Abstract
Recently, the potential health effects of trans-fatty acid consumption have raised concerns. A few studies have examined the risk of colorectal cancer with increasing consumption of trans-fatty acids, but none investigated the risk of rectal cancer, which may have different risk factors than colon cancer. Our objective was to explore the relationship between trans-fatty acid consumption and distal colorectal (sigmoid, rectosigmoid, and rectal) cancer using a case–control study of Whites (n = 1,516) and African Americans (n = 392) in North Carolina from 2001 to 2006. Matched cases and controls were interviewed about demographic information, lifestyle factors, and diet. White cases reported higher mean consumption of trans-fatty acid than White controls, but mean consumption was similar for African American cases and controls. Relative to the lowest quartile, the highest quartiles of energy-adjusted trans-fatty acid consumption were positively associated with distal colorectal cancer for Whites [adjusted ORs for the third and fourth quartiles are 1.54 (95%CI: 1.12, 2.13) and 1.45 (95%CI: 1.04, 2.03), respectively]. Consumption was not associated with distal colorectal cancer in African Americans [adjusted ORs for the third and fourth quartiles are 0.98 (95%CI: 0.47, 2.05) and 0.87 (95%CI 0.42, 1.81), respectively]. In conclusion, high consumption of trans-fatty acids was positively associated with distal colorectal cancer among Whites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, colorectal cancer is the third leading cause of cancer death among both men and women, accounting for approximately 10% of all cancer deaths each year [1]. Diet is thought to play a large role in the development of colorectal cancer [2]. Total dietary fat has been studied as a potential risk factor for colorectal cancer, but no overall association has been found [3–8]. It is possible, however, that specific types of dietary fat may be associated with colorectal cancer.
trans-Fatty acid consumption has been linked to a variety of diseases, including heart disease and type II diabetes [9, 10]. An ecologic study demonstrated relationships between trans-fatty acids and the rates of prostate, breast, and colon cancer in Europe [11]. Therefore, we hypothesized that trans-fatty acid might be involved in increasing the risk of developing colorectal cancer. Other studies have been performed examining the association between colorectal cancer and trans-fatty acid consumption but the results have been inconsistent [12–17]. Further, the majority of etiologic studies combine cancers of the colon and rectum, but the risk factors for these cancers may be distinct. In the EPIC study cohort, waist circumference, waist-hip ratio, and physical inactivity were positively associated with colon but not rectal cancer [18]. Studies of milk/dairy consumption have also reported different associations for the two locations (inverse associations were observed for colon but not rectal cancer) [19, 20]. The hypothesis of different risk factors was also supported by a review of physical activity and cancers of the colon and rectum [21, 22].
In addition to combining cancers of the colon and rectum, few studies have explored whether the association differs by race. Previous studies of Whites and African Americans residing in North Carolina demonstrated that these populations have different consumption patterns for “fats, oils, and snacks,” a grouping that included trans-fatty acids [23]. We used data from the North Carolina Colon Cancer Study II (NCCCS II) to investigate the potential association between consumption of trans-fatty acids and distal colorectal cancer by race.
Materials and methods
Study population
The NCCCS II is a population-based, matched case–control study conducted in central and eastern North Carolina. Subjects were enrolled from 33 counties representing urban, suburban, and rural areas of the state. The study received approval for human subjects research University of North Carolina School of Medicine Institutional Review Board.
Cases were identified using the rapid case ascertainment system of the North Carolina Central Cancer Registry. Individuals with a first diagnosis of histologically confirmed sigmoid colon, rectosigmoid, or rectal adenocarcinoma between May 2001 and September 2006 were classified as potential cases. Using this approach, the Registry identifies potential cases and sends their pathology report to study investigators within 2 to 4 weeks of an individual’s diagnosis. To be eligible for the study, subjects had to be between the ages of 40 and 80 (individuals under the age of 40 with colorectal cancer were assumed to be unrepresentative of most colorectal cancer cases), reside in one of the 33 counties included in the study, be able to give informed consent, be able to complete an interview, have a North Carolina driver’s license or identification card (if under the age of 65), and had no denial by the primary physician for us to contact them.
