Abstract
Descriptive studies of pancreatic cancer incidence have been sparse particularly in terms of tumor histology and stage. The purpose of this study was to examine the incidence rate trends of exocrine and endocrine pancreatic cancers by demographic and tumor characteristics using data from the Surveillance, Epidemiology, and End Results (SEER) program from 1977 to 2005. During this period, the incidence of exocrine pancreatic cancer generally decreased whereas the incidence of endocrine pancreatic cancer increased. This difference in trends by histology was evident across age, gender, and racial groups. It was also evident among different racial/ethnic groups using data from 1992 to 2005. Variation in trends was observed by stage. The incidence of exocrine cancers declined for all stages except regional. Endocrine cancer incidence increased for all tumor stages, and the increase was most prominent for localized tumors. When exocrine tumors were stratified by tumor subsite, the incidence of cancers in the tail and body regions increased while the incidence in other regions decreased. While better detection and classification of tumors through improved diagnostic procedures may be related to these changing trends, etiologic factors warrant study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is among the most fatal of all major epithelial cancers with an incidence rate that approximates its mortality rate [1]. In 2009, the American Cancer Society estimated that 42,470 new patients were diagnosed with and 35,240 deaths resulted from pancreatic cancer in the U.S., making it the 4th leading cause of cancer mortality among both sexes [2]. Pancreatic cancer is often asymptomatic, especially for early-stage tumors, and there is no established population-based screening method. As a result, less than 10% of pancreatic cancers are detected during the early potentially curable stage of disease and the overall 5-year survival rate is only about 5% [2].
The incidence of pancreatic cancer varies by demographic characteristics. Pancreatic cancer occurs predominantly among the elderly; the median age at diagnosis occurs in the seventh decade [3]. The incidence rate of pancreatic cancer is approximately 30% higher among men than women and 50% higher among blacks than whites and people of other races [2, 4]. Age-adjusted incidence rates appear to be declining, more so for men than women [5].
Although the observed decreases in incidence are encouraging, it is important to note that pancreatic cancer represents a heterogeneous disease with two general categories: exocrine ductal epithelial adenocarcinoma and islet cell or endocrine cancer. These two histologic types have distinctly different biology, clinical presentation and natural history, and therefore may display different epidemiological distributions. Exocrine pancreatic cancer constitutes the majority (>95%) of pancreatic malignancy [6]; therefore, when studied together, trends in exocrine pancreatic cancer incidence may mask differential trends in endocrine pancreatic cancer incidence. Although epidemiological studies have found increasing rates of pancreatic endocrine cancer [7–11], none have investigated histology-specific trends by race/ethnicity, tumor stage at diagnosis and tumor subsite, which may provide insights into the etiology of the observed trends. To address these issues, we conducted a more in-depth analysis of pancreatic cancer incidence trends from 1977 to 2005, using data from the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute. We investigated temporal trends in histology-specific incidence rates overall and stratified by age, gender, race/ethnicity, stage at diagnosis, and tumor subsite.
Materials and methods
Data were derived from the National Cancer Institute’s SEER program. The SEER program began collecting data in the early 1970s from nine population-based registries: Connecticut, Iowa, New Mexico, Utah, Hawaii, and the metropolitan areas of Detroit, San Francisco-Oakland, Atlanta, and Seattle-Puget Sound (SEER-9) [12]. These registries represent approximately 10% of the total United States population. In 1992, the SEER program was expanded to increase the coverage of minority populations, especially Hispanics, by adding four registries: San Jose-Monterey, Los Angeles, rural Georgia, and Alaskan Natives (SEER-13), amounting to a representation of about 14% of the U.S. population. Race was determined from medical records and registration information, and Hispanic ancestry was determined using algorithms that identify Spanish surnames [13]. Our analysis included data available for the racial categories of white, black and other (American Indian/Alaskan Native and Asian/Pacific Islander) since the early years of the SEER-9 registries. Non-Hispanic white, Hispanic white, non-Hispanic black, and Asian/Pacific Islander (API) were included in the analysis using data from the SEER-11 registries (SEER-13 registries excluding the Alaska Native and rural Georgia registries since these two registries included relatively few APIs or Hispanics). Analyses of Hispanic blacks and Hispanic APIs were not conducted due to insufficient numbers.
