Abstract
Objective
Eating behaviors, such as the timing, speed of eating, and frequently consuming hot drinks, fried, spicy, or barbecued foods may be associated with increased risks of esophageal cancer. We analyzed data from a population-based case–control study to examine whether eating behaviors are associated with risk of esophageal cancer.
Methods
Self-administered questionnaire was used to collect data on demographic, socioeconomic, and lifestyle characteristics, and a food frequency questionnaire was used to collect data on dietary behaviors from 1,472 control subjects, 286 cases with adenocarcinoma of the esophagus, 320 cases with esophagogastric junction adenocarcinoma (EGJAC), and 238 cases with esophageal squamous cell carcinoma (ESCC). We calculated odds ratios (ORs) and 95% confidence intervals (CIs) using unconditional multivariable adjusted logistic regression, adjusting for confounders.
Results
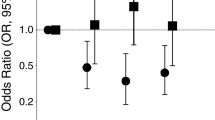
Frequency of hot drinks, home-fried foods, barbecued meats, spicy foods, and the timing of eating an evening meal were not associated with esophageal cancer risk. Those who frequently consumed fried ‘take-away’ food had increased risks of EGJAC (OR = 1.44, 95% CI = 1.01–2.05; p value = 0.04). Eating speed was inversely associated with ESCC risk (p for trend = 0.001).
Conclusion
We found no evidence that consumption of hot drinks, barbecued meats, spicy foods, or the timing of the evening meal are associated with increased risk of esophageal cancer in this Australian population. Associations with consumption of fried ‘take-away’ foods and eating speed await confirmation in future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is the eighth most common cancer by incidence, and the sixth most common cause of cancer-related deaths worldwide [1, 2]. There are two histological types: esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC) [2]. The incidence of EAC has been increasing in Western countries during the past three decades and now occurs more frequently than ESCC [3]. EAC occurs more commonly in men, and the incidence rises with age. ESCC has been strongly associated with high-level exposure to alcohol and tobacco smoking in western populations [4], while EAC has been associated with obesity, tobacco smoking, gastro-esophageal reflux disease (GERD) and Barrett’s esophagus [5]. The incidence of EAC has been increasing in Australia in line with trends observed elsewhere [6, 7]. A recent publication reported that in the two decades prior to 2005, the annual percentage change in the incidence of EAC in New South Wales, Australia [8] in men and women was 4.2% (95% CI = 2.7–5.8%) and 4.3% (95% CI = 1.8–7.0%), respectively. These rapid changes in incidence prompted the present study to identify risk factors for adenocarcinomas of the esophagus.
Some epidemiological studies have reported associations between some lifestyle and dietary behaviors and esophageal cancers [9, 10] albeit with inconsistent results. For example, a recent study conducted in Iran reported that people who drink tea at very high temperatures have markedly increased risks of ESCC, possibly due to thermal injury to the esophagus [11]. This finding has not been universal however [12]. There is also some evidence that consuming a diet rich in fried foods, particularly potatoes, [13] is related to moderate increase in esophageal cancer risk probably due to the formation of acrylamide, a probable human carcinogen in carbohydrate-rich foods [14]. Other studies have failed to confirm this finding [15]. Other dietary practices that have been associated with esophageal cancer include barbecuing meat [16–18], eating ‘spicy’ foods [19], eating evening meals late at night [20], and eating quickly with inadequate chewing of food [21].
We have used data collected in a nation-wide study of esophageal cancers to determine whether eating behaviors are associated with esophageal cancer risk in a western population such as Australia.
Materials and methods
A detailed description of the methods for this population-based case–control study has been published previously [22]. In summary, adult participants aged 18–79 with a histologically confirmed primary invasive EAC or esophagogastric junction adenocarcinoma (EGJAC) or ESCC of the esophagus diagnosed between 2001 and 2005 were identified through major treatment centers throughout Australia; those missed at these centers were identified by state-based cancer registries (notification of cancer diagnosis is mandatory in all states of Australia). Of 1,191 cases invited to participate in the study through the treatment centers, 928 (78%) agreed to take part, while of 386 cases invited to participate from the cancer registries, 253 (66%) agreed to take part. A total of 1,181 (75%) cases consented to take part in the study. Controls were randomly selected from the Australian Electoral Roll (enrollment is compulsory). We prospectively sampled controls from within strata of age (in 5-year age groups), sex, and state of residence. Female controls were intentionally over-sampled at all ages to accommodate their simultaneous enrollment in a parallel case–control study of ovarian cancer. Of 3,042 controls who were contacted and invited to take part in the study, 1,680 (55%) agreed to take part. In total 1,102 cases and 1,580 controls returned the main risk factor questionnaire. Details of the histological type and anatomical site of each tumor were abstracted from diagnostic pathology reports. Anatomical sites of tumors were categorized into ‘esophageal’ and ‘esophagogastric junction’ tumors according to the WHO classification [23]. The study was approved by the human research ethics committee of the Queensland Institute of Medical Research and all participating institutions. All study participants provided informed written consent to take part.
