Abstract
Objective of the study
Recent publications have reported an association between colon cancer and human papillomaviruses (HPV), suggesting that HPV infection of the colonic mucosa may contribute to the development of colorectal cancer.
Methods
The GP5+/GP6+ PCR reverse line blot method was used for detection of 37 types of human papillomavirus (HPV) in DNA from paraffin-embedded or frozen tissues from patients with colorectal cancer (n = 279) and normal adjacent tissue (n = 30) in three different study populations, including samples from the United States (n = 73), Israel (n = 106) and Spain (n = 100). Additionally, SPF10 PCR was run on all samples (n = 279) and the Innogenetics INNO-LiPA assay was performed on a subset of samples (n = 15).
Results
All samples were negative for all types of HPV using both the GP5+/GP6+ PCR reverse line blot method and the SPF10 INNO-LiPA method.
Conclusions
We conclude that HPV types associated with malignant transformation do not meaningfully contribute to adenocarcinoma of the colon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human papillomaviruses (HPV) have been detected in several types of squamous cell cancers, such as cancer of the cervix [1–7], vulva [8–10], vagina [10, 11], anus [12–15], penis [16–20], oral cavity [21], pharynx [22, 23], and larynx [24–27]. An association between colon cancer and human papillomaviruses (HPV) is controversial, with several recent publications suggesting that HPV infection of the colonic mucosa may contribute to the development of colorectal cancer [28–31]. However, there have been several investigations which failed to establish a link between HPV and colon cancer [32, 33] indicating that reports of an association between colon cancer and HPV may be due to contamination, detection of HPV false-positives, geographic differences in the study populations or variation in detection methods used. To clarify these discrepant findings, the present study investigates the relationship between HPV and colorectal cancer in three separate populations. The current study used two PCR-based methods GP5+/GP6+ [34] and SPF10 [35] for detection of HPV, which target the LI region of the HPV genome. In addition, we used two reverse hybridization techniques, the reverse line blot method (RLB) [36] and the INNO-LiPA HPV detection/genotyping assay [37].
Materials and methods
Colorectal samples for HPV DNA detection were gathered from three different studies conducted in Israel, Spain and the United States.
Samples from Israel
Samples from Israel were collected as part of a population-based case–control study (the Molecular Epidemiology of Colorectal Cancer Study—MECC) of all incident cases of colorectal cancer (n = 2,155) in northern Israel between March 31, 1998 and April 1, 2004. Incident colorectal cancer cases (CRC) were ascertained from five hospitals in northern Israel, and all cases for these analyses have histologically confirmed cancer of the colon or rectum. The controls (n = 2,268) were individually matched for exact year of birth, sex, clinic, and Jewish versus non-Jewish heritage. The study was approved by all relevant IRBs in the US and Israel, and written informed consent was given by study participants. Detailed descriptions of this study have previously been published [38].
Paraffin-embedded tumors with adequate residual tissue for microdissection were available for analysis. Tumor blocks were recut for uniform histopathologic review and microdissection, with the first slide of a series of 12 reviewed by a qualified pathologist (JKG) to confirm the original diagnosis and to circle areas for microdissection. Corresponding areas of normal tissue (with 0% tumor) from the same slide, or from another section of the same surgical resection, were circled for microdissection. DNA was extracted by carefully scraping tissue from designated areas of slides with a clean razor blade and transferring the samples to separate non-siliconized tubes. Xylene (350 μl) was added to each sample to dissolve the paraffin, and ethanol precipitation was performed by adding 150 μl of cold 100% ethanol to each sample. Samples were next spun at 14,000 rpm at room temperature for 10 min. The supernatant was expelled and pellets were lyophilized in a Speed Vac for 8 min on high heat. Pellets were then resuspended in 100 μl of proteinase K buffer (200 ng/μl proteinase K in 50 mM Tris, pH 8.3) and incubated overnight at 37°C. Samples were heated at 95°C for 8 min and quickly transferred to ice for 5 min to keep the DNA from re-naturing. DNA samples were then stored at −80°C. DNA from a total of 1,653 tumors was available for analysis. A subset of 110 microdissected DNA samples was randomly selected for HPV testing. One hundred and six out of 110 (96%) were successfully typed.
