Abstract
This study compares cancer mortality and incidence of ethnic German migrants from the Former Soviet Union (FSU) in Germany. Data were obtained from two migrant cohorts residing in the federal state of North Rhine-Westphalia (NRW) (n = 34,393) and Saarland (n = 18,619). Vital status of the NRW cohort was ascertained through local population registries. Causes of death were obtained from the NRW statistical office or from local health offices. Cancer incidence of the Saarland cohort was derived from the Saarland cancer registry using record linkage. From 1990 to 2005, we observed 708 cancer deaths and 586 incident cancer cases. In males, both cancer incidence and cancer mortality were similar to the German population. Female cancer incidence and mortality were lower, the latter significantly. Site-specific standardized mortality and incidence ratios showed great variation in comparison to Germans and were remarkably similar to each other for most sites. Lung cancer was elevated among males, but lower among females. Stomach cancer was higher contrasting with lower ratios for prostate cancer, male colorectal cancer, and female breast cancer. Results confirm that FSU-migrants suffer from cancers, which may be prevented by prevention programs. Furthermore, we cannot conclude a different health-seeking behavior compared to Germans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several epidemiological studies have demonstrated that cancer incidence and cancer mortality of migrants clearly differ from cancer patterns of the respective national populations [1–5]. Such studies led to new findings on the etiology of diseases [6, 7], but they are also important to develop targeted cancer prevention strategies [8, 9].
Since the beginning of the 1990s more than 2 million ethnic German migrants from the Former Soviet Union (FSU) migrated to Germany. Previous studies revealed unanticipated mortality patterns of these migrants: They had a lower mortality from all causes of death, mainly determined by a low mortality from cardiovascular disease [10, 11]. In contrast, males had a higher risk to die from external causes and deaths associated with these causes such as mental and behavioral disorders due to substance use [12]. In addition, this migrant population had a significantly elevated mortality from viral hepatitis and from some cancers associated with infectious agents such as stomach and liver cancer when compared to their host population [13, 14].
Only few migrant studies assess cancer incidence, and even less research is carried out comparing cancer incidence and mortality. Most investigations using both, cancer incidence and mortality, were occupational cancer studies, which describe health risks associated with workplace exposures [15–17].
Zeeb et al. [5] found evidence for a transition of cancer incidence and mortality patterns toward the host population among Turkish migrants in Germany. Swerdlow observed very low colorectal and breast cancer mortality for Vietnamese refugees in England and Wales, which contrasted with elevated mortality from stomach cancer in both sexes, cancers of the nasopharynx and liver in males [1]. Another study analyzed differences in cancer rates between first and second generation migrants relative to the host country and stratified by country of origin showing cancer site-specific patterns for succeeding generations [18]. Results from a study by Warshauer et al. [19] indicated increasing rates of colorectal and stomach cancer incidence and mortality of Puerto Rican-born residents after migration to New York City.
All previous investigations on FSU-migrants in Germany consider mortality as the endpoint. However, from this perspective the effects of risk factors and of later diagnosis or less optimal treatment cannot be disentangled. It is therefore crucial to investigate the cancer incidence pattern in this population.
This study is among the few migrant studies examining the extent to which cancer mortality is in line with cancer incidence. Two cohorts of FSU-migrants in Germany were compared to assess differences between these indicators and between migrants and the host population.
Materials and methods
This study used data of two migrant cohorts from the FSU that reside in two different federal states of Germany. One cohort has settled in the federal state of North Rhine-Westphalia (NRW) and the other one in the federal state of Saarland.
Mortality of the cohort in NRW from an earlier follow-up period was presented by Becher et al. [10] and Ott et al. [12]. The current study uses data of an extended follow-up period until 2005.
NRW cohort (cancer mortality)
The study population of the NRW cohort comprises FSU-migrants aged 15 years and above, who settled in NRW between 1990 and 2001. Methodological details on selection and follow-up procedures have been described elsewhere [20, 21]). Briefly, a list of all 281,356 FSU-migrants in NRW containing names, sex, dates of birth and arrival in Germany, first city of residence, and country of origin was obtained from the NRW reception center. Out of them, a cohort of 34,393 (16,734 males and 17,659 females) was quasi-randomly selected.
