Abstract
To identify etiological connections of lung cancer in Chinese women in Hong Kong, who are among the highest in lung cancer incidence and mortality, we conducted a case–control study, in which 279 female lung cancer cases and 322 controls were selected and frequency matched. A variety of information, including dietary habits, occupational history, smoking, domestic environmental exposures, and family history of cancer was collected, and their associations with lung cancer were analyzed with logistic analysis approach. In addition to positive associations with exposures to cooking emissions and to radon at home, smoking and family cancer history, we observed that increasing consumption of meat was linked to a higher risk, whereas consumptions of vegetables had a strong protective effect against lung cancer. Moderate consumption of coffee appeared to be beneficial against the disease. Those never employed and domestic helpers were at a higher risk. The results indicated that environmental exposures, risky personal behaviors, or lifestyle, as well as family cancer aggregation are among important contributors to the high incidence of lung cancer in Hong Kong females.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is a leading cause of cancer mortality in Hong Kong women, accounting for about one-third of cancer deaths [1]. Its age standardized incidence rate reached the highest around the world in the early 1990s [2] and was only surpassed by US females in 2000 [3]. Apart from Hong Kong, the high incidence and mortality rate were also reported among Chinese women living in mainland China [4], as well as in other countries [5–7], indicating a consistent result in this ethnic group.
A number of epidemiological studies were conducted to explore possible causation of lung cancer, in which cigarette smoking was found to be a major culprit in Chinese men [8]. However, smoking cannot adequately explain the high incidence in Chinese females, due to the fact that smoking in Chinese women in Hong Kong and in mainland was so uncommon, ranging from 3 to 5% [9]. Obviously, there are some other known and unknown risk factors that could be responsible for the excess risk among the population.
Lung cancer is a multifactor-causing disease, which may be related to both environmental exposures and genetic factors. To gain a more complete understanding about the risk factors for lung cancer and provide a sensible explanation for the high risk among this ethnic population, we conducted a population-based case–control study in Hong Kong Chinese women, in which a variety of factors was examined, including environmental exposures, dietary factors, family cancer history, occupations, as well as active and passive smoking. In our previous data analysis using the same database, we evaluated the effects of exposure to cooking emissions and smoking on lung cancer [10, 11], both of which were found to be potent risk factors in these women. In another recent report [12], we determined the associations of previous lung diseases and family cancer history with the occurrence of lung cancer. In the present analysis, we attempt to provide an overall picture of risk factors in the population using integrated data covering a wide range of variables including occupations and detailed dietary factors, which has been rarely done in addressing etiological issues of lung cancer in Hong Kong population.
Subjects and methods
The study was approved by the ethics committees of both the Chinese University of Hong Kong and Queen Elizabeth Hospital. Details of subject selection were described elsewhere [10]. Briefly, a total of 279 female patients aged 30–79 years were recruited from the largest oncology center in Hong Kong, with the criteria of newly diagnosed primary carcinomas of the lung (International Classification of Disease, Ninth Revision code 162) from 1 July 2002 to 30 June 2004. The cancer cases were confirmed histologically according to the WHO histological typing of lung tumors [13]. At the same time, 322 control subjects were selected from the same residential areas from which the cases were selected. The controls had no history of physician-diagnosed cancer at any site and were frequency-matched to the cases in 10-year age groups.
Data collection
Person-to-person interview was administered using standardized questionnaire in local dialect. The collected information included detailed active smoking history, environmental tobacco smoking (ETS) exposures at home and at workplace, cooking practices since childhood, residential radon exposure, family cancer history, dietary habits, occupations and education level.
Smoker was defined as one who had ever smoked more than 20 packs of cigarettes in lifetime, or more than one cigarette a day, or more than one cigar a week for 1 year. ETS exposure was defined among nonsmokers as having lived or worked with smoker(s) for at least 1 year and was regularly exposed to tobacco smoke. Regular exposure was defined as at least 1 h a day. We further divided ETS exposure into three categories, i.e., exposure at either home or work, at both home and work, and none at all.