Dietary data collection
Dietary data were obtained using a 135-item semi-quantitative food frequency questionnaire (FFQ). Controls were asked to report how often they consumed a specified amount of food item on the FFQ in the previous year. Cases were asked to report their usual frequency of consumption in the year before their diagnosis or if their diet had changed in the last 6–12 months, their usual diet. The FFQ was based on the instrument developed by Willett and colleagues [24] but was modified for use in Australia. The FFQ was validated against 12-day weighed food records and serum biomarkers and was found to provide reproducible intake estimates [25–27]. The FFQ estimates showed good correlations with weighed food records for consumption of tea (r = 0.88) and coffee(r = 0.81) [26]. Participants reported on average how many times they consumed a specified portion size of regular coffee (instant, filtered, plunger), decaffeinated coffee (instant, filtered, plunger), tea (not herbal or green teas), and green tea. The response options ranged from ‘never’ to ‘4+ times per day’. For analysis regarding the number of cups of hot beverages consumed, all types of coffee and all types of tea were combined to form the total amount of all hot drinks (tea and coffee, any type) consumed. Daily total intake of fruits and vegetables (in grams), total energy intake (in kJ) and caffeine intake (in milligrams) were calculated using food composition tables in Australia as contained in the electronic version of Nutrient Tables for use in Australia (NUTTAB) 2006 [28]. In addition to the main FFQ items, all participants completed additional questions about the usual temperature at which tea or coffee or (other hot beverages) was consumed (on a 6-point scale ranging from ‘room temperature’, ‘luke-warm’, ‘warm’, ‘warm to hot’, ‘hot’, to ‘very hot’) and the frequency of consumption of fried food (prepared at home or ‘take-away’), spicy foods, and barbecued meats. For barbecued meat, participants were asked how ‘well-done’ was the meat they tended to eat, with responses as follows: ‘I never eat BBQ meat’, ‘rare (still some blood)’, ‘medium-rare (pink in the middle)’, ‘medium (lightly cooked all the way through)’ or ‘well done’. We asked participants how often they ate foods that were ‘hot and spicy’ (e.g., curry, chili, Tabasco) during the past 10 years; with responses ranging from ‘never’, ‘less than once a month’, ‘about once a month’, ‘between once a month and once a week’, ‘about once a week’, ‘several times a week’, and ‘everyday’. Finally, we asked participants questions relating to eating speed and timing of evening meals.
Non dietary data collection
We collected data about other factors using a self-administered questionnaire. Information was collected on demography (age, sex), social background (education, income), as well as height and weight 1 year ago (1 year before diagnosis for cases). We calculated body mass index (BMI) by dividing weight in kilograms by the square of height in meters. BMI categories used for analysis were <25 kg/m2—‘normal weight’; 25–29.9 kg/m2—‘overweight’; and ≥30—‘obese’. Participants were asked whether, over their whole life, they had ever smoked more than 100 cigarettes, cigars, or pipes; positive responses elicited further questions about ages at which they started and stopped smoking and typical daily consumption. We derived the number of pack years of tobacco exposure by dividing the number of cigarettes smoked daily by 20 and multiplying by the total number of years smoked. To assess lifetime alcohol consumption we asked participants to report the frequency with which they consumed different classes of alcohol (low alcohol beer, regular beer, white wine, red wine, port/sherry, and spirits/liqueurs) between ages 20–29, 30–49, and >50, as applicable. Total alcohol consumption was summed across all age groups for all types of alcohol, from which we calculated a weighted average number of standard drinks (10 g ethanol) consumed per week between age 20 years and current age. We assessed the frequency of symptoms of gastro-esophageal reflux defined as the presence of heartburn (‘a burning pain behind the breastbone after eating’) or acid reflux (‘a sour taste from acid or bile rising up into the mouth or throat’) 10 years before diagnosis. We also assessed frequency of use of non-steroidal anti-inflammatory drugs (NSAIDs) including aspirin, and acid suppressants including proton pump inhibitors (PPIs) during the past 5 years.