Vital status was ascertained through local population registries. Participants who changed residence were censored at last known date of moving, deceased participants at date of death, and remaining participants at 31 December 2005. For deceased participants, causes of death were obtained either from the NRW statistical office (n = 2,294) through a record linkage system using sex, dates of birth and death, and last residence for identification [22] (ICD-9 codes for deaths before 1998, thereafter ICD-10) or from anonymized death certificates. These death certificates were available from local health offices and were coded according to ICD-10 by the official coding office in the state of Saarland (n = 152). Cause of death was not available for 134 cases (5.2% of all death).
Person-years (PY) were calculated for each sex, 5-year age group, and calendar year. Official WHO cause of death statistics were used to calculate standardized mortality ratios (SMR) [23].
Saarland cohort (cancer incidence)
The second study population of FSU-migrants in the Saarland provided information on cancer incidence. This cohort was not restricted to a particular age and consists of FSU-migrants who arrived in the Saarland between 1990 and 2005. Information on 26,384 FSU-migrants in the Saarland (more than 90% of all FSU-migrants who first settled in the Saarland) was directly obtained from all seven existing local reception centers containing names, sex, date of birth, German passport issue date, first city of residence, and country of birth. A sample of 18,619 (8,975 males and 9,644 females) individuals without missing data was drawn. More details are given by Winkler [24].
Passport issue date minus 6 month was used as an approximation for date of arrival in Germany up to 1993, taking this as mean processing time in local refugee offices into account. After 1993, a new German law shortened the processing period and thus, the arrival date was set 3 months earlier than issue date of the passport.
Record linkage based on the phonetic code of first and last name, sex, and date of birth was applied to assign cancer cases of the Saarland Cancer Registry to the cohort of migrants. For some individuals, city of residence was used as an additional variable to ensure correct identification. Therefore, most recent information on city of residence was collected through local registry offices. Twenty-one cases were not considered in the analysis because they were diagnosed in the country of origin.
As a result of strict data protection regulations, mortality follow-up was only available for 12.4% of the cohort up to now and PY of observation had to be approximated. The method of PY estimation was applied as described in detail by Winkler [24]: sex, age, and calendar year-specific PY were estimated by a two-step procedure. First, it was assumed that each cohort member who has not experienced a cancer diagnosis contributed PY until 31.12.2005. In a second step, PY were adjusted by sex- and age-adjusted German mortality rates and by a factor, which takes possible loss to follow-up into account.
German mortality rates for all causes except cancer were used since participants were censored at the date of cancer diagnosis, and thus all others could not have died from cancer. The factor of loss to follow-up was estimated from those 12.4% that had a complete mortality follow-up. Most loss to follow-up resulted from moves into other regions of Germany not covered by the Saarland cancer registry. Separate analysis of these 12.4% showed an age and calendar year-specific pattern of changing residence, which was taken into account. The yearly migration, however, was rather low with less than 2%. Additionally, a sensitivity analysis was performed (data not shown) to ensure the robustness of the estimated number of PY.
Cancer incidence data was provided by the cancer registry of the Saarland [25] and used to calculate the expected number of cases for standardized incidence ratio (SIR).
SMR and SIR were calculated for all cancers combined except nonmelanoma skin cancer (ICD-10: C44) and for specific cancer sites as shown in Table 1. All 95% confidence intervals (95% CI) were calculated using the exact method [26]. Analysis was performed using SAS version 9.1 [27].
Results
Table 2 presents descriptive results of both cohorts. The size of the Saarland cohort was about half the size of the cohort in NRW. Females were slightly overrepresented in both cohorts. The arrival period for entering the cohort was 4 years longer in the Saarland cohort. The NRW study population was restricted by age at migration of 15 years or older; the Saarland cohort had no age restriction. Thus, the Saarland cohort was on average younger. The NRW cohort accumulated 344,486.1 PY, whereas for the Saarland cohort 176,587.7 PY were estimated.
