Abstract
Background
Modifying multiple behavior risks is a promising approach to reduce cancer risk. Primary prevention advices of the European Code against Cancer were included in an educational intervention (EI) using social cognitive theories for motivating families with cancer experiences to adopt six cancer prevention behaviors.
Methods
A randomized clinical controlled trial recruited 3,031 patients from Primary Care among cancer patients’ relatives. The experimental group (EG) received four EI, one EI every six months, focused on tobacco, alcohol, diet, weight, sun and work, and based on social cognitive models. The impact of the first three EI was calculated measuring at baseline and 18 months later: (a) The percentage of people with each risk behavior; (b) The score reached in a Total Cancer Behavioral Risk (TCBR) indicator; (c) The Odds Ratios at the post-test.
Results
Five risk behaviors decreased significantly more (p < 0.01) in the EG than in the CG: Smoking (OR = 0.662), drinking (OR = 0.504), diet (OR = 0.542), weight (OR = 0.698), and sun (OR = 0.389). The TCBR indicator also decreased an average of nearly 5 points (28.42 vs. 23.82), significantly more (p < 0.001) in the EG.
Conclusion
Families with cancer experiences changed five cancer risk behaviors when approached in Primary Care with interventions based on social cognitive models.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The highest cancer mortality rates in Spain appear in the Principality of Asturias, a northern region of around 1,100,000 inhabitants, with cancer crude mortality rates of 417 per 100,000 in males and 215 per 100,000 in women. These rates in Cantabria, another northern region, are 343 per 100,000 in males and 171 per 100,000 in women [1]. Deaths from cancer are 27.31% of the total (33.64 in men and 20.56 in women) and 28.61 of the total (34.86 in men and 21.64 in women) in Asturias and Cantabria, respectively [2]. Most prevalent tumors could potentially be prevented by educative interventions because they have been linked to sun, diet, and smoking among others.
The European Code against Cancer (ECC) was established in 1987 due to a background of increasing cancer incidence and death rates, particularly in men, virtually worldwide. The ECC was revised in 1994 [3] and 2003 [4]. A target to reduce cancer mortality in Europe by 15% by the year 2000 was set. The current ECC is included in Table 1.
A recent study [5] shows that only Finland and Austria achieved reductions of 15% in cancer mortality. Cancer control seems to be failing in Spain, Portugal, and Greece. Rodríguez and Gutiérrez-Fisac [6] evaluated the fulfillment of the aim in Spain and found out that the mortality from cancer had increased 8 percentage points instead of decreasing, probably due, in part, to an insufficient preventive effort.
These data imply increasing the number of interventions focusing on the prevention of cancer and the diffusion of the ECC in Spain for the general public and for high-risk patients, above all in genetically predisposed individuals [7]. The identification of particular at-risk populations is increasingly possible [8], as can be persons with a family history of cancer. This article will address the latter group, because studies suggest that they may be more motivated to adopt preventive behaviors [9–12].
The primary prevention behaviors proposed by the ECC can be studied by means of psychosocial models that try to explain human behavior. We used a model that integrates insights of various theories, the A.S.E. Model [13–15], which has been applied to analyze various health behaviors [16–21] but not yet for studying multiple behavior changes.
The A.S.E. Model (now denominated the I-Change Model) incorporates elements from Fishbein-Ajzen [22], Bandura [23] and Prochaska and DiClemente’s [24] theories. It establishes that behavior is associated with three psychosocial determinants (attitude, social influence, and self-efficacy), through intention. An experimental design permits the effect of these determinants on behavior and its changes to be controlled.
Multiple health behavior change has been recognized of great importance and is recommended to increase efficiency [25–28], but there are only a few studies that test the efficacy of multiple lifestyle approaches [29–32]. Our study seems to be the only one that focuses on six risk factors included in the ECC within the Primary Care setting for families susceptible to primary prevention and, in this sense, is an advance on previous research.
Changing behaviors and evaluating changes due to an intervention is not easy [33]. The investigators usually report low enrollment rates [34], but methods to involve many people (telephone, mailing of written material, etc.) have some limitations [35, 36]. Furthermore, two-way interactions are likely more motivational [37]. Professionals in Primary Care can implement complex face-to-face interventions and evaluate them trying to overcome limitations.
