Abstract
Inflammation is postulated to play an important role in ovarian carcinogenesis. Prostaglandin endoperoxide synthase 2 (PTGS2) is responsible for the conversion of arachidonic acid to prostaglandins in response to inflammation. In a pooled analysis of two population-based studies, the Hawaii Ovarian Cancer Case–Control Study and the New England Case–Control Study, including 1,025 women with invasive ovarian carcinoma and 1,687 cancer-free controls, the association of ovarian cancer risk with the PTGS2 rs5275 polymorphism and the use of nonsteroidal antiinflammatory drugs (NSAIDs) were examined. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using unconditional logistic regression. In the pooled analysis, the CC genotype was associated with a reduced risk of nonserous ovarian carcinoma (OR = 0.66; CI: 0.44–0.98). In addition, the lowest risk was observed among carriers of the CC genotype who were users of only nonaspirin NSAIDs (OR = 0.43; CI:0.20–0.93) in all women combined. The association of PTGS2 rs5275 with nonserous ovarian carcinoma and possible effect modification by NSAID use needs further validation, preferably in prospective studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ovarian surface epithelium contributes to ovulation by lysis, and reconstruction of the ovarian cortex is thought to be the source of 90% of ovarian neoplasms [1]. Repeated episodes of ovulation-associated injury may contribute to ovarian carcinoma pathogenesis [2]. Ovulation is associated with an inflammatory response in mature follicles [3, 4] that leads to the release of reactive nitrogen and oxygen species directly damaging DNA, dysregulation of cytokines associated with neoplastic progression and overexpression of prostaglandins increasing tumor invasiveness [5, 6]. Hence, postovulatory tissue repair occurs in an environment that potentiates and promotes neoplastic risk.
Both animal models and observational studies in humans demonstrate that some potent nonsteroidal antiinflammatory drugs (NSAIDs) can inhibit the ovulatory process [3]. An inverse relation between the use of NSAIDs and the risk of ovarian cancer has been suggested [7]. Decreased ovarian cancer risk was reported among aspirin users by Prizment et al. [8], and three other studies observed inverse but nonsignificant associations of aspirin use with ovarian carcinoma risk [9–12]; however, these findings were not supported by other investigations [13–15], including results from an analysis of two large prospective studies [15]. These inconsistent findings may reflect methodological differences in assessing exposure [16].
NSAIDs interfere with prostaglandin biosynthesis by inhibiting cyclooxygenases-1 and -2 (COX1 and COX2), also known as prostaglandin endoperoxide synthases (PTGSs). Both enzymes catalyze the rate-limiting step in prostaglandin synthesis from arachidonic acid [17]. PTGS1 is constitutively expressed in most tissues; in contrast, PTGS2 is induced by various stimuli including several mitogens, cytokines, growth factors, and tumor promoters [18]. Increased expression of PTGS2 has been linked to inflammatory processes and ovarian cancer [19–22].
PTGS2 expression varies among individuals, and this variability may be influenced by common polymorphisms in the functional regions of the gene [23]. Recent investigations suggest that PTGS2 expression is regulated via the 3′ untranslated region (UTR) of the gene. This evidence was further substantiated by experiments directly showing that the PTGS2 3′ UTR confers posttranscriptional regulation through rapid mRNA turnover and translational inhibition [24]. The rs5275 SNP is located in the 3′UTR of the PTGS2 gene, and the C allele has been associated with lower steady-state PTGS2 mRNA levels [25]. PTGS2 is a small gene with only five common SNPs that are in strong linkage disequilibrium. The PTGS2 polymorphism has not been previously studied in relation to ovarian cancer risk.
Ovarian epithelial cancers are a heterogeneous group of neoplasms based on their clinical, histopathologic, and molecular features [26]. Morphologically, serous tumors resemble epithelium of the fallopian tube [27]. Endometrioid and clear cell histologic subtypes are more likely to arise from endometriotic foci [28]. Mucinous tumors are cystic tumors with mucin-secreting epithelial cells resembling either endocervical or colonic epithelium [27]. Evidence is accumulating that the major histologic subtypes of epithelial ovarian cancer have different risk factor profiles [29, 30].