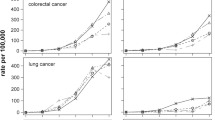
Follow-up of the NRW cohort was completed for 96.7% of the cohort members with a mean follow-up time of 10.1 years. Overall, 2,580 (7.5%) cohort members died. Causes of death were known for 94.8% of deceased persons, and 1,138 (3.3%) persons were lost to follow-up within the observation period, either because they moved abroad or to an unknown destination. During the observation period, 586 cohort members of the Saarland cohort were diagnosed as having cancer. Figure 1 shows the results of SIR and SMR analyses (observed and expected numbers of cases are shown in Table 1).
Cancer mortality in the NRW cohort
Cancer caused 708 (27.4%) of all deaths. Mortality for all cancer sites except nonmelanoma skin cancer in male FSU-migrants was comparable to the German population [SMR: 1.01 (95% CI: 0.92–1.11)]. Female cancer mortality was significantly lower with an SMR of 0.79 (95% CI: 0.71–0.89). The risk of dying from lung cancer was significantly elevated in males yielding an SMR of 1.28 (95% CI: 1.08–1.51) and lower among female migrants [0.52 (95% CI: 0.32–0.80)].
An elevated stomach cancer mortality [males: SMR: 1.44 (95% CI: 1.01–1.98); females: SMR: 1.40 (0.95–1.99)] was found for both, males and females. Liver cancer mortality was also higher among migrants (not significant). However, for colorectal cancer, the risk was lower among migrants compared to Germans [SMR: 0.67 (95% CI: 0.46–0.94)].
Breast cancer is the most common cancer site in females, and female FSU-migrants had a significantly lower mortality than German females yielding an SMR of 0.41 (95% CI: 0.27–0.59). Other cancers of the reproductive system except ovarian cancer showed a similar low risk without being significant. Among males, mortality from prostate cancer was significantly reduced at 0.64 (95% CI: 0.41–0.94). Deaths from leukemia yield an SMR of 0.65 in both sexes, but results are not significant.
Cancer incidence in the Saarland cohort
For male migrants, cancer incidence was similar to Germans [SIR: 0.97 (95% CI: 0.86–1.11)], whereas female migrants had an insignificant lower cancer incidence, [SIR: 0.91 (95% CI: 0.80–1.03)]. The SIR for stomach cancer was significantly elevated at 2.81 (95% CI: 1.85–4.11) for male and at 2.66 (95% CI: 1.65–4.07) for female migrants. Males had a high lung cancer SIR of 1.47 (95% CI: 1.14–1.88), but a reduced incidence of colorectal (cancer [SIR: 0.50 (95% CI: 0.30–0.79)]. Prostate cancer was also reduced, without being significant [SIR: 0.78 (95% CI: 0.55–1.09)]. Female SIR of lung cancer was significantly lower with 0.34 (95% CI: 0.13–0.75) as was breast cancer with 0.72 (0.55–0.93).
Comparison of both cohorts
SIR of the Saarland cohort is remarkably similar to the SMR of the NRW study population. This indicates that later diagnosis with poorer survival or treatment factors are unlikely. Statistically significant differences between SIR and SMR were observed for males for melanoma skin cancer with a higher and for leukemia with a lower SMR. Differences were also found for stomach cancer, female breast cancer, and for all cancer sites in females.
Discussion
Total cancer incidence and total cancer mortality of male FSU-migrants are comparable to the German population, but lower for female migrants. With regard to specific cancer sites, there are substantial differences.
Lung cancer is mainly caused by tobacco smoking and incidence as well as mortality has shown a great difference between the two sexes. Female migrants tend to smoke less than males and also less than German females. The average sex ratio (males to females) for lung cancer in the Russian Federation has consistently been 10:1 over the last 20 years [28]. In contrast, the sex ratio in the German population has fallen to 4:1 in 2003 and continues to decrease [28]. In our cohorts, the ratio found was 10:1 and 7:1 for mortality and incidence and is thus similar to that in the Russian Federation. This indicates a comparable smoking pattern as in the country of origin. The pattern was not repeated for other smoking related cancers such as laryngeal and bladder cancer, which may, however, be related to the small number of observed cases.
