Abstract
Objective
To examine the association of baseline and lifetime ethanol intake with cancer of the pancreas in the European Prospective Investigation into Cancer and Nutrition (EPIC).
Methods
Included in this analysis were 478,400 subjects, of whom detailed information on the intake of alcoholic beverages at baseline and over lifetime was collected between 1992 and 2000. During a median follow-up time of 8.9 years, 555 non-endocrine pancreatic cancer cases were observed. Multivariate Cox proportional hazard models were used to examine the association of ethanol intake at recruitment and average lifetime ethanol intake and pancreatic cancer adjusting for smoking, height, weight, and history of diabetes.
Results
Overall, neither ethanol intake at recruitment (relative risk (RR) = 0.94, 95% confidence interval (CI) 0.69–1.27 comparing 30+ g/d vs. 0.1–4.9 g/d) nor average lifetime ethanol intake (RR = 0.95, 95% CI 0.65–1.39) was associated with pancreatic cancer risk. High lifetime ethanol intake from spirits/liquor at recruitment tended to be associated with a higher risk (RR = 1.40, 95% CI 0.93–2.10 comparing 10+ g/d vs. 0.1–4.9 g/d), but no associations were observed for wine and beer consumption.
Conclusion
These results suggest no association of alcohol consumption with the risk of pancreatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is one of the most lethal cancers with a one-year survival rate of less than 20% [1]. Its incidence varies worldwide with high rates in the US, Australia, and Europe [1] suggesting that a certain proportion of pancreas cancer occurrence is due to environmental factors. However, only few environmental risk factors have been clearly identified so far. Smoking is the major established risk factor [2, 3]. In addition, excess body weight [4, 5], history of (type-2) diabetes mellitus [6], elevated blood levels of glucose [7, 8], and chronic hyperinsulinemia [7] have been associated with pancreatic cancer risk. Some epidemiological studies have also reported associations of increased pancreatic cancer risk with low intakes of fruit and vegetables [9] or elevated intakes of red and/or processed meat [10].
Alcohol consumption is an important determinant of chronic pancreatitis, a risk factor of pancreatic cancer [11, 12]. Thus, several prospective studies have examined the association between alcohol consumption at the time of enrolment into the study and pancreatic cancer risk [13–26]. No statistically significant associations of alcohol consumption with pancreatic cancer risk were observed in the largest of these cohort studies, each including more than 100 cases [16, 18, 21–25, 27], and numerous case–control studies (summarized in [1]), but three cohort studies, noted a statistically significantly higher risk of pancreatic cancer among consumers of alcoholic beverages compared with non-consumers [15, 17, 20]. In contrast, lifetime alcohol consumption habits have rarely been investigated [25, 28, 29].
Since differences in alcohol consumption habits concerning amount of alcohol consumed and type of alcoholic beverage might contribute to inconsistent findings between studies, it is of interest to examine this question in a large European study with a wide range of daily alcohol consumption. The European Prospective Investigation into Cancer and Nutrition (EPIC) offers the opportunity to examine the association between ethanol intake and pancreatic cancer risk in a more detailed way than it has been done before, especially because of its detailed assessment of lifetime alcohol consumption in most of the participating study centers.
Methods
Population
EPIC was conducted in 23 centers in 10 European countries [30]. About 521,448 participants were recruited for this study, mostly from the general population. Exceptions were the French cohort, which encompasses female members of a health insurance for school and university employees, and the Spanish and Italian centres, which include blood donors. In Utrecht, breast cancer screening participants were recruited for the study, and also the Florence cohort includes participants of a breast cancer screening program. In Oxford, half of the cohort members are ‘health conscious’ subjects from England, Wales, Scotland, and Northern Ireland. The cohorts of France, Norway, Utrecht, and Naples consist of women only [30].
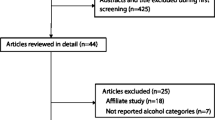
Of 521,448 participants, we excluded 27,094 prevalent cancer cases and subjects with missing follow-up information, 6,220 subjects without dietary or non-dietary information, and 9,674 subjects with an extreme ranking ratio for energy intake versus energy expenditure (top and bottom 1%). Finally, 60 pancreatic cancer cases were excluded from the analysis because of having a malignant tumor at another site prior to their pancreatic tumor or having a (neuro)endocrine tumor. Thus, the current analysis was based on 478,400 EPIC-participants including 555 incident non-endocrine pancreatic cancer cases. Lifetime ethanol intake was assessed only in some EPIC centres (see p. 6) and was, thus, based on 402 pancreatic cancer cases among 363,970 participants.