Potential cases were sent a letter describing the study, which was followed by a call from a race-matched enrollment specialist. The specialist explained the study and answered any questions that the patient had about participating. Potential cases who could not be reached were called again during various times/days of the week. A maximum of fifty attempts were made by phone and two letters about the study and our desire to get in-touch were mailed. If the patient consented, then the enrollment specialist scheduled an in person interview. On average, interviews took place within 5 months of diagnosis. White cases were under-sampled for recruitment in order to increase the proportion of African American cases in the study population.
Controls, individuals with no diagnosis of colorectal cancer, were selected from two sources: North Carolina Department of Motor Vehicles records (for controls under the age of 65) and Center for Medicare and Medicaid Services records (for controls age 65 and older). Randomized recruitment [24] was used to sample controls according to the expected age (within 5-years strata), sex, and race distribution of the cases. Potential controls were contacted in a manner similar to that of the cases. The same eligibility requirements (with the exception of physician contact) were applied to the control population.
Data collection
Data were collected by trained nurse interviewers at the person’s house or another convenient location. Individuals were offered a $25 incentive for participation in the study. All participants were queried regarding demographic information, lifestyle factors, and medical history. Information on physical activity was ascertained using a 7-days recall previously validated in a group of men and women aged 20–59 [25–27]. Height and weight were measured at the interview, and participants were also asked about their weight 1 year prior to diagnosis (for cases) or interview (for controls).
Dietary information was collected using the Diet History Questionnaire (DHQ) developed at the National Cancer Institute (NCI) [28–30]. This food frequency questionnaire allows participants to choose the portion size and frequency of foods that they consume and also accounts for differences in types of fats added during cooking. Information was collected on the types and amounts of fats added before consumption as well. In order to capture usual diet across seasons, we asked participants to use a reference period of the year prior to cancer diagnosis (for cases) or interview (for controls). Diet*Calc, a program developed by the NCI to accompany the DHQ, was used to determine average daily nutrient intakes, including trans-fatty acids, for each subject. The Diet*Calc program applies information from a nutrient database to the food frequency/portion size data collected by the questionnaire. trans-Fatty acid values were added to the Diet*Calc program in 2003 based on information from the University of Minnesota’s Nutrient Data System for Research (NDS-R). Further information can be found elsewhere [31].
Data analysis
Participants who self-identified their race as “other” or were missing information on race were removed from the analysis (n = 61). Participants with extreme or implausible dietary values [<800 or >5,000 kcal day−1 for men (n = 74) and <600 or >4,000 kcal day−1 for women (n = 34)] were also excluded from the analysis.
Energy adjustment allowed us to examine trans-fatty acid consumption uncorrelated with total energy intake, which was necessary because total energy intake was correlated with trans-fatty acid consumption (correlation was 0.77 for Whites and 0.81 for African Americans) and was a risk factor for disease (a logistic regression model controlling for possible covariates showed energy intake to be associated with distal colorectal cancer). We used the residual method to model trans-fatty acid consumption adjusted for energy intake. Specifically, the values of each participant’s energy-adjusted intakes were estimated based on a regression model in which energy intake was the independent variable and trans-fatty acid intake was the dependent variable [32]. trans-Fatty acid consumption was then categorized into quartiles based on the energy-adjusted consumption of the control group.
