Abstract
Cancer risk in adulthood may be influenced by aspects of childhood diet. In the absence of direct dietary data, indirect measures of childhood diet and nutritional status, such as anthropometric measurements, may be useful in investigating diet–cancer associations. Previous studies suggest that taller adults may have increased cancer risk. Peak growth for different anthropometric measures occurs at different times and so differential associations with cancer risk may indicate periods of development that are particularly important in determining future risk. 2,642 traced members of the Boyd Orr cohort had measures of foot length, shoulder breadth, height, and leg length made when they were aged 2–14 years; trunk length was derived from the difference between overall height and leg length. Subjects were followed-up over 59 years to determine all-cause (n = 547) and site-specific (n = 97 for lung, 69 breast, 59 colorectal, 33 prostate, 320 not related to smoking) cancer deaths and registrations. There were no strong associations between childhood anthropometric measurements and adult cancer risk. Odds ratios (ORs) were broadly consistent with a slight increase in risk with increasing childhood stature but no single measure was of particular importance. The strongest associations were seen for breast cancer (OR per standard deviation increase in foot length: 1.16 (95% CI: 0.90, 1.51), shoulder breadth: 1.16 (0.91, 1.49) and trunk: 1.26 (1.00, 1.60), and prostate cancer (OR for foot length: 1.22 (0.86, 1.75)). There was little effect of adjustment for confounding factors and very limited evidence that associations differed with measures made prior to the onset of puberty (comparing the associations in children aged <8 vs. 8+ years). There was no evidence that any of the five indicators of childhood growth was more strongly related to cancer risk than the other measures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An individual’s risk of cancer is influenced by their genetic predisposition together with their accumulation of protective and adverse exposures occurring before birth, throughout childhood and during adulthood [1]. There is growing evidence that cancer risk in adulthood may be influenced by aspects of childhood diet [2–5]. However, few studies with good quality records of diet measured in childhood have been followed up for sufficiently long periods of time to investigate diet–cancer associations. In the absence of such data, investigators have examined associations of cancer risk with indirect measures of childhood diet and nutritional status, such as height. These studies suggest that taller individuals are at increased risk of breast, colorectal, prostate and haematopoietic cancer [6]. As height is influenced not only by genes but also by growth influencing exposures such as diet, these studies provide indirect evidence of the importance of childhood diet in the aetiology of cancer.
The Boyd Orr cohort was one of the first studies to demonstrate an association between greater childhood stature and increased cancer risk. The association was specific to the leg length component of height [7]. This is in keeping with an analysis of the National Health and Nutrition Examination Survey (NHANES) in the USA showing adult leg length was the component of stature most strongly associated with risk of lung cancer (males), breast and cervical cancer (females) [8]. There is also a suggestion from a large case–control study that the leg component of height may be more strongly associated with advanced prostate cancer than the trunk component [9]. Such associations with different measures of childhood growth may provide insights concerning critical periods of development when nutrition may have its greatest impact upon cancer risk. For example, spurts in foot size and leg length occur before peak height velocity (PHV) whereas peak shoulder breadth growth occurs after PHV [10]. Leg length and foot length may therefore be markers of pre-pubertal growth-influencing exposures, and variations in trunk length and shoulder breadth indicate the impact on growth (and cancer risk) of post-pubertal exposures.
There is also evidence to suggest that the timing of PHV is important in determining future cancer risk. A recent study [11] reported a pattern of increasing risk of breast cancer with decreasing age at PHV. This relationship was unaffected by adjustment for age at menarche. Conversely, there was no independent effect of age at menarche on breast cancer risk after adjustment for age at PHV. In addition, growth at age 8+ years had a greater effect on breast cancer risk than growth at <8 years.