Exposure assessment
Diet over the previous 12 months was assessed using dietary assessment instruments that were specifically developed for each participating country [30]. Food frequency questionnaires were used in France, Varese, Turin, Florence, Ragusa, Naples, Spain, Germany, Greece, Great Britain, The Netherlands, Umea, Denmark, and Norway. In Malmö, a non-quantitative FFQ was combined with a 14 days dietary record on hot meals. Baseline ethanol and energy intake were calculated on the basis of these dietary assessment instruments [30]. Participants reported on how many standard glasses of beer and/or cider, wine, sweet liquor, distilled spirits, or fortified wines they consumed per day or per week during the 12 months prior to recruitment. Ethanol intake was calculated based on the average glass volume and ethanol content for each type of alcoholic beverage [31].
Information on past alcohol consumption was assessed as glass(es) of beverage consumed per week at different ages (20, 30, 40, and 50 years of age) in the lifestyle questionnaire. This information was assessed in most, but not all, study centers and was available for 364,789 participants (76.1% of the subjects included in the analysis). No information on alcohol consumption in the past was available from Naples (Italy), Bilthoven (The Netherlands), Sweden, and Norway. Consumption of alcoholic beverages at different ages and at recruitment was the basis to calculate average lifetime ethanol intake. Average lifetime ethanol intake was determined as a weighted average of the intake at different ages, with weights equal to the total subject specific time under investigation.
Information on history of prevalent diseases such as diabetes mellitus and on lifetime history of consumption of tobacco products was assessed including questions on smoking status (current, past, or never smoker), type of tobacco (cigarettes, cigars, or pipe), number of cigarettes currently smoked, and age when participants started and, if applicable, quit smoking. Height and weight were measured in all EPIC centres except for France, Norway, and Oxford, for which self-reported height and weight were assessed via questionnaire [30].
Outcome assessment
Cancer diagnoses were based on the population cancer registries in Denmark, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom. An active follow-up through study subjects as well as next-of-kin information, the use of health insurance records, and cancer and pathology registries were used in France, Germany, and Greece. Mortality data were also obtained from either the cancer or mortality registries at the regional or national level. Participants from centers that relied on registry data that have been reported to IARC were censored between December 2002 and December 2005, depending on the study center. For Germany and Greece, the end of the follow-up was considered to be the last known contact, the date of diagnosis, or the date of death, whichever came first.
Pancreatic cancer incidence data were coded according to International Classification of Diseases-Oncology (ICD-O) 2nd edition and included all invasive pancreatic cancers that were coded as C25 (C25.0–C25.3, C25.7–C25.9). All self-reports by the study participants were then confirmed by a review of the appropriate medical records. Of all 555 exocrine pancreatic tumors, 372 (67%) were microscopically confirmed, based on histology of the primary tumor (n = 211), histology of the metastasis (n = 34), cytology (n = 92), or autopsy (n = 35). For 33% of pancreatic tumors, microscopic confirmation was missing and diagnosis was based on the clinical symptoms, physical examination, and imaging results.
Statistical analysis
Participants were categorized according to their total ethanol intake at baseline and the average lifetime ethanol intake. Subjects were categorized into five groups (0, 0.1–4.9, 5.0–14.9, 15.0–29.9, or ≥30 g/day). The low ethanol intake of 0.1–4.9 g/day was chosen as the reference category such as to have a sufficiently high number of cases in the reference category. Subjects were also categorized by their intake of ethanol from beer, wine, and spirits and liquors.
