Abstract
A 14-year update to a previously published historical cohort study of aluminum reduction plant workers was conducted [1]. All men with three or more years at an aluminum reduction plant in British Columbia (BC), Canada between the years 1954 and 1997 were included; a total of 6,423 workers. A total of 662 men were diagnosed with cancer, representing a 400% increase from the original study. Standardized mortality and incidence ratios were used to compare the cancer mortality and incidence of the cohort to that of the BC population. Poisson regression was used to examine risk by cumulative exposure to coal tar pitch volatiles (CTPV) measured as benzene soluble materials (BSM) and benzo(a)pyrene (BaP). The risk for bladder cancer was related to cumulative exposure to CTPV measured as BSM and BaP (p trends <0.001), and the risk for stomach cancer was related to exposure measured by BaP (p trend BaP <0.05). The risks for lung cancer (p trend <0.001), non-Hodgkin lymphoma (p trend <0.001), and kidney cancer (p trend <0.01) also increased with increasing exposure, although the overall rates were similar to that of the general population. Analysis of the joint effect of smoking and CTPV exposure on cancer showed the observed dose–response relationships to be independent of smoking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
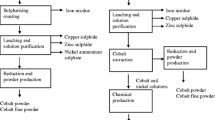
Aluminum is produced from bauxite by an electrolytic process that results in the generation of coal tar pitch volatiles containing polycyclic aromatic hydrocarbons [2, 3]. Epidemiologic studies have previously shown elevated risks of bladder [4–6] and lung cancer [7–9] and raised questions about increased risk of other cancers [4–11] in primary aluminum smelting workers.
We previously completed a study on mortality from cancer and other diseases and cancer incidence over a 30-year period among a cohort of workers in the ALCAN vertical stud Söderberg aluminum reduction facility in Kitimat, British Columbia (BC), Canada [1]. The study included all male workers who worked at least 5 years between 1954 and 1985. Information on health outcome was obtained from linkages with BC provincial mortality and cancer registries. Exposure to coal tar pitch volatiles (CTPV) was assessed and smoking data were obtained to examine for potential confounding. A total of 60,590 person-years, 338 deaths and 158 men diagnosed with cancer were observed. Significantly elevated rates were observed for bladder cancer incidence and brain cancer mortality. The risk of bladder cancer was related to cumulative exposure to CTPV. The risk for non-Hodgkin lymphoma also increased with increasing exposure to CTPV, although the overall rate was similar to that of the general population. A similar pattern was observed for kidney cancer but the findings for this site and also for non-Hodgkin lymphoma were based on small numbers of cases. The lung cancer rate was similar to that of the general population of BC, but showed an association with CTPV exposure that was of borderline statistical significance. The CTPV dose–response relationships for lung and bladder cancer remained essentially the same after adjusting for smoking.
We recently completed a 14-year extended follow-up of the same aluminum reduction facility with an expanded cohort, national cancer incidence and mortality follow-up and improved exposure assessment methods. The focus of this study was on exposure to coal tar pitch volatiles using two markers of exposure: benzene soluble materials (BSM) and benzo(a)pyrene (BaP).
Methods
As in the original study, a retrospective cohort approach was used. All male workers with three or more years of work experience at the Kitimat plant or at the power generating station in Kemano, BC, since operation began in 1954–1997, were included. Thus, all members of the original cohort (worked at least 5 years between 1954 and 1985) were also included in this study. It was possible to reduce the eligibility criterion from five working years in the original study to three working years in this study because of the better follow-up with linkages using national databases.
Determination of vital status, cancer and smoking information
The cohort members’ work histories up to 31 December 1997, including job title, department, starting date, and stopping date for each job assignment, were obtained from company records and supplemented with information from the original study. In the original study, the occupational histories had been obtained for the period from 1954 to 1985. This information was used in conjunction with computerized records available since 1989 and with data on paper records to obtain all members’ work history.
Vital status follow-up for each cohort member started after three years of employment was attained and ended on 31 December 1999. The cohort was linked with the Canadian Vital Statistics Death Database to identify those who died during the follow-up period between 1957 and 1999 and to ascertain their cause of death. Information from the tax files was incorporated in the linkage to help determine the vital status. The cohort was also linked with the population-based Canadian Cancer Registry to identify workers who were diagnosed with cancer and to ascertain their diagnoses.