This study has three aims: (1) To evaluate the impact of an educational intervention (EI) developed in Primary Care, on six preventive behaviors, among cancer risk families. (2) To measure the impact on a Total Cancer Behavioral Risk (TCBR) indicator. (3) To analyze the A.S.E. determinants as predictors of the six risk behaviors.
Methods
Subjects
Patients were recruited in 2001–2002, among those attending primary care centers in Asturias and Cantabria, two regions in the north of Spain that have the highest cancer incidence and mortality rates in our country [1]. The selection criteria were: age between 15 and 50 years and having a first or second-degree relative, dead or alive, affected by cancer, because this population increases the efficiency of the interventions [9, 11]. Patients who were willing to participate were asked to give their informed consent. People under 18 were included if they wished to participate and if their parents gave informed consent. The patients were given their next appointment (six months later) at the clinics, and were reminded by telephone up to a maximum of three times. The University’s review board approved the study. Twenty-four trained doctor–nurse units from 14 primary care centers took part.
Design
A randomized clinical controlled trial was designed. Patients were randomly assigned to the experimental (EG) and the control group (CG). The EG received a tailored educational intervention and the CG the usual care.
Intervention
The intervention used principles of health counseling that tailored the content of the information to the motivational stage of the respondent [38, 39]. It emphasized the advantages of the ECC preventive behaviors among pre-contemplative and contemplative patients, following Prochaska and Di Clemente’s stages of change classification [40]. A prior qualitative investigation [41] provided a list of the advantages and disadvantages of following the ECC advice (see example in Fig. 1) perceived by the target population. A question classified the patients into five stages of change to tailor the EI. Persons motivated to change received information on how to cope with barriers to change (self-efficacy enhancing information) and skills to be able to change. When advisable, they were sent to specific preventive programs (Fig. 1). Persons in action and maintenance were encouraged to continue to adopt their healthy behavior. A booklet and poster were used as reinforcement materials. Four individual face-to-face interventions were implemented in Primary Care centers, once every six months, during 2002–2003. The fourth intervention was carried out both in the EG and CG only for professional ethical reasons just after the post-test evaluation. Our study evaluates the impact of the first three interventions after a six-month follow-up. All respondents filled in a validated self-administered questionnaire [41].
Questionnaire
The questionnaire was completed at baseline (pre-test) and 18 months later and assessed outcomes and confounders (Table 2). Help was given by health care workers if the patients had questions.
Outcome variables
The primary prevention behaviors of cancer were measured in two ways: each behavior independently and dichotomically (risk/no risk); all the risk behaviors together, by means of the synthetic variable called Total Cancer Behavioral Risk (TCBR) indicator. Sample size was calculated to detect at least a variation pre–post in the TCBR = 1.5 points (α = 0.05; β = 0.10; estimated drop-outs = 20%).
Smoking and risk drinking, sun exposure and work were assessed by specific and dichotomus questions (Table 2). Body Mass Index was objectively measured by the doctors or nurses. Risk Diet was calculated by a Food Frequency Questionnaire [42] that included six theoretically protection foods and seven risk foods, frequently consumed in the region. It was estimated that there was a diet risk if the quotient between the annual frequency of consumption of protection food (PFCYF) and risk food (RFCYF) was less than 0.90. This indicator was validated by prediction, using the diet history of the patient, carried out by nutrition experts, as an external criterion.
Statistical analyses
Data analysis included basic descriptive statistics (Table 3). In order to study the comparability of EG and CG, Chi-square and Student’s t-test were used. Drop-out analyses were performed using logistic regression analysis (backward method) with social demographic factors, study variables (included in Table 2), family history of cancer, attitudes, social influences, self-efficacy, intention, and behaviors. Behaviors at the pre- and post-test were analyzed calculating and comparing the percentages. The Chi-square test was used to detect significant differences between groups and a logistic regression to control the status at baseline when comparing EG and CG at the post-test (Table 4). To assess the impact of the program on TCBR the average values of TCBR were also compared in the EG and CG, using t-tests.
Multiple linear regression analyses (backward method) were run to analyze predictors of TCBR at the post-test (Table 5) using a similar method as described for the drop-out analysis.