Cox proportional hazard regression was used to examine the association of ethanol intake with pancreatic cancer. Age was used as the primary time variable in the Cox models. Time at entry was age at recruitment, exit time was age when participants were diagnosed with cancer, died, were lost to follow-up, or were censored at the end of the follow-up period. The analyses were stratified by sex, by center to account for center effects such as follow-up procedures and questionnaire design, and by age at recruitment to account for violations of the proportional hazard assumption. To adjust for smoking habits and history, we included current tobacco smoking status (never smoker; current smoker with 1–14, 15–24, or 25+ cigarettes/day; former smoker who stopped less than 10 years ago, former smoker who stopped 10 or more years ago; smoking status unknown). Additionally, weight and height at baseline (continuous) were included in the models. Using body mass index (BMI) instead of height and weight did not alter the results. Since diabetes is strongly associated with pancreatic cancer risk and in a U-shaped manner with ethanol intake [32], we also included history of diabetes into our multivariate models. Energy intake is a suspected risk factor for pancreatic cancer and also related to ethanol intake but the risk estimates were virtually unchanged when we adjusted for energy intake from non-alcohol sources. The same was true when we ran models adjusting for physical activity at work and education. We tested for interaction of sex, smoking status (never, former, current smoker, missing), and BMI (<25 kg/m2, ≥25 kg/m2) with ethanol intake by including a cross-product term along with the main effect terms for each in the Cox regression model. The statistical significance of the cross-product term was evaluated using the likelihood ratio test. Heterogeneity between the categories of ethanol intake and between countries was assessed using likelihood chi-square tests. Since undiagnosed disease at baseline may have led to changes in ethanol intake, models excluding the first two years of follow-up were run for ethanol intake at baseline. All analyses were conducted using SAS version 9.1 (SAS Institute, Cary, North Carolina).
Results
Within a median follow-up time of 8.9 years (interquartile range 7.6–10.5), 239 pancreatic cancer cases were observed among men and 316 among women. Median age at pancreatic cancer diagnosis was 63.3 (interquartile range 57.9–69.0) years. Male non-drinkers at baseline were most common in the Spanish and least common in the Danish centres (Table 1). In women, non-drinking was much more frequent than in men. More than half of the female participants of the Spanish cohorts did not consume alcoholic beverages at baseline. Median ethanol intake among men was highest in the Spanish and Italian centres, whereas median intake among women was highest in the Danish centres. Baseline characteristics by the categories of ethanol intake at baseline are shown in Table 2. Male and female non-consumers of alcoholic beverages were older than consumers, differed by education and smoking habits, and had a higher prevalence of diabetes at baseline. Baseline characteristics were similar when considering only those participants for whom information on lifetime ethanol intake was available (data not shown). In our cohort, 29.4% of cases were current smokers (compared with 22.4% among non-cases), the percentage of subjects with diabetes is 6.9% in cases and 2.7% in non-cases.
We did not observe any statistically significant association between ethanol intake at recruitment and pancreatic cancer risk; these results were similar in the simple and the multivariately adjusted models besides slightly different risk estimates in the highest category of ethanol intake (Table 3). No statistically significant heterogeneity between categories of ethanol intake at baseline was observed (p = 0.60). Per 10 g intake of ethanol at recruitment, we observed an RR = 1.00 (95% CI 0.96–1.05; p-trend = 0.96). The observed associations did not change when we excluded the first two years of follow-up: the RR for individuals with an intake of 30+ g/day was 0.92 (95% CI 0.66–1.30) compared with subjects with an intake of 0.1–4.9 g/day (data not shown). Excluding 183 cases that were not histologically confirmed did not appreciably change our results (data not shown). The same was true for the exclusion of participants with a diagnosis of type-2 diabetes (data not shown). No statistically significant heterogeneity between countries (p = 0.67) or interaction by sex, smoking status, or BMI was observed (all p-interaction > 0.05).
Former drinkers did not have a statistically significantly different risk of pancreatic cancer than never drinkers (RR = 1.21, 95% CI 0.68–2.16). Therefore, we did not differentiate between former and current drinkers in our analysis of lifetime alcohol consumption. We did not observe a statistically significant association between average lifetime ethanol intake and pancreatic cancer risk (Table 3); no statistically significant heterogeneity between categories of ethanol intake was observed (p = 0.66). Neither statistically significant effect modification by sex, smoking status, or BMI (all p-interaction > 0.05) nor any indication of heterogeneity of effects by country (p = 0.63) was found. We observed a correlation of r = 0.66 (p < 0.0001) between alcohol intake at recruitment and average lifetime alcohol consumption.