We hypothesized that the PTGS2 rs5275 C allele is associated with decreased ovarian cancer risk and that this association might be stronger among NSAID users. We also evaluated whether the association of PTGS2 rs5275 genotype with risk varied by histology. To examine these associations, we pooled data from the Hawaii Ovarian Cancer Case–Control Study and the New England Case–Control Study of Ovarian Cancer. Both studies are part of the Ovarian Cancer Association Ovarian carcinomas Consortium, a forum for researchers to evaluate genetic associations with ovarian cancer with increased power [31].
Materials and methods
The New-England Case–Control Study of Ovarian Cancer (NECC) is a population-based study in New Hampshire and eastern Massachusetts that began in 1998 [32]. Histologically confirmed incident ovarian cancer cases were identified through hospital tumor boards and statewide cancer registries. Controls were selected through a combination of random digit dialing, town books, and drivers’ license lists, and were matched to the distribution of cases by 4-year-age groups and study center. Epidemiological data were collected by in-person administered questionnaires that included information about demographics, menstrual and reproductive history, medical and family history, and personal habits. Women were asked whether they had used NSAIDs continuously (at least once a week) for at least 6 months. Detailed history on the specific NSAID medication, frequency, and length of use was collected among users [10]. The NECC study included information from 723 women with invasive ovarian carcinoma and 1,095 controls.
The Hawaii Ovarian Cancer Case–Control Study (HAW) is a population-based study that includes women diagnosed with primary histologically confirmed epithelial ovarian cancer between 1993 and 2008. Incident cases were identified through the rapid-reporting system of the Hawaii Tumor Registry, which is part of the Surveillance, Epidemiology, and End-Results Program of the National Cancer Institute. Control subjects were randomly selected from participants in an annual survey of representative households, conducted by the Hawaii Department of Health under statutory provision resulting in almost 100% participation rates. Only invasive ovarian carcinoma cases (n = 302) were included in this analysis. Controls (n = 592) were frequency-matched to cases based on ethnicity and 5-year age groups in an approximate 1:2 ratio. Eligibility criteria for controls included age 18 years or older, residency in Hawaii for a minimum of 1 year, no prior history of ovarian cancer, and having at least one intact ovary. Socio-demographic, life style, and health-related information was collected during a ~2.5-h interview, using a structured pre-tested questionnaire [33]. Detailed history of NSAID use was added to the interview in 2001 and was available for 217 cases and 419 controls. To distinguish occasional versus long-term users of NSAIDs, participants were asked whether they ever used NSAIDs 12 or more times during a single year. Those who answered ‘yes’ were asked to provide detailed information on frequency of specific medications used, numbers of episodes of use, and duration of each episode. Based on this information, we defined women who used NSAIDs at least once a week continuously for 6 months or longer to be NSAID users to make it consistent with the NECC study definition.
Clinical and questionnaire data from both studies were merged into a common data set at the Ovarian Cancer Association Consortium (OCAC) coordinating center at Duke University. The combined data-set used in the pooled analysis included 1,025 cases and 1,687 controls. The following characteristics were available for all participants: case–control status, age at diagnosis/interview, race/ethnicity, education, tumor behavior and histologic subtype, family history of breast and/or ovarian cancer among first-degree female relatives (mothers and sisters) menopausal status, use of contraceptive steroids and menopausal hormones (estrogen alone or in combination with progestin), history of tubal ligation, and hysterectomy. Information on NSAID use was available for 940 cases and 1,514 controls that included all women interviewed after 2001 (217 cases and 419 controls) from the Hawaii study and all NECC study participants.