We made a great effort to collect detailed information on cooking practice. A composite index—the cooking dish-years was constructed to quantify the regular cooking habits in terms of the frequency and the duration of cooking, as well as three cooking methods (stir-frying, frying, and deep-frying), as described previously [10]. One stir-frying dish-year means cooking one stir-fried dish daily for a year. The total cooking dish-years was calculated by summing up the stir-frying dish-years, frying dish-years and deep-frying dish-years. The total cooking dish-years was used to express the amount of exposure to cooking emissions.
Exposure to radon at home was assessed based on detailed information about the lifetime residences (floor level, building material and wall surface covering materials, building age, and window opening practices, according to information available from a territory-wide indoor radon survey conducted in Hong Kong. The radon exposure was expressed as residential radon exposure index (RRE) [10]. In addition, information on diagnosed cancer in the lungs and any other site in first degree relatives (parents and siblings) and occupation, including job titles and job tasks according to the coding manual used for the Hong Kong Census [14] was gathered. Occupations were grouped into four categories: (1) professional/clerical/sales, (2) never employed/domestic helper, (3) cleaners, and (4) construction/industry/sewer workers.
In collection of data on diet, a reduced version of the Diet History Questionnaire designed by the National Cancer Institute was used [15]. Subjects were asked about their dietary habits during the past 5 years before the interview for controls, and prior to becoming ill for cases. The data included the frequency and amount of eating following groups of foods: (1) dark green vegetables, (2) orange or yellow vegetables, (3) all kinds of meat, (4) all kinds of fresh fruits (total fruits), (5) pickled vegetables, (6) supplement of multivitamins, and (7) coffee drink. Consumptions of the first three groups of food were quantified as average numbers of servings (one serving = 80 gram) per day/week/month, while the second three groups were expressed as the frequency of consumption. A coffee drinker was defined as one who drank at least one cup of coffee per week for 6 months or more. Coffee drinking was further quantified as cup-years, i.e., one cup-year means drinking one cup of coffee per day for 1 year.
Statistical analysis
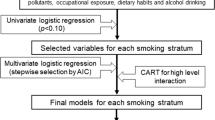
Unconditional logistic regression was applied to estimate associations of potential risk factors with lung cancer. Basically, three models were constructed to obtain odds ratios (ORs) for lung cancer. The first model was to estimate the main effect of each of the potential risk factors adjusted by age (there was a residual confounding effect), employment and years of education. Smoking amount was categorized as less than 25 and 25 or more pack-years. Similarly to our previous practice [10, 11], exposure to cooking emissions was also categorized into four groups using intervals of 50-dish years. The group of professional/clerical/sales workers who were assumed to be exposed to minimum potential hazards associated with lung cancer served as reference group. The second model was constructed to estimate the effects of smoking, total dish-years, family cancer history, radon index, and occupations, where all of these variables were included all at once, along with age, education, consumptions of total fruits, and vegetables. The final model was constructed to estimate the effects of dietary factors and coffee consumption, in which all of the dietary variables and coffee consumption were included all at once. In addition, all of other variables that were found to be significant predictors in the second model were included in the final models. All of the three models were fit using data of all subjects and that of nonsmokers alone. In the latter case, ETS was adjusted as well.
Finally, we made an estimation of population attributable fraction (PAF) in all subjects and in nonsmokers, respectively, based on the following method: \( {\text{PAF}} = 1 - \sum {{\frac{{P_{i} }}{{{\rm{OR}}_{i} }}}} \) for multiple categorical variables [16], where P i is the proportion of all cases that are in the stratum i, and OR i is an adjusted odds ratio in the stratum i. \( {\text{PAF}} = {\frac{{{\rm{Pe}} \times ({\rm{OR}}\,-\,1)}}{{1\,+\,{\rm{Pe}} \times ({\rm{OR}}\,-\,1)}}} \)for binary variables [17], where Pe is the prevalence of exposure in the control population and OR is an adjusted odds ratio for exposure to the independent variable under study.
