Abstract
Objective
To analyse the association between types of physical activity (occupational, recreational and household, vigorous and overall) and risk of primary oesophageal (OAC) or gastric adenocarcinoma (GAC).
Methods
From nine European countries, 420,449 participants were recruited between 1991 and 2000 and followed-up for a mean of 8.8 years to register incident GAC and OAC. Information on physical activity (PA), diet, lifestyle and health-related variables was obtained at baseline. Helicobacter pylori infection status was considered in a subset of 1,211 participants. Analyses were repeated by tumour site (cardia/non-cardia) and histological type (intestinal/diffuse).
Results
During the follow-up, 410 GAC and 80 OAC occurred. A lower risk of overall and non-cardia GAC was found for increasing levels of a PA index which combined occupational PA with weekly time spent in sports and cycling. The hazard ratio (HR) of GAC was 0.69, 95% CI: 0.50–0.94, for the comparison between active and inactive participants according to the PA index (HR = 0.44, 95% CI:0.26–0.74, for non-cardia GAC). No effect was found for cardia tumours or histological subtypes of GAC. PA of any kind was not associated with OAC.
Conclusions
Overall and distal (non-cardia) gastric tumours were inversely associated with time spent on cycling and sports and a total PA index. No association was found for any type of PA and risk of cardia cancers of the stomach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The overall incidence of stomach adenocarcinomas, which represent 95% of total gastric tumours, has been steadily declining for several decades [1]. Nevertheless, gastric cancer still remains as the fourth most common type of cancer worldwide with 934,000 estimated new cases per year [2]. Furthermore, whereas this declining trend regards the incidence of the most common distal (i.e., non-cardia) forms of gastric adenocarcinomas (GAC), tumours of the proximal region of the stomach (cardia) and those of the gastro-oesophageal junction (GEJ) are increasing in high-income countries [3, 4]. Oesophageal cancer appears to follow a similar pattern, with overall figures falling but drastic increases in incident oesophageal adenocarcinomas (OAC) in Europe and the United States [3–5].
This common rising pattern of adenocarcinomas of the oesophagus and proximal stomach in Western affluent areas might suggest the existence of a shared environmental background that would account for a common aetiology of these less frequent, albeit increasing, types of cancer. Among those lifestyle factors that have been studied in relation to the risk of cancer, there is physical activity (PA). Several tumours, especially those of the colon, breast, lung and endometrium have been shown to be associated with –and, to a variable extent, preventable by– PA to date [6–10]. But the association in relation to gastric or oesophageal cancer has been less studied, and the evidence for a protective role of PA is not yet conclusive [6, 11–17]. Furthermore, most of the studies did not show results by site or histological type of the tumours. According to recently published prospective data, the putative protection of PA on gastric cancer might be dependent on tumour site [18] and sex [19, 20]. The evidence for an association between PA and oesophageal cancer is even more scarce [15, 16, 20].
Since previous evidence is limited, our aim was to analyse the association of PA with GAC and OAC within EPIC (European Prospective Investigation into Cancer and Nutrition), a large-scale prospective study conducted in over half a million participants across ten European countries.
Subjects and methods
EPIC is an ongoing multi-centre prospective study carried out in 521,448 participants, mostly aged 25–70, recruited in 23 centres from 10 European countries between 1992 and 2000. The main aim of the EPIC study was the investigation of lifestyle (including diet), metabolic and genetic determinants of cancer and other chronic diseases, with a large-scale prospective epidemiological setting. Extensive dietary information of the previous year was gathered by means of validated questionnaires. Anthropometrical and lifestyle data were collected at recruitment, as well as information related to health issues, such as history of previous illness (cancer, diabetes, cardiovascular problems), or surgical operations. Blood samples were collected from approximately 74% of the EPIC participants. The rationale and detailed methodological issues of the study have been addressed in full in previous publications [21, 22].
Subjects were recruited from the general adult population residing in a given town or geographical area. In some centres (France, Utrecht—the Netherlands and Naples—Italy), only women were invited to participate, whereas half of the Oxford cohort consisted of non-meat eaters, and a large proportion of participants from Spain and the Italian centres Ragusa and Turin were blood donors. All participants gave their written informed consent. The protocols of the study were approved by the Ethical Review boards of the International Agency for Research on Cancer (IARC, Lyon) and the respective national/local Ethical Committees.