Elevated mortality from stomach and liver cancer of FSU-migrants has been shown previously [13], and the current study confirms a higher incidence for stomach cancer in migrants. Stomach cancer is a fatal malignancy with a low survival—the relative 5-year survival rate is 30–35% [29]—and thus the difference cannot be explained by differences in treatment and detection. H. pylori is one of the risk factors for gastric cancer. Additionally, alcohol consumption and nutritional factors, such as low fruit and vegetable consumption and high intake of nitrite containing foods, play a role in the pathogenesis of gastric cancer [30–32]. High alcohol consumption, together with hepatitis virus infection, and aflatoxin produced by certain molds or fungi might also provide an explanation for the elevated SMR of liver cancer.
Colorectal and pancreatic cancer mortality and incidence was lower among FSU-migrants. Yet there is no agreement yet on most important causes for colorectal cancer, but this cancer site as well as pancreatic cancer, is influenced by a diet rich in meat and animal proteins and low intake of fruits and vegetables together with low physical activity [33–36].
Breast cancer was reduced among FSU-migrants. Lower rates may partly be explained by a combined effect of higher birth rates, as seen in rates of Kazakhstan and of the Russian Federation.
For prostate cancer, the picture is very similar. SIR was also reduced, but not significantly and confirms the low SMR observed for prostate cancer mortality. SIR may partly be associated with health-seeking behavior of male FSU-migrants. Since prostate-specific antigen (PSA) testing may not be as common among migrants in Germany.
Cancer incidence and mortality of FSU-migrants in the two different German federal states were very similar. This was expected because both cohorts have equal underlying conditions regarding the health care system and stresses of migration. Additionally, it confirms all striking differences in cancer mortality compared to the German population found in earlier studies [10, 14].
Most differences between SIR and SMR may be explained by chance and the slightly different populations, which were used for the standardization procedure. Statistically significant differences between SIR and SMR for stomach and female breast cancer might indicate that FSU-migrants in Germany do not underutilize preventive services, as previously shown [37, 38]. However, from our data, we cannot conclude what finally causes these differences.
Since the federal refugee office assigns the local office randomly, data can be considered as missing at random and representativeness for both cohorts is ensured. Additionally, it was shown by various descriptive aspects that both cohorts are comparable in terms of country of origin, sex, year of birth, and year of immigration (data not shown, see Winkler [24]). Follow-up procedures of the NRW cohort were successfully performed and reflected in a completeness of 96.7%.
The method of estimating PY of the Saarland cohort on basis of a partial follow-up is sufficient for a detailed analysis. Data were obtained from cities throughout the Saarland. Selection of individuals was not linked to cancer incidence or any other factor. The estimation procedure itself relies on different assumptions, which were mentioned in the methods section.
Incident cancer cases within the Saarland cohort were derived through record linkage, done directly by the Saarland cancer registry. Minor problems arose from the fact that FSU-migrants tend to adjust their Russian names and/or first names to common German spelling. However, the phonetic identification of names using information on sex and date of birth can be considered as a valid method of identification.
Mortality and incidence were compared to different populations by using German and Saarland rates for calculating the expected numbers. To analyze cancer incidence Saarland rates were used for comparison, due to two reasons: first, the Saarland marks the study area and the population-based Saarland Cancer Registry provides high-quality data on cancer incidence and mortality since 1970 and meets international standards in terms of quality and completeness of data [29, 39–41]. Second, incidence data for the whole of Germany do not yet exist and estimations rely on the Saarland data.
This study confirms that migrants from the FSU in Germany suffer from cancers which can, to some extent, be prevented by health promotion programs such as smoking cessation and dietary change. On the other hand, the low risk for cancers of the reproductive system has been verified by incidence analysis. To discover underlying reasons for this phenomenon, further studies are needed with different designs to assess individual risk profiles and genetic backgrounds. From the information available, so far we cannot conclude that FSU-migrants have a different health-seeking behavior than Germans but rather a different risk factor exposure.