Results
Average age was around 65 years for both case and control groups, and marital status was similar in the two groups (Table 1). There were significant differences between the two groups in education and employment, in which lower education levels and more never employment were seen in cases than in controls (p < 0.05). The majority of lung cancer cases were identified as adenocarcinoma (62%), whereas squamous cell, large and small cell types accounted for a small proportion, respectively.
The values of total dish-years and radon index were significantly higher in cases than in controls (Table 2). Likewise, smoking, heavy smoking (≥25 pack-years) and family cancer history were more commonly seen in the cases. Total dish-years, smoking status, pack-years, and radon index were associated with increased risk of lung cancer. Furthermore, there were exposure–response trends in total dish-years and smoking pack-years (Table 2). Family history of lung cancer and any cancer also increased the risk. All of the associations remained statistically significant when all of relevant factors were taken into account, while the association with radon index was marginally significant. Among the four occupational categories, more cases were found in the category of never employed/domestic helpers than the controls (27 vs. 16%). The adjusted OR in relation to never employed/domestic helpers was 2.6 times, in comparison with clerical/sales workers. An upward risk was also seen in cleaners and other industrial workers. In the full model, all of the above variables were adjusted each other, in addition to age, education, consumption of total fruits, and vegetables.
The above analyses were also performed in nonsmokers after 66 smoking cases and 30 smoking controls were excluded. A slightly elevated risk was observed in relation to ETS at either home or work (OR = 1.14, 95% CI, 0.68, 1.93) and at both home and work (OR = 1.30, 95% CI, 0.72, 2.35). The strength of associations with family cancer history, radon index, and occupations was approximate to that observed in all subjects. However, a greater risk was observed in cooking dish years in nonsmokers, which showed a clearer exposure–response trend (OR: 1.24, 95% CI: 0.96, 2.01 in the category of 51–100; OR: 2.82, 95% CI: 1.48, 5.35 in 101 -150; OR: 4.24, 95% CI: 2.12, 8.47 in over 150).
In determination of the potential effects of dietary factors on lung cancer, a full model was constructed with all variables of the dietary factors along with age, employment, education, total dish-years, smoking, family cancer history, and radon index. As shown in Table 3, a higher risk was seen in increasing consumption of meat. Consumption of 1 serving/day or more was related to a double risk of that below 1 serving/day. Pickled vegetables slightly elevated the risk. On the other hand, consumptions of dark green vegetables and yellow/orange vegetables were inversely related to lung cancer risk, both of which showed a gradient with increasing amount. A similar trend was also observed in consumption of multivitamins, but the number of subjects in either irregular or regular consumption was small. In addition, consumption of coffee ranging from 1 to 10 coffee-years significantly lowered the risk. However, heavier drinkers, i.e., 10 or more coffee-years, tended to be associated with a slightly increased risk. When the similar full model was fit by restricting data to nonsmokers (data not shown), the directions and strengths of the above associations were approximate to those observed in all subjects. There was a slight difference seen in the effect of coffee consumption in nonsmokers: adjusted OR related to heavier coffee consumption was 1.62 (95% CI, 0.18, 0.78), somewhat greater than that obtained from all subjects, while a similar OR remained in the category of light coffee consumption (OR, 0.37; 95% CI, 0.18, 0.78).
An estimate of population-attributable fraction in all study subjects revealed that about 27% of lung cancer could be attributable to exposure to cooking emissions (Table 4). The fraction attributable to smoking, domestic radon exposure, low vegetable intake, and family cancer history ranged between 16 and 30%. In addition, about 9% of lung cancer could be explained by consumption of meat with 95% confidence interval of −20 and 29, indicating the point estimate was not stable. In the calculation that restricted to lifetime nonsmokers, there was not much difference from those obtained from all of the subjects, with the exception of a higher fraction of lung cancer (35%) that could be attributable to exposure to cooking emission.
