Abstract
Background
The Metropolitan Chicago Breast Cancer Taskforce was formed to address a growing black/white breast cancer mortality disparity in Chicago. The Taskforce explored three hypotheses: black women in Chicago receive fewer mammograms, black women receive mammograms of inferior quality, and black women have inadequate access to quality of treatment for breast cancer.
Methods
A total of 102 individuals from 74 Chicago area organizations participated in the Task Force participating in three work groups from January to September 2007. The work groups held focus groups of providers, organized town hall meetings in four Chicago communities, gathered black/white breast cancer mortality data for Chicago, the United States, and New York City, and conducted a mammography capacity and quality survey of mammography facilities.
Results
Chicago’s black and white breast cancer mortality rates were the same in 1980. By the late 1990s, a substantial disparity was present, and by 2005, the black breast cancer mortality rate was 116% higher than the white rate. In 2007, 206,000 screening mammograms were performed for women living in Chicago, far short of the 588,000 women in the 40–69 age range in Chicago. Facilities that served predominately minority women were less likely to be academic or private institutions (p < .03), less likely to have digital mammography (p < .003), and less likely to have dedicated breast imaging specialists reading the films (p < .003). Black women and providers serving them reported significant difficulties in accessing needed care for breast cancer screening and treatment.
Conclusion
There are significant access barriers to high quality mammography and treatment services that could be contributing to the mortality differences in Chicago. A metropolitan wide taskforce has been established to address the disparity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
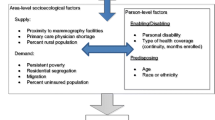
In October 2006, a group of Chicago breast cancer researchers released a report entitled “Breast Cancer in Chicago: Eliminating Disparities and Improving Mammography Quality” and called for a metropolitan Chicago summit to address the issue [1]. The major objective of the report was to present new data looking at breast cancer epidemiology in Chicago from 1980 to 2003. Trends in black/white female breast cancer incidence, mortality, stage of diagnosis and mammography screening rates in Chicago were analyzed. This was the first comprehensive study of breast cancer mortality disparity in Chicago and showed a substantial and growing disparity in Chicago black/white breast cancer mortality, a disparity that was greater than that reported for the United States as a whole [1, 2]. The authors of the report concluded that there were three possible hypotheses to explain the differences in breast cancer mortality: black women receive fewer mammograms, black women receive mammograms of inferior quality, and black women receive different quality of treatment for breast cancer, once diagnosed. In March 2007, a Breast Cancer Summit was held with researchers, providers, government, advocacy groups, survivors, and community groups to discuss the problem and propose solutions. The outcome of the Breast Cancer Summit was the Metropolitan Chicago Breast Cancer Taskforce that organized action workgroups around the three major hypotheses. Each workgroup was charged with reviewing the literature and data, conducting interviews and focus groups with providers, and holding Town Hall meetings with the public. The goal of the Task Force was to reach conclusions regarding the reasons for the mortality disparity, propose evidence-based recommendations for reducing the breast cancer mortality disparity in Chicago, and set forth strategies for successfully implementing them. The report, “Improving Quality and Reducing Disparities in Breast Cancer Mortality in Metropolitan Chicago”, [3] was released on 16 October 2007. This paper describes the process that was employed to create plans to eliminate the disparities, presents some of the data that guided the decision-making process, and discusses the key findings and recommendations of the Task Force.
Methods
A total of 102 individuals from 74 Chicago area organizations were involved in the Task Force and participated in the three Action workgroups addressing each of the three hypotheses. The Action workgroups met bi-weekly from March to September 2007 with additional meetings of workgroup subcommittees. The workgroups reviewed the literature, assembled the data, and proposed recommendations.
Breast cancer mortality rates for non-Hispanic black and non-Hispanic white women were assembled for Chicago using a methodology described elsewhere [2]. Breast cancer mortality rates from New York City for Black and White women were calculated (from vital records) using the same methodology. Breast cancer mortality from SEER was utilized to calculate the non-Hispanic Black and non-Hispanic breast cancer mortality rates in the United States from 1980 to 2005 [3, 4].
