Abstract
Objective
To test the hypothesis that bone mineral density (BMD), a possible surrogate of lifetime exposure to hormone/growth factor/vitamin D/calcium exposure, is higher in prostate cancer cases than controls.
Methods
Hip BMD was measured by dual X-ray absorptiometry in 222 Afro-Caribbean screening-detected prostate cancer cases and 1,503 screened non-cases, aged 45–79, in the population-based Tobago Prostate Survey. Because possible skeletal metastases may modulate BMD, men with prostate specific antigen >20 ng/ml or highly undifferentiated tumors (Gleason score ≥8) were excluded. Mean BMD, adjusted for age and body mass index, was compared in cases and non-cases by analysis of variance. Risk across age group-specific BMD quartiles was compared using logistic regression.
Results
Overall, adjusted mean hip BMD was higher in cases (1.157 g/cm2) than non-cases (1.134 g/cm2) (p = 0.02). In men aged 60–79, prostate cancer risk was two-fold higher (OR, 2.12; 95% CI: 1.21–3.71) in the highest BMD quartile compared to the lowest. There was no association in younger men (interaction, p = 0.055).
Conclusions
High bone density is associated with prostate cancer among older men, consistent with an etiological role for lifetime exposure to factors which modulate bone density. However, other etiologies may dominate prostate cancer risk among younger men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High prostate cancer incidence or prevalence has been reported in populations of African descent in the US [1], and on the Caribbean islands of Jamaica [2] and Tobago [3], compared with Caucasian populations. Androgen metabolism has been suspected as a contributor to the elevated risk of prostate cancer in populations of African descent compared with Caucasians, but data directly supporting this hypothesis are sparse. Higher serum androgen levels have been observed in some [4, 5], but not all [6] studies of African Americans compared with whites. A number of studies of an androgen receptor CAG repeat polymorphism have documented a higher frequency of shorter CAG repeats in populations of African descent compared with Caucasians and other ethnic groups [7–10]. Studies have shown that a shorter CAG repeat tract is associated with higher androgen receptor activity in cell lines [11, 12] and in mouse models [13].
Circulating levels of insulin-like growth factor I (IGF1) have also been associated with prostate cancer risk in prospective [14, 15] and case–control [16] studies of predominantly Caucasian populations though results have not been consistent [17]. Significantly higher serum IGF-1 levels have been observed in Afro-Caribbean men, compared with similar aged Pakistani and European men [18]. Nevertheless, circulating levels of androgens and growth factors may not accurately reflect intra-prostatic concentrations and metabolism and thereby characterize a man’s lifetime exposure to these mitogenic factors.
Bone mineral density (BMD) has been proposed as a surrogate measure of lifetime growth factor and endogenous sex hormone exposure [19, 20]. Bone contains functional receptors for IGF-1 [21] and sex steroid hormones [22] and is sensitive to IGFs and androgens [22, 23]. Moreover, BMD is considerably greater in men of African compared to Caucasian ancestry, and this skeletal difference has been attributed in part to ethnic differences in growth factor and sex steroid hormone production and/or sensitivity [24].
BMD has been positively associated with breast cancer risk [19] and prostate cancer risk in Caucasian populations [25], but these associations have not been examined in populations of African descent. Thus, we conducted the current study in a high risk Afro-Caribbean population residing on the island of Tobago. Age-specific screening-detected prostate cancer prevalence rates in the Tobago population are 3–4 times higher [3] than observed in a similarly screened US Caucasian population [26]. We tested the hypothesis that BMD, as a surrogate marker of lifetime sex hormone/growth factor exposure, would be higher in Afro-Caribbean men with screening-detected prostate cancer compared to men without prostate cancer: those with normal screening results (serum prostate specific antigen (PSA) <4 ng/ml and a normal digital rectal exam) and no biopsy, and those with abnormal screening results and one or more biopsies which were negative for prostate cancer.