Discussion
Lung cancer is the leading neoplasm in many countries, in terms of both incidence and mortality. Although cigarette smoking is a major recognized cause, which accounts for 80–90% of lung cancer cases, only a small fraction of smokers (1–15%) develop lung cancer [18]. In this study, majority of the subjects were nonsmokers. Smoking certainly cannot fully explain the high incidence and mortality of lung cancer experienced by Chinese women in Hong Kong. Clearly, other etiological factors can independently (in the absence of smoking) or jointly (in conjunction with smoking) cause lung cancer [19]. In our previous analyses [10, 11], we found that smoking and exposure to cooking emission were potent risk factors for lung cancer in the Hong Kong women, in which the two factors appeared to act independently. We also observed that a positive family history of any cancer was associated with over twofold risk of a negative family history [12]. The present analysis reconfirmed the associations, while additional factors, such as dietary habits, occupations, and exposure to radon at home were adjusted simultaneously. The current study further suggested that the exposure to cooking fume might explain about 26% of lung cancer occurring in the whole group, and 35% in nonsmoking women. Nearly 16% of lung cancer could be attributable to cigarette smoking, and about 22% to residential exposure to radon. More importantly, this study evaluated the roles of dietary habit and occupations in the development of lung cancer, while taking into account of all other factors, such as smoking, exposure to cooking emission, and family cancer history. The results added additional information to help understand lung cancer etiology in Hong Kong women.
The link of dietary factors to lung cancer as well as other cancers has been increasingly addressed [20, 21]. Diet is believed to play a major role in cancer etiology and prevention. However, few studies were available with respect to which specific dietary factors are most closely linked to lung cancer in Chinese population. In this study, we collected detailed dietary data in both frequency and quantitative assessment. We found inverse associations of lung cancer with vegetables, multivitamins, and moderate consumption of coffee, and a positive association with total meat. These associations were independent of other risk factors or confounders being considered. In addition, we observed a favorable effect of increasing intake of total fruits and an adverse effect of pickled vegetables, which were consistent with a previous Hong Kong study [22], though neither of them was significant.
Intake of vegetables, including dark green and yellow/orange vegetables, was found to be related inversely to the risk of lung cancer. There appeared a stronger association with yellow/orange vegetables, showing lower odds ratios with increasing intake amount. Intake 1 or more serving per week might be related to a reduced risk by half, in comparison with intake less than 1 serving per week. The result was in line with the previous studies showing that individuals with high dietary intake of vegetables had a lower risk for lung cancer than those with low vegetables intake [21]. Low vegetable intake was found to contribute 30% to the cancer risk in this population. Fruits and vegetables are the major dietary source of antioxidant micronutrients, such as vitamin A, vitamin C, lycopene, beta-carotene, lutein [23, 24]. Epidemiological data generally indicated a stronger protective association for fruits than vegetable consumption [25]. In this study, we did not observe a stronger association with fruits, however. A possible explanation might be that the sample size was not big enough given the wide range of confidence intervals. Further studies with larger sample sizes are necessary to confirm the association of fruits with lung cancer in Hong Kong women.
Intake of multivitamins was also found to be inversely associated with lung cancer risk, in which regular intake had a stronger effect than irregular intake. Anticarcinogenic effects of vitamin A, C, D, and E have been suggested in both population studies and experimental studies [25–27]. The evidence for intake of vitamin C and a variety of carotenoids or antioxidant index suggested protective associations [28]. It should be pointed out, however, that there were only a small number of the women who took vitamin supplement in this study. Therefore, caution should be given to the interpretation of the result.
