Abstract
There is some evidence from case–control studies that dietary fiber intake might be inversely associated with ovarian cancer risk, but there are limited prospective data. Therefore, we examined ovarian cancer risk in association with intake of dietary fiber in a prospective cohort of 49,613 Canadian women enrolled in the National Breast Screening Study (NBSS), who completed a self-administered food frequency questionnaire between 1980 and 1985. Linkages to national mortality and cancer databases yielded data on deaths and cancer incidence, with follow-up ending between 1998 and 2000. Data from the food frequency questionnaire were used to estimate intake of total dietary fiber, of fiber fractions, and of fiber from various sources. Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for the association between energy-adjusted quartile levels of fiber intake and ovarian cancer risk. During a mean 16.4 years of follow-up, we observed 264 incident ovarian cancer cases. Total dietary fiber and fiber fractions were not associated with ovarian cancer risk in this study population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is evidence from intervention studies that increases in dietary fiber intake are associated with a reduction in serum estrogen levels and reduced availability of steroid hormones (1–3). Given that serum estrogen has been shown to stimulate cell proliferation in ovarian epithelium (4) and to promote ovarian tumor progression (5), it is plausible that dietary fiber intake may be inversely associated with ovarian cancer risk.
To date, it appears that the relationship between dietary fiber intake and ovarian cancer risk has been examined in only one prospective cohort study (6). In that investigation, the authors found no association between total fiber intake and ovarian cancer risk (6). Given the current lack of prospective data regarding the role of dietary fiber in ovarian cancer etiology, we examined the relationships between total dietary fiber intake, intake of fiber fractions (soluble, insoluble, lignin, and cellulose), and source of dietary fiber (cereal, vegetable, and fruit) and ovarian cancer risk in a prospective cohort study of Canadian women.
Methods
Study population
The design of the study has been described in detail elsewhere (7). Briefly, 89,835 women aged 40–59 years were recruited into the Canadian National Breast Screening Study (NBSS) between 1980 and 1985 from the general Canadian population by various means, including personal invitation by letter, group mailings to employees of large institutions and to members of professional associations, advertisements in newspapers, and public service announcements on radio and television (8).
Questionnaires
At recruitment into the cohort, participants completed self-administered questionnaires that sought information on demographic characteristics, lifestyle factors, menstrual and reproductive history, and use of oral contraceptives and replacement estrogens. Women who reported having regular menstrual periods within the past 12 months were classified as premenopausal. Women whose menstrual periods ceased at least 12 months before enrolment into the study were considered to be postmenopausal (9).
Starting in 1982 (that is, after some participants had completed their scheduled visits to the screening centers), a self-administered food frequency questionnaire (FFQ) was distributed to all new attendees at all screening centers, and to women returning to the screening centers for re-screening (10). The FFQ sought information on usual portion size and frequency of consumption of 86 food items, and included photographs of various portion sizes to assist respondents with quantifying intake. A comparison between the self-administered questionnaire and a full interviewer-administered questionnaire, which has been subjected to both validity and reliability testing (10) and used in a number of epidemiologic studies (11), revealed that the two methods gave estimates of intake of dietary fiber, which strongly correlated with each other (correlation coefficient = 0.70) (10). A total of 49,613 dietary questionnaires was returned and available for analysis.
Calculation of fiber intake
Data from the completed self-administered food frequency questionnaires were used to estimate daily intake of energy and nutrients using a database for Canadian foods that has been described elsewhere (11). Data from the food frequency questionnaire were also used to estimate total dietary fiber intake by multiplying the frequency of consumption of each food by the nutrient content of the portion size and summing over all foods (10). Intake of fiber fractions were estimated from food intake values using the revised version of McCance and Widdowson’s food composition tables (12).
Ascertainment of incident ovarian cancer cases and deaths
Incident ovarian cancer cases and deaths amongst cohort members were ascertained respectively by means of computerized record linkages to the Canadian Cancer Database and to the National Mortality Database, both of which are maintained by Statistics Canada. The linkages to the databases yielded data on cancer incidence and mortality to December 31, 2000 for women in Ontario, December 31, 1998 for women in Quebec, and December 31, 1999 for women in other provinces.