Exclusion and final sample size
Of the 1,102 cases and 1,580 controls who returned the main risk factor questionnaire, 155 (141 cases and 14 controls) participants had no opportunity to complete a FFQ because the nutrition component of the study commenced 6 months after the main study, giving a total of 961 cases and 1,566 eligible controls. After further exclusion of participants who omitted responses to 10% or more of FFQ items, and those with implausible energy intake according to Willett’s criteria [24], we had 844 cases (286 EAC, 320 EGJAC, 238 ESCC) (88% of those who completed a FFQ),and 1,472 (94%) controls left for these dietary analyses.
Statistical analysis
The distributions of demographic characteristics and potential risk factors were compared among cases and controls using chi-square test for proportions. We estimated the risk of EAC, EGJAC and ESCC associated with categories of exposure variables by calculating the odds ratios (ORs) and 95% confidence intervals (CIs) for each of the case groups using unconditional multivariable logistic regression. The multivariable logistic regression model adjusted for the confounding effects of age, sex, educational status, cumulative history of smoking in pack years, heartburn and acid reflux symptoms in previous 10 years, body mass index in previous year, aspirin use in previous 5 years, vegetable, fruit, and total energy intake. Tests for linear trend were performed by treating the categorical variables as continuous predictors in the multivariable regression model. Category values were assigned as the midpoint of the range for each category. For beverage drinking temperature variables, we combined the lowest two categories and assigned the following values for trend analysis only: ‘room temperature/luke-warm’ 35°C (reference), ‘warm’ 50°C, ‘warm to hot’ 60°C, hot 65°C, and very hot 70°C. To assess the association between temperature of tea and coffee and esophageal cancer, we adjusted further for caffeine intake. All analyses were performed using SAS version 9.1 (SAS Institute, Inc., Cary, NC). p-values were two sided, and p < 0.05 was considered statistically significant.
Results
Characteristics of cases and controls are presented in Table 1. Esophageal cancer cases were more likely to be older (60+ years) and to be heavy smokers (30+ pack years) than controls. Cases with EAC and EGJAC were more likely to be men, obese, and to experience symptoms of reflux (monthly or more often) than ESCC cases and controls. ESCC cases were more likely to be heavy alcohol consumers (≥21 standard drinks/week) than EAC and EGJAC cases and controls. On average, controls were less likely (14.5%) to use PPIs than EAC (39.2%), EGJAC (37.2%), or ESCC (31.9%) cases.
Table 2 details the risk estimates for the associations between eating habits and risk of esophageal cancer. We found no evidence that those who ever drank hot tea or coffee had higher or lower risks of EGJAC or ESCC than those who did not after adjusting for confounders. Inclusion of income and PPI to the final model did not materially change the risk estimates. There was a suggestion of an elevated EAC risk among those who ever consumed hot tea or coffee but this is probably attributable to the very small number of EAC cases that never consumed hot tea or coffee. While the relative risks of esophageal cancer were not significantly different from the null with increasing temperature of consumption, the point estimates of risk for EAC and EGJAC were consistently less than one, and the linear trend analyses suggested a significant reduction in risk with increasing temperatures of beverage consumption for both of the adenocarcinoma subtypes. No such inverse trend was seen for ESCC. The number of cups of tea or coffee consumed per day was not associated with risk of esophageal cancers. When temperature at which tea or coffee was consumed was combined with the quantity consumed, there was no association between temperature and quantity of tea or coffee consumed and risks of esophageal cancers.
There was no association between the frequency of consumption of home-fried foods and risk of esophageal cancer. However, consuming ‘take-away’ fried foods once a week or more was associated with an increased risk of EGJAC (OR = 1.44, 95% CI: 1.01–2.05; p for trend = 0.04) compared to less than once a week. We reanalyzed the data stratifying by median age of the study population and found a positive association between fried ‘take-away’ foods and EGJAC in the older study participants with higher risk estimates (OR = 2.05, 95% CI = 1.12–3.76, p = 0.02); there was no such association in the younger age group.