The effects of various factors—including experimental condition and A.S.E. determinants—on risk behaviors at the post-test (Table 6) were analyzed using several logistic regressions in which the baseline covariables already mentioned, served as potential explanatory variables in the model.
All analyses were performed using SPSS, version 12.0 (SPSS Inc., Chicago, IL, USA).
Results
Sample characteristics
A total of 3,031 patients filled in the questionnaire at the pre-test, while 169 (5%) refused, mainly men (p < 0.01), due to lack of time owing to workload. At baseline patients were randomly assigned to the EG (n = 1.490; 49.1%) and CG (n = 1.541; 50.9%). No significant differences were found (p > 0.1) in socio-demographic and family history variables between groups, at pre-test.
The average age of our sample was approximately 35 years and consisted mainly of women. Only 3% of the sample was under 18. Most of our respondents had at least a secondary education; had between one and two relatives affected by cancer; the average time since the last death ranged between five and six years. Of the 1,273 smokers (42% of the full sample) 17.14% were in pre-contemplation, 68.57% in contemplation, and 14.29% in preparation. Of the 303 risk drinkers (10% of the full sample), 23%, 52%, and 25%, respectively. Of the 758 people at risk diet (25% of the full sample), 24.8%, 62.8%, and 12.4%, respectively. Of the 1,382 people at risk weight (45.6% of the full sample), 6.36%, 49.56%, and 44.08%, respectively. Of the 488 people at risk for sun exposure (16.1% of the full sample), 13.66%, 39.75%, and 46.59%, respectively. Finally, of the 92 people at risk work (3% of the full sample), 10%, 46.67%, and 43.33%, respectively.
The post-test questionnaire was filled in by 2,641 people: 1,336 (50.60%) patients in the EG and 1,305 (49.4%) in the CG. A total of 12.87% of the people at baseline were drop-outs. Table 3 shows averages and percentages of the individual characteristics of the socio-demographic, family history of cancer and study variables at post-test. No significant differences were found (p ≥ 0.13 in all variables).
Drop-out analyses
A total of 390 patients dropped-out in the post-test: 39.48% of the EG and 60.51% of the CG. Logistic regression analysis revealed that drop-outs were more likely to be younger (age OR = 0.96; 95% CI: 0.94–0.99) and had slightly higher cancer risk scores as assessed by the TCBR (OR = 1.027; 95% CI: 1.014–1.040).
Effect of EI on isolated risk behaviors and on TCBR
Table 4 summarizes the differences between study groups. The percentage of people with risk behaviors decreased significantly in all the behaviors in the EG, except risk weight. The percentages of people with risk behavior at the post-test were significantly lower in the EG than in the CG, with one exception: cancer risk at work. The EI had the greatest effect on reducing sun exposure risk.
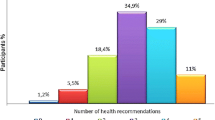
Furthermore, the TCBR dropped significantly in the EG from 28.42 (pre-test) to 23.82 (post-test) (p < 0.001); a smaller change was also noted in the CG (Fig. 2).
Table 5 shows the final model of multiple linear regression. First, the intervention was successful in reducing the TCBR. Controlling all the variables, those that are significantly associated with and reduce the TCBR in the post-test allows the following low-risk profile to be drawn: a woman from the EG, with university studies, high self-efficacy, and preventive attitude toward cancer. The older they are the less TCBR. The rest of controlled variables failed to be retained in this model. The highest standardized β coefficients were: belonging to the EG (−0.09), followed by the average attitude and gender. On the contrary, social influence and the TCBR score in the pre-test were associated with a higher TCBR in post-test.
Predictors of cancer risk behaviors
The outcomes of the various logistic regression analyses are shown in Table 6, and they permit the predictors of the six cancer risk behaviors at the post-test to be identified. The EI was successful for all behaviors but risk work: belonging to the EG reduced five out of six risk behaviors at the post-test. The ORs range between 0.389 and 0.698. After controlling for potential confounders, the results show that the intervention was effective above all in reducing risks related to sun exposure, excessive drinking, and unhealthy diet. The explained variance ranges from 23.6% (for risk work) to 78.7% (for risk weight).
Discussion
Our purpose was to test the efficacy of an intervention for families with cancer experiences, focusing on primary prevention behaviors as advised by the European Code against Cancer. We found significant changes in five out of six cancer risk behaviors and in the total cancer risk score.