Town Hall meetings, designed to elicit community input, were held in four low income, predominantly African American Chicago neighborhoods and were facilitated by community leaders. The opinions and perspectives of 184 African American women were obtained regarding their perceptions of the causes of breast cancer disparity in Chicago, their ability to access screening and treatment, financial limitations, and other barriers. In addition, focus groups and interviews were held with safety net primary care providers, mammography technicians, and general radiologists who read mammograms in community hospital settings to identify their perspectives on breast cancer care in Chicago. A general solicitation to primary care physicians in private practice, those in community health centers, and those working in the County Health system produced a group of eight diverse physicians and physician assistants who provided care to under represented minorities in Chicago. They participated in a focus group on the mammography process as it impacted their patients and practices. In addition, eight mammography technologists representing six Chicago area institutions were also participants in a separate focus group. Phone surveys of eight individuals involved with breast cancer treatment across the metropolitan area including medical oncologists, surgeons, and health advocates were also conducted to elicit ideas regarding barriers to treatment. The focus groups used a structured questionnaire and were facilitated. The phone surveys of eight radiologists from eight Chicago institutions were conducted by research assistants. The detailed accounts of these focus groups and surveys are included in the Taskforce report [3].
A mammography capacity survey in Chicago was conducted. All 87 providers of mammography services in metropolitan Chicago were identified from the Food and Drug Administration Web site of accredited facilities [5] and were mailed surveys. Eighty-two percent of Chicago area mammography providers returned these surveys (86% from Chicago facilities and 76% from suburban facilities), many after being individually contacted by Task Force members [3]. Mammography capacity was calculated using the Government Accountability Office methodology [3, 6]. For the 18% nonreporting facilities, an estimate of capacity was derived by using the average number of mammograms provided at the reporting facilities as the imputed baseline for capacity calculations.
Of 49 mammography screening facilities within the city of Chicago, 42 facilities completed the 35 question surveys and 40 facilities including all major academic facilities provided data on patient race/ethnicity. In order to examine potential differences in the quality of mammography services by race, facilities were surveyed about quality-related issues including the availability of digital mammography and ultrasound, the qualifications of those reading the mammograms, whether the facility was an academic, private nonacademic or public facility, and whether abnormal results were delivered face-to-face. A facility was considered predominately minority if greater than 75% of the clientele were reported to be either African–American or Hispanic. A facility was considered predominately white if >75% of their clientele were reported to be white. p values were calculated with chi-squared test for contingency tables or by Fischer Exact test based on weighted cell count rounded to the nearest integer. The lower of the two p values is reported.
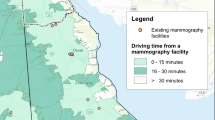
Finally, all 25 Chicago area acute care healthcare institutions were surveyed by phone to ascertain the extent of the breast cancer treatment facilities available and whether these treatment services had received approval from the American College of Surgeons Commission on Cancer [7]. There are 77 distinct community areas in Chicago of which 31 are predominately Black, 20 predominately white, 12 Hispanic, and 14 mixed. Maps depicting the 25 communities in Chicago with the highest breast cancer mortality were assembled and overlaid with the locations of the fourteen Chicago institutions that had American College of Surgeons Commission on Cancer approved cancer programs.
Results
Figure 1 presents the main findings that stimulated the work of the Task Force, including two more recently acquired years’ data. The breast cancer mortality rates for black and white women in Chicago were the same in 1980 (38 per 100,000, age adjusted). Rates remained similar until the early 1990s when they began to diverge. By the late 1990s, a substantial disparity was present. By 2005, the mortality gap had widened to 116% with the age-adjusted black mortality rate of 41.3 more than twice that of the age-adjusted white rate of 19.2. Thus, from a position of equity in 1980, a large gap in black/white breast cancer mortality emerged and continued to widen through 2005. This occurred because the black rate remained constant over this period, while the white rate declined by almost one half (49%).
