Abstract
Treatment of circadian rhythm disorders, whether precipitated by intrinsic factors (e.g., sleep disorders, blindness, mental disorders, aging) or by extrinsic factors (e.g., shift work, jet-lag) has led to the development of a new type of agents called ‘chronobiotics’, among which melatonin is the prototype. The term ‘chronobiotic’ defines as a substance capable of shifting the phase of the circadian time system thus re-entraining circadian rhythms. Melatonin administration synchronizes the sleep–wake cycle in blind people and in individuals suffering from delayed sleep phase syndrome or jet lag, as well in shift-workers. The effect of melatonin on sleep is probably the consequence of increasing sleep propensity (by inducing a fall in body temperature) and of a synchronizing effect on the circadian clock (chronobiotic effect). We successfully employed the timely use of three factors (melatonin treatment, exposure to light, physical exercise) to hasten the resynchronization after transmeridian flights comprising 12–13 time zones, from an average of 8–10 days to about 2 days. Daily melatonin production decreases with age, and in several pathologies, attaining its lowest values in Alzheimer’s dementia patients. About 45% of dementia patients have severe disruptions in their sleep–wakefulness cycle. Both in aged subjects having very minimal sleep disorders as well as in demented patients with a very severe disorganization of the sleep–wake cycle, melatonin treatment reduced the variability of sleep onset and restored sleep.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The circadian clock is one of the most indispensable biological functions
Many biological functions wax and wane in cycles that repeat each day, month, or year. Such patterns do not reflect simply organism’s passive response to environmental changes. Rather, they reflect the organism’s biological rhythms, that is, its ability to keep track of time and to direct changes in function accordingly. Because the earth rotates on its axis, it presents two environments, i.e., light and darkness; because the earth’s axis of rotation is tilted, durations of daily periods of darkness and light vary during the course of the year. Through evolution, animals responded to these environmental changes by preferentially adapting to them. This is the origin of biological rhythms that repeat approximately every 24 h, called circadian rhythms (from the Latin circa, for around, and dies, for day), and of rhythms that oscillate annually, following the recursive appearance of the seasons. Thus, when animals switch between diurnal, nocturnal or seasonal modes of their behavior, they are not simply responding passively to changes in external lighting conditions. They are responding to signals generated by a circadian pacemaker which is written in their genes that is synchronized with the cycles of the earth’s rotation, anticipates the transitions between day and night, and triggers appropriate changes in behavioral state and physiological substrates [1, 2]. In this way, the circadian pacemaker creates a day and night within the organism that mirrors approximately the world outside.
During the past decade, enormous progress has been made in determining the molecular components of the biological clock. The molecular mechanisms that underlie the function of the clock are universally present in all cells and consist of gene–protein–gene feedback loops in which proteins can downregulate their own transcription and stimulate the transcription of other clock proteins. Although anchored genetically, circadian rhythms are synchronized by (entrained) and maintain certain phase relationships to exogenous factors, especially the sleep portion of the light–dark schedule. These rhythms will persist with a period different from 24 h when external time cues are suppressed or removed, such as during complete social isolation or in constant light or darkness [1–3].
Research in animals and humans has shown that only a few such environmental cues, like light–dark cycles, are effective entraining agents (‘Zeitgebers’) for the circadian oscillator. An entraining agent can actually reset, or phase shift, the internal clock. Depending on when an organism is exposed to such an entraining agent, circadian rhythms can be advanced, delayed, or not shifted at all. Therefore, involved in adjusting the daily activity pattern to the appropriate time of day is a rhythmic variation in the influence of the Zeitgeber as a resetting factor.
In mammals, a hierarchically major circadian oscillator is located in the suprachiasmatic nuclei (SCN) of the hypothalamus. This circadian master clock acts like a multifunctional timer to adjust the homeostatic system, including sleep and wakefulness, hormonal secretions and various other bodily functions, to the 24-h cycle. Lesions of the SCN eliminate all circadian-driven rhythms. Inversely, SCN transplants to animals whose own SCN had been ablated, can restore circadian activity rhythms. Every single SCN cell exerts a waxing and waning of the firing rate with a predictable circadian rhythm. Synchronized by paracrine signals the SCN produces an output signal that ‘drives’ endogenously generated daily oscillations in hormones, sleep – wakefulness, alertness, performance, and many other physiological functions. The sinusoidal output signal produced by the SCN can be described by its period (cycle length), phase (position in the cycle), and amplitude (range between highest and lowest signal). The output amplitude reflects the ‘strength’ or robustness of the circadian timing system, which can also be described as the drive to restore homeostasis in response to stimuli or the extent to which circadian behavior is separated into distinct periods of activity and rest within one cycle [1–3].
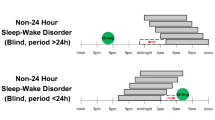
As mentioned, the SCN becomes synchronized to the environmental light–dark cycle by its primary Zeitgeber: light. The photic entrainment of the pacemaker is mediated by a specialized subset of intrinsically photosensitive ganglion cells that are spread throughout the retina rather than having a foveal concentration. Those specialized ganglion cells also receive input from rods and cones, acting as a redundant input pathway for synchronizing the circadian system, but can still function even if the rods and cones are so severely damaged that the individual is blind. Light input can still be obtained by the circadian system through these specialized ganglion cells that have a direct monosynaptic pathway to the SCN in the hypothalamus [1–3].