The intervention was successful in reducing the percentage of people with risk behaviors. The greatest effect was achieved for behaviors related to tanning, alcohol consumption, and nutrition, which decreased between approximately 67% and 30%, respectively. The only comparable intervention study that we have found also showed effects on three cancer primary prevention behaviors simultaneously [31]. Prochaska detected significant treatment effects for smoking, diet, and sun exposure after 24-month follow-up with interventions contact on primary care patients. The improvement percentages were very similar to ours. But their criterion for sampling did not include having relatives affected by cancer, so our results are not exactly comparable. This intervention had great impact on sun exposure, as we also found.
Our control group also reduced, but to a lesser extent, their risks as other authors found [43–45]; this could be due to concomitant programs, the educational effect of filling—in the questionnaire or contamination among patients. But the multivariate analyses clarify the effect of the EI on the EG, controlling the rest of the variables. The logistic regression analysis showed the efficacy of the intervention for behaviors related to tanning, alcohol, diet, tobacco, and weight. Having a favorable attitude toward cancer prevention in the pre-test was associated with the risk reduction in the behaviors related to tobacco, diet, weight, and above all the alcohol intake. Self-efficacy at baseline was more related to influencing diet and, above all, sun exposure. In different studies self-efficacy has been shown to be one of the best predictors of behaviors [46], including diet behavior [47]. For this reason interventions should be focused on removing barriers and providing skills to increase self-efficacy. As expected, engaging in risk behaviors at baseline increased the risk of engaging in similar behaviors at post-test, with the highest risks for addictive behaviors, smoking, and alcohol use.
Furthermore, the total cancer behavioral risk score (TCBR) also showed an average reduction of almost 5 points in the experimental group, a reduction that was found to be significant in the regression analysis. Other factors related to lowering overall risk scores were demographic characteristics, such as being older, a woman, and having university studies, findings also found by other researchers [48–50]. Again, the scores of the A.S.E. determinants in the pre-test were associated with the reduction of the TCBR, especially attitude and self-efficacy. Both had demonstrated their influence on preventive behavior considered separately [16–20], but in the present study they also show their association with a global indicator of cancer behavioral risk, decreasing it.
An interesting finding was that the cancer family history characteristics (number of relatives with cancer, survival and time from the last death due to cancer) had very little influence on the efficacy of the intervention. Some authors suggested that interventions may be more effective for persons with a family cancer risk history [9–11, 49, 51]. An explanation for our findings may be that we addressed persons who all had a certain cancer risk history. It is conceivable that this overall risk was more significant than specific details on the type and history of cancer risk.
Our sample had an over-representation of women like other studies [52, 53] for several reasons: women attend Primary Care centers more often than men do [54, 55] and are more favorable to cancer prevention, primary [14, 56, 57] and secondary [58, 59].
Study limitations and strengths
First, the drop-outs had a slightly higher cancer risk at baseline, which could have influenced the results also slightly increasing the impact. However, losing more patients among those at maximum risk is normal in intervention studies [60]. Second, we arbitrarily used one indicator to measure the TCBR. Nevertheless our indicator has been sensitive enough to detect a reduction of almost 5 points in the cancer risk of the experimental group. This reduction is consistent with the one also detected in the percentage of patients with risk behaviors after the intervention, and therefore seems valid and reliable. Third, our over-representation of females hinders the generalization of the results to males.
Finally, despite the limitations, the strength of our study is that significant changes were achieved in our population of families with cancer experience. However, our results were obtained after six-months of follow-up since the third intervention. It is known that time can decrease the effect of Health Education interventions, and so the National Health System should include systematic and periodic interventions to prevent cancer in the Primary Care protocols, as the centers involved in this research promised to do after the efficacy of the EI was demonstrated.
Future research is needed to foster the enrollment of more men in similar studies and to determine what motivates multiple health behavior changes in patients without family risks. It is also necessary to study the optimum periodicity of the interventions that maintain the effect by means of long-term follow-up studied.
Conclusion
A protocolized intervention reduced cancer behavioral risk in five out of six behaviors related to cancer in relatives of cancer patients. The intervention was feasible and well accepted in Primary Care centers.