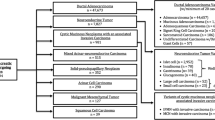
The SEER program coded tumor site and histology according to the International Classification of Diseases for Oncology (ICD-O) since 1977 [14]. Incident cases diagnosed between 1992 and 2000 were classified according to the second edition (ICD-O-2) [15], and cases diagnosed after 2000 were classified according to the third edition (ICD-O-3) [16]. All cases diagnosed before 2001 were converted to ICD-O-3. The SEER program coded histologic type using the Manual of Tumor Nomenclature between 1973 and 1976; and many of these codes cannot be updated to an ICD-O-3 code [17]. Therefore, we excluded data collected prior to 1977. All malignant tumors of the pancreas with the ICD-O-3 site codes C250–C254 and C257–C259 were included in the analysis; 75% were microscopically confirmed. Pancreatic cancers were further divided into two groups based on ICD-O-3 histology codes: (a) exocrine pancreatic cancer (8000–8149, 8156–8239, 8247–9970) and (b) endocrine pancreatic cancer (8150–8155, 8240–8246) [6]. Tumor stage at diagnosis was based on the general summary stage variable (localized, regional, distant, and unstaged) recorded by the SEER program. A localized cancer was defined as a malignancy limited to the organ of origin; distant metastases were defined when cancer cells had broken away from the primary tumor, had travelled to other parts of the body, and had begun to grow at the new location. Regional stage was defined as a tumor that extended beyond the limits of the organ of origin but had not metastasized [18].
We used SEER*Stat (version 6.3.6) software to obtain age-standardized incidence rates (calculated as the number of new cases per 100,000 person-years) adjusted to the 2000 U.S. standard population. The majority of pancreatic cases occur after the age of 60 [5], and early onset cancers are more likely to be related to a positive family history; therefore, histology-specific incidence rates were computed for persons <60 and ≥60 years of age, respectively. Analyses were also conducted stratified by gender, race/ethnicity, stage at diagnosis, and tumor subsite. Where sufficient numbers were available, analyses were conducted stratified by multiple characteristics simultaneously.
In trend analysis, year of diagnosis was grouped into six calendar-year categories (1977–1981, 1982–1986, 1987–1991, 1992–1996, 1997–2001, 2002–2005) for the long-term period (SEER-9) and three calendar-year categories (1992–1996, 1997–2001, 2002–2005) for the short-term period (SEER-11). Incidence rates were calculated when there were at least ten cases in a given age, gender, race/ethnicity, tumor stage, tumor subsite, or time category, and trend lines were plotted if at least two consecutive categories met this criterion. Incidence trends were plotted using semi-logarithmic plots so that rates of change could be compared [19]. The percent changes between the first and last calendar-year categories were calculated as were odds ratios (ORs) and 95% confidence intervals (CIs) comparing the incidence rates by age, gender, race/ethnicity, tumor stage at diagnosis, and tumor subsite.
Results
Age-standardized incidence rates of exocrine and endocrine pancreatic cancers by age, gender, and race/ethnicity for the long-term period and short-term period are presented in Tables 1 and 2, respectively. Exocrine cancer accounted for the majority (97%) of the pancreatic cancers. The incidence rates of exocrine and endocrine pancreatic cancers increased significantly with age; incidence rates among older adults (≥60) were 14–28 times higher for exocrine cancer and 3–8 times higher for endocrine cancer than that among younger adults (p-values < 0.01). The incidence of exocrine cancer was generally higher among men than women across racial/ethnic groups, especially among those aged <60 (ORs ranged 1.1–1.7; p-values < 0.01). However, there was no gender difference in the incidence of exocrine cancer among older non-Hispanic blacks or Hispanic whites (Table 2). Additionally, exocrine cancer rates were significantly higher among blacks than whites and other races (ORs ranged 1.4–2.1, p-values < 0.01; Table 1); and higher among non-Hispanic blacks than non-Hispanic whites, Hispanic whites, and APIs (ORs ranged 1.3–2.3, p-values < 0.01; Table 2). Gender and racial differences were less consistent for endocrine cancer.