We used unconditional logistic regression to investigate the relationship between trans-fatty acid consumption and distal colorectal cancer. Offset terms were included to account for the sampling probabilities used to identify eligible cases and controls [24]. Non-steroidal anti-inflammatory drug (NSAID) use and sex were assessed as potential effect measure modifiers, using tests of homogeneity and likelihood ratio tests comparing models with and without interaction terms (with an a priori p value cut-off for retention in the final model of <0.15). These variables were chosen because similar studies found that the association between trans-fatty acid consumption and colorectal cancer differed within strata of these variables [14, 15]. In addition, NSAID use has previously been inversely associated with colon cancer [33] and could play a biologic role if trans-fatty acid consumption promotes inflammation [34]. Likelihood ratio tests examining NSAID use as an effect measure modifier had p values of 0.36 in Whites and 0.90 in African Americans. p values for likelihood ratio tests examining sex as an effect measure modifier were 0.26 in Whites and 0.42 in African Americans. The following variables, which have been previously associated with colorectal cancer and may be associated with trans-fatty acid consumption, were assessed as potential confounders using backwards elimination with a 10% change-in-estimate criterion: body mass index (BMI) 1 year prior to diagnosis/interview (normal, overweight, and obese according to the World Health Organization cut-points), MET-minutes per day of physical activity (quartiles based on the control group), at least one-first-degree family member with a diagnosis of colorectal cancer (yes, no), NSAID use (never, rare, and frequent), smoking status (never, former, and current smoker), highest level of education (high school degree or less, some college, and college graduate/advanced degree), alcohol consumption (0, <1, ≥1 drink day−1), daily consumption of total fatty acids (energy-adjusted; quartiles based on the control group), saturated fatty acids consumption (quartiles based on the control group), calcium intake (dietary and supplemental; quartiles based on the control group), vegetable consumption (quartiles based on the control group), and red meat consumption (quartiles based on the control group). Although the actual number of missing observations was small, multiple imputation was performed to impute data for potential confounding variables with missing observations (physical activity: 5.2% missing, BMI 1 year prior: 3.7% missing, family history: 2.3% missing, smoking status: 0.9% missing, and NSAID use: 0.6% missing). The imputed data were generated based on values from other observations in the dataset without missing information. Characteristics that met our change-in-estimate criterion in one or both racial groups were included in the final models [highest level of education completed (among both groups), BMI 1 year prior to interview (among Whites), energy-adjusted total fatty acid consumption (among African Americans), and family history of colorectal cancer (among African Americans)]. In addition, the final model included a term for total energy intake, a term for stratum of matching variable (sex and 5-years categories of age), and an offset term (a constant within groups of age, sex, and race) to account for sampling probabilities [24]. The analysis was repeated using the data prior to imputation. The results were similar and therefore only the results of the models using multiple imputation are given.
In addition, we investigated the relationship between three specific tumor locations (sigmoid colon, rectosigmoid, or rectum) and trans-fatty acid consumption. Cases without a specified location were excluded from this analysis (n = 12). This analysis was performed using multinomial logistic regression. A limitation of this model is that we were not able to include offset terms. Potential confounders were reassessed for this model using backwards elimination with a 10% change-in-estimate criterion.
Results
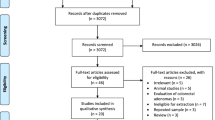
Among those who were eligible to participate in the study, 17% of cases and 26% of controls refused and 8% of cases and 18% of controls were untraceable or not reached. A total of 2,061 people completed interviews (1,045 cases and 1,016 controls), yielding study cooperation rates (interviewed/(interviewed + refused)) for cases and controls of 81 and 68% (Whites: 81 and 68%; African Americans: 82 and 65%) and response rates (interview/eligible) of 74 and 56% (Whites: 76 and 58%; African Americans: 70 and 46%), respectively.
Characteristics of the study population are shown according to case–control status and race in Table 1. Most of the study participants were at least 60 years old. A larger proportion of White and African American cases had a high school degree or less compared with controls (19.4 and 35.2% compared with 12.1 and 26.4%, respectively). Both White and African American cases were more likely than controls to be obese (36.7 and 49.5 vs. 28.3 and 41.3%, respectively). Cases had a higher average total energy intake compared to controls [mean (standard deviation) kcal/day of 2280.5 (855.8) vs. 2158.0 (813.6)]. African American cases and controls reported higher total energy intake than corresponding White cases and controls.
