Abstract
Objective
Dietary patterns have been inconsistently associated with breast cancer risk. We assessed dietary patterns in association with postmenopausal breast cancer risk using an exploratory approach.
Methods
In a case–control study on postmenopausal breast cancer risk, including incident breast cancer cases (aged 50–74 years) diagnosed between 2002 and 2005 in Germany, information from a food frequency questionnaire among 2,884 cases and 5,509 controls was used for the identification of dietary patterns using principal component factor analysis. Unconditional logistic regression was performed to calculate odds ratios (ORs) adjusted for potential confounders for the highest versus the lowest quintile of dietary pattern score.
Results
Two major dietary patterns were identified, i.e., a “healthy” (including high vegetable and vegetable oil intake) and an “unhealthy” (including high meat and deep-frying fat intake) dietary pattern. Overall, no associations between the dietary patterns and breast cancer risk were observed (OR = 1.04, 95% confidence interval (CI) = (0.88, 1.23) and OR = 0.96, 95% CI = (0.81, 1.13), respectively). Associations did not differ by ER/PR status, body mass index, hormone replacement therapy use, education, energy intake, and smoking status.
Conclusion
In conclusion, we did not find an association of a “healthy” or “unhealthy” dietary pattern with postmenopausal breast cancer risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diet is one of the modifiable risk factors for breast cancer, and several single foods, macro- and micronutrients (e.g., vegetables, fiber, and vitamins) have been investigated in association with breast cancer risk [1–3]. Thus far, only alcohol, being overweight and weight gain have been established as risk factors for breast cancer [4]. In addition, dietary patterns received much attention during the last years. Dietary patterns take the whole complexity of diet into consideration when compared to investigations of single food items and thus can be used to also account for interactions between foods and nutrients in assessing the association between diet and disease risk [5].
Several studies investigating dietary patterns in relation to breast cancer risk showed inverse associations with the “prudent/healthy” pattern (usually including high vegetable, fruit, whole grains, and fish intake) and positive associations with the “western/unhealthy” pattern (generally characterized by high red and processed meat, refined grains, potatoes, and butter intake) in the whole population [6–9] or in subgroups, e.g., among smokers [10]. Some studies showed only a positive association with the “western/unhealthy” pattern but no association for any other pattern [11, 12], whereas other studies showed only a protective effect for the “prudent/healthy” pattern either in the total population or in certain subpopulations (e.g., smokers or BMI < 25) [13–15]. Moreover, some studies found differing dietary patterns that were associated with breast cancer like the drinker pattern, the starch pattern, or the traditional patterns [16–23], while others found no association in their overall study population [10, 14]. A recent meta-analysis on dietary patterns and breast cancer risk resulted in a significant decreased association for the “prudent/healthy” dietary pattern, no association for the “western/unhealthy” dietary pattern and a significant positive association for the “drinker” pattern [24]. Due to the inconsistent results so far, we aimed at assessing the association between dietary patterns and breast cancer risk in a German case–control study.
Dietary patterns can be assessed in several ways. Either an a priori approach can be used, in which dietary patterns are built based on existing knowledge about dietary constitutes, or an a posteriori approach, in which the existing data from the study (i.e., from food frequency questionnaires) are used to identify the dietary patterns. We used the latter variant in order to explore our data directly using factor analysis.
Besides an overall breast cancer risk assessment, we also performed subgroup analyses according to estrogen and progesterone receptor (ER/PR) status, body mass index, hormonal replacement therapy use, educational status, energy intake, and smoking habits.