Samples from Spain
Patients with a new diagnosis of colorectal cancer at the Hospital Universitario de Bellvitge, in Barcelona, Spain, were recruited as part of a hospital-based case–control study from January 1996 to December 1998. All diagnosed cases were histopathologically confirmed. A total of 436 cases were diagnosed with sporadic CRC, of which a random sample of 100 was used for the current study. Tumor DNA was extracted from fresh frozen tissue. More detailed information on this study is available from a previous publication [39].
Samples from the USA
Cases of colorectal cancer were identified and recruited through the University of Michigan Tissue Core. Anonymous paraffin blocks from colon cancer specimens collected from surplus surgical tissue were available for 76 samples. Tumor blocks were recut for uniform histopathologic review and microdissection, with the first and last slides of a series of 12 reviewed by one pathologist (TJG) to confirm the original diagnosis and to circle areas for microdissection. Samples were processed as previously described [40].
HPV Genotyping
HPV genotyping was performed using the GP5+/GP6+ PCR reverse line blot (RLB) method [36, 41] for 37 HPV types on all tumor tissue samples (n = 279) and adjacent normal tissue (n = 30). Adequacy of amplifiable DNA was assessed using beta-globin primers used for the amplification of a 210-bp region as an internal control. All runs included positive controls consisting of HPV including HeLA cell line DNA which is positive for HPV type 18 and DNA extracted from a paraffin embedded head and neck cancer which is positive for HPV type 16, as well as negative water controls to exclude the possibility of contamination. The PCR reaction mixture (20 μl) contained 5 ng of genomic DNA, 2.5 μl of 10X PCR buffer (Applied Biosystems), 3.5 μl of 25 mM MgCl2 (Applied Biosystems), 2.5 μl each of 2 mM dNTP (New England Biolabs), 10 μM forward and reverse primers, and 1 U of AmpliTaq Gold DNA polymerase (Applied Biosystems). Cycling conditions were as follows: Initial denaturation at 94°C for 4 min, 40 cycles of 94°C for 60 s, 58°C for 2 min, 72°C for 1 min 30 s, and a final extension at 72°C for 4 min. A volume of 10 μl of the PCR product was analyzed by electrophoresis on 2% agarose gels stained with ethidium bromide. The reverse line blot method was used on all samples with amplifiable DNA, and the hybridization conditions are described elsewhere [36]. Additionally, HPV genotyping was verified using the SPF10 PCR primers and the INNO- LiPA method (Innogenetics) which is capable of detecting 26 HPV types. Biotinylated SPF10 PCR primers were used for the amplification of a 65-bp region of the L1 gene of a broad spectrum of HPV types was performed on all tumor samples (n = 279). All runs included positive controls consisting of HPV including HeLA cell line DNA and head and neck tumor DNA, as well as negative water controls. The PCR reaction mixture (50 μl) contained 2.0 μl of 5 ng of genomic DNA, 37.7 μL of AMP mix (Innogenetics), 2.3 μL of ENZ mix (Innogenetics) and 8.0 μL of water. Cycling conditions were as follows: initial denaturation at 94°C for 9 min, 40 cycles of 94°C for 30 s, 52°C for 45 s, 72°C for 45 s, and a final extension at 72°C for 5 min. A volume of 10 μl of the PCR product was analyzed by electrophoresis on 2% agarose gels stained with ethidium bromide. The INNO- LiPA assay was used on a subset of the samples (n = 15). Hybridization conditions were performed according to the protocol from the INNO-LiPA kit (Innogentics). All samples were processed in a laboratory that was separate from where the PCR amplification was performed to avoid false-positives due to contamination.
Results
A total of 279 colorectal samples from microdissected DNA and 30 normal adjacent tissues samples were analyzed from three different populations (Table 1). Cases were slightly older in Israel (mean of 72 (SD = 8.6)) than in Spain (mean of 66 (SD = 10)) and the United States (mean of 63 (SD = 11.6)). There was also a higher proportion of females in the Israeli sample (44%) when compared to the Spanish sample (33%). In the Israeli and Spanish samples, approximately 70% of the tumors from cases occurred in the colon, with approximately 30% occurring in the rectum. Tumors for all cases from the United States occurred in the colon.