Statistical Analysis
Of the 49,613 women for whom dietary data were available, we excluded women with extreme energy intake values (at least three standard deviations above or below the mean value for loge caloric intake) (n = 502); women with prevalent ovarian cancer at baseline (n = 20); and women who reported at baseline that they had had a bilateral oophorectomy (n = 315). These exclusions left 48,776 women available for analysis, amongst whom there were 264 incident cases of ovarian cancer. Study participants were considered to be at risk from their date of enrollment until the date of diagnosis of ovarian cancer, the date of termination of follow-up (the date to which cancer incidence data were available for women in the corresponding province), or the date of death, whichever occurred earliest.
Cox proportional hazards models (using age as the time scale) were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for the association between energy-adjusted quartile levels dietary fiber (total fiber, fiber fractions, and fiber from various sources) and ovarian cancer risk; energy adjustment was performed using the residual method (13). Multivariate models included the variables listed in the footnotes to Tables 2 and 3. To test for trend, we fitted the median value of each quartile as an ordinal variable in the risk models, and evaluated the statistical significance of the coefficient using the Wald test (14). We examined the associations overall and within strata defined by menopausal status. Stratified multivariate models included the variables listed in the footnotes to Tables 4 and 5. Tests for interaction were based on likelihood ratio tests comparing models with and without product terms representing the variables of interest. Use of the lifetest procedure in SAS™ showed that the proportional hazards assumption was met in this dataset. All analyses were performed using SAS version 9 (SAS Institute Cary, NC).
Results
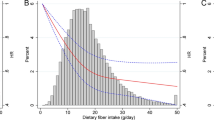
The average duration of follow-up for cohort members was 16.4 years, corresponding to a total of 801,414 person-years of follow-up for the cohort. The mean (S.D.) age at diagnosis for the cases was 59.4 (±7.2) years. For the cohort as a whole, the mean (±SD) energy-adjusted total dietary fiber intake was 20.1 g/day (±7.0). There was more than 2-fold variation in mean total dietary fiber intake values between the lowest and highest quartile levels (Table 1).
Compared to those with relatively low dietary fiber intake, women with high fiber intake were less likely to consume alcohol, to have ever smoked, and to have ever used oral contraceptives, but were more likely to participate in vigorous physical activity, to be postmenopausal at baseline, and to have a higher energy intake (Table 1). No appreciable variation was observed in mean age at baseline, body mass index, mean age at menarche, parity, or age at first birth by quartile levels of dietary fiber consumption.
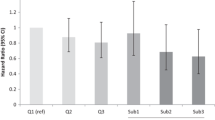
Tables 2 and 3 show that in age- and energy-adjusted models, ovarian cancer risk varied little in association with total dietary fiber intake, intake of specific fiber fractions, or by source of fiber intake. After multivariate adjustment, the hazard ratios remained essentially unchanged, although there was some suggestion of a weak inverse association with insoluble fiber intake (HR for the highest versus the lowest quartile level = 0.72, 95% confidence interval [CI] = 0.47–1.10, P trend = 0.09). For all fiber fractions and for fruit and vegetable fiber, the point estimates at the highest quartile level were all less than unity, but none of them was statistically significant. Mutual adjustment of the fiber fractions for each other and of the sources of dietary fiber for each other did not materially alter the hazard ratios (data not shown).