Few studies have examined associations of anthropometric measures other than body mass index, height and leg length with later cancer risk. To the best of our knowledge only two studies have investigated associations with foot length. Foot size was somewhat more strongly positively associated with breast cancer than adult height in a Hawaiian case–control study [12]. However, a similar study in Japan reported no evidence of an association of foot length or height with breast cancer risk [13]. Associations of shoulder breadth with cancer are inconsistent. Two studies have investigated the association of shoulder breadth with prostate cancer. One (n = 156 cases) found that men with broad shoulders had a reduced risk of prostate cancer [14]. However in a larger study (n = 174 cases) no association was found [15]. There is some ecological and case–control evidence that increased shoulder breadth may be associated with greater cancer risk [16, 17].
Earlier analyses of the associations of measures of linear growth with cancer in the Boyd Orr cohort [7, 18] were based on too few cancers (total n = 110) to study site-specific associations. Furthermore, these analyses did not make use of the other anthropometric measures (foot size and shoulder breadth) available on study members. Here we report an analysis of the association of overall and site-specific cancer risk with height, leg length, trunk, foot size and shoulder breadth over a 59 year follow-up of the cohort (1948–2007).
Methods
The Boyd Orr cohort
The Boyd Orr cohort is an historical cohort based on the records of 4,999 children from 1,343 mainly working class families living in 16 centres in England and Scotland who took part in a detailed survey of family diet and childhood health during 1937–1939 (see: http://www.epi.bris.ac.uk/boydorr) [19, 20]. As the purpose of the original survey was to examine growth and diet in relation to income, there are detailed socioeconomic data available on all study members (family income, social class, food expenditure and housing conditions).
Cohort members have data on infant feeding, childhood family diet and nutritional status recorded and, at the most recent update, 92% have been traced on the National Health Service Central Register (NHSCR). Surviving study members are now aged over 70 years and the research team is notified of all deaths and cancer registrations.
Childhood anthropometric measurements
Measures of height, leg length, foot length and shoulder breadth were made on cohort members in 1937–1939. Height, leg length and shoulder breadth were measured to the nearest millimetre using a stadiometer (height) and steel measuring tape (leg length and shoulder breadth). Leg length was measured as the distance from the summit of the iliac crest to the floor. Biacromial breadth was measured as the distance between the external margins of the acromion processes with the subject seated on a chair, with hands on knees and muscles relaxed [21]. Foot size has since been derived by measuring (to the nearest millimetre) the chalk imprints of each of the children’s feet made at the survey clinics. A research assistant visited the Rowett Research Institute Archive (where the original survey records are held) and measured foot length from these records as the maximum length from the subject’s heel to the tip of their toes for each foot. The research worker was blind to the subject’s vital status. For the analysis we used the mean of the left and right foot measures.
Outcome measures
Cancer events are based on NHSCR cancer registration and death certificate data. Registrations were examined in chronological order to identify the first cancer not coded as secondary, carcinomatosis, benign, in situ or uncertain. Death certificate data was used for subjects with no cancers identified from registrations, first considering the underlying cause of death and then looking at other causes of death in order. Again, if the first cause of death was coded as secondary, carcinomatosis, benign, in situ or uncertain, subsequent causes of death were examined in order to identify the first mention of a cancer not falling into these categories. If all cancers listed on registrations and death certificate were coded as secondary or carcinomatosis then the subject was included in the “all cancers” group; if all mentions of cancer were benign, in situ or uncertain then the subject was not included as a cancer case. Cancers considered to be related to smoking were: lung, oral cavity, nasopharynx, oropharynx, hypopharynx, nasal cavity and paranasal sinuses, larynx, oesophagus, stomach, pancreas, liver, kidney (body and pelvis), ureter, urinary bladder, uterine cervix and myeloid leukaemia [22]. Breast cancer cases were subdivided by age at death or registration (<50 vs. 50+ years) to look separately at associations with childhood anthropometric measurements in pre- and post-menopausal cancers as aetiology is known to differ [1]. Sensitivity analyses based on all cancers excluding “other skin” were very similar to those based on all cancers combined.