The Hawaii study protocol was approved by the Institutional Review Board of the University of Hawaii. The NECC study protocol was approved by the Human Subjects Review Committees at both Brigham and Women’s Hospital and Dartmouth Medical School, and each participant provided signed informed consent. In addition, Duke University has Institutional Review Board approval as a data coordinating center.
Genotyping
DNA was purified from whole blood using Qiagen Midi Kits (Qiagen, Valencia, CA). At each site, genotyping was performed using 5′ nuclease TaqMan allelic discrimination assay (TaqMan, Applied Biosystems, Foster City, CA, USA). Samples from cases and controls were intermixed on each plate, and laboratory personnel were blinded to the case–control status of the study participants. We used the following criteria to measure the acceptability of the genotyping results: (1) >3% sample duplicates included, (2) concordance rate for duplicate samples ≥ 98%, (3) overall call rate (by study) >95% and (4) call rate >90% for each 384-well plate and (5) cases and controls intermixed on each plate. Both studies met each of the criteria. Gene and allele nomenclature was according to the National Center of Biotechnology Information (http://www.ncbi.nlm.nih.gov/).
Statistical analysis
Statistical analysis was performed using SAS version 9.2 (SAS Institute, Cary, NC). A goodness of fit chi-square test was used to assess whether allele frequency distributions among controls overall and in each ethnic group were consistent with Hardy–Weinberg equilibrium. Unconditional multiple logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the association of the PTGS2 rs5275 genotype with ovarian carcinoma risk. ORs and CIs were estimated separately for heterozygous and homozygous variant C allele carriers, using women with the TT genotype as the reference group. We also performed genetic analyses testing a log-additive model in which genotype was categorized by three levels (0, 1, and 2) representing combinations of alleles. In addition, we compared risk among heterozygotes and homozygote C allele carriers combined (testing a dominant genetic model) (data not shown) and among women with the CC genotype compared to the TT and TC genotypes combined (testing a recessive genetic model). Based on the Akaike Information Criterion (AIC), the recessive model provided better fit for the data.
Using data available for the duration of NSAID use, we categorized women who never used NSAIDs for 6 months or longer as ‘nonusers’ and women who reported long-term use of NSAIDs as ‘users’. Among NSAID users, separate analyses were performed for women who used only acetylsalicylic acid or other salicylates (referred to as ‘aspirin’), nonaspirin NSAIDs only, or both.
To evaluate potential confounders, the distributions of genotype and NSAID use were examined by factors associated with ovarian cancer risk in a multiple logistic regression model. The following covariates were included into all models: age, ethnicity, education, family history of breast and/or ovarian cancer, menopausal status, use of contraceptive and menopausal hormones (estrogen alone and in combination with progestin), and, in combined analyses, study. Heterogeneity of effects by study, NSAID use and other covariates was examined using a Wald test of the genotype-covariate interaction term. Heterogeneity of associations of the rs5275 genotype with risk by histological type (serous, mucinous, endometrioid, clear cell, and other) was evaluated using Wald tests comparing ORs across strata by tumor behavior and histology in polytomous logistic regression models. Analyses were conducted for each study separately and for both studies combined. All p-values were based on two-tailed tests. Statistical significance was considered at a p value less than 0.05.
Results
Cases (age: 54.6; SD, 12.0) were (nonsignificantly) older than controls (age: 52.2; SD, 13.4) (Table 1). The distribution of PTGS2 rs5275 genotypes among control subjects was consistent with Hardy–Weinberg equilibrium in each stratum by ethnicity and by study and in all strata combined. The rare (C) allele frequency was higher among white non-Hispanic women (0.34) than among Asian women (0.22) and among women of mixed/other ethnicity (0.25) (p = 0.06) but was similar among white non-Hispanic women in Hawaii and NECC studies (p for heterogeneity among genotypes = 0.62). No significant associations of rs5275 genotype with age, ethnicity, parity, menopausal status, tubal ligation, hysterectomy, use of contraceptive or menopausal hormones, or NSAID use were observed (p > 0.05) (data not shown).