Prevalent cancer cases of any site according to baseline questionnaires were excluded for the present analysis (n = 23,633). Further exclusions included subjects lost to follow-up (n = 2,041), those lacking dietary information (n = 6,839) and participants for whom PA data were not available, including the whole cohorts from Norway (n = 37,725) and Umeå (n = 13,297). Eight participants initially diagnosed with cancer but not confirmed as cancer cases after examination were excluded for analyses. The final study sample consisted of 420,449 participants (130,087 men and 290,362 women) from 9 European countries: Denmark, France, Germany, Greece, Italy, Spain, Sweden, the Netherlands and United Kingdom).
Exposure assessment
Occupational activity
Participants were asked to choose the category that most accurately described the physical demand of their job, out of four possible options: sedentary occupation (e.g., office work), standing occupation (e.g., hairdresser, shop assistant, security guard), manual work (e.g., plumber, electrician, carpenter, cleaner, nurse) and heavy manual work (e.g., docker, bricklayer, miner). Due to small numbers, manual and heavy manual categories were combined in the analyses.
Leisure-time PA (recreational and household)
Detailed information was gathered on time spent (in hours/week) on several recreational activities, both in summer and winter: walking, cycling (either when going to work or as a recreational activity), gardening, do-it-yourself activities and sport (e.g., soccer, keep-fit, swimming, jogging, tennis, gym…). Household activity was also assessed as the total number of hours per week spent doing the housework (cleaning, doing the washing, cooking, taking care of children…), and the flights of stairs climbed per day were registered. A leisure-time physical activity variable was then computed weighing the time spent in each activity (walking, cycling, gardening, sport, do-it-yourself activities, housework and stair climbing) by its specific intensity score [23] and expressed as MET-h/week. For leisure-time activity, sex-specific quartiles were computed.
Vigorous PA
Participants were asked to declare the total amount of time (in hours/week) when the engaging in any of these activities had been vigorous enough as to cause sweating or a faster heartbeat. Vigorous PA was defined as none, ≤2 and >2 h/week.
Overall activity index
An overall PA index was computed (Cambridge/Bilthoven PA Index, CPAI) by combining occupational activity and time spent in sport and cycling, as previously described [24]. This index consists of four ordinal categories: inactive, moderately inactive, moderately active and active (see “Appendix”). Participants not working or with missing occupational data were ranked according to time spent in sports and cycling, only. The CPAI was validated against objectives measures of physical activity energy expenditure (PAEE) as determined by heart rate monitoring (Spearman’s rhoCPAI-PAEE = 0.27, p < 0.05; Ulf Ekelund, personal communication).
Follow-up procedures and endpoint assessment
Incident gastric and oesophageal tumours were identified through population cancer registries, except in France, Germany, Greece and Naples where other methods, including health insurance records, cancer and pathology hospital registries or active follow-up were used. Mortality data were based in national or regional mortality registries. Participants were censored at the date of diagnosis of a first incident tumour, death, loss to follow-up due to emigration or other cause, or end of follow-up, whichever came first. Closing date was that of the last complete follow-up, between December 2002 and 2005, depending on the study centre.
The 2nd edition of the International Classification of Diseases for Oncology [25] was used to code site (C15.0–C15.9: oesophagus, C16.0: gastric cardia and GEJ; C16.1–C16.8: stomach, non-cardia) and morphology (adenocarcinoma codes 8140/3, 8144/3 and 8145/3). The histological type was classified as intestinal or diffuse following the Laurén Classification [26].
An expert panel of pathologists was in charge of the validation of diagnosis and classification of tumours. The panel included a representative from each country participating in EPIC and a coordinator. Almost 60% of gastric tumours (n = 245) were histologically confirmed as adeoncarcinomas by the panel. Pathology reports and protocol forms were used for tumour classification in 23% of cases (n = 97), and 17% of gastric adenocarcinomas (n = 68) were classified according to the codes provided by the cancer registries to the IARC central database. For oesophageal adenocarcinomas, these figures were 69% (n = 55), 15% (n = 12) and 16% (n = 13), respectively. The methodological issues on the panel validation procedures and criteria have been detailed elsewhere [27].