Methods
Population
The Tobago Prostate Survey is a population-based, longitudinal prostate cancer screening study which has been conducted on the Caribbean island of Tobago, Trinidad and Tobago, since late 1997. More than 60% of the male population, aged 40–79, has participated. The study was approved by the Institutional Review Board of the University of Pittsburgh, and the Institutional Review Board of the Division of Health and Social Services, Tobago House of Assembly. Written informed consent was obtained from each participant. The methods have been described in detail [3]. Briefly, men with abnormal screening results, serum PSA ≥4 ng/ml, or abnormal digital rectal exam other than simple enlargement, were referred for sextant biopsy by surgeons at the local regional hospital. Thirty-one percent of screened men were referred for biopsy. Ninety percent of men referred for biopsy underwent biopsy. PSA assays (Abbot AxSYM PSA assay, Abbott Laboratories, Abbott Park, IL, USA) and biopsy pathology were completed at the University of Pittsburgh Pathology Laboratory.
Bone mineral density
Bone mineral density measurements were begun in March 2000. Men enrolled prior to that time were contacted to return for a bone density measurement. Men enrolled after that time were scheduled for a bone density measurement around the time of their first visit. Total hip BMD was measured using a Hologic QDR 4500W densitometer (Hologic Inc., Bedford, MA). Densitometry staff were trained and certified by Hologic. Densitometry quality assurance and quality control were completed by SYNARC, Inc. (Maynard, MA). Longitudinal machine stability was assessed from plots of daily spine phantom scans, and reviewed monthly. A weekly printout of quality control plots was generated to detect short-term inconsistencies and long-term drift. Quality control scans were reviewed to ensure that the BMD and bone mineral content of the scanner were within normal limits. The coefficient of variation for BMD was 0.44%. Scan analysis quality was ensured by central review of scans. In addition, scans that appeared unusual or difficult to analyze were flagged for review by SYNARC, Inc.
Data analysis
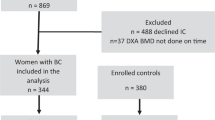
All men diagnosed with prostate cancer at baseline (prevalent cases) or at a second visit approximately two years after baseline (incident cases) were designated cases and were compared with screened men not diagnosed with prostate cancer (non-cases). No cases were observed in men younger than 45. Therefore, analyses were limited to men aged 45–79 with bone scan data (298 cases and 1,531 non-cases). Men of non-African ancestry were excluded from analyses (five cases, 10 non-cases). Bone metastases may modulate hip BMD. Since scintigraphy, the standard method for diagnosis of bone metastases, was not available on the island of Tobago, we excluded men most likely to be affected by skeletal metastases: those with highly undifferentiated tumors (Gleason scores 8, 9, 10) and/or high serum PSA values (PSA > 20 ng/ml). Excluded were 11 cases with Gleason ≥ 8 and PSA > 20 ng/ml; 16 cases with Gleason ≥ 8 and PSA ≤ 20 ng/ml; 42 cases with Gleason < 8 and PSA > 20 ng/ml; 16 non-cases with PSA > 20 ng/ml. Men undergoing orchiectomy or medical androgen ablation prior to densitometry (n = 2) were also excluded from the analyses. Remaining for analysis were 222 cases and 1,503 non-cases. Anthropometric measurements and total hip BMD were compared between cases and non-cases using analysis of variance (ANOVA). Models were constructed to compare BMD by prostate cancer status, adjusted for age (continuous), for age and body mass index (BMI, weight in kilograms/height in meters squared), and for age, BMI, and the interaction between age and BMD by prostate cancer status. Further ANOVA models were constructed in younger (age 45–59) and older (60–79) age groups. Quartiles were assigned based on the distribution of hip BMD in the study population aged 45–59, or aged 60–79. Prostate cancer risk associated with quartiles of hip BMD was calculated by logistic regression adjusted for age (continuous) and BMI among younger and older men. Similar logistic regression models were constructed to estimate the prostate cancer risk associated with hip BMD as a continuous variable. All statistical tests were two-sided and were considered statistically significant if p < 0.05.
Results
Bone density and related covariates were analyzed in 222 cases (179 prevalent and 43 incident cases) and 1,503 non-cases. The Gleason scores 5, 6 and 7 were observed in 2, 151, and 69 men, respectively.
Among prostate cancer cases, bone density was measured prior to diagnosis (mean 0.9 years, SD 0.7, median 0.7, range 0.1–2.38 years) in 92 men. Bone density was measured after diagnosis (mean 0.8 years, s.d. 0.6, median 0.6, range 0–2.7 years) in 130 men.