Sex and age-specific time trends
For both the long-term and short-term periods, the incidence rates for exocrine pancreatic cancer tended to decrease over time, whereas the incidence rates for endocrine pancreatic cancer increased (Fig. 1). From 1977–1981 to 2002–2005, the incidence rate for exocrine cancer decreased about 19% among men and 5% among women while rates for endocrine cancer rose about 106% among men and 125% among women (p-values < 0.05).
From 1977–1981 to 2002–2005, the incidence of exocrine cancer decreased about 11% in both age groups (p-values < 0.01, Fig. 1). The incidence rates of endocrine cancer rose 90% for younger adults and 149% for older adults (p-values < 0.01). When age comparisons were further stratified by race/ethnicity, similar findings were found among whites and non-Hispanic whites, which were the only two groups with sufficient numbers to conduct the analyses (data not shown).
Race/ethnicity-specific time trends
Slight decreases in the incidence of exocrine cancer and increases in the incidence of endocrine cancer were also observed when trends were stratified by race/ethnicity (Fig. 2). For example, among whites from 1977–1981 to 2002–2005, the incidence rate of exocrine cancer decreased 11% while the rate of endocrine cancer rose 138% (p-values < 0.01); among blacks, the incidence rate of exocrine cancer decreased 17% (p-value < 0.01) and the rate of endocrine cancer increased 50% (p-value = 0.16). From 1992–1996 to 2002–2005, the greatest changes were observed among non-Hispanic blacks where the incidence of exocrine cancer decreased 14% and the incidence of endocrine cancer increased 175% (p-values < 0.01). In comparison, among the other racial/ethnic groups less dramatic changes were observed for exocrine (decreased 0.2–3%) and endocrine cancers (increased 43–57%).
Stage-specific time trends
The most common tumor stage at diagnosis was distant (exocrine: 50%, endocrine: 62%), followed by regional stage (exocrine: 23%; endocrine: 20%, Fig. 3). Variation in trends by stage was observed among exocrine cancer. The incidence rates of localized and distant stage exocrine cancers decreased from 1977–1981 to 1987–1991 (−42 and −12%, p-values < 0.01) and then stabilized. In contrast, the incidence rate of unstaged exocrine cancer increased from 1977–1981 to 1987–1991 (23%, p-value < 0.01) and then decreased thereafter (−48%, p-value < 0.01). Additionally, regional stage exocrine cancer rose 32% from 1977–1981 to 2002–2005 (p-value < 0.01). Further analyses confined to each racial/ethnic group showed similar patterns for exocrine cancer (data not shown). Increases in the incidence rate of endocrine cancer were observed regardless of stage; however, the increase was most prominent for localized tumors. The incidence of localized endocrine cancer rose 400% (p-value < 0.01) from 1977–1981 to 2002–2005. In comparison, the increase in the incidence rate of regional stage (25%; p-value = 0.09) and distant stage (137%; p-value < 0.01) was less dramatic. No consistent trends were observed for unstaged endocrine cancer. Further analyses stratified by race/ethnicity were not conducted due to insufficient numbers of endocrine cancer.
Exocrine subsite-specific time trends
Variation in trends was observed when exocrine tumors were stratified by tumor subsite (Fig. 4). Over the long-time period incidence rates of exocrine cancer decreased for the head region (men: −17%, p-value < 0.01; women: −2%, p-value = 0.63), overlapping regions (men: −42%; women: −32%, p-values < 0.01), and unspecified regions (men: −38%, women: −23%, p-values < 0.01), but the incidence increased for the tail region (men: 69%, women: 68%, p-values < 0.01). Incidence rates for the body region decreased until about early 1990s (men: −21%, p-value < 0.01, women: −10%, p-value = 0.21), and then increased starting in 1997–2001 among men and starting in 1992–1996 among women (26 and 32%, respectively, p-values < 0.05). Similar patterns were observed when stratified by age and race (data not shown). Variations in incidence rates were observed for these subsites when the analyses were further stratified by stage at diagnosis. Incidence rates of tumors in the tail region increased for localized, regional, and distant stages over the whole period (150, 100, and 73%, respectively, p-values < 0.01), but decreased for unstaged tumors (−33%, p-value = 0.33). Similarly, since the early 1990s the incidence rates of tumors in the body region also increased for localized, regional, and distant stages (17, 73, and 31%, respectively, p-values < 0.01), and decreased for the unstaged tumors (−57%, p-value < 0.01). Incidence rates for the tumors in overlapping regions and unspecified regions generally decreased for all stages; and incidence rates for the tumors in the head region increased for the regional and distant stages and decreased for the localized and unstaged tumors. Analyses among other subsites of the exocrine pancreatic cancer (pancreatic duct, islets of langerhans, other specified parts of pancreas) and on endocrine cancer were not conducted due to insufficient numbers.
