of subsequent cancers across numerous anatomic sites. To our knowledge, this is the first large-scale population-based analysis of SPM risk profiles in US patients, and the only systematic analysis of excess risk of SPM arising in sites other than the canonical sites (head and neck, lung, and esophagus). The burden of SPM is high in HNSCC patients in the United States, with 168 excess second solid tumors developing per 10,000 person-years at risk. HNLE sites accounted for 89% of SPMs, with lung cancer accounting for the largest proportion of excess second cancer burden. This is in contrast to the traditional belief that second head and neck cancers are the most common SPMs in patients with an index HNSCC [18]. SPM risk was higher in female patients, consistent with the higher prevalence of ever-smoking in women developing HNSCC [30].
After the HNLE sites, the next SPM at elevated risk was colorectal cancer. Meaningfully elevated but lower risks of SPM were identified in several other sites (bladder, liver, stomach, salivary glands, and lymphoma). The breast and prostate were common sites of SPM, but the risk of each cancer was not elevated above the expected number of these cancers in a comparable reference population. In this analysis, we report that colorectal cancer represents the fourth most common second primary cancer associated with HNSCC, after the HNLE sites. While the elevation in risk was modest (SIR = 1.2) compared to HNLE second cancers, a 20% excess risk in a more highly prevalent cancer was able to translate to a meaningful number of additional cancer cases.
Colorectal cancer risk has only recently been definitively linked to tobacco exposure in a large prospective study by the American Cancer Society [31] and has now been added to the International Agency for Research on Cancer list of tobacco-related cancers [32]. Other IARC-designated tobacco-associated cancers that were also identified as elevated SPM risk in this study were cancers of the nasopharynx, stomach, liver, pancreas, kidney, and bladder, although absolute risk numbers for each of these sites were lower than for HNLE and colorectal cancers. The risk of subsequent lymphoma was also elevated in this study. Although lymphoma is not currently designated by IARC as a tobacco-associated cancer, Hodgkin’s lymphoma has been recently linked with tobacco exposure in several large case–control studies [33–36].
The elevated risk of cervical cancer in HNSCC patients was also recently reported in an international cancer registry study [5]. Causal links are likely to include both tobacco and human papillomavirus. In this study, we report a similar elevation in risk, strongest among patients with oropharyngeal SCC. However, the low prevalence of cervical cancer in the United States renders the clinical magnitude of this SPM quite small, approximately 0.5 excess cases per 10,000 person-years at risk.
The NNF statistic, or number of patients that would be needed to follow for one year in order to diagnose one additional SPM, provides context to the EAR results. For example, because hypopharynx SCC carries a high risk of SPM, the NNF for a subsequent solid tumor is 33, and the NNF to observe an additional lung cancer is 72. In contrast, the NNF to observe an additional colorectal cancer is 1,374 and an additional stomach cancer is 2,500. NNF statistics may be helpful in informing the design of prospective studies of screening in high-risk patients, but cannot of themselves prove the efficacy of any screening technique.
Our study does have some limitations. First, there are limitations to data recorded in the SEER registry. A small percentage of recurrences in an adjacent anatomic location could theoretically be misclassified as SPM. As in clinical practice, lung metastases may be misclassified as second primary lung cancers, and vice versa. We attempted to minimize misclassification in this study with the strict application of modified Warren and Gates criteria for SPM [25, 26]. Because cancer patients are subject to increased medical surveillance, asymptomatic and indolent cancers may be identified at a higher rate, leading to the appearance of elevated SPM risk. Most commonly, this occurs in “incidentalomas” of the thyroid and prostate, neither of which were a major source of SPMs in this study. Migration of patients out of a SEER geographic registry will lead to an underestimation of SPM risk. However, this phenomenon is most common among children and young adults, who make up a small percentage of HNSCC patients. Finally, SEER data do not record cancer risk factors such as tobacco use, alcohol use, and human papillomavirus status, and we were therefore unable to incorporate these factors into a wider analysis of risk factors for SPM.