Results for ethanol intake from different types of alcoholic beverages, which were mutually adjusted for each other, are shown in Table 4. Neither wine nor beer consumption was significantly associated with the risk of pancreatic cancer. For spirits/liquor consumption at baseline, we observed an increased risk of pancreatic cancer in participants with a daily intake of 5.0–9.9 g/day compared with subjects with an intake of 0.1–4.9 g/day (RR = 1.46, 95% CI 1.07–1.99; Table 4). However, the risk was not elevated in subjects with an intake of 10+ g/day. For an average lifetime consumption of spirits and liquor, we also noted an increased risk of pancreatic cancer in subjects with an average lifetime daily intake of 5.0–9.9 and 10+ g ethanol from spirits and liquor that, however, did not reach statistical significance in the multivariate model (RR = 1.30, 95% CI 0.91–1.85 and RR = 1.40, 95% CI 0.93–2.10, respectively). Since subjects who consume high amount of spirits and liquor are also often smokers, we repeated the analysis in subjects who never smoked or quit 10 or more years before baseline (n = 318 cases) to minimize residual confounding by smoking, which did not strongly change the results (10+ g vs. 0.1–4.9 g ethanol at baseline RR = 1.51, 95% CI 0.85–2.70 in the multivariate model). No statistically significantly heterogeneity between countries was observed for any of the alcoholic beverages (all p-heterogeneity > 0.05), nor was effect modification found by sex, smoking status, or BMI (all p-interaction > 0.05).
Discussion
In this large prospective cohort study with 555 incident pancreatic cancer cases, we neither observed a statistically significant association of ethanol intake at baseline nor of average lifetime ethanol intake with pancreatic cancer. This was true, even after excluding the first two years of follow-up.
Alcohol consumption has been suspected as a cause of pancreatic cancer because it is an important determinant of some forms of chronic pancreatitis, which is a risk factor of pancreatic cancer [11, 12]. Also, acetaldehyde, the first metabolite of ethanol, is a well-established carcinogen [33]. Further, fatty acid ethyl esters (non-oxidative ethanol metabolites) accumulate in the pancreas and may induce pancreatic injury [34, 35], and ethanol might affect the metabolism of carcinogens and, e.g., induce human liver cytochrome P450 2E1, which, then, can activate pre-carcinogens [20]. In the largest cohort study with more than one million participants and 3,751 pancreatic cancer deaths in 14 years of follow-up, no statistically significant association between alcohol consumption and pancreatic cancer risk was noted (comparing > 1 drink/day vs. none: men RR = 1.0, 95% CI 0.9–1.1, women RR = 0.9, 95% CI 0.8–1.1) [22], a result confirmed by other large cohort studies [16, 18, 21, 23, 24] including the present study. Two smaller cohort studies reported a statistically significantly increased risk of pancreatic cancer among consumers of alcoholic beverages compared with non-consumers [15, 17], and in the Iowa Women’s Health Study, a statistically significant 65% higher pancreatic cancer risk was observed in women who consumed more than two drinks per week compared with non-consumers [20]. Differences between studies might be due to different alcohol consumption patterns, differential errors in alcohol consumption assessment, differences in confounder patterns, such as smoking habits, and/or sample size and power of the study.
In contrast to current alcohol consumption, the association with alcohol consumption in the past and lifetime alcohol consumption has been investigated less frequently. Only one cohort study [25] examined the association of years of drinking and the cumulative amount of alcoholic beverage drunk over time with pancreatic cancer risk but no association was observed for either variable. Further, in two case–control studies, no statistically significant association between past alcohol consumption was seen when compared with non-drinkers [14, 18]. This is similar to the result in this study within EPIC, where no statistically significant association was observed between average lifetime ethanol intake and pancreatic cancer risk.