The Canadian Cancer Registry is a combined source of information on cancer diagnoses since 1970 from all the provincial cancer registries. Cancer incidence follow-up for each cohort member started after three years of employment was attained or in 1970 whichever was later, and continued until 31 December 1999. The Death Database and Cancer Registry are administered by Statistics Canada where the linkages are performed using the state-of-the-art probabilistic record linkage methodology [12].
The vital status of the cohort members not found through linkage was determined as follows. First, the cohort was linked with the BC Client Registry to determine their last known dates residing in BC. The Client Registry, administered by the BC Ministry of Health, keeps all records of health care recipients on the provincial medical system since 1984. This information was then combined with the members’ known locations at the last contact obtained in the original study, including union and pension records, to determine whether they should be censored at last date known to be alive. Workers were censored at their last contact dates if (i) they did not link to the BC client registry and their locations at last contact were “working at Kitimat” or “not in Canada” or (ii) they had been censored in the original study prior to 1985 and did not link to the Client Registry. Workers who were not censored and did not die during the follow-up period (1957–1999) were assumed to be alive at the end of the study period of 31 December 1999.
Smoking information was obtained through a self-administered questionnaire approach. Workers with contact information (current workers and pensioners) were sent a questionnaire to request information on their smoking habit. The results were supplemented with information collected in the original study. In that study, smoking information for current employees was also obtained through a mailed questionnaire. For cohort members not employed at that time, attempts were made to contact each person to ascertain smoking information. For those who could not be contacted, smoking information was obtained from next of kin, from another employee who knew the person well, or from the company health records.
Exposure assessment
Exposure to coal tar pitch volatiles was estimated using two different measures of exposure: benzene soluble material (BSM) and benzo(a)pyrene (BaP). In the original study, a BSM job exposure matrix (JEM) was developed by a committee that included company industrial hygienists and union health and safety representatives [1]. In this current study, a new BSM JEM was developed by enhancing the original JEM using existing exposure personal measurements through a sophisticated statistical modeling approach [13]. In addition, a BaP JEM was also developed since it has been suggested that BaP is a more specific marker of the carcinogenic potential of the potroom fumes [14–16].
The quantitative BSM and BaP JEMs were developed independently of each other using the same methodological approach to maximize the use of the exposure measurements and is described in more detail elsewhere [13]. While a large number of personal BSM and BaP measurements had been collected by the company and the Workers’ Compensation Board of BC from the mid-1970s onwards, exposure measurements were not available for all exposed jobs. Thus, different exposure assessment approaches were used for different levels of exposure information.
Statistical models were developed to derive annual arithmetic means for each potroom operations and maintenance job for 1977–2000. Variables included in the models were year, job, potroom group, season, and time period. Time periods were determined using dates of major technological changes. Within each time period of similar technology, the annual mean exposure was averaged to obtain the exposure estimate for that time period. For non-potroom locations, mean exposures were directly calculated. Exposure estimates for jobs without exposure measurements were extrapolated from exposure estimates from the statistical models after adjusting for the amount of time in exposed areas. Estimating pre-1977 exposure levels involved backwards extrapolation of 1977 exposure levels.
Categorical exposure estimates were assigned for jobs that had not been included in the statistical models (non-potroom locations, jobs with no measurements). Seven BSM exposure categories were used, including 0 (no exposed), 0.01–0.1, 0.1–0.2, 0.2–0.4, 0.4–1, 1–2, and >2 mg/m3. This scale was developed based on the four categories in the original BSM JEM (None, 0.01–0.2, 0.2–1, >1 mg/m3) for finer discrimination of exposure levels. For BaP, the exposure categories were determined from observing the range of predicted exposures over time from the BaP statistical exposure models, resulting in seven categories: 0, 0.05–0.5, 0.5–1, 1–3, 3–7, 7–14, and >14 μg/m3. For calculating cumulative exposure, the midpoints of the exposure categories were used. The highest exposure categories were assigned a value of 2.5 mg/m3 for BSM exposure and 18 μg/m3 for BaP exposure, respectively.