Statistical analysis
We restricted the analyses to study members who were aged 2–14 years at the time of their measurements. Measurements on younger children are more prone to inaccuracy and the number of older subjects was sparse. All anthropometric measures were transformed into sex-specific age standardized z-scores. For some measures, a cubic term for age was required to obtain a good fit and, although this term did not improve the fit for all measures, it was used throughout for consistency. The resultant z-scores measure the number of standard deviations a child’s measurement lies above or below the predicted value for his/her age (in months) and sex. Specific outcomes of interest were (a) all cancers combined, (b) lung cancer, (c) breast cancer, (d) colorectal cancer, (e) prostate cancer, (f) cancers not related to smoking, and (g) all-cause mortality.
We used logistic regression models to examine associations of childhood anthropometric measures with cancer incidence using the combined endpoint of death/registration as described above. Whilst Cox proportional hazards models/Poisson regression are the preferred methods for survival (cohort) data, the timings of our composite outcome (death/registration date) are not comparable. Nevertheless, sensitivity analyses confirmed that results using Cox or Poisson regression were very similar to those using logistic regression. Robust standard errors were calculated to take account of any clustering effects in children from the same household. Models in each table are based on subjects with complete data.
Confounders
Previously identified confounders include childhood and adult socioeconomic position. Childhood socioeconomic position was available from baseline household measures: social class of the head of household, per capita household income, and household food expenditure. Adult socioeconomic position was available for individuals and was indexed using Townsend score for area of residence. The Townsend score is an ecological measure of socioeconomic deprivation comprising census data on area levels of household overcrowding, unemployment, housing tenure and car ownership. It is possible that patterns of infant feeding may have a long-term impact on growth and cancer risk [23, 24] and so breast-feeding was also included as a possible confounding/mediating variable.
Data on birth weight, adult stature (height and inside leg length) and parental stature were collected by questionnaire from surviving survey members in 1997–1998 and were only available for a reduced subgroup of study members. The effects of controlling for these factors were investigated in separate models.
We also investigated whether associations differed (a) in males vs. females; (b) in subjects who were <8 vs. 8+ years when they were measured in childhood and (c) in subjects whose adult height was above vs. below average for sex. We used formal tests of statistical interaction (effect modification) to investigate differences in associations across these subgroups. The cut-off point of <8 or 8+ years is consistent with our previous analyses and ensures that all the subjects who were measured aged <8 were pre-pubertal [7].
Finally, the main analyses were repeated restricted to (a) cancer cases aged ≤60 at death or registration, i.e. early onset/premature cancers, and (b) cancer mortality only.
Results
Of the 4,999 original cohort members, 4,437 (88.8%) were aged 2–14 at the time of measurement. Measures of foot length, shoulder breadth, height, trunk and leg length were available for 2,648 (59.7%), 2,878 (64.9%), 2,960 (66.7%), 2,860 (64.5%) and 2,860 (64.5%) of these children respectively. A total of 2,969 (66.9%) of those aged 2–14 at measurement had at least one measure, and their baseline characteristics are given in Table 1. Childhood anthropometric measurements are summarized using the mean (standard deviation (SD)) in children aged 2, 5, 10 and 14 ± 3 months at the time of measurement. In these cross-sectional data, mean measures increased with age as would be expected. The SDs also increased, particularly at age 14, which is likely to reflect increasing variation as children reach their adolescent growth spurt. Differences between boys and girls were very small. Boys tended to have slightly larger dimensions at younger ages while girls, who reach their adolescent growth spurt earlier, were marginally larger at age 14. Adult height and inside leg length were available only for a subset of those with at least one childhood measure and show clear and expected differences between the sexes.
There were wide variations in the proportion of children measured in the different study centres. Children living in two districts (Edinburgh and Kintore) did not participate in the clinical survey and so had no anthropometric measures at all; in the remaining 14 survey districts the proportion of children aged 2–14 at the time of survey, who were measured varied from 33.8 to 89.2%. Girls and boys were equally likely to have been measured. However, those aged 2–14 at the time of the survey who had measurements tended to be younger and to come from a higher social class than those without.