In simple dichotomous analysis, we found no evidence that barbecued meat eaters had higher risks of EAC or EGJAC; however, the data suggested a decreased ESCC risk (OR = 0.58, 95% CI = 0.34–1.01; p value = 0.06) among those who ever consumed barbecued meat. Among barbecued meat consumers, neither frequency of consumption, nor preferred level of doneness of meat, nor frequency of consumption of meat and preferred level of doneness combined was associated with risk of esophageal cancers.
Frequency of consumption of ‘spicy’ foods, and the time at which the evening meal was eaten were not associated with risk of the esophageal cancers. Eating speed, however, was associated with ESCC risk: compared to slow eaters (last to finish eating), quick eaters (first to finish eating) had a decreased risk of ESCC (OR = 0.44; 95% CI = 0.28–0.72; p for trend = 0.001). The timing of eating an evening meal was not associated with esophageal cancer.
Discussion
In this large population-based case–control study, we found no evidence that drinking tea or coffee at very hot temperature was associated with increased risk of esophageal cancers. Results of studies from several populations including Iran [11], Taiwan [29], Turkey [30], China [31], India [19], England and Scotland [32], South America [9], Japan [33], and Greece [34] overwhelmingly show positive associations between drinking tea or coffee at very hot temperatures and ESCC, whereas studies from Sweden [12] did not find a positive association between drinking hot beverages and EAC, EGJAC, or ESCC risk. In populations where positive associations have been reported between temperature of tea or coffee and risk of esophageal cancer, the beverages are often consumed at ‘scalding’ temperatures, where the beverage is kept boiling. In contrast, in those populations where tea and coffee is allowed to cool before being consumed, or where cold milk is commonly added, null or inverse associations have been reported. Our results and those from other western populations suggest that the temperatures at which ‘hot’ beverages are generally consumed in these settings are not associated with an increase in esophageal cancer risk. In our study, the assessment of temperature at which hot beverages were normally consumed were based on self-reports only and are therefore subject to misclassification. However, we have no reason to believe that misclassification would be differential with regard to case–control status. We cannot exclude the possibility of reverse causality, however, whereby cases with esophageal cancer modified their dietary habits in the period before diagnosis (such as avoiding the use of very hot beverages, spicy foods, or other types of food that could cause irritation or pain at meal times).
In epidemiologic studies, high-temperature cooking methods including barbecuing have been associated with carcinogenic substances such as heterocyclic amines (HCA) and polycyclic aromatic hydrocarbons (PCAH) [35]. There is a paucity of data on barbecued meat intake, and very limited availability of HCA and PCAH databases that include a large number of different foods analyzed for their HCA and PCAH concentrations. As a result, reported frequencies of consumption of barbecued meats and ‘levels of doneness’ have often been the main methodology used to estimate the consumption of these carcinogens. Thus, comparing the range of consumption of barbecued meat as well as their HCA and PCAH content across populations is difficult. Our data suggested a lower risk of ESCC for those who ever (OR = 0.58, 95% CI = 0.34–1.01) compared to never consumed barbecued meat; however, we found no evidence that the frequency of consumption of barbecued meat or preferred level of ‘doneness’ was associated with esophageal cancer risk. We found no significant association between intake of BBQ meat and risk of EAC (OR = 0.74 (0.48–1.12), EGJAC (OR = 1.22 (0.85–1.77) or ESCC (OR = 0.99 (0.62–1.59). Earlier hospital-based case–control studies from Uruguay [17] and Argentina [16] found a twofold increased ESCC risk. Also, a pooled analysis of data from 5 hospital-based case–control studies from Argentina, Brazil, Paraguay, and Uruguay [9] found a slightly elevated but non-significant ESCC risk (OR = 1.22 (0.85–1.76) with daily intake of BBQ meat. Similarly, a population-based case–control study from the United States [18] found a non-significant elevated EAC risk (OR = 1.5 (0.5–4.8) with barbecuing as a cooking method. In that same US study there was no significant association for any combination of ‘doneness’ preference and beef intake, but high intake of gravy made with meat juices was associated with elevated EAC risk. Thus, from these studies, there is no strong overall evidence that consumption of barbecued meat is associated with increased risk of esophageal cancer risk. In our study, none of the respondents reported barbecued meat consumption on a daily basis. Almost 80% of our study population consumed barbecued meat less than weekly, and of these, more than half (46%) consumed barbecue meat less than once per month. Consumption of barbecued meat in Australia is commonly associated with social gatherings and group meals due to the seasonal nature of this activity. It is thus plausible that a reduced frequency of barbecued meat consumption and some unmeasured confounding by social factors may be associated with this null finding.