Any NSAID use was significantly associated with decreased ovarian cancer risk (OR = 0.79; CI: 0.67–0.95). Significant inverse associations with risk were observed among women who used both aspirin and nonaspirin NSAIDs, but not among women who used one of these types exclusively (Table 1). The proportion of NSAID users was higher (53% for cases and 65% for controls) among the Hawaii study participants than among women in the NECC study (38% for both cases and controls). Among cases, the proportion of women reporting aspirin use only was the same in both studies (14%). Also similar was the number of women who used NSAIDs from both groups (aspirin and nonaspirin) among controls. However, women with ovarian cancer in Hawaii reported the use of nonaspirin NSAIDs only (21%), and aspirin and nonaspirin NSAIDs (18%) to a greater extent than the NECC study cases (13 and 6%, respectively).
Use of any NSAIDs was significantly positively associated with education (p = 0.001), and use of contraceptive (p = 0.0001) and menopausal hormones (p < 0.0001) (data not shown). Postmenopausal women were significantly more likely to use aspirin and other salicylates (p < 0.0001), and less likely to use nonaspirin NSAIDs exclusively (p < 0.0001) than premenopausal women. Among Hawaii participants, women with family history of breast and/or ovarian cancer were more likely to use both aspirin and nonaspirin NSAIDs only than women who did not report ovarian cancer among first-degree relatives.
We did not observe significant associations of PTGS2 rs5275genotype with ovarian cancer risk among all women combined (OR = 0.86; CI: 0.66–1.12); or in the analyses restricted to white women only (Table 2). In sub-group analyses by study site, we found that homozygous rs5275 C allele carriers had significantly reduced ovarian cancer risk when compared to carriers of any T allele (recessive genetic model) (OR = 0.51; CI: 0.26–0.98) in the Hawaii study (OR = 0.51; CI: 0.26–0.98) but not in the NECC study (OR = 0.96; CI: 0.71–1.28; p for heterogeneity between studies = 0.10). No heterogeneity in the association of rs5275 with risk was observed by ethnicity (p for heterogeneity in all models tested ranged from 0.60 to 0.99).
The data were further examined by histological subtype of ovarian cancer (Table 3). PTGS2 rs5275 CC genotype was associated with nonsignificantly decreased risk among women with endometrioid, clear cell, mucinous, and other ovarian cancer histological types and slightly elevated risk of serous carcinoma. Because all nonserous histological types displayed an inverse relation between PTGS2 rs5275 genotype and ovarian cancer risk (p for heterogeneity = 1.00), they were grouped together. Among women with nonserous histology, CC genotype was associated with significantly reduced ovarian carcinoma risk compared to women with the TT genotype or any T allele carriers (recessive genetic model OR = 0.66; CI: 0.44–0.98; p = 0.04). A suggestion of heterogeneity in the CC genotype association was observed between nonserous and serous subtypes (p = 0.07). Although the distribution of histological subtypes among white women did not differ by study (p = 0.55), when all ethnicities were combined the HAW cases had a higher proportion of mucinous tumors than the NECC cases (12 vs. 7%) because of the higher incidence of mucinous tumors among Asian women (data not shown).
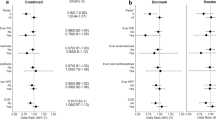
The joint association of the PTGS2 rs5275 genotype and NSAID use on ovarian carcinoma risk was examined (Table 4). Carriers of the CC allele who only used nonaspirin NSAIDs had the lowest risk of ovarian carcinoma compared to TT genotype carriers who did not use NSAIDs (OR = 0.43; CI: 0.20–0.93; p = 0.03). CC genotype carriers who were users of both aspirin and nonaspirin NSAIDs also had a nonsignificantly decreased ovarian cancer risk (OR = 0.42; CI: 0.18–1.01; p = 0.05), whereas women with the CC genotype who reported aspirin use alone had a nonsignificantly increased ovarian cancer risk (OR = 1.21; 95% CI: 0.60–2.44; p = 0.60).