A total of 2,642 (89.0%) subjects with at least one childhood anthropometric measure were successfully traced and are included in the analyses presented here. Those who were untraced were older at the time of the dietary survey (8.8 vs. 7.8 years); more likely to be female (12.7 vs. 9.1%); and were marginally more likely to be from households who had higher incomes, spent more on food and whose head was from a higher social class. There were no differences in childhood anthropometric measures between subjects who were traced and untraced.
Pairwise correlations between the five anthropometric measures (standardized for age and sex) were all highly statistically significant (p < 0.001) with correlation coefficients ranging from 0.28 (trunk/leg length) up to 0.89 (height/leg length). The largest coefficients were consistently observed in correlations with height and the smallest were generally in correlations with trunk. The correlation coefficient for foot and leg length (the two measures where peak growth occurs before PHV) was 0.70; the coefficient for shoulder breadth and trunk (with peak growth occurring after PHV) was 0.43.
Anthropometric measurements and cancer
The distribution of principal site-specific and overall cancers, and the ICD-9 and ICD-10 codes used for each are given in Table 2. Altogether 547 study members with anthropometric measurements developed cancer over the 59-year follow-up period. These included 97 cases of lung cancer, 69 cases of breast cancer, 59 colorectal cancer, 33 prostate cancer, and 320 cancers not related to smoking. Of the 69 breast cancer cases, 52 (75.4%) were aged 50+ at the time of death/registration, 7 (10.1%) were aged <50, and 10 (14.5%) had no date of death/registration and so we were unable to calculate their age. There were 983 deaths from all causes combined.
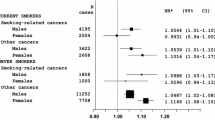
Odds ratios (OR) for cancer and all-cause mortality associated with a standard deviation (SD) increase in foot length, shoulder breadth, height, trunk, and leg length are presented in Table 3. All analyses are adjusted for sex and age at survey. What is most striking is the lack of any consistent association of childhood stature with cancer or all-cause mortality risk. ORs for all-cause mortality were close to or just below 1. Conversely, ORs for cancer tended to be more consistent with a slight increase in risk with increasing stature although the magnitude of these associations was very small. The strongest associations were seen for breast cancer (OR (95% CI) per SD increase in foot length: 1.16 (0.90, 1.51), shoulder breadth: 1.16 (0.91, 1.49) and trunk: 1.26 (1.00, 1.60)), and prostate cancer (OR (95% CI) for foot length: 1.22 (0.86, 1.75)). ORs for breast cancer were generally slightly attenuated when analyses were restricted to events in women aged 50+ at registration/death (OR (95% CI) per SD increase in foot length, shoulder breadth, height, trunk, and leg length: 1.09 (0.80, 1.47), 1.06 (0.80, 1.40), 1.02 (0.75, 1.40), 1.17 (0.91, 1.52), and 0.92 (0.66, 1.29) respectively).
Childhood socioeconomic position, breastfeeding and adult Townsend score were available for around 85% of subjects with anthropometric measures and follow-up data. Additional adjustments for these factors on this subgroup had no substantive effect. Birth weight, adult stature, and parental height were available for a reduced subgroup of study members who were still alive in 1997–1998 (25–30% of those with childhood anthropometric measurements and follow-up). Again, associations of childhood stature with cancers were broadly unchanged after adjustments for these factors.
Around half of children were aged <8 years at the time of the anthropometric measurements. The separate associations of stature with cancer risk for children aged <8 (who were pre-pubertal at the time) and those aged 8+ are shown in Table 4 along with formal tests of statistical interaction. Overall, there was little consistent evidence to suggest that stature at either age was more strongly associated with all-cause mortality or cancer risk. However, there was a suggestion that colorectal cancer might be positively associated with stature at age <8 and inversely associated with stature at age 8+.
Similar analyses were carried out comparing associations in males and females and in those whose adult height was above or below average for sex. There was no evidence of a difference in effect between the sexes. The analysis by adult height was again restricted to 25–30% of the study population but there was some evidence in this restricted group that increasing childhood stature (excluding trunk) may be associated with reduced lung cancer risk in shorter adults and increased risk in taller adults (e.g. OR (95% CI) for leg length: 0.35 (0.21, 0.59) vs. 1.13 (0.64, 2.01) (p for interaction = 0.002)).