Circadian rhythm disorders are precipitated by intrinsic and extrinsic factors
Among the innumerable periodic changes that underlie and support the overt circadian physiologic rhythms, the peak values occur in a characteristic sequence over the day (‘phase map’) in human healthy subjects [4]. Such a sequence and spacing reflects the order and temporal relationships of cause–effect in the normal interactions of the various bodily processes and is the very indicative of organism’s health [5]. Disruption of amplitude or phase of circadian rhythms can be produced endogenously, like that seen in many psychiatric disorders, blindness, circadian sleep disorders or chronic diseases. On the other hand, phase maps may undergo transitory disruptions when humans are compelled to make a rapid phase adjustment as, for example, after a rapid move to a new geographic longitude or as a consequence of shift work [6, 7]. Under such circumstances, the various individual 24-h components comprising the circadian phase map do not reset their phases to the new environmental times at the same rate, and become somewhat displaced in their relations to one another. To reset them to the new local time requires several days of exposure to the local phase setters.
The structure of the major circadian rhythm, the sleep–wake cycle, is dependent on a complex interaction of circadian phase and sleep–wake dependent processes [8, 9]. When sleep is displaced, as is the case with transmeridian travelers and shift workers, the normal phase relationship between the sleep–wake cycle and the endogenous circadian oscillator is perturbed, a situation which can lead to substantial deterioration in sleep quality. In contrast, normal individuals living on a day-oriented schedule show a balanced relationship between homeostatic and circadian processes that serves to promote uninterrupted bouts of approximately 8 h of sleep and 16 h of wakefulness per day. Therefore, the temporal alignment between the sleep–wake cycle and the endogenous circadian system is a determining factor in the quality of the subsequent sleep and waking episodes.
As above mentioned, two interacting processes regulate the timing, duration and depth, or intensity, of sleep: a homeostatic process that maintains the duration and intensity of sleep within certain boundaries and a circadian rhythm that determines the timing of sleep. The homeostatic process depends on immediate history: the interval since the previous sleep episode and the intensity of sleep in that episode. This drive to enter sleep increases, possibly exponentially, with the time elapsed since previous sleep episode. It declines exponentially once sleep has been initiated. The homeostatic sleep drive controls slow wave sleep rather than rapid eye movement (REM) sleep. In contrast, the phase and amplitude of the circadian rhythm are independent of the history of previous sleep but are generated by the major pacemaker, the SCN. The circadian variation of human sleep propensity is roughly the inverse of the core body temperature rhythm: maximum propensity for sleep and the highest continuity of sleep occur in proximity to the minimum temperature [8, 9].
Adaptive drives including a variety of mechanisms that influence sleep but which are independent of the time spent awake and of circadian rhythms should be also considered in sleep regulation. Adaptive factors modify the sleep–wake cycle according to changes in the environment, which are significant for the individual. They include behavioral factors, like motivation, attention and other psychological responses to the environment (e.g., bed comfort, social activity), noise, environmental temperature, physical exercise and food intake. Sleep recording during e.g., ultrashort sleep–wake paradigms or free-running conditions indicated that the peak propensity for REM sleep is observed near the nadir of the core body temperature cycle, at the middle of a normal night. In comparison, the occurrence of slow wave sleep is much more influenced by the duration of prior waking than by circadian phase. However, a cross-influence occurs since REM sleep can also be influenced by sleep deprivation just as slow wave activity shows circadian modulation [8, 9].
Day sleep in shift workers is often measured as 1–3 h shorter than night sleep on days off, or on day and evening work schedules [10, 11]. Following night shifts, most workers report no difficulties falling asleep and latencies to sleep onset are short. The short sleep latencies are accompanied by short latencies to non-REM sleep, which may represent the response to a physiological sleep debt. Shift workers, who typically show great variation in their degrees of circadian entrainment to particular sleep–wake cycles, also demonstrate a discrepancy in the amount and distribution of REM sleep. Shift work has been associated with a number of health problems including cardiovascular disease, impaired glucose and lipid metabolism, gastrointestinal discomfort, reproductive difficulties, and breast cancer. Despite years of night work, only a minority of workers show an appropriate reorientation of physiological rhythms such as those of 6-sulphatoxymelatonin, plasma melatonin, cortisol, and TSH. This can be related to the observable troughs in vigilance and the fragility of sleep particular to night work [10, 11].
Chronobiotics are useful to hasten the resynchronization after transmeridian flights
Drugs that influence the circadian apparatus are referred as chronobiotics [12]. The prototype of this type of drugs is melatonin. Melatonin is produced in most organisms from algae to mammals, and its role varies considerably across the phylogenetic spectra [13]. In humans, it plays a major function in the coordination of circadian rhythmicity, remarkable the sleep–wake cycle [14, 15]. Melatonin secretion is an ‘arm’ of the biologic clock in the sense that it responds to signals from the SCN and in that the timing of the melatonin rhythm indicates the status of the clock, both in terms of phase (i.e., internal clock time relative to external clock time) and amplitude. From another point of view, melatonin is also a chemical code of night: the longer the night, the longer the duration of its secretion. In many species, this pattern of secretion serves as a time cue for seasonal rhythms [14].