Materials and methods
Study population
The population-based case–control study MARIE (Mammakarzinom Risikofaktoren Erhebung) was conducted from August 2002 to September 2005 in two German study regions (Hamburg and Rhine-Neckar-Karlsruhe) to assess menopausal hormone therapy and lifestyle factors in relation to breast cancer risk. The study has been previously described in great detail [25]. In brief, German-speaking women aged 50–74 years and diagnosed with histologically confirmed primary invasive or in situ breast cancer were identified through participating clinics and cancer registries. For each patient, two age- and study center-matched controls were randomly selected using inhabitant registries. In total, 3,919 cases (64% of eligible) and 7,421 controls (43% of eligible), of which 3,464 cases and 6,657 controls were postmenopausal, took part in the study. The study was approved by the ethics committee of both the University of Heidelberg and the University of Hamburg, and conducted in agreement with the Helsinki declaration. All participants gave written informed consent.
Women were defined as postmenopausal if their last menstrual bleeding was at least 12 months before age at diagnosis for cases, and at least 12 months before age at recruitment for controls, if they reported having a bilateral oophorectomy or cessation of menses due to radiation or chemotherapy, if they had unclear menopausal status due to a hysterectomy or hormone use, or if they were older than 55 years.
In-person interviews were performed to collect information on demographic factors and on breast cancer risk factors such as menstrual history, reproductive history, hormonal replacement therapy for menopausal disorders, family history of breast cancer, breastfeeding, smoking, and alcohol consumption. In addition, a self-administered, validated 176-item food frequency questionnaire (FFQ), which recorded the nutritional habits 1 year prior to diagnosis (for cases) or recruitment (for controls), was completed by 2,944 cases and 5,625 controls.
The FFQ was very similar to the one used in the European Prospective Investigation into Cancer and Nutrition (EPIC) [26, 27] and included six additional food items rich in phytoestrogens (i.e., soy milk, soy beans, tofu, soy spread, sesame/flaxseeds and sunflower-/pumpkinseeds). For each food item in the FFQ, the information about portion size and consumption frequency was used to calculate intakes in gram per day. Nutrients were estimated using the German food composition table BLS II.3 (Bundesinstitut für Gesundheitlichen Verbraucherschutz und Veterinärmedizin) [26, 27]. This FFQ was validated for food groups, energy, and nutrient intake [26, 27]. Exclusion criteria for the analyses comprised participants with missing data and participants in the top and bottom 1% energy range. Thus, 2,884 cases and 5,509 controls were included in the current analyses.
Definition of food groups
The 176 FFQ food items were assigned to one of 80 food classes using the EPIC-Soft software [28]. Further, 76 of the 80 food classes and six phytoestrogen-rich food items were grouped into food groups based on nutrient profiles or culinary usage, similar to other studies [10, 29, 30]. Four food classes were defined as ‘unclassified’ and thus were not classified. Food items not fitting into any of the food groups or representing separate food groups were retained as individual food groups (e.g., eggs, butter, cabbages, and potatoes). In total, 33 food groups were defined (Table 1).
Factor analysis
Factor analysis was performed on 33 food groups. Principal components and maximum-likelihood estimates were used to extract factors explaining the maximum proportion of the variance in the correlation matrix of the food groups. Principal component factor analysis (PCFA) was performed using SAS statistical software environment (version 9.1). The number of factors to be retained in the model was determined by eigenvalues of the correlation matrix (greater than 1 for PCFA), Scree plots, proportion of variance (>75%) explained by the identified factors, and the natural interpretability of each factor. An orthogonal transformation (varimax) was used to rotate the correlation matrix in order to get a simpler data structure with greater interpretability [31]. Each individual was assigned a factor score for each identified pattern using the SAS procedure score. Thus, individuals with high scores for a dietary pattern have a greater tendency to follow the pattern than individuals with a low score. Labeling of the factor (i.e., dietary pattern) was performed quantitatively using a cut-off of 0.30 of the factor loadings. Also, a subgroup analysis by study center was conducted to assess the reproducibility of the dietary patterns retrieved. Confirmatory identification of dietary patterns was also performed using maximum-likelihood factor analysis using R statistical software environment (version 2.9.2). However, PCFA was more appropriate for these data because of potentially non-normal distributions, and only results for PCFA are shown.
