Abstract
Laboratory data suggest that caffeine or some components of coffee may cause DNA mutations and inhibit tumor suppressor mechanisms, leading to neoplastic growth. However, coffee consumption has not been clearly implicated in the etiology of human postmenopausal ovarian cancer. This study evaluated the relationship of coffee and caffeine intake with risk of epithelial ovarian cancer in a prospective cohort study of 29,060 postmenopausal women. The participants completed a mailed questionnaire that assessed diet and health history and were followed for ovarian cancer incidence from 1986 to 2004. Age-adjusted and multivariate-adjusted hazard ratios were calculated for four exposure variables: caffeinated coffee, decaffeinated coffee, total coffee, and total caffeine to assess whether or not coffee or caffeine influences the risk of ovarian cancer. An increased risk was observed in the multivariate model for women who reported drinking five or more cups/day of caffeinated coffee compared to women who reported drinking none (HR = 1.81, 95% CI: 1.10–2.95). Decaffeinated coffee, total coffee, and caffeine were not statistically significantly associated with ovarian cancer incidence. Our results suggest that a component of coffee other than caffeine, or in combination with caffeine, may be associated with increased risk of ovarian cancer in postmenopausal women who drink five or more cups of coffee a day.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the fifth most common cause of female cancer mortality in the United States [1]. While incidence has decreased since 1987, mortality rates have remained steady [1]. Currently, there are no effective screening measures for ovarian cancer, and as a result 71% of ovarian cancer cases are diagnosed at an advanced stage with a poor prognosis [2]. Presently, the most effective strategies for prevention of ovarian cancer are prophylactic oophorectomy and identification and reduction of modifiable risk factors. Established risk factors for ovarian cancer include age, family history of ovarian or breast cancer, postmenopausal hormone use, nulliparity, never use of oral contraceptives, tubal ligation, early menarche, and late menopause. However, data on other potentially modifiable risk factors such as diet are less consistent [1, 2].
One dietary factor that has been studied relative to ovarian cancer etiology is coffee, which is widely consumed in developed countries. Sixteen case–control studies [3–18] and six cohort studies [19–24] have examined the relationship between coffee intake and ovarian cancer with inconsistent results. Cohort studies tended to observe a higher risk for ovarian cancer than case–control studies, but in most cases, the results have not been statistically significant. Coffee is a complex food item with numerous chemical constituents and studies have not clearly demonstrated either an overall protective or detrimental effect with regard to ovarian cancer risk. Cell culture studies indicate that caffeine may affect cell cycle function, induce apoptosis, and alter cell cycle regulation; however, difference in cell types and caffeine concentrations make translation to human relevance unclear [25]. Other components of coffee, such as the diterpenes cafestol and kahweol [26], have been shown to be potentially protective against cancer.
We examined the relationship between coffee and/or caffeine and ovarian cancer using prospective data from the Iowa Women’s Health Study, a cohort of postmenopausal women. Our analysis explored four separate exposure variables: caffeinated coffee, decaffeinated coffee, total coffee (both caffeinated and decaffeinated), and total caffeine intake, a measure of caffeine from all food and beverage sources. Our hypothesis was that coffee, because it includes a significant amount of caffeine, is associated with an increased risk of ovarian cancer.
Materials and methods
Study design and population
The Iowa Women’s Health study (IWHS) focused on exploring the association of dietary and other lifestyle exposures with cancer occurrence. In 1986, a 16-page questionnaire was mailed to 98,826 women in Iowa aged 55–69 years who were randomly selected based on the Iowa state driver’s license list. A total of 41,836 women (42.3% response rate) completed and returned the questionnaire. These women constituted the cohort and have been followed for cancer incidence and mortality since 1986. Five follow-up questionnaires were mailed to update vital status, residence, and exposure information, and the percent response to each was high: 91% in 1987, 90% in 1989, 83% in 1992, 79% in 1997, and 69% in 2004. Data from the 1986 questionnaire was used for this analysis. Compared with non-respondents to the original 1986 questionnaire, respondents were three months older, had a lower mean body mass index (BMI) (weight in kilograms divided by height in meters squared), and were more likely to live in less affluent and rural counties. Incidence rates of all major cancers except for lung cancer were similar in respondents and non-respondents to the original questionnaire [27].