Like the effects induced by the external Zeitgeber light, effects by the internal Zeitgeber melatonin are also time-dependent. The greatest density of high-affinity melatonin receptors in humans is located in the SCN. Entraining free-running circadian rhythms by administering melatonin is only possible if the SCN is intact. Daily timed administration of melatonin to rats shifts the phase of the circadian clock, and this phase shifting may partly explain melatonin effect on sleep in humans, or ‘chronobiotic effect’ [12]). Indirect support for such a physiological role derived from clinical studies on blind subjects showing free running of their circadian rhythms while a more direct support for this hypothesis was provided by the demonstration that the phase response curve for melatonin was opposite (i.e., 180° out of phase) to that of light [15, 16].
Within the SCN, melatonin reduces neuronal activity in a time-dependent manner. In rodents, the effects of melatonin on SCN activity are mediated by at least two different receptors. They are insensitive during the day, but sensitive at dusk and dawn (MT2; causes phase shifts) and during early night period (MT1; decreases neuronal firing rate) [17]. Melatonin secreted during nighttime provides enough inertia to resist minor perturbations of the circadian timing system.
The evening increase in melatonin secretion is associated with an increase in the propensity for sleep [18]. Secretion of melatonin during the day, as occurs in diverse pathologic or occupational health situations, is strongly associated with daytime sleepiness or napping, and the administration of melatonin during the day induces sleepiness [19]. Melatonin (in a dose of 3–5 mg daily, timed to advance the phase of the internal clock) can maintain synchronization of the circadian rhythm to a 24-h cycle in sighted persons who are living in conditions likely to induce a free-running rhythm, and it synchronizes the rhythm in some persons after a short period of free-running. In blind subjects with free-running rhythms, it has been possible to stabilize, or entrain, the sleep–wake cycle to a 24-h period by giving melatonin, with resulting improvements in sleep and mood [20]. In normal aged subjects [21] and in demented patients with desynchronization of sleep–wake cycle [22] melatonin administration is helpful to reduce the variation of onset time of sleep. The phase shifting effects of melatonin were also sufficient to explain its effectiveness as a treatment for circadian-related sleep disorders such as jet lag or the delayed phase sleep syndrome [23–25].
Any transmeridian traveler needs some days to adapt himself/herself to the new situation, unless he/she stays in an environment that is totally isolated from outside and with lights on and off in the way of his usual residence. The time taken to adapt depends on the size of the phase shift and Zeitgeber strength (for example, photoperiod and light intensity), but often approximates to 1–1.5 h of adaptive shift per day, with worsening of symptoms after an eastbound flight as compared to a westbound flight.
With few exceptions, a compelling amount of evidence indicates that melatonin is useful for ameliorating ‘jet-lag’ symptoms in air travelers (see meta-analysis at Cochrane Data Base [26]). We examined the timely use of three factors (melatonin treatment, exposure to light, physical exercise) to hasten the resynchronization of in a group of elite sports competitors after a transmeridian flight comprising 12 time zones [23]. They were professional soccer players and their coaches who traveled from Buenos Aires to Tokyo to play the final game of the Intercontinental Coup. The day prior to departure, urine was collected from each subject from 18:00 to 06:00 h to measure the melatonin metabolite 6-sulphatoxymelatonin. Participants were asked to complete sleep log diaries. All subjects received 3 mg of melatonin p.o. daily at expected bedtime at Tokyo immediately after leaving Buenos Aires. Upon arrival at Tokyo the subjects performed a daily physical exercise routine outdoors at two restricted times of the day (from 08:30 to 11:30 h in the morning and from 15:00 to 18:00 h in the afternoon). Exposure to sunlight or physical exercise at other times of the day was avoided. We employed exposure to outdoors light attempting to cover symmetrically the phase delay and the phase advance portions of the phase–response curve reported for light in humans [27]. Conceivably this would lead to a suppression of circadian rhythmicity and to the sensitization the circadian clock for additional chronobiological manipulation. In addition, we administered non-photic stimulation (i.e., physical exercise) that practically coincided with outdoor light exposure as another manipulation tending to mask the circadian oscillator. Melatonin at local bedtime helped to resynchronize the circadian oscillator to the new time environment.
Individual actograms performed from sleep log data showed that all subjects became synchronized in their sleep to the local time in 24–48 h, well in advance to what would be expected in the absence of any treatment. Assessment of sleep quality by comparison of data before and after the transmeridian flight also indicated absence of significant changes in sleep or vigilance as a consequence of the transmeridian flight. Sleep quality and morning alertness at Tokyo correlated significantly with pre-flight 6-sulphatoxymelatonin excretion, an index of the amplitude of the circadian signal [23].