Statistical methods
Unconditional logistic regression was used to assess the association between the factor score and postmenopausal breast cancer risk. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the LOGISTIC procedure of the SAS statistical software package, version 9.1 (SAS Institute, Cary, NC). The factor score distribution among controls was used for quintile definition. Higher quintiles of the factor score were compared to the lowest quintile.
Univariate and multivariate odds ratios were estimated. All multivariate analyses were adjusted for year of birth (≤1934, 1935–1939, 1940–1944, 1945–1949, ≥1950), and study center (Rhine-Neckar-Karlsruhe, Hamburg), menopausal induction [natural with/without hormonal replacement therapy (HRT), bilateral oophorectomy (chemical or by radiation), hysterectomy, start of HRT], body mass index (BMI) (<22.5, 22.5–25, 25–30, ≥30 kg/m2), occupational level (low, simple, medium, higher, highest), first-degree family history of breast cancer (yes, no, unknown), history of benign breast disease (yes, no, unknown), number of pregnancies (≥28th week) (0, 1, 2, ≥3), age at menarche (<12, 12–14, ≥15), breastfeeding history (ever, never), total number of mammograms (0, 1–4, 5–9, ≥10, unknown), smoking habits (never, past, current), and total energy (kJ/day in continuous).
Since the association of dietary patterns with breast cancer risk may be modified by several risk factors, subgroup analyses were performed by BMI category (<25, ≥25 kg/m2), HRT use (never, ever), smoking habits (never, past, current), education level (low, medium, high) as a representative of socioeconomic status (dietary habits may differ between social groups), and energy intake (below and above median energy intake of the whole population). For the analysis of the dietary patterns by ER/PR status of the tumor (ER-positive/PR-positive, ER-positive/PR-negative or ER-negative/PR-positive, ER-negative-/PR-negative), polytomous logistic regression models were applied controlling for the above-mentioned adjustment variables in multivariate analyses. Further, a sensitivity analysis by exclusion of in situ carcinomas was performed.
To test for linear trend, median values of each factor score category were used as ordinal variables and entered in logistic regression models. Tests for heterogeneity between risk estimates were performed using the Q statistic. p values below 0.05 were considered significant.
Results
The 33 food groups included five non-alcohol beverage food groups as well as three groups on alcoholic beverages (liqueurs/spirits, wine, and beer), four groups on meat intake (poultry, processed, red meat, and offals), one group on fish intake, five groups on vegetable intake (cabbages, fruiting/leafy/other vegetables, legumes/soya, garlic/onion, potatoes), four groups on fat intake (butter, margarine, deep-frying fat, and oil and vinegar dressing), as well as eleven other food groups, as listed in Table 1. Baseline characteristics of the 2,884 cases and 5,509 controls included in the dietary pattern analyses are shown in Table 2. Cases and controls differed with respect to several characteristics: cases had fewer pregnancies, had less often breastfed, had more mammograms, and were more likely to have a non-natural induction of menopause, a first-degree relative with breast cancer, and a positive history of benign breast diseases when compared to controls. No differences in age at menarche, BMI, occupational level, smoking habits, and alcohol consumption were observed.
Two major dietary patterns were identified using PCFA: (1) high fruit, fruiting, leafy and other vegetables, garlic/onion, vegetable oils, and mayonnaise intake (further referred to as the “healthy” pattern) explaining 48.2% of the variance; (2) high processed and red meat, garlic/onion, and deep-frying fat intake (further referred to as the “unhealthy” pattern) explaining 29.8% of the variance (Table 3). Some baseline characteristics and food and nutrient intakes in quintile 1 and 5 of both dietary patterns are shown in Table 4. Within the “healthy” pattern, subjects in the highest quintile were younger, had higher energy, fat, protein, fiber, vitamin C, cholesterol, and salt intake when compared to subjects in the lowest quintile but not different with respect to BMI, carbohydrates and alcohol intake, and polyunsaturated to saturated fatty acids ratio. Within the “unhealthy” pattern, energy, fat, protein, alcohol, cholesterol, and salt intake, as well as BMI were higher in the highest compared to lowest quintile, whereas carbohydrates intake was lower. Only marginal differences were observed for age, polyunsaturated to saturated fatty acids ratio, fiber, and vitamin C intake.