Figure 2 presents the black/white breast cancer mortality disparity in Chicago, the United States, and New York City for the years 2000–2005. While there are black/white breast cancer mortality disparities for all three locations, the disparity has been smaller in the United States and New York City over the same time period, while the gap in Chicago has continued to grow. From 2002 through 2005, the breast cancer mortality disparity in Chicago has on average been twice that of the Unites States and five times that of the New York City.
Based on the response to the mammography survey, 206,000 screening mammograms were performed for women living in Chicago in 2007, far short of the 588,000 women in the 40–69 age range in Chicago according to the 2000 Census. According to the mammography centers’ responses, there is potential for 254,000 screening mammograms in Chicago. Using the Government Accountability Office methodology for determining mammography capacity, Chicago has the maximum potential to perform 371,000 mammograms [3, 6]. Both of these estimates are far short of the numbers needed to provide annual screening for the 588,000 women.
Predominantly minority populations were more likely to have their mammograms performed at public institutions (31 vs. 0%), less likely to be screened at academic (27 vs. 71%) and privatenonacademic institutions (43 vs. 29%), and p < .03 than predominately white populations. Predominately minority populations were also less likely than predominately white populations to receive care at facilities where digital mammography was used (18 vs. 71%, p < .003) and less likely to have all their mammograms read by a trained specialist (23% compared to 87%), p < .003.
Figure 3 presents the geographic distribution of the 25 community areas in Chicago with the highest breast cancer mortality rates and juxtaposes the locations of hospitals with American College of Surgeons Commission on Cancer approved cancer programs [7]. Of the 25 Chicago community areas (out of a total of 77) with the highest breast cancer mortality rates, 24 are predominately black and most are located on the south side of the city. Only one community area with a high breast cancer mortality rate has a hospital with an approved cancer program residing within it, and only there are two hospitals with approved cancer programs on the south side of Chicago.
Results from the Town Hall meetings, focus groups of primary care physicians, mammography technicians, and oncologists and radiologists identified a number of recurring themes. First, there was agreement that there needed to be more breast cancer education and outreach programs for black women and other minorities. Secondly, the mammography process was broken in Chicago, and both patients and providers could identify quality differences in the manner in which the centers provided care and reported back. Finally, there were a number of reported barriers to diagnosis and treatment identified including fear, the lack of primary care, the burden of insurance co-pays and deductibles, providers who refused to treat patients on Medicaid, and noncompletion of treatment for social or economic reasons.
Table 1 presents a series of quality measures for the breast cancer screening, diagnosis, and treatment process proposed by national organizations and the Taskforce [3, 8–10]. The Taskforce has recommended that these quality measures to be systematically measured in institutions across Metropolitan Chicago and used to drive improvement in breast care for all women. In Table 2, the key findings of the Taskforce are summarized [3].
Discussion
The Taskforce concluded that the problem of breast cancer disparity in Chicago had many components but was primarily caused by gaps in education and access to screening and gaps in the quality of breast care across the continuum of care. Recommendations by the Taskforce on remedies to the problem of black–white breast cancer mortality disparity address two overarching principles. The first was that no single entity in Chicago could “fix what was broken” and that this effort would thus require the participation of all institutions. Secondly, simply fixing one part of the breast health “system” would not be enough, all aspects had to be fixed together. What good would it be to expand outreach activities if the facilities do not have capacity? What good would it be to assure access to mammography, if the mammograms and the reading of the mammograms were of poor quality such that small cancers were missed? What good would be served by finding cancers but not having access to quality treatment?
The fact that black breast cancer mortality in Chicago has not decreased among black women since 1980 (it has actually increased by a small amount) suggests that the major advances in breast cancer diagnosis and treatment in the past 25 years have not benefited black women in Chicago, while white women have experienced a large decrease in mortality. That the disparity in Chicago is larger than that seen in New York City and the United States, which suggests something uniquely different and of great concern is occurring in Chicago with regard to breast cancer outcomes for black women. We believe that similar poor breast cancer outcomes may be present in other minority populations in Chicago, but do not have the data to corroborate the veracity of this hypothesis.