References
Martínez C, Peris R, Sánchez MJ (2002) Epidemiología descriptiva del cáncer en España. Tercer libro blanco de la Oncología en España. FESEO. Ergon, Madrid, pp 1–32
Instituto Nacional de Estadística (2004) INEbase; Defunciones según causa de muerte [online], Madrid. Available from: http://www.ine/inebase/menu3_soc.htm (Accessed 20 September 2006)
Boyle P, Veronesi U, Tubiana M et al (1995) European School of Oncology advisory report to the European Commission for the ‘Europe against cancer programme’ European code against cancer. Eur J Cancer 31(9):1395–1405 (Special Paper)
Boyle P, Autier P, Bartelink H et al (2003) European code against cancer and scientific justification: third version (2003). Ann Oncol 14(7):973–1005
Boyle P, d’Onofrio A, Maisonneuve P et al (2003) Measuring progress against cancer in Europe: has the 15% decline targeted for 2000 come about? Ann Oncol 4(8):1312–1325
Rodríguez F, Gutierrez-Fisac J (2000) El estado de salud y sus determinantes: evaluación de los objetivos 1 a 12. In: Álvarez C, Peiró S (eds) Informe SESPAS 2000: La salud pública ante los desafíos de un nuevo siglo. Escuela Andaluza de Salud Pública, Granada, pp 43–50
Tomatis L (2000) Etiologic evidence and primary prevention of cancer. Drug Metab Rev 32(2):129–137
Rimer BK (2000) Cancer control research 2001. Cancer Causes Control 11(3):257–270
Audrain J, Rimer B, Cella D et al (1999) The impact of a brief coping skills intervention on adherence to breast self-examination among first-degree relatives of newly diagnosed breast cancer patients. Psychooncology 8(3):220–229
Ryan EL, Skinner CS (1999) Risk beliefs and interest in counseling: focus group interviews among first-degree relatives of breast cancer patients. J Cancer Educ 4(2):9–103
Weston R (1999) Intervention and prevention. Eur J Cancer Prev 8(5):373–375
Halverson PK, Mays GP, Rimer BK, Lerman C, Audrain J, Kaluzny AD (1999) Adoption of a health education intervention for family members of breast cancer patients. Am J Prev Med 18(3):189–198
De Vries H, Mudde A, Leijs I et al (2003) The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Educ Res 18(5):611–626
De Vries H, Lezwijn J, Hol M, Honing C (2005) Skin cancer prevention: behaviour and motives of Dutch adolescents. Eur J Cancer Prev 14(1):39–50
De Vries H, Mesters I, Van de Steeg H, Honing C (2005) The general public’s information needs and perceptions regarding hereditary cancer: an application of the integrated change model. Patient Educ Couns 56(2):154–165
Brug J, Lechner L, De Vries H (1995) Psychosocial determinants of fruit and vegetable consumption. Appetite 25(3):285–296
Oostveen T, Knibbe R, de Vries H (1996) Social influences on young adults’ alcohol consumption: norms, modeling, pressure, socializing, and conformity. Addict Behav 21(2):187–197
Van Wechem SN, Van Assema P, Brug J (1997) Results of a community-based campaign to reduce fat intake. Nutr Health 11(3):207–218
De Vries H, Mudde AN (1998) Predicting stage transitions for smoking cessation applying the attitude-social influence-efficacy model. Psychol Health 13:369–385
De Vries H, Lechner L (2000) Motives for protective against carcinogenic substances in the workplace: a pilot study among Dutch workers. J Occup Environ Med 42(1):88–95
Lopez ML, Herrero P, Comas A et al (2004) Impact of cigarette advertising on smoking behaviour in Spanish adolescents as measured using recognition of billboard advertising. Eur J Public Health 14(4):428–432
Ajzen I (1991) The theory of planned behavior. Organ Behav Hum Decis Process 50 (2):179–211
Bandura A (1977) Self-efficacy—toward a unifying theory of behavioral change. Psychol Rev 84 (2):191–215
Prochaska JO, DiClemente CC (1982) Transtheorical therapy—toward a more integrative model of change. Psycother Theory Res Pract 19 (3):276–288
Glasgow RE, Goldstein MG, Ockene JK, Pronk NP (2004) Translating what we have learned into practice. Principles and hypotheses for interventions addressing multiple behaviors in primary care. Am J Prev Med 27(2 Suppl):88–101