Analysis
Standardized mortality ratio (SMR) and standardized incidence ratio (SIR) analyses were used to compare, respectively, the cancer mortality and incidence of the cohort with the BC population [17, 18]. All cancer diagnoses and mortality were classified using version 9 of the International Classification of Diseases coding system (ICD-9). The follow-up period for the mortality analysis was from 1957, the first year in which any cohort members attained the minimum employment of three years, to the end of 1999. BC mortality rates calculated by 5-year age groups and 5-year calendar periods for each cause of death for the years 1955–1999, were provided by Statistics Canada. The follow-up period for the cancer incidence analysis was from 1970, the first year for which complete tumor registry records were available, to the end of 1999. Cancer incidence rates were calculated using data from the population-based BC Cancer Registry by the same 5-year age and calendar periods for the years 1970–1999. Person years were calculated from the point at which cohort members attain 3 years of employment until the end of follow-up, death, cancer diagnosis (for the incidence analysis), or date last known to be alive. That is, when a specific cancer incidence site was examined, information on other cancer diagnoses was not used in censoring. Ninety-five percent confidence intervals for the SMRs and SIRs were calculated by comparison with the Poisson distribution. SMR and SIR analyses were performed using the Life table Analysis System (PCLTAS) developed by the US National Institute for Occupational Safety and Health (NIOSH) [19, 20].
Dose–response relationships were examined based on the cumulative CTPV exposure. For each job-year combination, the exposure level was obtained via the JEM described above where the exposure level was measured using the benzene soluble material index (BSM) and benzo[a]pyrene index (BaP). At any given time, the cumulative exposure level for each worker was estimated by aggregating exposure estimates of all job-year combinations from the date of starting employment to that time. The analyses were performed for cancer sites with at least 10 cases.
The cutpoints for the exposure categories were chosen based on the current threshold limit value (TLV) for BSM (0.2 mg/m3) [21]. The second cutpoint (Low/Low-Medium) is based on a 10-year exposure at the TLV. Cutpoints for the higher categories are based on a doubling of exposure. The lowest cutpoint identifies individuals with less than 10 years exposure at the midpoint lowest exposure category (<0.1 mg/m3). The cutpoints for BaP are based on the approximate relationship between BSM and BaP in the plant. Insufficient person-years to ensure at least one expected case for all cancer sites examined were observed in the highest BaP category (>160 BaP-years), so this category was combined with the previous one. The following exposure categories for BSM were used in the analyses:
The following exposure categories for BSM were used in the analyses:
-
No exposure—Less than 0.05 BSM-Year (mg/m3 year)
-
Low—0.05 to 2.0 BSM-Years
-
Low-Medium—2.0 to 4.0 BSM-Years
-
Medium—4.0 to 8.0 BSM-Years
-
Medium-High—8.0 to 16.0 BSM-Years
-
High—More than 16.0 BSM-Years.
The exposure categories for BaP used in the analyses included:
-
No exposure—Less than 0.5 BaP-Year (μg/m3 year)
-
Low—0.5 to 20 BaP-Years
-
Low-Medium—20 to 40 BaP-Years
-
Medium—40 to 80 BaP-Years
-
High—More than 80 BaP-Years.
Dose–responses analyses were performed using Poisson regression with relevant parameters estimated using maximum likelihood methods [15, 16]. The internal analyses directly compared the exposed groups to an unexposed group within the cohort, adjusting for calendar period and age as potential confounding factors. These analyses were performed with and without the smoking covariate to see if the health effects of occupational exposure were influenced by smoking (defined as never, ever or unknown). Specifically a worker was classified as ever smoker if that was indicated in either study. Smoking status specific analyses were also performed with a test for interaction to examine whether the trends differed between smokers and non-smokers.
Five-year calendar period and age categories were used. These categories were combined when necessary (small number of cases) to improve precision. The analyses were performed for selected cancer sites that indicated elevated risks in the above analyses, as well as those identified in the original study for both BSM and BaP indices. Tests for trend were computed by entering a single covariate with value computed as the midpoint of the cumulative dose category. For the largest category, the approximate mean cumulative exposure within the category was used—20 for BSM and 200 for BAP.