Data collection
The self-administered questionnaire included information on demographic characteristics, menstrual and reproductive health history, family cancer history, personal habits including diet, physical activity and smoking, weight and height, medication use, and medical conditions. Women reported demographic information including age, race, education level, and area of residence (e.g., rural, urban). Specific information regarding reproductive health history was collected and included: age when periods stopped for 12 months (which was defined as onset of menopause), number of births, oral contraceptive use, and hormone replacement therapy. Family history of major female cancers (breast, ovarian, uterine corpus, and uterine cervix) was assessed for living and deceased female blood relatives of participants. Self-reported weight and height were used to calculate BMI as a measure of relative weight. Women reported frequencies of moderate and vigorous physical activity and the data were categorized into three levels as follows: (1) moderate or vigorous physical activity performed a few times a month or less was considered low activity, (2) moderate physical activity one to four times a week or vigorous activity once a week was considered medium physical activity, and (3) moderate physical activity performed four or more times a week or vigorous physical activity performed two or more times a week was considered high physical activity.
The 1986 baseline questionnaire included a 127-item food frequency questionnaire (FFQ) that assessed food and beverage intake over the past year. The questionnaire specified a portion size for each food and beverage. For decaffeinated coffee and regular coffee, the specified portion size was one cup (eight fluid ounces). Participants recorded frequency of intake as “never or less than once per month,” “one to three cups per month,” “one cup per week,” “two to four cups per week,” “five to six cups per week,” “one cup per day,” “two to three cups per day,” “four to five cups per day,” or “six or more cups per day.”
The validity of the FFQ was evaluated by comparing nutrient values from the FFQ to those from the average of five 24-h dietary recall surveys for 44 study participants. Reliability of the instrument was examined by re-administering the FFQ three to six months after the initial FFQ was completed in this sample. The correlation between caffeine intake estimates from the dietary recalls and the FFQ was r = 0.95, suggesting excellent validity of the instrument for estimating caffeine intake. Test-retest reliability of the instrument for caffeine was also good (r = 0.82) [28].
Women who provided incomplete exposure information by leaving 30 or more items blank on the FFQ, had extremely low (<600 kcal) or high (>5,000 kcal) energy intakes, had a diagnosis of any cancer other than non-melanoma skin cancer at baseline, or reported bilateral oophorectomy were excluded from our analyses.
Ascertainment of incident epithelial ovarian cancer cases
Incident cases of epithelial ovarian cancer (ICD0-3 = 569) within the IWHS cohort from 1986 to 2004 were obtained through linkage to the State Health Registry of Iowa, part of the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) program. Participants contributed person-years of follow-up from baseline to one of the following outcomes: death, emigration from Iowa, date of ovarian cancer diagnosis, or date of bilateral oophorectomy. If one of these events did not occur, a participant was assumed to contribute follow-up time until 2004.
Statistical analysis
All analyses were performed using SAS version 9 (SAS Institute, Cary, NC). Hazard ratios (HRs) and 95% CI were calculated using Cox proportional hazards regression for the association between ovarian cancer incidence and the four exposure variables: caffeinated coffee, decaffeinated coffee, total coffee (decaffeinated + caffeinated coffee), and total caffeine intake. The caffeine variable includes all foods with chocolate (21 mg of caffeine per 100 g), tea (27 mg of caffeine per 100 g), coffee (58 mg per 100 g), and soda (13 mg per 100 g). Eighty-eight percent of total caffeine intake was contributed by coffee. Caffeinated coffee, decaffeinated coffee, and total coffee were categorized into five groups based on intake of cups per day: zero cups/day, less than one cup per day, one to two cups per day, three to four cups per day, and five or more cups per day. The cut points for the five groups were determined a priori based on similar studies of coffee intake and ovarian cancer. Total caffeine intake was categorized into quintiles. Age-adjusted and multivariate-adjusted hazard ratios of ovarian cancer among intake groups were calculated for all four exposure variables with the lowest intake group as the reference.
Potential covariates considered during modeling included biologically relevant factors (age, race, education level, smoking status, age of menopause, oral contraceptive use, postmenopausal hormone use, parity, family history of ovarian and breast cancer, physical activity, and energy intake) and factors found to be previously associated with ovarian cancer incidence in this cohort (intake of eggs, total vegetables, green leafy vegetables, lactose, and cholesterol) [29]. Information on tubal ligation, another possible risk factor for ovarian cancer, was not available. Variables were retained in the final model if they had biological relevance, had previously been shown to be a risk factor, or altered the HR estimate of ovarian cancer by at least 10%. A missing values category was included for each categorical variable in the model. Covariates included in the final multivariate model were age (at baseline, years), smoking (ever/never), BMI (continuous), age at menopause (continuous), parity (ever, never), duration of oral contraceptive use (≤1 month, 2–6 months, 7–12 months, 1–2 years, 3–5 years, ≥5 years), education level (<high school, high school, >high school), physical activity level (low, medium, high), and energy intake (kcal/day).
