Abstract
Background
There is considerable evidence that birth weight is positively associated with breast cancer risk, and seven single-nucleotide polymorphisms (SNPs) have been conclusively associated with this risk. We have hypothesized that breast cancer susceptibility loci may have a greater influence on breast cancer risk among women with higher birth weight, who are expected to have a larger pool of mammary stem cells that are susceptible to malignant transformation.
Patients and methods
In the context of a nationwide, population-based case–control study in Sweden, we retrieved recorded birth weight for 693 breast cancer cases and 747 control women who were also genotyped for most or all of the seven recently documented breast cancer susceptibility SNPs: rs2981582, rs12443621, rs8051542, rs3803662, rs889312, rs13281615, and rs3817198.
Results
We grouped heterozygotes with homozygotes for the wild-type allele, and we found a marginally significant interaction (p~0.07) between birth weight and rs2981582 (FGFR2), the genotype repeatedly identified as the top hit in genome-wide association studies. There were similar, though not significant, patterns for the other six SNPs.
Conclusions
Although our findings require confirmation, we found suggestive evidence that genetic susceptibility modifies the positive association of birth weight with breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Family history of breast cancer is an established risk factor for breast cancer [1]. Twin studies indicate that inherited genetic influences account for approximately 27% of the variation in breast cancer risk [2]. The proportion of breast cancer attributable to rare highly penetrant genes, such as BRCA1 and BRCA2, however, is probably no more than around 5% [3]. Hence, a number of more common variants in lower penetrance genes likely contribute substantially to the familial occurrence of breast cancer and account for higher attributable rates. Accumulating data support such a polygenic model of inherited breast cancer risk [4], in which each gene may confer only a small amount of risk individually—yet in combination, they would result in a noticeable increase in susceptibility to breast cancer [5, 6]. Recently, genome-wide association studies (GWAS) have provided the opportunity to comprehensively search the genome, in an unbiased approach for genetic variants with even modest associations with disease [7]. Through this approach, three GWAS have identified novel breast cancer susceptibility loci [8–10]. The Breast Cancer Association Consortium (BCAC) conducted a multi-stage genome-wide association study of breast cancer and identified seven single-nucleotide polymorphisms (SNPs) associated with breast cancer risk. These variants were genome-wide significant after replication in its final stage of 21,860 cases and 22,578 controls from 22 studies [8]. The Swedish and Singaporean Breast Cancer Association Consortium (SASBAC) contributed to the final replication stage in this consortium.
There is also considerable evidence that birth weight and other aspects of fetal growth are associated with breast cancer risk in later life [11–16]. Although the mechanisms underlying this association are poorly understood, it has been suggested that the size of the mammary stem cell pool and eventually mammary gland mass may represent intermediate manifestations of the early life processes that modulate risk of this disease in adult life [17, 18].
We hypothesized that, if breast cancer risk is positively associated with the size of the pool of mammary stem cells, this association would be stronger in the presence of breast cancer susceptibility loci and weaker or even absent in the absence of such loci. Evidence of an interaction of this type would provide strong support to the hypothesis that the mammary stem cell pool is critical in the intrauterine roots of breast cancer risk in adult life. Using birth weight as the only documented proxy of the stem cell pool [19], we examined the association between birth weight, breast cancer susceptibility loci, and risk of breast cancer in the SASBAC study. To our knowledge, no gene–environment interactions have been identified with these novel breast cancer susceptibility loci.
Subjects and methods
Study population
The Swedish and Singaporean Breast Cancer Association Consortium (SASBAC) rely on a Swedish case–control study, with genotyping conducted in Singapore. More specifically, the women included are participants in the Cancer and Hormones Replacement in Sweden (CAHRES) study, a nationwide, population-based case–control study of incident breast cancer among women 50–74 years old, born in Sweden and living there at any time between October 1, 1993, and March 31, 1995 [20–22]. In this study, breast cancer cases were identified through the six Swedish regional cancer registries in which 98% of all diagnosed cancer cases in Sweden are reported. A total of 3,979 eligible breast cancer cases were identified and invited to participate by their physicians. Of those invited, 3,345 (84%) agreed to participate. Non-participation was due to inability to contact patient or patient refusal in 11% of women and to patient death or physician refusal in the remaining instances. To serve as control subjects, a total of 4,188 women were randomly selected from the general population, according to the expected age frequency distribution of cases (in 5-year age groups), through the Total Population Register (currently the Tax Authority), which also provided their addresses and national registration numbers—unique ten-digit numbers assigned to all Swedish residents. Of the 4,188 controls selected in the study, 3,454 (82%) agreed to participate. Detailed information was obtained through a self-administered questionnaire mailed to cases and controls (20–22). The questionnaire covered, among others, reproductive and menstrual histories, family history of breast cancer, benign breast disease, mammography examinations, use of oral contraceptives, use of hormone replacement therapy, current and past anthropometric measurements, profession, alcohol consumption, and cigarette smoking.