Meat intake was another dietary factor found to be associated with lung cancer. The risk in those who ate one serving or more (over 80 g) per day was more than twofold of that in those eating less. The positive association with meat consumption was consistent with some other studies conducted in different populations [29, 30]. Most previous studies showed a moderately elevated risk that was associated with higher intake of fat, meat, or cholesterol [30–32], based on which the World Cancer Research Fund (WCRF) concluded that diets high in total fat, saturated/animal fat, and cholesterol possibly increase the risk of lung cancer [25]. In our study, meat intake could explain approximating 9% of lung cancer. It was worthwhile to point out that the variable of meat intake in this study referred to all kinds of meat intake, including red meat, poultry, and seafood. It has been suggested the link between fat and cancer risk depends on the type of fat consumed rather than total fat intake [28]. Consumption of red meat was especially thought to be linked to lung cancer and other cancers [33]. Therefore, the association between (red) meat intake and lung cancer might have been diluted in our study because of all kinds of meat consumption included. The Population Attributable Fraction could be bigger if only red meat intake was considered. Unfortunately, we were not able to separate the effect of red meat intake from others with the current data. It certainly deserves to be addressed in the future studies. The mechanism for the positive association with high meat intake has not been clearly understood, but mutagens and carcinogens, especially compounds known as heterocyclic amines (HCAs), has been identified in meats cooked at high temperatures [34, 35], which may be responsible for increasing lung cancer risk.
The link of coffee consumption to lung cancer was another interesting finding. The light drinking (1–10 coffee-years) was associated with a decreased risk, while slightly elevated risk was seen in heavier drinking. Previous studies reported a beneficial effect of consumption of coffee, especially decaffeinated coffee, on breast cancer [36] and colorectal cancer [37]. On the other hand, caffeine was found to have a carcinogenic effect and might elevate cancer risk [38, 39]. Among a limited number of studies examining coffee consumption and lung cancer, some suggested elevated risks associated with increasing coffee consumption [40]. A few studies, however, reported that consumption of decaffeinated coffee was associated with a statistically decreased risk of lung cancer, which indicated a protective effect against lung cancer [41, 42]. We detected an inverse relationship with moderate coffee consumption. Nevertheless, there were only a small number of coffee drinkers and no detailed information on the types of coffee consumed by each subject; hence, it prohibited us to draw a conclusion based on the current data. A further study addressing the association of coffee consumption with lung cancer would be worthwhile.
Lung cancer is the most common one among cancers that are associated with occupational exposures [43]. The proportion of lung cancer contributable to occupational exposures has been suggested to range from 9 to 15% [28]. The association between lung cancer and occupational history in women has not been studied as extensively as in men. Among a limited number of studies, certain occupations were linked to increase lung cancer risk in females, including cleaners, construction workers, metal product workers, rubber/plastic product makers, and sewer workers [44–46]. A recent cohort study conducted in nonsmoking women in Shanghai, China [47] found an excess risk of lung cancer in painters and rubber workers, though overall exposure to known or suspected occupational lung carcinogens was not associated with lung cancer risk. In our study, we observed an elevated risk in cleaners and industrial workers including sewer workers. The association in cleaners was in accord with the previous studies, in which cleaning service was linked to increased lung cancer risk [44, 45], possibly due to exposure to certain organic solvents that have a carcinogenic effect. For industrial workers, a wide range of carcinogens identified in different industries has been suggested [28, 47]. We did not classify job matrix and potential exposures specifically in this study due to the limited number of subjects.
It was also worthwhile to note that among the four categories of occupations, the greatest risk was seen in the never employed and domestic helpers. The result was persistent in the analysis either among all subjects or among nonsmokers alone. A possible explanation might be that housewives and domestic helpers were exposed more heavily to cooking emissions because they usually involved more cooking practice at home. A stratifying analysis of cooking practice displayed that the cases in never employed women had the highest total dish-years (118 dish-years), in comparison with other employed women (ranging from 52 to 86 dish-years). The result, in turn, corroborated the importance of cooking fumes as a risk factor for lung cancer.