All 279 samples from all three different studies were negative for all types of HPV using both the GP5+/GP6+ PCR reverse line blot method and the SPF10 INNO-LiPA method. Thus, the prevalence estimate was 0 (95% CI: 0–0.017) for all colorectal cancer cases, which excludes a true prevalence larger than 2% with P = 0.03. Prevalence estimates and 95% confidence intervals were calculated separately for colon and rectal cancers. The prevalence estimate was 0 (95% CI: 0–0.022) for colon alone (n = 214) and 0 (95% CI: 0–0.074) for rectum alone (n = 61). It can be seen that the confidence intervals are slightly wider for rectum alone given that we had a smaller sample size of rectal cancers. Therefore our data cannot entirely exclude a role for HPV infection in rectal cancer, although we did not detect any HPV in the rectum or colon.
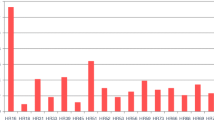
We computed a meta-analysis of the six previous studies, in addition to our study, to summarize the prevalence of HPV in colorectal cancer across studies (Table 2). We measured the inconsistency across study results by computing Cochran’s Q test for heterogeneity, which is the weighted sum of squared differences between individual study effects and the pooled effect across studies. A random effects model was used to allow the true effect size in the studies to vary, because studies often differ in terms of design, methods employed, samples sizes and patient population [42, 43]. Based on the Cochran Q = 574.71 (df = 6, P < 0.0001), there is clear evidence of significant heterogeneity across studies, with HPV prevalences ranging from 0 to 83.3%. The pooled prevalence estimate was 1.6% (0.017–74%), but the validity of this pooled estimate is difficult to interpret given the large heterogeneity observed in the data and suggests that the true prevalence is likely to be zero.
Discussion
Using two different highly sensitive and specific techniques for detecting the presence of HPV, the current study does not confirm previous reports of an association with colorectal cancer, and in fact, stands in stark contrast with some previously published results. There are several potential reasons for the lack of agreement, and the most likely appears to be a profound degree of contamination in other studies. There are numerous opportunities for HPV contamination of colorectal cancer specimens that do not actually harbor pathogenic infections. Pathology laboratories that are not specifically established to maintain HPV-free environments can lead to contamination of the tumor blocks. Research laboratories with experience in HPV-positive samples may accidentally cross-contaminate colorectal cancers at the time blocks are (1) recut for microdissection, (2) when DNA is extracted, or (3) when PCR amplification is performed.
Two studies (Buyru et al. 2006; Perez et al. 2005) did not report the results of negative water controls which generally identify and protect against the possibility of PCR contamination. Additionally, Buyru et al. 2006 used lymphocytes as negative controls. A frequent source of contamination can be traced to the re-use of microtome blades when paraffin-embedded tumor blocks are recut into sections for mounting or microdissection and DNA extraction. These blades are expensive, and in a surgical pathology laboratory that emphasizes diagnostic pathology preparation, it is usually not necessary to replace the blade after each block. Our study used a new blade for every block, and the microtome was thoroughly cleaned between each case. Although we cannot be certain that these procedures eliminated the possibility of HPV contamination in our study, it is likely that these protocols greatly reduced the probability. Furthermore, we did not observe HPV contamination in any sample. Template-free (water) controls were included in every PCR amplification run, and none showed evidence of HPV while all positive controls were observed.
It is also highly unlikely that our study failed to detect HPV infection that was truly present in the sample. We used two different techniques; GP5+/GP6+ reverse line-blots and the LiPA technique that are considered the state-of-the-art for HPV detection. The sensitivity of GP5+/GP6+ and LiPA has previously been reported to be more sensitive than other techniques used to detect HPV [36, 44]. Other studies exploring the role of HPV in colorectal cancer used techniques that are even less sensitive, making differential sensitivity extremely unlikely as an explanation for our findings [30].
Power is also important to consider for any study that fails to find an association or fails to replicate previously published results. Our study was larger than all of the other published studies combined (n = 279 vs. n = 234), and we designed our study to have 93% power to detect a difference in proportions of as little as 10% (n = 279) if the prevalence is 0 versus 0.1. The power to detect a difference in proportions of 10% if the prevalence is 0.7 versus 0.8, similar to those found in previous reports (see Table 2), is 97%.