Curry SJ (2004) Toward a public policy agenda for addressing multiple health risk behaviors in primary care. Am J Prev Med 27(2 Suppl):106–108
Pronk NP, Peek CJ, Goldstein MG (2004) Addressing multiple behavioral risk factors in primary care. A synthesis of current knowledge and stakeholder dialogue sessions. Am J Prev Med 27(2 Suppl):4–17
Gotay CC (2005) Behavior and cancer prevention. J Clin Oncol 23(2):301–310
Emmons KM, Stoddard AM, Gutheil C, Suarez EG, Lobb R, Fletcher R (2003) Cancer prevention for working class, multi-ethnic populations through health centers: the healthy directions study. Cancer Causes Control 14(8):727–737
Goldstein MG, Whitlock EP, DePue J (2004) Planning committee of the addressing multiple behavioral risk factors in primary care project. Multiple behavioral risk factor interventions in primary care Summary of research evidence. Am J Prev Med 27(2 Suppl):61–79
Prochaska JO, Velicer WF, Redding C et al (2005) Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med 41(2), 406–416
Emmons KM, McBride CM, Puleo E et al (2005) Project PREVENT: a randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidem Biomar 14(6):1453–1459
Thompson B, Coronado G, Chen L, Islas I (2006) Celebremos la salud! a community randomized trial of cancer prevention (United States). Cancer Causes Control 7(5):733–746
Ostroff J, Ross S, Steinglass P, Ronis-Tobin V, Singh B (2004) Interest in and barriers to participation in multiple family groups among head and neck cancer survivors and their primary family caregivers. Fam Process 43(2):195–208
Rector TS, Venus PJ, Laine AJ (1999) Impact of mailing information about nonurgent care on emergency department visits by Medicaid beneficiaries enrolled in managed care. Am J Manag Care. 5(12):1505–1512
Wahlberg AC, Cedersund E, Wredling R (2003) Telephone nurses’ experience of problems with telephone advice in Sweden. J Clin Nurs 12(1):37–45
Carney PA, Harwood BG, Greene MA, Goodrich ME (2005) Impact of a telephone counseling intervention on transitions in stage of change and adherence to interval mammography screening (United States). Cancer Causes Control 16(7):799–807
Pieterse ME, Seydel ER, DeVries H, Mudde AN, Kok GJ (2001) Effectiveness of a minimal contact smoking cessation program for Dutch general practitioners: a randomized controlled trial. Prev Med 32(2):182–190
Bolman C, De Vries H, Van Breukelen G (2002) A minimal-contact intervention for cardiac inpatients: long-term effects on smoking cessation. Prev Med 35(2):181–192
Prochaska JO, Velicer WF (1997) The transtheoretical model of health change. Am J Health Promot 12(1):38–48
López ML, García-Cueto E, Fernández JM. Del Valle MO, Cueto A (2003) Validation of a questionnaire to evaluate the attitude towards primary prevention advice from the European Code against cancer. Eur J Cancer Prev 12(2):157–164
López ML, Comas A, Del Valle MO, López S, García JB, Cueto-Espinar A (2004) Psychosocial factors associated with cancer behavioural risk in relatives of cancer patients. Eur J Cancer Prev 13(2):105–111
Carrel AL, Clark RR, Peterson SE, Nemeth BA, Sullivan J, Allen DB (2005) Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: a randomized, controlled study. Arch Pediat Adol Med 159(10):963–968
Powers AR, Struempler BJ, Guarino A, Parmer SM (2005) Effects of a nutrition education program on the dietary behavior and nutrition knowledge of second-grade and third-grade students. J School Health 75(4):129–133
Rothman RL, Malone R, Bryant B et al (2005) A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med 118(3):76–284
Dijkstra A, De Vries H (2000) Subtypes of precontemplating smokers defined by different long-term plans to change their smoking behavior. Health Educ Res 15(4):423–434