Discussion
This study found that time trends in pancreatic cancer incidence varied by histologic type. The incidence rates of exocrine pancreatic cancer generally decreased overtime, whereas the incidence rates of endocrine pancreatic cancer increased. These trends were consistently observed when stratified by age, gender, and race/ethnicity. The decrease in the incidence of exocrine cancer was stage- subsite- and time-dependent. Decreases in disease incidence were observed during early years for localized and distant stage tumors and during later years for unstaged tumors, whereas increases in incidence were observed for regional tumors across all years studied. Decreasing trends were observed for the head, overlapping, and unspecified regions, but increasing trends were observed for the tail region over the whole study period and for the body region since early 1990s. For endocrine cancer, the increasing incidence trends were observed among all stages of disease; however, the increase was most prominent for localized tumors.
Until now, only a few studies have evaluated time trends in pancreatic cancer incidence in the United States [4, 5, 7–9]. Our study adds to the existing published SEER data. Zhang et. al. [5] reported an overall decreasing trend in pancreatic cancer incidence for both men and women. Shaib et. al. [4] found that the proportion of localized tumors decreased whereas regional tumors increased and metastatic disease remained relatively stable from 1977–1981 to 1997–2001. However, these two previous studies did not investigate the trends for exocrine or endocrine cancers separately. The incidence trends for exocrine cancer observed in the current study, which accounted for about 97% of all pancreatic cancer cases, were similar to these previous findings and the overall decreases were shown to be consistent across age, gender, and racial/ethnic groups. Additionally, although the increasing incidence of endocrine cancer has previously been observed in the United States [7–9] and Europe [10, 11], our results demonstrated that the increases occur across different demographic groups and tumor stages.
Secular trends in cancer incidence may be affected by multiple factors, including improvements in cancer detection and diagnosis, classification accuracy, and changes in the exposure to risk factors. The changes in disease incidence likely reflect the combined impact of these factors. Improvements in detection and diagnosis may have influenced the incidence of pancreatic cancer. The diagnosis of pancreatic cancer is more difficult than other digestive tract cancers since the pancreas is not easily accessible [20]. The increased use of cross-sectional imaging (CT and MRI) and endoscopic ultrasound (EUS) over the past two decades have contributed to improved detection and diagnostic accuracy of pancreatic cancer [21, 22].
The impact of diagnostic technological advances on the overall incidence of pancreatic cancer may have varied according to histologic type. The introduction of EUS-guided fine needle aspiration (FNA) biopsy and multi-detector spiral CT likely accounted for better diagnostic accuracy resulting in the decreased incidence of unstaged exocrine cancer since the 1990s [23, 24]. Therefore, while the overall rates of exocrine cancer might have declined due to decreased exposure to risk factors, such as smoking as described below, the inclusion of previously unstaged tumors in a known stage category might have resulted in the stabilization of an earlier decline or a slight increase in incidence within the known stage categories. For endocrine cancer, the biggest impact of the technological advances might have been the improved detection. Non-functional endocrine tumors are harder to diagnose than functional tumors because they are not associated with a distinct clinical syndrome [25], but the widespread use of medical imaging has led to an increase in their incidental detection. A recent study demonstrated that 88% of non-functioning pancreatic endocrine tumors were detected incidentally by imaging [21]. Another study identified a high proportion (19%) of incidental pancreatic lesions as endocrine tumors; 63% were localized [26]. Additionally, functional endocrine cancers often are small; thereby the increased use of imaging and improvements in pathological diagnosis (e.g., immunohistochemistry) may have led to improved detection and diagnosis of early-stage tumors [25, 27].