More recently we performed a retrospective analysis of the data obtained from normal volunteers flying from Buenos Aires to Sydney, or from Sydney to Buenos Aires, by a transpolar route in the last 9 years. Seventy-five volunteers (46 males) were included in the study for the eastbound flight (Buenos Aires–Sydney) (median age: 48 years, range: 21–78 years). Fifty-nine volunteers (34 males) were included in the study for the westbound flight (Sydney–Buenos Aires) (median age: 53 years, range: 32–78 years). Exclusion criteria for the study were: presence of any kind of organic or psychiatric disorder, past history of neurological disorder, alcohol abuse or addiction to other drugs. For the eastbound study, all subjects received a fast release preparation containing 3 mg of melatonin (MelatolR, Elisium S.A., Buenos Aires) p.o. daily 30 min before expected sleeping time at Sydney immediately after leaving Buenos Aires and for the time of the study. Upon arrival at Sydney the subjects were advised to perform their routine normally and to walk outdoors for at least 30 min at two restricted periods of the day (from 08:00 to 11:00 h in the morning and from 13:00 to 16:00 h in the afternoon). They were advised to maintain a symmetrical distribution of activity (i.e., same duration of exercise at both daily times). Exposure to sunlight at other times of the day was reduced by using regular dark sunglasses. Participants were asked to complete sleep log diaries from day −2 (at Buenos Aires) to day 8 at Sydney.
For the westbound study all the volunteers were passengers on the transpolar flight back to Buenos Aires; most of them were continuously taking melatonin as described above for the time they spent at Australia (minimal time: 7 days). On the day of flight to Buenos Aires the subjects received a single dose of 3 mg of melatonin p.o. at about the expected sleeping time at Buenos Aires and they continued with this treatment for 8 days. As in the case of the eastbound study, the volunteers were advised to perform their routine normally at Buenos Aires and to walk outdoors for at least 30 min at two restricted periods of the day (from 08:00 to 11:00 h in the morning and from 13:00 to 16:00 h in the afternoon). Again, they were advised to maintain a symmetrical distribution of activity. Exposure to sunlight at other times of the day was reduced by using dark sunglasses. Participants were asked to complete their sleep log diaries from day −2 (at Sydney) to day 8 at Buenos Aires.
Sleep-log diaries included evaluation of overall quality of sleep, time to bed, time wake, number of awakening episodes and general sleep information. All subjects were asked to assess every day the quality of their sleep, morning freshness and daily alertness graphically on a 10 cm long line rated from 0 to 10 (visual analogic scale). Global assessment of sleep and wakefulness quality was derived from the data. Individual actograms were constructed from sleep log diaries (time to bed, time wake). Phase–shifts were determined by eye fitting. The number of days taken by every individual to reach that line, starting from the first day of the actogram, was computed.
Figure 1 (upper panel) shows the global assessment of sleep and wakefulness after the eastbound flight, recorded from day −2 and −1 (at Buenos Aires), day 0 (day of flight) and days 1–8 at Sydney. A non-parametric ANOVA generally indicated absence of significant changes as compared to pre-flight assessment. Mean resynchronization rate was 2.27±1.1 days. Figure 1 (lower panel) depicts the global assessment of sleep and wakefulness after the westbound flight, recorded from day −2 and −1 (at Sydney), day 0 (day of flight) and days 1–8 at Buenos Aires. A non-parametric ANOVA indicated absence of significant changes as compared to pre-flight assessment. Mean resynchronization rate was 2.54 ± 1.3 days. It should be noted that the expected minimal resynchronization rate after a 13-h flight without any treatment is 7–9 days. Data from Figure 1 indicate that the multifactorial approach (melatonin treatment, exposure to light, physical exercise) previously employed to resynchronize a group of elite soccer players flying west 12 time zones was effective to hasten the resynchronization of air travelers to a 13 time-zone eastbound or westbound transmeridian flights. To what extent other circadian rhythms became synchronized after the treatment employed is not known.
However, since tolerance to jet-lag or shift work are frequently associated with a lack or relatively minor internal desynchronization of circadian rhythms an accelerated resynchronization of other circadian rhythms would be expected.
Chronobiotics are useful to treat chronobiological disorders in demented patients
Alzheimer’s disease (AD) patients show a greater breakdown of the circadian sleep–wake cycle compared to similarly aged, non-demented controls. Demented patients spend their nights in a state of frequent restlessness and their days in a state of frequent sleepiness. These sleep–wake disturbances became increasingly more marked with progression of the disease. The sleep–wake disturbances in elderly people and particularly AD patients may result from changes at different levels: a reduction of environmental synchronizers or their perception, a lack of mental and physical activity, an age or disease related anatomical changes with loss of functionality of the circadian clock. Cross-sectional studies have shown that sleep disturbances are associated with increased memory impairment in AD patients, as well as with more rapid cognitive decline [28]. For these reasons, optimization in management of sleep disturbances is a treatment priority for AD patients.
In AD patients with disturbed sleep–wake rhythms there is a higher degree of irregularities in melatonin secretion [29]. An impairment of melatonin secretion is present that is related to both age and severity of mental impairment. The suppressed nocturnal GH and the increase of both the mean levels and nadir values of plasma cortisol are also related to mental impairments [30]. Shifts in the basic circadian sleep–wake rhythm of dementia patients can be severe, and in extreme cases may lead to complete day–night sleep pattern reversals.