Women with a previous cancer (other than non-melanoma skin cancer and cancer in situ of the cervix; n = 112 cases and 91 controls), as well as women who were premenopausal (n = 198 cases and 152 controls), or had unknown menopausal status (n = 217 cases and 100 controls) were excluded. Thus, there were 2,818 cases and 3,111 controls eligible for this study.
The present study was approved by the Institutional Review Boards at Karolinska Institutet, Uppsala University, Harvard School of Public Health and US Department of Defense, and was performed in compliance with the Helsinki Declaration.
Blood sampling
For genotype analysis, 1,500 women with invasive breast cancer and 1,500 controls were originally selected. For reasons unrelated to the objectives of the present investigation, all remaining eligible cases and controls who had taken menopausal hormone treatment for at least 4 years (191 cases and 108 controls), all women with self-reported diabetes mellitus (110 cases and 104 controls), and another 345 controls from the parent study selected for a parallel investigation were also included in the genotype analysis. Thus, 1,801 women with breast cancer and 2,057 control women were selected for genotype analysis. We contacted the selected women by mail, and those who gave informed consent received a blood sampling kit by mail. We obtained blood samples from 1,321 (73.3%) eligible breast cancer patients and 1,524 (74.1%) control women, but for technical reasons genotyping was not performed for 7 cases and 9 controls. Thus, genotype analysis was eventually performed for 1,314 cases and 1,515 controls.
Birth records
We attempted to identify birth records for breast cancer cases and controls, using the Swedish national registration numbers. Using information from the birth registry, research assistants visited 120 hospital and medical record archives to locate the original birth records for the study participants. Because this study included births occurring between 1918 and 1945 throughout all of Sweden, a large number of births at this time had occurred at home, and birth characteristic information had never been measured or recorded. We were able to locate birth records or midwife journals with adequate information on birth characteristics for about 50% of the participants.
Using a detailed form, perinatal characteristic information from available birth records was abstracted. Birth weight in grams and twin status were consistently listed in birth records. Less consistently, information was provided on birth length, head circumference and placental weight. In total, there were 710 breast cancer cases and 770 controls with both genotype information and birth weight data. We excluded 15 cases and 22 controls who were twin members and/or had missing information on one or more covariates. Eventually, there were 695 breast cancer cases and 748 control women with birth characteristic data and information on at least one of the evaluated SNPs.
Genotyping
We isolated DNA from 3 ml of whole blood with the Wizard Genomic DNA Purification Kit (Promega, Madison, WI) in accordance with the manufacturer’s instructions. The current analysis focuses on the 7 SNPs identified from the BCAC study that replicated with genome-wide significance: rs2981582, rs12443621, rs8051542, rs889312, rs3817198, rs13281615, and rs3803662. Genotyping of these SNPs was conducted by Sequenom iPLEX and Taqman [8].
Statistical analysis
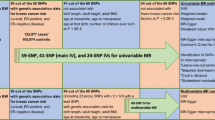
Initially, we examined the association between breast cancer risk and each of the following SNPs: rs2981582 (FGFR2), rs3803662 (TNRC9/LOC643714), rs889312 (MAP3K1), rs13281615 (8q24), rs3817198 (LSP1), rs12443621 (TNRC9/LOC643714), and rs8051542 (TNRC9/LOC643714). We considered these seven SNPs because they were identified in the BCAC genome-wide association study and were genome-wide significant after replication [8]. For each SNP, odds ratios (OR) and 95% confidence intervals (CI) for breast cancer risk were determined using logistic regression. To determine whether there was a linear trend with increasing number of variant alleles in each SNP, we calculated p values from Wald statistics including a continuous term in the model. Tests for interaction were based on a Wald test after inclusion of an interaction term. Data analysis was conducted using the SAS statistical software version 9.1 (SAS Institute, Cary, NC, USA). All p values presented are from two-sided tests of statistical significance.