The impact of improved diagnostic procedures may also have varied by tumor subsite. Early diagnosis of tumors in the body and tail regions has historically been more difficult since physical examination and blood test results are often normal, and they do not cause obstructive jaundice like tumors occurring in the head region [28]. Thus, in the past, at the time of diagnosis tumors that originated in the body and tail regions may have already spread to other pancreatic regions or metastasized [28]. Therefore, advanced imaging may have improved the early detection of tumors in the body and tail regions thereby increasing their incidence while decreasing the incidence of tumors in overlapping and/or unspecified regions.
The magnitude of the effects of improved technologies may have also varied by histologic type. The number of endocrine cancer is relatively small (<5% of all pancreatic cancers); therefore, increased detection through improved diagnostic capability would manifest in a relatively greater percentage change in the incidence rate for endocrine cancer than for exocrine cancer.
Accurate differentiation between endocrine and exocrine cancer can now be achieved using improved diagnostic tools, such as the percutaneous core and EUS-guided FNA biopsy [23, 29–31]. As clinicians and pathologists were more familiar with the more common exocrine than non-functional endocrine cancer, in the past they might have been more likely to arrive at a diagnosis of exocrine cancer [25]. But now with improved diagnostic modalities, and increasing awareness of and familiarity with both diseases, an increased proportion of endocrine tumors, particularly non-functional endocrine tumors, are being correctly diagnosed. Such relatively recent advances in pancreatic oncology could partly explain the increased incidence of endocrine cancer.
The change in observed incidence of endocrine cancer may also have been affected by diagnostic criteria. It is well known that the diagnosis of endocrine cancer is challenging [32]. Recently, a new WHO classification system for endocrine (or neuroendocrine) cancer has been developed based on a series of histopathological and biological characteristics [33]. This classification enables endocrine cancer to be diagnosed more accurately [32] and therefore may have increased the incidence rates of endocrine cancer.
Our knowledge about the risk factors for pancreatic cancer is generally limited particularly for endocrine cancer [20, 34]. Cigarette smoking is the only risk factor that has been consistently shown to increase the risk of pancreatic cancer, accounting for about 25% of the cases [20]. The increased risk is about twofold when smokers were compared to non-smokers [35, 36]. In the United States, cigarette smoking among persons 18 years of age or older rose rapidly from the 1930s to the 1950s, peaked in the early 1960s, and started to decline since the early 1970s [37]. The prevalence of smoking dropped more rapidly among men than women. Our findings of decreasing incidence trends in exocrine pancreatic cancer, which again represents the majority of pancreatic cases, paralleled the decreasing overall and gender-specific smoking trends, with a possible lag of several years. This may at least partially explain why the incidence of exocrine cancer decreased. Studies have also suggested possible associations between pancreatic cancer and other factors such as dietary factors and obesity [20, 38, 39]. It is unclear whether these factors were related to the trends in pancreatic cancer incidence. The impact of risk exposures on the incidence of endocrine cancer is difficult to infer because few studies have specifically investigated risk factors for this histologic type [20, 34].
Our results on age, gender, and racial differences for the overall incident rates of pancreatic cancer are consistent with previous studies [4]. Demographic characteristics are complex variables, implying possible differences in the exposure to many potential risk factors. Older people, men, and blacks may be more likely to be exposed to some risk factors than younger people, women, and other racial groups. Genetic background may also play a key role. For example, in comparison with whites, blacks are more likely to have K-ras mutations, which may be related to pancreatic cancer [40].
One potential limitation of the study is that 25% of the diagnosed cancers were microscopically unconfirmed. These patients were not excluded from the study because non-microscopic methods are usually sufficient for the diagnostic confirmation of pancreatic cancer [28, 41]. Nevertheless, we do not rule out possible misdiagnoses among patients without microscopic confirmation [42]. Our analysis showed that only 2% of endocrine tumors were not microscopically confirmed while the proportion was 25% for exocrine cancers. Therefore, the possible impact of misdiagnosis might be minimal for endocrine cancer and more substantial for exocrine cancer. However, most exocrine tumors are aggressive and can be diagnosed accurately even without microscopic confirmation [28]. Another limitation of the study was small sample size, especially for endocrine cancer, which limited the ability to study incidence trends by functional and non-functional cancers separately and by multiple demographic factors and tumor characteristics simultaneously.