Statistical analyses
Mean values (and standard deviations) or percentages were used as descriptive statistics (Kruskall–Wallis and χ2 tests were used to assess statistical significance). The risks of incident adenocarcinomas of the stomach and oesophagus were modelled through proportional hazards Cox regression, with attained age as the underlying time variable [28]. Entry time was defined as age at recruitment and exit time as age at case diagnosis or censoring. Models were stratified on age (in 1-year categories), and centre, to control for differences in study design, diagnosis and follow-up procedures. All analyses were adjusted for sex, height (m), weight (kg), educational level (no studies, primary, technical/professional school, secondary, university and missing), smoking status (never smoker, former smoker who quit ≥10 years ago, former smoker who quit less than 10 years ago, former smoker of unknown quitting, current smoker of <15 cigarettes/day, current smoker of 15–25 cigarettes/day, current smoker of ≥25 cigarettes/day, current smoker of unknown amount of cigarettes/day and missing), alcohol consumption at recruitment (g/day), energy intake (kcal/day) and daily consumption of fruit, red meat and processed meat (in g/day).
Separate regression models were defined to evaluate specific risks of gastric cancer by site (cardia and non-cardia) and histology (intestinal and diffuse). The interaction of the physical activity index with age and body mass index was evaluated with two-sided likelihood ratio tests comparing models with and without the interaction term. We explored the potential modifying effect of Helicobacter pylori infection on the association between PA and risk of GAC. For this purpose, we used data from a previous nested case–control study of H. pylori infection in regard to risk of gastric cancer carried out within the EPIC cohort [29]. Details on laboratory methods have been reported elsewhere [29]. Unconditional logistic regression was applied to derive odds ratios of incident stomach adenocarcinoma risks by PA separately by infection status in the subset of cases and non-cases not meeting the exclusion criteria.
Analyses of the physical activity index were repeated after exclusion of cases diagnosed within the first 2 years (n = 93) from the date of recruitment. Sensitivity analyses were also performed excluding subjects with self-reported diabetes or cardiovascular problems at baseline (n = 90,371).
The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were taken into consideration in the writing of the manuscript [30].
Results
For the present analysis, mean follow-up time was 8.8 years completing 3.7 million person-years. A total of 410 first primary incident GAC cases (85% of total incident gastric cancer cases) and 80 OAC (78% of the total) occurred during this time. The distribution of adenocarcinoma cases of the stomach and oesophagus by participating country is presented in Table 1. Distal adenocarcinomas of the stomach were more frequent than those of the cardia region. A similar number of intestinal and diffuse tumours were found, overall. In regard to OAC, almost all incident cases were diagnosed in northern European countries (Denmark, Sweden and United Kingdom), with very low number of cases in the Mediterranean area.
Subjects in the highest quartile of recreational PA had the highest body mass index (BMI), the highest intake of fruit and vitamin C and the lowest consumption of alcohol, red meat and β-carotene (Table 2). These participants had also attained a lower educational level and were more likely to report diabetes or cardiovascular problems at baseline. Smoking status also differed by levels of PA. Most people in the upper PA quartile were never smokers, whereas the higher frequency of smokers of ≥15 cigarettes/day was found in the lowest PA quartile.
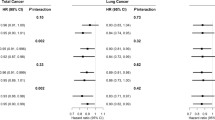
The main results of the evaluation of the prospective association between PA and risk of incident gastric and oesophageal adenocarcinomas are shown in Table 3. Levels of occupational activity were not related to GAC or OAC. No association was found for occupational or overall leisure-time PA and risk of GAC (neither all types nor site- or histological-specific tumours). Overall PA as estimated by the CPAI showed a significant reduction in GAC risk between 25 and 38% for different categories of PA when compared to the inactive group (hazard ratio (95% CI) = 0.69 (0.50–0.94) for active vs. inactive participants). This lower risk was consistent across categories with a statistically significant linear trend (p = 0.006). This result was restricted to non-cardia adenocarcinomas of the stomach, whereas it was not observed for intestinal or diffuse types. Vigorous PA was not associated with cancer risk in this analysis. For any variable studied, no effect of PA on the risk of developing OAC was found. Nevertheless, a closer analysis of different recreational activities revealed that participants regularly engaging in cycling and sport were less prone to develop GAC, especially at distal locations, whereas the habit of walking was associated with an increased GAC risk (Table 4).