The principal analyses were performed using a 3-year lag time. Latency effects were examined by repeating the dose–response analyses using different lags including 10 and 20 years. The fits of the models using different lags were compared by the magnitude of the trend statistic.
The analyses of smoking as an effect modifier examined the interaction between smoking and the exposure trend in the Poisson regression model. All Poisson regression analyses were done using the R statistical software package [22].
Results
This cohort study included a total of 6,423 males contributing 151,057 person-years at risk, of which 1,079 died during the mortality follow-up period between 1957 and 1999. This represents a 250% increase in person-years and 300% increase in deaths from the original study. Confirmed causes of death were available for over 98%. Most, 86.4%, were successfully traced with 872 individuals lost to follow-up. The majority of the men lost to follow-up worked in the early years—576 out of 872 (66%) ceased working before 1970.
During the cancer incidence follow-up period between 1970 and 1999, 662 male members were diagnosed with cancer. This represents a 400% increase in the number of individuals with cancer from the original study. Confirmed diagnoses were available for about 98%.
Mortality
The mortality results are given in Table 1. The mortality rate for all causes was significantly lower than that of the BC population (SMR = 0.87; 95% CI: 0.82–0.92), whereas the mortality rate for all cancers was very close to that of the BC population (SMR = 0.97; 95% CI: 0.87–1.08). Non-significant excess mortality risks were observed for oropharynx cancer (SMR = 2.38; 95% CI: 0.29–8.60), pleural cancer (SMR = 1.98; 95% CI: 0.24–7.14), brain cancer (SMR = 1.54; 95% CI: 0.93–2.40), stomach cancer (SMR = 1.4; 95% CI: 0.90–2.09) and for bladder cancer (SMR = 1.39; 95% CI: 0.72–2.43). The mortality rates for lung cancer (SMR = 1.07; 95% CI: 0.89–1.28) and non-Hodgkin lymphoma (SMR = 1.1; 95% CI: 0.60–1.85) were slightly higher than those of the BC population but the excess was not significant. The mortality rate for kidney cancer was lower than expected (SMR = 0.74; 95% CI: 0.30–1.52), but not significant.
Incidence
The incidence results are given in Table 2. The cancer rate for all causes was the same as that from the BC male population (SIR = 1.00; 95% CI: 0.92–1.08). Significantly increased cancer risks were seen for stomach cancer (SIR = 1.46; 95% CI: 1.01–2.04) and bladder cancer (SIR = 1.80; 95% CI: 1.45–2.21). Greater than 50% but non-significant increased risks were observed for lip cancer (SIR = 1.58; 95% CI: 0.72–2.99), cancer of the nasopharynx (SIR = 1.80; 95% CI: 0.58–4.20), pleural cancer (SIR = 2.22; 95% CI: 0.89–4.58), male breast cancer (SIR = 2.11; 95% CI: 0.44–6.17), and brain cancer (SIR = 1.48; 95% CI: 0.91–2.29). The lung cancer rate was slightly higher (SIR = 1.10; 95% CI: 0.93–1.30) and the rate for non-Hodgkin lymphoma was slightly lower (SIR = 0.93; 95% CI: 0.61–1.35) than expected. The kidney cancer rate was the same as that from the male BC population (SIR = 1.00; 95% CI: 0.62–1.52).
Dose–response
BSM
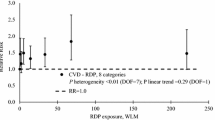
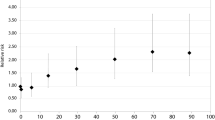
Poisson regression results for selected cancer incidence using the BSM index are presented in Table 3. Some evidence of a dose–response association was observed for stomach cancer. Excess risks were seen for the top three exposure categories. The risks did not increase monotonically, but a marginally significant trend was observed (p = 0.051). A dose–response was observed for lung cancer with a statistically significant trend (p < 0.001). A doubling of risk was seen in the two highest exposure categories (RR = 2.01; 95% CI: 1.14–3.57 for 8–16 and RR = 2.07; 95% CI: 1.16–3.68 for 16+). For bladder cancer, a dose–response association was seen (p = 0.001). The highest risk was observed in the penultimate exposure category (RR = 2.04; 95% CI: 1.03–4.03); with a slightly lower excess risk in the highest category (RR = 1.66; 95% CI: 0.80–3.42). For kidney cancer, a greater than sixfold increased risk was seen for the high exposure category (RR = 6.09; 95% CI = 1.16–31.93), with a significant dose–response association (p = 0.009). For brain cancer, no association with exposure was observed. A dose–response association was seen for non-Hodgkin lymphoma (p < .001). Over a sevenfold increased risk was seen for the two highest exposure categories (RR = 7.70; 95% CI: 1.62–36.60; RR = 7.10; 95% CI: 1.40–36.00) exposure categories.