We did not observe a statistically significant association of ethanol intake from wine with pancreatic cancer risk; results from previous studies are inconsistent [14, 20, 28], with one study reporting an inverse association with white wine (but not red wine) consumption [28]. For intake of ethanol from spirits/liquor, we observed positive, although not entirely consistent, associations with pancreatic cancer risk. Three [16, 17, 20] out of four [14] previous studies reported an increased risk of pancreatic cancer with increasing intake of spirits and hard liquor. It has been suggested that nitrosamines [36] and cadmium [37] in different types of liquor and spirits may contribute to the increased risk of pancreatic cancer in high consumers of these beverages, but alcoholic beverages are not important dietary sources of these two compounds. Due to the number of tests in our analysis, our findings might as well be due to chance or to residual confounding due to unaccounted for characteristics of subjects who consume high amounts of spirits/liquor. Subjects who consume high amounts of liquor and spirits are also often heavy smokers. Therefore, residual confounding by smoking might be an alternative explanation of our results, but our findings remained virtually unchanged when excluding current smokers and those who quit up to 10 years ago. EPIC includes several European countries with different alcohol consumption patterns, e.g. predominantly wine consuming countries in Southern Europe. However, effects for different types of alcoholic beverages were similar when the analyses were restricted to countries with specific drinking patterns (data not shown). Further studies on the role of alcohol in non-smokers to remove the issue of confounding by smoking and studies on the role of spirits/liquor are warranted.
The strengths of this study include its prospective design, the wide range of ethanol intake, the assessment of past alcohol consumption for the majority of the cohort, and the possibility to account for a large number of potential confounders. However, taking into account smoking, history of diabetes, height, weight, as well as education, physical activity, and energy intake from non-alcohol sources did not appreciably change the results of our study, which was also observed in a previous study [22]. Alcohol consumption was self-reported via questionnaire and might, thus, be affected by measurement error. However, the information of alcohol consumption has been shown to be valid and reliable in country-specific validation studies [38, 39] for most countries, with the exception of Norway, where an underestimation of alcohol consumption by the FFQ was observed [40]. EPIC was planned as a multi-center cohort study with a common core protocol to ensure a standardized collection of study information and a detailed protocol for the collection and standardization of clinical and pathological data of cancer information has been developed [30].
In conclusion, there was no indication of a statistically significant association between ethanol intake and pancreatic cancer risk in the EPIC cohort.
References
American Institute for Cancer Research/World Cancer Research Fund (1997) Food, nutrition and the prevention of cancer: a global perspective. American Institute for Cancer Research, Washington, DC
Larsson SC, Permert J, Hakansson N, Naslund I, Bergkvist L, Wolk A (2005) Overall obesity, abdominal adiposity, diabetes and cigarette smoking in relation to the risk of pancreatic cancer in two Swedish population-based cohorts. Br J Cancer 93:1310–1315. doi:10.1038/sj.bjc.6602868
Fuchs CS, Colditz GA, Stampfer MJ et al (1996) A prospective study of cigarette smoking and the risk of pancreatic cancer. Arch Intern Med 156:2255–2260. doi:10.1001/archinte.156.19.2255
Larsson SC, Orsini N, Wolk A (2007) Body mass index and pancreatic cancer risk: a meta-analysis of prospective studies. Int J Cancer 120:1993–1998. doi:10.1002/ijc.22535
Berrington de Gonzalez A, Spencer EA, Bueno-de-Mesquita HB et al (2006) Anthropometry, physical activity, and the risk of pancreatic cancer in the European prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 15:879–885. doi:10.1158/1055-9965.EPI-05-0800