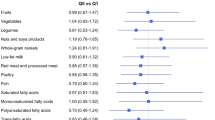
Table 5 shows the ORs for overall breast cancer risk and for subgroup analyses by ER/PR status. After adjustment for potential confounders, breast cancer risk did not differ among women in the highest compared to the lowest quintile of the “healthy” or the “unhealthy” dietary pattern. Also, no statistically significant trends were observed. Only for ER-/PR-negative tumors, a significant inverse association was observed for the “unhealthy” pattern (P for trend = 0.02). All other ER/PR subgroups did not show significant results for any pattern. For the “healthy” pattern, no heterogeneity was observed (P = 0.85), whereas the association of the “unhealthy” pattern was heterogeneous between the ER/PR subgroups (P = 0.05).
Further, subgroup analyses by BMI, HRT use, smoking habits, education level, and energy intake did not show any statistically associations between the dietary patterns and breast cancer risk (data not shown). In addition, associations were similar for both study centers (data not shown).
Sensitivity analysis by exclusion of in situ carcinomas did not result in changes of the estimates either for the “healthy” pattern or for the “unhealthy” pattern and breast cancer risk association.
Discussion
We identified two dietary patterns by PCFA, a “healthy” and an “unhealthy” dietary pattern. However, none of these dietary patterns was statistically significantly associated with postmenopausal breast cancer risk.
Our null results for the “healthy” and “unhealthy” dietary patterns in relation to postmenopausal breast cancer risk are in line with findings from several other studies, for instance with the results from three cohorts in which premenopausal [14] and postmenopausal [10, 21] breast cancer risk was not associated with any dietary pattern. A recent systematic review and meta-analysis found a decreased breast cancer risk for the highest compared with the lowest categories of “prudent/healthy” dietary patterns, whereas no association for a “western/unhealthy” dietary pattern was found [24]. Different from the “prudent/healthy” dietary patterns associated with breast cancer risk in other studies, the “healthy” pattern of our study was not characterized by high intake of dairy products and low intake of mayonnaise. High intake of mayonnaise in our “healthy” pattern can be explained by the fact that mayonnaise intake was primarily from salad dressings. High intake of sweets and desserts as well as grains, which were usually part of the “unhealthy/western” pattern, did not apply to this pattern in our study population.
There may be several reasons for the null findings of our study. One explanation for not finding an association for the “unhealthy” pattern with breast cancer risk may be due to the fact that this pattern rather represents the traditional dietary pattern consumed in Germany, containing high amounts of potatoes, onions, garlic, and grains besides the mentioned food groups of processed meat, red meat, and deep-frying fat. Further, the onset of the “unhealthy” pattern is more likely to be in childhood than the initiation of the “healthy” pattern. Women reporting a “healthy” diet 1 year before diagnosis are likely to have had the “unhealthy” dietary pattern during their childhood and adolescence, too. It is unknown which time period is mostly relevant for breast cancer risk and whether this period is recorded by the FFQ. However, it was reported that dietary behavior in childhood and adolescence might have implications on the development of breast cancer in adulthood [32, 33]. Thus, it might be possible that the diet, which is mostly related to breast cancer risk, was not recorded by the FFQ (e.g., during childhood or adolescence). Further, over- and underreporting of certain foods and total energy intake is of concern, especially in obese women [34–36]. This may have resulted in misclassification of women into categories of dietary patterns.