The growing black/white breast cancer mortality disparity in Chicago cannot be easily attributed to biological or co-morbid differences between blacks and whites but suggests that differential screening and treatment are contributors [3, 11–14]. The comparisons with the United States and New York City disparity ratios shown in Fig. 2 make this clear, as one would not expect that the biological changes or co-morbidities that are alleged to drive breast cancer mortality could appear since 1980 or affect black women differentially in New York compared to Chicago. Rather, the reasons must involve breakdowns in the access to and the quality of breast care for black women across Chicago.
The communities with the highest mortality for breast cancer in Chicago are also those communities without hospitals with American College of Surgeons approved cancer treatment facilities as shown in Fig. 3. These communities can be viewed as “health care deserts”, as one participant in the Town Hall meetings described them, abandoned over the years by health care providers. Feedback from women in these communities as well as interviews with providers of breast cancer care revealed major problems women face trying to access services often miles from their homes and requiring long bus and train rides. Added to this geographic problem is the likelihood that the quality of breast care for black women in Chicago is different from that received by white women. White women in Chicago are more likely than black women to attend academic and private facilities, and their mammograms more likely to be read by specially trained radiologists [3]. Research has demonstrated that specialists are more likely to detect early breast cancers than general radiologists, and that diagnostic mammograms performed by academic facilities are associated with higher diagnostic accuracy [15, 16]. Finally, white women are more likely than minority women to attend facilities with digital mammography, which research has demonstrated to be more effective in detecting breast cancer in women aged 40–50 [17].
The solutions to this disparity are neither straightforward nor simple. The literature suggests that the racial disparities in breast cancer outcomes can be reduced or eliminated by adequate screening and equivalent treatment [13, 18]. Racial disparity in health outcomes has been described as a significant quality of care problem that can be addressed by tracking race specific outcomes [19]. A number of studies have demonstrated that for diseases other than breast cancer, when the quality of care is measured, made transparent, and improved, the black/white disparity in various health care processes can be reduced or even eliminated [20, 21]. We believe the same is true for the processes of care that contribute to breast cancer mortality disparity in Chicago.
There are obvious challenges ahead. We are not aware of any community that has attempted to use quality improvement methodology to address racial disparity in breast cancer mortality across the continuum of care. While many institutions in Chicago have expressed an interest in joining such an effort, it will require developing new measurement tools and an unprecedented inter-institutional collaboration. Cost has also been shown to be a major barrier to the receipt of mammography services and should be eliminated as a barrier [22]. This will certainly be facilitated by a new state of Illinois rule, stimulated by the work of the Taskforce, which makes Illinois the first state to pay for mammograms and treatment for all uninsured women, under the Illinois Breast and Cervical Cancer Screening Program [23]. However, while the coverage of all uninsured women is significant, there is an absolute annual capacity deficit for screening mammography in Chicago of at least 200,000 screening mammograms [3]. Capacity building is necessary but probably not sufficient as we heard from women, providers, and community organizations that issues of public transportation, childcare, work and insurance co-pays are significant barriers even for insured women [3]. Navigation programs have been shown to provide some reduction in delay time to treatment and reduce anxiety in women and have been recommended by the Taskforce [24, 25]. While improving mortality is a daunting task, if we proceed in Chicago as we have been doing for the past 25 years, the outcomes for black women will likely fail to improve.
This is, of course, not a viable option. The Metropolitan Chicago Breast Cancer Taskforce has documented the problem and proposed solutions. Now the solutions must be pursued with all available energy. Philosophers have noted that it is not enough to identify a problem and then do nothing to fix it. As Martin Luther King, Jr. noted, “All that is necessary for evil to triumph is for good men to do nothing [26]”.