In our analyses involving n = 1,211 participants of a prior nested case–control study [22], Helicobacter pylori was detected in 83.2% of cases (n = 163) and 68.7% of non-cases (n = 697). In this subset of participants, a significant interaction was detected between H. pylori infection with type of occupation and recreational PA (Table 5). Nevertheless, there were no significant associations or a clear trend in regard to GAC in separate analyses for infected and not infected participants. The association between the total PA index and GAC persisted when adjusting for H. pylori seroprevalence.
Discussion
Overall physical activity (PA) was associated with a significant reduction in risk of developing total and non-cardia gastric adenocarcinomas in this study. No association overall was seen for increased PA in regard to OAC. Even when previous epidemiological data suggested the possibility of an independent association between physical activity and risk of tumours of the stomach and the oesophagus [11, 15, 16], the analysis of such relationship had not been sufficiently addressed in the context of large prospective studies until recently. Our study provides valuable results for gaining insight into this association [17–20].
Physical activity at work
A sizeable amount of the daily PA among workers is determined by the physical demand of their job. A sedentary job might add to a sedentary lifestyle in the promotion of overweight and obesity [6]. Nevertheless, we did not find a significant risk reduction in those subjects with manual or standing occupations when compared to sedentary workers, in regard to GAC or OAC. These null results agree with previous existing literature [15, 22] and do not support the finding by Severson et al. [14] relating gastric cancer risk with moderate or heavy working activities.
Leisure-time activity
The daily amount of recreational PA, probably the most variable component of energy expenditure, largely reflects individual preferences and health-based decisions (household activities are less subject to free choice). As such, recreational activity represents the key PA component in terms of prevention [31]. Whereas our study does not support an overall protective role for leisure-time PA (neither household nor recreational PA separately; data not shown), a more in-depth analysis suggested an inverse association for cycling and sporting activities (but direct for walking) and risk of GAC (Table 4). This association was site-specific, restricted to distal tumours, but unrelated to the histological type. It could be speculated that only physiologically demanding activities would be of a sufficient magnitude as to exert a relevant health effect [11, 32], but our data do not fully support this speculation. On the one hand, only those activities with high MET values were inversely associated with GAC (METcycling/sport = 6). On the other hand, the amount of vigorous PA was not associated with risk of GAC or OAC. This finding is in disagreement with previous evidence [16]. However, reported vigorous PA would not necessarily be expected to decrease the risk of the disease. An exercise would cause sweating or increased heartbeat when the intensity is high, but also when the physical fitness of the individual is poor, which would have a very different meaning in relation to cancer risk. Besides, high-intensity PA may be less prone to misclassification than other activities of light or moderate intensity (e.g., walking). Our results would support the practice of regular exercise of moderate to high intensity rather than episodes of exhausting activity.
Overall physical activity
The CPAI (see “Appendix”) was designed to capture relevant variability in overall PA by combining PA at work and recreational activities (sports and cycling), so that the ranking of participants reflected actual differences in PA [22]. Our results suggest a protective role of PA against GAC (but not OAC), showing a significant decrease in risk of non-cardia tumours by increasing PA categories of the index. The hazard ratio (HR) for the ‘active’ relative to the ‘inactive’ group was 0.44 (95% CI: 0.26–0.74; p for trend = 0.001). For total GAC, this HR was 0.69 (95% CI: 0.50–0.94). Few studies have analysed the effect of PA and risk of gastric cancer separately by site or histological type. A previous case–control study conducted in Canada estimated average lifetime PA of the participants and found this measure to be inversely associated with risk of total and cardia gastric cancer risk [11]. For non-cardia tumours, the age- and sex-adjusted inverse association found was weakened after controlling for a series of confounders in multivariate models. All those variables were controlled for in our analyses, except the Western dietary pattern. Nevertheless, we adjusted for those elements of this pattern of greater relevance for gastric or oesophageal cancer risk, such as consumption of red and processed meat, fruit, alcohol and total energy intake [6, 33, 34]. Other potential confounders tested (such as vegetable and fibre intake) had no significant effect on the associations under study (<5% coefficient change) and were finally discarded due to efficiency reasons. Therefore, it is not likely that the discrepant results could be attributed to residual confounding by diet. Only two previous prospective studies have reported results by site [18, 20]. In the first, recreational PA was associated with a significant reduction in non-cardia cancer risk [18]. Unfortunately, the authors did not include cardia tumours in their analysis. The second one showed an independent association for non-cardia adenocarcinomas only [20]. According to the available evidence, PA may be regarded as protective in relation to distal (non-cardia) forms of gastric cancer, although an effect would be more expected to be observed at cardia locations, which are probably associated with obesity [35]. Further prospective evidence might be needed before these results can be considered as conclusive.