Results from studies conducted in the United States appear to be different from those conducted in Europe. In the United States, most studies have shown that the “prudent” pattern is associated with a breast cancer risk reduction and/or the “western” pattern is associated with an increased risk of breast cancer in the entire study population or at least in a subgroup [8, 10, 13]. Most European studies, on the other hand, observed no association for the “prudent/healthy” and “western/unhealthy” patterns [16, 18, 22, 23], and in some studies even a protective effect of the “Animal Products” or the “Pork, Processed meat and Potato” pattern was found [17, 20]. The differences between the two dietary patterns might be more extreme in the United States. “Western” patterns in the United States may contain really low amounts of vegetables and fruits, and “prudent” patterns may be completely opposite to the “western” pattern, whereas in Europe these dietary patterns might not be totally separated. Thus, the identified patterns in this study may not represent dietary patterns that are associated with breast cancer risk. Despite similar labels, the “prudent” and “western” dietary patterns in the United States and Europe are actually different, possibly reflecting cultural differences in eating habits. Also, differences in agricultural practices, food processing and other growing influences may result in differing nutrient content or different content of carcinogens present as food additives, pesticides, and preservatives.
Subgroup analyses by smoking habits, energy intake, educational status, BMI, and HRT use did not yield statistically significant association for any dietary pattern with breast cancer risk. Diet may have a stronger effect in ER-/PR-negative tumors where the role of estrogen may be smaller than in ER-positive breast cancer. There was no difference by ER/PR status for the “healthy” dietary pattern. However, the “unhealthy” pattern showed a significant inverse association with ER-/PR-negative breast cancer risk. Thus far, only three studies investigated dietary patterns in relation to ER status defined breast cancer risk, with inconsistent results [6, 10, 21]. We do not have an explanation for our finding in the ER-/PR-negative subgroup and the “unhealthy” pattern and cannot exclude the possibility of a chance finding as a consequence of testing multiple hypotheses. Therefore, further studies are necessary to clarify the association between dietary patterns and breast cancer defined by ER/PR status.
A general problem of factor analysis is that there are several subjective decisions (e.g., number of patterns to be retained, prior classification into food groups, rotation method used, naming of the factors) [37]. These facts were also critically described in a review on dietary patterns and breast cancer risk [38]. However, the dietary patterns we identified are similar to those identified by other studies, with the “healthy” pattern resembling the “prudent” pattern and the “unhealthy” pattern being similar to the “meat/western” pattern [7, 10, 12, 14, 20, 23].
Although we used a validated food frequency questionnaire, measurement error and recall bias could not be excluded in this study [39]. Especially, recall bias is very likely as there is a median time range of 5.6 months (inter-quartile range of 1.7–14.9 months) between breast cancer diagnosis and completion of the FFQ. However, results did not differ for cases completing the FFQ within or after 5.6 months of diagnosis (data not shown). In addition, the FFQ employed may not have sufficiently accounted for all relevant food items in certain food groups. Fish, for example, was not asked in enough detail to subgroup the fish intake. Similarly, vegetable oils were asked with respect to dressings and frying fats and therefore only a food group “oil and vinegar dressing” including all types of oil and a group “deep-frying fat” were available to represent oil intake. These two groups loaded, however, either for the “healthy” (oil and vinegar dressing) or for the “unhealthy” pattern (deep-frying fat). In addition, fat intake was covered by butter and margarine food groups, which did not load strong for any of the patterns. Moreover, like in every case–control study, selection bias cannot be excluded since part of the study subjects did not complete the FFQ. Although we adjusted for a broad range of confounders and breast cancer risk factors, we cannot exclude residual confounding by factors not recorded in our study.
In conclusion, we found neither a “healthy” nor an “unhealthy” dietary pattern to be associated with the risk of breast cancer in German postmenopausal women.