References
Swerdlow AJ (1991) Mortality and cancer incidence in Vietnamese refugees in England and Wales: a follow-up study. Int J Epidemiol 20:13–19
Razum O, Zeeb H, Beck K, Becher H, Ziegler H, Stegmaier C (2000) Combining a name algorithm with a capture–recapture method to retrieve cases of Turkish descent from a German population-based cancer registry. Eur J Cancer 36:2380–2384
Stirbu I, Kunst AE, Vlems FA et al (2006) Cancer mortality rates among first and second generation migrants in the Netherlands: convergence toward the rates of the native Dutch population. Int J Cancer 119:2665–2672
Tyczyński J, Tarkowski W, Parkin DM, Zatoński W (1994) Cancer mortality among Polish migrants to Australia. Eur J Cancer 30A:478–484
Zeeb H, Razum O, Blettner M, Stegmaier C (2002) Transition in cancer patterns among Turks residing in Germany. Eur J Cancer 38:705–711
Marmot MG, Adelstein AM, Bulusu L (1984) Lessons from the study of immigrant mortality. Lancet i:1455–1457
McKeigue PM, Miller GJ, Marmot MG (1989) Coronary heart disease in South Asians overseas—a review. J Clin Epidemiol 42:597–609
McKeigue PM, Shah B, Marmot MG (1991) Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 337:382–386
Grulich AE, Swerdlow AJ, Head J, Marmot MG (1992) Cancer mortality in African and Caribbean migrants to England and Wales. Br J Cancer 66:905–911
Becher H, Razum O, Kyobutungi C et al. (2007) Mortalität von Aussiedlern aus der ehemaligen Sovietunion: Ergebnisse einer Kohortenstudie. Deutsches Ärzteblatt 23: A-1655–A-1662. (English version available at http://www.aerzteblatt.de/int/article.asp?id=58120)
Ronellenfitsch U, Kyobutungi C, Becher H, Razum O (2006) All-cause and cardiovascular mortality among ethnic German immigrants from the Former Soviet Union: a cohort study. BMC Public Health 6:16
Ott JJ, Winkler V, Kyobutungi C, Laki J, Becher H (2008) Effects of residential changes and time patterns on external cause mortality in migrants: results of a German cohort study. Scand J Public Health 36:524–531
Ott JJ, Paltiel AM, Winkler V, Becher H (2008) Chronic disease mortality associated with infectious agents: new challenges observed in a cohort study on migrants from the FSU. BMC Public Health 8:110
Kyobutungi C, Ronellenfitsch U, Razum O, Becher H (2006) Mortality from cancer among ethnic German immigrants from the Former Soviet Union, in Germany. Eur J Cancer 42:2577–2584
Fritschi L, Hoving JL, Sim MR et al (2008) All cause mortality and incidence of cancer in workers in bauxite mines and alumina refineries. Int J Cancer 123:882–887
Gun RT, Pratt N, Ryan P, Roder D (2006) Update of mortality and cancer incidence in the Australian petroleum industry cohort. Occup Environ Med 63:476–481
Lundberg I, Milatou-Smith R (1998) Mortality and cancer incidence among Swedish paint industry workers with long-term exposure to organic solvents. Scand J Work Environ Health 24:270–275
Thomas DB, Karagas MR (1987) Cancer in first and second generation Americans. Cancer Res 47:5771–5776
Warshauer ME, Silverman DT, Schottenfeld D, Pollack ES (1986) Stomach and colorectal cancers in Puerto Rican-born residents of New York City. J Natl Cancer Inst 76:591–595
Ronellenfitsch U, Kyobutungi C, Becher H, Razum O (2004) Large-scale population-based epidemiological studies with record linkage can be done in Germany. Eur J Epidemiol 19:1073–1074
Kyobutungi C (2008) Ethnic German immigrants from the former Soviet Union: mortality from external causes and cancers. In: Razum O (ed) Challenges in public health, vol 53. Peter Lang Verlag, Frankfurt
Klug SJ, Zeeb H, Blettner M (2003) Neue Möglichkeit der Recherche von Todesursachen in Deutschland über Statistische Landesämter am Beispiel einer retrospektiven Kohortenstudie. Gesundheitswesen 65:243–249