BaP
Poisson regression results for selected cancer incidence using the BaP index are presented in Table 4. For all cancer sites, except for bladder cancer, the dose–response association observed for BaP was similar to that observed for BSM. For bladder cancer, a stronger dose–response association was observed for BaP than for BSM (p < 0.001). A nearly doubling of risk was seen in the highest exposure category (RR = 1.92; 95% CI: 1.02–3.65).
The dose–response relationships with BaP as the exposure index were stronger and more consistently monotonic (increasing risk with increasing exposure) than with BSM as the exposure index. However, the cumulative BaP and BSM exposures were highly correlated (r = 0.94), and the resulting conclusions did not differ by the use of one index over the other. For the smoking adjustment and latency analyses, only results using the BaP index are presented.
Smoking adjustment
Among the 6,423 male workers in the cohort, 3,682 workers (57%) were smokers; 1,218 workers were never smokers (19%); and no smoking information was available for 1,523 workers (23%). Smokers had a higher mean cumulative BaP exposure than non-smokers (30.9 μg/m3 year vs. 20.9 μg/m3 year, p < 0.001).
For kidney cancer, brain cancer and non-Hodgkin lymphoma, there was little or no change in the observed dose–response association or estimated relative risks when smoking was added to the Poisson regression models for either BSM or BaP. For stomach cancer and lung cancer, there was a weakening of the dose–response associations with an approximately 10% reduction in the relative risk observed in the highest exposure categories. For bladder cancer, there was a slight wstrengthening of the dose–response associations with an approximately 10% increase in the relative risk observed in the highest exposure category. Results for lung, bladder and stomach cancer, adjusted for smoking are given in Table 5.
There was no evidence of an interaction between smoking and exposure dose–response (p = 0.11 for lung cancer, p > 0.5 for all other sites). For lung cancer, there was a slightly lower dose–response among smokers. All cancer sites had very small number of observed and expected cases in the non-smoking stratum, so the risk estimates for the individual cumulative exposure categories were unstable.
Latency
Dose–response relationships by both BSM and BaP indices were examined for lags 3, 10 and 20 years for all sites examined in the Poisson regression analysis. For all sites, the dose–response relationships seemed to be stable for different lag times with either BSM or BaP index. The 20-year lag time provided the best linear dose–response fit for stomach, lung, and bladder. For kidney cancer and non-Hodgkin lymphoma all latencies gave similar fits; a 3-year lag time giving the best fit for kidney cancer and a 10-year lag time for non-Hodgkin lymphoma. Table 6 gives the results for the best fitting lag time for stomach cancer, lung cancer, bladder cancer and non-Hodgkin lymphoma.
Discussion
In comparison with the original study, small increases were observed for both overall mortality and cancer ratios [1]. The difference was probably due to the better follow-up with linkages to national databases. The overall cancer incidence and mortality rates for the cohort were essentially the same as that for the general population. However, a number of dose–response relationships were observed.
A increased overall risk of bladder cancer was observed in comparison with the general population, with a dose–response relationship with exposure to CTPV. This finding was consistent with the original study, which was based on only 16 cases of bladder cancer [1]. Theriault and colleagues [4, 5] also found an increased risk of bladder cancer in aluminum workers in Quebec. Others have observed a dose–response relationship with CTPV [14, 23]. Two smaller cohort studies of aluminum workers in Norway [24] and in France [25] have also found an excess risk of bladder cancer for workers exposed to PAHs.