White cases had a higher mean intake of unadjusted trans-fatty acid than controls [mean (standard deviation) g day−1 of 6.1 (3.0) and 5.4 (2.9), respectively] (t-test p value < 0.001). The median intakes in g day−1 (interquartile range) among Whites were 5.6 (3.8, 7.7) for cases and 4.9 (3.2, 7.0) for controls (Wilcoxon rank-sum test p value < 0.001). Intakes were similar among African American cases and controls: a mean of 6.3 g day−1 for both cases and controls (standard deviation of 3.3 and 3.5, respectively) (t-test p value 0.97) and a median of 5.7 g day−1 (Wilcoxon rank-sum test 0.84). We determined which food items contributed most to trans-fatty acids consumption among both Whites and African Americans. The foods that each contributed over 5% to the White study population’s grams of trans-fatty acid intake were as follows: margarine (9.7%), biscuits (7.0%), fried fish (6.6%), fried potatoes (6.6%), crackers (5.8%), cookies/brownies (5.4%), and bread/rolls/croissants (5.1%). African Americans had fewer foods contributing more than 5% to the total trans-fatty acid consumption of the study population. Nonetheless, the major contributors were similar to those seen for Whites. They included: fried fish (12.6%), margarine (8.7%), biscuits (8.0%), fried potatoes (5.5%), and cookies/brownies (5.0%).
We modeled the association between total trans-fatty acid intake, prior to energy adjustment, and distal colorectal cancer, controlling for variables found to be confounders of the non-energy adjusted model (physical activity, education, calcium intake, and meat consumption), matching factors (sex and age), and offset terms. There was a positive relationship between increasing trans-fatty acid consumption and distal colorectal cancer for Whites. Odds ratios comparing the second, third, and fourth quartiles to the lowest quartile of consumption were 1.66 (95%CI: 1.20, 2.31), 1.74 (95%CI: 1.22, 2.48), and 2.44 (95%CI: 1.64, 3.65), respectively. For African Americans, the corresponding odds ratios were 1.22 (95%CI: 0.59, 2.52), 1.52 (95%CI: 0.68, 3.39), and 0.69 (95%CI: 0.30, 1.60), respectively.
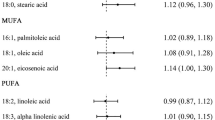
High consumption of energy-adjusted trans-fatty acids was positively associated with distal colorectal cancer for Whites (Table 2). The odds ratios for the energy-adjusted models were slightly decreased from those seen in the non-energy adjusted models. Both the third and fourth quartiles of trans-fatty acid consumption remained positively associated with distal colorectal cancer [third quartile: odds ratio 1.54 (95%CI: 1.12, 2.13); fourth quartile: odds ratio 1.45 (95%CI: 1.04, 2.03)]. A similar association was not seen for African Americans (Table 2) with the odds ratio comparing the fourth quartile to the lowest quartile being 0.87 (95%CI: 0.42, 1.81). We further examined the relationship looking at specific types of trans-fatty acid: 16:1 trans-hexadecenoic acid, 18:1 trans-octadecenoic acid, and 18:2 trans-octadecadienoic acid. The same relationships seen in total trans-fatty acid consumption were evident for these trans-fatty acid subtypes (Table 2).
Finally, we explored the relationships between consumption of trans-fatty acids and tumor location (sigmoid colon, rectosigmoid, or rectum). Although the results were more imprecise due to smaller numbers in each of the categories, in Whites, the trend toward a positive association was seen in the adjusted odds ratios for all three locations with moderate/high trans-fatty acid consumption compared to the lowest levels of consumption (Table 3). Again, no association was seen among African Americans (Table 3). Overall, associations with trans-fatty acid consumption did not clearly differ in either racial group based on the location of the cancer.