Results
Table 1 shows the distribution of cases and controls by important breast cancer risk factors. As expected, cases were more likely to be nulliparous, have lower parity, have more previous benign breast disease, and more prior use of postmenopausal hormone therapy relative to controls. There was no difference in the age distributions because, as indicated, cases and controls were frequency matched on age. In these data, the established associations of breast cancer risk with age at menarche, body mass index (BMI), and birth weight were not evident.
Four of the seven breast cancer susceptibility loci identified from the BCAC genome-wide association study were significantly associated with breast cancer risk in this population with the strongest association for rs2981582, in line with previous reports [8, 9] (Table 2). Women homozygous for this allele had an almost twofold (OR = 1.99, 95% CI 1. 45–2.72) increased risk of breast cancer relative to women homozygous for the wild-type allele, whereas women heterozygous for this SNP were at slightly higher risk of breast cancer compared to homozygotes for the wild-type allele (OR = 1.25, 95% CI 0.99–1.57). Of the remaining six polymorphisms, trend tests with increasing number of high-risk alleles were statistically significant in three instances (rs12443621, rs13281615, and rs3803662), whereas in the three other instances, trends were in the direction expected on the basis of the BCAC study [8], but statistically not significant.
Because rs2981582 in intron 2 of FGFR2 has been repeatedly identified as the top hit in GWAS of breast cancer [8, 9] and has demonstrated the largest excess risk in our study, we first examined the interaction between rs2981582 and birth weight in relation to breast cancer risk (Table 3). To increase power without invoking linear trends, we grouped heterozygotes with homozygotes for the wild-type allele, because the difference in risk between homozygotes for the variant allele and heterozygotes is substantially larger than that between heterozygotes and homozygotes for the wild-type allele. We found a marginally significant interaction between birth weight and rs2981582 (p for interaction 0.07). As shown in Table 3, the interaction is generated by a strong, though marginally significant, positive association between birth weight and breast cancer risk among homozygotes for the variant allele (p for trend 0.07) and a weak, and clearly non-significant, inverse association between birth weight and breast cancer risk among heterozygotes and homozygotes for the wild-type allele (p for trend 0.68). Among women with the highest category of birth weight (>4,000 g), being homozygous for the rs2981582 variant was associated with an over fivefold increased risk of breast cancer (OR = 5.52, 95% CI 1.96–15.56) relative to women with wild-type alleles and similar birth weight.
We also examined a potential interaction between birth weight and the other 6 SNPs (Table 3), following the same approach used for rs2981582. Although none of the other SNPs demonstrated a significant interaction with birth weight, we did note a consistently positive association between birth weight and breast cancer risk among women homozygous for the high-risk allele.
Discussion
In this population-based study, we evaluated the associations with breast cancer risk of seven SNPs previously identified in three GWAS [8–10]. In the current study, the association with breast cancer risk was statistically significant with respect to four of these SNPs, more strongly so—as expected—with the rs2981582 genotype, which has repeatedly been identified as the top hit in GWAS. After grouping heterozygotes with homozygotes for the wild-type allele, we found a marginally significant interaction (p~0.07) between birth weight and the rs2981582 genotype with respect to breast cancer risk. For the six remaining SNPs, there was an apparently stronger positive association between birth weight and breast cancer risk among women homozygous for the high-risk alleles than among carriers or homozygotes for the wild-type allele, although relatively large p values and multitude of comparisons hinder firm conclusions. These results suggest that the association of genetic susceptibility with breast cancer risk might be stronger among women with a larger mammary stem cell pool, as this is reflected in higher birth weight [19].