Although it is theoretically possible that there are geographical differences that might account for the profoundly disparate results of our study compared to the published literature, this seems unlikely given the large international sampling frame of our study. The present study includes nearly equal sample sizes of cases from a population-based study of colorectal cancer in Israel, a hospital-based study of colorectal cancer in Spain, and a hospital-based series of colorectal cancer cases from the United States. For example, the published study from Turkey described a prevalence of HPV of 81.2%, compared to our findings of 0% in Israel. The previously published study from the NIH group included cases from Baltimore and Houston, showing a prevalence of 51%. Cases from Michigan included in our study also showed a prevalence of 0%. Although there are no published European studies of HPV that we are aware of, our findings of 0% cases with HPV from Spain stand in striking contrast to the 74% reported in Argentina and 83% reported in Brazil.
Publication bias may also account for the differences between our findings and the previously published reports. We completed a systematic review of the literature, using Pubmed search terms (HPV, cancer, colon, rectum), and only two papers documented an absence of HPV in colon or rectal cancers, and both of these papers were published in 1992.
A possible limitation of the current study is the age of the samples used for detection of HPV. The paraffin blocks from the Israeli sample were prepared as early as 1999, and DNA was microdissected within an average of 194 days (approximately 6.5 months). The microdissected DNA was immediately stored at −80°C for approximately 7.5 years (SD = 1.9). DNA stored in at this temperature should be very stable allowing for detection of HPV DNA. It should be noted that the time between receiving the tumor block and date of extraction of DNA may lead to decreased sensitivity to detect the presence of HPV. However, the positive control Head and Neck tumor (positive for HPV type 16) used in this study was approximately 3 years old before DNA was extracted, which is a much longer time between receiving the block and extraction of DNA than any of the colorectal tumors. Therefore, we do not anticipate a decrease in ability to detect HPV in samples from the present study.
The age of onset of CRC in the samples (Israel mean = 72, Spain mean = 66 and US mean = 63) might hypothetically influence detection of HPV in the colon. Being that these individuals are older and therefore a ‘lower risk’ population, they are less likely to be infected with HPV, although colorectal cancer is indeed a disease of older populations. The youngest patients in our sample provide some evidence that even among younger patients, HPV is not detected (Israel = 38 years old, Spain = 23 years old, US = 20 years old). There is also a higher percentage of colon cancer cases (77% colon) than rectum cases (22% rectal, 1% unknown), whereas previous reports suggest that the proximity of the rectum to the anal canal may play a role in HPV infection of the rectum but not the colon. However, we did not detect HPV in rectal or colon cancers.
In summary, careful methodological assessment of HPV in an internationally representative series of colorectal cancer confirms the early reports by the Shah and Schroyer groups that HPV is not found in adenocarcinoma of the colon or rectum. Although several recent small studies have reported exceptionally high rates of HPV-positivity in colorectal adenocarcinoma, these reports are not consistent with the known tropism of HPV to squamous epithelium, the recognized pathobiology of squamous carcinoma compared to adenocarcinoma, or our careful international survey. We conclude that HPV infection is not a meaningful risk factor for adenocarcinoma of the colon or rectum.