Discussion
In this study, distal colorectal cancer was positively associated with consumption of trans-fatty acids among Whites. Compared with the lowest quartile of consumption, the two highest quartiles of trans-fatty acid consumption had the largest increase in relative risk of colorectal cancer. This was true for all subtypes of trans-fatty acid (16:1 trans-hexadecenoic fatty acid, 18:1 trans-octadecenoic fatty acid, and 18:2 trans-octadecadienoic fatty acid). In addition, increased consumption of trans-fatty acids was also positively associated with cancer for all three locations: the sigmoid colon, rectosigmoid, and rectum.
Among African Americans there was no association between distal colorectal cancer and increased consumption of trans-fatty acid. This was true among all subtypes of trans-fatty acid and all locations examined. We cannot explain why the association differs from that seen in Whites. The results presented for African Americans could be the result of sampling error among the control population, inaccurate dietary reporting, or residual confounding by an unknown factor. It could also be reflective of true dietary differences between Whites and African Americans. There were differences in the foods that contributed the largest percentage of trans-fatty acids; in particular, fried fish accounted for a larger proportion of the trans-fatty acids consumed by African Americans than Whites. Possibly, the method of frying the fish utilized less trans-fatty acids than expected, resulting in misclassification of trans-fatty acid consumption. It is possible that the food frequency questionnaire we utilized did not adequately represent the true diet of African Americans living in North Carolina. This could also be a chance finding. Additional studies in larger samples of African Americans will be useful in further elucidating these associations.
Previous studies have reported inconsistent results for the association of trans-fatty acid consumption and colorectal cancer [12–17] and adenomas [35–37]. Two cohort studies conducted in women found no association between trans-fatty acid consumption and colorectal cancer. These studies also report no difference in the association by cancer location [12, 17]. However, two case–control studies found an association with colon [15] and colorectal [14] cancer among women. Neither study detected an association among men. Two other case–control studies reported no overall association [13, 16]. One of these was conducted among a similar population in North Carolina as part of the NCCCS I [16], but in that study, only individuals with colon cancer were enrolled as cases. This study also examined the association by race but showed no association for either Whites or African Americans. Only three studies examined the association between trans-fatty acids and colorectal adenomas [35–37]. Two utilized food groupings and reported colorectal adenomas to be associated with consumption of “sweetened baked goods” but concluded there was no association with overall trans-fatty acids [36, 37]. The other study was a cross-sectional study taking place in North Carolina [35]. It reported a positive association between the highest quartile of trans-fatty acid consumption and the prevalence of colorectal adenomas. Our study is different from these previous works in that we concentrate on the sigmoid colon, rectosigmoid, and rectum and examine if the associations differ by race.
There are several potential mechanisms by which trans-fatty acid consumption could affect the risk of distal colorectal cancer. First, trans-fatty acids themselves could irritate the colonic mucosa. A study of male rats found the fat excretion:intake ratio was two times higher for rats fed trans-fatty acid compared to rats fed cis-fatty acids [38]. Though to our knowledge, no similar studies have been performed in humans, it is possible that trans-fatty acids present in fecal matter irritate the distal colon and rectum, resulting in increased proliferation, inflammation, and oxidative stress. Higher levels of a well-accepted oxidative stress marker [urinary 8-iso-PGF(2alpha)] was found in participants of a small randomized trial who consumed 6.0 g of trans-fatty acid per day for 6 weeks when compared with those given a diet free of trans-fatty acids over the same period [39]. In addition, systemic inflammatory markers [soluble tumor necrosis factor α receptor 1 and 2 (sTNF-R1 and -R2)] have been positively associated with trans-fatty acid intake in women from the Nurses’ Health Study cohort [34]. Bile acids resulting from the digestion of trans-fatty acids may also play a role. Some studies have shown that bile acids in the colon are metabolized by bacteria, producing carcinogenic compounds and increasing cellular proliferation [40, 41]. Insulin resistance is another plausible underlying mechanism that might explain the roles of trans-fatty acids in the development of distal colorectal cancer. Studies have found that trans-fatty acid intake increased insulin sensitivity in subjects with diabetes or insulin resistance, although this effect was not seen in healthy subjects [42]. Increased insulin stimulates cell signaling pathways that increase cellular proliferation [43], which has been positively associated with the incidence of colorectal cancer in animals [44].