There were no striking differences in analyses restricted to cancer cases aged ≤60 at death or registration. Analyses based on cancer mortality were also largely similar to those presented in Table 3 with the possible exception of breast cancer risk. In contrast to results based on all breast cancers, increases in all five anthropometric measures were associated with a 20–35% reduction in breast cancer mortality although these analyses were based on only 11 cases and the confidence intervals (CIs) include 1 (e.g. OR (95% CI) for foot length: 0.65 (0.40, 1.05)).
Discussion
There is a large body of evidence to support a weak but consistent association between adult height and cancer risk, with taller individuals experiencing a 20–60% increase in risk [6]. Associations with specific components of stature are rather less consistent, although most studies report stronger associations of cancer risk with the leg component [6]. We explored associations between cancer risk and five components of stature in childhood (foot length, shoulder breadth, height, trunk and leg length) and found no coherent evidence of any substantial stature–cancer associations. However, the limited associations that were observed were not inconsistent with existing evidence; specifically, cancer risk tended to increase slightly with increasing stature while the opposite direction of association was seen in relation to all-cause mortality.
The current analyses were based on a large cohort of children followed from a young age for 59 years. Detailed childhood anthropometric and socioeconomic data were available for over 2,600 participants and 92% of these subjects have been traced and followed-up. Over 500 cancers and 900 deaths have been identified in those cohort members with childhood anthropometric measurements, and this has led to a more detailed exploration of specific sites than was previously possible. Based on these numbers, we had over 80% power to detect ORs for all cancers combined consistent with those reported in the literature [6] although power was lower for site-specific cancers, analyses with additional adjustments, and analyses based on deaths or early cancers. The tables summarize the results from a large number of comparisons, and we have therefore focussed on the magnitude and consistency of ORs rather than on the results of individual significance tests.
With the exception of foot length, anthropometric measurements were made using standard methods. Implausible measurements or (in the case of foot length) pairs of measurements were excluded along with measurements in very young children (under 2 years). However, the possibility of measurement error cannot be ignored and, assuming the errors to be random, this is likely to have led to an underestimation of any stature–cancer associations. Such effects are likely to be minimal for associations with height and greatest for those with foot length.
Children with anthropometric measurements were younger and from a higher social class than those without. Untraced subjects were older, more likely to be female and, again, from higher social classes. In addition, there were specific restrictions in some of the adjusted analyses and, in particular, subjects included in analyses adjusted for birth weight, adult and parental stature had to be alive in 1997–1998 when the data were collected. Although these restrictions may limit the generalisability of our findings, there is no reason to suppose that they will have led to any differential bias, and it is reassuring that there were no differences in anthropometric measurements between cohort members who were and were not traced.
A previous analysis of these data [7] reported a positive association between cancer mortality (all sites combined) and increasing height and leg length which was most marked in children measured at age <8. We have failed to consistently replicate this finding with an updated dataset containing five times more cancers including registrations as well as deaths. The previous analysis (based on follow-up to 1995) was based on cancer deaths occurring early in follow-up, which might suggest that any effect is limited to premature deaths. The analyses presented here used a combined endpoint based on death and registration data and so we were unable to explore the timing of events directly, e.g. using Cox regression. However, results from analyses restricted to early cancers or to cancer mortality did not differ substantially from the main results in Table 3 and it seems likely that our previous positive association was a chance finding.