The mechanisms by which increased physical activity could affect the risk of gastric or other types of cancer are largely unknown. Both generalised and site-specific effects have been alleged to account for a protection of PA on overall cancer risk [6, 31, 36–38]. An effect on chronic inflammation or the modulation of oxidative stress would be plausible mechanisms, but it is unclear whether PA is able to inhibit any (or both) of them. In our study, we did not find indications that the significant association of PA and stomach cancer risk could be mediated by an effect of PA on body fat deposition (adjustment or stratification by BMI categories did not reveal significant interactions). The same was reported by others for overall [18] and non-cardia GAC [20]. Although a potential influence of sex-related factors cannot be discarded, we found no significant interactions by sex overall (data not shown). Of interest is that, recently, increased physical activity has been associated with the methylation level of CACNA2D3, a gene involved in the regulation of cell cycle [39]. This gene was found to be hypermethylated (i.e., silenced) in cultured gastric cancer cell lines [40]. Whether PA would be capable of epigenetic silencing of CACNA2D3 would first need to be established.
We studied the potential modulation of the PA effect on gastric cancer due to infection by H. pylori. Chronic inflammation of the gastric mucosa is an early event in H. pylori-associated gastric tumorigenesis. Our results do not clearly support that infection by H. pylori would be able to modulate the effect of PA on GAC risk. Although interactions by infection status were significant for different types of PA, the low number of cases analysed does not allow us to draw firm conclusions on this topic. Since no other study has taken into consideration H. pylori seroprevalence when analysing PA and GC risk, further research is needed to elucidate this point.
The EPIC study provides a unique epidemiological framework for testing PA and cancer interactions. The size and geographical distribution of the cohort was aimed at maximising the variability in exposures and confounders, and the prospective design makes it possible to assess the long-term effect of PA. The CPAI has been validated against measurements of energy expenditure based in heart rate monitoring. Although the correlation was not impressive (r = 0.27), the index was consistent across centres and suitable for ranking individuals (Ulf Ekelund, personal communication). Another strength is that bias due to outcome misclassification has largely been eliminated because the majority of cases were confirmed by a panel of expert pathologists. Further considerations apply when interpreting these results. First of all, the limited statistical power due to the low number of endpoint cases, in spite of the long follow-up period. The assessment of PA was indirect, based on an administered questionnaire, and some degree of misclassification may exist. Medical advice to increase PA could have occurred in participants with chronic disease at baseline. We therefore performed sensitivity analyses excluding those participants reporting diabetes or cardiovascular problems at recruitment. Neither the exclusion of these patients nor the GAC cases diagnosed within the first 2 years of follow-up modified the results noticeably. In spite of reported differences in recreational PA [41] and prevalence of H. pylori infection [42] across European countries, we found no significant heterogeneity by region (North vs. South; data not shown). The use of sex-specific cut-offs and the stratification by study centre should account for the variability in leisure-time PA by sex and country. A concern in relation to age arises when considering that ‘inactive’ participants were much older, on average, than those classified in any other PA category. While not an unexpected finding (older people reporting less PA), it is a disturbing one if taking into account that the ‘inactive’ group was set as the reference category for analyses. We cannot discard here the possibility of reverse causation if older people suffering from chronic gastritis (precursor of GAC) would have reduced their level of PA. In order to control for its effect in Cox models, we defined age as the underlying time variable and further stratified the models by 1-year categories, allowing comparisons within age strata instead of simply controlling for its effect in a cohort-wide model. In stratified analyses, the association with the CPAI remained significant only in the 55- to 60-year-old group, although there was no heterogeneity overall (data not shown). Finally, as in any observational study, the possibility of residual confounding cannot be totally discarded.