References
Bosch FX, de Sanjose S (2002) Human papillomavirus in cervical cancer. Curr Oncol Rep 4(2):175–183
Schiffman MH, Bauer HM, Hoover RN, Glass AG, Cadell DM, Rush BB et al (1993) Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 85(12):958–964
zur Hausen H (1996) Papillomavirus infections—a major cause of human cancers. Biochim Biophys Acta 1288(2):F55–F78
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV et al (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348(6):518–527
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV et al (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19
Schlecht NF, Kulaga S, Robitaille J, Ferreira S, Santos M, Miyamura RA et al (2001) Persistent human papillomavirus infection as a predictor of cervical intraepithelial neoplasia. JAMA 286(24):3106–3114
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S (2007) Human papillomavirus and cervical cancer. Lancet 370(9590):890–907
Madeleine MM, Daling JR, Carter JJ, Wipf GC, Schwartz SM, McKnight B et al (1997) Cofactors with human papillomavirus in a population-based study of vulvar cancer. J Natl Cancer Inst 89(20):1516–1523
Goffin F, Mayrand MH, Gauthier P, Alobaid A, Lussier C, Provencher D et al (2006) High-risk human papillomavirus infection of the genital tract of women with a previous history or current high-grade vulvar intraepithelial neoplasia. J Med Virol 78(6):814–819
Madsen BS, Jensen HL, van den Brule AJ, Wohlfahrt J, Frisch M (2008) Risk factors for invasive squamous cell carcinoma of the vulva and vagina—population-based case-control study in Denmark. Int J Cancer 122(12):2827–2834
Daling JR, Madeleine MM, Schwartz SM, Shera KA, Carter JJ, McKnight B et al (2002) A population-based study of squamous cell vaginal cancer: HPV and cofactors. Gynecol Oncol 84(2):263–270
Daling JR, Sherman KJ (1992) Relationship between human papillomavirus infection and tumours of anogenital sites other than the cervix. IARC Sci Publ 119:223–241
Frisch M, Glimelius B, van den Brule AJ, Wohlfahrt J, Meijer CJ, Walboomers JM et al (1997) Sexually transmitted infection as a cause of anal cancer. N Engl J Med 337(19):1350–1358
Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA et al (2004) Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer 101(2):270–280
Bjorge T, Engeland A, Luostarinen T, Mork J, Gislefoss RE, Jellum E et al (2002) Human papillomavirus infection as a risk factor for anal and perianal skin cancer in a prospective study. Br J Cancer 87(1):61–64
Tornesello ML, Duraturo ML, Losito S, Botti G, Pilotti S, Stefanon B et al (2008) Human papillomavirus genotypes and HPV16 variants in penile carcinoma. Int J Cancer 122(1):132–137
Heideman DA, Waterboer T, Pawlita M, Delis-van Diemen P, Nindl I, Leijte JA et al (2007) Human papillomavirus-16 is the predominant type etiologically involved in penile squamous cell carcinoma. J Clin Oncol 25(29):4550–4556
Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA et al (2005) Penile cancer: importance of circumcision, human papillomavirus and smoking in in situ and invasive disease. Int J Cancer 116(4):606–616
Rubin MA, Kleter B, Zhou M, Ayala G, Cubilla AL, Quint WG et al (2001) Detection and typing of human papillomavirus DNA in penile carcinoma: evidence for multiple independent pathways of penile carcinogenesis. Am J Pathol 159(4):1211–1218
Iwasawa A, Kumamoto Y, Fujinaga K (1993) Detection of human papillomavirus deoxyribonucleic acid in penile carcinoma by polymerase chain reaction and in situ hybridization. J Urol 149(1):59–63
Ritchie JM, Smith EM, Summersgill KF, Hoffman HT, Wang D, Klussmann JP et al (2003) Human papillomavirus infection as a prognostic factor in carcinomas of the oral cavity and oropharynx. Int J Cancer 104(3):336–344
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L et al (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720
Ringstrom E, Peters E, Hasegawa M, Posner M, Liu M, Kelsey KT (2002) Human papillomavirus type 16 and squamous cell carcinoma of the head and neck. Clin Cancer Res 8(10):3187–3192
Torrente MC, Ampuero S, Abud M, Ojeda JM (2005) Molecular detection and typing of human papillomavirus in laryngeal carcinoma specimens. Acta Otolaryngol 125(8):888–893
Almadori G, Cadoni G, Cattani P, Posteraro P, Scarano E, Ottaviani F et al (1996) Detection of human papillomavirus DNA in laryngeal squamous cell carcinoma by polymerase chain reaction. Eur J Cancer 32A(5):783–788