A significant dose–response relationship between CTPV exposure and lung cancer was observed. The original study of this cohort found a similar dose–response relationship but non-significant, likely due to the smaller number of cases (37) [1]. This current result was consistent with the findings from cohort studies of aluminum workers in Quebec, Canada [8, 9, 15] and in Sweden [26]. These studies have observed significantly increased lung cancer mortality risks with evidence of dose–response relationships. However, two other smaller cohort studies of aluminum workers in Norway [24] and France [25] found no excess risk of lung cancer with increasing exposure to PAHs.
A new finding in this study was the significantly elevated incidence rate of stomach cancer, with evidence of a dose–response relationship with exposure to CTPV. No association was observed in the original study based on only seven cases [1]. Although it is believed that occupational exposures do not play a major role in the gastric cancer, cohort studies of workers with potential PAH exposure have indicated an increased risk of stomach cancer, including metal-products industries [27] and coke oven workers [28]. A nested case–control study in China found a fivefold excess risk for coke oven workers with >15 year work duration, after adjusting for important confounders such as family history and diet factors [29]. The Quebec cohort study also found a significantly increased risk of stomach cancer [9]. Exposure to asbestos has also been suspected to link to stomach cancer development due to an observed increase in asbestos workers and exposure to asbestos may have occurred at this facility (see pleural cancer below) [30].
No overall excess risk of non-Hodgkin lymphoma was observed, but those with high exposure to BSM (8+ BSM-Years) or BaP (80+ BaP-Years) have a much higher rate than expected. There was also evidence of a dose–response relationship due to a reduced risk in non- or low-exposed categories. This finding was consistent with the original study based on only seven cases [1]. Another cohort study of aluminum workers in Washington State also found an elevated mortality for those exposed to CTPV [11]. A recent study of men living near a coke oven plant in Italy found a 2.4 times significantly increased risk of non-Hodgkin lymphoma, suggesting a link between non-Hodgkin lymphoma with exposure to PAHs [31].
No significant excess risk for kidney cancer was observed although there was evidence of a dose–response relationship with exposure to CTPV. The same pattern was seen in the original study although it was not significant perhaps due to the small number of cases (7) [1]. Although exposure to PAHs is a suspected risk factor for kidney cancer, evidence in the literature is inconclusive [32]. Two small case–control studies have suggested a weak association [33, 34] but other studies have not found an excess risk [35]
An overall non-significant excess risk of pleural cancer was seen for male workers in this study. With all seven cases being mesothelioma, the excess risk was probably due to exposure to asbestos in early years. This finding may have implications for the interpretation of the results for lung cancer and, potentially, some other cancers that may be related to asbestos exposure. A recent NIOSH study found small excess of stomach, esophageal, and colorectal cancer among industries with excesses of pleural cancer [36].
Non-significantly increased risks of brain cancer incidence and mortality were observed, but with little evidence of a dose–response relationship. This finding was consistent with the original study based on only eight cases [1].
Coal tar pitch volatiles measured as benzene soluble materials comprise a mixture of particulate contaminants, including polycyclic aromatic hydrocarbons (PAHs). One particulate PAH, benzo(a)pyrene (BaP) has been suggested to be a more specific marker of the carcinogenic potential of the potroom fumes than the broad mixture of benzene soluble materials [12–14]. We found that BaP was highly correlated with most particulate PAHs (Pearson r correlation range: 0.76–0.99). However, each pitch type had a different profile of particulate PAHs and thus the correlation between BaP and other PAHs improved when we accounted for pitch type. While benzo(b)fluoranthene has been suggested as a more stable indicator of PAH environmental exposure [37], it was very highly correlated with BaP (r = 0.97) within this smelter. The high correlation between the particulate PAHs and BaP suggests that benzo(a)pyrene is an appropriate indicator for the PAH mixture.
The study had a number of limitations. Besides smoking, which was only identified as ever or never for many workers, information on other potential risk factors, including lifestyle, genetic, and occupational exposure prior to or after employment at the Kitimat plant, was not available and could not be adjusted for in the risk estimation. As in other studies, there was always the possibility that some excess risks could have occurred by chance as a result of multiple comparisons. This was especially relevant for sub-categories or causes with small numbers of cases. Exposure measurement data were not available for the first 20 years that the smelter was open and exposure estimates for this period were extrapolated from exposure levels in the late-1970s, which may underestimate the true exposure levels. This and other limitations to the assessment of exposure could result in an underestimation of the risks associated with exposure or distort the shape of the dose–response relationship.