Other studies have shown that breast cancer risk increases with greater childhood height, greater height velocity, and early PHV [11, 25]. The magnitude of our overall breast cancer association (OR (95% CI) per SD increase in height 1.07 (0.81, 1.42)) is consistent with those reported in the literature (e.g. results from a pooled analysis of data from seven prospective studies reported relative risks (95% CI) per 5 cm increase in height of 1.02 (0.96, 1.10) and 1.07 (1.03, 1.12) for pre- and post-menopausal breast cancer respectively) [26]. Ahlgren et al. [11] report a stronger association with height at age 8+. In contrast, our results by age at measurement show little difference with, if anything, a slightly stronger association with height at age <8, although the number of breast cancer cases in each group is small and the confidence intervals are broadly consistent with theirs. Contrary to our original hypotheses, we found that greater trunk length rather than leg length was the component of stature most strongly associated with breast cancer risk. Few studies have looked at the components of stature in relation to breast cancer risk. A recent analysis of the British Women’s Heart and Health Study [27] reported that associations with trunk length were similar to those with leg length although, as these women were post-menopausal, greater trunk length could be due to lower levels of osteoporotic vertebral collapse, possibly reflecting circulating oestrogen levels, in turn being related to cancer risk.
Adult stature has previously been shown to be associated with cancer risk, and it has been hypothesized that differential associations with different components of stature may reflect the effect on cancer risk of exposures acting at critical periods of growth, particularly in adolescence. This analysis provides no consistent evidence to support such differential effects, but this finding must be viewed in the context of relatively weak overall height–cancer associations, limiting our capacity to tease out any subtle effects related to particular measures of body size. In a separate analysis of the Boyd Orr cohort [28] we have explored the extent to which childhood anthropometric measurements can be explained by diet, housing conditions and socioeconomic position. The results from these analyses indicate that there is no single factor or subgroup of factors that are of particular importance. Rather, all factors are associated to some degree with childhood anthropometric measurements even at this young age. There are many influences, genetic and environmental, governing final adult stature and future disease, and it is likely that a single measurement in childhood is not sufficient to represent all the complexities and inter-relationships involved.
References
Potischman N, Troisi R, Vatten L (2004) A life course approach to cancer epidemiology. In: Kuh D, Ben-Shlomo Y (eds) A life course approach to epidemiology. Oxford University Press, Oxford, pp 260–280
Frankel S, Gunnell D, Peters T, Maynard M, Davey Smith G (1998) Childhood energy intake and adult cancer—the Boyd Orr study. BMJ 316:499–504
Hislop TG, Coldman AJ, Elwood JM, Brauer G, Kan L (1986) Childhood and recent eating patterns and risk of breast cancer. Cancer Detect Prev 9:47–58
Maynard M, Gunnell D, Emmett P, Frankel S, Davey Smith G (2003) Fruit, vegetables and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. J Epidemiol Community Health 57:218–225
Potischman N, Weiss HA, Swanson CA et al (1998) Diet during adolescence and risk of breast cancer among young women. J Natl Cancer Inst 90:226–233
Gunnell D, Okasha M, Davey Smith G, Oliver SE, Sandhu J, Holly JMP (2001) Height, leg length, and cancer risk: a systematic review. Epidemiol Rev 23:296–325
Gunnell D, Davey Smith G, Frankel S et al (1998) Childhood leg length and adult mortality: follow-up study of the Carnegie (Boyd Orr) survey of diet and health in pre-war Britain. J Epidemiol Community Health 52:142–152
Albanes D, Jones DY, Schatzkin A, Micozzi MS, Taylor PR (1988) Adult stature and risk of cancer. Cancer Res 48:1658–1662
Zuccolo L, Harris R, Gunnell D et al (2008) Height and prostate cancer risk: a large nested case–control study (ProtecT) and meta-analysis. Cancer Epidemiol Biomarkers Prev 17:2325–2336