Clinical findings strongly argue in favor of disruption of the circadian timing system in AD [31–33]. Dementia is associated with circadian rhythm disturbances expressed in several dimensions including body temperature, hormonal concentrations and rest–activity cycles. Circadian alterations are detectable at an advanced stage of AD, with large acrophases between rest activity and core body temperature rhythms and reduced rhythm amplitudes and nocturnal rest, indicating a diminished capacity to synchronize body rhythms with behavior. Loss or damage of neurons in the hypothalamic SCN and other parts of the circadian timing system have been implicated in the circadian disturbances of demented patients [34–36]. The SCN of AD patients have tangles [37] indicating that the SCN is affected by AD.
The decreased secretion of melatonin with aging is well documented [38–44] and more profound reductions are reported in populations with dementia [29, 45–49]. Moreover a significantly positive correlation between the abnormalities of rest–activity cycle and decrease in melatonin secretion occurs [42]. An increased melatonin MT1 receptor immunoreactivity signal was reported in the hippocampus of AD patients and was attributed to the up-regulation of the receptor as a compensatory response to impaired melatonin levels [50]. In a recent study melatonin levels were determined in ventricular postmortem cerebrospinal fluid (CSF) of 121 subjects [51]. Melatonin levels were significantly decreased in the aged individuals with early neuropathological changes in the temporal cortex, where the AD process starts. Indeed, the decrease in CSF melatonin levels may be an early event in the development of AD, possibly occurring even before the clinical symptoms [51].
A chronobiological phenomenon in AD related to the sleep disturbances is ‘sundowning’. Symptoms of sundowning agitation include a reduced ability to maintain attention to external stimuli, disorganized thinking and speech, a variety of motor disturbances including agitation, wandering and repetitious physical behaviors, and perceptual and emotional disturbances [52]. The delirium-like symptoms associated with sundowning are usually more prevalent in the late afternoon to early evening. Medication toxicity, infection, electrolytic disturbance or environmental factors can all be triggers for sundowning. A chronobiological approach with bright-light therapy, restricted time in bed and diurnal activity may be an interesting therapeutic alternative in the management of sleep–wake disorders in AD patients. The aim of these therapeutics is to improve sleep and diurnal activity and consequently to increase the quality of life in AD patients [42, 53]. However, there is a very significant risk of retinal damage from repetitious exposure to the high intensities of visible light provided by bright light units in this population since a substantial number of studies have indicated that age related macular degeneration is the result of natural aging processes exacerbated by the cumulative effects of photo-oxidative damage [54, 55].
In a first examination of the sleep-promoting action of melatonin (3 mg p.o. for 21 days) in a small non-homogenous group of elderly patients with primary insomnia and with insomnia associated with dementia or depression, 7 out of 10 dementia patients having sleep disorders and treated with melatonin (3 mg p.o. at bed time) showed a decreased sundowning and reduced variability of sleep onset time [56]. In another study, 10 individuals with mild cognitive impairment were given 6 mg of melatonin before bedtime. Improvement was found in sleep, mood and memory [57].
Other studies include daily administration of 6–9 mg melatonin for longer periods of time to AD patients with sleep disorders and sundowning agitation. The retrospective account of 14 AD patients after a 2–3-year period of treatment with melatonin indicated that all improved sleep quality [58]. Sundowning, diagnosed clinically in all patients examined, was not longer detectable in 12 of them, and persisted attenuated in the other 2 patients. Another significant observation in this study was the halted evolution of the cognitive and mnesic alterations expected in comparable populations of patients not receiving melatonin. This should be contrasted with the significant deterioration of clinical conditions of the disease expected from patients after 1–3 years of evolution of AD. Further support to the hypothesis that melatonin is useful in AD patients was given by a case report study which included two 79 years old male monozygotic twins with AD diagnosed 8 years earlier [59].
The efficacy of melatonin for treatment of AD patients is also supported by other studies. Mishima and co-workers administered a 6 mg dose of melatonin for 4 weeks to 7 inpatients with AD who exhibited irregular sleep–waking cycle [42]. Melatonin significantly reduced percentage of nighttime activity compared to placebo. Cohen-Mansfield et’al. [60] reported the efficacy of melatonin (3 mg/day at bed time) for improving sleep and alleviating sundowning in 11 elderly AD patients. Analysis revealed a significant decrease in agitated behavior and a significant decrease in daytime sleepiness. In an open study using actigraphy to define sleep patterns in 7 AD patients a remarkable effect of a 3 mg dose of melatonin to reduce sundowning was reported [61]. The effect of melatonin was seen regardless of any concomitant medication employed to treat cognitive or behavioral signs of disease as demonstrated in a study including 45 AD patients with sleep disturbances treated for 4 months with 6–9 mg melatonin/day [22].