However, the current update study had several important strengths, particularly in comparison with the original study. It had a much longer follow-up period and an expanded cohort, resulting in substantial increases (three to fourfold) in number of cases and, hence, in power and the ability to explore dose–response relationships. It had better follow-up with linkages to the national databases, resulting in a smaller number of workers being censored. Lastly, the exposure assessment was based on sophisticated modeling of measurement data combined with expert opinions, resulting in more precise cumulative exposure estimates.
References
Spinelli J, Band PR, Svirchev LM, Gallagher RP (1991) Mortality and cancer incidence in aluminum reduction workers. J Occup Med 33:1150–1155
International Agency for Research on Cancer (1984) Polynuclear aromatic compounds, Part 3: Industrial exposures in aluminum production, coal gasification, coke production, and iron and steel founding. Monographs vol. 34. International Agency for Research on Cancer, Lyon
Benke G, Abramson M, Sim M (1998) Exposures in the alumina and primary aluminum industry: an historical review. Ann Occup Hyg 43(3):173–189
Theriault G, DeGuire L, Cordier S (1981) Reducing aluminum: an occupation possibly associated with bladder cancer. Can Med Assoc J 124:419–425
Theriault G, Tremblay C, Cordier S, et al (1984) Bladder cancer in the aluminum industry. Lancet I:947–950
Ronneberg A, Andersen A (1995) Mortality and cancer morbidity in workers from an aluminium smelter with prebaked carbon anodes—Part II: Cancer morbidity. Occup Environ Med 52(4):250–254
Anderson A, Dahlber BE, Magnus K, et al (1982) Risk of cancer in the Norwegian aluminum industry. Int J Cancer 29:295–298
Gibbs GW, Horowitz I (1985) Lung cancer mortality in aluminum reduction plant workers. J Occup Med 21:347–353
Gibbs GW (1985) Mortality of aluminum reduction plant workers, 1950 through 1997. J Occup Med 27:761–770
Rockette HE, Arena VC (1983) Mortality studies of aluminum reduction plant workers; potroom and carbon department. J Occup Med 25:549–557
Milham S (1979) Mortality in aluminum reduction workers. J Occup Med 21:475–480
Howe GR, Lindsay J (1981) A generalized record linkage computer system for use in medical follow-up studies. Comput Biomed Res 14:327–340
Friesen MC, Demers PA, Spinelli JJ, et al From expert-based to quantitative retrospective exposure assessment at a Soderberg aluminum smelter, Ann Occup Hyg. Available at http://annhyg.oxfordjournals.org/papbyrecent.dtl
Armstrong B, Tremblay C, Baris D, Theriault G (1994) Lung cancer mortality and polynuclear aromatic hydrocarbons: a case–cohort study of aluminum production workers in Arvida, Quebec, Canada. Am J Epidemiol 139(3):250–262
Armstrong BG, Tremblay CG, Cyr D, Theriault GP (1986) Estimating the relationship between exposure to tar volatiles and the incidence of bladder cancer in aluminum smelter workers. Scand J Work Environ Health 12(5):486–493
Farant JP, Gariépy M (1998) Relationship between benzo[a]pyrene and individual polycyclic aromatic hydrocarbons in a Söderberg primary aluminum smelter. Am Indust Hyg Assoc J 59:758–765
Breslow NE, Day NE (1987) Statistical methods in cancer research: volume II-the design and analysis of cohort studies. IARC, Lyon, France
Rothman KJ, Greenland S (1998) Modern epidemiology. Lippincott Williams & Wilkins
NIOSH (2000) Life Table Analysis System for the PC. US Department of Health and Human Services, Cincinnati, OH
Steenland K, Spaeth S, Cassinelli R II, Laber P, Chang L, Koch K (1998) NIOSH life table program for personal computers. Am J Ind Med 34(5):517–518
American Conference of Governmental Industrial Hygienists (ACGIH) (2005) TLVs and BEIs. ACGIH, Cincinnati