More frequent consumption of ‘take-away’ fried foods (but not foods fried at home) was associated with increased risk of EGJAC in our study population. This is consistent with the findings from several studies showing similar associations with fried foods [13, 36, 37] although previous studies did not indicate whether foods were fried within or outside of the home. However, another study failed to find an association between intake of fried potatoes and esophageal cancer risk [15]. Because our study population included participants as young as 18 years, we reanalyzed our data stratified by median age of the study population (<62 years, and ≥62 years). We found no evidence of an association between the dietary characteristics studied and the two histological types of esophageal cancer in the younger age group, while in the older participants, we found higher risk estimates for the association between fried ‘take-away’ foods and EGJAC in the older participants (OR = 2.05, 95% CI = 1.12–3.75; p value = 0.02). Interaction between frequency of consumption of fried ‘take-away’ foods and age in relation to EGJAC was significant (p for interaction = 0.01). Acrylamide, a toxic substance, produced during processing (baking, broiling, frying roasting) of foods as a result of heat induced reactions between amino group of free amino acids and the carbonyl group of reducing sugars has been implicated as a causative agent [38]. Foods rich in both of these precursors are largely derived from plant sources such as potatoes and cereals (barley, rice, and wheat) but not animal foods such as poultry beef and fish [38]. A recent study that investigated the association between ‘take-away’ food consumption and diet quality in Australia found that consumption of ‘take-away’ foods was associated with poorer diet quality and higher prevalence of obesity in men than women [39]. Thus, our findings may reflect residual confounding by other risk factors for esophageal adenocarcinoma including obesity and esophageal reflux symptoms, despite our attempts to control for such effects in the analysis. In our study we found a strong association between BMI and intake of fried ‘take-away’ foods among cases (p value = 0.007), and a weak association between esophageal reflux and intake of fried ‘take-away’ food (p value = 0.08). Among cases with reflux, those who were obese (42%) were more likely to eat fried ‘take-away’ food once a week or more than those with normal BMI (21%) (p value = 0.04). Among cases without reflux, no significant associations were found between intake of fried ‘take-away’ food and BMI (p value = 0.29).
We found no association between consumption of spicy foods and esophageal cancer risk. Reports from previous studies have been mixed. Similar to our finding, a case–control study from Taiwan found no significant association between spicy condiments and esophageal cancer risk [29], while a hospital-based case–control study from India [19], and a population-based case–control study from China limited only to men [40] reported positive associations. Excessive use of chilies and other hot spices is not common in Australia, and level of use of spicy foods may not be as high as would be found in China or India where positive associations have been reported. Ethnically, our study population was very homogeneous (96% of participants identified themselves as ‘White’) and thus the distribution of exposures such as consumption of spicy foods or temperature at which hot beverages are consumed would be expected to be narrower than regions with greater ethnic diversity. This may have limited our ability to identify true associations.
Our data suggested that ‘fast eaters’ have a 55% decreased risk of ESCC compared to ‘slow eaters’. This is in contrast to significant positive findings of a population-based case–control study of the association between fast eating and esophageal cancer risk in low (OR = 3.1) and high (OR = 4.0) esophageal cancer risk areas in China [21]. However, since neither study objectively measured the actual time taken to consume the meals, there is a possibility that the meaning of the term ‘fast’ eating within the context of each population can be interpreted differently. Also, we cannot verify whether possible early symptoms of esophageal cancer may have altered eating speed before cancer diagnosis, causing an apparent protective association of fast eating.
While we found no association between time of eating evening meal and risk of esophageal cancer, a prospective, randomized unblinded crossover trial of patients with symptomatic GERD and esophageal cancer from the United States reported a significant association between standardized late evening meal and increased supine reflux compared to when the same meal was consumed earlier in the day [20]. It is difficult to compare our result to this finding because the ‘standardized’ evening meal in that study comprised a ‘fast food’ or ‘take-away’ hamburger, French fries and soft drink, while for our study, the composition of an evening meal, which was not specified, would more likely be interpreted in the Australian context as a home cooked meal.