A sensitivity analysis was conducted to determine whether or not the inclusion or exclusion of women with unilateral oophorectomy history at baseline significantly altered the model. No significant differences in HR estimates were observed; therefore, women with unilateral oophorectomy were included in the final model.
Results
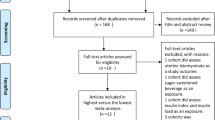
Of 41,836 potentially eligible participants at baseline, 3,829 (9.2%) were excluded due to a previous cancer diagnosis, 3,102 (7.4%) for incomplete FFQ data, and 5,845 (14.0%) due to bilateral oophorectomy. A total of 29,060 (69.5%) women were included in the final analysis. Baseline characteristics of cohort members relating to their level of total coffee intake are found in Table 1. Compared to women who drank no coffee, those who drank ≥5 cups/day were younger, had a lower BMI, had a lower level of education, were younger at menopause, were more likely to have had children, were more likely to use oral contraceptives, had lower physical activity levels, had ever smoked, resided in a city with a population >10,000, and had a higher energy intake.
Hazard ratios and 95% CI for ovarian cancer incidence by category of the exposure variables were calculated for: total coffee, decaffeinated coffee, caffeinated coffee, and caffeine (Table 2). A statistically significantly higher risk of ovarian cancer was observed for women who reported drinking ≥5 cups/day of caffeinated coffee compared to women who did not drink coffee (HR = 1.81, 95% CI: 1.11–2.95, p for trend = 0.15). No statistically significant associations with ovarian cancer risk were observed for the other caffeinated coffee consumption groups, and no obvious dose-response was observed. Similarly, no statistically significant associations were observed between decaffeinated coffee, total coffee, and caffeine intake and ovarian cancer risk.
Due to a relatively small number of ovarian cancer cases in the higher intake groups, we performed an analysis which combined the two highest intake groups for the caffeinated coffee and decaffeinated coffee analyses. The HR estimates associated with ≥3 cups of coffee/day were similar to the HR for the highest intake group in the original five-category intake group for both caffeinated and decaffeinated coffee, but the HR was not statistically significantly different from 1.0 (HR = 0.75, 95% CI: 0.44–1.26 for decaffeinated coffee, HR = 1.29, 95% CI: 0.89–1.89 for caffeinated coffee). Similar results were observed when we evaluated the risk of ≥4 cups/day for caffeinated and decaffeinated coffee.
Discussion
In this cohort study, no associations were found between decaffeinated coffee, total coffee, or caffeine intake and risk of ovarian cancer. We found that women who consumed ≥5 cups/day of caffeinated coffee intake were at approximately a twofold higher risk of ovarian cancer compared to coffee non-consumers; however, no dose-response was observed because no statistically significant increased risks were found in lower consumption groups.
Sixteen case–control studies and six cohort studies have examined the relationship between coffee intake and ovarian cancer (summarized in Tables 3 and 4). Among the case–control studies, three reported a statistically significant higher risk of ovarian cancer with higher levels of coffee intake [3, 6, 9], six reported a non-statistically significant higher risk [8, 10–12, 14, 17], and three found higher risk but did not report confidence intervals [4, 5, 7]. In contrast, one of the case–control studies found a statistically significant inverse association between coffee consumption and ovarian cancer [15], and three found inverse associations that were not statistically significant [13, 16, 18]. Of the six cohort studies, four reported slightly higher risks that were not statistically significant [19–21, 23], one found a statistically significant higher risk of ovarian cancer with higher levels of caffeine intake [22], and one found coffee intake to be protective against ovarian cancer but the association was not statistically significant [24]. In the most recent cohort study, Tworoger et al. used data collected from the Nurses Health Study and found that menopausal status was an effect modifier in their analysis of caffeine intake and ovarian cancer risk. For premenopausal women, the authors found an increased risk in ovarian cancer with increased caffeine intake (HR = 1.29; 95% CI: 0.78–2.14) but a modest decreased risk in ovarian cancer for postmenopausal women (RR = 0.89; 95% CI: 0.58–1.36). However, neither association was statistically significant. Our analysis found conflicting results as we found an increased risk for postmenopausal women who drink five or more cups of coffee a day. These results warrant the need for further research on postmenopausal status as a possible effect modifier. A meta-analysis reported a statistically non-significant 1.18-fold higher risk of ovarian cancer with higher coffee intake compared to the lowest intake group (95% CI: 0.97–1.44), however, methods for categorizing high vs. low coffee intake varied across studies [23]. When stratified by study design, a higher risk was reported in the cohort studies in comparison to the case–control studies (HR = 1.32, 95% CI: 0.99–1.77 vs. OR = 1.15, 95% CI: 0.89–1.47, respectively) [23]. Our findings of a statistically significant association in only the highest intake group and no dose-response are similar to those of one previous cohort study [22] and several case–control studies [3, 6, 9]. The observed statistically significant association in the highest coffee consumption group could be due to chance based on the lack of a dose-response relationship.