World Health Organization (2007) Regional office for Europe. Mortality database. [cited 2007 Jul 21] Available from: http://www.who.int/whosis/mort/download/en/index.html
Winkler V (2008) Specific aspects of the health profile in ethnic German migrants from the Former Soviet Union. PhD Thesis submitted to the Medical Faculty of Heidelberg University
Saarland cancer registry (2008) Interactive database [cited 2008 Jan 2] Available from: http://www.krebsregister.saarland.de/datenbank/datenbank.html
Breslow NE, Day NE (1987) Rates and rate standardization. In: Statistical methods in cancer research: volume II-the design and analysis of cohort studies. International Agency for Research on Cancer. IARC Scientific Publications, Lyon, pp 48–79
SAS Institute Inc (2004) SAS/STAT Software Release 9.1. SAS Institute Inc, Cary
World Health Organisation (2007) European health for all database. WHO Regional Office for Europe, Copenhagen. [cited 2007 Jul 21] Available from: http://data.euro.who.int/hfadb/
Robert Koch Institut und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. [Cancer in Germany 2003–2004. Occurence and Trends] [German] Krebs in Deutschland 2003–2004 Häufigkeiten und Trends. 6. überarbeitete Auflage. Berlin, 2008
Gonzalez CA, Pera G, Agudo A et al (2006) Fruit and vegetable intake and the risk of stomach and oesophagus adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Cancer 118:2559–2566
Kono S, Hirohata T (1996) Nutrition and stomach cancer. Cancer Causes Control 7:41–55
Zaridze D, Borisova E, Maximovitch D, Chkhikvadze V (2000) Alcohol consumption, smoking and risk of gastric cancer: case–control study from Moscow, Russia. Cancer Causes Control 11:363–371
Key TJ, Schatzkin A, Willett WC, Allen NE, Spencer EA, Travis RC (2004) Diet, nutrition and the prevention of cancer. Public Health Nutr 7:187–200
MacLennan R (1997) Diet and colorectal cancer. Int J Cancer 10:10–12
Martinez ME (2005) Primary prevention of colorectal cancer: lifestyle, nutrition, exercise. Recent Results Cancer Res 166:177–211
Michaud DS (2004) Epidemiology of pancreatic cancer. Minerva Chir 59:99–111
Aparicio ML, Döring A, Mielck A, Holle R, KORA Studiengruppe (2005) Differences between Eastern European immigrants of German origin and the rest of the German population in health status health care use and health behaviour: a comparative study using data from the KORA-Survey 2000. Soz Praventivmed 50:107–118
Wittig U, Merbach M, Siefen RG, Brähler E (2004) Complaints and health care system utilisation of ethnic German migrants from the Former Soviet Union to Germany and their families. Gesundheitswesen 66:85–92
Brenner H, Stegmaier C, Ziegler H (1994) Estimating completeness of cancer registration in Saarland/Germany with capture-recapture methods. Eur J Cancer 30A:1659–1663
Haberland J, Schön D, Bertz J, Görsch B (2003) Vollzähligkeitsschätzungen von Krebsregisterdaten in Deutschland. Bundesgesundheitsbl-Gesundheitsforsch-Gesundheitsschutz 46:770–774
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB (eds) (2002) Cancer incidence in five continents. IARC Sci Publ VIII: 352–353
Acknowledgments
The study was funded by a grant of the German Research Foundation, Graduate College 793: “Epidemiology of communicable and chronic noncommunicable diseases and their interrelationships.”
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Winkler, V., Ott, J.J., Holleczek, B. et al. Cancer profile of migrants from the Former Soviet Union in Germany: incidence and mortality. Cancer Causes Control 20, 1873–1879 (2009). https://doi.org/10.1007/s10552-009-9381-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9381-4