Residential radon is another environmental risk factor being studied. A substantially higher excess relative risk of lung cancer was linked to residential radon gas exposure [48, 49]. The current data also suggested an increased risk associated with residential radon exposure, though the association was marginally significant when all of other factors were adjusted. About 22% of lung cancer could be attributable to residential exposure to radon. However, we need to point out that the radon exposure level was estimated, not measured directly in this study, which might have resulted in a nondifferential misclassification of the exposure and lead to an underestimation of the association.
As in most case–control studies, selection bias could be a concerned issue in this study. Our cases were drawn from the largest oncology center and the participation rate reached up to 96%. The control subjects were selected from the same community where cases came from. The procedure was unlikely to introduce substantial selection bias. Recall bias would be another major concern for such a study, which might cause differential misclassification of exposures. To minimize the possibility of differential recall from awareness of disease status, we introduced the study to the subjects as a general “women health study”. However, nondifferential recall errors were likely present, as all of the information on individual exposures and dietary habits were obtained through questionnaires. Nondifferential recall bias might have led to underestimated associations. Another limitation of this study was that we did not assess the effects of the various factors in smokers alone due to a small number in this category. It was likely that smokers and nonsmokers were etiologically distinct in lung cancer. Inadequate study power prevented us from assessing the distinction between smokers and nonsmokers. However, the analysis with combined data of smokers and nonsmokers allowed us evaluating the role of smoking in lung cancer among these subjects.
In summary, this study provided additional understanding of possibly etiological links of various factors with lung cancer among Chinese women in Hong Kong. In addition to the well-established smoking effect, environmental exposures, including exposures to cooking emissions and radon at home, and family cancer history are contributing factors to lung cancer. Moreover, consumptions of meat, too little consumption of vegetables/fruits and multivitamins may increase lung cancer risk. Moderate consumption of coffee appears to have a beneficial effect. The findings highlight the importance and necessity of initiating/strengthening education programs that should focus on individual behavior and dietary habit changes in prevention and control of lung cancer in a population level.
Abbreviations
- ETS:
-
Environmental tobacco smoke
- RRE:
-
Residential radon exposure
- ORs:
-
Odds ratios
References
Hong Kong Cancer Registry (2002) Cancer Stat 2000. Hospital Authority, Hong Kong
Department of Health (1994) Coronary heart disease and lung cancer. Department of Health Hong Kong, Hong Kong, pp 33–49
International Agency for Research on Cancer (2001) GLOBOCAN 2000: Cancer Incidence, Mortality and Prevalence Worldwide. Available at http://www-dep.iarc.fr/globocan/globocan.htm. IARC. Accessed July 6, 2004
International Agency for Research on Cancer (1987) Cancer incidence in five continents, vol 5. IARC, Lyon
MacLennan R, Da Costa J, Day NE, Law CH, Ng YK, Shanmugaratnam K (1977) Risk factors for lung cancer in Singapore Chinese, a population with high female incidence rates. Int J Cancer 20:854–860