A final caveat is that the very definition of SPM is likely to be refined in the near future. Contemporary research has expanded upon the molecular background of field cancerization, revealing that abnormalities such as TP53 gene mutation, loss of heterozygosity, and high Ki-67 proliferation index are present in histologically normal mucosa adjacent to a head and neck tumor. It is likely that some cancers currently considered second HNLE cancers are in fact recurrences within an area of preexisting genetic field cancerization [9, 37]. For the purposes of this study, we were necessarily limited to clinical criteria for SPM.
Methodologic strengths of this study include large sample size, near complete follow-up, and high-quality control of the SEER program, which is considered the standard for quality among international cancer registries [26]. Biases attendant to institutional referral patterns and incomplete follow-up are minimized in a population-based study. Large sample size allows the identification of multiple SPMs with elevated risk in the HNSCC patient population, including more subtle risks not previously recognized in smaller studies. Risks are calculated relative to large SEER reference cohorts, thus maximizing both internal validity and generalizability of results. We advocate integration of both SIR and EAR measures in order to filter data to identify the most clinically meaningful SPM risks.
In conclusion, multiple primary cancers in patients with an index HNSCC are common in the United States and represent a significant obstacle to improvements in survival. Multiple investigators have demonstrated that SPMs negatively impact survival in HNSCC patients [16, 38, 39]. In addition to the well-described elevations in risk of SPMs of the head and neck, lung, and esophagus, our population-based analysis reveals significant elevations in the risk of colorectal cancer and of several other tobacco-related cancers. These findings underscore the broad public health consequences of tobacco use, which not only causes single cancers, but eventuates in long-term increased risk of a large number of multiple primary cancers. Continued tobacco use after the index HNSCC diagnosis has been shown to increase SPM risk [21, 40, 41] and would presumably increase the risk at all of these diverse sites. These findings may have impact on follow-up surveillance strategies in HNSCC patients. In high-risk patients, screening technologies, such as neck or chest computed tomography, endoscopy, or imaging beyond the canonical HNLE sites such as positron-emission tomography, may be more rationally applied. The hypotheses generated by these data will be helpful in informing future investigations of surveillance strategies in HNSCC patients.
References
Yamamoto E, Shibuya H, Yoshimura R, Miura M (2002) Site specific dependency of second primary cancer in early stage head and neck squamous cell carcinoma. Cancer 94:2007–2014
Sturgis EM, Miller RH (1995) Second primary malignancies in the head and neck cancer patient. Ann Otol Rhinol Laryngol 104:946–954
Leon X, Quer M, Diez S, Orus C, Lopez-Pousa A, Burgues J (1999) Second neoplasm in patients with head and neck cancer. Head Neck 21:204–210
Tepperman BS, Fitzpatrick PJ (1981) Second respiratory and upper digestive tract cancers after oral cancer. Lancet 2:547–549
Chuang SC, Scelo G, Tonita JM, Tamaro S, Jonasson JG, Kliewer EV, Hemminki K, Weiderpass E, Pukkala E, Tracey E, Friis S, Pompe-Kirn V, Brewster DH, Martos C, Chia KS, Boffetta P, Brennan P, Hashibe M (2008) Risk of second primary cancer among patients with head and neck cancers: a pooled analysis of 13 cancer registries. Int J Cancer 123:2390–2396
Vikram B (1984) Changing patterns of failure in advanced head and neck cancer. Arch Otolaryngol 110:564–565