Our study has strengths and limitations. Strengths of the study include the population-based design, the large sample size, and the rapid recruitment of cases soon after diagnosis from across the country. Weaknesses include the retrospective and self-report nature of dietary data collection. Of particular concern is that early symptoms of esophageal cancer may have caused changes in eating behavior before diagnosis among the cases. However, we repeated our analyses in the subgroup that did not report a change in their diet and observed no material differences in results. Assessment of temperature at which tea or coffee are normally consumed was based on self-report only and could not be independently verified. We were unable to quantify the amounts of heterocyclic amines or other possible causal factors in the barbecued meats to enable a more accurate determination of the association between barbecued meats and esophageal cancers.
In conclusion, we examined several behavioral factors in relation to the two histological types of esophageal cancer in our population and found null results even after stratification by age. The only significant finding was a modest increase (OR = 1.44) in EGJAC risk in relation to the consumption of fried ‘take-away’ foods in analysis involving all participants and a larger increase (OR = 2.05) in analysis involving older participants. Owing to the fact that this is the only significant finding out of several null results, we contend that type 1 error is the most likely explanation for this finding. Thus, our results suggest that eating habits per se are unlikely to explain the recent changes in incidence of esophageal cancer in the Australian population. We found no evidence that consumption of hot drinks, barbecued meats, spicy foods or the timing of the evening meal are associated with increased risk of esophageal cancer in this Australian population. Associations with consumption of fried ‘take-away’ foods and eating speed await confirmation in future studies.
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, 2007, Washington
Gallus S, La Vecchia C (2007) Is there a link between diet and esophageal cancer? Nat Clin Pract Gastroenterol Hepatol 4:2–3
Holmes RS, Vaughan TL (2007) Epidemiology and pathogenesis of esophageal cancer. Semin Radiat Oncol 17:2–9
Chen X, Yang CS (2001) Esophageal adenocarcinoma: a review and perspectives on the mechanism of carcinogenesis and chemoprevention. Carcinogenesis 22(8):1119–1129
Lord RV, Law MG, Ward RL, Giles GG, Thomas RJ, Thursfield V (1998) Rising incidence of oesophageal adenocarcinoma in men in Australia. J Gastroenterol Hepatol 13(4):356–362
Thomas RJS, Lade S, Giles GG, Thursfield V (1996) Incidence trends in oesophageal and proximal gastric carcinoma in Victoria. Aust NZ J Surg 66(5):271–275
Stavrou EP, McElroy HJ, Baker DF, Smith G, Bishop JF (2009) Adenocarcinoma of the oesophagus: incidence and survival rates in New South Wales, 1972–2005. Med J Aust 191(6):310–314
Castellsague X, Munoz N, De Stefani E, Victora CG, Castelletto R, Rolon PA (2000) Influence of mate drinking, hot beverages and diet on esophageal cancer risk in South America. Int J Cancer 88(4):658–664
Mason JB, Dickstein A, Jacques PF, Haggarty P, Selhub J, Dallal G et al (2007) A temporal association between folic acid fortification and an increase in colorectal cancer rates may be illuminating important biological principles: a hypothesis. Cancer Epidemiol Biomarkers Prev 16(7):1325–1329
Islami F, Pourshams A, Nasrollahzadeh D, Kamangar F, Fahimi S, Shakeri R et al (2009) Tea drinking habits and oesophageal cancer in a high risk area in northern Iran: population based case–control study. BMJ 338:b929
Terry P, Lagergren J, Wolk A, Nyren O (2001) Drinking hot beverages is not associated with risk of oesophageal cancers in a Western population. Br J Cancer 84(1):120–121
Galeone C, Pelucchi C, Talamini R, Levi F, Bosetti C, Negri E et al (2005) Role of fried foods and oral/pharyngeal and oesophageal cancers. Br J Cancer 92(11):2065–2069
Abnett CC (2007) Carcinogenic food contaminants. Cancer Invest 25:189–196
Pelucchi C, Franceschi S, Levi F, Trichopoulos D, Bosetti C, Negri E et al (2003) Fried potatoes and human cancer. Int J Cancer 105(4):558–560
Castelleto R, Castellsague X, Munoz N, Iscovich J, Chopita N, Jmelnitsky A (1994) Alcohol, tobacco, diet, mate drinking, and esophageal cancer in Argentina. Cancer Epidemiol Biomarkers Prev 3:557–564
De Stefani E, Munoz N, Esteve J, Vasallo A, Victora CG, Teuchmann S (1990) Mate drinking, alcohol, tobacco, diet, and esophageal cancer in Uruguay. Cancer Res 50(2):426–431