Relatively high total dietary fiber intake was associated with statistically non-significant reductions in risk of ovarian cancer in both premenopausal and postmenopausal women (Table 4). The risk for the highest compared to the lowest quartile level appeared to be somewhat lower among premenopausal (HR = 0.61, 95% CI = 0.33–1.12, P trend = 0.14) than postmenopausal women (HR = 0.86, 95% CI = 0.50–1.48, P trend = 0.95), and on formal testing, the interaction between dietary fiber and menopausal status was statistically significant (χ 2(3) = 8.31, P = 0.04). Similarly, ovarian cancer risk associated with fruit fiber intake was lower among premenopausal (HR = 0.63, 95% CI = 0.35–1.14, P trend = 0.10) than postmenopausal women (HR = 0.82, 95% CI = 0.48–1.40, P trend = 0.93), and the interaction between fruit fiber intake and menopausal status was statistically significant (χ 2(3) = 11.25, P = 0.01) (Table 5). There was no evidence of effect modification of the relationships between the other fiber fractions or sources of dietary fiber and ovarian cancer risk by menopausal status (Tables 4 and 5).
The results for each of the analyses presented above were similar after exclusion of case subjects diagnosed within 1 year of recruitment (n = 10).
Discussion
In the prospective study reported here, we found no association between total dietary fiber intake, intake of fiber fractions, or intake of fiber from various sources, and ovarian cancer risk over a 16-year follow-up period in the total study population.
The findings from our cohort for total dietary fiber intake differ from those of the majority of previous case–control studies (15–21), eight of which showed statistically significant inverse associations between dietary fiber and ovarian cancer risk (15–22). However, they are in keeping with those of the only prior prospective cohort study, which involved 139 cases (6). In addition, although fiber intake was not examined, both the European Prospective Investigation into Cancer (EPIC) (23) and a pooled analysis of 12 cohort studies (24) found no association between fruit and vegetable consumption and ovarian cancer risk. The association between fiber fractions and ovarian cancer risk has been examined previously in one case–control study (18), which, in contrast with our null results, showed inverse associations with intake of soluble and insoluble fiber, vegetable fiber, and cellulose.
High circulating levels of endogenous estrogens have been associated with ovarian cancer etiology (25, 26) and there is evidence that older age at menopause is associated with an increased risk of ovarian cancer due to greater exposure to endogenous estrogen (27). There is also evidence that dietary fiber may reduce endogenous sex hormone levels (28, 29), specifically serum estrone and estradiol levels in premenopausal women, by increasing sex hormone binding globulin (SHBG) leading to lower circulating levels of unbound or biologically available estrogen (2, 3, 27, 30). This may explain, in part, the interaction between dietary fiber and menopausal status observed here. However, additional studies are needed to confirm our findings.
Our data are limited by the possibility of error with respect to the measurement of diet and the calculation of total dietary fiber intake. Error in the measurement of daily intake of fiber may have resulted from inaccurate recall (31). However, this applies to the previous studies of dietary fiber and ovarian cancer as well. Our mean values for total fiber intake (20.1 g/day) are higher than the Canadian national average (10.8 g/day) for the same time period (32) This difference may be a consequence of a limitation of our food composition data. However, this limitation would have affected cases and non-cases similarly. Given the differences between national dietary fiber estimates and dietary fiber consumption in our study population, our findings may not be generalizable to all Canadian women. An additional limitation of our study is that information on menopausal status was collected only at baseline. However, given that the average age at menopause is 51 in North America (33) and that 88% of ovarian cancer cases in our study population were diagnosed at or above 51 years of age, it is evident that our results are largely representative of ovarian cancers diagnosed post-menopausally. Also, although we adjusted our estimates for a wide range of potentially confounding variables, uncontrolled confounding by dietary and other factors cannot be excluded. It is of note that the results of the two cohort studies to date differ from those of the majority of case–control studies. The discrepancy may reflect the greater susceptibility of case–control studies to selection and recall bias. Finally, the number of ovarian cancer cases may have been insufficient to allow detection of small effects.
In conclusion, the results of our study suggest that dietary fiber is not associated with risk of ovarian cancer.