Mean age in cases was 63.6 years compared with 56.8 years in non-cases (Table 1). Age-adjusted BMI was highly correlated with total fat mass (r = 0.84) and lean mass (r = 0.70) in both cases and non-cases (r = 0.84, r = 0.75, respectively, all p < 0.001). Age-adjusted BMI in cases was slightly higher than in non-cases, 27.6 kg/m2 (95% CI 27.1–28.2) compared with 27.0 kg/m2 (95% CI 26.8–27.2), p = 0.055. Age and BMI-adjusted hip BMD was higher in cases, 1.157 g/cm2 (95% CI 1.138–1.175) than controls, 1.134 g/cm2 (95% CI 1.127–1.141) (p = 0.02) (Table 1). However, there was an interaction between age and case status for hip BMD as shown in Fig. 1.
Adjusted hip BMD did not differ between 70 younger (aged 45–59) cases and 961 non-cases, 1.329 g/cm2 vs. 1.335 g/cm2, respectively, p = 0.76. In contrast, adjusted hip BMD was 0.26 standard deviation (SD) units higher in 152 cases than in 542 non-cases in the 60–79 year age group, 1.145 g/cm2 (95% CI 1.122–1.163) vs. 1.106 g/cm2 (1.094–1.118), p = 0.003 (p = 0.055 for age interaction).
After adjustment for age and BMI in logistic regression, prostate cancer risk, in men aged 60–79, increased across quartiles of BMD (test for trend, p = 0.004) (Table 2). Prostate cancer risk was about two-fold higher (OR: 2.12; 95% CI: 1.21–3.71) in the highest quartile compared with the lowest quartile quartile of hip BMD. In adjusted continuous analyses, prostate cancer risk increased 34% for each standard deviation unit of hip BMD (Table 2). Prostate cancer risk was not associated with BMD in men aged 45–59 (Table 2).
Discussion
We conducted a population-based study of the relationship between BMD, a lifetime marker of steroid hormone, growth factor, vitamin D and calcium exposure, and the risk of prostate cancer in apparently healthy men of African descent on the Caribbean island of Tobago. Screening-detected prevalence of prostate cancer was very high in this population, particularly among older men (22% of screened men aged 60–79) [3]. Total hip BMD was approximately one standard deviation higher across age groups 40–79 than observed in African American men, and more than one standard deviation greater than observed in Caucasian American men in the National Health and Nutrition Survey (NHANES) III [27, 28]. Factors contributing to the high BMD in this population remain to be elucidated, but the high BMD is consistent with the hypothesis of high exposure to endogenous sex steroid hormone and growth factors in the population. Among men without prostate cancer, we observed the anticipated pattern of decline in hip BMD across age groups as observed in other cross-sectional studies [27]. In contrast, BMD did not decline across age groups among the men with prostate cancer until age 70–79. The risk of prostate cancer increased with increasing BMD among older men, aged 60–79. Prostate cancer risk was two-fold higher in those in the highest quartile of BMD compared to those in the lowest quartile, independent of age and BMI.
Our results are consistent with cohort analyses among Caucasian men in the Framingham Study [25], which involved 100 cases primarily diagnosed at an older age. Incidence of prostate cancer was higher in the two upper age-specific quartiles of metacarpal cortical areas measured at mean age 61 years, with median age at prostate cancer diagnosis, 75.2 years. The relative risk for highest quartile compared with lowest was 1.6 (95% CI 0.9–3.0, p-value for trend across quartiles, 0.06). In contrast, the prospective NHANES I Epidemiologic Followup Study [29] found a nonsignificant trend toward lower prostate cancer incidence (n = 94) in the three higher BMD quartiles of radiographic estimated bone density measured at mean age 49 years in 1974–1975 and followed through 1992 for diagnosis of prostate cancer. The age, BMI and ethnicity adjusted odds ratio for highest compared with lowest quartile was 0.72 (95% CI 0.38–1.38, p-value for trend across quartiles, 0.37). Age at prostate cancer diagnosis was not reported. The potential for younger age at diagnosis of cases in the latter study, the inclusion of about 12% African Americans, and the use of BMD quartiles calculated across all age groups may have contributed to the difference between these two prospective studies.
A prospective study in older (aged 65+ years at baseline) Caucasian women [19] found a positive association between breast cancer risk and hip BMD which was of similar magnitude to the association between prostate cancer risk and hip BMD in older men observed in the current study.
The pattern of higher BMD observed in older men with prostate cancer may reflect greater peak BMD, as would result from higher steroid hormone/growth factor production early in life, or a slower decline in BMD in cases with age, as would result from maintenance of higher steroid hormone/growth factor levels into old age, or a combination of these patterns.