In a double blind study to examine the effects of melatonin on the sleep–wake rhythm, cognitive and non-cognitive functions in AD type of dementia it was observed that a 3 mg melatonin dose for 4 weeks significantly prolonged actigraphically evaluated sleep time, decreased activity at the night and improved cognitive function [62]. In a multicenter, randomized, placebo-controlled clinical trial of two dose formulations of oral melatonin 157 subjects with AD and nighttime sleep disturbance were randomly assigned to 1 of 3 treatment groups: placebo, 2.5 mg slow-release melatonin, or 10 mg melatonin given daily for 2 months [63]. When sleep was defined by actigraphy, trends for increased nocturnal total sleep time and decreased wake after sleep onset in the melatonin groups were observed. On subjective measures, caregiver ratings of sleep quality showed significant improvement in the 2.5 mg sustained-release melatonin group relative to placebo [63].
The mechanisms accounting for the therapeutic effect of melatonin in AD patients remain unknown. Melatonin treatment promotes mainly non-REM sleep in the elderly [64], and can be beneficial in AD by augmenting the restorative phases of sleep, including the augmented secretion of GH [65] and neurotrophins. In addition, in vitro experiments indicated that melatonin protects neurons against β-amyloid toxicity [66], prevents β-amyloid-induced lipid peroxidation [67] and alters the metabolism of the β-amyloid precursor protein [68]. Animal studies are also indicative of the efficacy of melatonin to prevent β-amyloid toxicity. For example, melatonin had the ability to protect against the circadian changes produced by β-amyloid peptide 25–35 microinjection in SCN of golden hamsters [69]. The demonstration of the direct relationship between melatonin and the biochemical pathology of AD was recently made in a transgenic mouse model of Alzheimer’s amyloidosis by monitoring the effects of administering melatonin on brain levels of β-amyloid abnormal protein nitration and survival of the mice. The administration of melatonin partially inhibited the expected time-dependent elevation of β-amyloid, reduced abnormal nitration of proteins and increased survival in the treated transgenic mice [70].
References
Buijs RM, Van Eden CG, Goncharuk VD, Kalsbeek A (2003) The biological clock tunes the organs of the body: timing by hormones and the autonomic nervous system. J Endocrinol 177:17–26
Hastings MH, Reddy AB, Maywood ES (2003) A clockwork web: circadian timing in brain and periphery, in health and disease. Nat Rev Neurosci 4:649–661
Gachon F, Nagoshi E, Brown SA, Ripperger J, Schibler U (2004) The mammalian circadian timing system: from gene expression to physiology. Chromosoma 113:103–112
Smolensky MH, Haus E (2001) Circadian rhythms and clinical medicine with applications to hypertension. Am J Hypertens 14:280S–290S
Cermakian N, Boivin DB (2003) A molecular perspective of human circadian rhythm disorders. Brain Res Brain Res Rev 42:204–220
Folkard S, Tucker P (2003) Shift work, safety and productivity. Occup Med (Lond) 53:95–101
Knutsson A, Boggild H (2000) Shift work and cardiovascular disease: review of disease mechanisms. Rev Environ Health 15:359–372
Hobson JA, Pace-Schott EF (2002) The cognitive neuroscience of sleep: neuronal systems, consciousness and learning. Nat Rev Neurosci 3:679–693
Pace-Schott EF, Hobson JA (2002) The neurobiology of sleep: genetics, cellular physiology and subcortical networks. Nat Rev Neurosci 3:591–605
Dorrian J, Lamond N, Holmes AL, etal. (2003) The ability to self-monitor performance during a week of simulated night shifts. Sleep 26:871–877
Lamond N, Dorrian J, Roach GD, etal. (2003) The impact of a week of simulated night work on sleep, circadian phase, and performance. Occup Environ Med 60:e13
Dawson D, Armstrong SM (1996) Chronobiotics – drugs that shift rhythms. Pharmacol Ther 69:15–36
Reiter RJ, Tan DX, Burkhardt S, Manchester LC (2001) Melatonin in plants. Nutr Rev 59:286–290
Cardinali DP, Pévet P (1998) Basic aspects of melatonin action. Sleep Med Rev 2:175–190
Kennaway DJ, Wright H (2002) Melatonin and circadian rhythms. Curr Top Med Chem 2:199–209
Lewy AJ, Bauer VK, Ahmed S, etal. (1998) The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 15:71–83
Dubocovich ML, Rivera-Bermudez MA, Gerdin MJ, Masana MI (2003) Molecular pharmacology, regulation and function of mammalian melatonin receptors. Front Biosci 8:D1093–D1108
Lavie P (2001) Sleep–wake as a biological rhythm. Annu Rev Psychol 52:277–303
Zhdanova IV, Wurtman RJ, Regan MM, Taylor JA, Shi JP, Leclair OU (2001) Melatonin treatment for age-related insomnia. J Clin Endocrinol Metab 86:4727–4730