Currently, there is a campaign to have trans-fatty acids removed from foods. Certain localities, including New York City, have banned trans-fatty acids from commercial food outlets [45, 46]. As of January 1, 2006, all food products sold in the United States were required to list the amount of trans-fatty acids in the nutritional information on packaging [47]. Although enrollment of the present study did not end until August of 2006, we do not believe that the removal and labeling of foods affected our results for a few reasons. First, it is not consumption immediately prior to the development of cancer but more distant diet that is likely to be etiologically relevant, so diet during this period of 8 months is not likely to have drastically affected the biologic changes leading to cancer. Second, the Diet*Calc system uses trans-fatty acid values for foods prior to January 2006 (when many companies began removing them from their foods) so the amount of trans-fatty acids in the food supply matches that of the amount we assigned to each food participants reported consuming.
This study has certain strengths. The study was large, population-based, and used dietary instruments previously validated in other study populations [28]. The interviews were conducted in person and captured information on a wide array of potential colorectal cancer risk factors. Many of the risk factors presented in Table 1 have distributions in the direction we would expect, thereby giving further confidence in the study population. There are some limitations as well. First, although there were a large number of White participants, the number of African Americans in our study population was small, contributing to imprecision in risk estimates. As in all case–control study designs, there is the potential for selection and recall bias. Attempts to minimize selection bias included utilizing population-based registries and trying to maximize participation rates with multiple follow-up calls and letters. However, the response rates were lower for controls than cases. This is especially true for African American controls, who had a response rate of 46%. If controls who refused to participate had trans-fatty acid intakes different than controls who agreed to participate, selection bias could have been introduced into the study. Recall bias would be present if cases recalled their trans-fatty acid consumption differently than controls. This would be unlikely because individuals would have to know which foods contribute to trans-fatty acid intake. Due to the inconsistency of previous research on this topic, it is unlikely cases would attribute their cancer to trans-fatty acid consumption. However, it is possible that cases and controls differently remember consuming unhealthy foods and therefore report consumption of foods containing trans-fatty acids in a varied manner. Also, the food frequency questionnaire grouped all foods of a certain type together although the amounts of trans-fatty acids may actually vary within each type of food based on the brand, preparation, etc. Thus, we were unable to discern if people eating certain foods had more or less trans-fatty acids in their diet than people eating different brands of a similar food. In addition, we were not able to separately examine the association for natural and synthetic sources of trans-fatty acids. It is possible that these two sources may have different effects on the risk of distal colorectal cancer. Moreover, although the NCI DHQ has been validated with regard to total fatty acids, saturated fatty acids, polyunsaturated fatty acids, and other nutrients [28], it has not been validated specifically for trans-fatty acid consumption. Finally, trans-fatty acid consumption may simply be acting as a marker for an unhealthy diet. We attempted to reduce this bias by including other markers of healthy/unhealthy behaviors in the model as well, such as energy intake and physical activity.
In conclusion, we have demonstrated that increased consumption of trans-fatty acid is associated with an increased risk of cancers in the sigmoid colon, rectosigmoid, and rectum in Whites. There was no association among African Americans. This research contributes to the growing literature supporting negative health effects of trans-fatty acid. Reductions in consumption of trans-fatty acids and their removal from foods should be advocated.