Garavello W, Ciardo A, Spreafico R, Gaini RM (2006) Risk factors for distant metastases in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 132:762–766
Slaughter DP, Southwick HW, Smejkal W (1953) Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 6:963–968
Ha PK, Califano JA (2003) The molecular biology of mucosal field cancerization of the head and neck. Crit Rev Oral Biol Med 14:363–369
Boice JD Jr, Fraumeni JF Jr (1985) Second cancer following cancer of the respiratory system in Connecticut, 1935–1982. Natl Cancer Inst Monogr 68:83–98
Veli EM, Schatzkin A (1999) Common environmental risk factors. In: Neugut AI (ed) Multiple primary cancers. Lippincott Williams & Wilkins, Philadelphia, pp 213–223
Gluckman JL, Crissman JD (1983) Survival rates in 548 patients with multiple neoplasms of the upper aerodigestive tract. Laryngoscope 93:71–74
Cooper JS, Pajak TF, Rubin P, Tupchong L, Brady LW, Leibel SA, Laramore GE, Marcial VA, Davis LW, Cox JD et al (1989) Second malignancies in patients who have head and neck cancer: incidence, effect on survival and implications based on the RTOG experience. Int J Radiat Oncol Biol Phys 17:449–456
de Vries N, Snow GB (1986) Multiple primary tumours in laryngeal cancer. J Laryngol Otol 100:915–918
de Vries N, Van der Waal I, Snow GB (1986) Multiple primary tumours in oral cancer. Int J Oral Maxillofac Surg 15:85–87
Lin K, Patel SG, Chu PY, Matsuo JM, Singh B, Wong RJ, Kraus DH, Shaha AR, Shah JP, Boyle JO (2005) Second primary malignancy of the aerodigestive tract in patients treated for cancer of the oral cavity and larynx. Head Neck 27:1042–1048
Rennemo E, Zatterstrom U, Boysen M (2008) Impact of second primary tumors on survival in head and neck cancer: an analysis of 2, 063 cases. Laryngoscope 118:1350–1356
Jones AS, Morar P, Phillips DE, Field JK, Husband D, Helliwell TR (1995) Second primary tumors in patients with head and neck squamous cell carcinoma. Cancer 75:1343–1353
Sikora AG, Morris LG, Sturgis EM (2009) Bidirectional association of anogenital and oral cavity/pharyngeal carcinomas in men. Arch Otolaryngol Head Neck Surg 135:402–405
Do KA, Johnson MM, Lee JJ, Wu XF, Dong Q, Hong WK, Khuri FR, Spitz MR (2004) Longitudinal study of smoking patterns in relation to the development of smoking-related secondary primary tumors in patients with upper aerodigestive tract malignancies. Cancer 101:2837–2842
Khuri FR, Kim ES, Lee JJ, Winn RJ, Benner SE, Lippman SM, Fu KK, Cooper JS, Vokes EE, Chamberlain RM, Williams B, Pajak TF, Goepfert H, Hong WK (2001) The impact of smoking status, disease stage, and index tumor site on second primary tumor incidence and tumor recurrence in the head and neck retinoid chemoprevention trial. Cancer Epidemiol Biomarkers Prev 10:823–829
Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jamison PM, Wingo PA, Howe HL, Anderson RN, Edwards BK (2004) Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer 101:3–27
Harlan LC, Hankey BF (2003) The surveillance, epidemiology, and end-results program database as a resource for conducting descriptive epidemiologic and clinical studies. J Clin Oncol 21:2232–2233
Fritz A, Percy C, Jack A (2000) International classification of diseases for oncology. World Health Organization, Geneva
Warren S, Gates O (1932) Multiple primary malignant tumors: a survey of the literature and a statistical study. Cancer 16:1358–1414
Curtis RE, Ries LA (2006) Methods. In: Curtis RE, Freedman DM, Ron E, Ries LA, Hacker DG, Edwards BK, Tucker MA, Fraumeni JFJ (eds) New malignancies among cancer survivors: SEER cancer registries, 1973–2000. National Cancer Institute, Bethesda, pp 9–14
Schoenberg BS, Myers MH (1977) Statistical methods for studying multiple primary malignant neoplasms. Cancer 40:1892–1898