References
Gandini S, Merzenich H, Robertson C, Boyle P (2000) Meta-analysis of studies on breast cancer risk and diet: the role of fruit and vegetable consumption and the intake of associated micronutrients. Eur J Cancer 36(5):636–646
Smith-Warner SA, Spiegelman D, Yaun SS et al (2001) Intake of fruits and vegetables and risk of breast cancer: a pooled analysis of cohort studies. JAMA 285(6):769–776
Michels KB, Mohllajee AP, Roset-Bahmanyar E, Beehler GP, Moysich KB (2007) Diet and breast cancer: a review of the prospective observational studies. Cancer 109(12 Suppl):2712–2749
Lof M, Weiderpass E (2009) Impact of diet on breast cancer risk. Curr Opin Obstet Gynecol 21(1):80–85
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9
Cottet V, Touvier M, Fournier A et al (2009) Postmenopausal breast cancer risk and dietary patterns in the E3 N-EPIC prospective cohort study. Am J Epidemiol 170(10):1257–1267
De Stefani E, Deneo-Pellegrini H, Boffetta P et al (2009) Dietary patterns and risk of cancer: a factor analysis in Uruguay. Int J Cancer 124(6):1391–1397
Wu AH, Yu MC, Tseng CC, Stanczyk FZ, Pike MC (2009) Dietary patterns and breast cancer risk in Asian American women. Am J Clin Nutr 89(4):1145–1154
Ronco AL, De Stefani E, Boffetta P, Deneo-Pellegrini H, Acosta G, Mendilaharsu M (2006) Food patterns and risk of breast cancer: a factor analysis study in Uruguay. Int J Cancer 119(7):1672–1678
Fung TT, Hu FB, Holmes MD et al (2005) Dietary patterns and the risk of postmenopausal breast cancer. Int J Cancer 116(1):116–121
Cui X, Dai Q, Tseng M, Shu XO, Gao YT, Zheng W (2007) Dietary patterns and breast cancer risk in the shanghai breast cancer study. Cancer Epidemiol Biomarkers Prev 16(7):1443–1448
Murtaugh MA, Sweeney C, Giuliano AR et al (2008) Diet patterns and breast cancer risk in Hispanic and non-Hispanic white women: the four-corners breast cancer study. Am J Clin Nutr 87(4):978–984
Agurs-Collins T, Rosenberg L, Makambi K, Palmer JR, Adams-Campbell L (2009) Dietary patterns and breast cancer risk in women participating in the black women’s health study. Am J Clin Nutr 80(3):621–628
Adebamowo CA, Hu FB, Cho E, Spiegelman D, Holmes MD, Willett WC (2005) Dietary patterns and the risk of breast cancer. Ann Epidemiol 15(10):789–795
Hirose K, Matsuo K, Iwata H, Tajima K (2007) Dietary patterns and the risk of breast cancer in Japanese women. Cancer Sci 98(9):1431–1438
Engeset D, Dyachenko A, Ciampi A, Lund E (2009) Dietary patterns and risk of cancer of various sites in the Norwegian European prospective investigation into cancer and nutrition cohort: the Norwegian women and cancer study. Eur J Cancer Prev 18(1):69–75
Edefonti V, Decarli A, La VC et al (2008) Nutrient dietary patterns and the risk of breast and ovarian cancer. Int J Cancer 122(3):609–613
Edefonti V, Randi G, Decarli A et al (2009) Clustering dietary habits and the risk of breast and ovarian cancers. Ann Oncol 20(3):581–590
Schulz M, Hoffmann K, Weikert C, Nöthlings U, Schulze MB, Boeing H (2008) Identification of a dietary pattern characterized by high-fat food choices associated with increased risk of breast cancer: the European prospective investigation into cancer and nutrition (EPIC)-Potsdam study. Br J Nutr 100(5):942–946
Männistö S, Dixon LB, Balder HF et al (2005) Dietary patterns and breast cancer risk: results from three cohort studies in the DIETSCAN project. Cancer Causes Control 16(6):725–733
Velie EM, Schairer C, Flood A, He JP, Khattree R, Schatzkin A (2005) Empirically derived dietary patterns and risk of postmenopausal breast cancer in a large prospective cohort study. Am J Clin Nutr 82(6):1308–1319
Sieri S, Krogh V, Pala V et al (2004) Dietary patterns and risk of breast cancer in the ORDET cohort. Cancer Epidemiol Biomarkers Prev 13(4):567–572