References
Rock CL, Flatt SW, Thomson CA, Stefanick ML, Newman VA, Jones LA, Natarajan L, Ritenbaugh C, Hollenbach KA, Pierce JP, Chang RJ (2004) Effects of a high-fiber, low-fat diet intervention on serum concentrations of reproductive steroid hormones in women with a history of breast cancer. J Clin Oncol 22:2379–2387
Rose DP, Goldman M, Connolly JM, Strong LE (1991) High-fiber diet reduces serum estrogen concentrations in premenpausal women. Am J Clin Nutr 54:520–525
Rose DP, Lubin M, Connolly JM (1997) Effects of diet supplementation with wheat bran on serum estrogen levels in the follicular and luteal phases of the menstrual cycle. Nutrition 13:535–539
Syed V, Zhang X, Lau KM, Cheng R, Mukherjee K, Ho SM (2005) Profiling estrogen-regulated gene expression in changes in normal and malignant human ovarian surface epithelial cells. Oncogene, 1–6
Cunat S, Hoffmann P, Pujol P (2003) Estrogens and epithelial ovarian cancer. Gynecol Oncol 94:25–32
Kushi LH, Mink PJ, Folsom AR, Anderson KE, Zheng W, Lazovich D, Sellers TA (1999) Prospective study of diet and ovarian cancer. Am J Epidemiol 149:21–31
Terry PD, Miller AB, Jones JG, Rohan TE (2003) Cigarette smoking and the risk of invasive epithelial ovarian cancer in a prospective cohort study. Eur J Cancer 39:1157–1164
Miller AB, Baines CJ, To T, Wall C (1992) Canadian national breast screening study. I. Breast cancer detection and death rates among women aged 40–49 years. Ii. Breast cancer detection and death rates among women aged 50–59 years. Can Med Assoc J 147:1459–1488
Rohan TE, Hartwick W, Miller AB, Kandel RA (1998) Immunohistochemical detection of c-erbb-2 and p-53 in benign breast disease and breast cancer risk. J Natl Cancer Inst 90:1262–1269
Jain M, Harrison L, Howe GR, Miller AB (1982) Evaluation of a self-administered dietary questionnaire for use in a cohort study. Am J Clin Nutr 36:931–935
Morgan AB, Jain M, Miller AB, Choi NW, Matthews V, Munan L, Burch JD, Feather J, Howe GR, Kelly A (1978) A comparison of dietary methods in epidemiologic studies. Am J Epidemiol 107:488–198
Paul AA, Southgate DAT (1978) Mccance and widdowson’s the composition of foods. London, Her Majesty’s Stationary Office
Willett WC, Stampfer MJ (1986) Total energy intake: Implications for epidemiologic analyses. Am J Epidemiol 124:17–27
Rothman KJ, Greenland S (1998) Modern epidemiology. Philadelphia (PA): Lippincott-Raven
Byers T, Marshall J, Graham S, Mettlin C, Swanson M (1983) A case–control study of dietary and nondietary factors in ovarian cancer. J Natl Cancer Inst 71:681–686
McCann SE, Freudenheim JL, Marshall J, Graham S (2003) Risk of human ovarian cancer is related to dietary intake of selected nutrients, phytochemicals and food groups. J Nutr 133:1937–1942
McCann SE, Moysich KB, Mettlin C (2001) Intakes of selected nutrients and food groups and risk of ovarian cancer. Nutr Cancer 39:19–28
Pelucchi C, La Vecchia C, Chatenoud L, Negri E, Conti E, Montella M, Calza S, Dal Maso L, Franceschi S (2001) Dietary fibres and ovarian cancer risk. Eur J Cancer 37:2235–2239
Tzonou A, Day NE, Trichopoulos D, Walker ASM, Papapostolou M, Polychronopoulou A (1984) The epidemiology of ovarian cancer in greece: a case–control study. Eur J Cancer Clin Oncol 20:1045–1052
Tzonou A, Hsieh CC, Polychronopoulou A, Kaprinis G, Toupadaki N, Trichopoulou A, Karakatsani A, Trichopoulos D (1993) Diet ad ovarian cancer: a case–control study in greece. Int J Cancer 55:411–414