R: The R Foundation for Statistical Computing Version 2.0.0 (2004-10-04), ISBN 3-900051-07-0. 2004
Tremblay C, Armstrong B, Theriault G, Brodeur J (1995) Estimation of risk of developing bladder cancer among workers exposed to coal tar pitch volatiles in the primary aluminum industry. Am J Indust Med 27(3):335–348
Romundstad P, Haldorsen T, Andersen A (2000) Cancer incidence and cause specific mortality among workers in two Norwegian aluminum reduction plants. Am J Indust Med 37:175–183
Moulin JJ, Clavel T, Buclez B, Laffitte-Rigaud G (2000) A mortality study among workers in a French aluminum reduction plant. Int Arch Occup Environ Health 73:323–330
Selden AI, Westberg HB, Axelson O (1997) Cancer morbidity in workers at aluminum foundries and secondary aluminum smelters. Am J Indust Med 32:467–477
Wu-Williams MC, Yu MC, Mack TM (1990) Life-style, workplace, and stomach cancer by subsite in young men of Los Angeles County. Cancer Res 50:2569–2576
Bye T, Romundstad PR, Ronneberg A, Hilt B (1998) Health survey of former workers in a Norwegian coke plant: Part 2. Cancer Incidence and cause specific mortality. Occup Environ Med 55:622–626
Xu Z, Brown LM, Pan GW, et al (1996) Cancer risks among iron and steel workers in Anshan, China, Part II: case–control studies of lung and stomach cancer. Am J Indust Med 30:7–15
Selikoff IJ, Hammond EL, Churg J (1968) Asbestos exposure, smoking, and neoplasia. J Am Med Assoc 204:104–110
Parodi S, Vercelli M, Stella A, Stagnaro E, Valerio F (2003) Lymphohaematopoietic system cancer incidence in an urban area near a coke oven plant: an ecological investigation. Occup Environ Med 60:187–193
Boffeta P, Jourenkova N, Gustavsson P (1997) Cancer risk from occupational and environmental exposure to polycyclic aromatic hydrocarbons. Cancer Causes Control 8:444–472
Kadamani S, Agal NR, Nelson RY (1989) Occupational hydrocarbon exposure and risk of renal cell carcinoma. Am J Indust Med 15:131–141
Mellemgaard A, Engholm G, McLaughlin JK, et al (1994) Risk of renal cell carcinoma in Denmark. IV. Role of occupation. Scand J Work Environ Health 20:160–165
Partanen T, Heikkila P, Hernberg S, et al (1991) Renal cell cancer and occupational exposure to chemical agents. Scand J Work Environ Health 17:231–239
Kang SK, Burnett CA, Freund E, Walker J, Lalich N, Sestito J (1997) Gastrointestinal cancer mortality of workers in occupations with high asbestos exposures. Am J Ind Med 31(6):713–718
Aubin S, Farant JP (2000) Benzo[b]fluoranthene, a potential alternative to benzo[a]pyrene as an indicator of exposure to airborne PAHs in the vicinity of Soderberg aluminum smelters. J Air Waste Manage Assoc 50(12):2093–2101
Acknowledgments
We are indebted to former and current members of the Alcan-Canadian Auto Workers Advisory Committee and Mr. Richard Lapointe for their support while conducting this research. Help from staff at the Kitimat operation in the collection of exposure data (Mr. Barry Boudreault, Mr. Jim Thorne) and the work history (Mr. Siok Yeok) have substantially simplified the tasks. We would like to thank the research staff who participated in this study: Ms. Donna Kan, Ms. Barbara Jamieson, Ms. Dianne Oleniuk, Ms. Jade Vo, Ms. Heather Neidig, Ms. Nela Walter, Ms. Elena Papadakis, Ms. Zenaida Abanto and Ms. Sharon Tamaro. The WCB provided personal air samples collected in the 1975–2000 period that were used in exposure assessment. This research was supported by grants from the BC Workers’ Compensation Board (WCB) and Alcan Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spinelli, J.J., Demers, P.A., Le, N.D. et al. Cancer risk in aluminum reduction plant workers (Canada). Cancer Causes Control 17, 939–948 (2006). https://doi.org/10.1007/s10552-006-0031-9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-006-0031-9