Rao S, Joshi S, Kanade A (2000) Growth in some physical dimensions in relation to adolescent growth spurt among rural Indian children. Ann Hum Biol 27:127–138
Ahlgren M, Melbye M, Wohlfahrt J, Sorensen TI (2004) Growth patterns and the risk of breast cancer in women. New Eng J Med 351:1619–1626
Kolonel LN, Nomura AMY, Lee J, Hirohata T (1986) Anthropometric indicators of breast cancer risk in postmenopausal women in Hawaii. Nutr Cancer 8:247–256
Kyogoku S, Hirohata T, Takeshita S, Hirota Y, Shigematsu T (1990) Anthropometric indicators of breast cancer risk in Japanese women in Fukuoka. Jap J Cancer Res 81:731–737
Demark-Wahnefried W, Conaway MR, Robertson CN, Mathias BJ, Anderson EE, Paulson DF (2007) Anthropometric risk factors for prostate cancer. Nutr Cancer 28:302–307
Chyou PH, Nomura AMY, Stemmermann GN (1994) A prospective study of weight, body mass index and other anthropometric measurements in relation to site-specific cancers. Int J Cancer 57:313–317
Micozzi MS (1987) Cross cultural correlations of childhood growth and adult breast cancer. Am J Phys Anthropol 73:525–537
Mondina R, Borsellino G, Poma S, Baroni M, Di Nubila B, Sacchi P (1992) Breast carcinoma and skeletal formation. Eur J Cancer 28:1068–1070
Gunnell D, Davey Smith G, Holly JMP, Frankel S (1998) Leg length and risk of cancer in the Boyd Orr cohort. BMJ 317:1350–1351
Gunnell DJ, Frankel S, Nanchahal K, Braddon FEM, Davey Smith G (1996) Lifecourse exposure and later disease: a follow-up study based on a survey of family diet and health in pre-war Bristain (1937–9). Public Health 110:85–94
Martin RM, Gunnell D, Pemberton J, Frankel S, Davey Smith G (2005) Cohort profile: the Boyd Orr cohort—an historical cohort study based on the 65 year follow-up of the Carnegie Survey of Diet and Health (1937–1939). Int J Epidemiol 34:742–749
Rowett Research Institute (1955) Family diet and health in pre-war Britain. Carnegie United Kingdom Trust, Dunfermline
World Health Organisation (2002) Tobacco smoke and involuntary smoking. Summary of data reported and evaluation
Martin RM, Davey Smith G, Mangtani P, Frankel S, Gunnell D (2002) Association between breast feeding and growth: the Boyd-Orr cohort study. Arch Dis Childhood Fetal Neonatal 87:193–201
Martin RM, Middleton N, Gunnell D, Owen CG, Davey Smith G (2005) Breastfeeding and cancer: the Boyd Orr cohort and a systematic review with meta-analysis. J Natl Cancer Inst 97:1446–1457
de Stavola BL, dos Santos Silva I, McCormack V, Hardy RJ, Kuh D, Wadsworth MEJ (2004) Childhood growth and breast cancer. Am J Epidemiol 159:671–682
van den Brandt PA, Spiegelman D, Yaun SS et al (2000) Pooled analysis of prospective cohort studies on height, weight and breast cancer risk. Am J Epidemiol 152:514–527
Lawlor DA, Okasha M, Gunnell D, Ebrahim S (2003) Associations of adult measures of childhood growth with breast cancer: findings from the British Women’s Heart and Health Study. Br J Cancer 89:81–87
Whitley E, Gunnell D, Davey Smith G, Holly J, Martin R (2008) Childhood circumstances and anthropometry: the Boyd Orr cohort. Ann Hum Biol 35:518–534
Acknowledgements
We acknowledge Professor Peter Morgan, the director of The Rowett Research Institute for the use of the archive and in particular Walter Duncan, honorary archivist to the Rowett Institute. We acknowledge the staff at the NHS Central Register at Southport and Edinburgh, and Professor John Pemberton for information concerning the conduct of the original survey. We wish to acknowledge all the participants and research workers in the original survey of 1937–1939. Clare Frobisher, Pauline Emmett and Maria Maynard undertook the re-analyses of the childhood household diet diaries. Tom Steuart-Feilding data entered cancer deaths and registrations. The World Cancer Research Fund supported the follow-up of the Boyd Orr cohort. Financial Support This work was funded by the World Cancer Research Fund.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whitley, E., Martin, R.M., Davey Smith, G. et al. Childhood stature and adult cancer risk: the Boyd Orr cohort. Cancer Causes Control 20, 243–251 (2009). https://doi.org/10.1007/s10552-008-9239-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9239-1