Manjarrez ME, Ocadiz R, Valle L, Pacheco C, Marroquin A, De la Torre C et al (2006) Detection of human papillomavirus and relevant tumor suppressors and oncoproteins in laryngeal tumors. Clin Cancer Res 12(23):6946–6951
Brandwein MS, Nuovo GJ, Biller H (1993) Analysis of prevalence of human papillomavirus in laryngeal carcinomas. Study of 40 cases using polymerase chain reaction and consensus primers. Ann Otol Rhinol Laryngol 102(4 Pt 1):309–313
Perez LO, Abba MC, Laguens RM, Golijow CD (2005) Analysis of adenocarcinoma of the colon and rectum: detection of human papillomavirus (HPV) DNA by polymerase chain reaction. Colorectal Dis 7(5):492–495
Bodaghi S, Yamanegi K, Xiao SY, Da Costa M, Palefsky JM, Zheng ZM (2005) Colorectal papillomavirus infection in patients with colorectal cancer. Clin Cancer Res 11(8):2862–2867
Buyru N, Tezol A, Dalay N (2006) Coexistence of K-ras mutations and HPV infection in colon cancer. BMC Cancer 6:115
Damin DC, Caetano MB, Rosito MA, Schwartsmann G, Damin AS, Frazzon AP et al (2007) Evidence for an association of human papillomavirus infection and colorectal cancer. Eur J Surg Oncol 33(5):569–574
Shah KV, Daniel RW, Simons JW, Vogelstein B (1992) Investigation of colon cancers for human papillomavirus genomic sequences by polymerase chain reaction. J Surg Oncol 51(1):5–7
Shroyer KR, Kim JG, Manos MM, Greer CE, Pearlman NW, Franklin WA (1992) Papillomavirus found in anorectal squamous carcinoma, not in colon adenocarcinoma. Arch Surg 127(6):741–744
de Roda Husman AM, Walboomers JM, van den Brule AJ, Meijer CJ, Snijders PJ (1995) The use of general primers GP5 and GP6 elongated at their 3′ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol 76(Pt 4):1057–1062
Kleter B, van Doorn LJ, ter Schegget J, Schrauwen L, van Krimpen K, Burger M et al (1998) Novel short-fragment PCR assay for highly sensitive broad-spectrum detection of anogenital human papillomaviruses. Am J Pathol 153(6):1731–1739
van den Brule AJ, Pol R, Fransen-Daalmeijer N, Schouls LM, Meijer CJ, Snijders PJ (2002) GP5+/6+ PCR followed by reverse line blot analysis enables rapid and high-throughput identification of human papillomavirus genotypes. J Clin Microbiol 40(3):779–787
Kleter B, van Doorn LJ, Schrauwen L, Molijn A, Sastrowijoto S, ter Schegget J et al (1999) Development and clinical evaluation of a highly sensitive PCR-reverse hybridization line probe assay for detection and identification of anogenital human papillomavirus. J Clin Microbiol 37(8):2508–2517
Poynter JN, Gruber SB, Higgins PD, Almog R, Bonner JD, Rennert HS et al (2005) Statins and the risk of colorectal cancer. N Engl J Med 352(21):2184–2192
Moreno V, Gemignani F, Landi S, Gioia-Patricola L, Chabrier A, Blanco I et al (2006) Polymorphisms in genes of nucleotide and base excision repair: risk and prognosis of colorectal cancer. Clin Cancer Res 12(7 Pt 1):2101–2108
Giordano TJ, Shedden KA, Schwartz DR, Kuick R, Taylor JM, Lee N et al (2001) Organ-specific molecular classification of primary lung, colon, and ovarian adenocarcinomas using gene expression profiles. Am J Pathol 159(4):1231–1238
Jacobs MV, Snijders PJ, van den Brule AJ, Helmerhorst TJ, Meijer CJ, Walboomers JM (1997) A general primer GP5+/GP6(+)-mediated PCR-enzyme immunoassay method for rapid detection of 14 high-risk and 6 low-risk human papillomavirus genotypes in cervical scrapings. J Clin Microbiol 35(3):791–795
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Ades AE, Lu G, Higgins JP (2005) The interpretation of random-effects meta-analysis in decision models. Med Decis Making 25(6):646–654
Klug SJ, Molijn A, Schopp B, Holz B, Iftner A, Quint W et al (2008) Comparison of the performance of different HPV genotyping methods for detecting genital HPV types. J Med Virol 80(7):1264–1274
Acknowledgements
This study was supported in part by NCI R01 CA81488, and the University of Michigan Comprehensive Cancer Center core grant (5P30 CA46592).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gornick, M.C., Castellsague, X., Sanchez, G. et al. Human papillomavirus is not associated with colorectal cancer in a large international study. Cancer Causes Control 21, 737–743 (2010). https://doi.org/10.1007/s10552-010-9502-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9502-0