In conclusion, this study found differences in epidemiological patterns between exocrine and endocrine cancers of the pancreas in the United States. While better detection and classification of tumors through improved diagnostic procedures may be related to the changing trends, other etiologic factors warrant further study.
References
Dunphy EP (2008) Pancreatic cancer: a review and update. Clin J Oncol Nurs 12(5):735–741
American Cancer Society (2009) Cancer facts & figures. American Cancer Society, Atlanta
Ries LAG, Melbert D, Krapcho M et al (1975–2005) SEER cancer statistics review. National Cancer Institute, Bethesda
Shaib YH, Davila JA, El-Serag HB (2006) The epidemiology of pancreatic cancer in the United States: changes below the surface. Aliment Pharmacol Ther 24(1):87–94
Zhang J, Dhakal I, Yan H, Phillips M, Kesteloot H (2007) Trends in pancreatic cancer incidence in nine SEER cancer registries, 1973–2002. Ann Oncol 18(7):1268–1279
Key C (2007) Chapter 7: cancer of the pancreas. In: Ries LAG, Keel GE, Eisner MP, Lin YD, Horner M-J (eds). SEER survival monograph: cancer survival among adults: US SEER Program, 1988–2001, patient and tumor characteristics. National Cancer Institute, SEER Program, NIH Pub. No. 07-6215, Bethesda, MD
Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ (2008) Changing incidence of pancreatic neoplasms: a 16-year review of statewide tumor registry. Pancreas 37(2):134–138
Halfdanarson TR, Rabe KG, Rubin J, Petersen GM (2008) Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol 19(10):1727–1733
Modlin IM, Lye KD, Kidd M (2003) A 5-decade analysis of 13, 715 carcinoid tumors. Cancer 97(4):934–959
Lepage C, Bouvier AM, Phelip JM, Hatem C, Vernet C, Faivre J (2004) Incidence and management of malignant digestive endocrine tumours in a well defined French population. Gut 53(4):549–553
Hemminki K, Li X (2001) Incidence trends and risk factors of carcinoid tumors: a nationwide epidemiologic study from Sweden. Cancer 92(8):2204–2210
Surveillance Epidemiology and End Results (SEER) Program. Available from http://www.seer.cancer.gov
Bach PB, Guadagnoli E, Schrag D, Schussler N, Warren JL (2002) Patient demographic and socioeconomic characteristics in the SEER-Medicare database applications and limitations. Med Care 40(8 Suppl):IV-19–IV-25
World Health Organization (1976) International classification of diseases for oncology. World Health Organization, Geneva
Percy C, Van Holten V, Muir C (1990) International classification of diseases for oncology, 2nd edn. World Health Organization, Geneva
Fritz AP, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (2000) International classification of diseases for oncology, 3rd edn. World Health Organization, Geneva
American Cancer Society (1951) Manual of tumor nomenclature. American Cancer Society, New York
SEER coding and staging manuals. Available from http://seer.cancer.gov/tools/codingmanuals/
Devesa SS, Donaldson J, Fears T (1995) Graphical presentation of trends in rates. Am J Epidemiol 141(4):300–304
Lowenfels AB, Maisonneuve P (2004) Epidemiology and prevention of pancreatic cancer. Jpn J Clin Oncol 34(5):238–244
Vagefi PA, Razo O, Deshpande V et al (2007) Evolving patterns in the detection and outcomes of pancreatic neuroendocrine neoplasms: the Massachusetts General Hospital experience from 1977 to 2005. Arch Surg 142(4):347–354
Fitzgerald TL, Smith AJ, Ryan M et al (2003) Surgical treatment of incidentally identified pancreatic masses. Can J Surg 46(6):413–418
Saftoiu A, Vilmann P (2009) Role of endoscopic ultrasound in the diagnosis and staging of pancreatic cancer. J Clin Ultrasound 37(1):1–17
Agarwal B, Abu-Hamda E, Molke KL, Correa AM, Ho L (2004) Endoscopic ultrasound-guided fine needle aspiration and multidetector spiral CT in the diagnosis of pancreatic cancer. Am J Gastroenterol 99(5):844–850