References
Hirschman J, Whitman S, Ansell D, Grabler P, Allgood K (2006) Breast cancer in Chicago: eliminating disparities and improving mammography quality. Sinai Urban Health Institute, Chicago
Hirschman J, Whitman S, Ansell D (2007) The black: white disparity in breast cancer mortality: the example of Chicago. Cancer Causes Control 18:323–333. doi:10.1007/s10552-006-0102-y
Metropolitan Chicago Breast Cancer Taskforce (2007) Improving quality and reducing disparities in metropolitan Chicago. Chicago, IL
http://www.nber.org/data/vital-statistics-mortality-data-multiple-cause-of-death.html
http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMQSA/mqsa.cfm
Government Accounting Office (GAO) (2002) Mammography-capacity generally exists to deliver services. Washington, DC, Apr. report no. GAO-02-532
American College of Radiology (ACR) (2003) Breast imaging reporting and data systems (BI-RADS), 4th edn. American College of Radiology, Reston, VA
Rosenberg RD, Yankaskas BC, Abraham LA, Sickles EA, Lehman CD, Geller BM et al (2006) Performance benchmarks for screening mammography. Radiology 241(1):55–56. doi:10.1148/radiol.2411051504
Li CI, Malone KE, Darling JR (2003) Differences in breast cancer stage, treatment and survival by race and ethnicity. Arch Intern Med 163:49–56. doi:10.1001/archinte.163.1.49
Newman LA (2004) Breast carcinoma in African–American and White women: application of molecular biology to understand outcome disparities. Cancer 101:1261–1263. doi:10.1002/cncr.20501
Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J et al (2006) Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med 144:541–553
Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D (2005) Comorbidity and survival disparities among Black and White Patients with breast cancer. JAMA 294:1765–1772. doi:10.1001/jama.294.14.1765
Sickles EA, Wolverton DE, Dee KE (2002) Performance parameters for screening and diagnostic mammography: specialists and general radiologists. Radiology 224:861–869. doi:10.1148/radiol.2243011482
Miglioretti DL, Smith-Bindman R, Abraham L, Brenner RJ, Carney PA et al (2007) Radiologist characteristics associated with interpretive performance of diagnostic mammography. J Natl Cancer Inst 99:1854–1863. doi:10.1093/jnci/djm238
Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum J, Acharyya S, Conant E, Fajardo L, Bassett D’OrsiC et al (2007) Diagnostic performance of digital versus film mammography for breast-cancer screening. NEJM 353:1773–1783. doi:10.1056/NEJMoa052911
Dignam J (2000) Differences in breast cancer prognosis among African–American and Caucasian women.CA Cancer J Clin 50:50–64. doi:10.3322/canjclin.50.1.50
Fiscella PF, Gold MR, Clancy C (2000) MInequality in quality. JAMA 283:2579–2584. doi:10.1001/jama.283.19.2579
Sehgal AR (2003) Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA 289:996–1000. doi:10.1001/jama.289.8.996
Trivedi AN, Zaslavsky A, Schneider EC, Ayanian JZ (2005) Trends in the quality of care and racial disparities in medicare managed care. NEJM 353:692–700. doi:10.1056/NEJMsa051207
Trivedi AN, Rakowski W, Ayanian JZ (2008) Effect of cost sharing on screening mammography in medicare health plans. NEJM 358:375–383. doi:10.1056/NEJMsa070929
Ferrante JM, Chen PH, The KimS (2008) Effect of patient navigation on time to diagnosis, anxiety, satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health 85(1):114–124
Battaglia TA, Roloff K, Posner MA, Freund KM (2007) Improving follow-up to abnormal breast cancer screening in an urban population: a patient navigation intervention. Cancer 109(2 Suppl):359–367
Acknowledgments
Funding: The Avon Foundation provided funds to support the work of the Metropolitan Chicago Breast Cancer Taskforce.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansell, D., Grabler, P., Whitman, S. et al. A community effort to reduce the black/white breast cancer mortality disparity in Chicago. Cancer Causes Control 20, 1681–1688 (2009). https://doi.org/10.1007/s10552-009-9419-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9419-7