In conclusion, we present prospective data showing a decreased risk of gastric adenocarcinoma associated with higher levels of PA. This association manifested principally in non-cardia tumours, whereas no effect was found for PA in relation to intestinal/diffuse forms of GAC or OAC. Further studies should be aimed at clarifying whether these associations would be causal.
References
Forman D, Burley VJ (2006) Gastric cancer: global pattern of the disease and an overview of environmental risk factors. Best Pract Res Clin Gastroenterol 20:633–649
Boyle P, Levin B (2009) World cancer report 2008. IARC, Lyon
Bertuccio P, Chatenoud L, Levi F et al (2009) Recent patterns in gastric cancer: a global overview. Int J Cancer 125:666–673
Steevens J, Botterweck AA, Dirx MJ, van Den Brandt PA, Schouten LJ (2009) Trends in incidence of oesophageal and stomach cancer subtypes in Europe. Eur J Gastroenterol Hepatol
Wu H, Rusiecki JA, Zhu K, Potter J, Devesa SS (2009) Stomach carcinoma incidence patterns in the United States by histologic type and anatomic site. Cancer Epidemiol Biomarkers Prev 18:1945–1952
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington DC
Monninkhof EM, Elias SG, Vlems FA et al (2007) Physical activity and breast cancer: a systematic review. Epidemiology 18:137–157
Samad AK, Taylor RS, Marshall T, Chapman MA (2005) A meta-analysis of the association of physical activity with reduced risk of colorectal cancer. Colorectal Dis 7:204–213
Tardón A, Lee WJ, Delgado-Rodríguez M et al (2005) Leisure-time physical activity and lung cancer: a meta-analysis. Cancer Causes Control 16:389–397
Voskuil DW, Monninkhof EM, Elias SG, Vlems FA, van Leeuwen FE (2007) Physical activity and endometrial cancer risk, a systematic review of current evidence 1. Cancer Epidemiol Biomarkers Prev 16:639–648
Campbell PT, Sloan M, Kreiger N (2007) Physical activity and stomach cancer risk: the influence of intensity and timing during the lifetime. Eur J Cancer 43:593–600
Davey SG, Shipley MJ, Batty GD, Morris JN, Marmot M (2000) Physical activity and cause-specific mortality in the Whitehall study. Public Health 114:308–315
Nomura AM, Stemmermann GN, Chyou PH (1995) Gastric cancer among the Japanese in Hawaii. Jpn J Cancer Res 86:916–923
Severson RK, Nomura AM, Grove JS, Stemmermann GN (1989) A prospective analysis of physical activity and cancer. Am J Epidemiol 130:522–529
Vigen C, Bernstein L, Wu AH (2006) Occupational physical activity and risk of adenocarcinomas of the esophagus and stomach. Int J Cancer 118:1004–1009
Wannamethee SG, Shaper AG, Walker M (2001) Physical activity and risk of cancer in middle-aged men. Br J Cancer 85:1311–1316
Yun YH, Lim MK, Won YJ et al (2008) Dietary preference, physical activity, and cancer risk in men: national health insurance corporation study. BMC Cancer 8:366
Sjödahl K, Jia C, Vatten L, Nilsen T, Hveem K, Lagergren J (2008) Body mass and physical activity and risk of gastric cancer in a population-based cohort study in Norway. Cancer Epidemiol Biomarkers Prev 17:135–140
Inoue M, Yamamoto S, Kurahashi N, Iwasaki M, Sasazuki S, Tsugane S (2008) Daily total physical activity level and total cancer risk in men and women: results from a large-scale population-based cohort study in Japan. Am J Epidemiol 168:391–403
Leitzmann MF, Koebnick C, Freedman ND et al (2009) Physical activity and esophageal and gastric carcinoma in a large prospective study. Am J Prev Med 36:112–119
Riboli E, Kaaks R (1997) The EPIC Project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol 26(Suppl 1):S6–S14
Riboli E, Hunt KJ, Slimani N et al (2002) European prospective investigation into cancer and nutrition (EPIC): study populations and data collection. Public Health Nutr 5:1113–1124
Ainsworth BE, Haskell WL, Whitt MC et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498–S504
Wareham NJ, Jakes RW, Rennie KL et al (2003) Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr 6:407–413
World Health Organization (1990) International classification of diseases for oncology. Second Edition (ICD-O 2). WHO, Geneva