Discussion
In this pooled analysis of two population-based studies, we explored the association of the PTGS2 rs5275 polymorphism with invasive ovarian carcinoma risk and possible effect of modification of the genetic association by NSAID use. The most pronounced decrease in ovarian cancer risk (57%) was observed among women who were users of nonaspirin NSAIDs and homozygous for the rs5275 C allele. CC allele carriers who were users of both aspirin and nonaspirin NSAIDs also had markedly decreased risk (58%) that was borderline significant (p = 0.05). No association with the risk of ovarian cancer was observed among CC genotype carriers who reported using aspirin alone. The PTGS2 rs5275 CC genotype was associated with a significantly decreased risk of ovarian cancer in the HAW study only. Endometrioid, clear cell, mucinous, and ‘other’ histologic types of ovarian carcinomas were inversely associated with the PTGS2 rs5275 CC genotype (p for heterogeneity neoplasms = 1.00). Although there was modest evidence for heterogeneity of the PTGS2 genotype effect between serous and nonserous neoplasms (p = 0.07); a significant 36% reduction in the risk of nonserous carcinoma among women with the PTGS2 rs5275 CC genotype compared to women homozygous for the common allele was observed.
Our finding of decreased ovarian cancer risk among NSAID users who were carriers of the PTGS2 rs5275 CC genotype is in accord with our priori hypothesis. Genetic variation in PTGS2 that alters expression levels or the biochemical function of prostaglandin endoperoxide synthase 2 may influence a woman’s risk of ovarian carcinoma. PTGS2 converts arachidonic acid to prostaglandin H2, which is a precursor to all other prostaglandins. Prostaglandins are integral components in the cellular response to inflammation, promoting cellular proliferation and angiogenesis [34]. Given its location in the 3′ UTR, the rs5275 SNP is a likely candidate to influence PTGS2 RNA half-life, which is controlled by sequence-specific elements in the region of the mRNA [24]. Previous studies have reported that in the proximal upstream region of this SNP there is a conserved AU-rich sequence element, which mediates posttranscriptional degradation of PTGS2 mRNA [24]. A functional analysis measuring PTGS2 mRNA suggests that the decreased ovarian carcinoma risk associated with the rs5275 C allele may be attributed to lower PTGS2 expression [25]. Although an inverse association of NSAID use and ovarian cancer has not been clearly established, no study has investigated potential effect modification of this association by PTGS2 genotype.
The absence of an association of the PTGS2 rs5275 SNP and aspirin with the risk of ovarian cancer risk might be explained by the dose-dependent action of aspirin on COX-1 and COX-2 [35]. Low-dose aspirin appears to be relatively specific for COX-1; whereas higher doses (≥1 g/day) appear to inhibit both COX-1 and COX-2 and may have a stronger antiinflammatory effects [35, 36]. Because low-dose aspirin is able to irreversibly inhibit platelet COX-1 [37], it is being widely used for the prevention of coronary heart disease. Results from a recent large-scale, long-term trial suggested that alternate day use of low-dose aspirin (100 mg) for an average 10 years of treatment does not lower cancer risk, including ovarian malignancy, although the potential benefit of higher doses of aspirin cannot be ruled out [36]. In this study, data on dose was not available for the majority of women, and NSAID users in this pooled analysis might have included women who used low dose aspirin and thus did not benefit from its antiinflammatory effect.
The observation that NSAID use and PTGS2 genotype were more strongly associated with endometrioid, clear cell, and mucinous tumors than with serous carcinoma is biologically plausible, although no differences in risk associated with NSAID use have been previously reported by ovarian histological types [15]. Endometrioid and clear cell carcinomas are associated with endometriosis [25], the presence of endometrial tissue outside the endometrium that causes a marked local inflammatory reaction [26]. Inflammation might also play a role in the etiology of ovarian mucinous neoplasms, which resemble colon cancer, as NSAID use has been consistently associated with a reduced risk of colorectal cancer [38, 39].