Huxley R, Ansary-Moghaddam A, Berrington de Gonzalez A, Barzi F, Woodward M (2005) Type-II diabetes and pancreatic cancer: a meta-analysis of 36 studies. Br J Cancer 92:2076–2083. doi:10.1038/sj.bjc.6602619
Stolzenberg-Solomon RZ, Graubard BI, Chari S et al (2005) Insulin, glucose, insulin resistance, and pancreatic cancer in male smokers. JAMA 294:2872–2878. doi:10.1001/jama.294.22.2872
Stattin P, Björ O, Ferrari P et al. (2007) Prospective study on hyperglycemia and cancer risk. Diabetes Care 30:561–567
Vainio H, Bianchini F (eds) (2003) Fruit and vegetables. IARC Press, Lyon
Larsson SC, Hakanson N, Permert J, Wolk A (2006) Meat, fish, poultry and egg consumption in relation to risk of pancreatic cancer: a prospective study. Int J Cancer 118:2866–2870. doi:10.1002/ijc.21732
Lowenfels AB, Maisonneuve P (2004) Epidemiology and prevention of pancreatic cancer. Jpn J Clin Oncol 34:238–244. doi:10.1093/jjco/hyh045
Michaud DS (2004) Epidemiology of pancreatic cancer. Minerva Chir 59:99–111
Klatsky AL, Friedman GD, Siegelaub AB (1981) Alcohol and mortality. A ten-year Kaiser–Permanente experience. Ann Intern Med 95:139–145
Hiatt RA, Klatsky AL, Armstrong MA (1988) Pancreatic cancer, blood glucose and beverage consumption. Int J Cancer 41:794–797. doi:10.1002/ijc.2910410603
Heuch I, Kvale G, Jacobsen BK, Bjelke E (1983) Use of alcohol, tobacco and coffee, and risk of pancreatic cancer. Br J Cancer 48:637–643
Hirayama T (1989) Epidemiology of pancreatic cancer in Japan. Jpn J Clin Oncol 19:208–215
Zheng W, McLaughlin JK, Gridley G et al (1993) A cohort study of smoking, alcohol consumption, and dietary factors for pancreatic cancer (United States). Cancer Causes Control 4:477–482. doi:10.1007/BF00050867
Friedman GD, van den Eeden SK (1993) Risk factors for pancreatic cancer: an exploratory study. Int J Epidemiol 22:30–37. doi:10.1093/ije/22.1.30
Shibata A, Mack TM, Paganini-Hill A, Ross RK, Henderson BE (1994) A prospective study of pancreatic cancer in the elderly. Int J Cancer 58:46–49. doi:10.1002/ijc.2910580109
Harnack LJ, Anderson KE, Zheng W, Folsom AR, Sellers TA, Kushi LH (1997) Smoking, alcohol, coffee, and tea intake and incidence of cancer of the exocrine pancreas: the Iowa Women’s Health Study. Cancer Epidemiol Biomarkers Prev 6:1081–1086
Nilsen TIL, Vatten LJ (2000) A prospective study of lifestyle factors and the risk of pancreatic cancer in Nord-Tröndelag, Norway. Cancer Causes Control 11:645–652. doi:10.1023/A:1008916123357
Coughlin SS, Calle EE, Patel AV, Thun MJ (2000) Predictors of pancreatic cancer mortality among a large cohort of United States adults. Cancer Causes Control 11:915–923. doi:10.1023/A:1026580131793
Stolzenberg-Solomon RZ, Pietinen P, Barrett MJ, Taylor PR, Virtamo J, Albanes D (2001) Dietary and other methyl-group availability factors and pancreatic cancer risk in a cohort of male smokers. Am J Epidemiol 153:680–687. doi:10.1093/aje/153.7.680
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2001) Coffee and alcohol consumption and the risk of pancreatic cancer in two prospective United States cohorts. Cancer Epidemiol Biomarkers Prev 10:429–437
Lin Y, Tamakoshi A, Kawamura T et al (2002) Risk of pancreatic cancer in relation to alcohol drinking, coffee consumption and medical history: findings from the Japan collaborative cohort study for evaluation of cancer risk. Int J Cancer 99:742–746. doi:10.1002/ijc.10402
Isaksson B, Jonsson F, Pedersen NL, Larsson J, Feychting M, Permert J (2002) Lifestyle factors and pancreatic cancer risk: a cohort study from the Swedish Twin Registry. Int J Cancer 98:480–482. doi:10.1002/ijc.10256
de Martel C, Llosa AE, Friedmana GD et al (2008) Helicobacter pylori infection and development of pancreatic cancer. Cancer Epidemiol Biomarkers Prev 17:1188–1194. doi:10.1158/1055-9965.EPI-08-0185
Bueno de Mesquita HB, Maisonneuve P, Moerman CJ, Runia S, Boyle P (1992) Lifetime consumption of alcoholic beverages, tea and coffee and exocrine carcinoma of the pancreas: a population-based case–control study in The Netherlands. Int J Cancer 50:514–522. doi:10.1002/ijc.2910500403
Jain M, Howe GR, St Louis P, Miller AB (1991) Coffee and alcohol as determinants of risk of pancreas cancer: a case–control study from Toronto. Int J Cancer 47:384–389. doi:10.1002/ijc.2910470313