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer statistics, 2007. CA Cancer J Clin 57:43–66
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington, DC
Franco A, Sikalidis AK, Solis Herruzo JA (2005) Colorectal cancer: influence of diet and lifestyle factors. Rev Esp Enferm Dig 97:432–448
Giovannucci E (2003) Diet, body weight, and colorectal cancer: a summary of the epidemiologic evidence. J Womens Health (Larchmt) 12:173–182
Giovannucci E, Goldin B (1997) The role of fat, fatty acids, and total energy intake in the etiology of human colon cancer. Am J Clin Nutr 66:1564S–1571S
Howe GR, Aronson KJ, Benito E et al (1997) The relationship between dietary fat intake and risk of colorectal cancer: evidence from the combined analysis of 13 case–control studies. Cancer Causes Control 8:215–228
Kushi L, Giovannucci E (2002) Dietary fat and cancer. Am J Med 113:63S–70S
Slattery ML, Potter JD, Duncan DM, Berry TD (1997) Dietary fats and colon cancer: assessment of risk associated with specific fatty acids. Int J Cancer 73:670–677
Odegaard AO, Pereira MA (2006) Trans fatty acids, insulin resistance, and type 2 diabetes. Nutr Rev 64:364–372
Zaloga GP, Harvey KA, Stillwell W, Siddiqui R (2006) Trans fatty acids and coronary heart disease. Nutr Clin Pract 21:505–512
Bakker N, Van’t Veer P, Zock PL (1997) Adipose fatty acids and cancers of the breast, prostate and colon: an ecological study. EURAMIC Study Group. Int J Cancer 72:587–591
Lin J, Zhang SM, Cook NR, Lee IM, Buring JE (2004) Dietary fat and fatty acids and risk of colorectal cancer in women. Am J Epidemiol 160:1011–1022
Nkondjock A, Shatenstein B, Maisonneuve P, Ghadirian P (2003) Assessment of risk associated with specific fatty acids and colorectal cancer among French-Canadians in Montreal: a case–control study. Int J Epidemiol 32:200–209
Theodoratou E, McNeill G, Cetnarskyj R et al (2007) Dietary fatty acids and colorectal cancer: a case–control study. Am J Epidemiol 166:181–195
Slattery ML, Benson J, Ma KN, Schaffer D, Potter JD (2001) Trans-fatty acids and colon cancer. Nutr Cancer 39:170–175
Vinikoor LC, Satia JA, Schroeder JC et al (2009) Associations between trans fatty acid consumption and colon cancer among whites and African Americans in the North Carolina colon cancer study I. Nutr Cancer 61:427--436
Limburg PJ, Liu-Mares W, Vierkant RA et al (2008) Prospective evaluation of trans-fatty acid intake and colorectal cancer risk in the Iowa Women’s Health Study. Int J Cancer 123:2717–2719
Pischon T, Lahmann PH, Boeing H et al (2006) Body size and risk of colon and rectal cancer in the European prospective investigation into cancer and nutrition (EPIC). J Natl Cancer Inst 98:920–931
Huncharek M, Muscat J, Kupelnick B (2009) Colorectal cancer risk and dietary intake of calcium, vitamin D, and dairy products: a meta-analysis of 26, 335 cases from 60 observational studies. Nutr Cancer 61:47–69
Jarvinen R, Knekt P, Hakulinen T, Aromaa A (2001) Prospective study on milk products, calcium and cancers of the colon and rectum. Eur J Clin Nutr 55:1000–1007
Slattery ML (2004) Physical activity and colorectal cancer. Sports Med 34:239–252
Friedenreich C, Norat T, Steindorf K et al (2006) Physical activity and risk of colon and rectal cancers: the European prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 15:2398–2407
Satia-Abouta J, Galanko JA, Potter JD, Ammerman A, Martin CF, Sandler RS (2003) Associations of total energy and macronutrients with colon cancer risk in African Americans and Whites: results from the North Carolina colon cancer study. Am J Epidemiol 158:951–962
Weinberg CR, Sandler DP (1991) Randomized recruitment in case–control studies. Am J Epidemiol 134:421–432
Ainsworth BE, Haskell WL, Whitt MC et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498–S504
Blair SN, Haskell WL, Ho P et al (1985) Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol 122:794–804