Endogenous levels of hormones, growth factors, or cytokines may provide a link between BMD and prostate cancer risk among older men. Androgens and estrogens are important determinants of bone density in men [30], with estrogens thought to play a relatively more important role in older men [31]. Although strong data from animal studies implicate both androgens and estrogens in the etiology of prostate cancer [32], few prospective studies or nested case–control studies have demonstrated that higher levels of serum androgens or estrogens are associated with an increased risk of prostate cancer among older men [33]. Serum levels of insulin have been associated with prostate cancer [34], and are also positively associated with BMD in men [35]. Insulin stimulates prostate cell proliferation in vitro [36]. Insulin-like growth factors are also important determinants of BMD [23], and serum levels have been associated with increased prostate cancer risk in several studies [14–16]. Finally, increased production of proinflammatory cytokines has been noted among individuals with low BMD [37]. In vitro data suggest that the proinflammatory cytokines, interleukin 1β and tumor necrosis factor-α, may have growth-inhibitory effects on prostate cancer cells [38–40]. Thus, the relationship between BMD and prostate cancer risk may involve a complex interplay of hormones, growth factors, and cytokines, and this relationship may differ by age.
An association between BMD and prostate cancer risk could be confounded by body size and adiposity. Obesity is a major determinant of BMD [41] and potential risk factor for prostate cancer [42]. In our study, men who developed prostate cancer had somewhat higher BMI than did men who did not develop prostate cancer. However, the association between BMD and prostate cancer remained after adjustment for BMI.
Our study had several strengths. It was the largest population-based study of BMD and of prostate cancer in men of African descent. Recruitment and prostate cancer screening in this prospective study were exactly the same for non-cases and prostate cancer cases reducing the likelihood of bias and misclassification. Standard, state-of-the-art BMD measurements were performed. An important limitation was our cross-sectional design. The relationship between BMD and prostate cancer is best studied in a prospective design because of the possible confounding effects of the disease on BMD, e.g., treatment, metastases, poor health. Restriction of our analyses to screening-detected cases with moderately differentiated tumors minimized the influence of ill health and metastases on BMD, but precluded study of the association of BMD to cancers which had advanced. The relatively small number of younger men with prostate cancer was a further limitation.
This is the first report to describe the relationship between BMD and the risk of prostate cancer in a population of African descent. Our results support a link between lifetime steroid hormone/growth factor exposure and the high prostate cancer risk that is characteristic of men of African descent. The lack of association of BMD with prostate cancer among the younger men suggested that other mechanisms may play a more prominent role in the etiology of early onset prostate cancer among men of African descent.
Abbreviations
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- IGFI:
-
Insulin-like growth factor I
- OR:
-
Odds ratio
- PSA:
-
Prostate specific antigen
- ANOVA:
-
Analysis of variance
- NHANES:
-
National Health and Nutrition Examination Survey
- SD:
-
Standard deviation
- CI:
-
Confidence interval
References
Ries LAG, Eisner MP, Kosary CL, et al (eds) (2005) SEER Cancer Statistics Review, 1975–2002, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2002/, based on November 2004 SEER data submission, posted to the SEER web site 2005, Table XXII-2