Variations in coffee preparation methods may explain some differences in study results. McCusker et al. [30] analyzed caffeine content in 14 different types of specialty coffee from coffee shops, and found that the amount of caffeine in an eight fluid ounce cup ranged from 72 to 130 mg. Coffee portion size and preparation methods vary among different cultures and time periods. For example, Australians typically drink instant coffee, whereas Americans tend to drink filtered coffee, and Italians consume mainly mocha and espresso. A study of pregnant women in the United States found that coffee cup sizes used by participants ranged from 2 to 32 fluid ounces and only 30% of coffee cups were seven to eight fluid ounces, which is the standard portion size used for most FFQ instruments, including the FFQ used for the IWHS [31]. Cut points for coffee intake groups differ widely among studies, as do covariates used in the data analyses.
Our hypothesis that caffeine was the primary carcinogenic component of coffee was not supported by our analyses that focused specifically on caffeine, which showed no statistically significant associations with ovarian cancer risk. A component of caffeinated coffee other than caffeine appears to increase the risk of ovarian cancer among ≥5 cups/day caffeinated coffee consumers in our cohort. Other explanations include the possibility that caffeine may work in combination with other components of coffee to increase risk. High coffee intake may be highly correlated with another exposure or behavior that contributes to ovarian cancer risk.
Coffee is a complex plant with many chemical components. Very little is known about these various components and their relationship with cancer risk. Some coffee components contain volatile heterocyclic compounds that may be carcinogenic [22]. Other components of coffee, such as the phytochemicals cafestol and kahweol, may play a protective role against carcinogens by preventing DNA damage, protecting against H2O2 oxidative stress, and acting as antioxidants [32]. More research is needed to better understand how the various chemical components of coffee interact in relation to ovarian cancer risk.
Another potentially relevant aspect of the coffee and ovarian cancer association is genetic variation in caffeine metabolism. Several recent studies have considered the effects of polymorphic variants in the CYP1A1 and CYP1A2 genes, cytochrome P450 enzymes involved in caffeine metabolism. Terry et al. [33] found that among women who consumed more than 204.5 mg caffeine/day, those who had the heterozygous CYP1A1 4889 (rs1048943) Ile/Val genotype had a higher risk of ovarian cancer compared to women with the homozygous CYP1A1 4889 Ile/Ile genotype (OR = 2.7, 95% CI = 1.2–6.2). Similarly, Goodman et al. [14] found that women who had the CYP1A2 (CYP1A2*1F, rs762551) AA genotype and reported drinking seven or more cups of coffee per week had a higher risk of ovarian cancer (OR = 2.5, 95% CI = 1.1–5.6) compared to women with the CYP1A2*1F AA genotype who did not drink coffee. Future studies should also consider genetic variation in DNA repair genes given the in vitro reports that caffeine may be misincorporated into DNA as a purine analog.
Strengths of this study include the use of a prospective study design, and a sizeable accumulation of epithelial ovarian cancer cases (n = 266) as a result of the long follow-up period. Limitations include the use of a single assessment of coffee and caffeine intake, which may have resulted in misclassification of the coffee and caffeine exposures over time. A follow-up FFQ was mailed to participants in 2004. Of the women included in the current analysis, 14,732 provided dietary intake data on both the 1986 and 2004 questionnaire. Mean caffeine intake decreased from 266.2 to 166.3 mg/day. Intake of caffeinated coffee, specifically, decreased from a mean of 12 cups/week in 1986 to seven cups/week in 2004. Similarly, mean intake of decaffeinated coffee decreased from 7.1 cups/week in 1986 to 3.6 cups/week in 2004. Caffeine intake decreased across all categories of baseline caffeinated coffee intake (no cups/day, <1 cup/day, 1–2 cups/day, 3–4 cups/day, or 5 or more cups/day). Individuals who had been classified as usually consuming five or more cups/day at the 1986 questionnaire reported an average of 2.4 cups/day of caffeinated coffee at the 2004 follow-up dietary intake assessment. Considering the average age of the women in 2004 was 79, this is not surprising. Additionally, the IWHS cohort is composed of postmenopausal, mainly Caucasian women, which limits the generalizability of results to ethnically similar populations and women who have completed menopause.