It has been suggested that the documented association of breast cancer risk with birth weight [12, 15, 16] could reflect the underlying association of this risk with the size of the mammary stem cell pool [19] and eventually mammary gland mass [17, 18]. In women who carry high-risk alleles, the association of birth weight (as a correlate of mammary stem cell pool) with breast cancer risk would be expected to be stronger. Our findings are compatible with this hypothesis, although the study was perhaps not sufficiently powered to document interactions of modest strength. Of note, in our study, associations were not statistically significant for the main effect of three of the seven SNPs identified in the context of GWAS [8]. When our study was initiated, the effect size of SNPs that could be related to breast cancer was not known, precluding reliable power calculations.
The evidence that the association between birth weight and breast cancer could be modified by genetic susceptibility was stronger for the SNP in FGFR2 than for any of the other susceptibility loci. SNPs in intron 2 of FGFR2 have emerged as top hits from multiple GWAS of breast cancer [8, 9] and have been significantly associated with breast cancer risk in a number of populations including Europeans [8, 9], Asians [8, 23], Ashkenazi Jewish [24], and African American women [25]. FGFR2, a tyrosine kinase receptor belonging to a family of genes involved in growth and proliferation, is overexpressed in breast tumors [26] and may function as an oncogene [27, 28]. In the current study, we did observe a marginally significant positive association (p~0.07) between birth weight and breast cancer among women who were homozygous for the risk allele of FGFR2. An interpretation of these results is that susceptibility loci in an oncogene such as FGFR2 put individual cells at higher risk of malignant transformation. To the extent that birth weight is a proxy for glandular mass, having an increased number of mammary stem cells with high-risk alleles would be associated with an increased risk of breast cancer.
Four additional loci not included in this study have recently been identified from further genotyping efforts in the BCAC [29] and CGEMS [30] genome-wide association studies and more are likely to be identified with pooling of GWASs. These additional loci have more modest effect sizes than FGFR2, and it is unlikely that loci will be discovered from subsequent pooling efforts with the same magnitude of association with breast cancer as has been demonstrated with FGFR2 [30]. With the possible exception of the FGFR2 gene, we know little about the mechanisms by which other susceptibility loci influence breast carcinogenesis. In this context, it would be of interest to examine whether carriers of the major breast cancer genes, BRCA1 and BRCA2, are at a disproportionally high risk for breast cancer if born with high birth weight.
A possible interaction between genetic susceptibility loci and birth weight in relation to breast cancer risk has not been previously investigated. In fact, there are few reliable studies of gene–environment interactions and breast cancer risk. Our results are compatible with the hypothesis that the pool of mammary stem cells is critical in the intrauterine roots of breast cancer risk in adult life. This is because the size of the pool of mammary stem cells, as reflected in birth weight, appears to interact with genetic susceptibility in modulating breast cancer risk.
References
Hankinson S, Tamimi R (2008) Hunter D. Breast cancer. In: Adami HO, Hunter D, Trichopoulos D (eds) Textbook of cancer epidemiology, 2nd edn. Oxford University Press, New York, pp 403–445
Lichtenstein P, Holm NV, Verkasalo PK et al (2000) Environmental and heritable factors in the causation of cancer—analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 343:78–85
Lux MP, Fasching PA, Beckmann MW (2006) Hereditary breast and ovarian cancer: review and future perspectives. J Mol Med 84:16–28
Pharoah PD, Antoniou AC, Easton DF, Ponder BA (2008) Polygenes, risk prediction, and targeted prevention of breast cancer. N Engl J Med 358:2796–2803
Pharoah PD, Antoniou A, Bobrow M et al (2002) Polygenic susceptibility to breast cancer and implications for prevention. Nat Genet 31:33–36
Ponder BA, Antoniou A, Dunning A et al (2005) Polygenic inherited predisposition to breast cancer. Cold Spring Harb Symp Quant Biol 70:35–41