Clinicopathological studies suggest that COX-2 expression in ovarian carcinoma tissue might represent an unfavorable prognostic factor [40, 41]. Although all these studies included small numbers of nonserous carcinomas, some differences in COX-2 expression by histology were observed. Denkert et al. [40] found nonsignificantly higher COX-2 expression among nonserous tumors (46 vs. 40% among serous). Ozel et al. [42] also reported insignificantly higher expression of COX-2 among nonserous than serous carcinomas (90 vs. 78%). Uddin et al. [43] observed nonsignificantly higher COX-2 expression among women with serous (62%) and endometrioid carcinomas (59%) than among women with clear cell tumors (25%). Seo et al. [44] reported higher COX-2 expression in serous and endometrioid carcinomas than in mucinous histological subtypes.
Strengths of this study include the population-based nature of both Hawaii and NECC studies, histologic confirmation of all case diagnoses, stringent genotyping quality control procedures, and the completeness of epidemiological data related to ovarian cancer risk. The pooled analysis included a relatively large number of cases and controls, and the statistical power was adequate (>90%) to detect ORs of 0.69 and lower at a critical level of 5% (two-sided) under a recessive genetic model. However, we note that the study power was limited to investigate the joint effects of genotype and NSAID use by histologic subtype. Another study limitation was that exploration of NSAID dose was not possible in this analysis. Due to the retrospective manner of collecting data on NSAID use in case–control studies, there is the potential for recall bias, although participants were likely unaware of the potential association of NSAID use with ovarian cancer risk.
In summary, we observed an inverse association between a potentially functional SNP in the 3′ UTR of the PTGS2 gene and nonserous ovarian carcinoma risk. The potential for a reduced risk of ovarian cancer among women with the CC genotype who use NSAIDs needs to be examined further in larger studies, preferably with prospective collection of risk factor information.
References
Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC (2001) Ovarian surface epithelium: biology, endocrinology, and pathology. Endocr Rev 22(2):255–288
Fathalla MF (1971) Incessant ovulation—a factor in ovarian neoplasia? Lancet 2(7716):163
Espey LL (1994) Current status of the hypothesis that mammalian ovulation is comparable to an inflammatory reaction. Biol Reprod 50(2):233–238
Richards JS, Russell DL, Ochsner S, Espey LL (2002) Ovulation: new dimensions and new regulators of the inflammatory-like response. Annu Rev Physiol 64:69–92
Ames BN, Shigenaga MK, Hagen TM (1993) Oxidants, antioxidants, and the degenerative diseases of aging. Proc Natl Acad Sci USA 90(17):7915–7922
Hofseth LJ, Ying L (2006) Identifying and defusing weapons of mass inflammation in carcinogenesis. Biochim Biophys Acta 1765(1):74–84
Schildkraut JM, Moorman PG, Halabi S, Calingaert B, Marks JR, Berchuck A (2006) Analgesic drug use and risk of ovarian cancer. Epidemiology 17(1):104–107
Prizment AE, Folsom AR, Anderson KE (2010) Nonsteroidal anti-inflammatory drugs and risk for ovarian and endometrial cancers in the Iowa Women’s Health Study. Cancer Epidemiol Biomarkers Prev 19(2):435–442
Tzonou A, Polychronopoulou A, Hsieh CC, Rebelakos A, Karakatsani A, Trichopoulos D (1993) Hair dyes, analgesics, tranquilizers and perineal talc application as risk factors for ovarian cancer. Int J Cancer 55(3):408–410