Terry P, Suzuki R, Hu FB, Wolk A (2001) A prospective study of major dietary patterns and the risk of breast cancer. Cancer Epidemiol Biomarkers Prev 10(12):1281–1285
Brennan SF, Cantwell MM, Cardwell CR, Velentzis LS, Woodside JV (2010) Dietary patterns and breast cancer risk: a systematic review and meta-analysis. Am J Clin Nutr 91(5):1294–1302
Flesch-Janys D, Slanger T, Mutschelknauss E et al (2008) Risk of different histological types of postmenopausal breast cancer by type and regimen of menopausal hormone therapy. Int J Cancer 123(4):933–941
Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J (1997) Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. Int J Epidemiol 26(Suppl 1):S71–S81
Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J (1997) Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the German part of the EPIC project. European prospective investigation into cancer and nutrition. Int J Epidemiol 26(Suppl 1):S59–S70
Voss S, Charrondiere UR, Slimani N et al (1998) EPIC-SOFT a European computer program for 24-hour dietary protocols. Z Ernahrungswiss 37(3):227–233
Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC (2000) Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr 72(4):912–921
Kroenke CH, Fung TT, Hu FB, Holmes MD (2005) Dietary patterns and survival after breast cancer diagnosis. J Clin Oncol 23(36):9295–9303
Rencher AC (2002) Methods of multivariate analysis. Wiley series in probability and mathematical statistics, 2nd edn. John Wiley & Sons, New York
Fuemmeler BF, Pendzich MK, Tercyak KP (2009) Weight, dietary behavior, and physical activity in childhood and adolescence: implications for adult cancer risk. Obes Facts 2(3):179–186
Ruder EH, Dorgan JF, Kranz S, Kris-Etherton PM, Hartman TJ (2008) Examining breast cancer growth and lifestyle risk factors: early life, childhood, and adolescence. Clin Breast Cancer 8(4):334–342
Voss S, Kroke A, Klipstein-Grobusch K, Boeing H (1997) Obesity as a major determinant of underreporting in a self-administered food frequency questionnaire: results from the EPIC-Potsdam Study. Z Ernahrungswiss 36(3):229–236
Braam LA, Ocke MC, Bueno-de-Mesquita HB, Seidell JC (1998) Determinants of obesity-related underreporting of energy intake. Am J Epidemiol 147(11):1081–1086
Bazelmans C, Matthys C, De HS et al (2007) Predictors of misreporting in an elderly population: the ‘Quality of life after 65’ study. Public Health Nutr 10(2):185–191
Martinez ME, Marshall JR, Sechrest L (1998) Invited commentary: factor analysis and the search for objectivity. Am J Epidemiol 148(1):17–19
Edefonti V, Randi G, La VC, Ferraroni M, Decarli A (2009) Dietary patterns and breast cancer: a review with focus on methodological issues. Nutr Rev 67(6):297–314
Kipnis V, Subar AF, Midthune D et al (2003) Structure of dietary measurement error: results of the OPEN biomarker study. Am J Epidemiol 158(1):14–21
Acknowledgments
We are grateful to all participants and clinical colleagues for supporting the study. We thank U. Eilber and D. Zoller for data management and dietary data calculation. Further, we thank R. Birr and S. Behrens for technical support. KB is funded by the Deutsche Forschungsgemeinschaft, Graduiertenkolleg 793. The “Deutsche Krebshilfe e.V.” is funding the MARIE study (grant number 70-2892-BR I).
Conflict of interest
No conflicts of financial or personal interest in any company or organization are reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
First affiliation––Department and institution in which the work was performed.
Rights and permissions
About this article
Cite this article
Buck, K., Vrieling, A., Flesch-Janys, D. et al. Dietary patterns and the risk of postmenopausal breast cancer in a German case–control study. Cancer Causes Control 22, 273–282 (2011). https://doi.org/10.1007/s10552-010-9695-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9695-2