Glover Jr FE, Coffey DS, Douglas LL, et al (1998) The epidemiology of prostate cancer in Jamaica. J Urol 159:1984–1987
CH Bunker AL Patrick BR Konety et al. (2002) ArticleTitleHigh prevalence of Screening-detected prostate cancer among Afro-Caribbeans: the Tobago Prostate Survey Cancer Epidemiol Biomark Prev 11 726–729
R Ross L Bernstein H Judd R Hanisch M Pike B Henderson (1986) ArticleTitleSerum testosterone levels in healthy young black and white men J Natl Cancer Inst 76 45–48 Occurrence Handle3455741 Occurrence Handle1:CAS:528:DyaL28Xmt1eqsQ%3D%3D
AH Wu AS Whittemore LN Kolonel et al. (1995) ArticleTitleSerum androgens and sex hormone-binding globulins in relation to lifestyle factors in older African-American, white, and Asian men in the United States and Canada Cancer Epidemiol Biomark Prev 4 735–741 Occurrence Handle1:CAS:528:DyaK2MXpslWnt74%3D
EA Platz EB Rimm WC Willett PW Kantoff E Giovannucci (2000) ArticleTitleRacial variation in prostate cancer incidence in hormonal system markers among male health professionals J Natl Cancer Inst 92 2009–2017 Occurrence Handle11121463 Occurrence Handle1:STN:280:DC%2BD3M3ls1ymtg%3D%3D Occurrence Handle10.1093/jnci/92.24.2009
VR Panz BI Joffe I Spitz T Lindenberg A Farkas M Haffejee (2001) ArticleTitleTandem CAG repeats of the androgen receptor gene and prostate cancer risk in black and white men Endocrine 15 213–216 Occurrence Handle11720249 Occurrence Handle1:CAS:528:DC%2BD3MXotVSrtbg%3D Occurrence Handle10.1385/ENDO:15:2:213
O Sartor Q Zheng JA Eastham (1999) ArticleTitleAndrogen receptor gene CAG repeat length varies in a race-specific fashion in men without prostate cancer Urology 53 378–380 Occurrence Handle9933058 Occurrence Handle1:STN:280:DyaK1M7ivFygug%3D%3D Occurrence Handle10.1016/S0090-4295(98)00481-6
RA Kittles D Young S Weinrich et al. (2001) ArticleTitleExtent of linkage disequilibrium between the androgen receptor gene CAG and GCC repeats in human populations: implications for prostate cancer risk Hum Genet 109 253–261 Occurrence Handle11702204 Occurrence Handle1:CAS:528:DC%2BD3MXptVKqtrg%3D Occurrence Handle10.1007/s004390100576
CL Bennett DK Price S Kim et al. (2002) ArticleTitleRacial variation in CAG repeat lengths within the androgen receptor gene among prostate cancer patients of lower socioeconomic status J Clin Oncol 20 3599–3604 Occurrence Handle12202660 Occurrence Handle1:CAS:528:DC%2BD38XntVynsr0%3D Occurrence Handle10.1200/JCO.2002.11.085
NL Chamberlain ED Driver RL Miesfeld (1994) ArticleTitleThe length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function Nucl Acids Res 22 3181–3186 Occurrence Handle8065934 Occurrence Handle1:CAS:528:DyaK2cXlvFOns7o%3D
Q Wang TS Udayakumar TS Vasaitis AM Brodie JD Fondell (2004) ArticleTitleMechanistic relationship between androgen receptor polyglutamine tract truncation and androgen-dependent transcriptional hyperactivity in prostate cancer cells J Biol Chem 279 17319–17328 Occurrence Handle14966121 Occurrence Handle1:CAS:528:DC%2BD2cXjt1GnsLw%3D Occurrence Handle10.1074/jbc.M400970200
MA Albertelli A Scheller M Brogley DM Robins (2006) ArticleTitleReplacing the mouse androgen receptor with human alleles demonstrates glutamine tract length dependent effects on physiology and tumorigenesis in mice Mol Endocrinol 20 1248–1260 Occurrence Handle16601069 Occurrence Handle1:CAS:528:DC%2BD28XltlSrsLo%3D Occurrence Handle10.1210/me.2006-0021
JM Chan MJ Stampfer E Giovanucci et al. (1998) ArticleTitlePlasma insulin-like growth factor-I and prostate cancer risk: a prospective study Science 279 563–566 Occurrence Handle9438850 Occurrence Handle1:CAS:528:DyaK1cXotVOqsg%3D%3D Occurrence Handle10.1126/science.279.5350.563