Oberg K, Eriksson B (2005) Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol 19(5):753–781
Bruzoni M, Johnston E, Sasson AR (2008) Pancreatic incidentalomas: clinical and pathologic spectrum. Am J Surg 195(3):329–332 (discussion 332)
Noone TC, Hosey J, Firat Z, Semelka RC (2005) Imaging and localization of islet-cell tumours of the pancreas on CT and MRI. Best Pract Res Clin Endocrinol Metab 19(2):195–211
Freelove R, Walling AD (2006) Pancreatic cancer: diagnosis and management. Am Fam Physician 73(3):485–492
Chatzipantelis P, Salla C, Konstantinou P, Karoumpalis I, Sakellariou S, Doumani I (2008) Endoscopic ultrasound-guided fine-needle aspiration cytology of pancreatic neuroendocrine tumors: a study of 48 cases. Cancer 114(4):255–262
Karlson BM, Forsman CA, Wilander E et al (1996) Efficiency of percutaneous core biopsy in pancreatic tumor diagnosis. Surgery 120(1):75–79
Amin Z, Theis B, Russell RC, House C, Novelli M, Lees WR (2006) Diagnosing pancreatic cancer: the role of percutaneous biopsy and CT. Clin Radiol 61(12):996–1002
Bajetta E, Catena L, Procopio G et al (2005) Is the new WHO classification of neuroendocrine tumours useful for selecting an appropriate treatment? Ann Oncol 16(8):1374–1380
Solcia E, Kloppel G, Sobin LH et al (eds) (2000) Histologic typing of endocrine tumours. WHO International Histological Classification of Tumours. Springer-Verlag, New York
Capurso G, Falconi M, Panzuto F et al (2009) Risk factors for sporadic pancreatic endocrine tumors: a case-control study of prospectively evaluated patients. Am J Gastroenterol 104(12):3034–3041
Silverman DT, Dunn JA, Hoover RN et al (1994) Cigarette smoking and pancreas cancer: a case-control study based on direct interviews. J Natl Cancer Inst 86(20):1510–1516
Boyle P, Maisonneuve P, Bueno de Mesquita B et al (1996) Cigarette smoking and pancreas cancer: a case control study of the search programme of the IARC. Int J Cancer 67(1):63–71
Garfinkel L (1997) Trends in cigarette smoking in the United States. Prev Med 26(4):447–450
Yeo TP, Hruban RH, Leach SD et al (2002) Pancreatic cancer. Curr Probl Cancer 26(4):176–275
Lowenfels AB, Maisonneuve P (2006) Epidemiology and risk factors for pancreatic cancer. Best Pract Res Clin Gastroenterol 20(2):197–209
Pernick NL, Sarkar FH, Philip PA et al (2003) Clinicopathologic analysis of pancreatic adenocarcinoma in African Americans and Caucasians. Pancreas 26(1):28–32
Branum GD, Pappas TN, Meyers WC (1995) The use of pancreatic ductoscopy in the operative management of benign and malignant pancreatic disorders. Surg Endosc 9(1):53–55
Porta M, Malats N, Pinol JL, Rifa J, Andreu M, Real FX (1994) Diagnostic certainty and potential for misclassification in exocrine pancreatic cancer. PANKRAS I Project Investigations. J Clin Epidemiol 47(9):1069–1079
Acknowledgements
This research was supported by the United States Military Cancer Institute via the Uniformed Services University of the Health Sciences under the auspices of the Henry M. Jackson Fundation for the Advancement of Military Medicine.
Author information
Authors and Affiliations
Corresponding author
Additional information
The opinions and assertions contained in this article represent the private views of the authors and do not reflect the official views of the United States Department of the Army, Navy, or Defense, National Cancer Institute, or United States Government.
An erratum to this article is available at http://dx.doi.org/10.1007/s10552-011-9816-6.
Rights and permissions
About this article
Cite this article
Zhou, J., Enewold, L., Stojadinovic, A. et al. Incidence rates of exocrine and endocrine pancreatic cancers in the United States. Cancer Causes Control 21, 853–861 (2010). https://doi.org/10.1007/s10552-010-9512-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9512-y