Begg CB, Zhang ZF, Sun M, Herr HW, Schantz SP (1995) Methodology for evaluating the incidence of second primary cancers with application to smoking-related cancers from the Surveillance, Epidemiology, and End Results (SEER) program. Am J Epidemiol 142:653–665
Breslow NE, Day NE (1987) Statistical methods in cancer research. IARC, Lyon, France
Freedman ND, Abnet CC, Leitzmann MF, Hollenbeck AR, Schatzkin A (2007) Prospective investigation of the cigarette smoking-head and neck cancer association by sex. Cancer 110:1593–1601
Hannan LM, Jacobs EJ, Thun MJ (2009) The association between cigarette smoking and risk of colorectal cancer in a large prospective cohort from the United States. Cancer Epidemiol Biomarkers Prev 18:3362–3367
IARC (2004) IARC monographs on the evaluation of carcinogenic risks to humans. In: IARC (ed) Tobacco smoke and involuntary smoking, vol 83. Lyon, France, pp 1179–1886
Besson H, Brennan P, Becker N, De Sanjose S, Nieters A, Font R, Maynadie M, Foretova L, Cocco PL, Staines A, Vornanen M, Boffetta P (2006) Tobacco smoking, alcohol drinking and Hodgkin’s lymphoma: a European multi-centre case–control study (EPILYMPH). Br J Cancer 95:378–384
Nieters A, Deeg E, Becker N (2006) Tobacco and alcohol consumption and risk of lymphoma: results of a population-based case–control study in Germany. Int J Cancer 118:422–430
Nieters A, Rohrmann S, Becker N, Linseisen J, Ruediger T, Overvad K, Tjonneland A, Olsen A, Allen NE, Travis RC, Bingham S, Khaw KT, Ardanaz E, Redondo ML, Basterrechea M, Martinez C, Tormo MJ, Rosso S, Tagliabue G, Masala G, Mattiello A, Tumino R, Boeing H, Bergmann M, Kaaks R, Trichopoulou A, Trichopoulos D, Peeters PH, Bueno-de-Mesquita B, Boffetta P, Brennan P, Ferrari P, Neasham D, Lund E, Berglund G, Manjer J, Hallmans G, Johansson I, Vineis P, Riboli E (2008) Smoking and lymphoma risk in the European prospective investigation into cancer and nutrition. Am J Epidemiol 167:1081–1089
Hjalgrim H, Ekstrom-Smedby K, Rostgaard K, Amini RM, Molin D, Hamilton-Dutoit S, Schollkopf C, Chang ET, Ralfkiaer E, Adami HO, Glimelius B, Melbye M (2007) Cigarette smoking and risk of Hodgkin lymphoma: a population-based case–control study. Cancer Epidemiol Biomarkers Prev 16:1561–1566
Braakhuis BJ, Tabor MP, Leemans CR, van der Waal I, Snow GB, Brakenhoff RH (2002) Second primary tumors and field cancerization in oral and oropharyngeal cancer: molecular techniques provide new insights and definitions. Head Neck 24:198–206
Chen MC, Huang WC, Chan CH, Chen PT, Lee KD (2010) Impact of second primary esophageal or lung cancer on survival of patients with head and neck cancer. Oral Oncol 46:249–254
Erkal HS, Mendenhall WM, Amdur RJ, Villaret DB, Stringer SP (2001) Synchronous and metachronous squamous cell carcinomas of the head and neck mucosal sites. J Clin Oncol 19:1358–1362
Day GL, Blot WJ, Shore RE, McLaughlin JK, Austin DF, Greenberg RS, Liff JM, Preston-Martin S, Sarkar S, Schoenberg JB et al (1994) Second cancers following oral and pharyngeal cancers: role of tobacco and alcohol. J Natl Cancer Inst 86:131–137
Day GL, Blot WJ, Shore RE, Schoenberg JB, Kohler BA, Greenberg RS, Liff JM, Preston-Martin S, Austin DF, McLaughlin JK et al (1994) Second cancers following oral and pharyngeal cancer: patients’ characteristics and survival patterns. Eur J Cancer B Oral Oncol 30B:381–386
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morris, L.G.T., Sikora, A.G., Hayes, R.B. et al. Anatomic sites at elevated risk of second primary cancer after an index head and neck cancer. Cancer Causes Control 22, 671–679 (2011). https://doi.org/10.1007/s10552-011-9739-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-011-9739-2