Cramer DW, Harlow BL, Titus-Ernstoff L, Bohlke K, Welch WR, Greenberg ER (1998) Over-the-counter analgesics and risk of ovarian cancer. Lancet 351(9096):104–107
Akhmedkhanov A, Toniolo P, Zeleniuch-Jacquotte A, Kato I, Koenig KL, Shore RE (2001) Aspirin and epithelial ovarian cancer. Prev Med 33(6):682–687
Lacey JV Jr, Sherman ME, Hartge P, Schatzkin A, Schairer C (2004) Medication use and risk of ovarian carcinoma: a prospective study. Int J Cancer 108(2):281–286
Tavani A, Gallus S, La VC, Conti E, Montella M, Franceschi S (2000) Aspirin and ovarian cancer: an Italian case-control study. Ann Oncol 11(9):1171–1173
Hannibal CG, Rossing MA, Wicklund KG, Cushing-Haugen KL (2008) Analgesic drug use and risk of epithelial ovarian cancer. Am J Epidemiol 167(12):1430–1437
Pinheiro SP, Tworoger SS, Cramer DW, Rosner BA, Hankinson SE (2009) Use of nonsteroidal antiinflammatory agents and incidence of ovarian cancer in 2 large prospective cohorts. Am J Epidemiol 169(11):1378–1387
Crew KD, Neugut AI (2006) Aspirin and NSAIDs: effects in breast and ovarian cancers. Curr Opin Obstet Gynecol 18(1):71–75
Smith WL, Garavito RM, DeWitt DL (1996) Prostaglandin endoperoxide H synthases (cyclooxygenases)-1 and -2. J Biol Chem 271(52):33157–33160
DuBois RN, Abramson SB, Crofford L et al (1998) Cyclooxygenase in biology and disease. FASEB J 12(12):1063–1073
Landen CN Jr, Mathur SP, Richardson MS, Creasman WT (2003) Expression of cyclooxygenase-2 in cervical, endometrial, and ovarian malignancies. Am J Obstet Gynecol 188(5):1174–1176
Shigemasa K, Tian X, Gu L, Shiroyama Y, Nagai N, Ohama K (2003) Expression of cyclooxygenase-2 and its relationship to p53 accumulation in ovarian adenocarcinomas. Int J Oncol 22(1):99–105
Khalifeh I, Munkarah AR, Lonardo F et al (2004) Expression of Cox-2, CD34, Bcl-2, and p53 and survival in patients with primary peritoneal serous carcinoma and primary ovarian serous carcinoma. Int J Gynecol Pathol 23(2):162–169
Li S, Miner K, Fannin R, Carl BJ, Davis BJ (2004) Cyclooxygenase-1 and 2 in normal and malignant human ovarian epithelium. Gynecol Oncol 92(2):622–627
Cok SJ, Morrison AR (2001) The 3′-untranslated region of murine cyclooxygenase-2 contains multiple regulatory elements that alter message stability and translational efficiency. J Biol Chem 276(25):23179–23185
Dixon DA, Kaplan CD, McIntyre TM, Zimmerman GA, Prescott SM (2000) Post-transcriptional control of cyclooxygenase-2 gene expression. The role of the 3′-untranslated region. J Biol Chem 275(16):11750–11757
Yang H, Gu J, Lin X et al (2008) Profiling of genetic variations in inflammation pathway genes in relation to bladder cancer predisposition. Clin Cancer Res 14(7):2236–2244
Cho KR, Shih I (2009) Ovarian cancer. Annu Rev Pathol 4:287–313
Mok SC, Kwong J, Welch WR et al (2007) Etiology and pathogenesis of epithelial ovarian cancer. Dis Markers 23(5–6):367–376
Mandai M, Yamaguchi K, Matsumura N, Baba T, Konishi I (2009) Ovarian cancer in endometriosis: molecular biology, pathology, and clinical management. Int J Clin Oncol 14(5):383–391
Chiaffarino F, Parazzini F, Bosetti C et al (2007) Risk factors for ovarian cancer histotypes. Eur J Cancer 43(7):1208–1213
Gates MA, Rosner BA, Hecht JL, Tworoger SS (2010) Risk factors for epithelial ovarian cancer by histologic subtype. Am J Epidemiol 171(1):45–53
Berchuck A, Schildkraut JM, Pearce CL, Chenevix-Trench G, Pharoah PD (2008) Role of genetic polymorphisms in ovarian cancer susceptibility: development of an international ovarian cancer association consortium. Adv Exp Med Biol 622:53–67