Laurén P (1965) The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 64:31–49
Carneiro F, Moutinho C, Pera G et al (2007) Pathology findings and validation of gastric and esophageal cancer cases in a European cohort (EPIC/EUR-GAST). Scand J Gastroenterol 42:618–627
Korn EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145:72–80
Palli D, Masala G, Del GG et al (2007) CagA+ Helicobacter pylori infection and gastric cancer risk in the EPIC-EURGAST study. Int J Cancer 120:859–867
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296
Hill MJ (1999) Diet, physical activity and cancer risk. Public Health Nutr 2:397–401
Friedenreich CM, Thune I (2001) A review of physical activity and prostate cancer risk. Cancer Causes Control 12:461–475
González CA, Pera G, Agudo A et al (2006) Fruit and vegetable intake and the risk of stomach and oesophagus adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Cancer 118:2559–2566
González CA, Jakszyn P, Pera G et al (2006) Meat intake and risk of stomach and esophageal adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC). J Natl Cancer Inst 98:345–354
Kubo A, Corley DA (2006) Body mass index and adenocarcinomas of the esophagus or gastric cardia: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 15:872–878
Friedenreich CM, Orenstein MR (2002) Physical activity and cancer prevention: etiologic evidence and biological mechanisms. J Nutr 132:3456S–3464S
Hardman AE (2001) Physical activity and cancer risk. Proc Nutr Soc 60:107–113
Pedersen BK, Hoffman-Goetz L (2000) Exercise and the immune system: regulation, integration, and adaptation. Physiol Rev 80:1055–1081
Yuasa Y, Nagasaki H, Akiyama Y et al. (2008) DNA methylation status is inversely correlated with green tea intake and physical activity in gastric cancer patients. Int J Cancer
Wanajo A, Sasaki A, Nagasaki H et al (2008) Methylation of the calcium channel-related gene, CACNA2D3, is frequent and a poor prognostic factor in gastric cancer. Gastroenterology 135:580–590
Haftenberger M, Schuit AJ, Tormo MJ et al (2002) Physical activity of subjects aged 50–64 years involved in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr 5:1163–1176
Webb PM, Crabtree JE, Forman D (1999) Gastric cancer, cytotoxin-associated gene A-positive Helicobacter pylori, and serum pepsinogens: an international study. The Eurogast Study Group. Gastroenterology 116:269–276
Acknowledgments
We would like to thank all EPIC participants for their collaboration.
Financial support
European Commission FP5 project (QLG1-CT-2001-01049). The EPIC study was funded by “Europe Against Cancer” Programme of the European Commission (SANCO); Ligue contre le Cancer (France); Société 3 M (France); Mutuelle Générale de l’Education Nationale; Institut National de la Santé et de la Recherche Médicale (INSERM); German Cancer Aid; German Cancer Research Center; German Federal Ministry of Education and Research; Danish Cancer Society; ISCIII of the Spanish Ministry of Health (RETICC RD06/0020); the participating regional governments and institutions of Spain; Cancer Research UK; Medical Research Council, UK; Greek Ministry of Health; Stavros Niarchos Foundation; Hellenic Health Foundation; Italian Association for Research on Cancer (AIRC); Dutch Ministry of Public Health, Welfare and Sports; Dutch Ministry of Health; Dutch Prevention Funds; LK Research Funds; Dutch ZON (Zorg Onderzoek Nederland); World Cancer Research Fund (WCRF); Swedish Cancer Society; Swedish Scientific Council; Regional Government of Skane, Sweden; Norwegian Cancer Society. Some authors are partners of ECNIS, a network of excellence of the EC (6FP contract 513943).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table 6.
Rights and permissions
About this article
Cite this article
Huerta, J.M., Navarro, C., Chirlaque, MD. et al. Prospective study of physical activity and risk of primary adenocarcinomas of the oesophagus and stomach in the EPIC (European Prospective Investigation into Cancer and nutrition) cohort. Cancer Causes Control 21, 657–669 (2010). https://doi.org/10.1007/s10552-009-9493-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9493-x