Hinds MW, Stemmermann GN, Yang HY, Kolonel LN, Lee J, Wegner E (1981) Differences in lung cancer risk from smoking among Japanese, Chinese and Hawaiian women in Hawaii. Int J Cancer 27:297–302
Kono S, Isa AR, Ogimoto I, Yoshimura T (1987) Cause-specific mortality among Koreans, Chinese and Americans in Japan, 1973–1982. Int J Epidemiol 16:415–419
Liu BQ, Peto R, Chen ZM, Boreham J, Wu YP, Li JY, Campbell TC, Chen JS (1998) Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ 317:1411–1422
Lam WK (2005) Lung cancer in Asian women—the environment and genes. Respirology 10:408–417
Yu ITS, Chiu YL, Au JSK, Wong TW, Tang JL (2006) Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmokers women. Cancer Res 66:4961–4967
Wang XR, Chiu Y, Qiu H, Au J, Yu IT (2009) The roles of smoking and cooking emissions in lung cancer risk among chinese women in Hong Kong. Ann Oncol 20:746–751
Wang XR, Yu ITS, Chiu YL, Qiu H, Fu Z, Goggins W, Au JSK, Tse LA, Wong TW (2009) Previous pulmonary disease and family cancer history increase the risk of lung cancer among Hong Kong women. Cancer Cause & Control 20:757–763
World Health Organization (1982) The World Health Organization histological typing of lung tumors. Second edition. Am J Clin Pathol 77:123–136
Hong Kong Census and Statistics Department (1981) Hong Kong 1981 Land Census Coding Manual. Hong Kong Government, Hong Kong, pp 33–39
National Cancer Institute (2002) NCI’s diet history questionnaire, DHQ-1. http://riskfactor.cancer.gov/DHQ/forms/files/shared/dhq1. Accessed June 7, 2002
Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C (1985) Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epi 122:904–914
Schlesselman JJ (1982) Case-control studies. Oxford University Press, New York, NY
Alberg AJ, Samet JM (2003) Epidemiology of lung cancer. Chest 123(suppl 1):21S–49S
Ahsan H, Thomas DC (2004) Lung cancer etiology. Independent and joint effects of genetics, tobacco, and arsenic. JAMA 292:3026–3029
Sjuladottir H, Tjoenneland A, Overvad K et al (2004) Does insufficient adjustment for smoking explain the preventive effects of fruits and vegetables on lung cancer? Lung Cancer 45:1–10
Alberg AJ, Samet JM (2005) Epidemiology of lung cancer. In: Sadler MJ, Caballero B, Strain JJ (eds) Encyclopedia of human nutrition. Academic Press, London, UK, pp 272–284
Chan-Yeung M, Koo LC, Ho JC, Tsang KW, Chau WS, Chiu SW, Ip MS, Lam WK (2003) Risk factors associated with lung cancer in Hong Kong. Lung Cancer 40:131–140
Steinmetz KA, Potter JD (1996) Vegetables, fruit, and cancer prevention: a review. J Am Diet Assoc 96:1027–1039
Smith-Warner SA, Spiegelman D, Yaun SS et al (2003) Fruits, vegetables and lung cancer: a pooled analysis of cohort studies. Int J Cancer 107:1001–1011
World Cancer Research Fund (1997) Food, Nutrition and the Prevention of Cancer: A Global Perspective. American Institute for Cancer Research, Washington DC, pp 130–147
de Klerk NH, Musk AW, Ambrosini GL, Eccles JL, Hansen J, Olsen N, Watts VL, Lund HG, Pang SC, Beilby J, Hobbs MS (1998) Vitamin A and cancer prevention II: comparison of the effects of retinol and beta-carotene. Int J Cancer 75:362–367
Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, Holick MF (2006) The role of vitamin D in cancer prevention. Am J of Pub Health 96:9–18
Alberg AJ, Ford JG, Samet JM (2007) Epidemiology of lung cancer. ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:29S–55S
Deneo-Pellegrini H, De Stefani E, Ronco A, Mendilaharsu M, Carzoglio JC (1996) Meat consumption and risk of lung cancer; a case-control study from Uruguay. Lung Cancer 14:195–205
Breslow RA, Graubard BI, Sinha R, Subar AF (2000) Diet and lung cancer mortality: a 1987 national health interview survey cohort study. Cancer Causes Control 11:419–431