Riboli E, Hunt KJ, Slimani N et al (2002) European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 5:1113–1124. doi:10.1079/PHN2002394
Klipstein-Grobusch K, Slimani N, Krogh V et al (2002) Trends in self-reported past alcoholic beverage consumption and ethanol intake from 1950 to 1995 observed in eight European countries participating in the European Investigation into Cancer and Nutrition (EPIC). Public Health Nutr 5:1297–1310. doi:10.1079/PHN2002406
Carlsson S, Hammar N, Grill V (2005) Alcohol consumption and type 2 diabetes. Diabetologia 48:1051–1054. doi:10.1007/s00125-005-1768-5
International Agency for Research on Cancer (1999) IARC monographs on the evaluation of the carcinogenic risk of chemicals to humans: re-evaluation of some organic chemicals, hydrazine and hydrogen peroxide (part two). World Health Organization, Lyon
Criddle DN, Raraty MGT, Neoptolemos JP, Tepikin AV, Petersen OH, Sutton R (2004) Ethanol toxicity in pancreatic acinar cells: mediation by nonoxidative fatty acid metabolites. PNAS 101:10738–10743. doi:10.1073/pnas.0403431101
Go VLW, Gukovskaya A, Pandol SJ (2005) Alcohol and pancreatic cancer. Alcohol 35:205–211. doi:10.1016/j.alcohol.2005.03.010
Villeneuve PJ, Johnson KC, Hanley AJ, Mao Y (2000) Alcohol, tobacco and coffee consumption and the risk of pancreatic cancer: results from the Canadian enhanced surveillance system case–control project. Canadian Cancer Registries Epidemiology Research Group. Eur J Cancer Prev 9:49–58. doi:10.1097/00008469-200002000-00007
Schwartz GG, Reis IM (2000) Is cadmium a cause of human pancreatic cancer? Cancer Epidemiol Biomarkers Prev 9:139–145
Kaaks R, Riboli E (1997) Validation and calibration of dietary intake measurements in the EPIC project: methodological considerations. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol 26(Suppl 1):S15–S25. doi:10.1093/ije/26.suppl_1.S15
Kaaks R, Slimani N, Riboli E (1997) Pilot phase studies on the accuracy of dietary intake measurements in the EPIC project: overall evaluation of results. European prospective investigation into cancer and nutrition. Int J Epidemiol 26(Suppl 1):S26–S36. doi:10.1093/ije/26.suppl_1.S26
Hjartaker A, Andersen LF, Lund E (2007) Comparison of diet measures from a food-frequency questionnaire with measures from repeated 24-hour dietary recalls. The Norwegian Women and Cancer Study. Public Health Nutr 10:1094–1103. doi:10.1017/S1368980007702872
Acknowledgments
European Commission: Public Health and Consumer Protection Directorate 1993–2004; Research Directorate-General 2005-; Deutsche Krebshilfe, Deutsches Krebsforschungszentrum, German Federal Ministry of Education and Research; Danish Cancer Society; Health Research Fund (FIS) of the Spanish Ministry of Health, Spanish Regional Governments of Andalucia, Asturias, Basque Country, Murcia and Navarra; the ISCIII Network RCESP (C03/09), Spain; Cancer Research UK; Medical Research Council, United Kingdom; Stroke Association, United Kingdom; British Heart Foundation; Department of Health, United Kingdom; Food Standards Agency, United Kingdom; Wellcome Trust, United Kingdom; Greek Ministry of Health; Greek Ministry of Education; Italian Association for Research on Cancer (AIRC); Italian National Research Council, Fondazione-Istituto Banco Napoli, Italy; Compagnia di San Paolo; Dutch Ministry of Public Health, Welfare and Sports; World Cancer Research Fund; Swedish Cancer Society; Swedish Scientific Council; Regional Government of Skåne, Sweden; Norwegian Cancer Society; Research Council of Norway; French League against Cancer (LNCC); National Institute for Health and Medical Research (INSERM), France; Mutuelle Générale de l’Education Nationale (MGEN), France; 3 M Co, France; Gustave Roussy Institute (IGR), France; and General Councils of France
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rohrmann, S., Linseisen, J., Vrieling, A. et al. Ethanol intake and the risk of pancreatic cancer in the European prospective investigation into cancer and nutrition (EPIC). Cancer Causes Control 20, 785–794 (2009). https://doi.org/10.1007/s10552-008-9293-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9293-8