Hirschhorn JN, Daly MJ (2005) Genome-wide association studies for common diseases and complex traits. Nat Rev Genet 6:95–108
Easton DF, Pooley KA, Dunning AM et al (2007) Genome-wide association study identifies novel breast cancer susceptibility loci. Nature 447:1087–1093
Hunter DJ, Kraft P, Jacobs KB et al (2007) A genome-wide association study identifies alleles in FGFR2 associated with risk of sporadic postmenopausal breast cancer. Nat Genet 39:870–874
Stacey SN, Manolescu A, Sulem P et al (2007) Common variants on chromosomes 2q35 and 16q12 confer susceptibility to estrogen receptor-positive breast cancer. Nat Genet 39:865–869
Trichopoulos D (1990) Hypothesis: does breast cancer originate in utero? Lancet 335:939–940
Michels KB, Xue F (2006) Role of birthweight in the etiology of breast cancer. Int J Cancer 119:2007–2025
Lagiou P (2007) Intrauterine factors and breast cancer risk. Lancet Oncol 8:1047–1048
Xue F, Michels KB (2007) Intrauterine factors and risk of breast cancer: a systematic review and meta-analysis of current evidence. Lancet Oncol 8:1088–1100
dos Santos Silva I, De Stavola B, McCormack V (2008) Collaborative group on pre-natal risk factors and subsequent risk of breast cancer. Birth size and breast cancer risk: re-analysis of individual participant data from 32 studies. PLoS Med 5:e193
Park SK, Kang D, McGlynn KA et al (2008) Intrauterine environments and breast cancer risk: meta-analysis and systematic review. Breast Cancer Res 10:R8
Adami H-O, Persson I, Ekbom A et al (1995) The aetiology and pathogenesis of human breast cancer. Mutat Res 333:29–35
Trichopoulos D, Lagiou P, Adami HO (2005) Towards an integrated model for breast cancer etiology: the crucial role of the number of mammary tissue-specific stem cells. Breast Cancer Res 7:13–17
Strohsnitter WC, Savarese TM, Low HP et al (2008) Correlation of umbilical cord blood haematopoietic stem and progenitor cell levels with birth weight: implications for a prenatal influence on cancer risk. Br J Cancer 98:660–663
Magnusson C, Baron J, Persson I et al (1998) Body size in different periods of life and breast cancer risk in post-menopausal women. Int J Cancer 76:29–34
Magnusson CM, Persson IR, Baron JA et al (1999) The role of reproductive factors and use of oral contraceptives in the aetiology of breast cancer in women aged 50 to 74 years. Int J Cancer 80:231–236
Magnusson C, Baron JA, Correia N et al (1999) Breast-cancer risk following long-term oestrogen- and oestrogen-progestin-replacement therapy. Int J Cancer 81:339–344
Liang J, Chen P, Hu Z et al (2008) Genetic variants in fibroblast growth factor receptor 2 (FGFR2) contribute to susceptibility of breast cancer in Chinese women. Carcinogenesis 29:2341–2346
Gold B, Kirchhoff T, Stefanov S et al (2008) Genome-wide association study provides evidence for a breast cancer risk locus at 6q22.33. Proc Natl Acad Sci U S A 105:4340–4345
Udler MS, Meyer KB, Pooley KA et al (2009) FGFR2 variants and breast cancer risk: fine-scale mapping using African American studies and analysis of chromatin conformation. Hum Mol Genet 18:1692–1703
Penault-Llorca F, Bertucci F, Adélaïde J et al (1995) Expression of FGF and FGF receptor genes in human breast cancer. Int J Cancer 61:170–176
Theodorou V, Kimm MA, Boer M et al (2007) MMTV insertional mutagenesis identifies genes, gene families and pathways involved in mammary cancer. Nat Genet 39:759–769
Katoh M (2008) Cancer genomics and genetics of FGFR2 (Review). Int J Oncol 33:233–237
Ahmed S, Thomas G, Ghoussaini M et al (2009) Newly discovered breast cancer susceptibility loci on 3p24 and 17q23.2. Nat Genet 41:585–590
Thomas G, Jacobs KB, Kraft P et al (2009) A multistage genome-wide association study in breast cancer identifies two new risk alleles at 1p11.2 and 14q24.1 (RAD51L1). Nat Genet 41:579–584
Acknowledgments
This work was supported by the US Department of Defense Breast Cancer Research Program, Office of the Congressionally Directed Medical Research Programs [Innovator Award W81XWH-05-1-0314].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamimi, R.M., Lagiou, P., Czene, K. et al. Birth weight, breast cancer susceptibility loci, and breast cancer risk. Cancer Causes Control 21, 689–696 (2010). https://doi.org/10.1007/s10552-009-9496-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9496-7