Ma J, Betts NM, Horacek T, Georgiou C, White A, Nitzke S (2002) The importance of decisional balance and self-efficacy in relation to stages of change for fruit and vegetable intakes by young adults. Am J Health Promot 16(3):157–166
Brunswick N, Wardle J, Jarvis MJ (2001) Public awareness of warning signs for cancer in Britain. Cancer Causes Control 12(1):33–37
Cohen M (2002) First-degree relatives of breast-cancer patients: cognitive perceptions, coping, and adherence to breast self-examination. Behav Med 28(1):15–22
Abroms L, Jorgensen CM, Southwell BG, Geller AC, Emmons KM (2003) Gender differences in young adults’ beliefs about sunscreen use. Health Educ Behav 30(1):29–43
Hadley DW, Jenkins J, Dimond E et al (2003) Genetic counseling and testing in families with hereditary nonpolyposis colorectal cancer. Arch Intern Med 163(5):573–582
Gonzalez CA, Navarro C, Martinez C et al (2004) The European prospective investigation about cancer and nutrition (EPIC). Rev Esp Salud Publica 78(2):167–176
Milch CE, Edmunson JM, Beshansky JR, Griffith JL, Selker HP (2004) Smoking cessation in primary care: a clinical effectiveness trial of two simple interventions. Prev Med 38(3):284–294
Kapur N, Hunt I, Lunt M, McBeth J, Creed F, Macfarlane G (2005) Primary care consultation predictors in men and women: a cohort study. Brit J Gen Pract 55(511):108–113
Vedsted P, Christensen MB (2005) Frequent attenders in general practice care: a literature review with special reference to methodological considerations. Public Health 119(2):118–137
Weinstock MA, Rossi JS, Redding CA, Maddock JE, Cottrill SD (2000) Sun protection behaviors and stages of change for the primary prevention of skin cancers among beachgoers in southeastern New England. Ann Behav Med 22(4):286–293
Baker AH, Wardle J (2003) Sex differences in fruit and vegetable intake in older adults. Appetite 40(3):269–275
Slattery ML, Kinney AY, Levin TR (2004) Factors associated with colorectal cancer screening in a population-based study: the impact of gender, health care source, and time. Prev Med 38(3):276–283
Nicholson FB, Korman MG (2005) Acceptance of flexible sigmoidoscopy and colonoscopy for screening and surveillance in colorectal cancer prevention. J Med Screen 12(2):89–95
McCann TJ, Criqui MH, Kashani IA et al (1997) A randomized trial of cardiovascular risk factor reduction: patterns of attrition after randomization and during follow-up. J Cardiovasc Risk 4(1):41–46
Acknowledgments
FIS 01/0311 and FICYT FC-02-PC-SPV01-14 grants supported this research. The authors wish to acknowledge: the contribution of the professionals, patients and sanitary authorities of the Principality of Asturias and Cantabria regions; the financial support of the RTICCC and ‘Obra Social Cajastur’.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
From Primary Care centers: Alonso Cortina, Mª Aurora; Alonso Montes, Flor; Álvarez González, Esperanza; Álvarez Gutiérrez, Lourdes; Blanco Diego, Julia; Blas Gutiérrez, Aurora de; Brun Gurpegui, Elisa; Cabañeros Vicente, Juan José; Cadaya Gabás, Mª Nieves; Castañeda García, Esperanza; Chamizo Vega, Carmen; Díez Lamadrid, Mª Josefa; Dorado Campos, Ofelia; Elena Sinobas, Pilar; Esparza Girón, Miguel; Fernández Prieto, Teresa; García Fernández, Ana Margarita; García Mata, Montserrat; Gonzalvo Rodríguez, Covadonga; Hermosa de la Llama, Mª Concepción; Lago García, Carmen Mª; Marín Ortega, Dolores; Plaza Verdesoto, Mª Fernanda; Sáiz Berzosa, Angélica; Sánchez Valles, Emma Rosa; Torre Arrarte, Begoña de la; Zumalacárregui Rodríguez, Mª Jesús. From the University of Oviedo: Martínez Canteli, Alejandra; Miguélez López, Ruth.
Rights and permissions
About this article
Cite this article
López, M.L., Iglesias, J.M., del Valle, M.O. et al. Impact of a primary care intervention on smoking, drinking, diet, weight, sun exposure, and work risk in families with cancer experience. Cancer Causes Control 18, 525–535 (2007). https://doi.org/10.1007/s10552-007-0124-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-0124-0