Skene DJ, Lockley SW, Arendt J (1999) Melatonin in circadian sleep disorders in the blind. Biol Signals Recept 8:90–95
Cardinali DP, Gvozdenovich E, etal. (2002) A double blind-placebo controlled study on melatonin efficacy to reduce anxiolytic benzodiazepine use in the elderly. Neuroendocrinol Lett 23:55–60
Cardinali DP, Brusco LI, Liberczuk C, Furio AM (2002) The use of melatonin in Alzheimer’s disease. Neuroendocrinol Lett 23:26–29
Cardinali DP, Bortman GP, Liotta G, etal. (2002) A multifactorial approach employing melatonin to accelerate resynchronization of sleep–wake cycle after a 12 time-zone westerly transmeridian flight in elite soccer athletes. J Pineal Res 32:41–46
Arendt J (2003) Importance and relevance of melatonin to human biological rhythms. J Neuroendocrinol 15:427–431
Beaumont M, Batejat D, Pierard C, etal. (2004) Caffeine or melatonin effects on sleep and sleepiness after rapid eastward transmeridian travel. J Appl Physiol 96:50–58
Herxheimer A, Petrie KJ (2002) Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev CD001520
Lewy AJ, Ahmed S, Sack RL (1996) Phase shifting the human circadian clock using melatonin. Behav Brain Res 73:131–134
McCurry SM, Reynolds CF, Ancoli-Israel S, Teri L, Vitiello MV (2000) Treatment of sleep disturbance in Alzheimer’s disease. Sleep Med Rev 4:603–628
Mishima K, Tozawa T, Satoh K, Matsumoto Y, Hishikawa Y, Okawa M (1999) Melatonin secretion rhythm disorders in patients with senile dementia of Alzheimer’s type with disturbed sleep–waking. Biol Psychiatry 45:417–421
Magri F, Sarra S, Cinchetti W, etal. (2004) Qualitative and quantitative changes of melatonin levels in physiological and pathological aging and in centenarians. J Pineal Res 36:256–261
Hoogendijk WJ, van Someren EJ, Mirmiran M, etal. (1996) Circadian rhythm-related behavioral disturbances and structural hypothalamic changes in Alzheimer’s disease. Int Psychogeriatr 8:245–252
Giubilei F, Patacchioli FR, Antonini G, etal. (2001) Altered circadian cortisol secretion in Alzheimer’s disease: clinical and neuroradiological aspects. J Neurosci Res 66:262–265
Harper DG, Stopa EG, McKee AC, etal. (2001) Differential circadian rhythm disturbances in men with Alzheimer disease and frontotemporal degeneration. Arch Gen Psychiatry 58:353–360
Swabb DF, Fliers E, Partiman TS (1985) The suprachiasmatic nucleus of the human brain in relation to sex, age and senile dementia. Brain Res 342:37–44
van Someren EJW (2000) Circadian rhythms and sleep in human aging. Chronobiol Int 17:233–243
Skene DJ, Swaab DF (2003) Melatonin rhythmicity: effect of age and Alzheimer’s disease. Exp Gerontol 38:199–206
Stopa EG, Volicer L, Kuo-Leblanc V, etal. (1999) Pathologic evaluation of the human suprachiasmatic nucleus in severe dementia. J Neuropathol Exp Neurol 58:29–39
Iguchi H, Kato KI, Ibayashi H (1982) Age-dependent reduction in serum melatonin concentrations in healthy human subjects. J Clin Endocrinol Metab 55:27–29
Dori D, Casale G, Solerte SB, etal. (1994) Chrono-neuroendocrinological aspects of physiological aging and senile dementia. Chronobiologia 21:121–126
Girotti L, Lago M, Ianovsky O, etal. (2000) Low urinary 6-sulphatoxymelatonin levels in patients with coronary artery disease. J Pineal Res 29:138–142
Siegrist C, Benedetti C, Orlando A, etal. (2001) Lack of changes in serum prolactin, FSH, TSH, and estradiol after melatonin treatment in doses that improve sleep and reduce benzodiazepine consumption in sleep-disturbed, middle-aged, and elderly patients. J Pineal Res 30:34–42
Mishima K, Okawa M, Hozumi S, Hishikawa Y (2000) Supplementary administration of artificial bright light and melatonin as potent treatment for disorganized circadian rest–activity and dysfunctional autonomic and neuroendocrine systems in institutionalized demented elderly persons. Chronobiol Int 17:419–432
Luboshitzky R, Shen-Orr Z, Tzischichinsky O, Maldonado M, Herer P, Lavie P (2001) Actigraphic sleep–wake patterns and urinary 6-sulfatoxymelatonin excretion in patients with Alzheimer’s disease. Chronobiol Int 18:513–524
Mishima K, Okawa M, Shimizu T, Hishikawa Y (2001) Diminished melatonin secretion in the elderly caused by insufficient environmental illumination. J Clin Endocrinol Metab 86:129–134
Skene DJ, Vivien-Roels B, Sparks DL, etal. (1990) Daily variation in the concentration of melatonin and 5-methoxytryptophol in the human pineal gland: effect of age and Alzheimer’s disease. Brain Res 528:170–174
Uchida K, Okamoto N, Ohara K, Morita Y (1996) Daily rhythm of serum melatonin in patients with dementia of the degenerate type. Brain Res 717:154–159