Zhang M, Lee AH, Binns CW (2003) Reproductive and dietary risk factors for epithelial ovarian cancer in china. Gynecol Oncol 92:320–326
Pan SY, Ugnat AM, Mao Y, Wen SW, Johnson KC, The Canadian Cancer Registries Epidemiology Research Group (2004) A case–control study of diet and the risk of ovarian cancer. Cancer Epidemiol Biomarkers Prev 13:1521–1527
Schulz M, Lahmann PH, Boeing H, Hoffmann K, Allen N, Key TJ, Bingham S, Wirfält E, Berglund G, Lundin E, Hallmans G, Lukanova A, Martínez Garcia C, González CA, Tormo MJ, Quirós JR, Ardanaz E, Larrañaga N, Lund E, Gram IT, Skeie G, Peeters PH, van Gils CH, Bueno-de-Mesquita HB, Büchner FL, Pasanisi P, Galasso R, Palli D, Tumino R, Vineis P, Trichopoulou A, Kalapothaki V, Trichopoulos D, Chang-Claude J, Linseisen J, Boutron-Ruault MC, Touillaud M, Clavel-Chapelon F, Olsen A, Tjønneland A, Overvad K, Tetsche M, Jenab M, Norat T, Kaaks R, Riboli E (2005) Fruit and vegetable consumption and risk of epithelial ovarian cancer: the european prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 14:2531–2535
Koushik A, Hunter DJ, Spiegelman D, Anderson KE, Arslan AA, Beeson WL, van den Brandt PA, Buring JE, Cerhan JR, Colditz GA, Fraser GE, Freudenheim JL, Genkinger JM, Goldbohm RA, Hankinson SE, Koenig KL, Larsson SC, Leitzmann M, McCullough ML, Miller AB, Patel A, Rohan TE, Schatzkin A, Smit E, Willett WC, Wolk A, Zhang SM, Smith-Warner SA (2005) Fruits and vegetables and ovarian cancer risk in a pooled analysis of 12 cohort studies. Cancer Epidemiol Biomarkers Prev 14:2160–2167
Riman T, Nilsson S, Persson IR (2004) Review of epidemiological evidence for reproductive and hormonal factors in relation to the risk of epithelial ovarian malignancies. Acta Obstet Gynecol Scand 83:783–795
Seeger H, Mueck AO (2006) The effects of estradiol metabolites and progestogens on the proliferation of human ovarian cancer cells. Panminerva Medica 48:13–17
Bagga D, Ashley JM, Geffrey SP, Wang HJ, Barnard RJ, Korenman S, Heber D (1995) Effects of a very low fat, high fiber diet on serum hormones and menstrual function. Implications for breast cancer prevention. Cancer 76:2491–2496
Prentice RL (2000) Future possibilities in the prevention of breast cancer: fat and fiber and breast cancer research. Breast Cancer Res 2:267–276
Slavin JL (2000) Mechanisms for the impact of whole grain foods on cancer risk. J Am Coll Nutr 19:300S–307S
Goldin BR, Woods MN, Spiegelman D, Longcope C, Morrill-LaBrode A, Dwyer JT, Gualitieri LJ, Hertzmark E, Gorbach SL (1994) The effect of dietary fat and fiber on serum estrogen concentrations in premenopausal women under controlled dietary conditions. Cancer 74:1125–1131
Willett WC, Stampfer MJ (1998) Nutritional epidemiology. New York (NY), Oxford University Press
Statistics Canada. Food statistics. Statistics Canada 5, (2005)
National Institute on Aging (2005) U.S. Department of Health and Human Services and National Institutes of Health. Menopause. AgePage 2005
Acknowledgments
Funded in part by the National Cancer Institute of Canada.
We thank Statistics Canada, the provincial and territorial Registrars of Vital Statistics, and the Cancer Registry directors for their assistance in making the cancer incidence and mortality data available.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silvera, S.A.N., Jain, M., Howe, G.R. et al. Dietary fiber intake and ovarian cancer risk: a prospective cohort study. Cancer Causes Control 18, 335–341 (2007). https://doi.org/10.1007/s10552-006-0107-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-006-0107-6