P Stattin A Bylund S Rinaldi et al. (2000) ArticleTitlePlasma insulin-like growth factor-I, insulin-like growth factor-binding proteins, and prostate cancer risk: a prospective study J Nat Cancer Inst 92 1910–1917 Occurrence Handle11106682 Occurrence Handle1:CAS:528:DC%2BD3cXptVehu7k%3D Occurrence Handle10.1093/jnci/92.23.1910
A Wolk CS Mantzoros S-O Andersson et al. (1998) ArticleTitleInsulin-like growth factor 1 and prostate cancer risk: a population-based, case–control study J Nat Cancer Inst 90 911–915 Occurrence Handle9637140 Occurrence Handle1:CAS:528:DyaK1cXktFOqsLc%3D Occurrence Handle10.1093/jnci/90.12.911
R Shi HJ Berkel H Yu (2001) ArticleTitleInsulin-like growth factor-I and prostate cancer: a meta-analysis Br J Cancer 85 991–996 Occurrence Handle11592771 Occurrence Handle1:CAS:528:DC%2BD3MXot1Sktb8%3D Occurrence Handle10.1038/sj.bjc.6691961
JK Cruickshank AH Heald S Anderson et al. (2001) ArticleTitleEpidemiology of the insulin-like growth factor system in three ethnic groups Am J Epidemiol 54 504–513 Occurrence Handle10.1093/aje/154.6.504
JA Cauley FL Lucas LH Kuller MT Vogt WS Browner SR Cummings (1996) ArticleTitleBone mineral density and risk of breast cancer in older women: the study of osteoporotic fractures. Study of Osteoporotic Fractures Research Group JAMA 276 1404–1408 Occurrence Handle8892715 Occurrence Handle1:STN:280:ByiD2cjoslA%3D Occurrence Handle10.1001/jama.276.17.1404
Zmuda JM, Cauley JA, Ljung BM, Bauer DC, Cummings SR, Kuller LH. Study of Osteoporotic Fractures Research Group (2001) Bone mass and breast cancer risk in older women: differences by stage at diagnosis. J Nat Cancer Inst 93:930–936
CA Conover (2000) Insulin-like growth factors and the skeleton E Canalis (Eds) Skeletal growth factors Lippincott Williams & Wilkins Philadelphia USA 101–116
KM Wiren ES Orwoll (1999) Androgens and bone: basic aspects ES Orwoll (Eds) Osteoporosis in men: the effects of gender on skeletal health Academic Press San Diego, USA 211–245
CJ Rosen (2000) ArticleTitleIGF-I and osteoporosis Clin Lab Med 20 591–602 Occurrence Handle10986623 Occurrence Handle1:STN:280:DC%2BD3M%2FmsVSksA%3D%3D
AM Parfitt (1997) ArticleTitleGenetic effects on bone mass and turnover-relevance to black/white differences J Am Coll Nutr 16 325–333 Occurrence Handle9263181 Occurrence Handle1:STN:280:ByiH3cfms1Y%3D
Y Zhang DP Kiel RC Ellison et al. (2002) ArticleTitleBone mass and the risk of prostate cancer: The Framingham Study Am J Med 113 734–739 Occurrence Handle12517363 Occurrence Handle10.1016/S0002-9343(02)01382-7
JP Richie WJ Catalona FR Ahmann et al. (1993) ArticleTitleEffect of patient age on early detection of prostate cancer with serum prostate-specific antigen and digital rectal examination Urology 42 365–374 Occurrence Handle7692657 Occurrence Handle1:STN:280:ByuD38rktlY%3D Occurrence Handle10.1016/0090-4295(93)90359-I
AC Looker HW Wahner WL Dunn et al. (1998) ArticleTitleUpdated data on proximal femur bone mineral levels of US adults Osteopor Internat 8 468–489 Occurrence Handle1:STN:280:DyaK1M%2FmslensA%3D%3D Occurrence Handle10.1007/s001980050093
J Cauley JM Zmuda A Patrick VW Wheeler D Hill C Bunker (2001) ArticleTitleTobago Bone Health Study: Epidemiologic Study of high bone mineral density on a population level J Bone Min Res 16 IssueIDSuppl 1 M357
Nelson RL, Turyk M, Kim J, Persky V (2002) Bone mineral density and the subsequent risk of cancer in the NHANES I follow-up cohort. BMC Cancer 2:22 (accessed 12 March 2004 at http://www.biomedcentral.com/1471-2407/2/22)
RL Wolf JM Zmuda KL Stone JA Cauley (2000) ArticleTitleUpdate on the epidemiology of osteoporosis Curr Rheumatol Rep 2 74–86 Occurrence Handle11123043 Occurrence Handle1:STN:280:DC%2BD3M7ktVWqsg%3D%3D
GA Greendale S Edelstein E Barrett-Connor (1997) ArticleTitleEndogenous sex steroids and bone mineral density in older women and men: The Rancho Bernardo Study J Bone Miner Res 12 1833–1843 Occurrence Handle9383688 Occurrence Handle1:CAS:528:DyaK2sXns1yjs78%3D Occurrence Handle10.1359/jbmr.1997.12.11.1833