Ward MH, Sinha R, Heineman EF, Rothman N, Markin R, Weisenburger DD et al (1997) Risk of adenocarcinoma of the stomach and esophagus with meat cooking method and doneness preference. Int J Cancer 71(1):14–19
Phukan RK, Chetia CK, Ali MS, Mahanta J (2001) Role of dietary habits in the development of esophageal cancer in Assam, the north-eastern region of India. Nutr Cancer 39(2):204–209
Piesman M, Hwang I, Maydonovitch C, Wong RK (2007) Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter? Am J Gastroenterol 102(10):2128–2134
Wu M, Zhao JK, Hu XS, Wang PH, Qin Y, Lu YC et al (2006) Association of smoking, alcohol drinking and dietary factors with esophageal cancer in high- and low-risk areas of Jiangsu Province, China. World J Gastroenterol 12(11):1686–1693
Whiteman DC, Sadeghi S, Pandeya N, Smithers BM, Gotley DC, Bain CJ et al (2008) Combined effects of obesity, acid reflux and smoking on the risk of adenocarcinomas of the oesophagus. Gut 57:173–180
Spechler SJ, Dixon MF, Genta R, Hainaut P, Lambert R, Siewert R (2000) Adenocarcinoma of the oesophago-gastric junction. In: Hamilton SR, Aaltonen LA (eds) Pathology and genetics Tumours of the digestive system WHO classification of tumours, vol 2, 3rd edn. IARC Press, Lyon
Willett W, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J et al (1985) Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 122:51–65
Ashton BA, Marks GC, Battistutta D, Green AC, The Nambour Study Group (1996) Under reporting of energy intake in two methods of dietary assessment in the Nambour trial. Aust J Nutr Diet 53:53–60
Marks GC, Hughes MC, van der Pols JC (2006) Relative validity of food intake estimates using a food frequency questionnaire is associated with sex, age, and other personal characteristics. J Nutr 136:459–465
McNaughton SA, Marks GC, Gaffney P, Williams G, Green AC (2005) Validation of a food-frequency questionnaire assessment of carotenoid and vitamin E intake using weighed food records and plasma biomarkers: the method of triads model. Eur J Clin Nutr 59:211–218
Food Standards Australia New Zealand (2007) NUTTAB 2006—Australian food composition tables. FSANZ, Canberra
Hung HC, Huang MC, Lee JM, Wu DC, Hsu HK, Wu MT (2004) Association between diet and esophageal cancer in Taiwan. J Gastroenterol Hepatol 19(6):632–637
Onuk MD, Oztopuz A, Memik F (2002) Risk factors for esophageal cancer in eastern Anatolia. Hepatogastroenterology 49:1290–1292
Ke L, Yu P, Zhang ZX, Huang SS, Huang G, Ma XH (2002) Congou tea drinking and oesophageal cancer in South China. Br J Cancer 86:346–347
Sharp L, Chilvers CE, Cheng KK, McKinney PA, Logan RF, Cook-Mozaffari P et al (2001) Risk factors for squamous cell carcinoma of the oesophagus in women: a case–control study. Br J Cancer 85:1667–1670
Kinjo Y, Cui Y, Akiba S, Watanabe S, Yamaguchi N, Sobue T et al (1998) Mortality risks of oesophageal cancer associated with hot tea, alcohol, tobacco and diet in Japan. J Epidemiol 8(4):235–243
Garidou A, Tzonou A, Lipworth L, Signorello LB, Kalapothaki V, Trichopoulos D (1996) Life-style factors and medical conditions in relation to esophageal cancer by histologic type in a low-risk population. Int J Cancer 68(3):295–299
Terry PD, Lagergren J, Wolk A, Steineck G, Nyren O (2003) Dietary intake of heterocyclic amines and cancers of the esophagus and gastric cardia. Cancer Epidemiol Biomarkers Prev 12(9):940–944
Takezaki T, Gao CM, Wu JZ, Ding JH, Liu YT, Zhang Y et al (2001) Dietary protective and risk factors for esophageal and stomach cancers in a low-epidemic area for stomach cancer in Jiangsu Province, China: comparison with those in a high-epidemic area. Jpn J Cancer Res 92:1157–1165
Gao YT, McLaughlin JK, Gridley G, Blot WJ, Ji BT, Dai Q et al (1994) Risk factors for esophageal cancer in Shanghai, China. II. Role of diet and nutrients. Int J Cancer 58(2):197–202
Friedman M, Levin CE (2008) Review of methods for the reduction of dietary content and toxicity of acrylamide. J Agric Food Chem 56(15):6113–6140
Smith KJ, McNaughton SA, Gall SL, Blizzard L, Dwyer T, Venn AJ (2009) Takeaway food consumption and its associations with diet quality and abdominal obesity: a cross-sectional study of young adults. Int J Behav Nutr Phys Act 6:29
Wang JM, Xu B, Rao JY, Shen HB, Xue HC, Jiang QW (2007) Diet habits, alcohol drinking, tobacco smoking, green tea drinking, and the risk of esophageal squamous cell carcinoma in the Chinese population. Eur J Gastroenterol Hepatol 19(2):171–176
Acknowledgments
We are grateful to the Matt Filson Research Fund for the additional funding provided to support this project. The Australian Cancer Study was supported by the National Health and Medical Research Council (NHMRC) of Australia (Program no.199600). DCW is supported by a Principal Research Fellowship from the NHMRC of Australia.