Goodman MT, Kolonel LN, Yoshizawa CN, Hankin JH (1988) The effect of dietary cholesterol and fat on the risk of lung cancer in Hawaii. Am J Epidemiol 128:1241–1255
Jain M, Burch JD, Howe GR, Risch HA, Miller AB (1990) Dietary factors and risk of lung cancer: results from a case-control study, Toronto, 1981–1985. Int J Cancer 45:287–293
Greenwald P, Clifford CK, Milner JA (2001) Diet and cancer prevention. Euro J Cancer 37:948–965
Berg I, Overvik E, Gustafsson JA (1990) Effect on cooking time on mutagen formation in smoke, crust and pan residue from pan-broiled pork. Food Chem Toxicol 28:421–426
Thiebaud HP, Knize MG, Kuzmicky PA, Hsieh DP, Felton JS (1995) Airborne mutagens produced by frying beef, pork and a soy-based food. Food Chem Toxicol 33:821–828
Baker JA, Beehler GP, Sawant AC, Jayaprakash V, McCann SE, Moysich KB (2006) Consumption of coffee, but not black tea, is associated with decreased risk of premenopausal breast cancer. Nutr Epidemiol 136:166–171
Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S, Tsugane S, JPHC Study Group (2007) Coffee consumption and risk of colorectal cancer in a population-based prospective cohort of Japanese men and women. Int J Cancer 121:1312–1318
Ito K, Nakazato T, Miyakawa Y, Yamato K, Ikeda Y, Kizaki M (2003) Caffeine induces G2/M arrest and apoptosis via a novel p53-dependent pathway in NB4 promyelocytic leukemia cells. J Cell Physiol 196:176–283
Terry KL, Titus-Ernstoff L, Garner EO, Vitonis AF, Cramer DW (2003) Interaction between CYP1A1 polymorphic variants and dietary exposures influencing ovarian cancer risk. Cancer Epidemiol Biomarkers Prev 12:187–190
Stensvold I, Jacobsen BK (1994) Coffee and cancer: a prospective study of 43, 000 Norwegian men and women. Cancer Causes Control 5:401–408
Mettlin C (1989) Milk drinking, other beverage habits, and lung cancer risk. Int J of Cancer 43:608–612
Baker JA, McCann SE, Reid ME, Nowell S, Beehler GP, Moysich KB (2005) Associations between black tea and coffee consumption and risk of lung cancer among current and former smokers. Nutr Cancer 52:15–21
Doll R, Peto R (1981) The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst 66:1191–1308
Brownson RC, Alavanja MC, Chang JC (1993) Occupational risk factors for lung cancer among nonsmoking women: a case-control study in Missouri (United States). Cancer Causes Control 4:449–454
Jahn I, Ahrens W, Bruske-Hohlfeld I et al (1999) Occupational risk factors for lung cancer in women: results of a case-control study in Germany. Am J Ind Med 36:90–100
Wu-Williams AH, Xu ZY, Blot WJ, Dai XD, Louie R, Xiao HP, Stone BJ, Sun XW, Yu SF, Feng YP, Fraumeni JF, Henderson BE (1993) Occupation and lung cancer risk among women in northern China. Am J Ind Med 24:67–79
Pronk A, Coble J, Ji B-T, Shu X-O, Rothman N, Yang G, Gao T-T, Zheng W, Chow W-H (2009) Occupational risk of lung cancer among lifetime non-smoking women in Shanghai, China. Occup Environ Med 66:672–678
Field RW, Steck DJ, Smith BJ, Brus CP, Fisher EL, Neuberger JS, Platz CE, Robinson RA, Woolson RF, Lynch C (2000) Residential radon gas exposure and lung cancer. The Iowa radon lung cancer study. Am J Epidem 151:1091–1102
Wang Z, Lubin JH, Wang L et al (2002) Residential radon and lung cancer risk in a high exposure area of Gansu Province, China. Am J Epidem 155:554–564
Acknowledgments
The work described in this paper was substantially supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project No. CUHK4103/02M).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiu, YL., Wang, XR., Qiu, H. et al. Risk factors for lung cancer: a case–control study in Hong Kong women. Cancer Causes Control 21, 777–785 (2010). https://doi.org/10.1007/s10552-010-9506-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9506-9