Terry KL, De VI, Titus-Ernstoff L, Shih MC, Cramer DW (2005) Androgen receptor cytosine, adenine, guanine repeats, and haplotypes in relation to ovarian cancer risk. Cancer Res 65(13):5974–5981
Tung KH, Goodman MT, Wu AH et al (2003) Reproductive factors and epithelial ovarian cancer risk by histologic type: a multiethnic case-control study. Am J Epidemiol 158(7):629–638
Backlund MG, Mann JR, DuBois RN (2005) Mechanisms for the prevention of gastrointestinal cancer: the role of prostaglandin E2. Oncology 69(Suppl 1):28–32
Thun MJ (2000) Beyond willow bark: aspirin in the prevention of chronic disease. Epidemiology 11(4):371–374
Cook NR, Lee IM, Gaziano JM et al (2005) Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial. JAMA 294(1):47–55
Awtry EH, Loscalzo J (2000) Aspirin. Circulation 101(10):1206–1218
Cuzick J, Otto F, Baron JA et al (2009) Aspirin and non-steroidal anti-inflammatory drugs for cancer prevention: an international consensus statement. Lancet Oncol 10(5):501–507
Potter JD (1999) Colorectal cancer: molecules and populations. J Natl Cancer Inst 91(11):916–932
Denkert C, Kobel M, Pest S et al (2002) Expression of cyclooxygenase 2 is an independent prognostic factor in human ovarian carcinoma. Am J Pathol 160(3):893–903
Munkarah A, Ali-Fehmi R (2005) COX-2: a protein with an active role in gynecological cancers. Curr Opin Obstet Gynecol 17(1):49–53
Ozel E, Pestereli HE, Simsek T, Erdogan G, Karaveli FS (2006) Expression of cyclooxygenase-2 and inducible nitric oxide synthase in ovarian surface epithelial carcinomas: is there any correlation with angiogenesis or clinicopathologic parameters? Int J Gynecol Cancer 16(2):549–555
Uddin S, Ahmed M, Hussain A et al (2010) Cyclooxygenase-2 inhibition inhibits PI3 K/AKT kinase activity in epithelial ovarian cancer. Int J Cancer 126(2):382–394
Seo SS, Song YS, Kang DH et al (2004) Expression of cyclooxygenase-2 in association with clinicopathological prognostic factors and molecular markers in epithelial ovarian cancer. Gynecol Oncol 92(3):927–935
Acknowledgments
The authors thank the physicians, administrators, and cancer registrars at the following institutions for their support of this study: Castle Memorial Hospital, Kaiser Foundation Hospital, Kapiolani Medical Center for Women and Children, Kuakini Medical Center, Queen’s Medical Center, Straub Clinic and Hospital, St Francis Hospital, Tripler Army Hospital, and Wahiawa General Hospital. We would also like to thank the NECC participants and their physicians. We are grateful to the family and friends of Kathryn Sladek Smith for their generous support of Ovarian Cancer Association Consortium through their donations to the Ovarian Cancer Research Fund. We thank Annette Lum-Jones and Ann Seifried for their assistance with genotyping. The findings and conclusions of this study do not necessarily represent the views of these physicians and institutions.
Financial Support
US Public Health Service grants R01-CA-58598, R01-CA-54419, P50-CA-105009, and contracts N01-CN-55424 and N01-PC-67001 from the National Cancer Institute, NIH, Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lurie, G., Terry, K.L., Wilkens, L.R. et al. Pooled analysis of the association of PTGS2 rs5275 polymorphism and NSAID use with invasive ovarian carcinoma risk. Cancer Causes Control 21, 1731–1741 (2010). https://doi.org/10.1007/s10552-010-9602-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9602-x