Liu RY, Zhou JN, van Heerikhuize J, Hofman MA, Swaab DF (1999) Decreased melatonin levels in postmortem cerebrospinal fluid in relation to aging, Alzheimer’s disease, and apolipoprotein E-epsilon 4/4 genotype. J Clin Endocrinol Metab 84:323–327
Ohashi Y, Okamoto N, Uchida K, Iyo M, Mori N, Morita Y (1999) Daily rhythm of serum melatonin levels and effect of light exposure in patients with dementia of the Alzheimer’s type. Biol Psychiatry 45:1646–1652
Ferrari E, Arcaini A, Gornati R, etal. (2000) Pineal and pituitary–adrenocortical function in physiological aging and in senile dementia. Exp Gerontol 35:1239–1250
Savaskan E, Olivieri G, Meier F, etal. (2002) Increased melatonin 1a-receptor immunoreactivity in the hippocampus of Alzheimer’s disease patients. J Pineal Res 32:59–62
Zhou JN, Liu RY, Kamphorst W, Hofman MA, Swaab DF, (2003) Early neuropathological Alzheimer’s changes in aged individuals are accompanied by decreased cerebrospinal fluid melatonin levels. J Pineal Res 35:125–130
Taylor JL, Friedman L, Sheikh J, Yesavage JA (1997) Assessment and management of “sundowning” phenomena. Semin Clin Neuropsychiatry 2:113–122
McGaffigan S, Bliwise DL (1997) The treatment of sundowning. A selective review of pharmacological and nonpharmacological studies. Drugs Aging 10:10–17
Beatty S, Koh H, Phil M, Henson D, Boulton M (2000) The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol 45:115–134
Hall NF, Gale CR (2002) Prevention of age related macular degeneration. BMJ 325:1–2
Fainstein I, Bonetto A, Brusco LI, Cardinali DP (1997) Effects of melatonin in elderly patients with sleep disturbance. A pilot study. Curr Ther Res 58:990–1000
Jean-Louis G, von Gizycki H, Zizi F (1998) Melatonin effects on sleep, mood, and cognition in elderly with mild cognitive impairment. J Pineal Res 25:177–183
Brusco LI, Marquez M, Cardinali DP (1998) Melatonin treatment stabilizes chronobiologic and cognitive symptoms in Alzheimer’s disease. Neuroendocrinol Lett 19:111–115
Brusco LI, Marquez M, Cardinali DP (1998) Monozygotic twins with Alzheimer’s disease treated with melatonin: case report. J Pineal Res 25:260–263
Cohen-Mansfield J, Garfinkel D, Lipson S (2000) Melatonin for treatment of sundowning in elderly persons with dementia. Arch Gerontol Geriatr 31:65–76
Mahlberg R, Kunz D, Sutej I, Kuhl KP, Hellweg R (2004) Melatonin treatment of day–night rhythm disturbances and sundowning in Alzheimer disease: an open-label pilot study using actigraphy. J Clin Psychopharmacol 24:456–459
Asayama K, Yamadera H, Ito T, Suzuki H, Kudo Y, Endo S (2003) Double blind study of melatonin effects on the sleep–wake rhythm, cognitive and non-cognitive functions in Alzheimer type dementia. J Nippon Med Sch 70:334–341
Singer C, Tractenberg RE, Kaye J, etal. (2003) A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep 26:893–901
Monti JM, Alvarino F, Cardinali D, Savio I, Pintos A (1999) Polysomnographic study of the effect of melatonin on sleep in elderly patients with chronic primary insomnia. Arch Gerontol Geriatr 28:85–98
van Coevorden A, Mockel J, Laurent E, etal. (1991) Neuroendocrine rhythms and sleep in aging men. Am J Physiol 260:E651–E661
Pappolla MA, Sos M, Omar RA, etal. (1997) Melatonin prevents death of neuroblastoma cells exposed to the Alzheimer amyloid peptide. J Neurosci 17:1683–1690
Daniels WM, van Rensburg SJ, van Zyl JM, Taljaard JJ (1998) Melatonin prevents beta-amyloid-induced lipid peroxidation. J Pineal Res 24:78–82
Song W, Lahiri DK (1997) Melatonin alters the metabolism of the beta-amyloid precursor protein in the neuroendocrine cell line PC12. J Mol Neurosci 9:75–92
Furio AM, Cutrera RA, Castillo TV, etal. (2002) Effect of melatonin on changes in locomotor activity rhythm of Syrian hamsters injected with beta amyloid peptide 25–35 in the suprachiasmatic nuclei. Cell Mol Neurobiol 22:699–709
Matsubara E, Bryant-Thomas T, Pacheco QJ, etal. (2003) Melatonin increases survival and inhibits oxidative and amyloid pathology in a transgenic model of Alzheimer’s disease. J Neurochem 85:1101–1108
Acknowledgements
These studies were supported by the University of Buenos Aires (ME 075), the Consejo Nacional de Investigaciones Científicas y Técnicas, Argentina and the Agencia Nacional de Promoción Científica y Tecnológica (PICT 14087), Argentina.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cardinali, D.P., Furio, A.M., Reyes, M.P. et al. The Use of Chronobiotics in the Resynchronization of the Sleep–wake Cycle. Cancer Causes Control 17, 601–609 (2006). https://doi.org/10.1007/s10552-005-9009-2
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-9009-2