Richardson MT, Ainsworth BE, Jacobs DR, Leon AS (2001) Validation of the Stanford 7-day recall to assess habitual physical activity. Ann Epidemiol 11:145–153
Subar AF, Thompson FE, Kipnis V et al (2001) Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the eating at America’s Table Study. Am J Epidemiol 154:1089–1099
Thompson FE, Subar AF, Brown CC et al (2002) Cognitive research enhances accuracy of food frequency questionnaire reports: results of an experimental validation study. J Am Diet Assoc 102:212–225
Subar AF, Midthune D, Kulldorff M et al (2000) Evaluation of alternative approaches to assign nutrient values to food groups in food frequency questionnaires. Am J Epidemiol 152:279–286
Dixon LB, Zimmerman TP, Kahle LL, Subar AF (2003) Adding carotenoids to the NCI Diet History Questionnaire Database. J Food Comp Anal 16:269–280
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124:17–27
Baron JA, Sandler RS (2000) Nonsteroidal anti-inflammatory drugs and cancer prevention. Annu Rev Med 51:511–523
Mozaffarian D, Pischon T, Hankinson SE et al (2004) Dietary intake of trans fatty acids and systemic inflammation in women. Am J Clin Nutr 79:606–612
Vinikoor LC, Schroeder JC, Millikan RC et al (2008) Consumption of trans-fatty acid and its association with colorectal adenomas. Am J Epidemiol 168:289–297
McKelvey W, Greenland S, Chen MJ et al (1999) A case–control study of colorectal adenomatous polyps and consumption of foods containing partially hydrogenated oils. Cancer Epidemiol Biomarkers Prev 8:519–524
McKelvey W, Greenland S, Sandler RS (2000) A second look at the relation between colorectal adenomas and consumption of foods containing partially hydrogenated oils. Epidemiology 11:469–473
Colandre ME, Diez RS, Bernal CA (2003) Metabolic effects of trans fatty acids on an experimental dietary model. Br J Nutr 89:631–639
Kuhnt K, Wagner A, Kraft J, Basu S, Jahreis G (2006) Dietary supplementation with 11trans- and 12trans-18:1 and oxidative stress in humans. Am J Clin Nutr 84:981–988
O’Keefe SJ (2008) Nutrition and colonic health: the critical role of the microbiota. Curr Opin Gastroenterol 24:51–58
Reddy BS, Simi B, Patel N, Aliaga C, Rao CV (1996) Effect of amount and types of dietary fat on intestinal bacterial 7 alpha-dehydroxylase and phosphatidylinositol-specific phospholipase C and colonic mucosal diacylglycerol kinase and PKC activities during stages of colon tumor promotion. Cancer Res 56:2314–2320
Riserus U (2006) Trans fatty acids and insulin resistance. Atheroscler Suppl 7:37–39
Bruce WR, Giacca A, Medline A (2000) Possible mechanisms relating diet and risk of colon cancer. Cancer Epidemiol Biomarkers Prev 9:1271–1279
Lee DY, Lupton JR, Aukema HM, Chapkin RS (1993) Dietary fat and fiber alter rat colonic mucosal lipid mediators and cell proliferation. J Nutr 123:1808–1817
Department of Health and Mental Hygiene Board of Health (2006) Notice of adoption of an amendment (§81.50) to article 81 of the New York City Health Code
Okie S (2007) New York to trans fats: you’re out!. N Engl J Med 356:2017–2021
Food and Drug Administration (2003) Federal register, food labeling; trans fatty acids in nutrition labeling; consumer research to consider nutrient content and health claims and possible footnote or disclosure statements; final rule and proposed rule. National Archives and Records Administration 68:41433–41506
Acknowledgments
Grant support was received from the National Institutes of Health (P30DK34987, R01CA66635, T32DK07634).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vinikoor, L.C., Millikan, R.C., Satia, J.A. et al. trans-Fatty acid consumption and its association with distal colorectal cancer in the North Carolina Colon Cancer Study II. Cancer Causes Control 21, 171–180 (2010). https://doi.org/10.1007/s10552-009-9447-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9447-3