Conflict of interest statement
None of the authors had a personal or financial conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix: The Australian Cancer Study Investigators
Appendix: The Australian Cancer Study Investigators
Investigators: David C. Whiteman MBBS, PhD, Penelope M. Webb MA, D Phil, Adele C. Green MBBS, PhD, Nicholas K. Hayward PhD, Peter G. Parsons PhD, David M. Purdie PhD.
Clinicalcollaborators: B. Mark Smithers FRACS, David Gotley FRACS PhD, Andrew Clouston FRACP PhD, Ian Brown FRACP.
ProjectManager: Suzanne Moore RN, MPH.
Database: Karen Harrap BIT, Troy Sadkowski BIT.
ResearchNurses: Suzanne O’Brien RN MPH, Ellen Minehan RN, Deborah Roffe RN, Sue O’Keefe RN, Suzanne Lipshut RN, Gabby Connor RN, Hayley Berry RN, Frances Walker RN, Teresa Barnes RN, Janine Thomas RN, Linda Terry RN MPH, Michael Connard B Sc, Leanne Bowes B Sc, MaryRose Malt RN, Jo White RN.
Clinical contributors
Australian Capital Territory: Charles Mosse FRACS, Noel Tait FRACS.
New South Wales: Chris Bambach FRACS, Andrew Biankan FRACS, Roy Brancatisano FRACS, Max Coleman FRACS, Michael Cox FRACS, Stephen Deane FRACS, Gregory L. Falk FRACS, James Gallagher FRACS, Mike Hollands FRACS, Tom Hugh FRACS, David Hunt FRACS, John Jorgensen FRACS, Christopher Martin FRACS, Mark Richardson FRACS, Garrett Smith FRACS, Ross Smith FRACS, David Storey FRACS.
Queensland: John Avramovic FRACS, John Croese FRACP, Justin D’Arcy FRACS, Stephen Fairley FRACP, John Hansen FRACS, John Masson FRACP, Les Nathanson FRACS, Barry O’Loughlin FRACS, Leigh Rutherford FRACS, Richard Turner FRACS, Morgan Windsor FRACS.
SouthAustralia: Justin Bessell FRACS, Peter Devitt FRACS, Glyn Jamieson FRACS, David Watson FRACS.
Victoria: Stephen Blamey FRACS, Alex Boussioutas FRACP, Richard Cade FRACS, Gary Crosthwaite FRACS, Ian Faragher FRACS, John Gribbin FRACS, Geoff Hebbard FRACP, George Kiroff FRACS, Bruce Mann FRACS, Bob Millar FRACS, Paul O’Brien FRACS, Robert Thomas FRACS, Simon Wood FRACS.
WesternAustralia: Steve Archer FRACS, Kingsley Faulkner FRACS, Jeff Hamdorf FRACS.
Rights and permissions
About this article
Cite this article
Ibiebele, T.I., Taylor, A.R., Whiteman, D.C. et al. Eating habits and risk of esophageal cancers: a population-based case–control study. Cancer Causes Control 21, 1475–1484 (2010). https://doi.org/10.1007/s10552-010-9576-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9576-8