MC Bosland (2000) ArticleTitleThe role of steroid hormones in prostate carcinogenesis J Natl Cancer Inst Monogr 27 39–66 Occurrence Handle10963619 Occurrence Handle1:CAS:528:DC%2BD3cXlvVSnt7g%3D
AW Hsing JKV Reichardt FZ Stanczyk (2002) ArticleTitleHormones and prostate cancer: current perspective and future directions Prostate 52 213–235 Occurrence Handle12111697 Occurrence Handle1:CAS:528:DC%2BD38XmsVWqtbk%3D Occurrence Handle10.1002/pros.10108
AW Hsing C Streamson Y-T Gao E Gentzchien L Chang FZ Stanczyk (2001) ArticleTitleSerum levels of insulin and leptin in relation to prostate cancer risk: a population-based case–control study in China J Natl Cancer Inst 93 783–789 Occurrence Handle11353789 Occurrence Handle1:CAS:528:DC%2BD3MXkt1OktLs%3D Occurrence Handle10.1093/jnci/93.10.783
RP Stolk PL Daele ParticleVan HA Pols et al. (1996) ArticleTitleHyperinsulinemia and bone mineral density in an elderly population: The Rotterdam Study.[erratum appears in Bone. 1996; 19: 566] Bone 18 545–549 Occurrence Handle8805995 Occurrence Handle1:STN:280:BymA1Mblt1A%3D Occurrence Handle10.1016/8756-3282(96)00079-8
DM Peehl TA Stamey (1986) ArticleTitleSerum-free growth of adult human prostatic epithelial cells In Vitro Cell Dev Biol 22 82–90 Occurrence Handle2419302 Occurrence Handle1:STN:280:BimC3sbmvVE%3D
JA Cauley JM Zmuda AB Newman et al. (2003) ArticleTitleCirculating levels of soluble cytokine receptors predict incident fractures in older men and women: The Health Aging and Body Composition Study (HABC) J Bone Miner Res 18 IssueIDSuppl 2 S84
M Kawada M Ishizuka T Takeuchi (1999) ArticleTitleEnhancement of antiproliferative effects of interleukin-1beta and tumor necrosis factor-alpha on human prostate cancer LNCaP cells by coculture with normal fibroblasts through secreted interleukin-6 Jpn J Cancer Res 90 546–554 Occurrence Handle10391095 Occurrence Handle1:CAS:528:DyaK1MXjsVOmu7g%3D
Y Nakajima A DelliPizzi C Mallouh N Ferreri (1995) ArticleTitleEffect of tumor necrosis factor-alpha and interferon-gamma on the growth of human prostate cancer cell lines Urol Res 23 205–210 Occurrence Handle8533204 Occurrence Handle1:STN:280:BymD1M%2FotV0%3D Occurrence Handle10.1007/BF00393299
OW Rokhlin AV Gudkov S Kwek RA Glover AS Gewies MB Cohen (2000) ArticleTitlep53 is involved in tumor necrosis factor-alpha-induced apoptosis in the human prostatic carcinoma cell line LNCaP Oncogene 19 1959–1968 Occurrence Handle10773886 Occurrence Handle1:CAS:528:DC%2BD3cXjtV2qu7g%3D Occurrence Handle10.1038/sj.onc.1203453
ES Orwoll L Bevan KR Phipps (2000) ArticleTitleDeterminants of bone mineral density in older men Osteopor Internat 11 815–821 Occurrence Handle1:STN:280:DC%2BD3M7isV2nsA%3D%3D Occurrence Handle10.1007/s001980070039
AM Nomura (2001) ArticleTitleBody size and prostate cancer Epidemiol Rev 23 126–131 Occurrence Handle11588836 Occurrence Handle1:STN:280:DC%2BD3Mrkt1Sltg%3D%3D
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was supported, in part, by funding or in-kind services from the Division of Health and Social Services, Tobago House of Assembly, the University of Pittsburgh Cancer Institute, the Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh, contract DAMD 17-99-109015, U.S. Department of Defense, and grants R01 CA84950, R25-CA57703, U.S. National Cancer Institute, R01-AR049747, U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Rights and permissions
About this article
Cite this article
Bunker, C.H., Zmuda, J.M., Patrick, A.L. et al. High bone density is associated with prostate cancer in older Afro-Caribbean men: Tobago Prostate Survey. Cancer Causes Control 17, 1083–1089 (2006). https://doi.org/10.1007/s10552-006-0047-1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-006-0047-1