In conclusion, our study found a statistically significantly higher risk of ovarian cancer among women who reported drinking five or more cups of caffeinated coffee per day compared to non-consumers of coffee. Future studies of coffee, caffeine, and the risk of ovarian cancer should consider other components of coffee that may interact with caffeine to increase the risk of ovarian cancer, and the potential for interactions with genetic polymorphisms involved in caffeine metabolism and DNA repair.
References
American Cancer Society (2006) How many women get ovarian cancer?. American Cancer Society, Inc, Atlanta
Hankinson SE, Danforth KN (2006) Ovarian cancer. In: Schottenfeld D, Fraumeni JF Jr (eds) Cancer epidemiology and prevention, 3rd edn. Oxford University Press, New York
Trichopoulos D, Papapostolou M, Polychronopoulou A (1981) Coffee and ovarian cancer. Int J Cancer 28:691–693. doi:10.1002/ijc.2910280606
Byers T, Marshall J, Graham S, Mettlin C, Swanson M (1983) A case–control study of dietary and nondietary factors in ovarian cancer. J Natl Cancer Inst 71:681–686
Cramer DW, Welch WR, Hutchinson GB, Willett W, Scully RE (1984) Dietary animal fat in relation to ovarian cancer risk. Obstet Gynecol 63:833–838
La Vecchia C, Franceschi S, Decarli A et al (1984) Coffee drinking and the risk of epithelial ovarian cancer. Int J Cancer 33:559–562. doi:10.1002/ijc.2910330502
Tzonou A, Day NE, Trichopoulos D, Walker A, Saliaraki M, Papapostolou M, Polychronopoulou A (1984) The epidemiology of ovarian cancer in greece: a case–control study. Eur J Cancer Clin Oncol 20:1045–1052. doi:10.1016/0277-5379(84)90107-X
Miller DR, Rosenberg L, Kaufman DW et al (1987) Epithelial ovarian cancer and coffee drinking. Int J Epidemiol 16:13–17. doi:10.1093/ije/16.1.13
Whittemore AS, Wu ML, Paffenbarger RS Jr et al (1988) Personal and environmental characteristics related to epithelial ovarian cancer. II. Exposures to talcum powder, tobacco, alcohol, and coffee. Am J Epidemiol 128:1228–1240
Hartge P, Schiffman MH, Hoover R, McGowan L, Lesher L et al (1989) A case–control study of epithelial ovarian cancer. Am J Obstet Gynecol 161:10–16
Polychronopoulou A, Tzonou A, Hsieh CC et al (1993) Reproductive variables, tobacco, ethanol, coffee and somatometry as risk factors for ovarian cancer. Int J Cancer 55:402–407. doi:10.1002/ijc.2910550312
Kuper H, Titus-Ernstoff L, Harlow BL, Cramer DW (2000) Population based study of coffee, alcohol and tobacco use and risk of ovarian cancer. Int J Cancer 88:313–318 10.1002/1097-0215(20001015)88:2<313::AID-IJC26>3.0.CO;2-5
Tavani A, Gallus S, Dal Maso L et al (2001) Coffee and alcohol intake and risk of ovarian cancer: an Italian case–control study. Nutr Cancer 39:29–34
Goodman MT, Tung KH, McDuffie K, Wilkens LR, Donlon TA (2003) Association of caffeine intake and CYP1A2 genotype with ovarian cancer. Nutr Cancer 46:23–29. doi:10.1207/S15327914NC4601_03
Jordan SJ, Purdie DM, Green AC, Webb PM (2004) Coffee, tea and caffeine and risk of epithelial ovarian cancer. Cancer Causes Control 15:359–365. doi:10.1023/B:CACO.0000027482.00077.8b
Riman T, Dickman PW, Nilsson S, Nordlinder H, Magnusson CM, Persson IR (2004) Some life-style factors and the risk of invasive epithelial ovarian cancer in Swedish women. Eur J Epidemiol 19:1011–1019. doi:10.1007/s10654-004-1633-8
Baker JA, Boakye K, McCann SE et al (2007) Consumption of black tea or coffee and risk of ovarian cancer. Int J Gynecol Cancer 17:50–54. doi:10.1111/j.1525-1438.2006.00773.x
Song J, Kristal AR, Wicklund KG, Cushing-Haugen KL, Rossing MA (2008) Coffee, Tea, Colas, and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev 17:712–716. doi:10.1158/1055-9965.EPI-07-2511
Snowdon DA, Phillips RL (1984) Coffee consumption and risk of fatal cancers. Am J Public Health 74:820–823
Stensvold I, Jacobsen BK (1994) Coffee and cancer: a prospective study of 43,000 Norwegian men and women. Cancer Causes Control 5:401–408. doi:10.1007/BF01694753
Larsson SC, Wolk A (2005) Coffee consumption is not associated with ovarian cancer incidence. Cancer Epidemiol Biomarkers Prev 14:2273–2274. doi:10.1158/1055-9965.EPI-05-0280
Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE (2007) Intake of coffee and tea and risk of ovarian cancer: a prospective cohort study. Nutr Cancer 58:22–27
Steevens J, Schouten LJ, Verhage BA, Goldbohm RA, Van Den Brandt PA (2007) Tea and coffee drinking and ovarian cancer risk: results from the Netherlands Cohort Study and a meta-analysis. Br J Cancer 97:1291–1294. doi:10.1038/sj.bjc.6604008
Tworoger SS, Gertig DM, Gates MA, Hecht JL, Hankinson SE (2008) Caffeine, alcohol, smoking, and the risk of incident epithelial ovarian cancer. Cancer 112(5):1169–1177. doi:10.1002/cncr.23275
Bode AM, Dong Z (2007) The enigmatic effects of caffeine in cell cycle and cancer. Cancer Lett 247(1):26–39. doi:10.1016/j.canlet.2006.03.032
Cavin C, Holzhaeuser D, Scharf G, Constable A, Huber WW, Schilter B (2002) Cafestol and kahweol, two coffee specific diterpenes with anticarcinogenic activity. Food Chem Toxicol 40:1155–1163. doi:10.1016/S0278-6915(02)00029-7
Bisgard KM, Folsom AR, Hong CP, Sellers TA (1994) Mortality and cancer rates in nonrespondents to a prospective study of older women: 5-year follow-up. Am J Epidemiol 139:990–1000
Pereira MA, Parker ED, Folsom AR (2006) Coffee consumption and risk of type 2 diabetes mellitus. Arch Intern Med 166:1311–1316. doi:10.1001/archinte.166.12.1311
Kushi LH, Mink PJ, Folsom AR, Anderson KE, Zheng W, Lazovich D, Sellers TA (1999) Prospective study of diet and ovarian cancer. Am J Epidemiol 149:21–31
McCusker RR, Goldberger BA, Cone EJ (2003) Caffeine content of specialty coffees. J Anal Toxicol 27:520–522
Bracken MB, Triche E, Grosso L et al (2002) Heterogeneity in assessing self-reports of caffeine exposure: implications for studies of health effects. Epidemiology 13:165–171. doi:10.1097/00001648-200203000-00011
Lee KJ, Jeong HG (2007) Protective effects of kahweol and cafestol against hydrogen peroxide-induced oxidative stress and DNA damage. Toxicol Lett 173(2):80–87. doi:10.1016/j.toxlet.2007.06.008
Terry KL, Titus-Ernstoff L, Garner EO, Vitonis AF, Cramer DW (2003) Interaction between CYP1A1 polymorphic variants and dietary exposures influencing ovarian cancer risk. Cancer Epidemiol Biomarkers Prev 12:187–190
Acknowledgments
The authors thank Aaron R. Folsom, MD, MPH for providing the Iowa Women’s Health Study data and Ching-Ping Hong, MS and Gretchen Cutler, MPH for assistance in data preparation prior to data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lueth, N.A., Anderson, K.E., Harnack, L.J. et al. Coffee and caffeine intake and the risk of ovarian cancer: the Iowa Women’s Health Study. Cancer Causes Control 19, 1365–1372 (2008). https://doi.org/10.1007/s10552-008-9208-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9208-8